Академический Документы
Профессиональный Документы
Культура Документы
Pneumoniae, Was The First Acute-Phase Protein To Be Described and Is An Exquisitely
Загружено:
Labontu Iustina0 оценок0% нашли этот документ полезным (0 голосов)
90 просмотров11 страницCrp
Оригинальное название
Crp
Авторское право
© © All Rights Reserved
Доступные форматы
DOCX, PDF, TXT или читайте онлайн в Scribd
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документCrp
Авторское право:
© All Rights Reserved
Доступные форматы
Скачайте в формате DOCX, PDF, TXT или читайте онлайн в Scribd
0 оценок0% нашли этот документ полезным (0 голосов)
90 просмотров11 страницPneumoniae, Was The First Acute-Phase Protein To Be Described and Is An Exquisitely
Загружено:
Labontu IustinaCrp
Авторское право:
© All Rights Reserved
Доступные форматы
Скачайте в формате DOCX, PDF, TXT или читайте онлайн в Scribd
Вы находитесь на странице: 1из 11
CRP, named for its capacity to precipitate the somatic C-polysaccharide of Streptococcus
pneumoniae, was the first acute-phase protein to be described and is an exquisitely
sensitive systemic marker of inflammation and tissue damage (1). The acute-phase
response comprises the nonspecific physiological and biochemical responses of endothermic
animals to most forms of tissue damage, infection, inflammation, and malignant neoplasia.
In particular, the synthesis of a number of proteins is rapidly upregulated, principally in
hepatocytes, under the control of cytokines originating at the site of pathology. Other acute-
phase proteins include proteinase inhibitors and coagulation, complement, and transport
proteins, but the only molecule that displays sensitivity, response speed, and dynamic range
comparable to those of CRP is serum amyloid A protein (SAA) (Table 1) (1).
Plasma CRP is produced only by hepatocytes, predominantly under transcriptional control
by the cytokine IL-6, although other sites of local CRP synthesis and possibly secretion have
been suggested. De novo hepatic synthesis starts very rapidly after a single stimulus, serum
concentrations rising above 5 mg/l by about 6 hours and peaking around 48 hours. The
plasma half-life of CRP is about 19 hours and is constant under all conditions of health and
disease, so that the sole determinant of circulating CRP concentration is the synthesis rate
(3), which thus directly reflects the intensity of the pathological process(es) stimulating CRP
production. When the stimulus for increased production completely ceases, the circulating
CRP concentration falls rapidly, at almost the rate of plasma CRP clearance. In unselected
general populations of ostensibly healthy subjects, the median CRP value is slightly higher
than among blood donors and tends to increase with age, presumably reflecting the
increasing incidence of subclinical pathologies (4). However, surprisingly in view of the
sensitivity, speed, and range of the CRP response, subjects in the general population tend
to have stable CRP concentrations characteristic for each individual, apart from occasional
spikes presumably related to minor or subclinical infections, inflammation, or trauma.
Importantly, acute-phase CRP values show no diurnal variation and are unaffected by
eating. Liver failure impairs CRP production, but no other intercurrent pathologies and very
few drugs reduce CRP values unless they also affect the underlying pathology providing the
acute-phase stimulus. The CRP concentration is thus a very useful nonspecific biochemical
marker of inflammation, measurement of which contributes importantly to (a) screening for
organic disease, (b) monitoring of the response to treatment of inflammation and infection,
and (c) detection of intercurrent infection in immunocompromised individuals, and in the
few specific diseases characterized by modest or absent acute-phase responses (Table 3)
(1). It is not known why systemic lupus erythematosus and the other conditions listed with
it in Table 2 fail to elicit major CRP production despite evident inflammation and tissue
damage, nor why the CRP responses to intercurrent infection are apparently intact in
patients with such conditions.
CRP belongs to the pentraxin family of calcium-dependent ligand-binding plasma
proteins, the other member of which in humans is serum amyloid P component
(SAP). The human CRP molecule (Mr115,135) is composed of five identical
nonglycosylated polypeptide subunits (Mr 23,027), each containing 206 amino
acid residues. The protomers are noncovalently associated in an annular
configuration with cyclic pentameric symmetry (6) (Figure 1). Each protomer has
the characteristic "lectin fold," composed of a two-layered sheet with flattened
jellyroll topology.
http://www.jci.org/articles/view/18921#SEC1
C-reactive protein
Email this page to a friendShare on facebookShare on twitterBookmark & SharePrinter-friendly version
C-reactive protein is produced by the liver. The level of CRP rises when there is inflammation throughout the body.
This article discusses the blood test done to measure the amount of CRP in your blood.
How the Test is Performed
A blood sample is needed. This is usually taken from a vein. The procedure is called a venipuncture.
How to Prepare for the Test
No preparation is necessary for this test.
How the Test Will Feel
When the needle is inserted to draw blood, some people feel moderate pain, while others feel only a prick or stinging
sensation. Afterward, there may be some throbbing.
Why the Test is Performed
The CRP test is a general test to check for inflammation in the body. It is not a specific test. That means it can reveal
that you have inflammation somewhere in your body, but it cannot pinpoint the exact location.
Your doctor may order this test to:
Check for flare-ups of inflammatory diseases such as rheumatoid arthritis, lupus, or vasculitis
Determine if anti-inflammatory medicine is working to treat a disease or condition
However, a low CRP level does not always mean that there is no inflammation present. Levels of CRP may not be
increased in people with rheumatoid arthritis and lupus. The reason for this is unknown.
A more sensitive CRP test, called a high-sensitivity C-reactive protein (hs-CRP) assay, is available to determine a
person's risk for heart disease. Many consider a high CRP level to be a risk factor for heart disease. However, it is not
known whether CRP is merely a sign of cardiovascular disease or if it actually plays a role in causing heart problems.
