Академический Документы
Профессиональный Документы
Культура Документы
Diabetes Drugs
Загружено:
Bilal Haider LashariИсходное описание:
Оригинальное название
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Diabetes Drugs
Загружено:
Bilal Haider LashariАвторское право:
Доступные форматы
Diabetes Mellitus:
Pharmacology and Disease
Management
Michael King, MD
Assistant Professor
Residency Program Director
University of Kentucky
Dept. of Family & Community Medicine
Objectives
1. Compare pharmacologic interventions for
patients with diabetes.
2. Optimize management of diabetes to
decrease potential microvascular and
macrovascular complications.
Therapies
Constantly evolving treatments & evidence
Important to know the type and physiology
of diabetes
Type 1:
Insulin (many types and preparations)
Some new options (pramlintide)
Type 2:
Oral agents and/or insulin/and or new options
Selecting an Oral Agent
Considerations:
Efficacy for glycemic reduction
Mechanism of action
Side effects/contraindications
Associated metabolic changes
Patient adherence
Cost
T2DM Treatments and Decrease in A1C
Drug Class
HbA1c % Decrease
Sulfonylureas
(Glyburide, Glipizde, Glimepiride)
1.0 to 2.0
Meglitinides (Repaglinide, Nateglinide) 0.5 to .5
Biguanides (Metformin) 1.0 to 2.0
Glitazones (Rosiglitazone, Pioglitazone) 0.5 to 1.4
Alpha-Glucosidase Inhib.
(Acarbose, Miglitol)
0.5 to 0.8
Amylin Analogue (Pramlintide) 0.5 to 1.0
Incretin Mimetic (Exenatide) 0.5 to 1.0
DPP-4 Inhib (Sitagliptin) 0.5 to 0.8
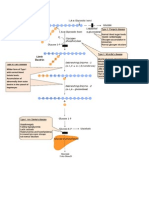
Pathophysiologies and Pharmacotherapy
Mechanisms of Action
Insulin
deficiency
Insulin
Resistance
Excess hepatic
glucose output
Intestinal
glucose
absorption
Sulfonylureas
Meglitinides
Metformin
Glitazones
Alpha-
Glucosidase Inhib.
DPP-4 Inhib.
ADA Algorithm for
Management of Type 2 Diabetes
LESS well-validated therapies after lifestyle and Metformin
Step 2:
Add Pioglitazone (if no hypoglycemia, edema, HF, bone loss)
OR
Add GLP-1 agonist (if no hypoglcemia, weight loss,
nausea/vomiting)
Step 3:
Combination of preferred Sulfonylurea and Pioglitazone (no
GLP-1 agonist) OR
Add basal insulin (no sulfonylurea, pioglitazone, or GLP-1)
Final: Add Intensive Insulin
Diabetes Care, Vol. 32; 2009, 193-203
Insulin Secretagogues
Sulfonylureas: Long acting agents
Second generation: glipizide, glyburide, glimepiride
Cheapest oral medication
Meglitinides: Short acting (<1hr half life)
Repaglinide (Prandin), Nateglinide (Starlix)
Expensive
Combinations
Glyburide/Metformin (Glucovance),
Glipizide/Metfomin (Metaglip),
Rosiglitazone/Glimepiride (Avandaryl),
Pioglitazone/Glimeperide (Duetact)
Sulfonylureas
Little benefit beyond half of max dose
Risks: Hypoglycemia, weight gain
Renal Insufficiency/Failure:
Avoid Glyburide (active metabolites, renally
cleared)
Glipizide (Glucotrol), inactive metabolites, and
glimepiride (bilary/fecal excretion) preferred
Sulfonylureas
Many drug interactions:
action (NSAIDs, warfarin, salicylates, allopurinol,
alcohol, B-blockers)
action (steroids, diuretics, L-thyroxine,
estrogen/progestins)
Decreases Microvascular enpoints, only
trends toward decreasing macrovascular
(UKPDS).
