Академический Документы
Профессиональный Документы
Культура Документы
The Global Library of Women
Загружено:
vishramki20090 оценок0% нашли этот документ полезным (0 голосов)
72 просмотров6 страницThis is an article by Diagnosis and Management of Postoperative Infection
Patrick Duff, MD
Авторское право
© © All Rights Reserved
Доступные форматы
DOCX, PDF, TXT или читайте онлайн в Scribd
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документThis is an article by Diagnosis and Management of Postoperative Infection
Patrick Duff, MD
Авторское право:
© All Rights Reserved
Доступные форматы
Скачайте в формате DOCX, PDF, TXT или читайте онлайн в Scribd
0 оценок0% нашли этот документ полезным (0 голосов)
72 просмотров6 страницThe Global Library of Women
Загружено:
vishramki2009This is an article by Diagnosis and Management of Postoperative Infection
Patrick Duff, MD
Авторское право:
© All Rights Reserved
Доступные форматы
Скачайте в формате DOCX, PDF, TXT или читайте онлайн в Scribd
Вы находитесь на странице: 1из 6
The Global Library of Womens Medicine
Diagnosis and Management of Postoperative Infection
Patrick Duff, MD
Professor of Obstetrics and Gynecology,
Division of Maternal-Fetal Medicine,
Residency Program Director, and Associate Dean for Student Affairs,
University of Florida College of Medicine, Gainesville, Florida, USA
INTRODUCTION
OPERATIVE SITE INFECTION
PREVENTION OF POSTOPERATIVE INFECTION
REFERENCES
INTRODUCTION
Infection of the operative site is the single most common complication associated with pelvic
surgery. This chapter reviews the epidemiology, diagnosis, and management of the two most
common postoperative infections postcesarean endometritis and pelvic cellulitis after
hysterectomy. It also considers several potentially serious and even life-threatening
complications of operative site infection, namely wound infection, pelvic abscess, and septic
pelvic vein thrombophlebitis. The discussion concludes with an assessment of selected methods
to prevent postoperative infection.
OPERATIVE SITE INFECTION
Epidemiology
Operative site infection (endometritis and pelvic cellulitis) is the most common complication of
cesarean delivery and hysterectomy. In the absence of antibiotic prophylaxis, approximately 30
40% of women having an unscheduled cesarean delivery develop endometritis; after a scheduled
cesarean, approximately 1015% are infected.1, 2 Approximately one-third of women having a
vaginal hysterectomy have pelvic cellulitis if they do not receive prophylactic antibiotics. The
incidence of infection is lower after abdominal hysterectomy (approximately 15%).2, 3
The principal risk factors for postcesarean endometritis are young age, low socioeconomic status,
preexisting infection of the lower genital tract (bacterial vaginosis and group B streptococcal
colonization), extended duration of labor and ruptured membranes, multiple internal vaginal
examinations, and invasive fetal monitoring.4 Pelvic cellulitis, in turn, is more prevalent in
premenopausal women having vaginal versus abdominal hysterectomy and in women who have
bacterial vaginosis, who have an extended duration of surgery, and who lose an excessive
amount of blood intraoperatively.2
Microbiology
Puerperal endometritis and pelvic cellulitis are polymicrobial, mixed aerobicanaerobic
infections. The dominant pathogens are aerobic Gram-positive cocci (group B streptococci,
enterococci, and staphylococcal species), anaerobic Gram-positive cocci (Peptococci and
Peptostreptococci species), aerobic Gram-negative bacilli (Escherichia coli, Klebsiella
pneumoniae, and Proteus species), and anaerobic Gram-negative bacilli (Bacteroides and
Prevotella species). These microorganisms are part of the endogenous vaginal flora and are
introduced into the upper genital tract coincident with vaginal examinations during labor and/or
instrumentation during surgery.4
Diagnosis
The most common clinical manifestations of endometritis and pelvic cellulitis are fever within
2448 hours of surgery, tachycardia, tachypnea, and lower abdominal pain and tenderness in the
absence of any other localizing signs of infection. The other disorders that should be considered
in the initial differential diagnosis of postoperative fever are extensive atelectasis, pneumonia,
viral syndrome, pyelonephritis, and appendicitis.1, 2, 4 Distinction among these entities usually
can be made on the basis of the physical examination and a few selected laboratory tests such as
a complete blood count, urinalysis and urine culture, and, in some patients, a chest x-ray. As a
matter of routine, blood cultures should be performed only in immunosuppressed patients,
patients at risk for endocarditis, patients who appear severely ill, and those who have a poor
response to therapy. Cultures of the upper genital tract are virtually impossible to obtain without
contaminating the specimen by the microorganisms in the vagina;5 therefore, they rarely add
significant information that enhances clinical decision-making.
Management
Patients with an operative site infection require treatment with antibiotics that are active against a
broad range of pelvic pathogens. Several extended-spectrum cephalosporins, penicillins, and
carbapenems may be used as single agents to treat these infections.6, 7 These drugs are listed in
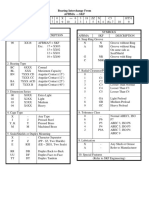
Table 1.
Table 1. Single Agents for Treatment of Postoperative Infection
Drug Intravenous dose Interval
Carbapenems
Ertrapenem 1 g Every 24 h
Imipenem-cilastatin 500 mg Every 6 h
Meropenem 1 g Every 8 h
Cephalosporins
Cefoxitin 2 g Every 6 h
Cefotetan 2 g Every 12 h
Ceftizoxime 2 g Every 812 h
Cefotaxime 2 g Every 8 h
Cefipime 12 g Every 12 h
Penicillins
Ampicillin-sulbactam 3 g Every 6 h
Piperacillin-
tazobactam
3.375 g Every 6 h
Ticarcillin-clavulanate 3.1 g Every 6 h
Combination antibiotic therapy also plays a key role in treatment of endometritis and pelvic
cellulitis. In fact, in many medical centers, combinations of generic agents may be less expensive
than the single agents reviewed. At our center, the two-drug combination of intravenous
clindamycin (900 mg every 8 hours) plus gentamicin (7 mg/kg ideal body weight every 24
hours) and the three-drug regimen of metronidazole (500 mg every 12 hours) plus penicillin (5
million units every 6 hours) or ampicillin (2 g every 6 hours) plus gentamicin (7 mg/kg ideal
body weight every 24 hours) are the most cost-effective regimens for treatment of postoperative
infections. Aztreonam (1 g every 8 hours) could be substituted for gentamicin in these
combination regimens; however, it is much more expensive.6, 7
Approximately 9095% of patients with endometritis or pelvic cellulitis will defervesce within
4872 hours of the start of antibiotic therapy. Parenteral drugs should be continued until the
patient has been afebrile and asymptomatic for 24 hours. At this point, the drugs can be
discontinued and the patient discharged. Extended courses of oral antibiotics are neither
necessary nor desirable. They simply increase expense and the risk of side-effects without
conferring measurable clinical benefit.8
The two most common reasons for a poor response to therapy are resistant organisms and wound
infection.1 If a resistant organism is suspected, patients receiving single-agent therapy or
clindamycin plus gentamicin should have their treatment changed to combination treatment with
metronidazole plus penicillin or ampicillin plus gentamicin. In patients receiving the three-drug
regimen of metronidazole plus penicillin plus gentamicin resistance is extremely unlikely.
If the poor response is thought to be caused by a wound infection, the patient should be treated as
outlined in the following section. Subsequent sections review two other unusual causes of
refractory postoperative fever pelvic abscess and septic pelvic vein thrombophlebitis. In
addition, the differential diagnosis of persistent postoperative fever should include drug fever,
recrudescence of connective tissue disease, and infection at the site of regional anesthesia (e.g.,
an epidural abscess).
Wound Infection
Surgical wound infections occur in approximately 3% of patients having major laparotomy
incisions for procedures such as cesarean delivery or abdominal hysterectomy.1, 2 The
frequency of wound infection is less than 1% in women undergoing postpartum sterilization,
interval sterilization, or other operative laparoscopy procedures. The following factors increase
the probability of postoperative wound infection: obesity, diabetes, immunodeficiency disorder,
use of systemic corticosteroids, smoking, wound hematoma, and preexisting infection such as
chorioamnionitis and pelvic inflammatory disease.
The principal microorganisms that cause wound infections after obstetric or gynecologic surgery
are aerobic staphylococci and streptococci; aerobic Gram-negative bacilli, such as E. coli, K.
pneumoniae, and Proteus species; and anaerobes. Staphylococci and streptococci are inoculated
into the wound from the skin, and the latter organisms are transferred from the pelvic cavity as
the surgeon closes the abdominal wound.9
Wound infections may take one of two forms: an incisional abscess or wound cellulitis.1 Patients
with the former condition typically have erythema and warmth at the margins of the wound and
purulent drainage from the incision itself. Patients with wound cellulitis have an intense
erythematous reaction that spreads outward from the wound. The affected skin is warm and quite
tender to the touch, but purulent drainage does not exude from the incision.
