Академический Документы
Профессиональный Документы
Культура Документы
23 02
Загружено:
Ferdian MusthafaОригинальное название
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
23 02
Загружено:
Ferdian MusthafaАвторское право:
Доступные форматы
23
An eruption is caused by coxsackievirus A16 or
enterovirus 71. Breast-fed infants are most frequently
affected.
Blistering is present in the distal portions of the extremi-
ties and oral mucosa. It disappears in 4 to 7 days. Oral
enanthema occurs on the buccal mucosa and tongue.
Erythema or aphtha-like eruptions may also occur.
The only treatment that is usually necessary is oral
hydration.
Hand, foot and mouth disease (HFMD) occurs suddenly after 2
to 5 days of latency. In about half of cases, slight fever is present
for 1 or 2 days. Dispersed small blisters with red halos appear on
the hands, soles, knee joints and buttocks (Fig. 23.9). The blisters
are oval, and their long axis is often parallel to the dermatoglyph-
ic line. Some degree of tenderness, but not itching, may accom-
pany these. The blisters disappear in 4 to 7 days without
rupturing. Painful erythema, blisters, or aphtha-like erosions that
number from a few to several dozen occur on the buccal mucosa
and tongue. They resolve in several days. When caused by
enterovirus 71, HFMD may be accompanied by aseptic meningitis.
The main causative viruses are coxsackievirus A16 and
enterovirus 71. These proliferate in the intestinal tract and are
found in stool and in pharyngeal secretions. The viruses are
spread by droplet and oral infection. The infectiousness is so high
that widespread outbreaks sometimes occur in hospitals. HFMD
occurs most commonly in 1- to 2-year-old breast-fed infants and
in summer epidemics.
No treatment is necessary. Symptomatic therapy is performed
only in cases with severe symptoms.
It is caused by human papillomavirus (HPV) infection.
It occurs most frequently on the fingers, toes, soles and
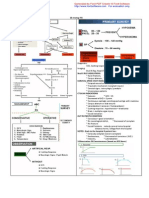
Outline
1. Verruca vulgaris
Treatment
Pathogenesis, Epidemiology
Clinical features
Outline
5. Hand, foot and mouth disease (HFMD)
Clinical images are available in hardcopy only.
Clinical images are available in hardcopy only.
Clinical images are available in hardcopy only.
aa
bb
cc
B. Viral infections whose main symptom is verruca
Fig. 23.9 Hand, foot and mouth disease.
a: Vesicles accompanied by red halo and slight
tenderness. b: Eruptions on the knees. c: Vesicles
accompanied by sharp pain and aphtha in oral
mucosa .
Go Back to the Top To Order, Visit the Purchasing Page for Details
B. Viral infections whose main symptom is verruca 433
23
dorsal surfaces of hands. It is largely asymptomatic.
Liquid nitrogen cryotherapy, topical glutaraldehyde appli-
cation, carbon dioxide gas laser therapy, and electro-
surgery are useful. Some cases heal spontaneously.
Verruca vulgaris is caused by human papillomavirus (HPV), a
virus in the Papovaviridae family. The most frequent HPV infec-
tion is HPV-2, followed by HPV-4, HPV-7, HPV-26, and HPV-
27 (Table 23.1). The virus invades the skin from minor external
injury and infects the epidermal cells. It replicates simultaneously
with differentiation of epidermal cells, leading to maturation of
viral particles in the granular cell layer. The viral particles are
released concurrently with exfoliation of verruca, causing spread-
ing to other areas.
Verruca vulgaris occurs most commonly on the hands and feet
of infants, after a latency of 3 to 6 months. It begins with small
papules. They enlarge, elevating in verrucous shape and becom-
ing several millimeters to several centimeters in diameter (Fig.
23.10). Usually multiple but sometimes solitary eruptions of ver-
ruca vulgaris aggregate, coalesce, and may form plaques. It is
largely asymptomatic and has specific clinical features. There are
some types of verruca vulgaris that are given characteristic clini-
cal diagnostic names according to the clinical features, type of
virus and the affected site.
