Академический Документы
Профессиональный Документы
Культура Документы
Things You Need To Know in Surgical Dept1
Загружено:
Hani NadiahОригинальное название
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Things You Need To Know in Surgical Dept1
Загружено:
Hani NadiahАвторское право:
Доступные форматы
GKS2012/9r Page Together in Delivering Excellence (T.I.D.E.
) 1
Thingsyouneedtoknowinsurgicaldept
1. FluidandElectrolytes
(i) Contentineachpintofsolution
Sol. Content Na K Ca Cl HCO
3
NS NaCl9g(0.9%) 150 150
HS NaCl4.5g(0.45%) 77 77
D5% Dextrose50g/L
D10% Dextrose100g/L
HM NaCl+KCl+CaCl2
+Nalactate
131 5 2 111 29
3%Sal NaCl30g(3%) 513 513
(ii) Dehydration
Mild Moderate Severe
Adult 5% 7.5% 10%
Paeds* <3% 39% >9%
*accordingtoAcuteDiarrhoeaProtocol2011
(iii) Fluidrequirement
Total=Maintenance+Deficit+Ongoinglosses
Maintenance=40cc/kg/day
ForPaeds:(useHollidaySegarFormula)
4cc/kg/hfor1
st
10kg
2cc/kg/hfornext10kg
1cc/kg/hforsubsequentkg
Deficit=10%Bodywt
*replaceover12hrs
Ongoinglosses=lossesfromRTAspiration,
Drainage,thirdspaceloss,plasmalossetc
*usuallyreplacepershiftwithHM/NS
InallheadinjurypatientgiveonlyNS
InburnpatientParklandcorrectionbyHM
InpaedspatientusuallyuseNSD5%
(iv) Assessdegreeofdehydrationbasedon
Mentalstatus
Eyesunkeneye/cryingwithtears
Breathing
Mucosa/tongue
Skinturgor
Pulsevolume
PR/BP
CRT
Peripherywarm/cold
Urineoutput*goodUO=0.51cc/kg/h
(v) Narequirement
Totalrequirement=Maintenance+Deficit
Maintenance=23mmol/kg/d
Deficit(inmmol)=(140x)Wt0.6
*toconverttog,dividewith23.3
(vi) Krequirement
Totalrequirement=Maintenance+Deficit
Maintenance=0.51mmol/kg/d
Deficit(inmmol)=(4x)Wt0.4
*toconverttog,dividewith13.3
RulesofKcorrection:
Rateshouldnot>1.5gperhour
Concentrationshouldnot>3gin1L(1.5gin500ml)
IfhypoKuseMistKCl15mlTDS
Ifseverehypoload1gKClin100ccNSover1hr
Or2gKClin200ccNSover2hr
*makesuretakeECG/putoncardiacmonitoringduring
loadingANDrepeatRPpostloading2hrs
IfhyperKuseoralKalimate15gTDS
Ifseverehyperinsulinchase
IVCaGluconate10%10ccover25minthen
IVDextrose50%50ccthen
IVActrapid10unit
ECGchanges
HypoK HyperK
FlatTwave
NarrowQRS
STdepression
Uwave
SmallP
TalltentedTwave
WidenQRScomplex
Ventriculartachy/fibrillation
(vii) Hyperglycaemia
DKA HHS/HONK
Absoluteinsulindeficiency Relativeinsulindeficiency
Dx:
pH<7.3
Dxt>14
BloodKetone>2(geta
ketonestick)
Dx:
Serumosmolarity>320
Dxt>33
*Osm=2(Na+K)+Glu+Urea
Principleofmanagement:
1. Fluidresuscitation2largeboreIVcannula(green
18Gorgrey16G)in2antecubitalfossa1for
maintenance,1forbolus
2. Insulintherapy(nottostartfirstifKlessthan3.3),
targetDxtinDKA811,HHS1416thendoseof
insulin,ifhypodonotstopinsulin,insteadtouse
D10%drip
3. CorrectionofelectrolytesBUSE&VBG4hrly,
makesuregoodurineoutputandnoECGevidence
ofhyperKwhenplanningtoloadK
4. Treatunderlyingcauses(sepsis,MIetc)
*IndicationofHCO
3
ifHCO
3
<10,give100meq(10amp)
*ifresolvedandpatienttoleratingorallytochangetobasal
bolusregime0.50.8u/kg/dandtitratewithoverlapping1
