Академический Документы
Профессиональный Документы
Культура Документы
BOD Dermatology
Загружено:
lizzy596Исходное описание:
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
BOD Dermatology
Загружено:
lizzy596Авторское право:
Доступные форматы
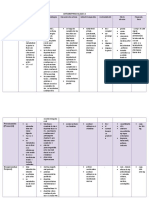
Dermatology Lecture List
1. Introduction
2. Eczematous Dermatitis & Urticaria
3. Common Dermatologic Problems
4. Path of Inflammatory Skin Disease
5. Pathophysioogy of Non-Melanoma Skin Cancer
6. Blistering Disorders
7. Nevi and Malignant Melanoma
01: Introducing
Definitions
Primary Lesions
Initial (and sometimes the only) manifestation of skin disorder
Macule
flat lesion, can be any shape, size, or color, cant palpate!
Papule Plaque
raised lesion, any shape or color. 1 cm is the cutoff (papule is smaller)
Nodule
spherical-ish lesion from dermis or subQ fat. If large = tumor
Wheal
= hive round lesion results from edema in dermis
Bulla Vesicle
blister. 1 cm is the cutoff (bulla is smaller)
Pustule
a bulla or vesicle filled with pus
Secondary Lesions
s in skin which are superimposed upon or occur subsequently to primary lesions
Erosion
all or part of epidermisi is lost. heals WITHOUT scarring (dermis not involved)
Ulcer
hole in skin: loss of full thickness of epidermis + part/all of dermis. heals WITH scarring
Excoriation
linear erosion from scratching
Fissure
crack/split in skin
Scale
thick stratum corneum
Crust
scab: dried stuff
Atrophy
thinning of skin. generalized: phsyiologic aging; or localized: stretch marks
Lichenification
thickening of skin. exxaggeration of normal skin markings, results from repeated rubbing or
scratching
Arrangement of Lesions
Linear
curved (just kidding)
Annular
ring-shaped
Serpiginous
wandering or twisting, like a snake
Herpetiform
tight clustering of lesions heaped on top of on another; taken from the fashionable style of paris
herpes
Dermatomal
lesions in a dermatome: shingles!
02: Eczematous Dermatitis & Urticaria
Atopic Dermatitis
Definition
Atopic Dermatitis (AD) = chronic pruritic
inflammation of skin associated with allergy
Eczema = often used synonymously with AD,
but it technically means a specific reaction
pattern of erythema, scaling, and vesicles; can
have many causes
acute: erythema, vesicles, edema, serous
exudate
chronic: lichenification, scale,
hyperpigmentation
Pathophysiology
Complicated: involves T cells, Langerhans cells,
Eos, keratinocytes, cytokines, IgE
Type I HSR: IgE in most. IL-4 may play major
role in causing IgE (IL-4 inhibits IFN-)
Immunology review: dependent on which
cytokines are present, Th0 are driven
towards Th1 (IL-12) or Th2 (IL4)
IL-4 stimulate B cells to make IgE
Aeroallergens: seasonal variation, + test to skin
dust in most patients
Hyperresponsive Langerhans cells and T cell
activation
Defective epidermal barrier: ceramides
penetration of irritants, allergens, and microbes
S. aureus: up to 90% colonization; anti-staph
antibiotics leads to rapid response
Food: Specific food elimination (nuts, etc) may
be useful with severe AD, but not much of a
difference in mild/moderate cases.