The diagnosis of incisional abscess or wound cellulitis usually can be established by physical
examination. In problematic cases, the wound should be aspirated with an 18- or 20-gauge
needle. Aspiration of pus confirms the diagnosis and provides material for Gram stain and
culture.
If an incisional abscess is present, the wound must be opened and drained, and the fascial layer
should be examined to be certain that it is intact. The wound should be evacuated of all purulent
and necrotic material and then irrigated with copious amounts of normal saline. A thin layer of
gauze should be placed at the base of the wound, and the defect should be covered with a sterile
dressing. The dressing should be changed and the wound irrigated with normal saline at least
twice each day. Patients should be treated with an antibiotic that is active against staphylococci
and streptococci, in addition to the antibiotics they already may be receiving for treatment of
endometritis or pelvic cellulitis. In view of the increasing prevalence of MRSA organisms,
vancomycin, 1 g every 12 hours, is probably the optimal agent to add to the regimen.6, 7
Depending on the patient's response to treatment, two subsequent options are possible. The
wound can be allowed to close by secondary intention. Alternatively, once the infection has
cleared and healthy granulation tissue is evident at the base of the wound, the edges of the
incision may be reapproximated with Steri-Strips or with staples or sutures applied under local
anesthesia.
For patients with wound cellulitis but not an actual incisional abscess, drainage of the incision
usually is not necessary. However, antibiotics with specific activity against staphylococci and
streptococci must be administered, as noted. Antibiotics should be continued until all clinical
evidence of infection has resolved; the usual course of therapy is 57 days.
Pelvic Abscess
A pelvic abscess occurs in less than 1% of patients undergoing obstetric or gynecologic
surgery.4 The most likely pathogens to cause an abscess are anaerobic bacteria and aerobic
Gram-negative bacilli. In patients having cesarean delivery, an abscess is most likely to develop
in the leaves of the broad ligament, in the posterior cul-de-sac, or between the bladder and
anterior uterine wall. In patients who have had a vaginal or abdominal hysterectomy, an abscess
typically forms at the apex of the vagina or in an adnexa that is left in place.
Patients with a postoperative abscess invariably have had endometritis or pelvic cellulitis
diagnosed, have been treated with parenteral antibiotics, and then have had a persistent spiking
fever after 23 days of therapy. They usually are tachycardic and tachypneic and have lower
abdominal pain and tenderness. Depending on the location of the abscess, a fluctuant mass may
be palpable adjacent to the uterus, in front of or behind the uterus, or at the apex of the vaginal
vault.
Patients with a pelvic abscess usually have an elevated white blood cell count with a distinct shift
to immature cell forms. The most cost-effective imaging study to confirm the presence of an
abscess is an ultrasound examination or CT scan.
Patients should be treated with broad-spectrum parenteral antibiotics that cover the full range of
potential pathogens.6, 7 One intravenous antibiotic regimen that has been studied extensively is
the combination of clindamycin (900 mg every 8 hours) or metronidazole (500 mg every 12
hours) plus penicillin (5 million units every 6 hours) or ampicillin (2 g every 6 hours) plus
gentamicin (7 mg/kg of ideal body weight every 24 hours). Aztreonam (1 g every 8 hours) may
be substituted for gentamicin in patients who have renal impairment. Parenteral antibiotics
should be continued until the patient has been afebrile and asymptomatic for 24 hours. Patients
subsequently should receive oral antibiotics to complete a 10-day course of therapy. One
reasonable combination of oral antibiotics is metronidazole, 500 mg, twice daily, plus
doxycycline, 100 mg, twice daily.
Affected patients also require surgical drainage of the abscess. In patients with abscesses lateral
to, or in front of, the uterus, drainage may be accomplished by insertion of a catheter under
ultrasound or CT guidance. In patients with an abscess in the posterior cul-de-sac or at the apex
of the vaginal cuff, drainage may be possible via a small colpotomy incision. In other situations,
laparotomy may be necessary to ensure complete drainage of the abscess.
Septic Pelvic Vein Thrombophlebitis
Along with abdominal wound infection and pelvic abscess, septic pelvic vein thrombophlebitis is
one of the most serious complications of pelvic surgery. It occurs in approximately 0.51% of
patients having major procedures such as cesarean delivery or hysterectomy.10
Affected patients typically have been treated with parenteral antibiotics for presumed
endometritis or pelvic cellulitis and continue to have fever and pelvic pain. Some patients have a
palpable mid-abdominal mass that is caused by a thrombus in one of the ovarian veins, usually
the right. Patients who have multiple small thrombi in the pelvic vasculature may not have a
discrete palpable mass.
The best imaging tests to confirm the diagnosis of septic pelvic vein thrombophlebitis are CT
scan and magnetic resonance imaging.11 The former is less expensive. Both provide excellent
visualization of large clots in the ovarian vessels or vena cava. Neither is particularly accurate in
identifying emboli in the smaller pelvic vessels. In some patients, the diagnosis is established by
exclusion, i.e., by observing the patient's positive response to an empirical trial of heparin.
The currently recommended treatment regimens for septic pelvic vein thrombophlebitis are
based almost entirely on retrospective studies (level 2 evidence). Moreover, only recently have
accurate imaging studies been available to confirm that patients actually had the condition for
which they were being treated. With these caveats in mind, the following treatment guidelines
appear prudent. First, patients should be treated with broad-spectrum intravenous antibiotics until
they have been afebrile and asymptomatic for a minimum of 24 hours. Clindamycin (900 mg
every 8 hours) or metronidazole (500 mg every 12 hours) plus penicillin (5 million units every 6
hours) or ampicillin (2 g every 6 hours) plus gentamicin (7.5 mg/kg ideal body weight every 24
hours) is a well-validated regimen for treatment of severe, polymicrobial pelvic infections.10, 12
Second, patients also should be treated for 710 days with therapeutic doses of unfractionated
heparin or low-molecular-weight heparin. Enoxaparin now is available in generic form and is
almost comparable in cost to unfractionated heparin. Enoxaparin requires less monitoring than
unfractionated heparin and is less likely to cause heparin-induced thrombocytopenia.13 In
patients who clearly have large thrombi extending into the vena cava or who have had clinical
evidence of septic pulmonary emboli, therapeutic anticoagulation (first with heparin, then with
coumadin) should be continued for a more extended period of time, i.e., 36 months.10, 12
PREVENTION OF POSTOPERATIVE INFECTION
Several interventions are of proven effectiveness in decreasing the frequency of infection after
major pelvic surgery. First, patients who have preexisting medical illnesses should be stabilized
before surgery. Second, to the greatest extent possible, prolonged preoperative hospitalization
should be avoided so that the patient's risk of being colonized with hospital-acquired bacteria is
reduced. Compared with the patient's endogenous bacterial flora, such organisms are more likely
to be resistant to commonly used antibiotics. Third, the physician should pay strict attention to
those surgical techniques that clearly have been proven to reduce the rate of postoperative
infection. For example, the risk of postcesarean endometritis is decreased when the placenta is
removed by traction on the umbilical cord rather than by manual extraction.14, 15
Similarly, in obese patients having cesarean delivery, closure of the lower half of the
subcutaneous layer reduces the frequency of wound infection, hematoma, seroma, and
dehiscence.16 This layer should be reapproximated with a suture such as 3-0 Vicryl, Dexon, or
Polysorb, placed in a continuous manner.
Finally, patients undergoing most major pelvic surgery procedures (urgent and scheduled
cesarean delivery, vaginal and abdominal hysterectomy, pregnancy termination, and emergency
cerclage) should receive prophylactic antibiotics. Prophylactic antibiotics have three major
mechanisms of action. They decrease the size of the bacterial inoculum at the surgical site. They
alter the environment at the operative site to make it less hospitable to the growth of bacteria.
Finally, by concentrating in white blood cells, the antibiotics also enhance the phagocytosis of
pathogenic bacteria.2, 3, 17, 18, 19, 20, 21
The drug selected for prophylaxis should have reasonably broad coverage against most pelvic
pathogens. It should be inexpensive, nontoxic, and easy to administer. It also should not be a
drug used as the primary treatment for an established infection. Cefazolin (1 g intravenous or
intramuscular), a first-generation cephalosporin, meets all of the criteria outlined and is an
excellent choice for prophylaxis. If the patient has a history of an immediate hypersensitivity
reaction to beta-lactam antibiotics and is not pregnant, an effective alternate drug is doxycycline,
100 mg intravenous. If the patient is pregnant, the most reasonable alternative is a single
intravenous dose of clindamycin (900 mg) plus gentamicin (1.5 mg/kg of actual weight).
