Академический Документы
Профессиональный Документы
Культура Документы
Perio-Endo Continuum A Review
Загружено:
Zahra Khairiza AnriОригинальное название
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Perio-Endo Continuum A Review
Загружено:
Zahra Khairiza AnriАвторское право:
Доступные форматы
J Conserv Dent. 2008 Apr-Jun; 11(2): 5462.
doi: 10.4103/0972-0707.44046
PMCID: PMC2813095
Raja Sunitha V, Pamela Emmadi, Ambalavanan Namasivayam, Ramakrishnan
Thyegarajan, and Vijayalakshmi Rajaraman
Department of Periodontics, Meenakshiammal Dental College and Hospital, Alapakkam Road, Maduravoyal,
Chennai, India
Correspondence: Dr. V. Sunitha Raja, Department of Periodontics, Meenakshiammal Dental College and
Hospital, Alapakkam Road, Maduravoyal, Chennai - 602 102, India. E-mail:sunitha.smiles@gmail.com
Received August 26, 2007; Revised September 20, 2007; Accepted October 4, 2007.
Copyright Journal of Conservative Dentistry
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which
permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly
cited.
Abstract
INTRODUCTION
The tooth, the pulp tissue within it and its supporting structures should be viewed as one
biologic unit. The interrelationship of these structures influences each other during
health, function and disease. The interrelationship between periodontal and endodontic
diseases has aroused much speculation, confusion and controversy. The relationship
between the periodontium and the pulp was first discovered by Simring and Goldberg in
1964.[1] The periodontium and pulp have embryonic, anatomic and functional
interrelationship. Ectomesenchymal cells proliferate to form the dental papilla and
follicle, which are the precursors of the periodontium and the pulp respectively. This
embryonic development gives rise to anatomical connections, which remain throughout
life.[2]
Three main pathways have been implicated in the development of periodontal-
endodontic lesions, namely[3] :
1. Dentinal tubules
2. Lateral and accessory canals
3. Apical foramen
Pulpal and periodontal problems are responsible for more than 50% of tooth
mortality.[4] Periodontal disease is a slowly progressing disease that may have an
atrophic effect on the dental pulp. Periodontal treatments such as deep root planning,
usage of localized medicaments and periodontal injury or wounding may accelerate
pulpal inflammation and provoke the interrelated disease process.[5,6]
PATHWAYS OF COMMUNICATION
Pulpal and periodontal tissues are closely related and the disease transmission between
these two lesions has been demonstrated by many studies, which showed significant
microbiological similarities between infected root canals and advanced periodontitis.[7
10] Other than these microbial findings, similarities in the composition of cellular
infiltrates also suggest the existence of communication between the pulp and the
periodontal tissues.[11] These findings infer that cross-contamination between the pulp
and periodontal tissues is possible.
The possible pathways for ingress of bacteria and their products [Figure 1] into these
tissues can broadly be divided into: anatomical and nonphysiological pathways.[12]
Anatomical pathways
The most important among the anatomical pathways are vascular pathways such as the
apical foramen and the lateral canals and tubular pathways.
Apical Foramen: The pulp and periodontal tissues are derived from highly vascular
mesenchymal tissues of the tooth germ. The blood supply maintains a connection
between these tissues via the apical foramen and lateral canals throughout the
development of the tooth. The apical foramen is the principal and most direct route of
communication between the periodontium and the pulp. Although periodontal disease
has been shown to have a cumulative damaging effect on the pulp tissue, total
disintegration of the pulp is only a certainty if bacterial plaque involves the main apical
foramen, compromising the vascular supply. Following necrosis of the pulp, various
bacterial products like enzymes, metabolites, antigens etc. reach the periodontium
through the apical foramen, initiating and perpetuating an inflammatory response there.
This results in destruction of periodontal tissue fibers and resorption of the adjacent
alveolar bone. External resorption of the cementum can also occur concurrently.
Lateral canals: In addition to the apical foramen, which is the main avenue of
communication, there are a multitude of branches connecting the main root canal
system with the periodontal ligament. These root canal ramifications were first described
nearly 100 years ago by Preiswerk (1901). These ramifications are now currently termed
as accessory canals. The term accessory canal is now used to describe any ramification
that connects the root canal system to the periodontal ligament.[12] As the root
develops, ectomesenchymal channels get incorporated, either due to dentine formation
around existing blood vessels or breaks in the continuity of the Hertwigs root sheath, to
become lateral or accessory canals.[13] Lateral canals normally harbor connective tissue
and vessels which connect the circulating system of the pulp with that of the periodontal
ligament. In some instances, the lateral or accessory canal is obliterated by calcification,
but patent communications of varying sizes (10-250m) may remain in many cases. The
majority of the accessory canals are found in the apical part of the root and lateral canals
in the molar furcation region. The frequency of these ramifications on the root surface
are as follows: apical third 17%, coronal third 1.6% and body of the root 8.8%.[14]
Bender et al., stated that periodontal endodontic problems were much more frequent in
the molars than in the anterior teeth because of the greater number of accessory canals
present in the molars. The percentage of lateral canals in the furcation is 46% in first
molars[15] and 50 to 60% in any multirooted teeth.[16]
Radiographically, it is seldom possible to identify lateral canals unless they have been
filled with a contrasting root canal filling material following endodontic therapy. The
radiographic indications of the presence of lateral canals before obturation are:
1. Localized thickening of periodontal ligament on the lateral root surface
2. A frank lateral lesion
It is essential that the dentist recognizes and is familiar with canal ramifications and
variations. The ideal treatment of periodontal pocket formation associated with
untreated accessory root canals is total debridement and total obturation of the root
canal system.[17]
Tubular pathways
These comprise dentinal tubules which contain the odontoblastic process that extends
from the odontoblast at the pulpal dentin border to the dentino-enamel junction or the
cement-dentinal junction. Passage of microorganisms between the pulp and periodontal
tissues is possible through these tubules, when the dentinal tubules are exposed in areas
of denuded cementum.