Defective cell-mediated immunity: pts
susceptible to viral and fungal skin infections
due to epidermal barrier and lack of
defensins in skin
Over 2/3 have family or personal history of atopy
(allergy)
Clinical
60% get AD in first year of life; only 10% get it
between the ages of 6-20
Pruritis is universal feature: itch rash
dry skin
Skin
poorly-demarcated, erythematous, scaly plaques
oozing, excoriations, crusts
lichenification (if chronic)
any area can be affected, but distribution varies
with age, typically in flexor creases
Associated Findings
ichthyosis vulgaris: fish-like scaling
piyriasis alba: scaly hypopigmented plaques
dennie-morgan sign: infraorbital eyelid folds
follicular prominence
hyperlinear palms
Histopathology
not needed for diagnosis
acanthosis: tickened epiderms
spongiosis: intraepidermal intercellular edema
dermal infiltrate of lymphs, monocytes, mast
cells
Course
60% spontaneous remission by age 5
95% remission by age 20
Treatment
hydration: no soap
topical anti-inflammatory agents (corticosteroids)
topical calcineurin inhibitors
calcineurin is a protein phosphatase that
activates IL-2 transcription
IL-2 growth and differentiation of T cells
calcineurin is inhibited by pimecrolimus,
tacrolimus, and cyclosporine
may risk of skin cancer and lymphoma
antihistamines
antistaph antibiotics (topical or systemic)
Contact Dermatitis
Definition
An acute, subacute, or chronic inflammation of
epidermis and dermis caused by external agents
two types
primary irritant: something irritates the skin
directly. Not immune-mediated.
allergic: Type IV HSR
Etiologic Agents
allergic dermatitis:
poison ivy, oak, etc. contain Rhus antigen
nickel
most allergens are haptens
irritant dermatitis:
frequent hand washing, diaper contents
Clinical
pruritis/burning of skin
delayed onset of 7-10 days in allergic dermatitis
(but with repeated exposure, can be accelerated
to 12 hrs)
Skin
acute: erythema, edema, vesicles, erosions
subacute: mild erythema, less vesiculation,
some thickening
chronic: lichenification, hyperpigmentation,
scale, excoriations, NO vesicles
lesions are localized to areas that were exposed
to irritant
02: Eczematous Dermatitis & Urticaria
Histopathology
acute: spongiosis in epidermis, vesicles and
lymphocytes in dermis
intraepidermal vesicles, spongiosis, mixed
perivascular infiltrate in upper dermis
subacute: acanthosis and scale/crust
less epidermal edema, but exocytosis, scaling,
crust
chronic: psoriasiform epidermal hyperplasia,
parakeratosis, dermal fibrosis
minimal edema, but acanthosis,parakeratosis
lichen simplex chronicus: pronounced acanthosis
and hyperkaratosis
irritant dermatitis has more superficial vesicles
and PMNs compared with allergic
Lab
patch test: apply allergen to skin
Treatment
antihistamines, topical (or systemic if severe)
corticosteroids, dressings
Urticaria and Angioedema
Definition
Urticaria (Hives) = pruritic eruption of transient
edematous papules and plaques called wheals.
Angioedema = large edematous plaques of the
dermis and subcutaneous tissue
Types
IgE-mediated
completment-mediated
physical (vibration, cold)
mast cell degranlators (morphine, etc)
hereditary angioedema: C1 inactivator
C1 is always active continues to generate
vasoactive C3a & C5a
capillary permeability
Treat with Danazol ( concentration C1
inactivator)
Pathophysiology
Most IgE mediated
complement-mediated urticaria triggered by
immune complexes anaphylatoxin release
mast cell degranulation
Clinical
pruritic lesions that last hours rather than days
wheals occur whin 36 hours after challenge with
causative agent
angioedema swelling of mucous membranes
involving larynx, can compromise airway
Skin
wheals can have multiple shape, size
dermographism: a linear wheal with flar occurs
where skin is stroked with a firm object
Histopathology
edema of dermis and subq tissue
infiltrate is eosinophil-rich if IgE mediated or
PMN-rich of complement mediated
Course
new lesions may develop for weeks after
offending agent removed
only 50% of patients are free of the problem in 1
year
hereditary angioedema can be fatal
Treatment
antihistamines are mainstay of therapy
symptomatic: cool bath, antipruritic lotions
epinephrine for laryngeal edema & anaphylaxis
danazol for hereditary angioedema
03:Common Skin Disorders: Acne, