Академический Документы
Профессиональный Документы
Культура Документы
Pathophysiology Lecture Notes Topic: Heart Failure Lecturer: Dr. Dexter MD FRC Path Upadhya
Загружено:
applesncoreОригинальное название
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Pathophysiology Lecture Notes Topic: Heart Failure Lecturer: Dr. Dexter MD FRC Path Upadhya
Загружено:
applesncoreАвторское право:
Доступные форматы
1
Pathophysiology Lecture Notes
Topic: HEART FAILURE
Lecturer: Dr. Dexter MD FRC Path
Upadhya
2
PATIENT 1:
A 58-year-old man complains that he fatigues easily and
that each night his ankles swell. He reports that these
symptoms have developed slowly over the past 4 months.
He states that he often has to get up at night either to urinate
or catch my breath,. He denies any episodes of chest pain.
The patients record shows that he has a history of
hypertension; his BP was 160/110 at his last visit. He was
given prescriptions for antihypertensive medications, but he
never filled them or followed up for BP monitoring.
His vital signs are: pulse, 89 beats/min; respiratory rate, 32
breaths/min; temperature, 99F; BP, 175/120 mmHg.
Physical examination reveals 1+ pitting pedal edema, cold
and clammy skin, an enlarged liver, S3 and S4 heart
sounds, and bibasilar crackles in the lungs with slightly
diminished breath sounds.
3
QUESTIONS:
1. What is the likely diagnosis?
2. What are the differentials you suspect in this
patient?
3. What hemodynamic abnormalities predispose to
his condition?
4. What is cause for the bibasilar crackles in the
lungs?
5. What is the pathogenic mechanism responsible for
the bibasilar crackles?
6. Give basis for other clinical presentations of this
patient
7. What are the most common causes of death in this
condition?
9. What would be the radiological feature of chest X-
ray of this patient?
4
Differential diagnosis for patient 1:
Congestive heart failure
Renal failure
Most likely diagnosis in this patient is:
Congestive heart failure (CHF)
Reasons:
Ankle edema (pitting type)
Dyspnea in the night
Cold and clammy skin
Enlarged liver
Audible S3 and S4
5
Congestive Heart Failure (CHF)
Definition of CHF:
Inadequate pumping function of the heart,
leading to congestion and resulting in fluid
accumulation in the lungs and peripheral
tissues
The symptoms and signs depend on:
Onset acute/chronic
Primary involvement of the side left/right
ventricles or both
6
Classification of Heart Failure (NYHA)
Can complete any activity
requiring 7 mets:
Carry 11 kg up 8 steps
Carry objects weighing 36 kg
Shovel snow
Spade soil
Ski
Play squash, handball or
basketball
Jog/walk 8 km/h
None Ordinary
physical
activity does
not cause
undue fatigue,
dyspnea,
palpitation
I
Example Limitation Definition NYHA
Class
1 MET is the rate of energy expenditure while at rest. A 4 MET activity expends
4 times the energy used by the body at rest. If a person does a 4 MET activity
for 30 minutes, he or she has done 4 x 30 = 120 MET-minutes (or 2.0 MET-
hours) of physical activity. A person could also achieve 120 MET-minutes by
doing an 8 MET activity for 15 minutes.
7
Can complete any activity
requiring 5 mets:
Garden
Roller skate
Walk 7 km/h on level ground
Slight Ordinary
physical
activity causes
fatigue,
dyspnea,
palpitation, or
angina
II
Example Limitation Definition NYHA
Class
8
Can complete any activity
requiring 2 mets:
Shower or dress without
stopping
Strip and make bed
Clean windows
Play golf
Walk 4 km/h
Moderate Comfortable at
rest; less than
ordinary
physical activity
causes fatigue,
dyspnea,
palpitation, or
angina
III
Example Limitation Definition NYHA
Class
9
Cannot do or cannot
complete any activity
requiring 2 mets; cannot do
any of the above activities
Severe Symptoms at
rest; any
physical activity
increases
discomfort
IV
Example Limitation Definition NYHA
Class
10
Congestive Heart Failure may start with:
Left Ventricular Failure (LVF)
Or
Right ventricular failure (RVF)
11
LEFT VENTRICULAR FAILURE (LVF)
Clinical Presentation:
Breathlessness (dyspnea) -
particularly when lying down (orthopnea)
or at night [paroxysmal nocturnal
dyspnea (PND)]
Blood-tinged sputum (hemoptysis)
Chest pain (occasional)
Fatigue, nocturia, and confusion
12
Etiology of LVF:
Inappropriate workloads placed on the heart:
-Volume overload (example: MR or AR)
-Pressure overload (example: systemic
hypertension)
Restricted filling of the heart (example: constrictive
pericarditis)
Myocardial loss - as in MI
Decreased myocardial contractility as in
poisoning or infections
13
Pathophysiologic changes associated
with heart failure:
Hemodynamic changes
Neurohumoral changes
Cellular changes
14
Heart failure can arise from:
Systolic dysfunction
Diastolic dysfunction
Combination of both
In most patients, a combination of systolic
and diastolic dysfunction is responsible for
the symptoms of heart failure
Hemodynamic Changes:
15
Causes of Systolic Dysfunction
Coronary artery disease
Valvular heart disease
Hypertension
Aging
Dilated cardiomyopathy
16
Hemodynamic Changes in
Systolic dysfunction
Pressure-volume relationship shows a
low ejection with a high or low ventricular
pressure during ejection
Reduction in the stroke volume (SV) & a
decrease in cardiac output (CO)
(CO = SV x HR)
17
Normal Left ventricular pressure-volume loop
1
2
3
4
EDV
Mitral valve
closes(S
1
)
Aortic valve
opens
1 to 2 : Isovolumetric ventricular contraction
2 to 3 : Left ventricular ejection
3 to 4 : Isovolumetric ventricular relaxation
4 to 1 : Left ventricular filling
Aortic valve
closes(S
2
)
ESV
Mitral valve
opens
SV
18
Changes in left ventricular P-V loop in
Systolic Dysfunction:
Example: Patient with systemic hypertension
(Increase in afterload on LV)
L
e
f
t
v
e
n
t
r
i
c
u
l
a
r
p
r
e
s
s
u
r
e
Left ventricular volume
A
B
Loop A: Normal
Loop B: Increased
afterload
Increase in ventricular
pressure during systole
Decrease in SV
Increase in ESV
19
Changes in left ventricular P-V loop in
Systolic Dysfunction:
Example: Patient with acute Myocardial Infarction
(Loss of myocardium)
Loop A: Normal
Loop B: Loss of myocardium
Decrease in ventricular
pressure during systole
Increase in ventricular
diastolic pr
Decrease in SV
Increase in ESV
20
To maintain cardiac output, the heart responds with
the following compensatory mechanisms:
i) Increased preload (Frank-Starling relationship)
Heart operates at a larger end-diastolic pressure
ii) Increased release of catecholamines
iii) Cardiac muscle can hypertrophy and ventricular
volume can increase
When each of these mechanisms reach certain
limit, the heart ultimately fails
Hemodynamic Changes in
Systolic dysfunction
21
i) Compensated LV failure - SV is partially
restored due to increased preload (EDV) shown
by the PV loop C:
(Curve B: PV loop soon after loss of myocardium)
22
Frank-Starling relationship
Systolic contractile performance (represented by
stroke volume or CO) is proportional to preload within
the normal physiologic range
23
ii) SV is partially restored by an Increased
release of catecholamines
abcd PV loop soon after heart failure
abcd Change in PV loop due to catecholamines
24
Diastolic dysfunction (also called HF
with preserved systolic function or HF
with preserved EF)
Causes: Any disease that produces
Decreased relaxation (Eg:constrictive
pericarditis)
Increased stiffness of ventricle
(Eg:hypertrophic cardiomyopathies)
25
Hemodynamic Changes in
Diastolic dysfunction
In diastolic dysfunction ventricular filling is impaired,
resulting in reduced ventricular end-diastolic volume,
increased end-diastolic pressure, or both
Diastolic pressure-volume curve is shifted to the
left, with an accompanying increase in left ventricular
end-diastolic pressure
Contractility and ejection fraction (EF) remain
normal
Markedly reduced LV filling can produce low CO
and systemic symptoms
Elevated left atrial pressures can produce
pulmonary congestion 26
Volume (mL)
P
r
e
s
s
u
r
e
(
m
m
H
g
)
Diastolic Pressure-
Volume curve
abcd PV loop before heart failure (control)
abcd Change in PV loop due to failure
Changes in left ventricular P-V loop in
Diastolic Dysfunction:
27
Stroke Volume (SV)
SV is the volume of blood ejected by each
ventricle in a beat
It is the difference between end diastolic
volume and end systolic volume
SV = (EDV ESV) ml per beat
SV increases with an increase in EDV
SV increases with a decrease in ESV
When both increase in EDV and decrease
in ESV occur, SV increases maximally
28
Ejection Fraction (EF)
EF is the fraction of end diastolic volume
that is ejected in one beat
SV
EF = -----------
EDV
It is an index of myocardial contractility
Increase in EF indicates positive inotropic effect
Decrease in EF indicates negative inotropic effect
29
Neurohumoral Changes in Heart
Failure:
Increased sympathetic activity
Activation of Renin-Angiotensin-
Aldosterone system
Increased release of ADH
(vasopressin)
Release of cytokines and peptides
30
Neurohumoral Changes (continued):
Increased sympathetic activity:
-Occurs early in the heart failure
-Elevated plasma norepinephrine levels
-Increased cardiac contractility and rate
-Initially it may be helpful to improve SV
-Continued effect leads to increased preload
and afterload which can worsen heart failure
31
Neurohumoral Changes (Continued):
Activation of renin-angiotensin-aldosterone
system (RAAS):
-Release of renin due to reduced renal blood flow
-Fluid and salt retention causing increase in preload
-Consequence of continued hyperactivity of RAAS
initiates a vicious circle:
Severe vasoconstriction combined with increased
plasma volume Increased both preload & afterload
Further reduction in cardiac output Further
reduction in glomerular filtration rate RAAS
activation (cycle repeats)
32
Neurohumoral Changes (Continued):
Other cytokines/peptides in heart failure:
The interleukins (ILs) IL-1 accelerates myocyte
hypertrophy
Tumor necrosis factor- (TNF-) causes myocyte
hypertrophy and cell death (apoptosis)
Endothelin stimulates vasoconstriction in pulm
vasculature, myocyte growth, myocardial fribrosis
Atrial natriuretic peptide (ANP) and Brain natriuretic
peptide (BNP) cause natriuresis and vasodilatation
33
Brain natriuretic peptide (BNP):
Also known as beta-type natriuretic
peptide
Secreted by ventricular myocytes when
stretched
Level in circulation is increased during
CHF
Measurement of this peptide in
circulation is important in differential
diagnosis and evaluation of heart failure
34
Inefficient intracellular calcium
handling
Adrenergic desensitization
Myocyte hypertrophy
Cell death (apoptosis)
Myocardial fibrosis
The cellular changes in ventricular
myocardium in heart failure is
collectively known as ventricular
remodeling
Cellular Changes:
35
Basis for clinical presentations in
patient with CHF due to LVF
Clinical Presentation:
Breathlessness (dyspnea) -
particularly when lying down (orthopnea)
or at night [paroxysmal nocturnal
dyspnea (PND)]
Blood-tinged sputum (hemoptysis)
Chest pain (occasional)
Fatigue, nocturia, and confusion
36
Hemodynamic Basis for
Heart Failure Symptoms: Dyspnea
37
i) Shortness of Breath (Dyspnea):
Elevated pulmonary capillary pressures due to an
elevated left ventricular and atrial pressures
pulmonary venous congestion and pulmonary
edema
Stimulation of juxtacapillary J receptors resulting
in reflex shallow and rapid breathing
Edema of the bronchial walls can lead to small
airway obstruction and produce wheezing known
as "cardiac asthma"
38
ii) Shortness of Breath (Dyspnea):
Replacement of air in the lungs by blood or
interstitial fluid
Reduction of vital capacity, restrictive physiology
and closure of small airways
The work of breathing increases as the patient
tries to distend stiff lungs, which can lead to
respiratory muscle fatigue and the sensation of
dyspnea
39
iii) Shortness of Breath (Dyspnea):
Ventilation-perfusion mismatch
Widening of the alveolar-arterial O2 gradient,
hypoxemia and increased dead space
Dyspnea
40
iv) Cause for Orthopnea:
In the recumbent position because of reduced
blood pooling in the extremities and abdomen
Increase in blood return leads to marked
elevations in ventricular pressures
Orthopnea
Patients usually learn to minimize orthopnea by
sleeping with the upper body propped up by two
or more pillows
41
v) Cause for Paroxysmal Nocturnal Dyspnea:
Changes during sleep such as:
-Reduced adrenergic support
-Increased vagal activity
-Normal nocturnal depression of resp center
Theses changes aggravate pulmonary pooling of
blood causing sudden onset of severe
respiratory distress at night called paroxysmal
nocturnal dyspnea (PND)
42
Physical examination in CHF due to LVF:
Elevated respiratory rate and heart rate
Pale, cold and sweaty skin
Peripheral pulse may reveal pulsus alternans
Auscultation of the lungs bibasilar rales,
described as "crackling leaves"
Bases of the lung fields may be dull to percussion
Cardiac examination: apical impulse is often
displaced laterally and sustained; S3 and
sometimes S4 can be heard
Because many patients with LVF also have
accompanying failure of the RV, signs of right
ventricular failure may also be present
43
Physical Examination finding:
Rales, Pleural Effusion:
Increased fluid in the alveolar spaces can be heard
as rales. Increased capillary pressures can also
cause fluid accumulation in the pleural spaces
Displaced and Sustained Apical Impulse:
When the apical impulse can be felt during the
latter part of systole, it is sustained. Sustained
impulses suggests an increase in left ventricular
volume or mass. In addition, when left ventricular
volume is increased as a compensatory
mechanism of heart failure, the apical impulse is
displaced laterally
44
Chest x-ray characterized by bats wing
density, cardiac enlargement in patient
with pulmonary edema due to LVF
45
Third Heart Sound (S3):
S3 is a low-pitched sound that is heard during rapid
filling of the ventricle in early diastole.
The increased end-systolic volumes and pressures
characteristic of the failing heart are responsible for
the prominent S3
S3 is a consistent physical finding in CHF
When it arises because of left ventricular failure, the
third heart sound is usually heard best at the apex
Physical Examination finding:
46
Fourth Heart Sound (S4):
It is a low-pitched sound at end-diastole that occurs
concomitantly with atrial contraction
S4 can sometimes be heard if the ventricles are stiff
It is best heard laterally over the apex at the point of
maximal impulse, particularly when the patient is
partially rolled over onto the left side
S4 is commonly heard in any patient with heart
failure resulting from diastolic dysfunction or IHD
Physical Examination finding:
47
Phonocardiogram showing S3 and S4 along
with EKG
EKG
Systole Diastole
48
Pale, Cold, and Sweaty Skin:
Pale & Cold: Patients with CHF failure often have
peripheral vasoconstriction in order to maintain
blood flow to the central organs and head
Sweating: Increased sweat gland activity as a part
of thermoregulation when body heat cannot be
dissipated through the constricted vascular bed of
the skin
Physical Examination finding:
49
Patient 02:
A 44-year-old obese man is referred for evaluation of day
time hypersomnolence. Patient reports falling asleep
while driving and has been involved in multiple car
accidents in the past one year. His wife tells that he has
15-20 seconds of apnea during sleep and is a heavy
snorer.
PE: Pulse 94; BP 170/90; He is 5 10 and weighs 300 lbs;
He has bilateral lower limb edema; Distended neck veins
cardiac examination: Right ventricular heave, Right
sided S3 and S4; P2 component of S2 is loud; Systolic
murmur heard best at the right lower sternal border
50
Most likely diagnosis in this patient is:
Obstructive Sleep Apnea complicating
cor pulmonale
Other differentials:
Narcolepsy
Major depression
Sleeping sickness
Chronic fatigue syndrome
Evidences of right ventricular failure secondary to
pulmonary hypertension suggests cor pulmonale
51
Cor pulmonale:
Condition characterized by enlargement
of right ventricle with failure as a sequel
of pulmonary disease
Pulmonary diseases:
-Pulmonary vascular diseases
-COPD
52
Right ventricular failure (RVF)
Causes:
-Secondary to LVF because of the increased
afterload placed on the right ventricle
-Increased flow from a congenital shunt can cause
reactive pulmonary artery constriction, increased
right ventricular afterload
-As a sequel of pulmonary disease (cor pulmonale)
because of destruction of the pulmonary capillary
bed or hypoxia-induced vasoconstriction of the
pulmonary arterioles
-Right ventricular ischemia or infarction
53
Pathophysiology of acute RVF: the vicious cycle
54
Pathophysiology of RVF:
High afterload on right ventricle
RV pressure exceeding LV pressure
Interventricular septum bowing to the left
ventricular chamber
Insufficient filling of the left ventricle
Pulmonary congestion
Rarely, the bowing can be so severe that left ventricular
outflow can be partially obstructed. This phenomenon is
termed a "reversed Bernheim effect."