Plantar wart
Verruca vulgaris occurs on the soles. A keratotic lesion forms
without distinct elevation. It resembles tylosis and clavus, but can
be differentiated from those by scraping. If surface scraping of
the keratotic lesion causes petechiae, the diagnosis is plantar wart.
Myrmecia
A small, dome-shaped nodule forms on the soles. It is caused
by HPV-1 infection (Fig. 23.11) and may resemble molluscum
contagiosum. It is also called deep palmoplantar wart. It has a
red, cratered appearance. Tenderness is often present. It is a type
of plantar wart.
Clinical features
Pathogenesis
Clinical images are available in hardcopy only.
Clinical images are available in hardcopy only.
Clinical images are available in hardcopy only.
Fig. 23.11 Myrmecia.
A dome-shaped nodule accompanied by tender-
ness occurred. Scraping the nodule revealed that
the lesion had invaded the deep intradermal por-
tion.
Clinical images are available in hardcopy only.
Fig. 23.10 Verruca vulgaris.
Table 23.1 HPV types and clinical symptoms.
1 Myrmecia
2,4,7,26-29 Verruca vulgaris
3,10 Flat warts (verruca plana juvenilis)
5,8,9,12,14,15,17,19-26,36,47,50 Epidermodysplasia verruciformis
57,60 Epidermal cyst in the soles
6,11 Condyloma acuminatum
16,18,31, 33-35, 39-41, 51-60 Cervical dysplasia, endocervical cancer
13, 32 Oral focal epithelial hyperplasia
30, 40 Pharyngeal carcinoma
Type Symptoms
434 23 Viral Infections
23
Pigmented wart
This is caused by infection of HPV-4 or HPV-65, or of HPV-
60 in rare cases. It has the clinical features of verruca vulgaris
and blackish pigmentation; it is also called a black wart.
Punctate wart
This is caused by HPV-63 infection. Multiple, punctate, white
keratotic lesions of 2 mm to 5 mm in diameter occur on the hands
and soles.
Filiform wart
A long, small, thin protrusion of several millimeters in diame-
ter occurs on the face, head region or neck (Fig. 23.12).
There is hyperkeratosis, incomplete keratinization and thicken-
ing of the papillary epidermis, accompanied by thickening of the
granular cell layer in the epidermis. Cells with vacuolar degener-
ation and large keratohyaline granules are found in the granular
cell layer. These cellular changes, called koilocytosis, are charac-
teristic of HPV infection (Fig. 23.13).
The main treatment for verruca vulgaris is liquid nitrogen
cryotherapy. Local injection of bleomycin and cauterization by
electrical scalpel or carbon dioxide laser are conducted on sites
where cryotherapy is not fully effective, including hands and
soles. For multiple lesions, coix seed (Coix lacryma-jobi L.)
extract may be administered orally. Topical application of glu-
taraldehyde is useful. Topical vitamin D and oral retinoids have
been reported effective for severe cases.
Synonym: Verruca plana juvenilis
Multiple, slightly elevated, flat papules of 2 mm to 10 mm in
diameter occur on the face (forehead and cheeks). These may
coalesce or appear in linear pattern from autoinfection (Kbner
phenomenon) (Fig. 23.14). The papules are normal skin color or
light pink and nearly asymptomatic. They may disappear sponta-
neously with scaling, which is followed by inflammatory symp-
toms such as itching and reddening. However, flat wart may
persist for several years.
Flat wart is a viral wart that is often caused by HPV-3 or HPV-10.
Some cases heal spontaneously. Liquid nitrogen cryotherapy is
conducted. Coix seed (Coix lacryma-jobi L.) extract may be
administered orally.
Treatment
Pathogenesis
Clinical features
2. Flat wart
Treatment
Pathology
Clinical images are available in hardcopy only.
Fig. 23.12 Filiform wart.
Fig. 23.13 Histopathology of verruca vul-
garis.
Clinical images are available in hardcopy only.
Fig. 23.14 Flat wart.
Clinical images are available in hardcopy only.