Nonphysiological pathways
These include iatrogenic root canal perforations. Improper manipulation of endodontic
instruments can also lead to perforation of the root.[12] The second group of artificial
pathways between periodontal and pulpal tissues are vertical root fractures, caused by
trauma which occurs in both vital and nonvital teeth. The incidence of root fractures is
more in the roots that are filled with lateral condensation technique and the teeth
restored with intracanal posts.[12]
ETIOPATHOGENESIS OF PERIO-ENDO LESIONS
Effect of periodontal lesions on the pulp
The etiologic factors involved in the evolution of perio-endo lesions can be of a varied
nature. However, it is widely accepted that microbial agents are the main cause [Figure
2]. The formation of bacterial plaque on denuded root surfaces, following periodontal
disease, has the potential to induce pathologic changes in the pulp through lateral or
accessory canals. This process, the reverse of the effects of a necrotic pulp on the
periodontal ligament, has been referred to as retrograde pulpitis.[1] The effect of
periodontal lesions on the pulp can result in atrophic and other degenerative changes
like reduction in the number of pulp cells, dystrophic mineralization, fibrosis, reparative
dentin formation, inflammation and resorption.
Atrophic changes: The pulp tissue of a periodontally involved tooth has cells which are
small and have more collagen depositions than normal. Due to impaired nutrition, the
pulp cells slowly degenerate. The death of the cell is so gradual that morphologic
evidence sometimes appears to be lacking. The cause of these atrophic changes is the
disruption of blood flow through the lateral canals, which leads to localized areas of
coagulation necrosis in the pulp. These areas are eventually walled off from the rest of
the healthy pulp tissue by collagen and dystrophic mineralization.
With slowly advancing periodontal disease, cementum deposition may act to obliterate
lateral canals before pulpal irritation occurs. This may explain why, not all periodontally
involved teeth demonstrate pulpal atrophy and canal narrowing. Pressure atrophy may
also occur because of mobility of these periodontally involved teeth.
Inflammatory changes: The causative agents of periodontal disease are found in the
sulcus and are continually challenged by host defenses. An immunologic or
inflammatory response is elicited in response to this microbiologic challenge. This
results in the formation of granulomatous tissue in the periodontium. When periodontal
disease extends from the gingival sulcus towards the apex, the inflammatory products
attack the elements of the periodontal ligament and the surrounding alveolar bone.
A clear cut relationship between progressive periodontal disease and pulpal involvement,
however, does not invariably exist. The most common periodontal lesion produced by
the pulp disease is the localized apical granuloma. It is produced by the diffusion of
bacterial products through the root apex, with the formation of vascular granulation
tissue. Subsequently, resorption of the alveolar bone and occasionally of the root itself
may occur.[17]
Resorption: Resorption of the sides of the roots is frequently found adjacent to the
granulation tissue overlying the roots. When the periodontal lesions are deep, resorption
may also be found within the root canals, often opposite lateral canals, and at the apical
foramen. Since this resorptive process extends into the dentin peripherally towards the
pulp, and the activating factors are produced from the periodontal lesion, a name which
reflects the etiology of this phenomenon, peripheral inflammatory root resorption
(PIRR) was proposed.[18]
Effects of periodontal treatment procedures on the dental pulp
Scaling and root planing This procedure removes the bacterial deposits. However,
improper root planning procedures can also remove cementum and the superficial parts
of dentin, thereby exposing the dentinal tubules to the oral environment. Subsequent
microbial colonization of the root dentin may result in bacterial invasion of the dentinal
tubules.[3] As a consequence, inflammatory lesions may develop in the pulp. The initial
symptom is sharp pain of rapid onset that disappears once the stimulus is removed. The
increase in intensity of pain may be explained by one or both of the following two
reasons. Firstly, the smear layer formed on the root surface by the scaling procedures
will be dissolved within a few days. This, in turn, will increase the hydraulic conductance
of the involved dentinal tubules[19] and decrease the peripheral resistance to fluid flow
across dentin. Thereby, pain sensations are more readily evoked. Secondly, open
dentinal tubules serve as pathways for diffusive transport of bacterial elements in the
oral cavity to the pulp, which is likely to cause a localized inflammatory pulpal
response.[20]
Acid etching : Root conditioning using citric acid during periodontal regenerative
therapy helps to remove bacterial endotoxin and anaerobic bacteria and to expose
collagen bundles to serve as a matrix for new connective tissue attachment to
cementum.[11] Though beneficial in the treatment of periodontal disease, citric acid
removes the smear layer, an important pulp protector. Cotton and Siegel reported that
citric acid, when applied to freshly cut dentine, has a toxic effect on the human dental
pulp.[21] However, several other studies have concluded that pulpal changes after the
application of citric acid does not show any significant changes in the pulp.[22,23]
Effects of endodontic infection on the periodontium
It has been demonstrated that intrapulpal infection tends to promote epithelial
downgrowth along a denuded dentin surface.[24] Also, experimentally induced
periodontal defects around infected teeth were associated with 20% more epithelium
than noninfected teeth. Noninfected teeth showed 10% more connective tissue coverage
than infected teeth.[25] Therefore, it is essential that pulpal infections be treated first,
before undertaking periodontal regenerative procedures.
CLASSIFICATION OF PERIO-ENDO LESIONS
A close relationship exists between disease of the dental pulp and periodontal disease,
and it expresses itself in several ways. The most commonly used classification was given
by Simon, Glick and Frank in 1972 [Figure 3].[26] According to this classification, perio-
endo lesions can be classified into:
1. Primary endodontic lesion
2. Primary periodontal lesion
3. Primary endodontic lesion with secondary periodontal involvement
4. Primary periodontal lesion with secondary endodontic involvement
5. True combined lesion
PRIMARY ENDODONTIC LESION
An acute exacerbation of a chronic apical lesion on a tooth with a necrotic pulp may
drain coronally through the periodontal ligament into the gingival sulcus. This condition
may clinically mimic the presence of a periodontal abscess. In reality, however, it would
be a sinus tract originating from the pulp that opens into the periodontal ligament.