Normal Results
Normal CRP values vary from lab to lab. Generally, there is no CRP detectable in the blood.
Your doctor may also use a highly sensitive test called hs-CRP to help determine your risk of heart disease.
According to the American Heart Association:
You are at low risk of developing cardiovascular disease if your hs-CRP level is lower than 1.0mg/L
You are at average risk of developing cardiovascular disease if your levels are between 1.0 and 3.0 mg/L
You are at high risk for cardiovascular disease if your hs-CRP level is higher than 3.0 mg/L
Note: Normal value ranges may vary slightly among different laboratories. Talk to your doctor about the meaning of
your specific test results.
The examples above show the common measurements for results for these tests. Some laboratories use different
measurements or may test different specimens.
What Abnormal Results Mean
A positive test means you have inflammation in the body. This may be due to a variety of different conditions,
including:
Cancer
Connective tissue disease
Heart attack
Infection
Inflammatory bowel disease (IBD)
Lupus
Pneumococcal pneumonia
Rheumatoid arthritis
Rheumatic fever
Tuberculosis
This list is not all inclusive.
Note: Positive CRP results also occur during the last half of pregnancy or with the use of birth control pills (oral
contraceptives).
Risks
Veins and arteries vary in size from one patient to another and from one side of the body to the other. Obtaining a
blood sample from some people may be more difficult than from others.
Other risks associated with having blood drawn are slight but may include:
Excessive bleeding
Fainting or feeling light-headed
Hematoma (blood accumulating under the skin)
Infection (a slight risk any time the skin is broken)
Alternative Names
CRP; High-sensitivity C-reactive protein; hs-CRP
http://www.nlm.nih.gov/medlineplus/ency/article/003356.htm
13.0 C-Reactive Protein
The main biologic sign of inflammation is an increase in the
erythrocyte sedimentation rate (ESR). In addition an increase
in plasma concentrations of a group of proteins known as
acute-phase proteins is a good indicator of local inflammatory
activities and tissue damage. The acute phase proteins
include C-reactive protein (CRP), inflammatory mediators
(e.g. complement components c3 and c4, fibrinogen, etc.
CRP is prominent among the acute-phase proteins because it
provides fast and adequate information of the actual clinical
situation; as a result CRP is a direct and quantitative measure
of the acute-phase reactions.
Measures of CRP add to the diagnostic procedure in selected
cases (e-g. in the differentiation between a bacterial and a
viral infection). An extremely elevated CRP is suggestive of a
possible bacterial infection. The CRP level may be useful also
for monitoring the effect of treatment and for early detection of
postoperative complications or intercurrent infections. The
CRP is a parameter for inflammatory activity.
CRP is a method of choice for screening for inflammatory and
malignant diseases and monitoring therapy in inflammatory
disease. Elevations of CRP occur in nearly to diseases states,
including bacterial infection, viral infections, myocardial
infraction specificity rules out CRP as a definitive diagnostic
tool.
CRP levels rise following the tissue injury or surgery. In
uncomplicated cases the level of CRP peaks about 2 days
postoperatively and gradually returns to normal levels within 7
to 10 days. CRP is synthesized more rapidly than other acute
Tests for CRP
Rapid latex agglutination test
Principle: The test is based on the reaction between patient
serum containing CRP as the antigen & the corresponding
antibody coated to the treated surface of latex particle. The
coated particles enhance the detection of an agglutinate
reaction when antigen is present in the serum being tested.
Specimen- Serum
Reagent & materials required
CRP latex reagent
Glycine saline buffer
Capillary pipette
Applicator sticks
Glass slide
Serologic pipettes & rubber bulb
Reporting
Positive reaction agglutination
Negative reaction absence of agglutination
http://www.cartercenter.org/resources/pdfs/health/ephti/library/lecture_notes/med_lab_tech_students/LN_I
mm_Serology_final.pdf
CRP is an extremely sensitive, nonspecific, acute-phase reactant produced in response to most forms of
tissue injury, infection, and inflammation and regulated by cytokines, including interleukin-6, interleukin-
1, and tumor necrosis factor-.
38
Although reportedly expressed by some mononuclear populations, these
cells do not secrete CRP, and circulating CRP is exclusively produced by hepatocytes.
3940
The stimuli
responsible for the generally modest elevations in plasma CRP predictively associated with coronary events
are not known. They may arise in the atheromatous lesions themselves and reflect the extent of
atherosclerosis and the local inflammation that predisposes to plaque instability, rupture, and occlusive
thrombosis. On the other hand, increased CRP production may result from inflammation elsewhere in the
body that is somehow proatherogenic and procoagulant. Chronic low-grade infections may be associated
with increased risk of CHD,
41
42
as is the chronic inflammation of rheumatoid arthritis.
43
Many coagulation
proteins, including fibrinogen, are acute-phase reactants; elevation of fibrinogen is a well-recognized risk
factor for coronary events,
4
and increased CRP values may just be a signal of the acute-phase response in
general.
However, there is substantial evidence that CRP may contribute directly to the pathogenesis of
atherothrombosis. CRP is a ligand binding protein that binds to the plasma membranes of damaged
cells.
44
45
Aggregated but not soluble native CRP selectively binds LDL and VLDL from whole plasma and, as
we have previously proposed, could thereby participate in their atherogenic accumulation.
46
Complexed
CRP also activates complement and can be proinflammatory,
47
whereas CRP has recently been found to be a
potent stimulator of tissue factor production by macrophages in vitro.
48
Tissue factor is the main initiator
of coagulation in vivo, and its local concentration in the arterial wall is clearly related to coronary
thrombotic events.
49
50
51
There are conflicting reports about the presence of CRP in atheromatous
lesions,
52
53
54
and claims that CRP affects platelet function are also controversial.