55
Bernheim's syndrome or effect:
Systemic congestion resembling the
consequences of right heart failure
(enlarged liver, distended neck veins, and
oedema) without pulmonary congestion in
subjects with left ventricular enlargement
from any cause
A reduction in the size of the right
ventricular cavity occurs due to
encroachment by the hypertrophied or
aneurysmal ventricular septum
56
Clinical Presentation of RVF:
Shortness of breath
Pedal edema
Abdominal pain
57
Basis for shortness of breath in RVF:
i) Left ventricular failure causing pulmonary edema
ii) Existing pulmonary diseases such as pulmonary
embolus, chronic obstructive pulmonary disease
iii) Congestion of the hepatic veins with formation
of ascites which produces restricted diaphragmatic
Movements and dyspnea
iv) Reduced right-sided cardiac output leading to
Acidosis, hypoxia, and air hunger
58
If the cause of right-sided failure is a left-
sided defect such as mitral stenosis, the
onset of right heart failure can sometimes
lessen the symptoms of pulmonary edema
because of the decreased load placed on
the left ventricle
59
Basis for Pedal Edema, Anasarca, Ascites:
Right ventricular failure
Elevated right-sided pressure
Accumulation of fluid in the systemic veins and
venous congestion
Dependent edema (swelling of the feet and
legs), Generalized edema (anasarca), Ascites
(edema is of pitting type)
60
Basis for the Abdominal pain:
Expansion of the liver from fluid accumulation
can cause distention of the liver capsule with
accompanying right upper quadrant abdominal
pain
61
Physical examination in RVF:
Elevated jugular venous pressures &
Hepatojugular reflux
Sustained systolic heave of the sternum (due
to right ventricular hypertrophy
S3 heard best at the sternal border
Because the most common cause of right
ventricular failure is left ventricular failure,
signs of left ventricular failure are often also
present
62
Elevated Jugular Venous Pressure:
Elevated atrial pressures indicate that the
preload of the ventricle is adequate but
ventricular function is decreased and fluid is
accumulating in the venous system
Other causes of elevated jugular pressures:
-Pericardial tamponade
-Constrictive pericarditis
-Massive pulmonary embolism
63
EKG
JVP
Normal Heart Sounds
64
Hepatojugular reflux:
Pressing on the liver for approximately 5 sec
leads to displacement of blood into the vena
cava and an increase in jugular venous
pressure
65
P-V loop in progressive LVF
Curve A: Normal
Curve B: Immediate effect of reduced
contractility following AMI;
Compensation not started
Curve C: Compensated LV failure - SV is partially restored
due to increased preload
Curve D: Decompensated LV failure despite increase in
preload, SV remains low and heart is over stretched
1
Pathophysiology Lecture Notes
Topic: EKG & CARDIAC ARRYTHMIAS
Lecturer: Dr. S. Upadhya
2
Definition and Types of Arrhythmias
Arrhythmias are abnormal rhythms of
the heart
Classification:
Based on heart rate:
Bradyarrhythmias & Tachyarrhythmias
Based on site of origin:
Supraventricular & Ventricular
Based on mechanism:
Automatic, Triggered, or Re-entrant
arrhythmias
3
Clinical presentation of patients
with arrhythmias:
Palpitation
Lightheadedness
Syncope
Nonspecific presentations:
fatigue, dyspnea, or exertional
intolerance
4
Patient 01:
A 66-year-old man complains sudden onset of
transient loss of consciousness and postural tone
since 8 months. The episode lasts for about 10-15
seconds and the patient recovers promptly without
any resuscitative measures. Episodes are often
associated with palpitations and lightheadedness.
PE: BP 95/56 mm Hg
Heart Rate - 44 beats/min, regular
JVP: shows prominent a waves
Rest of her physical examination is unremarkable
EKG: Number of P waves exceed that of QRS; P-R
interval-not measurable; Long R-R intervals
5
Most likely diagnosis in patient 01 is:
Complete Heart Block
Other differentials are:
Sick sinus syndrome
Ventricular tachycardia
Aortic stenosis
Pulmonary stenosis
Postural hypotension
Vasomotor syncope
The presenting symptom in this patient is:
Syncope
6
Causes for Cardiac Syncope:
Organic heart diseases-Aortic stenosis, mitral
stenosis, hypertrophic cardiomyopathy, and
ischemic heart disease
Syncope due to a sudden drop in CO-aortic
dissection and pericardial tamponade
Arrhythmias-both bradycardic or tachycardic
type
7
Syncope due to cardiac arrhythmias:
Bradyarrhythmias:
Sinus node disease, second- and third-degree
heart block and bradycardia associated with
pacemaker malfunction
Tachyarrhythmias:
Ventricular tachycardia, torsades de pointes,
Ventricular fibrillation and supraventricular
tachycardia
Patients with bradycardia often experience sudden loss of
consciousness without warning, whereas those with
tachyarrhythmias are more likely to describe palpitations
8
Components of conducting system of the Heart
1. Sinoatrial node
3. Atrial internodal
pathways
2. Atrioventricular node
4. Bundle of His
5. Bundle branches
6. Purkinje fibers
The bundle of His normally forms the only electrical
connection between the atria and the ventricles 9
Sequence of spread
of cardiac action
potentials
AP originates at SA node
AP conducts to AV node
rapidly
AV delay occurs
At the same time
spreads over atria slowly
Spreads rapidly
to the apex
through bundle
of His and
bundle branches
Spreads rapidly
over both the
ventricles from
apex to base
through the
Purkinje fibers
10
Diagnosis of cardiac arrhythmias:
The 12-lead electrocardiogram
Vagal maneuvers carotid massage
Electrophysiological (EP) studies - The ability to
trace specific pathways and map conduction
11
Certain basics of EKG/ECG:
The sites selected for ECG recording
Limbs: Right arm (RA), Left arm (LA), Left leg (LL)
Leads connecting limbs are called Limb leads
Leads kept on chest wall are called Chest leads
Three lead systems are:
Standard bipolar limb leads (3 in number):
Lead I, Lead II and Lead III
Augmented unipolar limb leads (3 in number):
aVR, aVL and aVF
Unipolar chest leads (6 in number):
V1, V2, V3, V4, V5 and V6
12
Genesis of EKG waves
P
S
P wave:
atrial
depolarization
wave
QRS complex:
Ventricular
depolarization
wave
Set of three waves
Due to changing
direction of wave
of depolarization
in sequence
SA node
13
Genesis of ECG waves
Ventricles remain in
depolarized state for
sometime before they
get repolarized
No potential is recorded
Corresponds to plateau
phase of ventricular AP
T
T
T wave: Ventricular repolarization wave
14
Normal ECG tracing
ECG paper: Contains 1 mm x 1 mm boxes
V
o
l
t
a
g
e
(
m
V
)
Time in sec
0.1 mV
0.04 second
Paper speed: 25 mm per second
1 mm on x-axis = 1/25 = 0.04 sec
15
Normal ECG waves, segments & intervals
PR
interval QT interval
ST
segment
V
o
l
t
a
g
e
Time (sec)
PR
segment
QRS
interval
16
Frontal Plane
17
Horizontal Plane
18
Calculate PR, QRS and QT intervals in this ECG
PR interval = 0.04 x 4 = 0.16 sec (Normal: 0.12-0.20 sec)
QRS interval = 0.04 x 2 = 0.08 sec (Normal: 0.08-0.10 sec)
QT interval = 0.04 x 8= 0.34 sec (Normal: 0.32-0.43 sec)
19
Heart rate can be calculated from ECG
R-R interval gives one cardiac cycle length
60
Heart rate = ---------------------- beats per minute
R-R interval
R-R interval
60 60
Heart rate of above ECG = ----------- = -------- = 50 beats per minute
30x.04 1.2
20
R-R interval
What is the heart rate of this patient?
R-R interval = 23 boxes = 23x0.04 = 0.92 sec
Heart rate = 60/0.92 = 65 beats/min
R-R interval varies inversely with heart rate
Lead II ECG
300
150 100 75 60
21
ECG findings:
Rhythm - Regular
Rate 60 to100 beats/min
QRS Duration - Normal
P Wave - Visible before each QRS complex
P-R Interval - Normal (<5 small Squares. Anything above
and this would be 1st degree block)
Indicates that the electrical signal is generated by the
sinus node and travelling in a normal fashion in the heart
Normal Sinus Rhythm
22
Bradyarrhythmias:
TWO basic mechanisms for
bradyarrhythmias:
1. Reduced activity of the pacemaker
2. Conduction block
23
Action Potential of SA node (pace maker):
Has got only three phases
M
e
m
b
r
a
n
e
p
o
t
e
n
t
i
a
l
(
m
V
)
0
- 65
Phase
4
Phase 3
Phase 0
Has an unstable resting phase (phase 4)
called prepotential or pacemaker potential
which is responsible for automaticity of
the SA node
Threshold
24
Mechanism of Bradyarrhythmias: 1. Reduced
automaticity of the sinus node:
-Result in slow heart rates or pauses
-If sinus node pacemaker activity ceases, the
heart will usually be activated at a slower rate by
other cardiac tissues with pacemaker activity
(usually AV node)
-Reduced sinus node automaticity can occur
during periods of increased vagal tone (sleep,
carotid sinus massage), with increasing age and
secondary to drugs (beta-blockers, calcium
channel blockers)
25
Effect of stimulation of Vagus (parasympathetic)
nerve on heart:
On SA node: Decreases heart rate
Known as negative chronotropic effect
Mechanism: ACh binds with M2 receptors in SAN;
Decrease in rate of rise of phase 4 and hyperpolarization
of resting membrane potential lead to slow heart rate
Norm
al
Normal heart rate
Heart rate after
parasympathetic
nerve stimulation
26
EKG showing bradyarrhythmia due to SA Node pause.
The cardiac impulse is initiated by the junctional tissue
(AV node), producing junctional escape beat (J) in EKG
P P P
27
Mechanism of Bradyarrhythmias: 2. Conduction
block:
The AV node and His bundle are the most
vulnerable sites for blocked conduction between
the atria and ventricles
Atrioventricular block can occur:
-Increasing age
-Increased vagal input
-Congenital disorders such as muscular dystrophy,
tuberous sclerosis, and maternal SLE
-Acquired disorders such as sarcoidosis, gout,
Lyme disease, SLE, ankylosing spondylitis, and
coronary artery disease
28
Common Bradyarrhythmias:
Sinus bradycardia
First-degree heart (AV) block
Second-degree heart (AV) block
Third-degree heart (complete AV) block
29
Patient 02:
A 35-year-old male is referred to a cardiology
clinic for evaluation. Patient is asymptomatic. He
was incidentally noted to have bradycardia.
Physical examination:
Pulse: 40/min, regular BP: 90/46 mm Hg
JVP: Normal
Heart sounds: Normal S1 & S2 without any
murmurs, gallops
Lab:
EKG: Markedly prolonged RR intervals with HR
of 40 beats/min; PR interval & QRS interval are
within limits.
Blood: Normal; Chest X ray: Normal
30
Most likely diagnosis in this patient:
Sinus Bradycardia
Differential diagnosis:
Hypothyroidism
Hypothermia
Digitalis toxicity
Beta-blocker toxicity
Physiological causes of Bradycardia:
-Increased vagal tone
-Sleeping
31
Sinus Bradycardia
ECG findings:
Rhythm Regular (constant RR intervals)
Rate - less than 60 beats per minute (long RR int)
QRS Duration - Normal
P Wave - Visible before each QRS complex
P-R Interval - Normal
Examples: Athletic person, increased vagal tone, Inferior wall MI,
Hypothyroidism, Patient with brain injury with raised intracranial
tension, Drug toxicity (Digitalis, Beta-blockers & Ca+2 channel
blocker)
32
1st Degree AV Block
ECG findings:
Rhythm Regular
Rate - Normal
QRS Duration - Normal
P Wave - Ratio 1:1
P Wave rate - Normal
P-R Interval - Prolonged (>5 small squares)
Mechanism: A conduction delay through the AV node but
all electrical signals reach the ventricles. This rarely causes
any problems by itself.
Example: Trained athletes
33
2nd Degree Block Mobitz Type 1 (Wenckebach)
ECG findings:
Rhythm - Regularly irregular
Rate - Normal or Slow
QRS Duration - Normal
P:QRS ratio - 1:1 for 2,3 or 4 cycles then 1:0.
P Wave rate - Normal but faster than QRS rate
P-R Interval - Progressive lengthening of P-R interval until a
QRS complex is dropped
Conduction block of some, but not all atrial beats getting
through to the ventricles at the AV node
Dropped QRS complex
34
Second degree Heart Block
Mobitz Type I or Wenchebach:
35
2nd Degree Block Mobitz Type 2
ECG findings:
Rhythm - Regular between the conducted beats
Rate - Normal or Slow
QRS Duration may be prolonged (infranodal block)
P:QRS ratio - 2:1, 3:1
P Wave rate - Normal but faster than QRS rate
P-R Interval - Normal or prolonged but constant
Cause: Electrical excitation sometimes fails to pass through
the A-V node or bundle of His downwards
Electrical conduction of the conducted beats is the same
always (hence have a constant P-R interval)
Dropped QRS complex
Dropped QRS complex
36
3rd Degree Block: Complete AV block
ECG findings:
Rhythm - Regular
Rate - Slow
QRS Duration - Prolonged
P Wave - Unrelated to QRS (AV dissociation)
P Wave rate - Normal but faster than QRS rate
P-R Interval - Variation
No atrial impulses pass through the atrioventricular node.
Ventricles generate their own impulse through an 'escape
mechanism' from a focus somewhere within the ventricle at
a regular, slow rate 37
Tachyarrhythmias:
THREE basic mechanisms for
Tachyarrhythmias:
1.Increased automaticity of pacemaker
2.Spontaneous depolarizations
3.Reentrant circuit most common
38
Mechanism of Tachyarrhythmias:1.Increased
automaticity of the pace maker:
More rapid phase 4 depolarization of the action
potential of SA node leads to faster heart rate
Before increased HR
With increased HR
Phase 4
Examples: Sinus Tachycardia as in hyperthyroidism,
Anxiety, Pheochromocytoma and pulm embolus 39
Sinus Tachycardia
ECG findings:
Rhythm - Regular
Rate - More than 100 beats per minute
QRS Duration - Normal
P Wave - Visible before each QRS complex
P-R Interval - Normal
The impulse generating the heart beats are normal,
but they are occurring at a faster pace than normal
Occurs in: Exercise, stress, fright, fever
40
EAD=Early Afterdepolarization
DAD=Delayed Afterdepolarization
Ventricular
Action Potential
Mechanism of Tachyarrhythmias: 2.
Spontaneous depolarizations:
If repolarization is delayed (longer plateau
period), spontaneous depolarizations can occur
in phase 3 or phase 4 of the ventricular/atrial
action potential
These depolarizations can repetitively reach
threshold and cause tachycardia
41
Summary of ionic basis of phases of action
potential from Ventricular muscle fiber
Current
P
h
a
s
e
0
Phase 1
Phase 2 (Plateau phase)
P
h
a
s
e
3
Phase 4
42
Examples of tachyarrhythmias from
spontaneous depolarizations (EAD/DAD) are:
- Long QT syndrome - Due to several specific
ion channel defects
-Torsades de pointes
CIoss III onfiorrhyfhmic drugs bIock I
+
chonneIs ond
hence fheir foxicify moy produce fochyorrhyfhmios
43
EKG
Long QT syndrome: Reduced function of potassium
channels leads to a prolonged plateau period, leading
to a prolonged QT interval
These patients are prone
to triggered activity
because of reactivation of
sodium and calcium
channels [early
afterdepolarizations (EAD)]
Triggered activity in the
ventricles can lead to life-
threatening ventricular
arrhythmias
Action
Potential
44
Torsades de pointes:
A twisting polymorphic ventricular
tachycardia, is a specific type of triggered
arrhythmia that is observed in situations where
the QT interval has been prolonged
A cardiac arrhythmia, which may cause
blackouts or even sudden death
The phrase "Torsades de Pointes" is French and
literally means "twisting of the points", referring to
the characteristic appearance of the EKG during
the rhythm abnormality
45
Torsades de pointes is dangerous because it may
turn into fatal ventricular fibrillation (VF)
46
Mechanism of Tachyarrhythmias: 3.
