Академический Документы
Профессиональный Документы
Культура Документы
Disseminated Intravascular Coagulation
Загружено:
Mary MarjorieАвторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Disseminated Intravascular Coagulation
Загружено:
Mary MarjorieАвторское право:
Доступные форматы
Disseminated Intravascular Coagulation
Etiology
A variety of disorder can initiate DIC. It may result from obstetric complication such as toxemia,
amniotic fluid embolus, or abruption placentae, in which tissue thromboplastin is released from the
placenta. Infection, particularly gram- negative infection, leads to endotoxins that leads to endothelial
damage or stimulate the release or thromboplastin from monocytes. Many carcinomas release
substances that trigger coagulation. Major trauma, such as burns or crush injuries and widespread
deposits from antigen- antibody complexes result in endothelial damage, releasing thromboplastin and
initiating process.
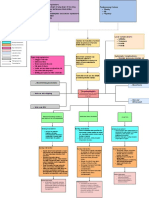
Pathophysiology
Disseminated Intravascular Coagulation is a condition, often life- threatening that involves both
excessive bedding and excessive clotting. It occurs as a complication of numerous primary problems,
which activate the clotting process in the microcirculation throughout the body. Clotting may be induced
by the release of tissue thromboplastin or by injury to the endothelial cells, causing platelet adhesion.
The process cause multiple thromboses and infarctions but also consumes the available clotting factors
and platelets and stimulates the fibronolytic process. This consumption of clotting factors and
fibrinolysis then leads to hemorrhage and eventually to hypotension or shock.
Chronic DIC is a milder form and may be difficult to diagnose: blood counts may be normal or
abnormal. It usually due to chronic infection, and thromboembolism is the dominant feature.
Signs and Symptoms
Whether hemorrhage or thrombosis dominates, the clinical effects depend somewhat on the
underlying cause. Obstetric patients usually manifest increased bleeding, whereas cancer patients tend
to have more tromboses. More often, hemorrhage is the critical problem. Tis is indicated by a low
plasma fibrinogen level, thrombocytopenia, and prolonged bleeding time, PT, APTT, and thrombin time.
Accompanying hemorrhage are the effects of low blood pressure or shock. Multiple bleeding sites are
common, petechiae or ecchymoses may be present on the skin or mucosa, mucosal bleeding is
common, and hematuria may develop. Vascular occlusions are frequently present in small blood vessels
but occasionally affect the large vessels as well, causing infarcts in the brain or other organs.
Respiratory impairment is evident as difficulty in breathing and cyanosis. Neurologic effects
include seizures and decreased responsiveness. Acute renal failure wit oliguria often accompanies shock.
Treatment
A fine balance is required to treat the coagulation imbalance, particularly in life- threatening
cases. Treatment is difficult, dependent on whether hemorrhages or thrombosis are dominant. The
underlying cause, such as infection, must be treated successfully, as well as the major current problem,
whether it be excessive clotting or hemorrhage. The prognosis depends on the severity of the primary
problem.
Вам также может понравиться
- The Yellow House: A Memoir (2019 National Book Award Winner)От EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Рейтинг: 4 из 5 звезд4/5 (98)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeОт EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeРейтинг: 4 из 5 звезд4/5 (5795)
- Never Split the Difference: Negotiating As If Your Life Depended On ItОт EverandNever Split the Difference: Negotiating As If Your Life Depended On ItРейтинг: 4.5 из 5 звезд4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceОт EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceРейтинг: 4 из 5 звезд4/5 (895)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersОт EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersРейтинг: 4.5 из 5 звезд4.5/5 (345)
- The Little Book of Hygge: Danish Secrets to Happy LivingОт EverandThe Little Book of Hygge: Danish Secrets to Happy LivingРейтинг: 3.5 из 5 звезд3.5/5 (400)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureОт EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureРейтинг: 4.5 из 5 звезд4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryОт EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryРейтинг: 3.5 из 5 звезд3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerОт EverandThe Emperor of All Maladies: A Biography of CancerРейтинг: 4.5 из 5 звезд4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaОт EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaРейтинг: 4.5 из 5 звезд4.5/5 (266)