For most patients, a single dose of antibiotics is sufficient to attain the desired therapeutic
effect.17, 18, 19, 20, 21 Until recently, the usual standard of care was to administer the antibiotic
immediately after the infant's umbilical cord was clamped. However, Sullivan et al. 22 showed
that women who received prophylaxis 1560 min prior to the start of surgery had a significantly
lower incidence of endometritis (RR 0.2; 95% confidence interval 0.150.94) than women who
received prophylaxis after the umbilical cord was clamped. Subsequent investigations in
obstetric patients have confirmed the value of administering antibiotics before surgery rather
than after the umbilical cord is clamped.23
For women having gynecologic procedures, the drug should be administered on call to the
operating room. When patients have extended procedures (e.g., more than 34 hours), a second
dose of antibiotic should be administered at the appropriate interval after surgery. Overall,
prophylaxis reduces the rate of postcesarean and postabortal endometritis and posthysterectomy
pelvic cellulitis by approximately 5060%. In indigent patient populations with a high baseline
rate of wound infection, the frequency of wound infection also is reduced. Prophylaxis usually
does not influence the frequency of urinary tract infection.
Summary of Key Points
Postoperative infection is the most common complication of pelvic surgery. Endometritis is the
principal infection that occurs after cesarean delivery; pelvic cellulitis is the major complication
of hysterectomy (level 1 evidence).
Postoperative infection is caused by multiple aerobic and anaerobic bacteria (level 1 evidence).
Postoperative infections should be treated promptly with antibiotics that cover the broad range of
pelvic pathogens. One appropriate regimen is a combination of clindamycin or metronidazole
plus penicillin or ampicillin plus gentamicin. Alternatively, extended-spectrum cephalosporins,
penicillins, or carbapenems may be used as single agents (level 1 evidence, strength of
recommendation A).
Although endometritis and pelvic cellulitis usually respond promptly to broad-spectrum
antibiotics, some patients have serious sequelae such as wound infection, pelvic abscess, and
septic pelvic vein thrombophlebitis (level 1 evidence).
Prophylactic antibiotics are highly effective in decreasing the frequency of infection after
obstetric and gynecologic surgery (level 1 evidence, strength of recommendation A).
REFERENCES
1. Duff P: Infections in pregnancy. In Ling FW, Duff P (eds): Obstetrics & Gynecology. Principles for
Practice. New York, McGraw-Hill, 2001
2. Jamie W, Duff P: Preventing infections during elective C/S and abdominal hysterectomy. Contemp Obstet
Gynecol 60-69, 2003
3. Duff P, Park RC: Antibiotic prophylaxis in vaginal hysterectomy: A review. Obstet Gynecol 55:(S):193-
198, 1980
4. Duff P: The pathophysiology and management of postcesarean endomyometritis. Obstet Gynecol 67:269-
274, 1986
5. Duff P, Gibbs RS, Blanco JD et al: Endometrial culture techniques in puerperal patients. Obstet Gynecol
61:217-221, 1983
6. Duff P: Antibiotic selection in obstetric patients. Infect Dis Clin North Am 11:1-12, 1997 PubMed
7. Duff P: Antibiotic selection in obstetrics: making cost-effective choices. Clin Obstet Gynecol 45:59-72, 2002
PubMed
8. Milligan DA, Brady K, Duff P: Short-term parenteral antibiotic therapy for puerperal endometritis. J
Matern Fetal Med 1:60-104, 1992
9. Gibbs RS, Blanco JD, St. Clair PJ: A case-control study of wound abscess after cesarean delivery. Obstet
Gynecol 62:498-503, 1983
10. Duff P: Septic pelvic vein thrombophlebitis. In Charles D (ed): Obstetric and Perinatal Infections. St.
Louis, Mosby Year Book, 1993.
11. Brown CEI, Lowe TE, Cunningham FG et al: Puerperal pelvic vein thrombophlebitis: impact on
diagnosis and treatment using x-ray computed tomography and magnetic resonance imaging. Obstet Gynecol