B. Viral infections whose main symptom is verruca 435
23
Genital verrucous papules are caused by HPV-6 or HPV-
11. This is an STD.
Latency is 2 to 3 months.
Cryotherapy and laser surgical removal are the main
treatments.
The latency of condyloma acuminatum is 2 to 3 months. Mul-
tiple verrucous papules of papillary or cauliflower shape occur in
the genitalia or perianal region (Fig. 23.15). Keratinization is
rarely present. The papules are infiltrative at the surface and may
give off foul odor. Condyloma acuminatum may enlarge. Kera-
tinization and ulceration may closely resemble squamous cell
carcinoma (Buschke-Lowenstein tumor).
Condyloma acuminatum is caused by HPV-6 or HPV-11.
Most cases occur in the sexually active years, transmitted through
sexual activity. The virus invades through minor external injury
of the genitalia, perianal region, or vaginal introitus, and infects
epidermal basal cells, inducing abnormal cellular proliferation.
Proliferation of the epidermis results in formation of papillary
tumors (warts).
Condyloma acuminatum can be diagnosed by the clinical fea-
tures; however, biopsy may be needed for differential diagnosis,
such as from Bowenoid papulosis, a tumor that is often caused by
HPV-16 and that histologically resembles Bowens disease.
Treatment for condyloma acuminatum is the same as for verru-
ca vulgaris. Liquid nitrogen cryotherapy and surgical removal
using electrical scalpel or carbon gas laser are conducted. Local
injection of bleomycin is used in intractable cases.
Multiple black papules of 2 to 20 mm in diameter occur on the
genitalia of young people (Fig. 23.16). Small papules may coa-
lesce and form plaques. HPV-16 is detected in the lesion.
Bowenoid papulosis is histopathologically indistinguishable from
Bowens disease. It rarely becomes malignant, and it may heal
spontaneously. The prognosis is good. Liquid nitrogen cryothera-
py and electrical cauterization are the main treatments. Bowenoid
papulosis is thought to be an atypical type of condyloma acumi-
natum.
4. Bowenoid papulosis
Treatment
Diagnosis, Differential diagnosis
Pathogenesis
Clinical features
Outline
3. Condyloma acuminatum
Clinical images are available in hardcopy only.
Clinical images are available in hardcopy only.
Fig. 23.15 Condyloma acuminatum.
The verrucous papules resemble cauliflower.
Clinical images are available in hardcopy only.
Fig. 23.16 Bowenoid papulosis.
The papules caused by Bowenoid papulosis are
blackish in most cases or close to normal skin
color in some cases.
436 23 Viral Infections
23
The main causes are HPV-5, HPV-8, HPV-17 and HPV-20
infection. Susceptibility to the virus is inherited, usually autoso-
mal recessively; however, some cases with autosomal dominant
and X-linked dominant patterns have been reported. Congenital
cellular immunocompromise against HPV is thought to be asso-
ciated with the occurrence. Relatively large, flat-wart-like, red-
dish-brown keratotic patches appear on the dorsal surfaces of the
hands and trunk of infants, often coalescing to form plaques or
reticular arrangements. Pityriasis-versicolor-like leukoderma and
erythema may occur (Fig. 23.17). Multiple cells containing
bright and enlarged cytoplasm are histopathologically observed
in the upper suprabasal cell layer. The eruptions gradually spread
on the whole body surface. Malignant skin tumor (e.g., squamous
cell carcinoma, basal cell carcinoma, Bowens disease) occurs in
about half of adolescent and older patients. There is no specific
treatment for epidermodysplasia verruciformis. Sunscreen is used
for prevention, because lesions on sun-exposed areas tend to
worsen. Oral retinoid administration is effective.
A wart forms as a result of infection by the molluscum
contagiosum virus.
Infants are most frequently affected.
Small, multiple, dome-shaped nodules of 2 mm to 10 mm
in diameter occur. Autoinfection is caused by wart con-
tents adhering to the epidermis.
Tweezer excision of the wart is the most effective treat-
ment.
Multiple molluscum contagiosum may appear on the face
of patients with AIDS.