Biguanide: Metformin
Decreases hepatic glucose production (main)
Increased muscle glucose utilization (less
prominent)
Combines well with SU, acarbose, glitazones,
DPP4 inhib or insulin
Preffered Initial Treatment:
Less hypoglycemia, wt loss, enhances lipids,
improves insulin resistence
Improves macrovascular enpoints (UKPDS)
Metformin : Contraindications
Renal insufficiency
Serum CR >1.5 males, >1.4 females
Hepatic insufficiency
CHF
Dehydration
ETOH abuse
Hx of metabolic acidosis
Type I diabetes
Category B in Pregnancy
Metformin: Side Effects and Caveats
Nausea, diarrhea: may be self limited
Lactic acidosis; Identify risk factors
Hold with IV contrast (48 hrs before)
Uncommon to see benefit past 2000mg
per day (max of 2550 mg)
Metformin: New Preparations
Glucovance = metformin + glyburide
Metaglip = metformin + glipizide
Avandamet = metformin + rosiglitazone
Actosplus met = metformin + pioglitazone
Janumet = metformin + januvia
The same precautions apply
Thiazolidendiones
Increases peripheral insulin sensitivity
Activates PPAR (peroxisome proliferator
activated receptor gamma)
Combination therapy with insulin, SU,
metformin (mentioned previously)
Glitazones: General considerations
Do not use if baseline LFTs >3x normal
Can precipitate clinical heart failure so use
cautiously
Contraindicated with NYHA HF Class III-IV
CVD? Black box warning
Glitazones: A Benefit or Harm?
Data is clear to support A1C reduction (disease
surrogate)
No clear difference clinically in other oral hypogylcemic
therapies
No clear evidence to support improved patient oriented
outcomes (mortality, MI, CVA)
Some evidence supports increased CV risk of events,
edema and HF episodes/ hospitalization
Richter,B, et al. Cochrane Database Syst Rev. 2007; (3).
Richter,B, et al. Cochrane Database Syst Rev. 2006; (4).
Nissen, SE, et al. NEJM. 2007;356:2457-71.
Remember Glucagon?
Effects of glucagon in glucose metabolism
and utilization
Suppressing something instead of
increasing something
Homoestasis = sum of the parts
Alpha + Beta = Glucose Control
Glucagon and Insulin
Newer products focus on this physiology:
Amylin analogue, Incretin Mimetic and DPP-4
Inhibitors
Pramlintide (Symlin):
Synthetic Amylin
Amylin:
Produced with insulin (beta cells)
Works with insulin and glucagon to maintain normal blood
glucose
As beta cell function declines, diabetics become Insulin and
Amylin deficient
Effects:
suppress glucagon excretion
control postprandial hyperglycemia
delay gastric emptying, promote satiety
Approved:
Type 1 diabetes, not achieving goal A1C
Type 2 diabetes, using insulin and not at goal.
Pramlintide
SC Injection before meals
Lowers post prandial glucose
Less fluctuation during the day
Less mealtime insulin necessary
Cannot be combined with insulin.
Improves A1C control compared to insulin alone.
Reduction in body weight compared to insulin
alone.
Expensive
Pramlintide: Side Effects
Mainly nausea (Dose dependent)
Hypoglycemia with insulin
Others: fatigue, abd pain
No Cardiac, Hepatic or Renal toxicity
No lipid abnormalities
Medical School Revisited?
Incretins: intestinal hormones released during
eating
GIP: glucose dependent insulino-tropic peptide
GLP1: glucagon-like peptide
~ 60% of post-meal insulin secretion due to
incretins (impaired in T2DM)
Dipeptidyl peptidase-4 enzyme (DPP-4):
inactivates GLP1 and GIP
GLP-1 and Glucose Homeostasis
Enhances glucose dependent insulin
secretion, AND
Suppresses glucagon secretion
Promotes satiety, leading to reduction of
food intake
Regulates the rate of gastric emptying,
limiting postprandial glucose excursions
Incretin Mimetic: Exenatide ( Byetta)
Amino acid sequence partially overlaps that of the
human incretin hormone GLP-1
T2DM, not achieved target A1C levels with metformin,
sulfonylurea, or combination.
Approved in combination with Metformin and
Sulfonylureas
No hypoglycemia unless taken with a sulfonylurea.
Consider decreasing sulfonylurea dose
Exenatide: Caveats
Not an insulin substitute in insulin-requiring
patients
Not for use Type 1 DM or with DKA
Not recommended in patients with end-stage
renal disease or renal impairment (GFR <30), or
severe gastrointestinal disease
Pancreatitis??