2hrswithIVIslidingscale
(viii) PreparingDMpatientforelectiveand
emergencysurgery
Elective Emergency
Minor Major TreatDKA
PostponesurgeryuntilRBS<20
unlesslifethreatening
Aim711mmol/Lduringsurgery
GiveD5%orDS+20mmolKCl
8hrly+IVIinsulinslidingscale
OHAgive
normalregime
Insulinomit
ondayof
surgery
DXTQID
OHAomit
longacting
(glibenclamide)
DXTQID
*IfRBS>15,to
startinsulin
slidingscale
GKS2012/9r Page Together in Delivering Excellence (T.I.D.E.) 2
2. AcidBasebalance&Oxygentherapy
(i) ABGinterpretation
Norms
pH7.357.45
pO
2
80100mmHg
pCO
2
3545mmHg
HCO
3
2226
*ToconvertmmHgtokPadivide7.5
(ii) IfpH>7.45
pCO
2
<35 HCO
3
>26
RespiratoryAlkalosis MetabolicAlkalosis
Hyperventilation
stroke
SAH
meningitis
anxiety
hyperthermia
PE
salicylatespoisoning
profusevomiting
hypoK
burn
(iii) IfpH<7.35
pCO
2
>45 HCO
3
<22
Respiratory
Acidosis
MetabolicAcidosis
NAGMAHAGMA
Respiratory
failure
RTA
Diarrhoea
Addisonds
Pancreaticfistula
NH
4
ingestion
Drugacetazolaminde
Increaseinorganic
acidproduction
lactoacidosisshock,
sepsis,hypoxia
uricacid
ketoneDM,alcohol
drugmetformin,
metanol
*aniongap=[Na+K][Cl+HCO
3
]
(iv) Oxygendissociationcurve
LeftsideofcurvepHTDPG(2,3dephosphoglycerate)
RightsideofcurvepHTDPG(2,3dephosphoglycerate)
p50pointwheresaturationofHbreaches50%(atpO
2
=26.6)
ICUpoint(PaO
2
,SaO
2
)=(60mmHg,91%)=lowestacceptable
paO2inICUpatientbecausefurtherdropbeyondthispoint
leadtodrasticdropinSaO
2
MixedvenouspointatSaO
2
=75%
(v) Indicationforintubation
Todeliverpositivepressureventilation
Airwayprotectionfromaspiration
Duringsurgicalproceduresinvolvingneckand
headinnonsupineposition
Neuromuscularparesis
Proceduresincreasesintracranialpressure
Profounddisturbancenconsciousness
Severepulmonaryandmultisystemicinjury
3. Painmanagement
(i) Effectofpain
Hypoventilation
Secretionretention
Mentalunrest
(ii) WHOpainmedicationladder
Painscore03 46 710
Mild Moderate Severe
TPCM1gQID TPCM1gQID
+
CapTramadol
50mgQID
S/CMorphine5
10mg4hrly
TPCM/Cap
Tramadol
**UncontrolledtorefertoAPSforPCAorepiduraletc
Otheroptions:
TArcoxia(Etoricoxibe)90/120mgOD
TPonstan(Mefenemicacid)500mgTDS
IV/IMVoltaren(DiclofenacNa)75mgTDS
*forheadinjuryTPCMandTArcoxia
*forribinjurys/cmorphine
4. Operativecare
(i) Preoperativecare
Clinicalassessment,investigationandpreparation
Getinformedconsent
Hxtakingprevioussurgery,choiceofanaesthesia,
complicationofpreviousoperation
Underlyingcomorbid,smoking,alcoholic,
heart/respi/kidneydiseases
Currentmedicationtowithholdaspirin/warfarin
Physicalexaminationshortneck(difficultintubate),
obese,CVSRespistatus
Vitalsigns,sugarcontrol,bodyweight/height
FBC/Coag/RP/LFT/RBS/CXR/ECG
Correctionofcoagulationdisorder,electrolyte
imbalance,sugarlevel,bloodpressure
Prophylacticantibiotics
Anaestheticteampreopassessment
GKS2012/9r Page Together in Delivering Excellence (T.I.D.E.) 3
Choiceofprophylacticantibiotics
Operation Preferredantibiotics
Laporopencholecystectomy
IVCefuroxime1.5g+
IVMetronidazole500mg
ERCP