Primary endodontic lesions usually heal following root canal therapy. The sinus tract
extending into the gingival sulcus or furcation area disappears at an early stage, if the
necrotic pulp has been removed and the root canals are well sealed.[3]
PRIMARY PERIODONTAL LESION
These lesions are caused primarily by periodontal pathogens. In this process, chronic
periodontitis progresses apically along the root surface. In most cases, pulpal tests
indicate a clinically normal pulpal reaction. There is frequently an accumulation of
plaque and calculus and the presence of deep pockets may be detected.[3]
COMBINED DISEASES
Primary endodontic lesion with secondary periodontal involvement
If a primary endodontic lesion remains untreated, it may become secondarily involved
with periodontal breakdown. Plaque accumulation at the gingival margin of the sinus
tract leads to plaque induced periodontitis in this area. When plaque and calculus are
detected, the treatment and prognosis of the teeth are different from those of the teeth
involved with only endodontic disease. The tooth now requires both endodontic and
periodontal treatment.
Primary endodontic lesion with secondary periodontal involvement may also occur as a
result of root perforation during root canal treatment, or where pins and posts may have
been misplaced during restoration of the crown. Symptoms may be acute, with
periodontal abscess formation associated with pain, swelling, pus or exudates, pocket
formation, and tooth mobility. A more chronic response may occur without pain, and
involves the sudden appearance of a pocket with bleeding on probing or exudation of
pus.
Root fractures may also present as primary endodontic lesions with secondary
periodontal involvement. These typically occur in root canal treated teeth, often with
posts and crowns. The signs may range from a local deepening of periodontal pocket to a
more acute periodontal abscess formation.[3]
Primary periodontal disease with secondary endodontic involvement
The apical progression of a periodontal pocket may continue until the apical tissues are
involved. In this case, the pulp may become necrotic as a result of infection entering
through lateral canals or the apical foramen. In single-rooted teeth, the prognosis is
usually poor. In molar teeth, the prognosis may be better. Since not all the roots may
suffer the same loss of supporting tissue, root resection can be considered as a treatment
alternative.
If the blood supply circulating through the apex is intact, the pulp has good prospects for
survival. It has been reported that pulpal changes resulting from periodontal disease are
more likely to occur when the apical foramen is involved. In these cases, bacteria
originating from the periodontal pocket are the most likely source of root canal infection.
The treatment of periodontal disease can also lead to secondary endodontic involvement.
Lateral canals and dentinal tubules may be opened to the oral environment by scaling
and root planning or surgical flap procedures. It is possible for a blood vessel within a
lateral canal to be severed by a curette and for the microorganisms to be pushed into the
area during treatment, resulting in pulp inflammation and necrosis.[3]
True combined lesion
True combined endodontic periodontal disease occurs less frequently than other
endodontic-periodontal problems. It is formed when an endodontic lesion progressing
coronally joins an infected periodontal pocket progressing apically.[26] The degree of
attachment loss in this type of lesion is invariably large and the prognosis guarded. This
is particularly true in single-rooted teeth. In molar teeth, root resection can be an
alternative treatment. The radiographic appearance of combined endodontic periodontal
disease may be similar to that of a vertically fractured tooth. If a sinus tract is present, it
may be necessary to raise a flap to determine the etiology of the lesion.
DIAGNOSIS OF PERIODONTAL-ENDODONTIC LESIONS
Diagnosis of primary endodontic disease and primary periodontal disease usually
present no clinical difficulty. In primary periodontal disease, the pulp is vital and
responsive to testing. In primary endodontic disease, the pulp is infected and nonvital.
However, primary endodontic disease with secondary periodontal involvement, primary
periodontal disease with secondary endodontic involvement, or true combined diseases
are clinically and radiographically very similar. Accurate diagnosis can be achieved by
careful history taking, examination and the use of special tests [Table 1]. The extra oral
and intra oral tissues are examined for the presence of any abnormality or disease.
The following steps in diagnosis, aids in deciding an appropriate treatment plan:[3]
VISUAL EXAMINATION
Examination of soft tissues, alveolar mucosa and attached gingiva is done for any
inflammation, ulcerations or sinus tracts. The teeth are examined for any caries,
defective restorations, erosions, abrasions, cracks, fractures, and discolorations like pink
spot which is indicative of internal resorption. Magnifying loupes and operating
microscope can be used for enhanced magnification and illumination
RADIOGRAPHS
Radiographic examination aids in detection of carious lesions, extensive or defective
restorations, pulp caps, root fractures, periradicular radiolucencies, thickened
periodontal ligament and alveolar bone loss. Radiographic changes can be detected only
after inflammation or bacterial by-products originating from the dental pulp cause
sufficient demineralization of the cortical bone. Initially, periradicular bone resorption
from endodontic origin is confined to only cancellous bone. Therefore, it is difficult to
identify bone loss caused due to endodontic disease in the initial stages. However,
periodontal disease causing alveolar bone loss and the presence of calculus can be
effectively detected by radiographs.
PULP VITALITY TESTING
Teeth with vital pulps will react to cold test with sharp brief pain response that usually
does not last more than few seconds. An intense and prolonged pain response often
indicates pulpal changes and irreversible pulpitis. Lack of response may indicate pulp
necrosis.
POCKET PROBING
The presence of a deep solitary pocket in the absence of periodontal disease may indicate
the presence of a lesion of endodontic origin or a vertical root fracture. Periodontal
probing helps in differentiating between endodontic and periodontal disease. It can also
be used to track a sinus resulting from an inflammatory periapical lesion that extends
cervically through the periodontal ligament space. In periodontal lesions, numerous
defects are present throughout the mouth and subgingival calculus can be detected.
TREATMENT OF PERIODONTAL-ENDODONTIC LESIONS
Before the commencement of any kind of advanced restorative work to treat a perio-
endo lesion, the prognosis of the tooth should be considered carefully. Whether there is a
functional need for the tooth, whether the tooth is restorable after the lesion has been
treated and whether the patient is suitable for a lengthy, costly and invasive treatment
are factors that should be taken into consideration. If any of these factors are deemed
negative, extraction is the treatment of choice.
When the pulp is nonvital and infected, conventional endodontic therapy alone will
resolve the lesion. Surgical endodontic therapy is not necessary, even in the presence of
large periradicular radiolucencies and periodontal abscesses. If primary endodontic
lesions persist, despite extensive endodontic treatment, the lesion may have secondary
periodontal involvement or it may be a true combined lesion.