Reentrant circuit:
Re-entry requires an area of slow conduction,
unidirectional block, and two pathways:
A- Block at slow tract & fast moves down
B- Slow moves retrograde in fast tract and
blocks the incoming next fast
C- Retrograde fast reenters in the slow tract
A
B C
47
Examples for re-entrant arrhythmias:
-Aatrial tachycardia, atrial flutter or atrial
fibrillation
-Supra Ventricular reentrant tachycardia as in
Wolff-Parkinson-White syndrome
-Ventricular Tachycadia
48
Patient 03:
A 17-year-old boy is referred to a cardiologist by
a primary care physician for evaluation of
recurrent spells of dizziness. During the
episodes, he feels intense anxiety with
palpitations and breathlessness. He is
asymptomatic in between episodes; There is no
h/o chest pain or syncope.
Physical examination:
No abnormalities detected
Lab:
EKG: Short PR interval; wide QRS with a slurred
upstroke.
Blood: Normal; Chest X ray: Normal
49
Most likely diagnosis in this patient:
Wolff-Parkinson-White Syndrome
Differential diagnosis:
Atrial fibrillation
Atrial flutter
Syncopy
Nodal re-entry tachycardia
Ebstein anomaly
Electrophysiologic studies confirm presence
of a bypass tract (Bundle of Kent)
50
Wolff-Parkinson-White syndrome:
An accessory atrioventricular connection is found
in approximately 1 in 1000 persons
Because part of the ventricle is "preexcited" over
the accessory pathway rather than via the AV
node, the surface ECG shows a short PR interval
and a relatively wide QRS with a slurred upstroke,
termed a delta wave
If enough time has elapsed so that the accessory
pathway has recovered excitability, the cardiac
impulse can travel in retrograde fashion to the
atria over the accessory pathway and initiate a
reentrant supraventricular tachycardia
51
In WPW syndrome, the
Bundle of Kent (the Extra
Pathway) can Complete the
Circuit allowing Re-Entry
tachycardia
Wolff-Parkinson-White syndrome:
EKG findings:
Short PR interval
Wide QRS
Delta wave
(at arrow)
52 53
Patient 04:
A 46-year-old woman arrived in the ER complaining
of sudden onset of palpitations, lightheadedness,
and shortness of breath. These symptoms began
approximately 2 hours previously.
PE: BP 95/70 mm Hg
Heart Rate - averages 170 beats/min, regular
Rest of her physical examination is unremarkable
EKG: abnormal P waves; P-R intervals are within
normal limits; normal QRS complexes
54
Questions:
What is the likely cause of the patients high
heart rate?
Why was the patient lightheaded, dizzy, and
short of breath?
What electrophysiological abnormality has
caused this condition?
How do you interpret the EKG findings of this
patient?
55
Most likely diagnosis in patient is:
Supraventricular Tachycardia
Other differentials are:
Ventricular tachycardia
Acute MI
Pulmonary embolism
56
Tachyarrhythmias are also classified as:
Supraventricular Tachycardia (SVT)
Ventricular Tachycardia (VT)
To differentiate them, look at the QRS complex:
If the QRS complex is narrow - SVT
If the QRS complex is wide VT
57
Narrow, QRS complex:
Indicates that depolarization of the ventricles must
be occurring normally over the specialized
conduction tissues and the arrhythmia must be
originating at or above the AV node.
Tachycardia with such QRS are - SVT
Wide QRS complex:
Indicates that ventricular depolarization is NOT
occurring normally over the specialized conduction
tissues
Tachycardia with such QRS are - VT
58
SVT: Narrow QRS
VT: Wide QRS
59
Supraventricular Tachycardia (SVT)
ECG findings:
Rhythm - Regular
Rate - 140-220 beats per minute
QRS Duration - Normal (narrow)
P Wave - Often buried in preceding T wave
P-R Interval - Depends on site of supraventricular pacemaker
Impulses stimulating the heart are not being generated by
the sinus node, but instead are coming from a collection of
tissue around and involving the atrioventricular (AV) node
60
Commonly occurring
SVTs:
Atrial Tachycardia
Atrial Flutter
Atrial Fibrillation
AV nodal reentrant
tachycardia
Atrioventricular
reentrant tachycardia
61
Atrial Flutter
ECG findings:
Rhythm - Regular
Rate - Around 110 beats per minute
QRS Duration - Usually normal
P Wave - Replaced with multiple F (flutter) waves, usually at
a ratio of 2:1 (2F - 1QRS) but sometimes 3:1
P Wave rate - 300 beats per minute
P-R Interval - Not measurable
As with SVT the abnormal tissue generating the rapid heart
rate is in the atria; the AV node is not involved in this case
62
Patient 05:
A 44-year-old male complains of occasional
palpitations, shortness of breath, dizziness and
chest discomfort.
Physical examination:
Pulse: Irregularly irregular
JVP: absent a waves
Heart sounds: variable intensity S1 with
occasional S3
Lab:
EKG: Variable ventricular rate (90-190); Irregular
RR intervals.
Blood: CK-MB normal
Chest X ray: Normal
63
Most likely diagnosis in this patient:
Atrial Fibrillation (AF)
Differential diagnosis:
Atrial tachycardia
Atrial flutter
Supraventricular tachycardia
Wolff-Parkinson-White syndrome
Most common complication of AF:
systemic thromboembolism
64
Atrial Fibrillation
ECG findings:
Rhythm - Irregularly irregular
Rate - usually 100-160 beats per minute but slower if on
medication
QRS Duration - Usually normal
P Wave - Not distinguishable as the atria are firing off
all over
P-R Interval - Not measurable
Many sites within the atria are generating their own
electrical impulses, leading to irregular conduction of
impulses to the ventricles that generate the irregular pulse 65
Ventricular Tachycardia (VT)
ECG findings:
Rhythm - Regular
Rate - 180-190 Beats per minute
QRS Duration Prolonged (wide QRS)
P Wave - Not seen
Mechanism: Abnormal tissues in the ventricles generating a
rapid and irregular heart rhythm
Associated with a poor cardiac output
66
Ventricular Fibrillation (VF)
ECG findings:
Rhythm - Irregular
Rate - 300+, disorganized
QRS Duration - Not recognizable
P Wave - Not seen
This patient needs to be defibrillated!! QUICKLY
Disorganized electrical signals cause the ventricles to quiver
instead of contract in a rhythmic fashion
Patient becomes unconscious as there in NO cardiac output
This condition may occur during or after a myocardial infarct. 67
A Quick approach to Arrhythmias:
First look at the heart rate:
>100 bpm = tachycardia
<60 bpm = bradycardia
Are there extra beats? Ectopic Beats
Secondly assess the origin of the arrhythmia:
If the QRS < 120ms (a narrow complex), then it is
either a sinus arrhythmia, supraventricular rhythm or
a junctional tachycardia
If the QRS > 120ms it is either a ventricular
tachycardia or a supraventricular rhythm with
additional bundle branch block, additional accessory
AV pathway
1
Pathophysiology Lecture Notes
Topic: CORONARY ARTERY DISEASE
Lecturer: Dr. S. Upadhya
2
Patient 01:
A 64-year-old man is brought to ER with nausea, dyspnea
and a crushing substernal chest pain. The pain has lasted
for about 30 min, radiates to left arm and jaw, not
relieved by rest. Personal history reveals a sedentary
lifestyle, moderate hypercholesterolemia, obesity, diabetes
and smoking.
Physical Examination: BP 100/60 mmHg; rapid low volume
pulse; diaphoresis; Bibasilar rales on chest auscultation.
Laboratory findings:
EKG - shows elevation of ST segment with prominent
Q waves and inverted T waves
Blood biomarkers: Elevated CK-MB; elevated troponin T & I
Blood count: Mild leukocytosis
Chest X ray: Bilateral mild pulm edema without pleural
disease or widening of the mediastinum
3
Most likely diagnosis in patient 01:
Acute Myocardial Infarction
Other differential diagnosis:
Gastroesophageal reflux disease
Myocarditis
Pneumothorax
Pulmonary embolism
Acute pancreatitis
Anxiety
4
Clinical presentations of CAD include:
Silent ischemia
Angina pectoris
Acute coronary syndromes
unstable angina and acute myocardial
infarction (MI)
Sudden cardiac death
5
Etiology of CAD:
Atherosclerotic obstruction of the large
epicardial vessels - the most common cause
Spasm of the coronary arteries
Emboli
Congenital abnormalities -rare cause
6
-Most common cause
-Risk factors include:
Hypertension,
Hypercholesterolemia,
Diabetes mellitus,
Smoking,
Family history of
atherosclerosis
Atherosclerosis:
Etiology of CAD:
7
-Can occur in any population but is
most prevalent in Japanese.
-Vasoconstriction is mediated by
histamine, serotonin,
catecholamines, and endothelium-
derived factors.
-Because spasm can occur at any
time, the chest pain is often not
exertion-related.
Spasm of
coronary
vessels:
Etiology of CAD:
8
-Rare cause of CAD
-Usually occurs from vegetations in
patients with endocarditis
Emboli:
Etiology of CAD:
9
-Congenital coronary artery
abnormalities occurs in 12%.
of the population.
-A high origin of the ostia may reduce
diastolic coronary artery blood flow
-Persistence of embryonal
connections with mediastinal vessels
may lead to coronary artery fistulae
Congenital:
Etiology of CAD:
10
Patient 02:
54-year-old chronic smoker complains of pain in the calf
muscles by an half mile walk associated with coldness and
numbness in both the legs since a year. The symptoms are
relieved by rest. Patient also gives history of sexual
dysfunction. Patient has a strong family history of
hypercholesterolemia.
PE: BP 160/100 mm Hg; Low volume peripheral pulses in
both lower limbs; Loss of hair on dorsum of
feet; Atrophy of calf muscles; Bruits on femoral artery.
Lab: Elevated LDL and decreased HDL; elevated total serum
cholesterol
Angiogram: Narrowing of arterial lumens at multiple sites in
the aortoiliac region
Plain X ray: Irregular arterial calcifications in abdominal aorta
and iliac arteries
11
Differential diagnosis in patient 02:
Atherosclerosis
Diabetic neuropathy
Vasculitis
Collagen vascular disease
The most likely diagnosis:
Atherosclerosis
Arterial biopsy: Fibrofatty plaque formation
with dystrophic calcification, atheroma.
Fibrous cap by smooth muscles and collagen
with necrotic lipid core and fibrous plaque
12
Pathophysiology of atherosclerosis
13
Sites of severe atherosclerosis in
order of frequency:
Abdominal aorta & iliac arteries
Proximal coronary arteries
Thoracic aorta, femoral and popliteal
arteries
Internal carotid arteries
Vertebral, basilar and middle cerebral
arteries
14
Pathogenesis of atherosclerosis:
15
Pathogenesis of atherosclerosis:
Infiltration of low-density lipoproteins (LDL) into
the subendothelial region due to the shear stress
by flowing blood
Oxidation of LDL
Macrophages take up oxidized LDL through
receptors
Foam cell formation
Formation of fatty streaks
Oxidized LDL also has other deleterious
effects:
-stimulation of release of cytokines
-inhibition of NO production
16
Stimulation and movement of vascular smooth
muscle (VSM) cells from the media to the intima
Proliferation of VSM, lay down of collagen and
other matrix molecules
VSM cells also take up oxidized LDL and
become foam cells
Formation of atherosclerotic plaques
characterized by localized fibrous thickenings of
the arterial wall associated with lipid-infiltration
that may eventually calcify
Accumulation of lipid in foam cells is a key
event in the progression of atherosclerotic
lesions
Pathogenesis of atherosclerosis:
17
As the atherosclerotic lesions age, T cells and
macrophages are attracted
The intercellular "soup" in the plaques contains
a variety of cell-damaging substances, including
ozone
As plaques mature, a fibrous cap forms over
them
The plaques with defective or broken caps are
most prone to rupture
The lesions alone may distort vessels &
obstruct the flow
Ulceration and rupture of plaques trigger
the formation of thrombi that obstruct flow
Pathogenesis of atherosclerosis:
18
Relation to Dietary Cholesterol and
atherosclerosis:
Lowering plasma cholesterol slows the progress
of atherosclerosis How?
Review the main pathways for the metabolism
of lipids
HDL is referred to as "good cholesterol" and
LDL is referred to as "bad cholesterol
19
Pathways for metabolism of ingested lipids
Cholesterol
20
Summary of main pathways for the metabolism of
lipids:
Dietary cholesterol and triglycerides (TGs) enter circulation
in the form of chylomicrons
Under the influence of lipoprotein lipase, chylomicrons
release TGs to fat depots and muscles, and the resulting
chylomicron remnants are taken up by the liver
The liver synthesizes cholesterol and packages it (along
with TGs) with specific proteins to form very low-density
lipoproteins (VLDL)
VLDL enter the circulation and donate TGs to tissues
under the influence of lipoprotein lipase
VLDL become cholesterol-rich intermediate-density
lipoproteins (IDL) and low-density lipoproteins (LDL)
when it loses TGs in tissues
21
Summary of main pathways for the metabolism of lipids
(continued from previous slide):
The LDL supply cholesterol to the tissues for production of
cell membranes and the cholesterol as precursor for all
steroid hormones
LDL are taken up by peripheral tissues as well as liver
The oxidized LDL are taken up by macrophages and
smooth muscle cells in atherosclerotic lesions
Liver releases high density lipoproteins (at this stage
called, nascent HDL) into circulation
HDL take cholesterol from peripheral cells and transport it
to the liver where it is metabolized, keeping plasma and
tissue cholesterol low
22
Dietary antioxidant agents such as vitamin E, and -
carotene has been used to inhibit oxidation of LDL
Reducing saturated fatty acids and increasing
polyunsaturated fatty acids (PUFA) & Omega-3 fatty acids
Nutritional aspects of atherosclerosis:
Dietary supplementation of Vit B6, B12 & FA:
-Hyperhomocystinemia is associated with accelerated
atherosclerosis (about 7% population are affected)
-Homocysteine is a significant source of H2O2 and
other reactive forms of oxygen, and would accelerate
the oxidation of LDL
-Homocysteine is metabolized by enzymes that are
dependent on vitamin B6, vitamin B12, and folic acid
-Dietary supplementation of these vitamins reduces
plasma homocysteine, usually to normal
23
How Hypertension is a risk factor for
atherosclerosis?
Elevated blood pressure
Increase in shear stress on the endothelium
Infiltration of low-density lipoproteins (LDL) into
the subendothelial region
Atherosclerosis
24
Clinical Manifestations of atherosclerosis:
Angina pectoris
Myocardial infarction
Thrombotic strokes
In the abdominal aorta - aneurysmal
dilation and rupture
In the renal vessels - renovascular
hypertension
In the circulation to the legs - vascular
insufficiency causes intermittent claudication,
Frank gangrene of the extremities
In intestine - clot formation and obstruction
may occur in vessels supplying the intestines
25
Pathophysiology of
Coronary Artery Disease (CAD)
26
Anatomy of Coronary Circulation:
The right (RCA) and left (LCA) coronary arteries
arise in the root of the aorta just above the aortic
valve orifice
The coronary arteries (large and medium-sized) run
along the epicardial surface and send arterioles into
the myocardium
LCA: Quickly divides into the left anterior
descending artery (LAD) and Left circumflex artery
(LCX) arteries.
LAD: usually follows the anterior interventricular
groove and, in some people, continues over the
apex.