68:789-795, 1986
12. Duff P, Gibbs RS: Pelvic vein thrombophlebitis: Diagnostic dilemma and therapeutic challenge. Obstet
Gynecol Surv 38:365-373, 1986
13. Marik PE, Plante LA. Venous thromboembolic disease and pregnancy. N Engl J Med 2008;359: 2025-33.
14. Lasley DS, Eblen A, Yancey MK et al: The effect of placental removal method on the incidence of
postcesarean infections. Am J Obstet Gynecol 176:1250-1254, 1997 PubMed
15. Yancey MK, Clark P, Duff P: The frequency of glove contamination during cesarean delivery. Obstet
Gynecol 83:538-542, 1994 PubMed
16. DelValle GO, Combs P, Qualls C et al: Does closure of Camper fascia reduce the incidence of post-
cesarean superficial wound disruption? Obstet Gynecol 80:1013-1017, 1992
17. Duff P: Prophylactic antibiotics for cesarean delivery: A simple cost-effective strategy for prevention of
postoperative morbidity. Am J Obstet Gynecol 157:794-798, 1987
18. Chelmow D, Ruehl MS, Huang E: Prophylactic use of antibiotics for nonlaboring patients undergoing
cesarean delivery with intact membranes: a meta-analysis. Am J Obstet Gynecol 84:656-661, 2001 PubMed
19. Smaill F, Hofmeyr GJ: Antibiotic prophylaxis for cesarean section (Cochrane Review) The Cochrane
Library, Issue 3, Oxford: Update Software. 2002 PubMed
20. Mittendorf R, Aronson MP, Berry RE et al: Avoiding serious infections associated with abdominal
hysterectomy: a meta-analysis of antibiotic prophylaxis. Am J Obstet Gynecol 169:1119-1124, 1993 PubMed
21. ACOG: Antibiotic prophylaxis for gynecologic procedures. American College of Obstetricians and
Gynecologists. Washington, DC; ACOG Practice Bulletin No. 23 19, January 2001
22. Sullivan SA, Smith T, Chang E, Hulsey, VanDorsten JP, Soper D. Administration of cefazolin prior to
skin incision is superior to cefazolin at cord clamping in preventing postcesarean infectious morbidity: a
randomized controlled trial. Am J Obstet Gynecol 2007; 196:455.31-455.e5.
23. Duff P. A simple checklist for preventing major complications associated with cesarean delivery. Obstet
Gynecol 2010; 116: 1393-6.
Вам также может понравиться
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeОт EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeРейтинг: 4 из 5 звезд4/5 (5794)
- Arvind Singhal vs. Max Therapiya Ltd.Документ28 страницArvind Singhal vs. Max Therapiya Ltd.vishramki2009Оценок пока нет
- Mona Lisa PDFДокумент3 страницыMona Lisa PDFvishramki2009Оценок пока нет
- Spine AnatomyДокумент8 страницSpine Anatomyvishramki2009Оценок пока нет
- The Yellow House: A Memoir (2019 National Book Award Winner)От EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Рейтинг: 4 из 5 звезд4/5 (98)
- Mona Lisa PDFДокумент3 страницыMona Lisa PDFvishramki2009Оценок пока нет
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceОт EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceРейтинг: 4 из 5 звезд4/5 (895)
- The Indian Stamp (Tamil Nadu Amendment) Act, 1958 Act 14 of 1958Документ125 страницThe Indian Stamp (Tamil Nadu Amendment) Act, 1958 Act 14 of 1958vishramki2009100% (1)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersОт EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersРейтинг: 4.5 из 5 звезд4.5/5 (344)
- Mona Lisa PDFДокумент3 страницыMona Lisa PDFvishramki2009Оценок пока нет
- The Little Book of Hygge: Danish Secrets to Happy LivingОт EverandThe Little Book of Hygge: Danish Secrets to Happy LivingРейтинг: 3.5 из 5 звезд3.5/5 (399)
- Gestational Trophoblastic DiseaseДокумент3 страницыGestational Trophoblastic Diseasevishramki2009Оценок пока нет
- A Deadly Way of Doing Business - A Case Study of Corporate Crime IДокумент91 страницаA Deadly Way of Doing Business - A Case Study of Corporate Crime Ivishramki2009Оценок пока нет
- The Emperor of All Maladies: A Biography of CancerОт EverandThe Emperor of All Maladies: A Biography of CancerРейтинг: 4.5 из 5 звезд4.5/5 (271)
- Padre Henrique HenriquesДокумент6 страницPadre Henrique Henriquesvishramki2009Оценок пока нет
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaОт EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaРейтинг: 4.5 из 5 звезд4.5/5 (266)
- Ijsrp p0812 PDFДокумент12 страницIjsrp p0812 PDFvishramki2009Оценок пока нет