55
However, the capacity of
CRP to enhance tissue factor production suggests a possible causative link between increased CRP values
and coronary events.
Although the number of cases was relatively small, results of the present prospective study of a large
cohort of initially healthy middle-aged men indicate that modest elevations in serum CRP concentration
significantly predict future coronary events. These observations strengthen the association between low-
grade inflammation and the progression and complications of atherosclerosis. Further work is required to
clarify the underlying pathophysiological mechanisms, but modulation of the acute-phase response
generally and/or the functions of specific acute-phase proteins specifically, especially CRP, already
constitutes novel potential therapeutic https://circ.ahajournals.org/content/99/2/237.fullc targets in
CHD.
The Role of C-Reactive Protein
M. Saljoughian, PharmD, PhD
Department of Pharmacy Services
Alta Bates Summit Medical Center
Berkeley, California
7/18/2008
US Pharm. 2008;33(7):HS12-HS15.
The human body responds to injury and infection by a process called inflammation. During an inflammatory process
in the body, the levels of C-reactive protein (CRP), a pro-inflammatory cytokine, rise dramatically. It has been
suggested that testing CRP levels in the blood may be an additional way to assess cardiovascular disease risk.
Laboratory findings from clinical and research studies also suggest that inflammation is an important factor in
atherosclerosis. This is the process in which fatty deposits build up in the inner lining of arteries.
1
The American Heart Association and the Centers for Disease Control and Prevention published a joint scientific
statement in 2003 on the use of inflammatory markers in clinical and public health practice.
2
This statement was
developed after systematically reviewing the evidence of association between inflammatory markers (mainly CRP)
and coronary heart disease and stroke. A more sensitive CRP test, called a high-sensitivity C-reactive protein (hs-
CRP) assay, is available to determine heart disease risk more accurately.
1
In 1930, Tillett and Francis originally discovered CRP as a substance in the serum of patients with acute inflammation
that reacted with the C-polysaccharide of pneumococcus. Initially, it was thought that CRP might have a pathogenic
role, as it was elevated in people with a variety of illnesses, but discovery of its hepatic synthesis and secretion
closed that debate. Measuring and charting CRP values can prove useful in determining disease progression or the
effectiveness of treatments. CRP is used mainly as a marker of inflammation.
3
Various analytic methods are available for CRP determination, such as enzyme-linked immunosorbent assay
(ELISA), immunoturbidimetry, rapid immunodiffusion, and visual agglutination. In general, both the CRP test and
another test, called the erythrocyte sedimentation rate (ESR), measure the increase in inflammatory generated
proteins. The CRP test is a direct measurement of C-reactive protein, while ESR indirectly measures many proteins
associated with inflammation.
1
Causes of Inflammation
There are many conditions that cause inflammation. Genetics play a role, as does the environment. Environmental
factors include diet, exposure to toxins, germs, pollutants, and inhalants. Some people have a genetic predisposition
to increased inflammation, which can cause them to develop an illness such as rheumatoid arthritis.
4,5
Acute inflammation is a complex biological response of vascular tissues to harmful stimuli, such as pathogens,
damaged cells, or irritants. It is a protective attempt by the body to remove the injurious stimuli as well as to initiate
the healing process for the tissue. Chronic inflammation is a pathologic condition characterized by concurrent active
inflammation, tissue degeneration, and attempts at repair. Chronic inflammation is not characterized by the classic
signs of acute inflammation (i.e., swelling, redness, pain, heat, loss of function). Instead, chronically inflamed tissue is
characterized by the infiltration of mononuclear immune cells (i.e., monocytes, macrophages, lymphocytes, plasma
cells) and tissue destruction, which include angiogenesis and fibrosis.
Cigarette smoking, hypertension, atherogenic lipoproteins, and hyperglycemia are well-established promoting factors
in atherogenesis. These risk factors give rise to a variety of noxious stimuli that cause the release of certain
chemicals and the activation of cells involved in the inflammatory process. These events are thought to contribute not
only to the formation of plaque but may also contribute to its disruption, resulting in the formation of a blood clot.
Thus, virtually every step in atherogenesis is believed to involve substances involved in the inflammatory response
and cells that are characteristic of inflammation.
6
In addition, there is research that indicates that an infection--possibly one caused by a bacterium or a virus--might
contribute to or even cause atherosclerosis.
7
The infectious bacterium Chlamydia pneumoniae has been shown to
have a role in atherosclerotic plaque. The herpes simplex virus has also been proposed as an initial inflammatory
infectious agent in atherosclerosis. Viral infections tend to give a lower CRP level than bacterial infection. Bacterial
infection with Helicobacter pylori is now known to be the major cause of inflammatory stomach lesions. The treatment
for this condition routinely includes antibiotic therapy.
In diseases such as allergies, anemia, arthritis, fibromyalgia, fibrosis, heart attack, aortic valve stenosis, kidney
failure, lupus, pancreatitis, and psoriasis, the levels of inflammatory cytokines are elevated, which induces damage to
the tissues. In surgical complications, the inflammatory cytokines prevent healing.
CRP and New Cardiovascular Events
Scientific studies have found that the higher the hs-CRP levels, the higher the risk of having a heart attack. In fact,
the risk for heart attack in people with high hs-CRP levels has been determined to be twice that of those whose hs-
CRP levels are lower. These prospective studies included men, women, and the elderly. Studies have also found an
association between sudden cardiac death, peripheral arterial disease, and high hs-CRP levels. However, not all of
the established cardiovascular risk factors were controlled for when the association was examined. The true
independent association between hs-CRP and new cardiovascular events has yet to be established.