In case of secondary periodontal involvement, root canal therapy is instituted
immediately and the cleaned and shaped root canal is filled with calcium hydroxide
paste, which has bactericidal, anti inflammatory and proteolytic property, inhibiting
resorption and favoring repair. It also inhibits periodontal contamination of
instrumented canals via patent channels connecting the pulp and periodontium before
periodontal treatment removes the contaminants. Treatment results should be evaluated
after two to three months and only then should periodontal treatment be considered.
This allows sufficient time for initial tissue healing and better assessment of the
periodontal condition. Prognosis of primary endodontic disease with secondary
periodontal involvement depends on periodontal treatment and patient response.[17]
Primary periodontal lesions should be treated first by proper hygiene phase therapy.
Poor restorations and any developmental grooves that are difficult to be altered and
make oral hygiene maintenance problematic for the patient should be removed.
Periodontal surgery is performed after the completion of hygiene phase therapy. Pulpal
pathology may be induced while carrying out periodontal therapy in lesions involving the
furcation area. Periodontal therapy may consist of procedures that attempt to treat
periodontal pockets and promote regeneration. The techniques used include new
attachment techniques, gingivectomy, apically displaced flap, removal of the tooth side
of pocket by tooth extraction or by hemisection or root resection. In such cases, root
canal therapy is not indicated unless pulp vitality test results show change. Re-evaluation
must be performed periodically after therapy to check for possible retrograde endodontic
problems. The prognosis is entirely dependent on the periodontal therapy, in such cases.
Early stage periodontal lesions with secondary endodontic involvement may present as
reversible pulpal hypersensitivity, which can be treated purely by periodontal therapy.
Periodontal treatment removes noxious stimuli, and secondary mineralization of
dentinal tubules allows the resolution of hypersensitivity. If pulpal inflammation is
irreversible, root canal treatment is carried out, followed by periodontal treatment. In
some cases, periodontal surgical intervention is advantageous.[17]
The prognosis of periodontal lesions is poorer than endodontic lesions and is dependent
on the apical extensions of the lesion. A favorable endodontic prognosis is obtained only
when the tooth is in a closed and protected environment. As the lesion advances the
prognosis approaches that of a true combined lesion.[27]
True combined lesions are treated initially as for primary endodontic lesions with
secondary periodontal involvement. Prior to surgery, palliative periodontal therapy
should be completed and root canal treatment carried out on the roots to be saved. The
prognosis of a true combined perio-endo lesion is often poor or even hopeless, especially
when periodontal lesions are chronic, with extensive loss of attachment. Root
amputation, hemisection or bicuspidization may allow the root configurations to be
changed sufficiently for a part of the root structure to be saved. The prognosis of an
affected tooth can also be improved by increasing bony support, which can be achieved
by bone grafting and guided tissue regeneration. These advanced treatment options are
based on responses to conventional periodontal and endodontic treatment over an
extended time period.
Iatrogenic lesions like perforation during root canal instrumentation or preparation of
the canal for post and core, require a surgical approach or sealing through an access
cavity with a zinc oxide eugenol, glass ionomer or mineral trioxide aggregate sealing
material immediately.[28]
DISCUSSION AND CONCLUSION
The periodontal-endodontic lesion develops by extension of either periodontal
destruction apically combining with an existing periapical lesion or an endodontic lesion
marginally, combining with an existing periodontal lesion. From the diagnostic point of
view, it is important to realize that as long as the pulp remains vital, although inflamed
or scarred, it is unlikely to produce irritants that are sufficient to cause pronounced
marginal breakdown of the periodontium.
Inflammatory processes in the periodontium associated with necrotic dental pulp and
periodontal disease have an infectious etiology. The essential difference between the two
disease entities is their respective source of infection. Rarely will established endodontic
lesions involve the marginal periodontium, unless they are developing close to the bone
margin. A potential pathway for infectious elements in the root canal in such instances
may be lateral canals.
Acute manifestations of root canal infections can result in rapid and extensive
destruction of the attachment apparatus. Abscesses may drain off in different directions,
either through a sinus tract along the periodontal ligament space or through extra
osseous fistulation into the gingival sulcus or pocket. Following proper endodontic
therapy, these lesions should be expected to heal without a persistent periodontal defect.
Many studies in the literature indicate that combined periodontal and endodontic
therapy is essential for successful healing of a periodontal-endodontic lesion. It has been
said that either endodontic or periodontic treatment alone would not lead to a
satisfactory prognosis, if both disease entities are present and that both must be
considered together.[29,30] Hiatt and Amen[31] claimed that persistent periodontal
disease may clear up only after definitive periodontal therapy is followed by successful
endodontic treatment. Most authors agree that both forms of therapy are essential for
successful healing of combined lesions. However, the problem arises over which lesion
came first and which caused or perpetuated the clinical problem. It is generally agreed
that pulpal disease could initiate or perpetuate periodontal disease; the opposite theory
is controversial. Johnson and Orban[32] showed that periodontal disease that remained
after unsuccessful endodontic therapy cleared up after successful endodontic therapy.
Several authors have also shown the remission of severe periodontal bone loss after
endodontic therapy alone. Simring and Goldberg[1] postulated that endodontic therapy
is indicated in the treatment of terminal periodontal disease that does not respond to
periodontal therapy.
The effect of periodontal inflammation on the pulp is controversial and conflicting
studies abound.[11,20,3336] It has been suggested that periodontal disease has no
effect on the pulp, at least until it involves the apex.[34] On the other hand, several
studies suggested that the effect of periodontal disease on the pulp is degenerative in
nature including an increase in calcifications, fibrosis and collagen resorption, as well as
a direct inflammatory effect.[37,38] However, it seems that the pulp is not directly
affected by periodontal disease, until recession has opened up an accessory canal to the
oral environment. Therefore, treatment of combined lesions should aim at eliminating
both the problems.
Treatment and prognosis of primarily endodontic and primarily periodontal disease is
very straightforward. However, prognosis of combined forms of the lesions is more
difficult to predict. Endodontic therapy is more predictable and completion of this
therapy before periodontal procedures has a positive effect on periodontal healing. The
most guarded prognosis is given for true combined lesions. In general, assuming that
endodontic therapy is adequate, what is of endodontic origin will heal.[3] However, in
cases of combined disease, the prognosis of combined diseases rests with the severity
and extent of the periodontal lesion and the efficacy of periodontal therapy. In
conclusion, it is essential to understand that in perio-endo lesions, the endodontic
treatment is the more predictable of the two. However the success of endodontic therapy
is dependent on the completion of periodontal therapy. The complete treatment of both
aspects of perio-endo lesions is essential for successful long-term results.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
1. Simring M, Goldberg M. The pulpal pocket approach: Retrograde periodontitis. J
Periodontol. 1964;35:2248.