- Never Split the Difference: Negotiating As If Your Life Depended On ItОт EverandNever Split the Difference: Negotiating As If Your Life Depended On ItРейтинг: 4.5 из 5 звезд4.5/5 (838)
- Y13 1040Документ9 страницY13 1040vishramki2009Оценок пока нет
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryОт EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryРейтинг: 3.5 из 5 звезд3.5/5 (231)
- Bhoominathan - Judgment CDJ 2010 MHC 6506Документ33 страницыBhoominathan - Judgment CDJ 2010 MHC 6506vishramki2009Оценок пока нет
- Ancient Tamil Vattezhutthu Alphabets Recognition in Stone Inscription Using Wavelet Transform and SVM ClassifierДокумент5 страницAncient Tamil Vattezhutthu Alphabets Recognition in Stone Inscription Using Wavelet Transform and SVM Classifiervishramki2009Оценок пока нет
- Antibiotic Prophylaxis in Surgery PDFДокумент74 страницыAntibiotic Prophylaxis in Surgery PDFHugo GuadarramaОценок пока нет
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureОт EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureРейтинг: 4.5 из 5 звезд4.5/5 (474)
- Hum. Reprod.-2006-Condous-2706-10Документ5 страницHum. Reprod.-2006-Condous-2706-10vishramki2009Оценок пока нет
- Team of Rivals: The Political Genius of Abraham LincolnОт EverandTeam of Rivals: The Political Genius of Abraham LincolnРейтинг: 4.5 из 5 звезд4.5/5 (234)
- 7 Assessing The Motor Component of The Gcs Scoring SystemДокумент11 страниц7 Assessing The Motor Component of The Gcs Scoring Systemvishramki2009Оценок пока нет
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyОт EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyРейтинг: 3.5 из 5 звезд3.5/5 (2259)
- Sonographic Evaluation of First-Trimester BleedingДокумент18 страницSonographic Evaluation of First-Trimester Bleedingvishramki2009Оценок пока нет
- Medical Termination of Pregnancy RulesДокумент17 страницMedical Termination of Pregnancy Rulesvishramki2009Оценок пока нет
- AДокумент3 страницыAvishramki2009Оценок пока нет
- memohcMEMORANDUM SHOWING THE PROCEDURE FOR APPOINTMENT AND TRANSFER OF CHIEF JUSTICES AND JUDGES OF HIGH COURTSДокумент20 страницmemohcMEMORANDUM SHOWING THE PROCEDURE FOR APPOINTMENT AND TRANSFER OF CHIEF JUSTICES AND JUDGES OF HIGH COURTSvishramki2009Оценок пока нет
- Judicial Activism Meaning and ImplicationsДокумент8 страницJudicial Activism Meaning and Implicationsvishramki2009Оценок пока нет
- The Unwinding: An Inner History of the New AmericaОт EverandThe Unwinding: An Inner History of the New AmericaРейтинг: 4 из 5 звезд4/5 (45)
- Small and Commercial Quantity Under Ndps ActДокумент14 страницSmall and Commercial Quantity Under Ndps Actvishramki2009Оценок пока нет
- The Medical Termination of Pregnancy Act, 1971 (Act No. 34 of 1971)Документ4 страницыThe Medical Termination of Pregnancy Act, 1971 (Act No. 34 of 1971)Suresh MuruganОценок пока нет
- 2013 STPL (Web) 152 SCДокумент10 страниц2013 STPL (Web) 152 SCvishramki2009Оценок пока нет
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreОт EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreРейтинг: 4 из 5 звезд4/5 (1090)
- AnilRai Vs ST of Bihar-AIR 2001 SC 3173Документ14 страницAnilRai Vs ST of Bihar-AIR 2001 SC 3173vishramki2009Оценок пока нет
- Constitutional DurabilityДокумент5 страницConstitutional Durabilityvishramki2009Оценок пока нет
- Judgment: ReportableДокумент30 страницJudgment: Reportablevishramki2009Оценок пока нет
- Vidyodaya Trust VsДокумент11 страницVidyodaya Trust Vsvishramki2009Оценок пока нет
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)От EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Рейтинг: 4.5 из 5 звезд4.5/5 (120)
- Vidyodaya Trust VsДокумент11 страницVidyodaya Trust Vsvishramki2009Оценок пока нет
- Science Magazine February 2020Документ133 страницыScience Magazine February 2020Elena González GonzálezОценок пока нет
- c270 KW NTA855G2 60 HZДокумент31 страницаc270 KW NTA855G2 60 HZAhmad El KhatibОценок пока нет
- Pharmalytica Exhibitor List 2023Документ3 страницыPharmalytica Exhibitor List 2023Suchita PoojaryОценок пока нет
- Coding DecodingДокумент21 страницаCoding DecodingAditya VermaОценок пока нет
- Gujral FCMДокумент102 страницыGujral FCMcandiddreamsОценок пока нет
- Patel 2013Документ116 страницPatel 2013hnphuocОценок пока нет