8
CRP and Recurrent Events
A growing number of studies have examined whether high hs-CRP levels can predict recurrent cardiovascular
disease, stroke, and death in different settings. High levels of hs-CRP consistently predict recurrent coronary events
in patients with unstable angina and acute myocardial infarction (heart attack). Higher hs-CRP levels also are
associated with lower survival rates in these patients. Many studies have suggested that after adjusting for other
prognostic factors, hs-CRP is useful as a risk predictor.
8
Studies also suggest that higher levels of hs-CRP may increase the risk that an artery will reclose after it has been
opened by balloon angioplasty. High levels of hs-CRP in the blood also seem to predict prognosis and recurrent
events in patients with stroke or peripheral arterial disease. CRP inhibition can be a safe and effective therapy for
myocardial and cerebral infarctions.
8
When to Measure CRP
If a person's cardiovascular risk factors (i.e., smoking, hypertension, high blood cholesterol, diabetes, being
overweight or obese, physical inactivity) are low, the possibility of developing cardiovascular disease is less than 10%
in 10 years, and no test is immediately warranted. If the risk factors are in the intermediate range, the possibility is
10% to 20% in 10 years, and such a test can help predict a cardiovascular or stroke event as well as help direct
further evaluation and therapy. However, the benefits of therapy based on this strategy remain uncertain. A person
with a high-risk score (>20% in 10 years) or established heart disease or stroke should be treated intensively
regardless of hs-CRP levels.
9
Diagnostic Criteria
As previously mentioned, CRP is used mainly as a marker of inflammation. Measuring and charting CRP values can
prove useful in determining cardiovascular and noncardiovascular disease progress or the effectiveness of
treatments. Blood samples are analyzed in a medical laboratory or at the point of testing. Patients who are scheduled
for a CRP test will be asked not to eat or drink anything for 12 hours before the test.
The ranges for evaluating hs-CRP levels are given in Table 1. If, after repeated testing, patients have persistently
unexplained, markedly elevated hs-CRP levels (>10.0 mg/L), they should be evaluated to exclude noncardiovascular
causes. Patients with autoimmune diseases or cancer, as well as other infectious diseases, may also have elevated
CRP levels.
10
Mode of Action
The CRP gene is located on the first chromosome and is a 224-residue protein with a monomer molar mass of 25106
dalton. The protein is an annular pentameric disk in shape. Proteins with this type of configuration are known
as pentraxins. CRP binds to phosphorylcholine on microbes. It is thought to assist in complement binding to foreign
and damaged cells, and it enhances phagocytosis by macrophages, which express a receptor for CRP. It is also
believed to play an important role in innate immunity, as an early defense system against infections.
11
Arterial damage is thought to result from inflammation due to chemical insults. CRP can be used as a marker for the
extent of this damage, but by itself it is not a specific prognostic indicator. Clinicians only look at the CRP values with
prolonged elevation, so a single measurement would be meaningless.
In different disease states, one or two amino acids get "lopped off" CRP. It retains its activity, but these losses open it
up to glycosylation, and it may have sugars such as glucose, galactose, and mannose attached to it. The patterns of
glycosylation vary in different diseases, but are similar among patients who have the same disease. Previous work
has shown that CRP increased the rate at which a particular parasite could invade blood cells.
12
The study showed
that the various CRPs had very different potencies in this regard. The authors speculate that subtyping CRP may give
us more insight into heart attack mechanisms. Although the study did not demonstrate whether this glycosylation of
CRP was a "good" or a "bad" thing, it offered circumstantial evidence that the differing glycosylation is part of CRP's
mode of action.
12
The Role of CRP in Cancer
The role of inflammation in cancer is well known. Some organs of the body show greater risk of cancer when they are
chronically inflamed. Blood samples of persons with colon cancer have an average CRP concentration of 2.69 mg/L.
Persons without colon cancer average 1.97 mg/L. The difference was statistically significant (P <.001).
13
These
findings concur with previous studies that indicated that anti-inflammatory drugs could lower colon cancer risk.
14
Pharmacist Recommendation
It is important for patients to make lifestyle changes to reduce their risk for cardiovascular disease, especially if the
CRP level is intermediate or high (Table 2).
15
For those with an elevated CRP level, taking aspirin may provide
protection from cardiovascular disease. Statins, the most commonly prescribed drugs for lowering cholesterol, may
also reduce CRP levels. Clinicians should prescribe the correct medications and dosage to treat the disease
condition.
http://www.uspharmacist.com/content/c/10944/?t=men's_health,cardiovascular_disease
Elevated C-reactive Protein (CRP)
What is elevated C-reactive protein?
C-reactive protein (CRP) is a substance produced by the liver that increases in the presence of inflammation in the body. An
elevated CRP level is identified with blood tests and is considered a non-specific "marker" for disease. Data from a large number of
studies suggest that over time chronic, imperceptible, low-level internal inflammation can lead to many serious, age-related diseases
including heart disease, some forms of cancer and neurodegenerative conditions such asAlzheimer's and Parkinson's disease.
However, CRP levels don't appear to help predict the risk of heart disease in patients already being treated for risks such as high
blood pressure or high LDL ("bad") cholesterol. A 2010 analysis of British data on 4,853 patients found that CRP levels didn't yield
any more information about the risk of heart disease than LDL ("bad") cholesterol levels or high blood pressure in patients who
already were being treated with a cholesterol-lowering statin drug or with medication to lower blood pressure.
For those reasons, the researchers concluded that measuring CRP in patients with other known risk factors for heart disease may
not be necessary. These results, presented at a 2010 American Heart Association meeting and later published in the European
Heart Journal, conflict with findings from an earlier study with more than 17,000 patients which showed that treating elevated CRP
with statin drugs reduced cardiovascular events by 37 percent in healthy individuals whose only risk factor for heart disease was
elevated CRP. This earlier study called JUPITER (Justification for the Use of Statins in Prevention: an Intervention Trial Evaluating
Rosuvastatin) found that patients taking the drug rosuvastain were half as likely to need angioplasty or bypass surgery, half as likely
to suffer a heart attack or stroke, and 20 percent less likely to die than study participants who received the placebo. That study was
published in 2008 in The New England Journal of Medicine.