27
LCA
LCX
LAD
RCA
Coronary Veins
Coronary Circulation
Posterior descending
artery
Acute marginal
artery
28
Coronary Perfusion in Right dominant
individuals (85%):
LAD artery supplies:
Anterior free wall of LV
Anterior part of septum
Apex
LCX artery supplies:
Most of lateral free wall of LV
RCA supplies:
Right ventricle
Large part of Inferior wall
Posterior wall of LV
Posterior part of septum
SA node, AV node
29
In Left coronary dominant individuals
(15%):
The LCX supplies:
Major part of Inferior wall
Posterior wall of LV
Apex
The remaining perfusion is same as
that in RCA dominance
30
LAD
territory
RCA & LCX
territory
Coronary Circulation:
Septal
perfusion
31
2 & 3: Ventricular systole
1 & 4: Ventricular diastole
Physiology of coronary circulation:
Coronary Perfusion during different phases of
the cardiac cycle
Coronary blood flow is maximum during ventricular
diastole and least during isovolumetric contraction
32
Physiology of coronary circulation:
The coronary bloodflow is mainly controlled by
local metabolic autoregulation
Sympathetic stimulation does not cause significant
vasoconstriction
Myocardium cannot function anaerobically for
extended periods by building up an oxygen debt
At rest the heart produces 70% of its ATP from
oxidation of fatty acids and 30% from oxidation of
carbohydrates
During exercise, lactate becomes an important
substrate for the myocardial metabolism
33
Pathophysiology of CAD:
Myocardial metabolic requirement accounts for
7% of the body's resting oxygen consumption
Cellular ischemia occurs when there is:
i) Increased O2 demand (as in thyrotoxicosis and
aortic stenosis)
ii) An absolute reduction in O2 supply (as in
atherosclerosis or spasm)
iii) A combination of i & ii - cocaine abuse
increases oxygen demand (by inhibiting reuptake
of norepinephrine at adrenergic nerve endings in
the heart) and can reduce oxygen supply by
causing vasospasm
34
Pathophysiology of CAD:
Atherosclerosis of large coronary arteries is the
predominant cause of angina and myocardial infarction
Most common sites: In areas exposed to increased
shear stresses such as bending points and bifurcations
Fissuring of the atherosclerotic plaque can lead to platelet
accumulation and transient episodes of thrombotic
occlusion, usually lasting 1020 min (in unstable angina)
Platelet release of vasoconstrictive factors such as
thromboxane A2 or serotonin can cause vasoconstriction
and contribute to decreased flow
Deep arterial injury from plaque rupture can cause
formation of a fixed thrombus and cut off total blood flow
(as in myocardial infarction)
35
Pathophysiology of CAD:
A: Normal artery
B: Platelet aggregation & cytokine mediated
reactions
C: Formation of atheroma
36
Pathogenesis of Acute
Coronary Syndromes:
The integral role of
platelets
Plaque
Fissure or
Rupture
Platelet
Aggregation
Platelet
Activation
Platelet
Adhesion
Thrombotic
Occlusion
37
ADP
Ticlopidine
Clopidogrel
Heparin
LMW Heparin
Direct Thrombin
Inhibitors
Aspirin
Epinephrine
Collagen Arachidonic
Acid
Thrombin
IIb/IIIa
receptors
Fibrin
The
Platelet
The
Platelet
38
Within 60 sec after coronary artery occlusion
Myocardial oxygen tension in the affected cells
falls to zero
Rapid shift to anaerobic metabolism in myocytes
Lactic acid production
Dysfunction of myocardial relaxation and
contraction
If perfusion is not restored within 4060 min, an
irreversible stage of injury occurs
Pathophysiology of CAD:
39
Irreversible stage of injury:
Possible causes:
-Severe ATP depletion
-Increased extracellular calcium concentrations
-Lactic acidosis
-Free radicals
Cellular features:
Diffuse mitochondrial swelling
Damage to the cell membrane
Marked depletion of glycogen
Pathophysiology of CAD:
40
Clinical Manifestations of CAD:
Chest Pain
Shortness of breath
Fourth heart sound (S4)
Shock
Tachycardia
Bradycardia
Nausea and Vomiting
41
Chest Pain:
Chest pain is mediated by sympathetic afferent
fibers T1-T5
In the spinal cord, the pain impulses probably
converge with impulses from other structures
and hence radiated to the chest wall, back, and
arm
The actual trigger for nerve stimulation is
adenosine. Blocking adenosine receptor (P1)
with aminophylline leads to reduced anginal
pain
42
Ischemia without pain may be due to:
i) Autonomic dysfunction of afferent nerves
Examples: Patients with peripheral neuropathy or
transplanted heart
ii) Transient reduced perfusion
iii) Differing pain thresholds
43
Myocardial ischemia
Systolic dysfunction of
LV
Pulmonary congestion
Shortness of breath
Myocardial stiffness
Diastolic dysfunction
Fourth Heart Sound (S4)
Basis for clinical manifestations in CAD
44
Clinical presentations of CAD:
Angina pectoris
Acute coronary syndromes (ACS)
45
Typical angina is a syndrome defined by the
presence of three primary findings:
-Substernal chest discomfort/pain
-Aggravated by exertion or emotional
stress, and
-Relieved by nitroglycerine or rest
Atypical angina: lacks one of the three main
characteristics
If only the first feature is present, the discomfort
is more likely to be noncardiac in origin and is
often accompanied with conditions of the lungs,
esophagus, and chest wall
Angina pectoris
46
Diagnosis of Angina pectoris:
Typical symptoms
ECG
Stress testing with ECG or
imaging (echocardiographic or
nuclear)
Coronary angiography for
significant symptoms or positive
stress test
47
ECG in angina:
ECG changes during an attack:
T wave discordant to the QRS complex
ST-segment depression
Decreased R-wave height
The ECG between attacks:
At rest is normal (30%)
In the remaining 70%, the ECG shows
evidence of previous infarction, hypertrophy, or
nonspecific ST-segment and T-wave (ST-T)
abnormalities
48
ECG changes in angina pectoris
Depression of ST segment; T wave inversion
ST segment
depression
T wave inversion
Patients ECG
Normal ECG
P
Q
R
T
S
49
Location of lesion (ischemia/MI) by
observing changes in 12 lead ECG:
Inferior (diaphragmatic) wall: Lead II, III & aVF
Anterior wall/Anteroseptal: V1-V4
Lateral wall: Lead I, aVL, V5, V6
Right Ventricle: V1, V2 & sometimes V3
Septal wall : V3, V4 with or without reciprocal
changes in II, III & aVF
50
ST segment depression Myocardial ischemia
Lead II
51
Lateral wall ischemia
52
Inferior & Lateral wall ischemia
53
Stress testing:
If a patient has a normal resting ECG and can
exercise, exercise stress testing with ECG is done
In patients with atypical symptoms, a negative
stress ECG usually rules out angina pectoris and
CAD; a positive result may or may not represent
coronary ischemia and indicates need for further
testing
Imaging tests can help assess LV function and
response to stress; identify areas of ischemia,
infarction, and viable tissue; and determine the site
and extent of myocardium at risk
54
Angiography in CAD:
Coronary angiography is the standard for diagnosing
CAD but is not always necessary to confirm the
diagnosis
It is indicated primarily to locate and assess severity
of coronary artery lesions
Angiography may also be indicated when knowledge
of coronary anatomy is necessary to advise about
work or lifestyle needs (eg, discontinuing job or sports
activities)
Obstruction is assumed to be physiologically
significant when the luminal diameter is reduced
more than 70% of original
55
Acute Coronary Syndromes (ACS):
Unstable Angina (UA)
Non-ST elevation Myocardial Infarction
(NSTEMI)
ST-elevation Myocardial Infarction
(STEMI)
These syndromes represent acute myocardial ischemia
Most likely due to obstructive coronary artery disease
All require early diagnosis and clinical management
Produce potentially catastrophic complications,
including death
56
7KURPEXV )RUPDWLRQ DQG $&6
8$ 167(0, 67(0,
3ODTXH 'LVUXSWLRQ)LVVXUH(URVLRQ
7KURPEXV )RUPDWLRQ
1RQ676HJPHQW (OHYDWLRQ $FXWH
&RURQDU\ 6\QGURPH
676HJPHQW
(OHYDWLRQ
$FXWH
&RURQDU\
6\QGURPH
Old
Terminology:
New
Terminology:
57
Unstable Angina - Definition
Characters of Chest pain:
-Occurs at rest
-Prolonged, lasting greater than 20 minutes
-Has been present in the past but has changed
in frequency, severity, or threshold needed to
bring on symptoms
58
Unstable Angina: precipitating factors
Inappropriate tachycardia
anemia, fever, hypoxia, tachyarrhythmias,
thyrotoxicosis
High afterload
aortic valve stenosis, LVH
High preload
high cardiac output, chamber dilatation
Inotropic state
sympathomimetic drugs, cocaine intoxication
59
Unstable Angina: pathogenesis
Plaque disruption
Acute thrombosis
Vasoconstriction: platelet-
dependent and thrombin-
dependent vasoconstriction,
mediated by serotonin and
thromboxane A
2
60
Diagnosis of Unstable angina:
Characteristic chest pain
ECG:
-Transient ST-segment depression or deep,
-Symmetric T-wave inversion during
episodes of ischemic chest pain
61
Prinzmetals or Variant Angina: clues to
diagnosis
A form of unstable angina caused by coronary
spasm
Patients are usually younger, female, smokers, and
without other significant risk factors for coronary
artery disease
Transient ST-segment elevation during chest pain
Intermittent chest pain: often repetitive; usually at
rest; typically in the early morning hours & rapidly
relieved by nitroglycerine
Patients often have manifestations of other
vasospastic disorders such as migraine headaches
and Reynaud's phenomenon
Most attacks resolve without progression to MI
Angiography shows no obstructions in vessels
62
Non-ST-segment elevation MI
(NSTEMI, subendocardial MI):
Myocardial necrosis - evidenced by cardiac
markers in blood
Absent acute ST-segment elevation or Q
waves in ECG
Nonspecific ECG changes seen are ST-
segment depression, T-wave inversion, or
both
Symptoms are the same as in STEMI
63
Clinical history of ischemic type
chest pain >20 minutes
Changes in serial ECG tracings
Rise and fall of serum cardiac
enzymes (biomarkers)
WHO Criteria
MXVW PHHW Z RXW Rf 3 FULWHULD
ST Elevation Myocardial Infarction
(STEMI):
64
Causes for acute MI:
Atherosclerosis most common
Other causes:
-Coronary emboli caused by endocarditis, mural
thrombi, prosthetic valves, or neoplasms;
-Inflammatory processes, including viral
infections such as with coxsackie B;
-Radiation-induced coronary stenosis;
-Congenital abnormalities in a coronary artery;
-Cocaine abuse.
Rare causes:
Hurlers syndrome, homocystinuria, rheumatoid
arthritis, and systemic lupus erythematosus.
65
The physical examination in STEMI:
General: Restless agitated, anguished facies,
clenched fist (Levines sign)
Increased Heart rate and Respiratory rate
Low grade fever (nonspecific response to
myocardial necrosis)
Signs of hypoperfusion-low volume pulse, pale,
cold and clammy, ashen extremities
Evidence of heart failure - Jugular venous
distention, crackles on lung exam, left ventricular
heave
S3 and S4 gallops & murmurs
66
Bradycardia in acute MI:
Inferior wall myocardial infarction (due to
occlusion of RCA) is associated with ischemia of
AV node and conduction defects
Inferior wall MI can also cause vagus nerve
dysfunction and conduction defects
Dysfunction of the SA node is rarely seen in
coronary artery disease, because this area
receives blood from both the right and the left
coronary arteries
Basis for sign/symptoms in AMI
67
Nausea and Vomiting:
Due to activation of the vagus nerve in an
inferior wall myocardial infarction
Tachycardia:
Due to elevated levels of catecholamines as
a compensatory mechanism during low
cardiac outputs
Basis for sign/symptoms in AMI
68
Different Evidences of MI
Evidence of cell death Pathology
Evidence for reduction of tissue
perfusion & abnormal wall
motion
Imaging
Evidence of myocardial cell
death recovered from blood
Biochemistry
Evidence for ischemia, injury &
loss of electrical function
EKG
69
ECG changes in STEMI
ECG changes:
Elevation of ST segment; pathologic Q wave
A. Normal ECG prior to MI
B. During acute stage of MI: Marked ST elevation
C. After a few hours of MI: Pathologic Q waves, less ST elevation
and inverted T wave
D. After many days of MI: Pathologic Q wave alone persists
indicating old infarct
Q
R
T
S Q
R
T
S
Q
R
T
S
Q
R
T
S
A B C D
70
ECG changes in STEMI
71
Acute anterior left ventricular infarction (tracing obtained
within a few hours of onset of illness)
There is striking hyperacute ST-segment elevation in
leads I, aVL, V4, and V6 and reciprocal depression in
other leads.
Artery most likely affected is : LAD artery 72
ST segment elevation Myocardial infarction
73
Acute Septal wall Infarction
Note the striking ECG changes in V2, V3 with
reciprocal changes in II, III & aVF
The artery most likely affected is: LAD artery
74
Acute Anteroseptal Infarction
ECG changes in V1, V2, V3 & V4
Arteries involved: RCA and LAD artery
75
Acute Inferior wall MI
ECG changes in II, III and aVF
Artery involved: RCA
76
Biomarkers in acute MI
Myoglobin
MB isoenzyme of creatine kinase
(CK-MB)
Lactate dehydrogenase isoenzyme
(LH-I)
Cardiac troponin I (cTnI)
Cardiac troponin T (cTnT)
77
Copyright 2007 American College of Cardiology Foundation. Restrictions may apply.
Anderson, J. L. et al. J Am Coll Cardiol 2007;50:652-726
Timing of Release of Various Biomarkers After Acute
Ischemic Myocardial Infarction
78
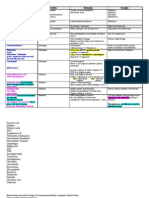
7-10 days 48-72 hours 10-12 hours LD-I
24 hours 8-10 hours 1-2 hours Myoglobin
CK-MB, MB isoenzyme of creatine kinase; LD-I, lactate dehydrogenase
isoenzyme; cTnI, cardiac troponin I; cTnT, cardiac troponin T
7-10 days 12-48 hours 4-6 hours cTnT
3-10 days 12 hours 4-6 hours cTnI
2-4 days 18 hours 4-6 hours CK-MB isoforms
Time to Return
to Normal
Time to Peak
Elevation
Time to
Initial
Elevation
Biomarker
Cardiac Biomarkers
79
Why Troponin-I is an important Biomarker?