Herniarepairwithmesh
Laparoscopicrepair
Breastsurgery
IVCefuroxime1.5g
PreferredantibioticinourdeptIVCefobid(Cefoperazone)
2g+Flagyl(Metronidazole)500mg
(ii) Postoperativecare(complications)
PODfever >38.5C Prevention
1 Wind Atelectasis Incentivespirometry,chest
physiotherapy,ambulate
3 Water UTI/Pneumonia EarlyoffCBD,propuppatient,
sitpatientonchair,hand
washingonhandling,RT
insert,oral/trachytoileting
5 Walk DVT Encourageambulation,S/C
Clexane0.4mgOD,TED
stocking
7 Wound Woundinfection,
abscess
Preopshowerandskinprep,
continueantibioticspostop,
dressingofwound
10 Wonder Drugs
Preopbowelprep(Fleet/Foltran)toprevent
intraoperativecontaminationbyfaecalmasses
OPSIpreventionpenicillin(age<21),vaccinationpost
splenectomy(Haemophilusinfluenzab,meningococcal*,
pneumococcal)*pthavetoselfpurchase
Onceevidenceofbowelmovement(bowelsounds,
flatus/BO)encourageorallyASAPtoprevent
Refeedingsyndrome
Identifyrisk:malignancy,anorexia,alcoholism,GI
surgery,starvation
Closemonitoringduringperiodofrefeedingwith
involvementofnutritionist
Parenteralphosphateadministration18mmol/din
additiontooralsupplement
5. PrimaryandSecondarySurvey
(i) PrimarysurveyABCresuscitation
Airway
Ifpatientgag/talk/coughairwaypatent
Cervicalcollarforallheadinjury
Sxofairwayobstruction:stridor,hoarsenessofvoice
LookforFBinthethroat
Performsuctionandcheckgagreflex
Ifgag,nasopharyngeal(notforbasalskull
fracture)/oropharyngealtubeorintubation
Breathing
Lookforchestexpansionsymmetry?
Pneumo/haemothorax?
Flailchestparadoxicalbreathing
RecheckETT,CXR
Tensionpneumothorax
Thoracocentesisifpneumothoraxchesttube
insertion
Oxygentherapy
Circulation
Listentoheartlookformuffledheartsound
Correcthypotension
Intraabdominalinjury
Abnormalbruits
CardiacBP/PRmonitoring
Beckstriad(muffledHS,JVP,hypotension)
Disability*
GCSassessment
1315mildheadinjury
812moderateheadinjury
<8severeheadinjury
Neurologicalassessmentcranialnerve,power,tone,
reflexes,sensation
Longbonefracturestenderness,crepitus
Pupilreflexes
ConsciousnessAlert,Verbalise,Pain,Unresponsive
Cervicalspineinjury
CTBrain/CervicalspineICB,pneumocranium,spine
disarticulation,fractures
Exposure*
Otherinjuries
Abrasion/lacerationwounds
Checkperineumbloodinurethralmeatus
Logrollstepdeformities,analtone,DPRexamination,
spinedeformities
Chestspring/pelvicspring
LifethreateninginTrauma
Trachea
Chest
expan
sion
Breathing Mx
Tension
pneumo
thorax
Deviate
away
BPlow
venou
sreturn
IVC
Thoraco
centesisthen
chesttube
Flailchest Central
parado
xical
lung
contusion
Pain
scareto
breath
Analgesiaand
oxygen
Open
pneumo
thorax
Central
3sidedflap+
chesttube
PEEP
Cardiac
tamponade
Central
Heart
cannot
expand
Pericardio
centesis
ShorthistoryAMPLE
AllergyMedicationPMHxLastmeal
Eventsurroundinginjury
Afterprimarysurvey
Monitorcardiac,SPO
2
,BP,Urineoutput
LabGXM,ABG,toxicologyscreening,urine
analysis,UPT,otherbaselineIx
Adequateresusbasedonbloodgasandu/o
RadiographicIxCXR,PXR,FAST
GCSScore
Eye Verbal Motor
6 Obey