- Manual of Sensorless Brushless Motor Speed Controller: Pentium SeriesДокумент4 страницыManual of Sensorless Brushless Motor Speed Controller: Pentium Seriesfosavo5839Оценок пока нет
- Airport Security Post 9-11Документ7 страницAirport Security Post 9-11lewisОценок пока нет
- Isulat Lamang Ang Titik NG Tamang Sagot Sa Inyong Papel. (Ilagay Ang Pangalan, Section atДокумент1 страницаIsulat Lamang Ang Titik NG Tamang Sagot Sa Inyong Papel. (Ilagay Ang Pangalan, Section atMysterious StudentОценок пока нет
- DP November 2017 Examination Schedule en PDFДокумент4 страницыDP November 2017 Examination Schedule en PDFSuperlucidoОценок пока нет
- Quartile1 PDFДокумент2 страницыQuartile1 PDFHanifah Edres DalumaОценок пока нет
- 12-Week Off-Season Training Programme Junior Rugby (U18 - U21)Документ5 страниц12-Week Off-Season Training Programme Junior Rugby (U18 - U21)LeBron JamesОценок пока нет
- EXAMPLE 8.6 Veneer Grades and RepairsДокумент2 страницыEXAMPLE 8.6 Veneer Grades and RepairsnickОценок пока нет
- Kelas ChondrichtyesДокумент15 страницKelas ChondrichtyesanitagustinawatiОценок пока нет
- Azure Machine Learning StudioДокумент17 страницAzure Machine Learning StudioNurain IsmailОценок пока нет
- Nomenclatura SKFДокумент1 страницаNomenclatura SKFJuan José MeroОценок пока нет
- Dharmakirti39s Commentary On ChakrasamvaraДокумент15 страницDharmakirti39s Commentary On ChakrasamvaraThiago AlbuquerqueОценок пока нет
- Preview: Proquest Dissertations and Theses 2002 Proquest Dissertations & Theses Full TextДокумент24 страницыPreview: Proquest Dissertations and Theses 2002 Proquest Dissertations & Theses Full TextFelipe AguilarОценок пока нет
- Kinder DLL Week 8Документ15 страницKinder DLL Week 8Jainab Pula SaiyadiОценок пока нет
- Free Electron TheoryДокумент8 страницFree Electron TheoryNeelam KapoorОценок пока нет
- Dairy Products Theory XIIДокумент152 страницыDairy Products Theory XIIDskОценок пока нет
- Warehouse Management Solution SheetДокумент2 страницыWarehouse Management Solution Sheetpatelnandini109Оценок пока нет
- AIR Conditioner: Owner'S ManualДокумент52 страницыAIR Conditioner: Owner'S Manualashley diazОценок пока нет
- Veronte Autopilot Kit DatasheetДокумент2 страницыVeronte Autopilot Kit DatasheetEkmedzicОценок пока нет
- CulvertsДокумент18 страницCulvertsAmmar A. Ali100% (1)
- Solar Charge Controller: Solar Car Solar Home Solar Backpack Solar Boat Solar Street Light Solar Power GeneratorДокумент4 страницыSolar Charge Controller: Solar Car Solar Home Solar Backpack Solar Boat Solar Street Light Solar Power Generatorluis fernandoОценок пока нет
- DJI F450 Construction Guide WebДокумент21 страницаDJI F450 Construction Guide WebPutu IndrayanaОценок пока нет
- Case 445Документ4 страницыCase 445ForomaquinasОценок пока нет
- Wang Jinhui - Competitive Physics - Thermodynamics, Electromagnetism and Relativity (2019, World Scientific Publishing Co. Pte. LTD.)Документ961 страницаWang Jinhui - Competitive Physics - Thermodynamics, Electromagnetism and Relativity (2019, World Scientific Publishing Co. Pte. LTD.)Paritosh PandeyОценок пока нет
- The Process: by Andy ZoppeltДокумент4 страницыThe Process: by Andy ZoppeltMark Stephen HuBertОценок пока нет
- The Obesity Code: Unlocking the Secrets of Weight LossОт EverandThe Obesity Code: Unlocking the Secrets of Weight LossРейтинг: 4 из 5 звезд4/5 (6)
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsОт EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsОценок пока нет
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeОт EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeРейтинг: 2 из 5 звезд2/5 (1)
- The Age of Magical Overthinking: Notes on Modern IrrationalityОт EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityРейтинг: 4 из 5 звезд4/5 (24)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaОт EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaРейтинг: 4.5 из 5 звезд4.5/5 (266)
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisОт EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisРейтинг: 4.5 из 5 звезд4.5/5 (42)
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedОт EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedРейтинг: 5 из 5 звезд5/5 (80)