Category C in Pregnancy
DPP4 Inhibitors
Sitagliptin (Januvia, 2006) and Saxagliptin
(Onglyza, 2009)
DPP4 inhibitors
Improves A1C, fasting and post-prandial glycemia
Oral Monotherapy, with metformin or a glitazone
Not for Type 1 DM
Recommended doses:
Sitagliptin 100 mg PO QD
Saxagliptin 5 mg PO QD
DPP-4 Inhibitors
Side Effects and Cautions
Adverse reactions was similar to placebo, including
hypoglycemia, some concern of slight increase in upper
respiratory infections
Renal Insufficiency
No renal toxic effects but is efficacious at lower doses
in renal insufficiency and ESRD (even hemodialysis)
Sitagliptin:
50mg: Moderate RI, CrCl <50 but >30 mL/min
(Cr >1.7 in men, >1.5 in women)
25mg: Severe RI, Cr Cl <30 mL/min
(Cr >3.0 in men, >2.5 in women)
Saxagliptin:
2.5 mg daily, Moderate or Severe RI, CrCl 50 mL/min
Insulin: Sometimes a
Necessary Therapy
-cell
function
PLUS
Insulin
Diet
Exercise
PLUS
Oral agents
Normal
Absent
Type 2
PLUS
Combination
oral agents
Type 1
Disease progression (years)
Insulin Therapy
Useful for both type 1 and type 2
Basal bolus
Mimic normal physiology
Know the timing
Basal or longer acting: NPH, glargine
Bolus: regular, lispro, aspart
ADA Algorithm for
Management of Type 2 Diabetes
Well-Validated Core Therapies
Step 1: at Diagnosis
Lifestyle Modification and Metformin
Step 2: Add Basal Insulin OR
Add preferred Sulfonylurea
Not glyburide or chlorpropamide
If fails then stop sulfonylurea and add basal insulin
Step 3: Add Intensive Insulin
Diabetes Care, Vol. 32; 2009, 193-203
Oral Agents + Insulin
Type 2 Diabetes:
Improves glycemic control
Lower doses of exogenous insulin
Addresses multiple causes of
hyperglycemia
Insulin Initiation and Titration
Start q hs NPH or Glargine (10 U or 0.2 U/kg)
Daily BS, 2U q3d until fasting controlled, or 4U q3d if >180
BS <70, 4U or 10%,
whichever is greater
A1C >7, Fasting BS 70-130, then need 2
nd
Injection of Insulin
A1C >7, recheck pre-meal BS, may need 3
rd
Injection of Insulin as above
A1C >7, check 2hr postprandials and adjust preprandial Rapid-Insulin
BS pre-Lunch pre-Dinner pre-Bed
Add 2
nd
Injection
Rapid Insulin
at Breakfast
NPH at Breakfast or
Rapid Insulin at Lunch
Rapid Insulin
at Dinner
1.
2.
3.
4.
5.
Diabetes Care, Vol. 32; 2009, 193-203
Insulins: Basal Therapy
Fasting Control
Insulins Onset Peak Duration
Long-Acting Analogues:
Glargine (Lantus)
Detemir (Levemir)
2-3 hrs
1 hr
None
None
24+ hrs
up to 24 hrs
Intermediate Acting:
NPH
1-3 hrs 4-10 hrs 10-18 hrs
Insulins: Bolus Therapy
Prandial Control
Insulins Onset Peak Duration
Rapid Acting Analogues:
Lispro (Humalog)
Aspart (Novolog)
Glulisine (Apidra)
10-15 mins 1-2 hrs 3-5 hrs
Short Acting:
Regular
0.5-1 hr 2-4 hrs 4-8 hrs
Insulins: Premixed
Prandial Control
Insulins Onset Peak Duration
Humalog Mix 75/25 =
75% Lispro Protamine / 25% lispro
Humalog Mix 50/50 =
50% Lispro Protamine / 50% lispro
Novolog mix 70/30 =
70% Aspart Protamine / 30 % aspart
10-15
mins
1-3 hrs 10-16 hrs
70/30 = 70% NPH / 30% regular
50/50 = 50% NPH / 50% regular
0.5-1 hr 2-10
hrs
10-18 hrs
Summary
Diabetes management is individualized and
involves the patient and a provider-directed team
Establishing tight glycemic control is the key to
management
Lifestyle changes to prevent onset of diabetes
and CVD are the first step
Type 2 diabetes is progressive; management will
likely ultimately require insulin
Providers should employ an aggressive,
treat-to-target strategy
Вам также может понравиться
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryОт EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryРейтинг: 3.5 из 5 звезд3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)От EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Рейтинг: 4.5 из 5 звезд4.5/5 (121)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaОт EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaРейтинг: 4.5 из 5 звезд4.5/5 (266)