5 Orientated Localisepain
4 Spontaneous Confuse
Withdraw
pain
3 Tocall
Inappropriatebut
comprehensible
Flexion
2 Topain Incomprehensible Extension
1 Close Mute Nomovement
FASTscan(FocalAbdominalSonographyforTrauma)
6areasoffocalscan:
Morisonpouch(betweenliverandRtkidney)
SpacebetweenspleenandLtkidney
Leftparacolicspace
Rightparacolicspace
PouchofDouglas/Rectovesicalpouch
Pericardialcavity
GKS2012/9r Page Together in Delivering Excellence (T.I.D.E.) 4
Safetytriangleforchesttubeinsertion
(ii) Secondarysurvey(*)
=headandtoecompleteexaminationafter
primarysurvey
Signofbasalskullfracture
Periorbitalhaematoma(racooneyes)
Mastoidhaematoma(battlesign)
Haematympanum
CSFrhinorrhoea
CSFotorrhoea
6. Managementofdrowsyandunconscious
patient
(i) Causes
1. Bilateralcorticaldiseases/processes
a. Traumaheadinjury
b. HypoxiaHIE,sinusthrombosis,CVA
c. Infectioncerebralabscess,meningitis,
encephalitis
d. HaemorrhageSAH,SDH
e. MetabolicDKA,HHS,hypoorhyperNa/K,
hypoglycaemia
f. Organfailureliverorrenal
g. Postictal
h. Endocrinethyroidstorm,myxoedema,Addison
crisis
i. Drugsopiates,alcohol,opioid,alcohol,cocaine,
benzodiazepine,antidepressant
2. Brainstemdisorder~Supratentoral/infratentoral
lesionsSDH,EDH,ICB
(ii) Diagnosisandmanagement
PriorityshouldbegiventoABCresuscitationandperform
examinationsimultaneously,then:
1. Obtainquickhistoryfromwitness
a. Onsetabrupt/gradual
i. Acute(sec/min)CVA,cardiacarrest,SDH,
headinjury
ii. Subacute(minhrs)sepsis,infections,drug,
hypo
iii. Protracted
b. Recentcomplaintsheadache,depress,weakness,
vertigo
c. Recentinjury
d. Previousmedicalillness
2. Examination
a. VitalsT,PR,BP,RR
b. Skinpetechialrashes,ecchymosis
(meningoencephalitis)
c. Neurologicalassessment
i. Posture
Lackofmovementofoneside
Intermittenttwitching
Multifocalmyoclonus
Decortication
decerebration
ii. Levelofconsciousness
iii. Neckrigidity
iv. PupilsizesHornerSyndrome(ptosis,myosis,
anhydrosisandenophthalmus),atropine
overdose,opioidpoisoning,ICBetc
v. Funduscopy
vi. Brainstemreflexpupilreflexes
vii. Cornealreflex
viii. Dollseyereflex(eyemovetooppositesideof
movementsoitalwaysgoestocentre)if
negativebrainsteminjured
d. Racooneyes~basalskull#
e. Otorrhoea/rhinorrhoea
f. Nails,dxtmarks
g. Breathing
i. CheyneStrokerapid,shallowwithperiodic
apnoeicepisodesheartfailure,strokes,
traumaticbraininjuries,tumours,COpoisoning,
morphine,toxicmetabolicencephalopathy
ii. Kussmauldeeplabouredbreathing(usuallymet
acidosis)e.g.DKA,renalfailure
iii. Biotbreathingclusterpattern~pontine
malfunction
iv. Gaspingseverehypoxia
3. Ix
FBC
RBS
ESR/CRP
LFT/RP
BloodC+S
ECG/CXR
Urinetoxicology
ABG/VBG/Lactate
KIVLP
Serumtoxicology
CTBrain
SkullXrayetc.
4. ImmediateMx
MaintainIVline,O
2
therapy
BloodsampleforRBS
Controlseizures
ConsiderIVglucose,thiamine,naloxone,flumazenil
5. FurtherMx
DependingontheHxandexaminationfindings,TFT,
carboxyHblevels,BFMPandplasmaosmolarity
(increasedinmethanol,ethyleneglycolandisopropyl
alcohol)mayberequired.