The latency of molluscum contagiosum is between 14 and 50
days. Small, multiple, flat-surfaced, glossy, centrally concave,
dome-shaped nodules of 2 mm to 10 mm in diameter occur (Fig.
23.18). They contain an opaque white gruel-like substance. They
are asymptomatic except for mild itching. The trunk and extremi-
ties of infants are most frequently affected. When sexually trans-
mitted, the genitalia, lower abdomen, and medial thighs are
involved.
Warts are produced by molluscum contagiosum, a virus in the
Poxviridae family. Cells at the center of the skin lesion are dis-
torted or destroyed, giving the appearance of large hyaline bodies
(molluscum bodies) that contain large amounts of cytoplasmic
Pathogenesis, Epidemiology
Clinical features
Outline
6. Molluscum contagiosum
5. Epidermodysplasia verruciformis
Clinical images are available in hardcopy only.
Clinical images are available in hardcopy only.
Clinical images are available in hardcopy only.
Clinical images are available in hardcopy only.
Fig. 23.17 Epidermodysplasia verruciformis.
Large, flat, verrucous, reddish-brown keratotic
macules occur. The eruptions elevate and form
tumors in some cases.
C. Viral infections whose main symptom is erythematous eruptions 437
23
virus material. Molluscum contagiosum is spread by contact
infection. The virus enters through a break in the skin or a hair
follicle, and proliferates in the suprabasal cell layer of the epider-
mis. When a wart is scratched, the contents adhere to the epider-
mis and cause autoinfection. Children with atopic dermatitis are
most commonly affected. In recent years, the numbers of infec-
tions in healthy children at swimming schools, in adults from STDs,
and in patients with immunodeficiency have been increasing.
Molluscum contagiosum is characterized by lobulated, endo-
phytic hyperplasia that produces a circumscribed intracutaneous
pseudotumor. The keratinocytes contain very large intracytoplas-
mic inclusions (molluscum bodies).
Molluscum contagiosum is easily diagnosed by the clinical
features. In sudden occurrence of multiple molluscum contagio-
sum in adults, AIDS involvement is highly suspected.
Tweezer excision of the lesions is most effective. Cryo-coagu-
lation therapy and application of 40% silver nitrate are also use-
ful. Molluscum contagiosum heals spontaneously in some cases.
It is an infectious disease caused by the measles virus.
Young children are most frequently affected. It occurs in
epidemics with intervals of several years, often during
the spring.
A fever and common-cold-like symptoms occur after an
Outline
1. Measles
Treatment
Diagnosis
Pathology
Clinical images are available in
hardcopy only.
Clinical images are available in
hardcopy only.
Clinical images are available in hardcopy only.
Fig. 23.18 Molluscum contagiosum.
The small papules are glossy on the surface and umbilicated at the center.
Fig. 23.19 Histopathology of molluscum
contagiosum.