- The Little Book of Hygge: Danish Secrets to Happy LivingОт EverandThe Little Book of Hygge: Danish Secrets to Happy LivingРейтинг: 3.5 из 5 звезд3.5/5 (400)
- Never Split the Difference: Negotiating As If Your Life Depended On ItОт EverandNever Split the Difference: Negotiating As If Your Life Depended On ItРейтинг: 4.5 из 5 звезд4.5/5 (838)
- The Emperor of All Maladies: A Biography of CancerОт EverandThe Emperor of All Maladies: A Biography of CancerРейтинг: 4.5 из 5 звезд4.5/5 (271)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeОт EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeРейтинг: 4 из 5 звезд4/5 (5794)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyОт EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyРейтинг: 3.5 из 5 звезд3.5/5 (2259)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersОт EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersРейтинг: 4.5 из 5 звезд4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnОт EverandTeam of Rivals: The Political Genius of Abraham LincolnРейтинг: 4.5 из 5 звезд4.5/5 (234)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreОт EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreРейтинг: 4 из 5 звезд4/5 (1090)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceОт EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceРейтинг: 4 из 5 звезд4/5 (895)
- Neuroplasticity and NeurorehabilitationДокумент164 страницыNeuroplasticity and Neurorehabilitationn0rbertt0% (1)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureОт EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureРейтинг: 4.5 из 5 звезд4.5/5 (474)
- Understanding Fat OxidationДокумент10 страницUnderstanding Fat OxidationPaulo CesarОценок пока нет
- The Unwinding: An Inner History of the New AmericaОт EverandThe Unwinding: An Inner History of the New AmericaРейтинг: 4 из 5 звезд4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)От EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Рейтинг: 4 из 5 звезд4/5 (98)
- CVS Exam (RCT)Документ7 страницCVS Exam (RCT)kenners100% (11)
- Pharma ChartsДокумент33 страницыPharma ChartsNooreen Hussain100% (1)
- Chapter 19 - Cell Junctions and Cell AdhesionДокумент56 страницChapter 19 - Cell Junctions and Cell AdhesionFelix Ezomo100% (1)
- Planning Monitoring Training For Team SportsДокумент52 страницыPlanning Monitoring Training For Team SportsSoccerCTC100% (1)
- HRV Clinical GuideДокумент58 страницHRV Clinical GuidePriscila LucaОценок пока нет
- Urolithiasis - Modified LectureДокумент35 страницUrolithiasis - Modified Lecturemarina_shawkyОценок пока нет
- Cardiac Rehabilitation ProtocolДокумент5 страницCardiac Rehabilitation Protocolmarkhabm100% (1)
- SOAP - Case Study FormatsДокумент8 страницSOAP - Case Study FormatsDr-Sanjay SinghaniaОценок пока нет
- Standards of Medical Care in Diabetes 2015Документ99 страницStandards of Medical Care in Diabetes 2015Juan Carlos Sánchez Suárez100% (1)
- Citing & Referencing Guide: BMJ Vancouver StyleДокумент13 страницCiting & Referencing Guide: BMJ Vancouver StylePaolo Alva PreciadoОценок пока нет
- Abi Wakt Hai Mujhe Chor JaДокумент2 страницыAbi Wakt Hai Mujhe Chor JaBilal Haider LashariОценок пока нет
- Firdaus E Bareen by Abdul Haleem ShararДокумент167 страницFirdaus E Bareen by Abdul Haleem Shararapi-3714708100% (3)
- Iqbal On ExistentialismДокумент135 страницIqbal On ExistentialismBilal Haider LashariОценок пока нет
- Also Pakistan 2Документ25 страницAlso Pakistan 2Bilal Haider LashariОценок пока нет
- Citing & Referencing Guide: BMJ Vancouver StyleДокумент13 страницCiting & Referencing Guide: BMJ Vancouver StylePaolo Alva PreciadoОценок пока нет
- Sayyid Saeed Akhtar Rizvi - God of IslamДокумент144 страницыSayyid Saeed Akhtar Rizvi - God of Islamapi-3820665Оценок пока нет