2. Mandel E, Machton P, Torabinejad M. Clinical diagnosis and treatment of endodontic
and periodontal lesions. Quintessence Int.1993;24:1359. [PubMed: 8511265]
3. Rotstein I, Simon JH. Diagnosis, prognosis and decision making in the treatment of
combined periodontal-endodontic lesions.Periodontol 2000. 2004;34:265303.
4. Bender IB. Factors influencing radiographic appearance of bony lesions. J
Endod. 1982;8:16170. [PubMed: 6951916]
5. Seltzer S, Bender IB, Ziontz M. The interrelationship of pulp and periodontal
disease. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1963;16:147.
6. Stallard RE. Periodontic-endodontic relationships. Oral Surg Oral Med Oral
Pathol. 1972;34:314. [PubMed: 4504573]
7. Tanner A, Visconti CR, Holdeman RA, Sundquist G, Socransky SS. Similarity of
Wolinella recta strains isolated form periodontal pockets and root canals. J
Endod. 1982;8:294300. [PubMed: 6955433]
8. Kipioti A, Nakou M, Legakis N, Mitis F. Microbiological findings of infected root
canals and adjacent periodontal pockets in teeth with advanced periodontitis. Oral Surg
Oral Med Oral Pathol. 1984;58:21320. [PubMed: 6384871]
9. Kobayashi T, Hayashi A, Yoshikawa R, Okuda K, Hara K. The microbial flora from
root canals and periodontal pockets of non vital teeth associated with advanced
periodontitis. Int Endod J. 1990;23:1006. [PubMed: 2391182]
10. Kerekes K, Olsen I. Similarities in microflora of root canals and deep periodontal
pockets. Endod Dent Traumatol. 1990;6:15.[PubMed: 2202588]
11. Bergenholtz, Lindhe J. Effect of experimentally induced marginal periodontitis and
periodontal scaling on the dental pulp. J Clin Periodontol. 1978;5:5973. [PubMed:
97332]
12. Zehnder M, Gold SI, Hasselgren G. Pathologic interaction in pulpal and periodontal
tissues. J Clin Periodontol. 2002;29:66371.[PubMed: 12390561]
13. Solomon C, Chalafin H, Kellert M. The endodontic periodontal lesion, a rational
approach to treatment. J Am Dent Assoc.1995;126:4739. [PubMed: 7722108]
14. DeDeus QD. Frequency location and direction of the lateral, secondary and accessory
canals. J Endod. 1975;1:3616.[PubMed: 10697487]
15. Vertucci FJ, Williams RJ. Furcation canals in the human mandibular first
molars. Oral Surg. 1990;69:743.
16. Rahmat A, Barkhordar, Stewart GG. The potential of periodontal pocket formation
associated with untreated accessory root canals.Oral Surg Oral Med Oral
Pathol. 1990;70:76972. [PubMed: 2263338]
17. Mhairi RW. The pathogenesis and treatment of endo-perio lesions. CPD
Dent. 2001;2:995.
18. Lindhe J. Clinical periodontology and implant dentistry. 4th ed. Blackwell
Munksgaard; 2003. pp. 33945.
19. Gold S, Hasselgren G. Peripheral inflammatory root resorption: A review of literature
with case reports. J Clin Periodontol.1992;19:52334. [PubMed: 1447376]
20. Adriaens PA, De Boever JA, Loesche WJ. Bacterial invasion of root cementum and
radicular dentin of periodontally diseased teeth in humans: A reservoir of
periodontopathic bacteria. J Periodontol. 1988;59:22230. [PubMed: 3164373]
21. Cotton WR, Siegel RL. Human pulpal response to citric acid cavity cleanser. J Am
Dent Assoc. 1978;96:63944. [PubMed: 273636]
22. Yeung S, Clarke N. Pulpal effect of citric acid applied topically to root surfaces. Oral
Surg Oral Med Oral Pathol. 1983;56:31720.[PubMed: 6579464]
23. Kitchings SK, del Rio CE, Aufdemorte DE, Meffert RM, Lane JJ. The pulpal response
to topically applied citric acid. Oral Surg Oral Med Oral Pathol. 1984;58:199
206. [PubMed: 6592513]
24. Blomlof L, Lengheden A, Lindskog S. Endodontic infection and calcium hydroxide
treatment. Effects on periodontal healing in mature and immature replanted monkey
teeth. J ClinPeriodontol. 1992;19:6528.
25. Jansson L, Ehnevid H, Blomlof L, Weintraub A, Lindskog S. Endodontic pathogens
in periodontal disease augmentation. J Clin Periodontol. 1995;22:598602. [PubMed:
8583015]
26. Simon JH, Glick DH, Frank AL. The relationship of endodontic-periodontic lesions. J
Clin Periodontol. 1972;43:202.
27. Newman, Takei, Klokkevold, Carranza . 10th ed. Saunders; 2006. Clinical
Periodontology; pp. 8890.
28. Chen SY, Wang HL, Glickman GN. The influence of endodontic treatment upon
periodontal wound healing. J Clin Periodontol.1997;24:44956. [PubMed: 9226384]
29. Schilder H. Endodontic-periodontal therapy. In: Grossman L, editor. Endodontic
Practice. 6th ed. Philadelphia: Lea and Febiger; 1965.
30. Simon P, Jacobs D. The so-called combined periodontal-pulpal problem. Dent Clin
North Am. 1969;13:4552. [PubMed: 5249437]
31. Hiatt W, Amen C. Perioodntal pocket elimination by combined therapy. Dent Clin
North Am. 1964;133:44.