What are the symptoms of elevated C-reactive protein?
Elevated CRP levels have no outward, noticeable symptoms.
What are the causes of elevated C-reactive protein?
The inflammation signaled by CRP is influenced by genetics, a sedentary lifestyle, too much stress, and exposure to environmental
toxins such as secondhand tobacco smoke. Diet has a huge impact, particularly one that contains a lot of refined, processed and
manufactured foods.
How is elevated C-reactive protein diagnosed?
CRP levels can be measured via a blood test. In evaluating cardiac risk, physicians look at a very narrow range of CRP levels, from
zero to 3.0 and above. This requires a special test called high sensitivity CRP (hs-CRP), which may be able to reveal inflammation
at the micro-vascular level. If this test shows that CRP is less than 1.0 mg per liter of blood, the risk of heart disease is considered
low; if it is between 1.0 and 3.0, the risk is average; if it is above 3.0, the risk is deemed high.
The American Heart Association (AHA) recommends CRP testing when doctors aren't sure how to treat patients with an
intermediate risk of heart disease, such as a 10-20 percent risk of having a heart attack in the next 10 years However, AHA
guidelines do not recommend CRP testing for individuals at either high risk of low risk. (Other physicians, including Dr. Weil, think
that all adults should have an hs-CRP test whenever their cholesterol is tested.)
There are two tests for CRP. One can show a non-specific elevation of CRP that occurs with general inflammatory changes in the
body; the other test is hs-CRP - highly sensitive CRP - which is a measure of inflammation in blood vessels. This is the test needed
to help establish heart disease risk.
People who have arthritic conditions tend to have high CRP levels because inflammation underlies these disorders. Arthritis may
push test results far beyond the range used to assess heart disease risk. When inflammation levels are being assessed in patients
with rheumatoid arthritis, inflammatory bowel disease or other autoimmune conditions, the hs-CRP test is not used. Instead,
inflammation is evaluated with a test that measures levels in excess of 10 mg/L. With most active infections and inflammatory
processes, CRP levels are above 100 mg/L. Under these circumstances, the CRP test is used to follow the trend. Declining CRP
levels are a sign that inflammation is decreasing. When checking CRP for arthritic and autoimmune disorders, a level of 10 mg/L or
lower is considered "normal."
Because an hs-CRP test isn't useful to assess cardiovascular risk among people with inflammatory diseases, these patients have to
rely on such well-recognized risk factors as high blood pressure or high cholesterol, whether or not they smoke, their weight and
their risk of diabetes. In addition to such standard measures for reducing the risk of cardiovascular disease as exercise, keeping
weight under control, practicing stress reduction techniques and getting adequate sleep, Dr. Weil recommends that people with
these disorders make an effort to reduce inflammation and their risk of heart disease by following an anti-inflammatory diet.
What is the conventional treatment of elevated C-reactive protein?
Conventional physicians may prescribe the same (statin) drugs used to lower LDL cholesterol to also lower levels of C-reactive
protein. In addition, they will typically recommend exercise and weight loss where appropriate, since both can help lower CRP. In
general, conventional physicians recommend the same lifestyle changes shown to reduce heart disease - diet, exercise, not
smoking, drinking less alcohol, following a heart-healthy diet - to lower levels of CRP.
What therapies does Dr. Weil recommend for elevated C-reactive protein?
Dr. Weil recommends an anti-inflammatory diet that includes two to three servings of fish such as salmon or sardines per week. If
you don't eat fish, he suggests taking fish oil supplements. He also recommends taking anti-inflammatory herbs including ginger
andturmeric and following your doctor's recommendations for heart health - quit smoking, watch your diet (particularly avoid foods
that predominantly consist of flour and/or sugar), and get regular exercise. A recent study at Johns Hopkins showed that as fitness
levels decline, CRP levels go up. The researchers weren't sure if poor fitness leads to an increase in CRP or vice versa, but
exercise is an important part of maintaining heart health in any case. http://www.drweil.com/drw/u/ART03424/Elevated-Creactive-
Protein-CRP.html
Вам также может понравиться
- Sepsis Diagnosis and Monitoring: Fast Early ReliableДокумент24 страницыSepsis Diagnosis and Monitoring: Fast Early ReliableI Nyoman Gede Semarajana100% (1)
- Biology of C Reactive Protein in Health and Disease PDFДокумент324 страницыBiology of C Reactive Protein in Health and Disease PDFdanielleeОценок пока нет