Three distinct tissue-specific isoforms of Troponin-I
(TnI) have been identified: two in skeletal muscle and
one in cardiac muscle
The cardiac isoform of TnI (cTnI) has never been
isolated from skeletal muscle
cTnI appears to be uniformly distributed throughout
the atria and ventricles
The absolute specificity of cTnI for cardiac tissue
makes it an ideal biomarker of myocardial injury
When interpreting the results of cTnI assays it is
important to remember that, although cTnI is 100%
specific for cardiac injury, it is not 100% specific for
AMI
80
AMI,
Skeletal muscle injury,
Decreased renal function
Myoglobin
AMI,
Left ventricular hypertrophy,
Renal failure,
Hypertension,
Skeletal muscle injury,
Chronic skeletal
myopathies,
Hypothyroidism
Creatine kinase (CK), CK-
MB
Condition Biomarker
Conditions Associated with Increased Biomarker
Levels
81
AMI,
Musculoskeletal disease,
Renal disease,
Polymyositis,
Dermatomyositis
Cardiac Troponin-T
AMI,
Cardiac injury,
CHF,
Unstable angina,
Myocarditis
Cardiac Troponin-I
AMI,
Cardiac injury,
Renal failure,
Leukemia,
Lactate Dehydrogenase
Condition Biomarker
Conditions Associated With Increased Biomarker
Levels
82
Importance of Serial Sampling:
Since patients present at varying times following the
onset of symptoms, it is necessary to obtain serial
measurements of biomarkers for optimal diagnostic
accuracy
A protocol for measuring cTnI levels requires testing at
admission and at 3, 6, and 9 hours
Serial measurements of cTnI, together with the ECG
results and the patients history and symptoms, are
necessary to make the differential diagnosis between AMI
and other cardiac conditions as well as for determining
whether AMI patients are in the early or late phase
following infarction
83
Conditions that can cause SHOCK in acute
MI:
Obstruction of the left main coronary artery or LAD
artery : severe LV dysfunction
Necrosis of the septum due to occlusion of LAD artery
Rupture of the anterior free wall of LV from occlusion of
the LAD artery
Rupture of the lateral free wall of LV from occlusion of
the left circumflex coronary artery
(Rupture of lateral & anterior walls lead to formation of
pericardial effusion and cardiac tamponade)
Rupture of the papillary muscles from occlusion of the
circumflex artery can produce severe mitral regurgitation
Rupture of myocardial tissue usually occurs
47 days after the acute infarction
84
COMPLICATIONS OF ACUTE MI
Tachyarrhythmias including VF
Bradyarrhythmias including heart block
LV failure - Pulmonary edema
RV failure - RV infarct
Cardiogenic shock
Acute Mitral Regurgitation
Rupture IV septum
Pulmonary embolism
Cardiac rupture
Dressler's syndrome
85
Diagnosis of underlying disorders or
Complications following
Acute MI by certain physical findings
86
Atrial or ventricular
arrhythmias/Heart block
Fast, slow or
irregular pulse
High vagal tone (Inferior-
Posterior MI)
Hypotension,
Bradycardia
High sympathetic tone
(anterior MI)
Hypertension,
Tachycardia
Possible Reason Physical Findings
Pericarditis, Dresslers
syndrome (Posterior MI)
Pericardial friction
rub
87
LV systolic dysfunction
(signs of CHF if
dysfunction is >25%)
S3 gallop, pulm rales,
pulsus alternans
Cardiogenic shock Hypotension, cool
clamy skin, cyanotic,
altered mentation,
oliguria
Decreased LV
compliance
S4 gallop
Possible Reason Physical Findings
88
Papillary muscle
rupture
Systolic murmur of MR
Ventricular septal
rupture (septal MI)
Harsh systolic murmur,
palpable thrill at left sternal
border
RV failure (RV
infarction)
Jugular venous distension,
hypotension, RV S3, S4
gallop, clear lungs
Possible Reason Physical Findings
1
Pathophysiology Lecture Notes
Topic: VALVULAR HEART DISEASES
Lecturer: Dr. S. Upadhya
2
Classification of valvular heart disease
Dysfunctional cardiac valves can be:
Narrow (stenosis) or
Leaky (regurgitation/insufficiency)
The most common are:
Mitral stenosis (MS)
Mitral regurgitation (MR)
Aortic stenosis (AS)
Aortic regurgitation (AR)
3
Patient 01:
A 50 year old male presents with complaints of
substernal chest pain, which increases with
exertion, and shortness of breath which is
starting to limit his lifestyle. He has no risk factors
for coronary artery disease.
On Physical Exam you find the following:
Delayed carotid upstroke
Apical impulse is sustained but not displaced
laterally
An ejection systolic murmur in the second
intercostal space
ECG: Left axis deviation with high voltage QRS in
V4-V6
4
The most likely diagnosis in patient 01 is:
Aortic stenosis
Other differentials:
Mitral regurgitation
Mitral valve prolapse
Hypertrophic Obstructive
Cardiomyopathy
Myocardial Infarction
5
Heart Sounds
Heart sounds are generated by:
9 Opening and closing of the heart valves
9 Turbulence in blood flow
9 Vibrations in the support structures of the
heart
6
First Heart Sound (S1):
Signals the beginning of ventricular
systole
Generated by mitral and tricuspid valve
closure M1T1
Loudest over the apex
Heard best by using the diaphragm of the
stethoscope
The intensity is determined primarily by:
-Valve mobility,
-Force of ventricular contraction
-Velocity of valve closure
(most important)
7
Loud S1:
Mitral stenosis
Short PR interval
Tachycardia
Hyperdynamic
states
S1 with varying intensity from beat to beat in
atrial fibrillation, reflecting variable
contractility
Soft S1:
Mitral regurgitation
Long PR interval
Poor systolic function
LBBB
Variations of S1
8
Second Heart Sound (S2):
Generated by the closure of the aortic (A2)
and pulmonic (P2) valves A2P2
Best heard at the left upper sternal border
(over the base of the heart)
A2 is the louder component and is audible at
all locations on the chest wall
In normals, P2 is heard only at the upper left
sternal border and is always less audible than
A2 at this location
Abnormalities of S2 primarily due to:
-Alterations in intensity
-Alteration in timing of closure of valves
9
Loud S2:
Systemic hypertension
Pulm hypertension
ASD
Hyperdynamic
states
Aortic dilatation
Soft S2:
Aortic stenosis
Pulmonic stenosis
Aortic regurgitation
Variations of S2
10
Splitting of S2 (A2 P2):
Normal split: A2P2 heard as two sounds during
inspiration and single during expiration
Wide splitting of S2 (a widely split S2 having
normal respiratory variation) occurs when P2 is
delayed (e.g., RBB block)
Fixed splitting of S2 occurs when respiration-
induced changes in filling are similar in both
ventricles: e.g.,characteristic in atrial septal
defect
11
Paradoxical splitting of S2 (P2 A2):
Typically in:
-LBB Block because of delay in
depolarization of LV
-Severe Aortic stenosis delay in closure of
aortic valve
Normally the interval from A2 to P2 would
lengthen during inspiration
In paradoxical splitting, the interval shortens
during inspiration
12
Diastolic Sounds : S3 & S4
Ventricular gallop (S3):
Occurs in early diastole; Corresponds to the end
of the rapid filling phase of the ventricular diastole
Low-frequency sound, best heard with the bell of
the stethoscope lightly applied to the apex (LV
S3) or left lower sternal border (RV S3); best
heard in the left lateral decubitus position
Caused by interplay between ventricular filling
and ventricular compliance
Pathologic S3 is associated with abnormally high
LV filling pressures, low cardiac output, and a
dilated, poorly contractile LV (e.g., congestive
heart failure)
13
Diastolic Sounds: S3 & S4 (continued)
Atrial gallop (S4):
A dull, low-frequency sound that precedes S1
Best heard over apex with the bell of the
stethoscope in the left lateral position
The S4 is attributed to forceful atrial
contraction to fill a noncompliant or stiff
ventricle (e.g., coronary artery disease)
The S4 disappears in atrial fibrillation
14
Heart murmurs
Classification:
Systolic while the ventricle is contracting;
between S1 and S2
Diastolic while ventricle is filling;
between S2 and S1
Continuous murmur
Pay attention on:
- Timing and duration
- Intensity (grade I to VI)
- Quality (blowing, harsh, rumbling)
- Radiation (to the neck, axilla, or back)
All diastolic and continuous murmurs are abnormal
and pathological
15
Systolic Murmurs:
A midsystolic (or early systolic) ejection murmur:
-begins with S1 and ends before S2
-classically diamond-shaped (crescendo-decrescendo)
Pansystolic murmur:
-begins with S1 and extend to S2
-classically high frequency, blowing in quality, and
relatively uniform in intensity
-all pansystolic murmurs are pathologic
Late systolic murmur:
-occurs in the latter part of systole, well after S1 and end
in or after S2
-all late systolic murmurs are pathologic
16
Apex, LLSB Mitral valve
prolapse
Late
systolic:
Apex, LLSB HCM
Second IS Aortic stenosis Midsystolic
(Early
systolic):
Neck LLSB Tricuspid
regurgitation
LLSB VSD
Axilla or
back
Apex Mitral
regurgitation
Pansystolic:
Radiation Heard best Example Timing
LLSB=Lower left sternal border
HCM=Hypertrophic cardiomyopathy
IS=Intercostal space
Examples for Systolic Murmurs:
17
Left sternal
border
Tricuspid
stenosis
Apex, with
the bell
Mitral stenosis Middiastolic rumble:
(low pitched)
Left sternal
border, third
intercostal
space
Aortic
Regurgitation
Early diastolic:
(decrescendo)
Heard best Example Timing
Examples for Diastolic Murmurs:
All diastolic murmurs are pathological
18
Left first and
second
Intercostal
space, Left
sternal border
Patent ductus
arteriosus (PDA)
Continuous
murmur:
(systolic-
diastolic)
Heard best Example Timing
Continuous Murmur
19
Iso
ventr
con
tractio
n
R
apid
ejection
R
educed
ejectio
n
Iso
ventr
relaxation
R
apid ventr
fillin
g
R
educed
ventr
filling
A
trial systole
Normal Left ventricular
and aortic pressure
changes
Phonocardiogram
20
Patient 02:
An active 75 year old farmer comes to the
physicians office after experiencing a
fainting spell while working in field. The
episode occurred without warning and he
had no symptoms following the episode.
However, on close questioning he admits to
some breathlessness and vague chest
heaviness with his usual heavy exertion over
the past few months. He has been healthy all
his life, doesnt smoke and has not seen a
doctor in 30 years. He served in the army
and no abnormalities were reported during
his induction physical
21
Physical Exam of patient 02:
Robust looking older man
BP 130/90; Pulse 68 bpm, regular; RR-12; T-98.6 F
JVP 6 cm with normal a and v waves
Carotids: Difficult to palpate, delayed upstroke
Lungs: Clear
Heart: Palpation: Palpable thrill over the mid LSB. PMI
5 ICS, 2 cm lateral to the MCL. Palpable presystolic
impulse followed by a sustained ventricular lift.
Auscultation: Loud S
4;
S
1
is normal. A single S
2
(P2) is heard at the upper left sternal border but no A
2
is
heard at the lower left sternal border. There is a 4/6
systolic ejection murmur (crescendo-decrescendo)
heard best at the R 2nd interspace that radiates widely
to the LSB, and to the neck. No diastolic murmurs.
Abdomen and extremities are unremarkable
22
Most likely diagnosis in Patient:
Aortic stenosis
Other possible differentials:
Mitral regurgitation
Mitral valve prolapse
Hypertrophic Obstructive Cardiomyopathy
Myocardial Infarction
23
Aortic Stenosis (AS)
Causes of Aortic Stenosis:
Patients above 70; Prevalent in
patients with diabetes or
hypercholesterolemia
Degenerative
Patients age 30-70; Accompanying
AR and MS is frequent
Rheumatic
Patients below age 30 Congenital
Clinical presentation Type
24
The normal aortic valve area is approximately 3.54 cm2.
Critical aortic stenosis occurs when the area is < 0.8 cm2.
At this point, the systolic gradient between the left ventricle
and the aorta exceeds 150 mm Hg, and patients become
symptomatic
Calcified valve
Pathogenesis of AS:
Abnormal flow through valves
Fibrosis and calcification
Stenosis
25
Pathophysiology of AS:
Stenosed aortic valve increases afterload on the LV
Increased LV pressure during systole
Increased left ventricular wall thickness while the cavitary
radius remains relatively unchanged due to parallel
replication of sarcomeres producing
"concentric hypertrophy"
Decrease in ventricular compliance
Significant increase in left ventricular end-diastolic
pressure
26
Aortic stenosis: Hemodynamic changes
Narrowing around the
aortic valve
Aortic valve acts as
major resistance for
flow (afterload) during
ejection
Left ventricular
pressure rises to very
high levels during
systole
Left ventricular
hypertrophy
Systolic murmur
appears
27
Pressure profile in AS
28
Pressure gradient
between LVP
and AP during
ejection
Systolic Murmur
Pressure profile in
Aortic Stenosis
Phonocardiogram
29
Clinical Manifestations of AS and basis:
The three characteristic features of AS are:
Chest pain, Syncope & CHF
i) Chest pain (angina pectoris):
Mechanisms
coronary artery disease;
increased oxygen demands because of
ventricular hypertrophy;
decreased oxygen supply as a result of
excessive compression of the vessels;
coronary artery obstruction from calcium
emboli arising from a calcified stenotic valve
30
ii) Syncope: Syncope is due to decreased
cerebral perfusion
Cause for syncope in AS
the fixed obstruction to out flow;
transient atrial arrhythmias with loss of effective
atrial contribution to ventricular filling;
arrhythmias arising from ventricular tissues
iii) Congestive heart failure (CHF):
LVHdiastolic dysfunction of LVprogressive
increase in left ventricular end-diastolic pressure
elevated pulmonary venous pressure
pulmonary edemaRVF
Progressive LV dilation and contractile failure
systolic dysfunction of LVRVF
31
Physical examination in AS:
Palpation of the carotid pulse reveals a pulsus
parvus et tardus - both decreased (parvus) and
late (tardus) relative to the apical impulse
Auscultation:
-a midsystolic murmur is heard, loudest at the
base of the heart, and often with radiation to the
sternal notch and the neck
-a high-pitched aortic ejection sound can be
heard just after the first heart sound
-a fourth heart sound (S4) is often present
32
ABNORMALITIES OF THE ARTERIAL PULSE
AS: pulsus parvus et
tardus or Anacrotic pulse
AR: Water-hammer,
Bisferiens pulse
HOCM: Bisferiens pulse
CHF: Pulsus Alternans
Cardiac Tamponade:
Pulsus Paradoxus
33
Patient 03:
A 24-year-old male presents with chest pain, dyspnea on
exertion and episodes of syncope while playing. His family
history is significant for similar illness in his brother who
died suddenly while playing.
Physical Examination: Double peaked pulse (bisferiens pulse),
Loud S4; A systolic murmur heard over lower left sternal
border. The murmur increases by Valsalva but decreases by
squatting and passive leg raising.
Laboratory:
EKG: Left axis deviation due to LV hypertrophy
Echo: Asymmetrical septal hypertrophy with marked thickening
of the LV septal wall
34
Most likely diagnosis in patient:
Hypertrophic Obstructive Cardiomyopathy
(HOCM) or Idiopathic Hypertrophic Subaortic
Stenosis (IHSS)
Other differentials:
Aortic stenosis
Restrictive cardiomyopathy
Glycogen storage diseases
Fabry disease
HOCM: an autosomal dominant disease, may
cause sudden death in young due to lethal
cardiac arrhythmias
35
Hypertrophic obstructive cardiomyopathy
(HOCM):
Subvalvular aortic stenosis due to severe
hypertrophy of the septum of the left heart
Manifested by a systolic murmur noted on physical
examination
Obstruction of outflow tract in this case is G\QDPLF
Greater obstruction occurs when preload is
decreased - Standing and Valsalva's maneuver
(both decrease venous return) and the murmur
becomes intense
Both of these maneuvers cause a decrease in the
intensity of murmur in case of organic AS, because
less volume of blood flows across the stenotic
aortic valve
36
37
Patient 04:
A 55 year old salesman is referred for
evaluation of a heart murmur. He had applied
for a pilots license and was denied because of
the murmur. He is asymptomatic and
physically active. He denies chest pain,
dyspnea or dizzy spells and gives no history of
a murmur being mentioned during his last
physical exam five years ago. He has no family
history of heart disease. He has never had high
blood pressure or diabetes, doesnt smoke, and
takes no medications. A lipid profile done five
years ago was reported to be OK.
38
Physical Examination of patient 04:
BP - 145/45; P - 78 reg; RR 12; Temp:98.6F
Carotids: Very brisk with sharp collapse
JVP: 5 with normal a and v waves
Lungs: Clear
Heart:
Palpation: PMI is enlarged (4fb), in the anterior axillary
line
Auscultation: S
1
normal, S
2
soft. A early peaking
systolic ejection murmur at the upper RSB and a
holodiastolic blowing murmur, heard best at the lower
LSB when you ask the patient to hold his breath in
expiration and lean forward. There is a different 2/6
low-pitched diastolic murmur at the apex.
Pulses are all very prominent and brisk; audible pulse
over the femoral arteries
39
The most likely diagnosis in patient 04 is:
Aortic Regurgitation
Other differentials:
Mitral stenosis
Pulmonary regurgitation
Tricuspid stenosis
Ventricular Septal defect
40
Additional Testing
ECG: LVH with massive voltage in the lateral
precordial leads (V4-V6)
Chest X-Ray: Large heart, predominant left
ventricular enlargement. No congestive heart
failure
Echo: Marked left ventricular dilation, estimated
EF 65%.