- Robertsonian TranslocationДокумент1 страницаRobertsonian TranslocationBilal Haider LashariОценок пока нет
- MOA of AntifungalsДокумент1 страницаMOA of AntifungalsBilal Haider LashariОценок пока нет
- Tick Borne DiseaseДокумент2 страницыTick Borne DiseaseBilal Haider LashariОценок пока нет
- Limbic LobeДокумент1 страницаLimbic LobeBilal Haider LashariОценок пока нет
- JVP Pressure Tracing: Opening of AV Valve Closure of AV ValveДокумент1 страницаJVP Pressure Tracing: Opening of AV Valve Closure of AV ValveBilal Haider LashariОценок пока нет
- Sample Hardy-Weinberg Genetics: Hetrezygous Population 49.5%Документ1 страницаSample Hardy-Weinberg Genetics: Hetrezygous Population 49.5%Bilal Haider LashariОценок пока нет
- Citing & Referencing Guide: BMJ Vancouver StyleДокумент13 страницCiting & Referencing Guide: BMJ Vancouver StylePaolo Alva PreciadoОценок пока нет
- Glycogen Storage DiseasesДокумент1 страницаGlycogen Storage DiseasesBilal Haider LashariОценок пока нет
- 6thChapterAcid BasedisorderДокумент5 страниц6thChapterAcid BasedisorderBilal Haider LashariОценок пока нет
- Septic Shock: Stephen Trzeciak, R. Phillip Dellinger, and Joseph E. ParrilloДокумент14 страницSeptic Shock: Stephen Trzeciak, R. Phillip Dellinger, and Joseph E. ParrilloMedranoReyesLuisinОценок пока нет
- Famous People and The Person I Admire The MostДокумент2 страницыFamous People and The Person I Admire The MostdinhmailausОценок пока нет
- Nursing TheoriesДокумент15 страницNursing TheoriesPatrick Rivera Oca100% (1)
- Neet Pyq Cell - The Unit of LifeДокумент4 страницыNeet Pyq Cell - The Unit of LifeAyush DuttaОценок пока нет
- Qrs Complexes: Fast & Easy Ecgs - A Self-Paced Learning ProgramДокумент49 страницQrs Complexes: Fast & Easy Ecgs - A Self-Paced Learning ProgramMuhammad Hatta HamzahОценок пока нет
- BT1001 Biology For Engineers PDFДокумент2 страницыBT1001 Biology For Engineers PDFsanthi saranyaОценок пока нет
- Ethanol Injection Method Liposomes PDFДокумент2 страницыEthanol Injection Method Liposomes PDFElizabeth100% (1)
- Animal's Circulartory System.Документ2 страницыAnimal's Circulartory System.CHANON KIATKAWINWONGОценок пока нет
- Anaphy Lab - Activity in Cell and MicroscopeДокумент5 страницAnaphy Lab - Activity in Cell and MicroscopeAlvin Cris RongavillaОценок пока нет
- Forces in BodyДокумент48 страницForces in Bodytema_racamaОценок пока нет
- Unit 4 Introduction To Bones and The SkullДокумент22 страницыUnit 4 Introduction To Bones and The SkullrynОценок пока нет
- Bacterial Decolorization and Degradation of Azo DyesДокумент12 страницBacterial Decolorization and Degradation of Azo DyesFernanda Stuani PereiraОценок пока нет
- Jurnal 11Документ14 страницJurnal 11Zulvi RiriОценок пока нет
- 100-Day Contract With Dairy CowДокумент22 страницы100-Day Contract With Dairy CowMarjorie SalgadoОценок пока нет
- 2.2 Drug Absorption From The GITДокумент15 страниц2.2 Drug Absorption From The GITCari MosehuusОценок пока нет
- Qatar - Blueprint and Reference (Dec 2016)Документ7 страницQatar - Blueprint and Reference (Dec 2016)Jashim Jumli IIОценок пока нет
- CiticolineДокумент8 страницCiticolineadityaОценок пока нет
- Human Evolution 4Документ5 страницHuman Evolution 4Sanket PatilОценок пока нет
- Role of Jalauka in Diabetic Foot UlcerДокумент12 страницRole of Jalauka in Diabetic Foot UlcerMinakshi Gulshan SharmaОценок пока нет
- Organization of Living BeingsДокумент6 страницOrganization of Living BeingsSanhitha RameshОценок пока нет
- Effects of Soaking On Yield and Quality of Agarwood OilДокумент8 страницEffects of Soaking On Yield and Quality of Agarwood OilNilamdeen Mohamed ZamilОценок пока нет
- Spinal Cord Injury NotesДокумент13 страницSpinal Cord Injury Notescorememories10Оценок пока нет