- Laboratory Diagnosis of Hypersensitivity and AutoimmunityДокумент41 страницаLaboratory Diagnosis of Hypersensitivity and AutoimmunityDenish Calmax AngolОценок пока нет
- EsrДокумент5 страницEsraftab ahmadОценок пока нет
- A Methodical Approach To Interpreting The Platelet Parameters of The Complete Blood CountДокумент11 страницA Methodical Approach To Interpreting The Platelet Parameters of The Complete Blood CountAlex YohanaОценок пока нет
- Krvlju Prenosive Bolesti Hematogene Transmisivne Bolesti 2017Документ121 страницаKrvlju Prenosive Bolesti Hematogene Transmisivne Bolesti 2017Jankovic NatasaОценок пока нет
- MEDICINSKA STATISTIKA I INFORMATIKAДокумент18 страницMEDICINSKA STATISTIKA I INFORMATIKADragutin DikovicОценок пока нет
- VDRL Test and Its InterpretationДокумент11 страницVDRL Test and Its InterpretationSauZen SalaZarОценок пока нет
- Systemic Lupus ErythematosusДокумент40 страницSystemic Lupus ErythematosusAkshan SentinelОценок пока нет
- HIV Disease and NutritionДокумент10 страницHIV Disease and Nutritionmariosan81Оценок пока нет
- Funkcija BubregaДокумент7 страницFunkcija BubregaMilica TrkuljaОценок пока нет
- Measure CRP Levels with Latex TurbidimetryДокумент2 страницыMeasure CRP Levels with Latex TurbidimetryDharmesh Patel100% (1)
- Cytokines & Their ActionsДокумент59 страницCytokines & Their ActionsSharanabasappa DurgОценок пока нет
- Diseases of the Immune System ExplainedДокумент55 страницDiseases of the Immune System ExplainedMeera ANN AJIОценок пока нет
- Approved Nigerian National Blood PolicyДокумент24 страницыApproved Nigerian National Blood PolicyUkaegbu Chibueze JnrОценок пока нет
- Nucleic Acid TestingДокумент55 страницNucleic Acid TestingShaiji ShahidОценок пока нет
- Cerebrospinal Fluid CSF Analysis and InterpretatioДокумент6 страницCerebrospinal Fluid CSF Analysis and InterpretatioIoana CucuОценок пока нет
- Barr Body Test ExplainedДокумент3 страницыBarr Body Test ExplainedChristyl JoОценок пока нет
- An Overview of Autoimmune and Paraneoplastic EncefaliteДокумент14 страницAn Overview of Autoimmune and Paraneoplastic Encefaliterafael rocha novaesОценок пока нет
- Introduction To Endocrinology For Clinical StudentsДокумент28 страницIntroduction To Endocrinology For Clinical StudentsOhwovoriole ToketemuОценок пока нет
- Path Phys4Документ73 страницыPath Phys4Наталія Вікторівна ДавиденкоОценок пока нет
- Kidney TB Presentation on Pathogenesis, Clinical Features and TreatmentДокумент18 страницKidney TB Presentation on Pathogenesis, Clinical Features and Treatmentdrmsupriya091159Оценок пока нет
- The Golden Hours in Treatment Am J Gastroenterol 2012 Aug 107 (8) 1146Документ5 страницThe Golden Hours in Treatment Am J Gastroenterol 2012 Aug 107 (8) 1146hojadecoca1313Оценок пока нет
- Scientist Viva AnswerДокумент2 страницыScientist Viva Answermonday125Оценок пока нет
- Micronutrients in Neurology and DiseaseДокумент16 страницMicronutrients in Neurology and DiseaseSrinivas PingaliОценок пока нет
- Lupus AnticoagulantДокумент27 страницLupus AnticoagulantAndrew Arnold David Villanueva100% (1)
- Evidence Based Medicine Beginners HandbookДокумент40 страницEvidence Based Medicine Beginners HandbookcmegmhiОценок пока нет
- Ljiljana Markovic Van MDFДокумент30 страницLjiljana Markovic Van MDFRamo DženitaОценок пока нет
- ANCA Associated VasculitisДокумент62 страницыANCA Associated VasculitispoluashokОценок пока нет
- PHARM CARE PD SLE NewДокумент58 страницPHARM CARE PD SLE NewbrevmanaОценок пока нет
- Hematologija Covjeka PDFДокумент23 страницыHematologija Covjeka PDFCrvena LoknicaОценок пока нет
- Hiv PPДокумент37 страницHiv PPJitendra YadavОценок пока нет
- Comprehensive Report On Rapid Plasma Reagin Test (RPR)Документ3 страницыComprehensive Report On Rapid Plasma Reagin Test (RPR)Kim RuizОценок пока нет
- TSH Acculite Clia Rev 4Документ2 страницыTSH Acculite Clia Rev 4ghumantuОценок пока нет
- Rheumatoid Arthritis: Polyarthritis As Its Most Common Feature. in Addition, Other Tissues May Be DamagedДокумент8 страницRheumatoid Arthritis: Polyarthritis As Its Most Common Feature. in Addition, Other Tissues May Be Damagedحنين حسن عبد علي حسينОценок пока нет
- Lipidi sadržaj vrste masnih kiselina i zadaća u organizmu/TITLEДокумент14 страницLipidi sadržaj vrste masnih kiselina i zadaća u organizmu/TITLERileShampionОценок пока нет
- Endocrine Case StudiesДокумент16 страницEndocrine Case StudiesIdrissa John Sebeh Conteh0% (1)
- Comparing Primary and Secondary Immune ResponsesДокумент3 страницыComparing Primary and Secondary Immune ResponsesMarta DaОценок пока нет
- Chronic Myeloid Leukemia DiagnosisДокумент4 страницыChronic Myeloid Leukemia DiagnosisKarl Jimenez SeparaОценок пока нет
- Management of Poisoning - Booklet PDFДокумент344 страницыManagement of Poisoning - Booklet PDFkrysteenОценок пока нет
- Neurological Manifestations of HIV/AIDSДокумент34 страницыNeurological Manifestations of HIV/AIDSashuОценок пока нет
- Chapter 29 - Introduction To Leukocyte NeoplasmsДокумент4 страницыChapter 29 - Introduction To Leukocyte NeoplasmsNathaniel SimОценок пока нет