6. DefinitiveMxdependsonthecause.
However,whilethepatientisundergoingevaluation,it
isessentialto:
pressureareacare
careofthemouth,eyesandskin
physiotherapytoprotectmusclesandjoints
risksofdeepveinthrombosis
risksofstressulcerationofthestomach
nutritionandfluidbalance
urinarycatheterization
monitoringoftheCVS
infectioncontrol
maintenanceofadequateoxygenation,withthe
assistanceofartificialventilationifnecessary
Algorithm
ABCoflifesupport
OxygenandI.Vaccess
Stabilizecervicalspine
Bloodglucose
Controlseizures
ConsiderI.Vglucose,thiamine,naloxone,flumazenil
Briefexaminationandobtainhistory
Investigate
Reassessthesituationandplanfurther
Anteriorborderof
mlatissimusdorsi
(anterioraxillary
line)
Lateralborderof
mpectoralismajor
46
th
rib
GKS2012/9r Page Together in Delivering Excellence (T.I.D.E.) 5
7. Approachtopatientinshock
(i) Differencebetweenseptic,spinaland
hypovolaemicshock
Septic
EarlyLate
Spinal Hypovolaemic
Skin Warm
Pink
Cool
Pale
Warm
Pink
Cool
Pale
JVP
Cardiac
output
Systemic
vascular
resistance
Mixed
venous
O
2
content
Inotropes Dopamine Dopamine Noradrenaline
Mx
IVAbx
Methypred
*unrespons
ivetofluid
resus
Fluid
resus/blood
transfusion
Hypovolaemicshock("Tennis"staging)
I II III IV
<15% 1530% 3040% >40%
750ml 750ml1.5litre 1.52litres >2litres
(ii) Conceptof:
a. Thirdspaceloss
Fluidaccumulationininterstitial
tissue/lumenofparalyticbowels
egpostGITsurgery,pancreatitis
(acuteparapancreaticfluid
collection)
Tendstomobilisebackto
intravascularspaceinPOD3
Bewareoffluidoverloadsign
b. Plasmaloss
Occurafter1
st
12hrspostburn
injury
Slowlydecreaseatthe2
nd
12hrs
Plasmalosscausesoedemaof
tissueinvolved
c. Acutebloodloss
d. Spinalshock
Lossofsensationaccompaniedby
motorparalysiswithinitialloss
andgradualrecoveryofreflexes
followingspinalcordinjury
Phase1(01day)
arreflexia/hyporeflexia,lossof
descendingfacilitation
Phase2(12day)initialreflex
retain,denervation,
supersensitivity
Phase3(14wks)hyperreflexia,
axonsupportedsynapsegrowth
Phase4(112mths)
hyperreflexia,spasticity,soma
supportedsynapsegrowth
8. Managementofwound
(i) Typesofwoundsbydegreeof
contamination
a. Clean
Nontraumaticwithoutinflammation
e.g.vascular,endocrine,eye
procedure,withoutinvolving
respiratory,GIT/GUT
b. Cleancontaminated
Highpotentialforinfection
GIT/GUT/Respiprocedurewithout
spillage
Woundopenfordrainage
c. Contaminated
SpillagefromGIT/Biliary/GUT
d. Dirtyinfected
Traumaticwoundfromdirtysource
Woundembeddedwithforeignbody
Indicatedforwounddebridementto
removenecrotictissues
(ii) Woundclosure
a. Primarywoundclosure
woundclosedimmediatelyafterop
b. Secondarywoundclosure
woundleftopenandletithealed
overtime
c. Delayedprimaryclosureorsecondary
suturing
Duetoinfected/contaminatedwound,
unabletocloseatthetimeafterop
done
Doneafterwoundisclean
(iii) Stagesofwoundhealing
a. Early(D1)haemostasisand
inflammatorystage
b. Intermediate(D2D3)proliferative
withmigrationofmesenchymal
tissues,angiogenesisand
epithelisation
c. Late(D45)woundcontractionand
scarring(D21)
GKS2012/9r Page Together in Delivering Excellence (T.I.D.E.) 6
9. Burnresuscitation
(i) Pathophysiologyofburn
Zoneofcoagulation:irreversibletissueloss(necrosis)
Zoneofstasis:reducedtissueperfusion,potentially
salvageabletissue(lossoftissueinthiszonecanlead
towounddeepeningandwidening)
Zoneofhyperaemia:increasedtissueperfusion,
mostlikelyrecovertissueunlessuntreatedsevere
sepsisandprolongedhypotension
Systemicresponsedevelopedoncetheburn
reaches30%ofTBSA,asaresultofcytokinesand
otherinflammatorymediators
CVS
(i) increasedcapillarypermeabilityleadsto
lossofintravascularproteinandfluidinto
interstitialcompartment
(ii) peripheralandorganvasoconstriction
causedbyTNFmyocardialcontractility
systemichypotensionandorgan
hypoperfusion
RespibronchoconstrictionALI
MetabolicBMR3,catabolism
Immunedownregulating
(ii) Burnclassification
Accordingtodepth(degree)
Isuperficialepidermis:onlyerythema,noblister,healin34
days
IIAsuperficialpartialthicknessinvolvedpapillarydermis:
redwarm,oedematous,blistered,sensoryintact,healless
than2weeks
IIBdeeppartialthicknessinvolvedreticulardermis:damage
dermalappendages,sweatgland,nerves,hairfollicles,heal
atleast3weeks
IIIfullthicknessburninvolvedalllayersofskinandsome
subcutaneoustissueinitiallypainlessinsensatedrysurface
thatappearwhitecrackwithexposedunderlyingfat
IVfullthicknesswithinvolvementoffascia,muscles,and
bones
Accordingtothesurfacearea:
Smallarearulesofpalm(1%patientspalmSA)
Largearearulesofnine
AccordingtoLundandBrowder
(iii) Fluidresuscitation
IVfluidinexcessofmaintenanceisgiventoallpatientwith
burn>20%bodysurfaceareausingParklandformulafor
reducingtheoccurrenceofburninducedshock
Choiceofsolution=Ringerlactate/HM(crystalloid)
ParklandFormula=4BWBSA%.