- The Unwinding: An Inner History of the New AmericaОт EverandThe Unwinding: An Inner History of the New AmericaРейтинг: 4 из 5 звезд4/5 (45)
- Team of Rivals: The Political Genius of Abraham LincolnОт EverandTeam of Rivals: The Political Genius of Abraham LincolnРейтинг: 4.5 из 5 звезд4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyОт EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyРейтинг: 3.5 из 5 звезд3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreОт EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreРейтинг: 4 из 5 звезд4/5 (1091)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)От EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Рейтинг: 4.5 из 5 звезд4.5/5 (121)
- Abortion Care Thrombose ProfylaxeДокумент22 страницыAbortion Care Thrombose ProfylaxeambiebieОценок пока нет
- Nursing Care Plan: Congestive Heart Failure-Deep Vein ThrombosisДокумент19 страницNursing Care Plan: Congestive Heart Failure-Deep Vein ThrombosisRiza Angela BarazanОценок пока нет
- Management of Stroke PDFДокумент6 страницManagement of Stroke PDFtarmo angsanaОценок пока нет
- DVTДокумент46 страницDVTLuqman ArifОценок пока нет
- Antiphospholipid SyndromeДокумент8 страницAntiphospholipid Syndromeramona_jitkОценок пока нет
- (Traves D. Crabtree) BRS Surgical Specialties PDFДокумент254 страницы(Traves D. Crabtree) BRS Surgical Specialties PDFCosmin Alexa100% (2)
- Portal Hypertension SurgeryДокумент6 страницPortal Hypertension SurgeryjackSNMMCОценок пока нет
- After SurgeryДокумент3 страницыAfter SurgeryPADAYON MEDISINAОценок пока нет
- Target MDS 1Документ44 страницыTarget MDS 1aftabssmОценок пока нет
- Hematology & Oncology - Passmedicine 2012Документ64 страницыHematology & Oncology - Passmedicine 2012dheajst100% (1)
- Ash Vte Treatment - PPTДокумент45 страницAsh Vte Treatment - PPTRobby Paguh TariganОценок пока нет
- Cureus 0013 00000017832Документ8 страницCureus 0013 00000017832raulОценок пока нет
- Clinical Guide To The Use of Antithrombotic Drugs in Coronary Artery Disease - D. Angiolli, Et. Al., (Informa, 2008) WW PDFДокумент306 страницClinical Guide To The Use of Antithrombotic Drugs in Coronary Artery Disease - D. Angiolli, Et. Al., (Informa, 2008) WW PDFSergiu PlescaОценок пока нет
- Pathanatomy Unit 1 - Unit 6 Q&AДокумент12 страницPathanatomy Unit 1 - Unit 6 Q&AChris Queiklin0% (1)
- Cases Midtem For SOCIAL LEGISLATIONДокумент44 страницыCases Midtem For SOCIAL LEGISLATIONAlfie OmegaОценок пока нет
- Oral Contraceptive Pill: Health Benefits and AdvantagesДокумент9 страницOral Contraceptive Pill: Health Benefits and AdvantagesblennОценок пока нет
- Eac HemaДокумент150 страницEac HemaRemelou Garchitorena AlfelorОценок пока нет
- Precipitating Factors Predisposing Factors: Sitting Down or Lying Down For Too Long ObesityДокумент1 страницаPrecipitating Factors Predisposing Factors: Sitting Down or Lying Down For Too Long ObesitySureen RegularОценок пока нет
- 2020 Therapeutic Strategies For Thrombosis - New Targets and ApproachesДокумент20 страниц2020 Therapeutic Strategies For Thrombosis - New Targets and ApproachesVladimir BasurtoОценок пока нет
- The Investigation of A Complaint by Mrs Q Against Aneurin Bevan Health Board A Report by The Public Services Ombudsman For WalesДокумент52 страницыThe Investigation of A Complaint by Mrs Q Against Aneurin Bevan Health Board A Report by The Public Services Ombudsman For WalesCaerphilly ObserverОценок пока нет
- Literature Review On DVTДокумент4 страницыLiterature Review On DVTaflsdefaq100% (1)
- ASRA Guidelines For CNBДокумент66 страницASRA Guidelines For CNBAshiyan IrfanОценок пока нет
- Adverse Effects of Hormonal ContraceptivesДокумент153 страницыAdverse Effects of Hormonal ContraceptivesTWGAScОценок пока нет
- Ajovy - Fremanezumab - Drug Information - UpToDateДокумент6 страницAjovy - Fremanezumab - Drug Information - UpToDateDiana PhamОценок пока нет
- 4 Perioperative NursingДокумент216 страниц4 Perioperative Nursingmaricor_28174462Оценок пока нет
- Buerger's Disease (Thromboangiitis Obliterans)Документ6 страницBuerger's Disease (Thromboangiitis Obliterans)Mikaela Eris CortelloОценок пока нет
- Baveno IVДокумент10 страницBaveno IVdepe_cutzОценок пока нет
- Pre Blend Lesson 4Документ9 страницPre Blend Lesson 4Envie AestheticsОценок пока нет
- Nattokinase - Optimum Health Vitamins PDFДокумент13 страницNattokinase - Optimum Health Vitamins PDFAnonymous SQh10rG100% (1)
- Investigation and Management of Erythrocytosis: ReviewДокумент6 страницInvestigation and Management of Erythrocytosis: ReviewCamilo CaceresОценок пока нет