C. Viral infections whose main symptom is erythematous eruptions
Go Back to the Top To Order, Visit the Purchasing Page for Details
Вам также может понравиться
- Burden of Congenital Rubella Syndrome (CRS) in India:: A Systematic ReviewДокумент23 страницыBurden of Congenital Rubella Syndrome (CRS) in India:: A Systematic ReviewFerdian MusthafaОценок пока нет
- 12 Strategi NSДокумент2 страницы12 Strategi NSFerdian MusthafaОценок пока нет
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceОт EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceРейтинг: 4 из 5 звезд4/5 (890)
- Vertigo Blok15Документ23 страницыVertigo Blok15Mul YaniОценок пока нет
- The Yellow House: A Memoir (2019 National Book Award Winner)От EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Рейтинг: 4 из 5 звезд4/5 (98)
- 2 1 Gavic PDFДокумент38 страниц2 1 Gavic PDFFerdian MusthafaОценок пока нет
- The Little Book of Hygge: Danish Secrets to Happy LivingОт EverandThe Little Book of Hygge: Danish Secrets to Happy LivingРейтинг: 3.5 из 5 звезд3.5/5 (399)
- 10 Gallstone enДокумент5 страниц10 Gallstone enFerdian MusthafaОценок пока нет
- 013 191 UrethrographyДокумент4 страницы013 191 UrethrographyFerdian MusthafaОценок пока нет
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeОт EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeРейтинг: 4 из 5 звезд4/5 (5794)
- Acute Diarrhea Long FINAL 120604Документ24 страницыAcute Diarrhea Long FINAL 120604Aizat KamalОценок пока нет
- Never Split the Difference: Negotiating As If Your Life Depended On ItОт EverandNever Split the Difference: Negotiating As If Your Life Depended On ItРейтинг: 4.5 из 5 звезд4.5/5 (838)
- WHO NHD 02.4 Module3 EngДокумент59 страницWHO NHD 02.4 Module3 EngFerdian MusthafaОценок пока нет
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureОт EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureРейтинг: 4.5 из 5 звезд4.5/5 (474)
- World Asthma Day BK GR DR 2013Документ2 страницыWorld Asthma Day BK GR DR 2013Ferdian MusthafaОценок пока нет
- 5-Role of Endoscopic TransilluminationДокумент4 страницы5-Role of Endoscopic TransilluminationFerdian MusthafaОценок пока нет
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryОт EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryРейтинг: 3.5 из 5 звезд3.5/5 (231)
- 12 Strategi NSДокумент2 страницы12 Strategi NSFerdian MusthafaОценок пока нет
- Medical Tribune - July 2013Документ55 страницMedical Tribune - July 2013Prio Sapto UtomoОценок пока нет
- The Emperor of All Maladies: A Biography of CancerОт EverandThe Emperor of All Maladies: A Biography of CancerРейтинг: 4.5 из 5 звезд4.5/5 (271)
- 10 Cardiac Rehabilitation AfterДокумент5 страниц10 Cardiac Rehabilitation AfterFerdian MusthafaОценок пока нет
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreОт EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreРейтинг: 4 из 5 звезд4/5 (1090)
- 115 FullДокумент7 страниц115 FullFerdian MusthafaОценок пока нет
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyОт EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyРейтинг: 3.5 из 5 звезд3.5/5 (2219)
- Adj 12020Документ9 страницAdj 12020Ferdian MusthafaОценок пока нет
- Team of Rivals: The Political Genius of Abraham LincolnОт EverandTeam of Rivals: The Political Genius of Abraham LincolnРейтинг: 4.5 из 5 звезд4.5/5 (234)
- Verruca e VulgarisДокумент4 страницыVerruca e VulgarisFerdian MusthafaОценок пока нет
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersОт EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersРейтинг: 4.5 из 5 звезд4.5/5 (344)
- Template Untuk Ngeprint Cover CDДокумент2 страницыTemplate Untuk Ngeprint Cover CDFerdian MusthafaОценок пока нет
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaОт EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaРейтинг: 4.5 из 5 звезд4.5/5 (265)
- Adj 12020Документ9 страницAdj 12020Ferdian MusthafaОценок пока нет
- Template Untuk Ngeprint Cover CDДокумент2 страницыTemplate Untuk Ngeprint Cover CDFerdian MusthafaОценок пока нет
- Jurnal Pakai 2 (Diagnosis, Tatalaksana) Efusi PerikardiumДокумент9 страницJurnal Pakai 2 (Diagnosis, Tatalaksana) Efusi PerikardiumSatrya DitaОценок пока нет