- 2011 - Metformin - Multi-Faceted Protection Against CancerДокумент22 страницы2011 - Metformin - Multi-Faceted Protection Against CancerVladDaculОценок пока нет
- C B C I: Omplete Lood Ount NterpretationsДокумент44 страницыC B C I: Omplete Lood Ount NterpretationsridhoniОценок пока нет
- Multiple Myeloma Epidemiology, Symptoms & TreatmentДокумент15 страницMultiple Myeloma Epidemiology, Symptoms & TreatmentDinda YusditiraОценок пока нет
- Seronegative Antiphospholipid SyndromeДокумент3 страницыSeronegative Antiphospholipid SyndromealexandruОценок пока нет
- 1.6 Epidemiological Indicators - MSF Medical GuidelinesДокумент4 страницы1.6 Epidemiological Indicators - MSF Medical Guidelineskyaw zawОценок пока нет
- Multiple Myeloma OverviewДокумент52 страницыMultiple Myeloma OverviewanmegpraОценок пока нет
- Jurnal PNHДокумент10 страницJurnal PNHsoriaputuОценок пока нет
- 05 - Respiratory Pathology 2 (25 Min)Документ25 страниц05 - Respiratory Pathology 2 (25 Min)Felix Miquel AcostaОценок пока нет
- Evaluation of Biotin InterferenceДокумент4 страницыEvaluation of Biotin InterferenceAnonymous ekfrxJejnОценок пока нет
- AML Pita DR MardiahДокумент71 страницаAML Pita DR MardiahSarly Puspita AriesaОценок пока нет
- N.sepsis 2Документ129 страницN.sepsis 2cooldude_secbad1712100% (1)
- Chronic Lymphoid LeukaemiaДокумент23 страницыChronic Lymphoid LeukaemiaAyensuaОценок пока нет
- Glomerular DiseasesДокумент28 страницGlomerular DiseasesNagaraj Reddy100% (1)
- Shankland NHL Lancet Review PDFДокумент10 страницShankland NHL Lancet Review PDFNadhila ByantОценок пока нет
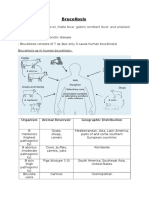
- Brucellosis: Aka: Mediterranean Fever, Malta Fever, Gastric Remittent Fever, and Undulant FeverДокумент11 страницBrucellosis: Aka: Mediterranean Fever, Malta Fever, Gastric Remittent Fever, and Undulant Feverfairuz160194Оценок пока нет
- 10 Lupus Anticoagulants 1Документ28 страниц10 Lupus Anticoagulants 1medico medicoОценок пока нет
- Differentiating Blighted Ovum from Early Pregnancy with SonographyДокумент8 страницDifferentiating Blighted Ovum from Early Pregnancy with SonographyLabontu IustinaОценок пока нет
- UricДокумент6 страницUricLabontu IustinaОценок пока нет
- Nefropatologie C8 Prof DR CaruntuДокумент58 страницNefropatologie C8 Prof DR CaruntuLabontu IustinaОценок пока нет
- Management of acute fever in childrenДокумент7 страницManagement of acute fever in childrenRiriОценок пока нет
- Guias ESC para Insuficiencia Cardiaca CronicaДокумент128 страницGuias ESC para Insuficiencia Cardiaca CronicaKarla HernandezОценок пока нет
- Information On Flail Mitral ValveДокумент44 страницыInformation On Flail Mitral ValvePrasant PandaОценок пока нет
- Adult Hemodynamic Instability DefinitionsДокумент1 страницаAdult Hemodynamic Instability DefinitionsLabontu IustinaОценок пока нет
- Birmingham Vasculitis Activity Score (Version 3) : Ann Rheum Dis. 2008 Dec 3. (Epub Ahead of Print)Документ1 страницаBirmingham Vasculitis Activity Score (Version 3) : Ann Rheum Dis. 2008 Dec 3. (Epub Ahead of Print)Moldoveanu Elena LuciaОценок пока нет
- IHJ Cardiovascular Case Reports (CVCR) : Ujjawal Kumar, Rupesh GeorgeДокумент3 страницыIHJ Cardiovascular Case Reports (CVCR) : Ujjawal Kumar, Rupesh GeorgeLabontu IustinaОценок пока нет
- Rifampicin-Induced Acute Renal Failure: A Series of 60 PatientsДокумент6 страницRifampicin-Induced Acute Renal Failure: A Series of 60 PatientsLabontu IustinaОценок пока нет
- Kjped 60 77Документ9 страницKjped 60 77Labontu IustinaОценок пока нет
- Medication Guidelines For Obstetrics and Gynaecology: First Edition Antimicrobial Safety in Pregnancy and LactationДокумент81 страницаMedication Guidelines For Obstetrics and Gynaecology: First Edition Antimicrobial Safety in Pregnancy and Lactationdewi ayu nurul saputriОценок пока нет
- Information On Flail Mitral ValveДокумент44 страницыInformation On Flail Mitral ValvePrasant PandaОценок пока нет
- Use of Paracetamol During Pregnancy and Child Neurological DevelopmentДокумент7 страницUse of Paracetamol During Pregnancy and Child Neurological DevelopmentLabontu IustinaОценок пока нет
- Entresto Prescribing InformationДокумент3 страницыEntresto Prescribing InformationLabontu IustinaОценок пока нет
- CPG Adrenal Suppression Secondary To Exogenous Glucocorticoids For WebsiteДокумент7 страницCPG Adrenal Suppression Secondary To Exogenous Glucocorticoids For WebsiteLabontu IustinaОценок пока нет
- EHRASurvey ManagementofAFinCKDPatients FinalManuscriptДокумент10 страницEHRASurvey ManagementofAFinCKDPatients FinalManuscriptLabontu IustinaОценок пока нет
- Cardioversion of Atrial Fibrillation and AtrialДокумент13 страницCardioversion of Atrial Fibrillation and AtrialLabontu IustinaОценок пока нет
- BVASДокумент2 страницыBVASAsad KakarОценок пока нет
- Takeaways For Clinicians From The KDIGO 2020 Clinical Practice Guideline For Diabetes Management in CKDДокумент1 страницаTakeaways For Clinicians From The KDIGO 2020 Clinical Practice Guideline For Diabetes Management in CKDLabontu IustinaОценок пока нет