Doppler: Severe aortic regurgitation. The aorta
is slightly enlarged (4.2 mm)
41
Aortic Regurgitation (AR)
Endocarditis
Rheumatic disease
Ankylosing spondylitis
Congenital
Aortic site:
Aortic aneurysm
Heritable disorders of connective tissue - Marfan's
syndrome, Ehlers-Danlos syndrome, Osteogenesis
imperfecta
Inflammatory - Aortitis (Takayasu), Syphilis, Ankylosing
spondylitis, Rheumatoid arthritis and SLE
Aortic dissection
Causes for AR:
Valvular site
42
Pathology of AR:
Valvular cusp abnormality
Aortic dilatation
Aortic inflammation
Aortic tears with loss of commissural
support
43
Pathophysiology of AR:
Regurgitant aortic valve produces a volume load
on the left ventricle
Increased end diastolic volume and pressure
Elongation and replication of sarcomeres in series,
leading to increased ventricular volume
Enlarged ventricular cavity producing
"eccentric hypertrophy"
Chronic AR leads to huge ventricular volumes
44
Comparison between the eccentric (volume overload)
and the concentric (pressure overload) hypertrophy
45
Aortic insufficiency (A. regurgitation):
Hemodynamic changes
An incompetent (leaky) aortic valve allows
blood to regurgitate from aorta to LV
during ventricular diastole
An elevated left ventricular end diastolic
volume and pressure ( preload)
Increased left ventricular and aortic
systolic pressures
Decreased aortic diastolic pressure
Widened aortic pulse pressure
Diastolic murmur appears
46
Aortic pressure (AP)
Left atrial pressure
Left ventricular pressure (LVP)
Pressure profile in AR
Diastolic Murmur
High LVP and AP
during systole
Low AP during diastole
High pulse pressure
Phonocardiogram
47
Clinical Manifestations of AR and basis:
Patient remains asymptomatic as the heart
responds to the volume load
When the compensatory mechanisms fail,
symptoms appear
Symptoms:
-Shortness of breath (due to pulm edema)
-Hypotension often with cardiovascular
collapse
48
Physical examination in AR: (i-iv)
i) Hyperdynamic (pounding) arterial pulses:
- A widened pulse pressure is responsible for
several characteristic peripheral signs
- Palpation of the peripheral pulse reveals a
sudden rise and then drop in pressure
(water-hammer or Corrigan's pulse)
- Head bobbing (DeMusset's sign)
- Rhythmic pulsation of the uvula (Mller's
sign)
- Arterial pulsation seen in the nail bed
(Quincke's pulse)
49
ii) Apical impulse:
Hyperdynamic and displaced laterally due to
the increased volume and forceful contraction
of the left ventricle
iii) S1 (First heart sound):
Will be soft and sometimes absent - because
of early mitral valve closure from aortic
regurgitation and elevated ventricular
pressures
50
iv) Auscultation for murmurs in AR:
Three murmurs may be heard:
-A high-pitched, blowing, early diastolic murmur
usually perceived best along the left sternal border
a high-pitched early diastolic murmur due to
regurgitant flow
-Austin Flint murmur at the apex: a diastolic rumble
from regurgitant flow from the aortic valve
impinging on the anterior leaflet of the mitral valve
producing functional mitral stenosis
-A crescendo-decrescendo systolic murmur, which
is thought to arise from the increased stroke
volume flowing across the aortic valve, can be
heard at the left sternal border
51
Mitral Stenosis (MS)
Causes of MS:
Type Comments
a) Rheumatic: Most common
Narrowing results from fusion and
thickening of the commissures,
cusps, and chordae tendineae
b) Calcific: Usually causes mitral regurgitation
but can cause mitral stenosis
c) Congenital: Presents in infancy or childhood
d) Collagen- SLE and rheumatoid arthritis;
vascular: Rare cause of MS
52
Mitral Stenosis : Pathophysiology
Scarring & fusion of valve
apparatus
Nl valve area: 4-6 cm
2
Mild mitral stenosis:
MVA <2-2.5 cm
2
Minimal symptoms
Mod mitral stenosis
MVA >1.5 cm
2
usually
does not produce
symptoms at rest
Severe mitral stenosis
MVA < 1.0 cm
2
left atrial pressure
pulmonary venous
pressure dyspnea
Atr ial view of mitr al
valve in patient with
r heumatic mitr al stenosis.
53
Pathophysiology of MS:
Mitral valve is narrow
Insufficient blood flows to LV during ventricular diastole
Enlargement of LA with accumulated volume of blood
Elevated left atrial pressure during ventricular diastole
Elevated pulmonary venous pressure and elevated
right-sided pressures (pulmonary artery, right ventricle,
and right atrium)
Dilation and systolic dysfunction of the right ventricle
because of pulmonary hypertension
54
Mitral stenosis: Hemodynamic changes
Narrowing of mitral valve
reduces the amount of
blood that flows forward
through mitral valve
The left atrium enlarges
and left atrial pressure
builds up
There will be a pressure
gradient between left
atrium and left ventricle
throughout the diastole
Mid Diastolic murmur
appears
55
Pressure profile in MS
56
Pressure gradient
between LVP
and LAP throughout
ventricular filling
Diastolic Murmur
Pressure profile in MS
Phonocardiogram
57
Clinical Manifestations of MS:
The anterior cusp is twice the area of the posterior
cusp. The valve area is usually 56 cm2;
Clinically relevant mitral stenosis usually occurs
when the valve area decreases to less than 1 cm2
Symptoms:
i) Dyspnea and orthopnea due to elevated LAP,
elevated pulm venous and capillary pressures
ii) Fatigue
iii) Hemoptysis
iv) Palpitations & Tachycardia - Increased left atrial
size predisposes to atrial tachyarrhythmias
v) Hoarseness of voice Enlarged LA can impinge
on recurrent laryngeal nerve (Ortner's syndrome)
58
Physical examination:
i) Auscultation of heart:
The characteristic murmur of MS is a late low
-pitched diastolic rumble
In addition, an opening snap may be heard in
the first portion of diastole
Diastolic rumble occurs because of turbulent
flow across the narrowed mitral valve orifice
Opening snap, analogous to the ejection click
described for AS
The opening snap is heard only when the
patient has relatively mobile leaflets
59
ii) Auscultation of the lungs:
Reveals bilateral rales because elevated
pulmonary capillary pressures lead to
accumulation of intra-alveolar fluid
60
Atrial fibrillation is common in MS:
Acute hemodynamic decompensation may occur
when organized contraction of the atrium is lost
Thrombus in the left atrium is observed in approx.
20% of patients with MS due to stasis in LA
Prevalence of thrombus increases with age,
presence of atrial fibrillation, severity of stenosis,
and any reduction in cardiac output
Embolic events lead to neurologic symptoms
Neurologic symptoms such as transient numbness
or weakness of the extremities, sudden loss of
vision can occur
61
Etiology:
Mitral valve prolapse is now probably the most
common cause, followed by coronary artery
disease
MR may be acute or chronic or congenital:
Acute causes:
-Ruptured chordae tendineae as in infective
endocarditis; Trauma; Acute rheumatic fever
-Ruptured or dysfunctional papillary muscles as in
Ischemia; Myocardial infarction;Myocardial abscess
-Perforated leaflet as in infective endocarditis
Mitral Regurgitation (MR)
62
Chronic causes:
-Inflammatory as in Rheumatic heart disease and
Collagen vascular disease
-Infection as in Infective endocarditis
-Degenerative as in Myxomatous degeneration of
the valve leaflets; Calcification of the mitral annulus
-Rupture or dysfunction of the chordae tendineae
or papillary muscles as in Infective endocarditis;
Trauma; Acute rheumatic fever; Myocardial
infarction
63
Pathophysiology of MR:
Mitral valve fails to close properly during
ventricular systole
Regurgitation of blood into the LA from the LV
occurs during systole
Enlargement of LA and LV to accommodate
volume load
Concomitant hypertrophy of the ventricular wall
Increased diastolic filling of the left ventricle
64
Pathophysiology of MR:
In acute mitral regurgitation, the sudden
volume overload on the LA and LV is not
compensated for by chamber enlargement
and hypertrophy
Prominent atrial v waves with transmission of
this elevated LA pressure
Elevated pressure in pulmonary capillaries
Development of pulmonary edema
65
MR: Hemodynamic changes
An incompetent (leaky) mitral valve allows
blood to regurgitate from LV to LA during
ventricular systole
An elevated left atrial volume and pressure
during ventricular systole
Left ventricular volume and also pressure
increase during ventricular diastole
There is no pressure gradient between LA
and LV throughout during ventricular filling
Systolic murmur appears
66
Aortic pressure
Left atrial pressure
Left ventricular pressure
Mitral Insufficiency (Regurgitation)
Systolic Murmur
An elevated LAP during
systole with no gradient
between LVP and LAP
during ventricular diastole
Phonocardiogram
67
Symptoms of MR:
The presentation of MR depends on how
quickly valvular incompetence develops
Patients with chronic mitral regurgitation
develop symptoms gradually over time
Common complaints in chronic MR include:
Dyspnea, easy fatigability, and palpitations
Dyspnea - due to pulmonary edema
Fatigue - due to decreased forward blood flow
to the peripheral tissues
Palpitations - due to atrial fibrillation
Common complaints in acute MR include:
symptoms of left heart failure - shortness of
breath, orthopnea, and shock
68
Physical Examination in MR:
i) Laterally displaced and Hyperdynamic
Apical Impulse:
Reason for lateral displacement - The
compensatory increase in left ventricular
volume and wall thickness
Reason for hyperdynamic - The ventricle now has
a low-pressure chamber (LA) into which to eject
blood
When mitral regurgitation develops suddenly, the
apical impulse is not displaced or
hyperdynamic, because the LV has not had
enough time for compensatory volume
increases to occur
69
ii) Holosystolic (pansystolic) Murmur:
Regurgitant flow into the LA produces a high-
pitched murmur that is heard throughout systole
The murmur begins with S1, continues to the S2
Murmur is of constant intensity throughout systole
Unlike the murmur of AS, there is no variation in
the intensity of the murmur as the heart rate
changes
The murmur does not change in intensity with
respiration
It is heard best at the apex and radiates to the
axilla
70
iii) Muffled S1 and S2:
The murmur often obscures the first and second
heart sounds
iv) Loud S3:
A third heart sound is heard in a patient with
severe MR or if heart failure is present
71
Mitral Valve Prolapse (MVP)
Other terms: Floppy valve, Barlows
Etiology
Congenital
Marfans syndrome
RHD
Sequelae of MI
Pathophysiology
Valve leaflet has redundant tissue
Extra tissue balloons into LA, click sound
72
Mitral Valve Prolapse
Incidence
10-20 % of population
F > M
Clinical Presentation
Asymptomatic
Symptomatic
Palpitations
Arrhythmias
Atypical Chest Pain
73
Mitral Valve Prolapse
74
MVP-Physical Exam/Diagnosis
Thin, young females
Abnormalities
Skeletal
Heart
Auscultation
Mid-systolic click & late systolic murmur
EKG
Normal
Abnormal: Arrhythmias; non-
Specific ST-T changes
75
Physiologic maneuvers in the differential
diagnosis of heart murmurs:
1. Respiration:
Right-sided murmurs typically increase with
inspiration, while left-sided murmurs generally are
louder during expiration (RILE)
2. Valsalva maneuver:
Most murmurs decrease in length and intensity
during the Valsalva maneuver
Two excepfions ore - fhe sysfoIic murmurs oI
hyperfrophic cordiomyopofhy (HC0) & mifroI
voIve proIopse (0VP) - fhey become Iouder
76
Valsalva maneuver:
Esophageal
Pressure
(cm H2O)
Arterial
Pressure
(mm Hg)
77
Physiologic maneuvers in the differential
diagnosis of heart murmurs and sounds
3. Handgrip (isometric exercise):
Murmurs of MR , AR and VSD increase with
handgrip due to increase in afterload on LV
4. Transient arterial occlusion:
Transient external compression of both arms by
bilateral cuff inflation to 20 mmHg greater than
peak systolic pressure augments the murmurs of
MR, AR and VSD (due to increase in afterload on
LV)
This maneuver does not affect the murmurs due
to other causes
78
Physiologic maneuvers in the differential
diagnosis of heart murmurs and sounds
5. Positional changes:
i) Standing - Most murmurs diminish with
standing due to reduced preload. Exceptions:
the murmur of HCM & MVP become louder
ii) Squatting - Most murmurs become louder with
prompt squatting (or usually passive leg
raising), while the murmurs of HCM and MVP
typically soften and may disappear due to
increased preload
1
Pathophysiology Lecture Notes
Topic: HYPERTENSION & SHOCK
Lecturer: Dr. S. Upadhya
2
Pathophysiology of Hypertension
3
Patient 01:
A 55-year-old male smoker with a history of high blood
cholesterol visits his family physician for a health checkup.
He has not visited a doctor for the last 5 years. His BP
recording reveals that he has severe hypertension,
averaging about 190/130 mm Hg. Isotopic renography
reveals that the patient has compromised renal function, and
additional tests reveal that the patient has a high plasma
renin activity. Based on this evidence, the patients
physician orders an intra-arterial digital subtraction
angiography to definitively visualize the patient's renal artery
anatomy. This renal angiogram reveals a significant
asymmetric renal artery stenosis at the upstream junction of
the left renal artery and abdominal aorta that reduces the
entrance to the renal artery by 75%
4
Questions:
Based on this patient's history, what is the likely cause
of his left renal artery stenosis?
Is there any connection between the patients severe
renal artery stenosis and his hypertension?
Patients with hypertension associated with renal artery
stenosis have been shown to be at increased risk for
target organ damage (TOD), specifically to the heart
and kidneys. What unique feature of this patient's
hypertension might be best associated with increased
TOD?
Given the patient presentation in this case study, which
type of the drugs might be particularly beneficial to the
patient in treating the effects of his type of
hypertension?