32. Johnson HB, Orban BJ. Interradicular pathology as related to accessory root
canals. J Endod. 1948;3:215. [PubMed: 18861948]
33. Bender IB, Seltzer S. The effect of periodontal disease on the pulp. Oral Surg Oral
Med Oral Pathol. 1972;33:45874.[PubMed: 4621862]
34. Czarnecki RT, Schilder H. A histological evaluation of the human pulp in teeth with
varying degrees of periodontal disease. J Endod.1979;5:24253. [PubMed: 398874]
35. Gold SI, Moskow BS. Perioodntal repair of periapical lesions: The borderland
between pulpal and periodontal disease. J Clin Periodontol. 1987;14:2516. [PubMed:
3475293]
36. Wong R, Hirch RS, Clarke NG. Endodontic effects of root planning in
humans. Endod Dent Traumatol. 1989;5:1936.[PubMed: 2700338]
37. Langeland K, Rodrigues H, Dowden W. Periodontal disease, bacteria and pulpal
histopathology. Oral Surg Oral Med Oral Pathol.1974;37:25770. [PubMed: 4520855]
38. Mandi FA. Histological study of the pulp changes caused by periodontal disease. J Br
Endod Soc. 1972;6:802.
Figures and Tables
Figure 1
The possible anatomic pathways of communication between the pulp and the periodontium; apical
foramen, lateral canals and dentinal tubules
Figure 2
Diagrammatic representation of the etiopathogenesis of endo perio lesions. (Modified from Rotstein I,
Simon JHS. Diagnosis, prognosis and decision making in the treatment of combined periodontal-
endodontic lesions. Periodontology 2000 2004:34;265-303)
Figure 3
Diagrammatic representation of possible endo perio problems based on the classification of Simon
JH, Glick DH, Frank JL 26, 27
Table 1
Various diagnostic procedures that can be used to identify perio endo lesions
Visual examination
Soft Tissues
Inflammation
Ulcerations
Sinus tracts
Teeth
Caries
Defective restorations
Abrasions
Cracks
Fractures
Discolorations
Palpation
Periradicualr abnormalities
Cannot differentiate between endodontic and periodontal lesion
Compare with control teeth
Percussion
Periradicular inflammation
Compare with control teeth
Mobility
Loss of periodontal support
Fractured roots
Recent trauma
Periradicular abscess
Radiographs
Periradicular bone resorption of endodontic origin - not effective
Bone loss due to periodontal disease - effective
Pulp vitality testing
(Cold test, Electric test, Blood flow tests, Cavity test)
Abnormal response Degenerative changes
No response Pulp necrosis
Moderate transient response Normal vital pulp
Quick painful response Reversible pulpitis
Lingering painful response Irreversible pulpitis
Pocket probing
Probing depth
Clinical attachment level
Sinus tracking
Fistula tracking
Semi rigid radioopaque material (gutta percha)
Cracked tooth testing
Transillumination
Wedging
Staining
(Modified from Rotstein I, Simon JHS. Diagnosis, prognosis and decision making in the
treatment of combined periodontal-endodontic lesions. Periodontology 2000
2004:34;265-303)
Вам также может понравиться
- Self-Assessment Colour Review of Small Animal Soft Tissue SurgeryДокумент194 страницыSelf-Assessment Colour Review of Small Animal Soft Tissue Surgerymiliindianu100% (3)
- Module 9Документ2 страницыModule 9ahsie1Оценок пока нет
- Oral Wound Healing: Cell Biology and Clinical ManagementОт EverandOral Wound Healing: Cell Biology and Clinical ManagementHannu LarjavaОценок пока нет
- Management of Pericoronitis of Newly-Erupted Permanent Tooth Using ElectrosurgeryДокумент4 страницыManagement of Pericoronitis of Newly-Erupted Permanent Tooth Using ElectrosurgeryLatifa Hanif ZuhriОценок пока нет
- Black Pigmentation in Primary Dentition Case Report and Literature ReviewДокумент5 страницBlack Pigmentation in Primary Dentition Case Report and Literature ReviewlaloОценок пока нет
- Causes and Pathophysiology of Cushing's Syndrome - UpToDateДокумент15 страницCauses and Pathophysiology of Cushing's Syndrome - UpToDateRoberto López MataОценок пока нет
- Infection ControlДокумент58 страницInfection ControlYoyen Gonzaga100% (10)
- Sensory Analysis v2 2Документ16 страницSensory Analysis v2 2Alyssa BalverdeОценок пока нет
- Endodontic-Periodontal Lesion: A Two-Way Traffic: Dr. Anindya Priya Saha, Dr. Anindya Chakraborty and Dr. Sananda SahaДокумент6 страницEndodontic-Periodontal Lesion: A Two-Way Traffic: Dr. Anindya Priya Saha, Dr. Anindya Chakraborty and Dr. Sananda Sahanovia chantikaОценок пока нет
- Understanding Periodontitis: A Comprehensive Guide to Periodontal Disease for Dentists, Dental Hygienists and Dental PatientsОт EverandUnderstanding Periodontitis: A Comprehensive Guide to Periodontal Disease for Dentists, Dental Hygienists and Dental PatientsОценок пока нет
- Generalized Aggressive Periodontitis in Preschoolers: Report of A Case in A 3-1/2 Year OldДокумент6 страницGeneralized Aggressive Periodontitis in Preschoolers: Report of A Case in A 3-1/2 Year OldDyah Wulan RamadhaniОценок пока нет
- ChronicPerio 16 12 14Документ39 страницChronicPerio 16 12 14vsdeepsОценок пока нет
- Bulk Fill Resin RestorationДокумент18 страницBulk Fill Resin RestorationNuningK93Оценок пока нет
- Longevity of Posterior Composite RestorationДокумент15 страницLongevity of Posterior Composite Restorationvrana23Оценок пока нет
- Comparison of Two Treatment Modalities Operculectomy Vs Thirdmolar Removal For Management of PericoronitisДокумент4 страницыComparison of Two Treatment Modalities Operculectomy Vs Thirdmolar Removal For Management of PericoronitisghinaОценок пока нет
- DEntal Anxiety ScaleДокумент5 страницDEntal Anxiety ScaleDiah WardaniОценок пока нет
- TUTORIAL IN ENGLISH Blok 12Документ7 страницTUTORIAL IN ENGLISH Blok 12Ifata RDОценок пока нет
- Chronic and Aggressive PeriodontitisДокумент46 страницChronic and Aggressive PeriodontitisMoola Bharath ReddyОценок пока нет
- Restoring Posterior Tooth with Semidirect TechniqueДокумент4 страницыRestoring Posterior Tooth with Semidirect Techniquemartariwansyah100% (1)
- Fish Bone Analysis of Self-Medication in IndonesiaДокумент6 страницFish Bone Analysis of Self-Medication in IndonesiaDedy MahendraОценок пока нет
- Pengaruh Aplikasi Topical Dengan Larutan NaF Dan SnF2 Dalam Pencegahan Karies Ni Made Sirat JKG Denpasar PDFДокумент11 страницPengaruh Aplikasi Topical Dengan Larutan NaF Dan SnF2 Dalam Pencegahan Karies Ni Made Sirat JKG Denpasar PDFZaenuriОценок пока нет
- Clinical Applications of Biodentine in Pediatric Dentistry A Review Ofliterature 2332 0702 1000179 PDFДокумент6 страницClinical Applications of Biodentine in Pediatric Dentistry A Review Ofliterature 2332 0702 1000179 PDFZita AprilliaОценок пока нет
- IndianJDentSci92126-1778286 045622Документ8 страницIndianJDentSci92126-1778286 045622Debora NatalynaОценок пока нет
- Caries ProfundaДокумент8 страницCaries ProfundacyntiamalikfaОценок пока нет
- Surgical Periodontal TherapyДокумент11 страницSurgical Periodontal TherapyGonzalo Becerra LeonartОценок пока нет
- Acc Pain FauziДокумент8 страницAcc Pain FauziMuchlis Fauzi EОценок пока нет
- Jurnal Scalling Dan Root PlaningДокумент17 страницJurnal Scalling Dan Root PlaningJesicaОценок пока нет
- Causes and prevention of ledging and blockages in root canalsДокумент19 страницCauses and prevention of ledging and blockages in root canalsBunga Erlita RosaliaОценок пока нет
- Effect of Splinting on Periodontal HealthДокумент4 страницыEffect of Splinting on Periodontal HealthSweetz Viena ParamitaОценок пока нет
- Gingival Enlargement Causes, Classification and GradingДокумент49 страницGingival Enlargement Causes, Classification and Gradingdhwanit31100% (1)
- Other Predisposing Factors of Dental CalculusДокумент26 страницOther Predisposing Factors of Dental CalculusKkumkum Swami100% (1)
- Potential of Lauric Acid, Miristic Acid and Combination Gel As Inhibiting The Growth of Porphyromonas Gingivalis Bacteria in GingivitisДокумент9 страницPotential of Lauric Acid, Miristic Acid and Combination Gel As Inhibiting The Growth of Porphyromonas Gingivalis Bacteria in GingivitisInternational Journal of Innovative Science and Research TechnologyОценок пока нет
- Aulia Rizqi Niami - J2a017048 - Skenario 4Документ29 страницAulia Rizqi Niami - J2a017048 - Skenario 4Aulia Rizqi NiamiОценок пока нет
- Klasifikasi Impaksi Caninus Rahang Atas Pada Pemeriksaan Radiograf Panoramik Dan CBCT Sebagai Penunjang OdontomyДокумент8 страницKlasifikasi Impaksi Caninus Rahang Atas Pada Pemeriksaan Radiograf Panoramik Dan CBCT Sebagai Penunjang OdontomyRahmi WastriОценок пока нет
- Instrumen Endodontik PatahДокумент8 страницInstrumen Endodontik PatahKhamila TusyОценок пока нет
- 63 - CASE REPORT Epulis GranulomaДокумент3 страницы63 - CASE REPORT Epulis GranulomaRina NovitrianiОценок пока нет
- SOCA Blok 12Документ21 страницаSOCA Blok 12safiraОценок пока нет
- Bagi '18211 - Scenario in Englis3.docx'Документ6 страницBagi '18211 - Scenario in Englis3.docx'ithanur316Оценок пока нет
- Esthetic Management of Anterior Teeth with GiomerДокумент7 страницEsthetic Management of Anterior Teeth with GiomerFoysal Sirazee100% (1)
- Immunology of Dental Caries WordДокумент12 страницImmunology of Dental Caries WordsiyaОценок пока нет
- Classification of PulpitisДокумент18 страницClassification of PulpitisEkrar Okto ViarОценок пока нет
- BURNING MOUTH SYNDROME REVIEWДокумент26 страницBURNING MOUTH SYNDROME REVIEWMariatun Zahro NasutionОценок пока нет
- Introduction To Dental Implantology: Dr. Nigam Sattar KhanДокумент49 страницIntroduction To Dental Implantology: Dr. Nigam Sattar KhanNigam SattarОценок пока нет
- Trauma From OcclusionДокумент3 страницыTrauma From OcclusionSuganya MurugaiahОценок пока нет
- Splinting 150507152946 Lva1 App6891 PDFДокумент92 страницыSplinting 150507152946 Lva1 App6891 PDFade ismailОценок пока нет
- Decoronation of An Ankylosed Permanent Incisor: Alveolar Ridge Preservation and Rehabilitation by An Implant Supported Porcelain CrownДокумент4 страницыDecoronation of An Ankylosed Permanent Incisor: Alveolar Ridge Preservation and Rehabilitation by An Implant Supported Porcelain CrownJuan Carlos MeloОценок пока нет
- Materi Tutor in EnglishДокумент7 страницMateri Tutor in EnglishDea RachnadewiОценок пока нет
- Necrotizing Ulcerative PeriodontitisДокумент15 страницNecrotizing Ulcerative PeriodontitisPoushya Riceg0% (1)
- Radiographic Signs of Bone FracturesДокумент16 страницRadiographic Signs of Bone FracturesFatimah Az-ZahrahОценок пока нет
- Black Triangle PDFДокумент4 страницыBlack Triangle PDFzinniaОценок пока нет
- Biofilm: A New View of PlaqueДокумент8 страницBiofilm: A New View of PlaquesmilefxrОценок пока нет