*Firsthalftobegiveninfirst8hrsafterinjury
*Secondhalftobegiveninnext16hrsafterinjury
*Colloidshouldnotbeusedin1
st
24hrspostburnbecauseit
mayleadtoseverepulmonarycomplication(ARDS)dueto
excessivecapillaryleakage
GKS2012/9r Page Together in Delivering Excellence (T.I.D.E.) 7
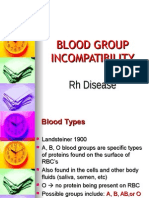
10. Bloodandbloodproduct
(i) ABOandRhesusgroup
a. UniversaldonorforFBCOnegative
b. UniversaldonorforFFPAB
1unitPCexpectedtoincrease24%
Haematocrite
Hb 3=Hct
(ii) Typeofcrossmatching
GSH(GroupScreenHold)
Patientsbloodtypeisdetermined,
bloodisscreenedforantibody
Typeandcrossfromthesamplecan
beorderedifneededlater
GXM(Groupcrossmatch)
Patientsbloodsenttobloodbankand
crossmatchforspecificdonorunitfor
possiblebloodtransfusion
(iii) Typeofbloodproductandindication
Packedcell1unit=350450cc
Indicatedatacutebloodloss
Hb<10forpatientwithh/oCAD/COPD
HealthysymptomaticpatientwithHb<8
1unitPCexpectedtoincrease11.5gofHb
Plateletindicatedif<20
1unitshouldincrease>20
Plateletcountbeforesurgeryhavetobe>50
FFPtoreplaceclottingfactor
Incaseofwarfarinoverdose,DIVC,liverdisease,
TTP
Cryoprecipitatetoreplacefibrinogen,vWF,and
otherclottingfactors
HAS4.5%or20%
Temporarilyforpatientwith
hypoproteinaemia(liverds/nephrotic)with
fluidoverload
Replaceinabdominaltapping
1DIVCregime=2platelet,4cryoprecipitate,6
FFP
(iv) Rateoftransfusion
1pintpackedcellusuallytransfusedover4hrs
withIVfrusemide30mginbetweentransfusion
(v) Transfusioncomplication
Early
(Within24hrs)
Late
(>24hrs)
Acutehaemolyticreaction
Anaphylaxis
Bacterialcontamination
Febrilereaction
Allergicreaction
Fluidoverload
Transfusionrelatedacutelung
injury
Infection(Hep
B/C/HIV/protozoa
/prion)
Ironoverload
Posttransfusion
purpura
11. Acuteabdomen
(i) Definition
Acutesevereabdominalpainthatcausespatienttoseekfor
medicalattention
Peritonealsign
Tendernessonpalpation
Percussiontenderness
Voluntaryguearding
Involuntaryguarding
Rigidity
Reboundtenderness
Inspectionsurgicalscar,distention
Palpationtenderness,hernia,motiontenderness,CVAP
(costovertebralanglepain)
Auscultationbowelsoundsandbruises
Percussionliverandspleensize
Peritonismmotionless,oftenwithkneeflex
(ii) Indicationofsurgicalreferral
Ruptureoforgan
Peritonitis
Colic
Obstructionofboweletc
(iii) Management
ABCresuscitation
Treatshock
Antibiotic
IVfluidresuscitation
Analgesics
KeepNBM
BloodIx:FBC,RP,LFT,CRP,Amylase,ABG,
UFEME,BloodC+S
US/CTtolookforfreefluid
AXR/ECG
Consent
(iv) Painrelief
NonopioidPCM,ibuprofen,diclofenac,aspirin
(musculoskeletalpain,renal,biliarycolic)
Contraindication:pepticulcer,floatingdisorder
OpioidMorphine,dimorphine,pethidine,tramadol
Contraindication:notusedintraumaticheadinjuryorhepatic
failure
Вам также может понравиться
- CPG - Management Stable Angina Pectoris July 2010Документ78 страницCPG - Management Stable Angina Pectoris July 2010umiraihana1100% (1)
- Classification of FractureДокумент2 страницыClassification of FractureHani NadiahОценок пока нет
- HPI GuidelinesДокумент5 страницHPI GuidelinesHani NadiahОценок пока нет
- 4th Edition of Clinical Practice Guidelines Management of Dyslipidemia 2011Документ88 страниц4th Edition of Clinical Practice Guidelines Management of Dyslipidemia 2011Farah Aishah HamdanОценок пока нет
- SchizophreniaДокумент67 страницSchizophreniaHazirah Mokhtar100% (1)
- 20 - Toronto Notes 2011 - Ophthamology PDFДокумент46 страниц20 - Toronto Notes 2011 - Ophthamology PDFSisterzzShopDua0% (1)
- Maqbool - Textbook of Ear, Nose and Throat Diseases, 11th EditionДокумент451 страницаMaqbool - Textbook of Ear, Nose and Throat Diseases, 11th EditionAfi Ramadani100% (2)
- DM Thappa - Essentials in Dermatology, 2nd EditionДокумент479 страницDM Thappa - Essentials in Dermatology, 2nd EditionHani Nadiah85% (20)
- DM Thappa - Essentials in Dermatology, 2nd EditionДокумент479 страницDM Thappa - Essentials in Dermatology, 2nd EditionHani Nadiah85% (20)
- Elective Posting - IMSДокумент15 страницElective Posting - IMSHani NadiahОценок пока нет
- RAДокумент64 страницыRAHani NadiahОценок пока нет
- Cwu GuidelineДокумент16 страницCwu GuidelineHani NadiahОценок пока нет
- Mmi Maid: Making An Informed Decision: Problem Based Learning (PBL) Session Department: MedicineДокумент1 страницаMmi Maid: Making An Informed Decision: Problem Based Learning (PBL) Session Department: MedicineHani NadiahОценок пока нет
- 8 - Toronto Notes 2011 - Emergency MedicineДокумент62 страницы8 - Toronto Notes 2011 - Emergency Medicineprekos 65100% (3)
- Lower LimbДокумент52 страницыLower LimbHani NadiahОценок пока нет
- Upper LimbДокумент28 страницUpper LimbHani NadiahОценок пока нет
- Radiology 2013Документ80 страницRadiology 2013Hani NadiahОценок пока нет
- Antenatal CareДокумент41 страницаAntenatal CareHani NadiahОценок пока нет
- SchizophreniaДокумент67 страницSchizophreniaHazirah Mokhtar100% (1)
- DressДокумент8 страницDressHani Nadiah0% (1)
- Quick Reference MDDДокумент8 страницQuick Reference MDDyus97Оценок пока нет
- CPG Management of Major Depressive DisorderДокумент58 страницCPG Management of Major Depressive DisorderMohd FirdausОценок пока нет
- BottomsДокумент8 страницBottomsHani NadiahОценок пока нет
- Surgical Ho Guide PDFДокумент76 страницSurgical Ho Guide PDFMardiana KamalОценок пока нет
- Andre Tan's Surgical NotesДокумент163 страницыAndre Tan's Surgical NotesHani Nadiah75% (4)
- Andre Tan's Surgical NotesДокумент163 страницыAndre Tan's Surgical NotesHani Nadiah75% (4)
- Clinical ClerkshipДокумент44 страницыClinical ClerkshipCk KmaОценок пока нет
- Manage UA/NSTEMI Guideline 2011Документ62 страницыManage UA/NSTEMI Guideline 2011Mohd RafiОценок пока нет
- Admit OrdersДокумент3 страницыAdmit OrdersHani NadiahОценок пока нет
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceОт EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceРейтинг: 4 из 5 звезд4/5 (890)
- The Yellow House: A Memoir (2019 National Book Award Winner)От EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Рейтинг: 4 из 5 звезд4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingОт EverandThe Little Book of Hygge: Danish Secrets to Happy LivingРейтинг: 3.5 из 5 звезд3.5/5 (399)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeОт EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeРейтинг: 4 из 5 звезд4/5 (5794)
- Never Split the Difference: Negotiating As If Your Life Depended On ItОт EverandNever Split the Difference: Negotiating As If Your Life Depended On ItРейтинг: 4.5 из 5 звезд4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureОт EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureРейтинг: 4.5 из 5 звезд4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryОт EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryРейтинг: 3.5 из 5 звезд3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerОт EverandThe Emperor of All Maladies: A Biography of CancerРейтинг: 4.5 из 5 звезд4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreОт EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreРейтинг: 4 из 5 звезд4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyОт EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyРейтинг: 3.5 из 5 звезд3.5/5 (2219)
- Team of Rivals: The Political Genius of Abraham LincolnОт EverandTeam of Rivals: The Political Genius of Abraham LincolnРейтинг: 4.5 из 5 звезд4.5/5 (234)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersОт EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersРейтинг: 4.5 из 5 звезд4.5/5 (344)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaОт EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaРейтинг: 4.5 из 5 звезд4.5/5 (265)