5
The most likely diagnosis in patient 01:
Systemic Hypertension due to renal artery
stenosis
Other differential:
Primary hyperaldosteronism
Cushings syndrome
Reninoma
Pheochromocytoma
6
Definitions:
Hypertension (HTN) is a manifestation of
several diseases
Hypertension is generally defined as an arterial
pressure greater than 140/90 mm Hg in adults
on at least three consecutive visits
If the cause remains unknown, it is termed
essential hypertension or primary hypertension
Hypertension in which the cause is known is
called secondary hypertension
About 88% of population suffer from primary
hypertension
7
Regulation of BP by Renin-angiotensin-
aldosterone mechanism
Long term mechanism of regulation of BP
The mechanism is mediated by hormones
The mechanism regulates BP by regulating blood volume
The activation of the system in response to a low BP
produces a series of responses to increase blood volume
Blood
volume
Cardiac
output
Arterial
BP
Blood volume is altered by altering salt and water in body
8
Regulation of arterial BP by
Renin-angiotensin-aldosterone mechanism
Retention of Salt and
Water increases plasma
volume, Cardiac output
and Blood Pressure
Increase in TPR and
Blood Pressure
9
Pathogenesis of HTN:
Recall Ohms law for systemic circulation:
Mean arterial pressure =
Total peripheral resistance X Cardiac output
Mechanisms causing hypertension:
Increased peripheral vascular resistance
Prolonged increase in cardiac output
Increased blood volume
Increased blood viscosity
10
COMMON CAUSES OF HYPERTENSION
Essential hypertension
Coarctation of aorta
Salt sensitivity
Renal abnormalities
Abnormalities of the RAAS
Disorders of adrenal gland
Neurological disorders
Nitric oxide deficiency
Insulin resistance
11
Coarctation of the Aorta:
Congenital narrowing of the aorta distal to the
origin of the left subclavian artery
Blood pressure is elevated in the arms, head, and
chest but lowered in the legs
Because of low renal blood flow, plasma renin
level is increased
Stimulation of Renin-angiotensin-aldosterone
system in a positive feedback manner
Elimination of the constriction by resecting the
narrowed segment of the aorta usually cures the
condition
12
The pressure tracings from the thoracic and
abdominal aorta obtained from a 4-month-old infant
who exhibited dyspnea, difficulty feeding, and poor
weight gain
Physical examination reveals a weak femoral pulse
compared to the radial pulse with a radio-femoral
delay
Diagnosis: Coarctation of aorta just above the
diaphragm
13
Salt sensitivity:
About 55% of whites who are salt sensitive have
hypertension
A larger percentage of African origins who are salt
sensitive also have hypertension
These figures have obvious significance in terms of
recommendations about salt intake in hypertension
14
Renal causes for hypertension:
Constriction of one or both renal arteries
Tumors of the renin-secreting juxtaglomerular
cells
Ureteral obstruction: Increase in renal interstitial
pressure and stimulation of renin secretion
Acute and chronic glomerulonephritis: Kidney
loses the ability to excrete salt and thus ECF
volume is expanded
Liddle's syndrome: a condition in which there is
abnormal Na+ retention due to over-activation of
the epithelial sodium channels (ENaC)
15
Liddles syndrome
Young patient presenting with high BP
H/O family members with early onset
severe hypertension
Autosomal dominant transmission
Suppressed renin
Suppressed aldosterone
Abnormality of epithelial sodium channels
(ENaC) in distal nephron
16
Adrenal Gland Disorders:
-Conns syndrome
-Hypersecretion of deoxycorticosterone (DOC) due
to 17-hydroxylase deficiency, 11-hydroxylase
deficiency (congenital adrenal hyperplasia)
-Glucocorticoid remediable aldosteronism (GRA):
An autosomal dominant disorder in which ACTH
produces prolonged hypersecretion of aldosterone
as well as glucocorticoids. The genes encoding
aldosterone synthase and 11-hydroxylase are 95%
identical and located close together on
chromosome 8
-Glucocorticoid Excess (Cushings syndrome)
-Pheochromocytoma-disorder of adrenal medulla
17
HTN related to Insulin Resistance:
There is a higher incidence of insulin resistance,
hyperinsulinemia, hyperlipidemia, and obesity in
patients with essential hypertension and in their
normotensive relatives than in the general
population or in patients with hypertension from
known causes
This combination of abnormalities is called
syndrome X or the metabolic syndrome
Possible mechanism for HTN: Insulin resistance
causes increased insulin secretion and that the
resulting hyperinsulinemia stimulates the
sympathetic system, causing hypertension
18
Clinical Presentation of HTN:
Hypertension by itself does not cause symptoms
Mostly it is discovered during routine screening
or when patients seek medical advice for its
complications
The hypertensive patients may present with:
-Myocardial infarction
-Congestive heart failure
-Strokes of thrombotic and hemorrhagic
origin
-Hypertensive encephalopathy - confusion,
disordered consciousness, and seizures
-Renal failure
19
Physical findings in HTN:
Observable changes are generally found only in
advanced cases. These include:
-Hypertensive retinopathy - narrowed arterioles
seen on funduscopic examination; retinal
hemorrhages and exudates along with papilledema
-Left ventricular hypertrophy and cardiac
enlargement
-Bruits in the renal artery on auscultation
-A rise in BP on standing - occurs in essential
hypertension and is is usually absent in other
forms of hypertension 20
FLOW CHART SHOWING COMPLICATIONS OF HYPERTENSION
21
Some basics of CARDIAC OUTPUT
and VENOUS RETURN
22
Venous return (VR)
Venous return is the amount of blood received by the
right atrium per minute
In normal person, it is same as cardiac output (5 L/min)
The pressure gradient between the right atrium and
the peripheral veins is the driving force for VR
Higher the gradient, greater will be the venous return;
Lower the gradient, less will be the venous return
Factors that increase this gradient improve VR
Factors that increase venous return are:
Negative intrathoracic pressure
Increase in total blood volume (preload)
Contraction of skeletal muscles
23
The vascular function curve
V
e
n
o
u
s
r
e
t
u
r
n
(
L
/
m
i
n
)
Right atrial pressure (mm Hg)
It is the plot between the venous return and right atrial pressure
Normal
point
An inverse relationship exists
between RAP and VR in the
range 0 to 7 mm Hg of RAP
No further increase in VR
occurs when RAP < 0 mm Hg
as veins collapse at negative
pressures
Mean circulatory pressure
or
Mean filling pressure
24
The effect of changing total blood volume on
vascular function curve
N
N = Normal blood volume
Low blood volume:
Curve shifts downward
& to the LEFT
Mean circulatory
pressure falls
Increased blood volume:
Curve moves upward & to RIGHT
Mean circulatory pressure rises
25
Cardiac function curve or Starlings curve:
Reflects the contractile function of ventricle
Normal
CO and VR are dependent on each other
Interaction between them is best understood by
combining the two function curves 26
Combining cardiac function curve and
vascular function curve
Steady state point
&RPELQLQJ WKH WZR FXUYHV KHOSV WR SUHGLFW WKH
FKDQJHV LQ &O/9P XQGHU YDULRXV FRQGLWLRQV
27
The factors that change the cardiac and
vascular function curves
Factor Curve that gets altered
Change in myocardial Cardiac function curve
contractility
Change in blood volume Vascular function curve
[C for C; V for V]
28
Effect of increasing myocardial contractility
on combined curves:
Positive inotropic agents
Eg:Sympathetic nerves,
digitalis
Normal
N
N
Increase in contractility
Increase in cardiac output
Decrease in RAP
Increase in venous return
Steady state point moves
upward & to the left
29
Effect of increasing total blood volume
on combined curves:
Increased blood volume:
Eg:Infusion of IV fluids
Normal
N
N
Increase in blood volume
Increase in venous return
Increase in RAP
Increase in cardiac output
Steady state point moves
upward & to the right
30
Progressive course of the Heart Failure
D
A
B
C
31
Progressive course of Heart Failure
Following acute MI
Immediate effect of reduced contractility: (Point B)
There is a reduction in CO; This soon changes due to
the compensatory changes in the heart
Compensated failure: (Point C)
Blood volume expansion has partially restored the
CO by Starlings mechanism; This gradually progresses
to massive volume expansion
Decompensated failure: (Point D)
As failure progresses, there is severe reduction in
contractility despite extreme increase in preload due
to overstretching of ventricle.
At this point, increase in preload is harmful to heart!
32
Pathophysiology of Shock
33
Patient 02:
20-year old soldier, body weight 70 kg, is brought
to the field hospital with a profusely bleeding gun
wound in the left thigh
PE: Patient appears anxious and confused; The
skin is cold and wet; BP is 65/40 mmHg; HR is 144
beats/min; Pulse is weak and rapid
Lab: Hematocrit is decreased
Imaging: Arteriogram shows abrupt termination of
dye propagation in the left femoral artery
34
The most likely diagnosis in patient 02 is:
Hypovolemic shock due to femoral artery bleed
The bleeding is stopped by ligation of the bleeding
arteries, and blood transfusions are given instantly
(whole blood with a normal packed cell volume,
PCV, of 0.45)
The arterial pressure increases to a steady level of
105/70 mmHg, and the heart rate is reduced to 100
bpm. The condition of the soldier is clearly
improved and his cardiac output is measured to 3.5
l per min.
35
Definition of cardiovascular SHOCK:
An abnormality of the circulatory system in which
there is inadequate tissue perfusion because of a
relatively or absolutely inadequate cardiac output
36
The causes and types of shock:
A. Hypovolemic shock:
Inadequate volume of blood to fill the vascular
system
B. Distributive shock (also called vasogenic or
low-resistance shock):
Increased size of the vascular system produced by
vasodilation in the presence of a normal blood
volume
C. Cardiogenic shock:
Inadequate output of the heart as a result of
myocardial abnormalities
D. Obstructive shock:
Inadequate cardiac output as a result of obstruction
of blood flow in the lungs or heart
37
A. Hypovolemic shock:
Conditions:
Hemorrhage
Trauma
Surgery
Burns
Fluid loss due to severe vomiting or diarrhea
38
Physical findings in Hypovolemic Shock:
A rapid, thready pulse
Cold, pale, clammy skin
Intense thirst
Rapid respiration
Restlessness or, alternatively, torpor
Markedly decreased urine output
Lactic acidosis (the blood lactate level rises from a
normal value of about 1 mmol/L to 9 mmol/L or
more) - depresses the myocardium, decreases
peripheral vascular responsiveness to
catecholamines, and may cause coma
39
Compensatory reactions activated by
Hypovolemic Shock:
Vasoconstriction
Tachycardia
Venoconstriction
Tachypnea
Increased movement of interstitial fluid into
capillaries
Increased secretion of ADH
Increased secretion of glucocorticoids
Stimulation of renin-angiotensin-aldosterone
Increased secretion of erythropoietin
Increased synthesis of plasma proteins
40
Baroreceptor are mechanoreceptors
that detect arterial blood pressure (BP)
Increase in MAP
Stretching of carotid sinus
and aortic arch
Increased firing rate of
baroreceptors
Action potentials travel
via IX CN and X CN
Cardiovascular regulatory
centers in brain stem
41
Baroreceptor response to decrease in BP
Increase in sympathetic nerve activity
& decrease in parasympathetic nerve
activity to the heart
Increase in sympathetic nerve
activity to veins and arterioles
Increase in heart rate and
increase in contractility
Increase in
venous return
Vasoconstriction
of arterioles
Increase in cardiac output
(CO = HR x SV)
Increase in
TPR
Increase in arterial BP
(MAP = CO x TPR)
Example : Hemorrhage Fall in arterial BP
Decrease in baroreceptor impulses to cardiovasc. regulatory centers
Compensatory Mechanisms
Neurohormonal Activation
Most important hormones involved in maintaining
normal cardiovascular homeostasis include:
Angiotensin II
Epinephrine
Norepinephrine
Vasopressin (ADH)
ACTH
Aldosterone
MAP = ( MAP = ( SV x SV x HR) x HR) x TPR TPR
Sympathetic Nervous System Sympathetic Nervous System
Contractility Contractility
Tachycardia Tachycardia
Vasoconstriction Vasoconstriction
Compensatory Mechanisms:
Sympathetic Nervous System
Decreased MAP Decreased MAP
MAP = ( MAP = ( SV x SV x HR) x HR) x TPR TPR
Renin Renin- -Angiotensin Angiotensin- -Aldosterone Aldosterone
( ( renal perfusion) renal perfusion)
Salt Salt- -water water retention retention
& Thirst & Thirst
Sympathetic Sympathetic
augmentation augmentation
Vasoconstriction Vasoconstriction
Compensatory Mechanisms:
Renin-Angiotensin-Aldosterone (RAAS)
Decreased systemic blood pressure Decreased systemic blood pressure
Central baroreceptors Central baroreceptors
Stimulation of hypothalamus Stimulation of hypothalamus
Release of Vasopressin by Release of Vasopressin by
Posterior pituitary gland Posterior pituitary gland
Vasoconstriction Vasoconstriction
Increased systemic BP Increased systemic BP
- -
Compensatory Mechanisms:
Neurohormonal Activation Vasopressin
Vasopressin (ADH) Mechanism
Compensatory Neurohormonal Stimulation:
Summary
Decreased Cardiac Output
Sympathetic
nervous system
Renin-angiotensin
system
Antidiuretic hormone
(vasopressin)
Heart
rate
Contractility Vasoconstriction Circulating volume
Arteriolar
Blood
Pressure
Cardiac
output
Stroke
volume
+
- +
Venous
Venous
return to heart
( preload)
Peripheral
edema
and pulmonary
congestion
48
Consequences of increased vasomotor
discharge during hypovolemic shock:
Vasoconstriction is generalized, sparing only the
vessels of the brain and the heart
Vasoconstriction in the skin - Coolness and pallor
Vasoconstriction in the kidney Drop in GFR.
This reduces water loss, but it reaches a point at
which nitrogenous products of metabolism
accumulate in the blood (prerenal azotemia). If
hypotension is prolonged, there may be severe
renal tubular damage, leading to acute renal
failure.
49
The reason for tachypnea and its importance in
hypovolemia:
The fall in blood pressure and the loss of red cells
results in stimulation of the carotid and aortic
chemoreceptors stimulation of respiratory
centerChemoreceptor reflex
Stimulation of respiration increases thoracic
pumping and improves venous return
Stimulation of respiration also increases
vasoconstrictor discharge
50
VICIOUS CYCLES IN SHOCK-1
Fall in Blood Pressure
Low cerebral
blood flow
Ischemic brainstem depression
Loss of
sympathetic tone
Cardiac depression &
peripheral vasodilation
51
VICIOUS CYCLES IN SHOCK-2
Inadequate bloodflow to organs
Tissue hypoxia
Lactic acid accumulation & fall in pH
Metabolic acidosis
Cardiac depression
52
CELLULAR DAMAGE IN SHOCK
53
Refractory Shock:
The shock persists for hours and eventually
reaches a state in which there is no longer any
response to vasopressor drugs
Even if the blood volume is returned to normal,
cardiac output remains depressed
Factors that make shock refractory are:
-Precapillary sphincters are constricted for several
hours but then relax while postcapillary venules
remain constricted. Therefore, blood flows into the
capillaries and remains there
-Cerebral ischemia depresses vasomotor and
cardiac discharge, causing blood pressure to fall
and making the shock worse
-Reduced myocardial blood flow
54
Traumatic Hypovolemic Shock:
Traumatic shock involves severe damage to
muscle and bone - as seen in battle casualties and
automobile accident victims
Significant bleeding into the injured areas
Breakdown of skeletal muscle is a serious
additional problem when shock is accompanied by
extensive crushing of muscle (crush syndrome)
Free radicals generated at the sites cause further
tissue destruction (reperfusion-induced injury)
Increased Ca2+ in damaged cells can reach toxic
levels
Large amounts of K+ enter the circulation
Myoglobinuria worsens renal failure
55
A complication of shock that has a very high
mortality rate is:
Pulmonary damage with production of acute
respiratory distress syndrome (ARDS)
The cause for ARDS: Capillary endothelial cell
damage and damage to alveolar epithelial cells
with the release of cytokines
56
B. Distributive shock:
Conditions:
Anaphylaxis
Sepsis
Fainting (neurogenic)
In distributive shock, most of the symptoms and
signs described under hypovolemic shock are
present
Vasodilation causes the skin to be warm rather than
cold and clammy
57
Patient 03:
A 5-year-old female with no apparent medical problems is
stung by a bee while playing. Her reaction to the sting was a
greater than normal redness and itching at the site of the
sting but was otherwise uneventful. Her physician warns her
mother that this child might be allergic to bee venom and
should try to avoid being stung again. Unfortunately, 1 month
later while playing in her back yard near a bed of flowers, she
gets stung on her hand by a bee. Her mother cleans the sting
with some rubbing alcohol and applies a band-aid. However,
the area of the sting begins to turn red and swell, developing
a wheal of about a 3-cm radius around the sting within 2
minutes. The girl then rapidly develops severe difficulty
breathing and is rushed to the ER. Examination in the ER
reveals a swollen stiff abdomen, blood pressure of 80/50 mm
Hg and a heart rate of 120, with urticaria and angioedema
over her arms, abdomen, and thighs. 58
Questions:
What is the cause of the redness and swelling at
the site of the bee sting on this girl's hand?
What is the likely predominant mediator of the
redness and swelling at the sight of the bee sting?
What is the cause of the patient's low systolic,
diastolic, and pulse pressure?
How does this injection of epinephrine also help
counteract the shock associated with
anaphylaxis?
59
The most likely diagnosis in patient 03:
Anaphylactic shock
Differential diagnosis:
Septic shock
Neurogenic shock
60
Septic shock: a form of distributive shock
Most common cause of death in ICUs in USA
Initiated by release of bacterial toxins
A complex condition that includes:
-Hypoperfusion resulting from loss of plasma into
the tissues ("third spacing")
-Reduced cardiac function resulting from toxins
that depress the myocardium
-Excess production of Nitric oxide and vasodilation
-Capillary endothelial damage and depletion of
intravascular volume
-Cellular hypoxia, lactic acidosis & multiorgan
failure
61
How to assess the type of shock?
A patient is admitted with severe infection in
intensive care and is placed on a ventilator. He is
showing signs of hypoperfusion.
He may be either in hypovolemic or in septic shock.
Treatment of this patient requires definite diagnosis
of shock
(Vasopressors such as dopamine could be
catastrophic to a hypovolemic patient; but are a
valid treatment choice in septic shock)
Solution: Pulmonary artery catheterization (Swan-
Ganz catheter) and measurements of pressures
62
CO=Cardiac Output SVR=Systemic vascular resistance
PWP=Pulmonary wedge pressure CVP=Central venous pressure
= Increase; = Decrease
Distributive
Hypovolemic
CVP PWP SVR CO
A comparison of readings obtained from a Swan-Ganz
catheter to distinguish hypovolemic & distributive shock
63
C. Cardiogenic shock:
Conditions:
Myocardial infarction
Congestive Heart Failure
Arrhythmias
64
Cardiogenic Shock: Pathophysiology
Extensive infarction of LV (>30%)
Impaired pumping of blood to myocardium
Inadequate resting metabolic needs
Positive feedback vicious cycle
Congestion of the lungs and viscera resulting from
failure of the LV to put out all the venous blood
("congested shock)
The symptoms are:
Those of hypovolemic shock plus congestion of lungs
and viscera
The incidence of shock in patients with myocardial
infarction is about 10%, and the mortality rate is 6090%
65
A comparison of readings obtained from a Swan-Ganz
catheter in the three major categories of shock
Distributive
Cardiogenic
Hypovolemic
CVP PWP SVR CO
CO=Cardiac Output SVR=Systemic vascular resistance
PWP=Pulmonary wedge pressure CVP=Central venous pressure
= Increase; = Decrease 66
D. Obstructive shock:
Conditions:
Pulmonary embolism (massive)
Tension pneumothorax
Pericardial tamponade
Cardiac tumor
67
Patient 04:
A 54 year old man develops sudden onset of
dyspnea and hypotension in the coronary care unit.