- Gambaran Radiografi Oklusa Kista DentigerousДокумент6 страницGambaran Radiografi Oklusa Kista DentigerousErlin ZukeОценок пока нет
- Daya Hambat Ekstrak Buah Mengkudu (Morinda CitrifoliaДокумент9 страницDaya Hambat Ekstrak Buah Mengkudu (Morinda CitrifoliaAhmad Willy AntonОценок пока нет
- Variasi Normal Lesi Rongga MulutДокумент34 страницыVariasi Normal Lesi Rongga MulutAfaf MahmoudОценок пока нет
- Epulis FissuratumДокумент9 страницEpulis FissuratumDilaC.FareshaОценок пока нет
- Smoking Habits and Alcohol Consumption in Patients Diagnosed With Oral Lichen Planus: A Case ReportДокумент17 страницSmoking Habits and Alcohol Consumption in Patients Diagnosed With Oral Lichen Planus: A Case ReportkuntumОценок пока нет
- Fixed Partial Denture GuideДокумент25 страницFixed Partial Denture GuideKyrkОценок пока нет
- Schenke in 2006Документ17 страницSchenke in 2006Rest0Оценок пока нет
- The Relationship of Endodontic-Periodontic LesionsДокумент6 страницThe Relationship of Endodontic-Periodontic LesionsPam FNОценок пока нет
- Periodontitis Classification and Staging PDFДокумент9 страницPeriodontitis Classification and Staging PDFAnonymous 7YkiHucQlOОценок пока нет
- Rationale of Endodontic TreatmentДокумент30 страницRationale of Endodontic Treatmentaakriti100% (1)
- Cara Penggunaaan DevitalДокумент2 страницыCara Penggunaaan DevitalKrisbudiSetyawanОценок пока нет
- Review Article: Hypodontia: An Update On Its Etiology, Classification, and Clinical ManagementДокумент9 страницReview Article: Hypodontia: An Update On Its Etiology, Classification, and Clinical Managementionut1ilie-1Оценок пока нет
- Diagnosing Dental and Orofacial Pain: A Clinical ManualОт EverandDiagnosing Dental and Orofacial Pain: A Clinical ManualAlex J. MouleОценок пока нет
- Dentine Hypersensitivity: Developing a Person-centred Approach to Oral HealthОт EverandDentine Hypersensitivity: Developing a Person-centred Approach to Oral HealthОценок пока нет
- Pernicious Anemia in Young: A Case Report With Review of LiteratureДокумент5 страницPernicious Anemia in Young: A Case Report With Review of LiteratureeditorijmrhsОценок пока нет
- Testicular CancerДокумент48 страницTesticular Cancerluckyswiss7776848Оценок пока нет
- Glaucoma QuizДокумент2 страницыGlaucoma QuizvoodooariaОценок пока нет
- Sanford Resume 3 21 18Документ2 страницыSanford Resume 3 21 18api-329968843Оценок пока нет
- Sgarbossa CriteriaДокумент5 страницSgarbossa Criteriajacknaim7090Оценок пока нет
- Non Pneumatic Anti Shock Garment To Stabilize Women With Hypovolemic Shock Secondary To Obstetric HemorrhageДокумент2 страницыNon Pneumatic Anti Shock Garment To Stabilize Women With Hypovolemic Shock Secondary To Obstetric HemorrhagednnivОценок пока нет
- Health Drama: To Meet One of The Tasks English Course Lecturer: Deny Abdillah M, M.PDДокумент6 страницHealth Drama: To Meet One of The Tasks English Course Lecturer: Deny Abdillah M, M.PDnadia hanifaОценок пока нет
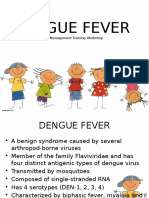
- Children's Dengue FeverДокумент74 страницыChildren's Dengue FeverJohn Christopher LucesОценок пока нет
- Article On PODC 2Документ13 страницArticle On PODC 2Janice M. GombaОценок пока нет
- C SectionДокумент7 страницC SectionJet-Jet GuillerganОценок пока нет
- 2017 Bethesda System of Reporting Thyroid CytopathologyДокумент6 страниц2017 Bethesda System of Reporting Thyroid CytopathologyLuisОценок пока нет
- 2005-4144s1 04 Nipper-Hemodialysis OverviewДокумент19 страниц2005-4144s1 04 Nipper-Hemodialysis Overviewsaleh1978Оценок пока нет
- Ischemic Heart Disease 19.9.90Документ27 страницIschemic Heart Disease 19.9.90Hamidreza GoodarzynejadОценок пока нет
- Secure Rooms and Seclusion Standards and Guidelines:: A Literature and Evidence ReviewДокумент59 страницSecure Rooms and Seclusion Standards and Guidelines:: A Literature and Evidence ReviewRoegie LeppagoОценок пока нет
- RBCDH: Methods For Estimating Body Weight and Height in Hospitalized Adults: A Comparative AnalysisДокумент10 страницRBCDH: Methods For Estimating Body Weight and Height in Hospitalized Adults: A Comparative AnalysisBoh Cucu KaraengОценок пока нет
- Recycling Banks To Reduce Scavenging at Dumps in Lagos, NigeriaДокумент11 страницRecycling Banks To Reduce Scavenging at Dumps in Lagos, NigeriaMary NgbakoОценок пока нет
- HCD Magazine 2014 VOL14Документ70 страницHCD Magazine 2014 VOL14hashim.mjОценок пока нет
- Policy Write Up GMC200 Great EasternДокумент15 страницPolicy Write Up GMC200 Great EasternPrakash VellayanОценок пока нет
- Pharmaco VigilanceДокумент31 страницаPharmaco VigilanceRasika NatuОценок пока нет
- What Is Immunotherapy?Документ19 страницWhat Is Immunotherapy?Najia ChoudhuryОценок пока нет
- PTSD EssayДокумент2 страницыPTSD Essayapi-335023853Оценок пока нет
- Bedside BrochureДокумент2 страницыBedside Brochureapi-438607141100% (1)
- Aplastic AnemiaДокумент7 страницAplastic Anemianeil052288% (8)
- Correspondence Regarding Christchurch Hospital RedevelopmentДокумент74 страницыCorrespondence Regarding Christchurch Hospital RedevelopmentCharlie Mitchell100% (1)
- Acute Heart Failure For Nurse FinalДокумент21 страницаAcute Heart Failure For Nurse FinalAnonymous AZNHObw8Оценок пока нет