- Non Malignant Reactive Disorders of LymphocytesДокумент8 страницNon Malignant Reactive Disorders of LymphocytesGilo IlaganОценок пока нет
- The Integumentary System: Functions and Disorders of the Largest OrganДокумент24 страницыThe Integumentary System: Functions and Disorders of the Largest OrganMichael Ramirez100% (1)
- Immunization - Dr. SarahДокумент14 страницImmunization - Dr. Sarahf6bk6xnppyОценок пока нет
- The Unwinding: An Inner History of the New AmericaОт EverandThe Unwinding: An Inner History of the New AmericaРейтинг: 4 из 5 звезд4/5 (45)
- Homeostatic Imbalances: in The Integumentary SystemДокумент27 страницHomeostatic Imbalances: in The Integumentary SystemMarilou Dacles IIОценок пока нет
- Food PoisoningДокумент7 страницFood PoisoningSushanta DasОценок пока нет
- Beta-Lactams and Other Antibiotics: Dosing GuideДокумент3 страницыBeta-Lactams and Other Antibiotics: Dosing GuideBobet ReñaОценок пока нет
- Isolation and Barrier Nursing 168 - June 2012Документ2 страницыIsolation and Barrier Nursing 168 - June 2012tharakaОценок пока нет
- Nursing Care Plan for Acute Pain in TonsillitisДокумент5 страницNursing Care Plan for Acute Pain in Tonsillitisesteffie21100% (1)
- AIDS Drug Side EffectsДокумент5 страницAIDS Drug Side EffectsMasooda Hassan Khan100% (3)
- Dengue Biweekly 686 20231207Документ12 страницDengue Biweekly 686 20231207Gyzka salwa gema fitriОценок пока нет
- MycologyДокумент5 страницMycologyAstari PuspaningdyahОценок пока нет
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)От EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Рейтинг: 4.5 из 5 звезд4.5/5 (119)
- Rubella & FlavivirusДокумент53 страницыRubella & Flaviviruskiedd_04Оценок пока нет
- Traditional Chinese Medicine For Human Papillomavirus (HPV) Infections: A Systematic ReviewДокумент7 страницTraditional Chinese Medicine For Human Papillomavirus (HPV) Infections: A Systematic ReviewDiego Gomes100% (1)
- Liver Function Test InterpretationДокумент89 страницLiver Function Test InterpretationprashanthshamОценок пока нет
- General Medical MicrobiologyДокумент20 страницGeneral Medical MicrobiologySadiya RhasyaОценок пока нет
- Lymphatic System and Immunity - Seeleys - NotesДокумент9 страницLymphatic System and Immunity - Seeleys - NotesLol lol100% (2)
- PTP Guideline 2014Документ35 страницPTP Guideline 2014mukeshkumar@ibasukkurОценок пока нет
- Dettol HygieneДокумент20 страницDettol Hygieneruchita1989Оценок пока нет
- A Review On Epidemiology, Pathogenesis and Treatment of LeptospirosisДокумент7 страницA Review On Epidemiology, Pathogenesis and Treatment of LeptospirosisIJAR JOURNALОценок пока нет
- PHARMACOLOGY-Drugs Acting On The Immune SystemДокумент12 страницPHARMACOLOGY-Drugs Acting On The Immune SystemMarianne Joyce ManzoОценок пока нет
- Clinical Virology Manual (PDFDrive)Документ639 страницClinical Virology Manual (PDFDrive)Shweta KumariОценок пока нет
- History of Medicine TransДокумент5 страницHistory of Medicine TransMigs MedinaОценок пока нет
- Pathophysiology of Viral GastroenteritisДокумент2 страницыPathophysiology of Viral GastroenteritisJun MingОценок пока нет
- Table 6 2 RobbinsДокумент1 страницаTable 6 2 RobbinsJessica Bittar CamargoОценок пока нет
- 31041313Документ10 страниц31041313carolinapolotorresОценок пока нет
- Pertanyaan ReferatДокумент2 страницыPertanyaan ReferatBuydh BfdsfsОценок пока нет
- Representative Questions on Fungal Lectures and LabsДокумент8 страницRepresentative Questions on Fungal Lectures and LabsYousefM.R.AlmassriОценок пока нет
- Roosendaal Study of Vaccinated vs. Unvaccinated Children in The Netherlands: Results SurveyДокумент4 страницыRoosendaal Study of Vaccinated vs. Unvaccinated Children in The Netherlands: Results Surveythomas_austin_189% (9)
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionОт EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionРейтинг: 4 из 5 звезд4/5 (402)
- Roxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingОт EverandRoxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingРейтинг: 5 из 5 звезд5/5 (4)