- Spironolactone-Induced Unilateral GynecomastiaДокумент3 страницыSpironolactone-Induced Unilateral GynecomastiaLabontu IustinaОценок пока нет
- Eplerenone As A Treatment For Resistant Hypertension in PregnancyДокумент4 страницыEplerenone As A Treatment For Resistant Hypertension in PregnancyLabontu IustinaОценок пока нет
- New Zealand Data Sheet: OrxigaДокумент49 страницNew Zealand Data Sheet: OrxigaLabontu IustinaОценок пока нет
- Pneumoniae, Was The First Acute-Phase Protein To Be Described and Is An ExquisitelyДокумент11 страницPneumoniae, Was The First Acute-Phase Protein To Be Described and Is An ExquisitelyLabontu IustinaОценок пока нет
- Eplerenone Levels in Maternal Serum, Cord Blood, and Breast Milk During Pregnancy and LactationДокумент3 страницыEplerenone Levels in Maternal Serum, Cord Blood, and Breast Milk During Pregnancy and LactationLabontu IustinaОценок пока нет
- Activity Report: Esc Council On StrokeДокумент9 страницActivity Report: Esc Council On StrokeLabontu IustinaОценок пока нет
- Endocrinologie Ed.6 - Constantin DumitracheДокумент15 страницEndocrinologie Ed.6 - Constantin DumitracheLabontu Iustina100% (1)
- Transcription Factor Bach2 Balances Tolerance and ImmunityДокумент2 страницыTranscription Factor Bach2 Balances Tolerance and ImmunityLabontu IustinaОценок пока нет
- Donny UfoaksesДокумент27 страницDonny UfoaksesKang Bowo D'wizardОценок пока нет
- Phys114 Ps 1Документ11 страницPhys114 Ps 1Reine Amabel JarudaОценок пока нет
- Legal Research MethodsДокумент10 страницLegal Research MethodsCol Amit KumarОценок пока нет
- Types of LogoДокумент3 страницыTypes of Logomark anthony ordonioОценок пока нет
- Mama Leone's Profitability AnalysisДокумент6 страницMama Leone's Profitability AnalysisLuc TranОценок пока нет
- 277Документ18 страниц277Rosy Andrea NicolasОценок пока нет
- Hencher - Interpretation of Direct Shear Tests On Rock JointsДокумент8 страницHencher - Interpretation of Direct Shear Tests On Rock JointsMark2123100% (1)
- Obsolescence 2. Book Value 3. Depreciation 4. Depletion EtcДокумент9 страницObsolescence 2. Book Value 3. Depreciation 4. Depletion EtcKHAN AQSAОценок пока нет
- Ipo Exam Revised SyllabusДокумент1 страницаIpo Exam Revised Syllabusজ্যোতিৰ্ময় বসুমতাৰীОценок пока нет
- Product Catalog 2016Документ84 страницыProduct Catalog 2016Sauro GordiniОценок пока нет
- Linguistics: Chapter 1 - 10Документ41 страницаLinguistics: Chapter 1 - 10Ahmad A. JawadОценок пока нет
- The Rich Hues of Purple Murex DyeДокумент44 страницыThe Rich Hues of Purple Murex DyeYiğit KılıçОценок пока нет
- Call SANROCCO 11 HappybirthdayBramanteДокумент8 страницCall SANROCCO 11 HappybirthdayBramanterod57Оценок пока нет
- 256267a1Документ5 083 страницы256267a1Елизавета ШепелеваОценок пока нет
- ThesisДокумент250 страницThesislax mediaОценок пока нет
- Ilham Bahasa InggrisДокумент12 страницIlham Bahasa Inggrisilhamwicaksono835Оценок пока нет
- January 2013 Igcse Timetable 22-06-2012Документ2 страницыJanuary 2013 Igcse Timetable 22-06-2012Rizwanur RahmanОценок пока нет
- All MeterialsДокумент236 страницAll MeterialsTamzid AhmedОценок пока нет
- Denodo Job RoleДокумент2 страницыDenodo Job Role059 Monisha BaskarОценок пока нет
- Class 9th Chemistry Unit#4 Structure of MoleculesДокумент8 страницClass 9th Chemistry Unit#4 Structure of MoleculesIrfanullahОценок пока нет
- FINAL - Plastic Small Grants NOFO DocumentДокумент23 страницыFINAL - Plastic Small Grants NOFO DocumentCarlos Del CastilloОценок пока нет
- COT EnglishДокумент4 страницыCOT EnglishTypie ZapОценок пока нет
- Merchandise Floor Ready Standards - Supplier InformationДокумент46 страницMerchandise Floor Ready Standards - Supplier InformationGarmentLearner100% (1)
- 01 Design of Flexible Pavement Using Coir GeotextilesДокумент126 страниц01 Design of Flexible Pavement Using Coir GeotextilesSreeja Sadanandan100% (1)
- Application Programming InterfaceДокумент12 страницApplication Programming InterfacesorinproiecteОценок пока нет
- Fiery Training 1Документ346 страницFiery Training 1shamilbasayevОценок пока нет
- Dr. Malik's Farms BrochureДокумент18 страницDr. Malik's Farms BrochureNeil AgshikarОценок пока нет
- Manju Philip CVДокумент2 страницыManju Philip CVManju PhilipОценок пока нет
- The Impact of Information Technology and Innovation To Improve Business Performance Through Marketing Capabilities in Online Businesses by Young GenerationsДокумент10 страницThe Impact of Information Technology and Innovation To Improve Business Performance Through Marketing Capabilities in Online Businesses by Young GenerationsLanta KhairunisaОценок пока нет
- Useful Coaching Questions: Questions To Create A State Change Questions To Ask When Something Goes WrongДокумент2 страницыUseful Coaching Questions: Questions To Create A State Change Questions To Ask When Something Goes WrongAntonioОценок пока нет