- The Unwinding: An Inner History of the New AmericaОт EverandThe Unwinding: An Inner History of the New AmericaРейтинг: 4 из 5 звезд4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)От EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Рейтинг: 4.5 из 5 звезд4.5/5 (119)
- Blood Banking and Serology and Immunology Refresher Exam With AnswersДокумент8 страницBlood Banking and Serology and Immunology Refresher Exam With AnswersJohn Rhel DenqueОценок пока нет
- MR - ASHUTOSHRAUT 0869 1005900Документ4 страницыMR - ASHUTOSHRAUT 0869 1005900Ashutosh RautОценок пока нет
- Handout On Other Blood Group SystemДокумент7 страницHandout On Other Blood Group SystemSlrc IdoОценок пока нет
- BOC Study Guide Errata 09082010Документ42 страницыBOC Study Guide Errata 09082010D.L67% (3)
- Blood Transfusion PDFДокумент7 страницBlood Transfusion PDFBaboolal100% (2)
- Assignment: Department of PhysiologyДокумент34 страницыAssignment: Department of PhysiologyMaria NeyveliОценок пока нет
- A Patients Guide To Preventing Medical ErrorsДокумент285 страницA Patients Guide To Preventing Medical Errorscyncyn6616100% (1)
- Blood GroupДокумент31 страницаBlood GroupGanesh PatroОценок пока нет
- Immunology QuestionsДокумент41 страницаImmunology QuestionsNazima Nasrullah100% (1)
- 02 Review of LiteratureДокумент8 страниц02 Review of LiteratureAnnapoorna SHОценок пока нет
- Branham - Transfusion Medicine Instructional PlanДокумент12 страницBranham - Transfusion Medicine Instructional Planapi-610404410Оценок пока нет
- Reading Skill PBTДокумент20 страницReading Skill PBTGesa HayuОценок пока нет
- Adult Blood Transfusion: Answers To Some Common QuestionsДокумент4 страницыAdult Blood Transfusion: Answers To Some Common QuestionsEdward NodzoОценок пока нет
- Blood Group in AnimalДокумент15 страницBlood Group in AnimalAashish Dhakal100% (3)
- Erythroblastosis FetalisДокумент5 страницErythroblastosis FetalisfitriarpsОценок пока нет
- RH IncompatibilityДокумент9 страницRH IncompatibilitySerafin Dimalaluan III50% (2)
- Blood Transfusion MCQsДокумент12 страницBlood Transfusion MCQschanakarn Vipusmith100% (1)
- Shirish M Kawthalkar - Essentials of Clinical Pathology-Jp Medical LTD (2018)Документ446 страницShirish M Kawthalkar - Essentials of Clinical Pathology-Jp Medical LTD (2018)poopziОценок пока нет
- Blood Group Incompatibility RH DiseaseДокумент35 страницBlood Group Incompatibility RH DiseaseRay SadisОценок пока нет
- Blood Bank HarrДокумент7 страницBlood Bank HarrAhrisJeannine EscuadroОценок пока нет
- The Abo Blood Group SystemДокумент3 страницыThe Abo Blood Group Systemchippai123Оценок пока нет
- PMLS2 EsentialsДокумент38 страницPMLS2 EsentialsKen Novero100% (1)
- Blood Distribution System Using Data MiningДокумент5 страницBlood Distribution System Using Data MiningRahul SharmaОценок пока нет
- Module 1 CompleteДокумент57 страницModule 1 CompleteHarpreet BurmiОценок пока нет
- هياДокумент82 страницыهياrubayassir160Оценок пока нет
- Blood Type Test ExperimentДокумент8 страницBlood Type Test ExperimentUpz PhaОценок пока нет
- (CLINPATH) 2.02 Transfusion II - Dr.-VillamayorДокумент7 страниц(CLINPATH) 2.02 Transfusion II - Dr.-VillamayorpasambalyrradjohndarОценок пока нет
- Draft - Recommended Methods For Blood Grouping Reagents Evaluation PDFДокумент55 страницDraft - Recommended Methods For Blood Grouping Reagents Evaluation PDFwidya astutiОценок пока нет
- IMMUNOHEMATOLOGYДокумент126 страницIMMUNOHEMATOLOGYmico guecoОценок пока нет
- Rationale: Most Patients Prescribed To Receive Platelet Transfusions Exhibit Moderate ToДокумент2 страницыRationale: Most Patients Prescribed To Receive Platelet Transfusions Exhibit Moderate TojoanneОценок пока нет