He was admitted five days back following an acute
MI. He was on thrombolytic agents.
PE: tachycardia; weak, thready pulse; tachypnea;
low BP; Pallor; cool, moist skin; mild cyanosis of lips
and fingers; He has significant pulsus paradoxus
(fall in arterial pulse is 16 mm Hg with inspiration);
Elevated JVP with absence of y descent
Auscultation of heart: Heat sounds are muffled
Auscultation of lungs: not significant
ECG: Low voltage waves
Imaging: Diastolic compression of the right ventricle;
Pericardial effusion
68
The most likely diagnosis in patient 04 is:
Pericardial tamponade
Other differentials:
Myocardial infarction
Pulmonary embolism
Tension pneumothorax
Constrictive pericarditis
5upfure oI IoferoI ond onferior Iree woII IoIIowing
0I hos high risk oI pericordioI fomponode
69
Pericardial tamponade (an example of
obstructive shock):
Sudden filling of the pericardial space with fluid
Diagnosis:
Sudden onset of shortness of breath
Physical examination findings:
Three classic signs of pericardial tamponade
(Beck's triad):
Hypotension
Elevated jugular venous pressure, and
Muffled heart sounds
Additional finding: Paradoxic pulse (pulsus
paradoxus)
70
Hemodynamics of pericardial tamponade:
[Normal: The pericardium is filled with 3050 mL
of fluid; Intrapericardial pressure is about the
same as the intrapleural pressure]
Sudden addition of fluid Increase in
intrapricardial pressure to the level of the RA and
RV pressures RV collapses, preventing filling
of the heart from systemic veins
Four chambers of the heart occupy a relatively
fixed volume in the pericardial sac
Equilibration of ventricular and pulmonary artery
diastolic pressures with RA and LA pressures, all
at approximately intrapericardial pressure
71
Jugular Venous Pulse in pericardial tamponade:
JVP is elevated due to fluid in the cavity
JVPulse tracing shows:
-Normal x descent since RA can fill during
ventricular contraction
-Absent y descent: because the filling of RA is
prevented by the pericardial fluid surrounding the
chamber
Loss oI fhe "y" descenf ossociofed wifh on
eIevofed JVP is diognosfic oI pericordioI
fomponode
72
P
r
e
s
s
u
r
e
(
m
m
H
g
)
Normal
RV
Failure
Constrictive
Pericarditis:
Rapid y descent
Makes v wave
prominent
Pericardial
Tamponade:
Loss of
y descent
Comparison of JVP tracings in Normal
and abnormal conditions
73
Pulsus Paradoxus in pericardial tamponade:
Arterial systolic blood pressure normally drops
about 5 mm Hg with inspiration.
Marked inspiratory drop in systolic blood
pressure (>10 mm Hg) is an important physical
finding in the diagnosis of cardiac tamponade
A
r
t
e
r
i
a
l
P
r
e
s
s
u
r
e
T
r
a
c
i
n
g
74
The ECG findings in tamponade:
-Low voltage (amplitude) of the QRS complexes
-Electrical alternans (cyclic beat-to-beat
shift in the QRS axis)
Other causes of low voltage ECG:
-chronic obstructive pulmonary disease
-pleural effusion
-pneumothorax
-cardiomyopathy
-obesity
75
Cardiac Output
or
Venous Return
Central Venous pressure
Normal Blood Volume
Hypervolemia
Hypovolemia
Normal Contractility
Increased Contractility
Decreased Contractility
N
A
N: Normal
A: Hypovolemic shock
B: Cardiogenic shock with volume expansion
E: During exercise
B
E
COMBINED GRAPH SHOWING CERTAIN CONDITIONS
76
PWP &
CVP
in cardiogenic
shock
Вам также может понравиться
- The 12-Lead Electrocardiogram for Nurses and Allied ProfessionalsОт EverandThe 12-Lead Electrocardiogram for Nurses and Allied ProfessionalsОценок пока нет
- Cardio Notes, Heart FailureДокумент17 страницCardio Notes, Heart FailureJoy DunwanОценок пока нет
- A Simple Guide to the Heart beats, Related Diseases And Use in Disease DiagnosisОт EverandA Simple Guide to the Heart beats, Related Diseases And Use in Disease DiagnosisРейтинг: 5 из 5 звезд5/5 (1)
- Preload and AfterloadДокумент4 страницыPreload and AfterloadNeranga SamaratungeОценок пока нет
- Blood Vessel (Student)Документ148 страницBlood Vessel (Student)Jerkin Razhed PostanesОценок пока нет
- Systolic Dysfunction:: Types of Heart FailureДокумент13 страницSystolic Dysfunction:: Types of Heart FailureElisabeth F. OjhaОценок пока нет
- Inotropes, Excellent Article, With DosingДокумент47 страницInotropes, Excellent Article, With DosingNavojit ChowdhuryОценок пока нет
- S1 and S2: Valves) at The Start of The Systolic Contraction of The VentriclesДокумент10 страницS1 and S2: Valves) at The Start of The Systolic Contraction of The VentriclesCHARIEMAE CA�AZARESОценок пока нет
- Arrhythmias: Sing Khien Tiong Gpst1Документ34 страницыArrhythmias: Sing Khien Tiong Gpst1preethi preethaОценок пока нет
- ACLS Algorithms Adult 2010 Revised May 31 2011Документ12 страницACLS Algorithms Adult 2010 Revised May 31 2011arturschander3614Оценок пока нет
- Cardiac Output and Hemodynamic MeasurementДокумент29 страницCardiac Output and Hemodynamic Measurementdeepa100% (1)
- IV PDFДокумент63 страницыIV PDFelbagouryОценок пока нет
- Adrenergic Agonist and AntagonistДокумент35 страницAdrenergic Agonist and AntagonistFirjat AfiataОценок пока нет
- Immunopathology Guide for Medical StudentsДокумент21 страницаImmunopathology Guide for Medical StudentsapplesncoreОценок пока нет
- Endocrine Notes - All in One FileДокумент182 страницыEndocrine Notes - All in One FilekjОценок пока нет
- A Simple Guide to Hypovolemia, Diagnosis, Treatment and Related ConditionsОт EverandA Simple Guide to Hypovolemia, Diagnosis, Treatment and Related ConditionsОценок пока нет
- Intra Aortic Balloon PumpДокумент5 страницIntra Aortic Balloon PumpZainal 'babeh' Arifin100% (1)
- Hematopoietic SystemДокумент39 страницHematopoietic SystemapplesncoreОценок пока нет
- Critical Care Drugs 1Документ21 страницаCritical Care Drugs 1Asri ErnadiОценок пока нет
- CardiopathophysiologyДокумент63 страницыCardiopathophysiologyapplesncoreОценок пока нет
- Cardiac PhysiologyДокумент25 страницCardiac PhysiologyElai SungaОценок пока нет
- A Simple Guide to Circulatory Shock, Diagnosis, Treatment and Related ConditionsОт EverandA Simple Guide to Circulatory Shock, Diagnosis, Treatment and Related ConditionsОценок пока нет
- Hyperkalemia and HypokalemiaДокумент37 страницHyperkalemia and HypokalemiaDiena AshlihatiОценок пока нет
- Cardiac Nursing II Study GuideДокумент6 страницCardiac Nursing II Study GuiderunnermnОценок пока нет
- Cardiac Arrest, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsОт EverandCardiac Arrest, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsОценок пока нет
- Ekg Panum or OsceДокумент69 страницEkg Panum or OsceGladish RindraОценок пока нет
- Cardiac MedicationsДокумент8 страницCardiac Medicationsangeline totaram100% (2)
- Common Asthma MedicationsДокумент1 страницаCommon Asthma MedicationsHeart of the Valley, Pediatric CardiologyОценок пока нет
- Heartbeat Irregularities ExplainedДокумент5 страницHeartbeat Irregularities ExplainedKayelyn-Rose Combate100% (1)
- HW InotropesДокумент3 страницыHW InotropesNatalie YeohОценок пока нет
- Mitral Valve Regurgitation, A Simple Guide To The Condition, Treatment And Related ConditionsОт EverandMitral Valve Regurgitation, A Simple Guide To The Condition, Treatment And Related ConditionsОценок пока нет
- ECG Changes in myocardial infarctionДокумент25 страницECG Changes in myocardial infarctionginaulОценок пока нет
- Cs-Cardiac-023-Essential Cardiac LabsДокумент2 страницыCs-Cardiac-023-Essential Cardiac LabsColeen YraolaОценок пока нет
- Hypertensive Crisis: Megat Mohd Azman Bin AdzmiДокумент34 страницыHypertensive Crisis: Megat Mohd Azman Bin AdzmiMegat Mohd Azman AdzmiОценок пока нет
- OutputДокумент12 страницOutputzenishzalamОценок пока нет
- Cardiac Output Regulation and MeasurementДокумент18 страницCardiac Output Regulation and MeasurementGauravSinghОценок пока нет
- Cardiac Cycle: Mechanical Event and Their Electrical and Clinical CorrelationДокумент28 страницCardiac Cycle: Mechanical Event and Their Electrical and Clinical Correlationhawas muhammed100% (1)
- Describe The Factors Affecting Cardiac OutputДокумент6 страницDescribe The Factors Affecting Cardiac OutputSis SukarnoОценок пока нет
- Mechanical Properties of The Heart IДокумент30 страницMechanical Properties of The Heart ISeba W WolfОценок пока нет
- Cardio-Vascular Disease: Mitral Stenosis & Mitral RegurgitationДокумент25 страницCardio-Vascular Disease: Mitral Stenosis & Mitral Regurgitationyulia silviОценок пока нет
- DRUGS AND DEFIBRILLATION IN CARDIAC ARRESTДокумент20 страницDRUGS AND DEFIBRILLATION IN CARDIAC ARRESTAfrida Sahestina100% (1)
- HTNДокумент54 страницыHTNapi-232466940Оценок пока нет
- Bio Physio NuggetsДокумент141 страницаBio Physio NuggetsUjjwal PyakurelОценок пока нет
- Nursing Responsibilities For The Patient Will Undergo Cardiac CatheterizationДокумент4 страницыNursing Responsibilities For The Patient Will Undergo Cardiac CatheterizationCharlene Jacobe Cornista100% (1)
- Physiology notes on cardiac muscle and the heart's conductive systemДокумент37 страницPhysiology notes on cardiac muscle and the heart's conductive systemDany SamuelОценок пока нет
- Cardiomyopathy Joisy AloorДокумент31 страницаCardiomyopathy Joisy AloorJoisy AloorОценок пока нет
- Functional Human Physiology: For The Exercise and Sport Sciences The Cardiovascular System: Cardiac FunctionДокумент186 страницFunctional Human Physiology: For The Exercise and Sport Sciences The Cardiovascular System: Cardiac FunctionBery Agana F. PurbaОценок пока нет
- Diabetic Ketoacidosis and Hyperosmolar Hyperglycaemic StateДокумент55 страницDiabetic Ketoacidosis and Hyperosmolar Hyperglycaemic StateEva PrimanandaОценок пока нет
- IV Lab Practice Problems Answers SP 2013 PALДокумент2 страницыIV Lab Practice Problems Answers SP 2013 PALjmraczynskiОценок пока нет
- L9 PDFДокумент22 страницыL9 PDFMiles HuiОценок пока нет
- 2 Cardiovascular System: Describe The Systemic Circulation in The Body and Give Its ImportanceДокумент28 страниц2 Cardiovascular System: Describe The Systemic Circulation in The Body and Give Its ImportanceBhavin ChangelaОценок пока нет
- 6.3 Defence Against Infectious DiseaseДокумент43 страницы6.3 Defence Against Infectious DiseaseAlacrity Xenoion SpadesОценок пока нет
- CardioДокумент7 страницCardioGerald AndrinОценок пока нет
- Esi (1Документ114 страницEsi (1Ferina Mega SilviaОценок пока нет
- Disorders of The Circulatory System Table-AnswersДокумент2 страницыDisorders of The Circulatory System Table-Answersapi-281108263Оценок пока нет
- Evaluation of Chest Pain in Primary Care Patients-AAFPДокумент3 страницыEvaluation of Chest Pain in Primary Care Patients-AAFPnouval_iqbalОценок пока нет
- Introduction to Cardiovascular PhysiologyДокумент29 страницIntroduction to Cardiovascular PhysiologyMariuca MaryОценок пока нет
- Lecture On Atrial Pressure Changes and JVP by Dr. RoomiДокумент9 страницLecture On Atrial Pressure Changes and JVP by Dr. RoomiMudassar Roomi100% (2)
- Anti Asthmatic DrugsДокумент8 страницAnti Asthmatic DrugsNavjot BrarОценок пока нет
- Tocolytic Agents and Anticonvulsants for Preterm LabourДокумент95 страницTocolytic Agents and Anticonvulsants for Preterm LabourPriya jОценок пока нет
- Procedure For Patent Ductus Arteriosus (PDA) Device ClosureДокумент13 страницProcedure For Patent Ductus Arteriosus (PDA) Device ClosurejaganjaggiОценок пока нет
- Arterial Lines in PACU: Presented by Autum Jacobs RN, BSNДокумент34 страницыArterial Lines in PACU: Presented by Autum Jacobs RN, BSNinuko1212Оценок пока нет
- Head To Toe Checklist (Masroni)Документ13 страницHead To Toe Checklist (Masroni)hillary elsaОценок пока нет
- Bones and JointsДокумент20 страницBones and JointsapplesncoreОценок пока нет
- Fluid and Hemodynamic DisordersДокумент19 страницFluid and Hemodynamic DisordersapplesncoreОценок пока нет
- Renal Pathology Guide on Kidney Structure and FunctionДокумент37 страницRenal Pathology Guide on Kidney Structure and Functionapplesncore100% (1)
- Gastrointestinal Tract (Partial Edit)Документ47 страницGastrointestinal Tract (Partial Edit)applesncoreОценок пока нет
- Cover Letter Language ExamplesДокумент2 страницыCover Letter Language ExamplesapplesncoreОценок пока нет
- Pathology of The Lung Objectives: Define and Use in Proper Context The Following TermsДокумент45 страницPathology of The Lung Objectives: Define and Use in Proper Context The Following TermsapplesncoreОценок пока нет
- Pediatric PathologyДокумент27 страницPediatric PathologyapplesncoreОценок пока нет
- Blood Vessel Functions and DiseasesДокумент36 страницBlood Vessel Functions and DiseasesapplesncoreОценок пока нет
- Pathology of Infections Objectives: ©bharti B-Pathologyof infections-SGUSOM 2Документ25 страницPathology of Infections Objectives: ©bharti B-Pathologyof infections-SGUSOM 2applesncoreОценок пока нет
- Lecture 9Документ7 страницLecture 9applesncoreОценок пока нет
- Neoplasia Path NotesДокумент13 страницNeoplasia Path NotesapplesncoreОценок пока нет
- Gluteraldehyde, Peracetic Acid Alcohol, Iodophors QAC (Quarternary Ammonium Compounds)Документ3 страницыGluteraldehyde, Peracetic Acid Alcohol, Iodophors QAC (Quarternary Ammonium Compounds)applesncoreОценок пока нет
- Draft of PICO 2questionДокумент5 страницDraft of PICO 2questionapplesncoreОценок пока нет
- Lecture 1Документ2 страницыLecture 1applesncoreОценок пока нет
- Chapter 3 ImmunoДокумент4 страницыChapter 3 ImmunoapplesncoreОценок пока нет
- Bordetella PertussisДокумент5 страницBordetella PertussisapplesncoreОценок пока нет
- Epidemiology 2Документ5 страницEpidemiology 2applesncoreОценок пока нет
- My Labeled Slides - UterusДокумент19 страницMy Labeled Slides - UterusapplesncoreОценок пока нет
- Midterm GOLD NotesДокумент41 страницаMidterm GOLD NotesapplesncoreОценок пока нет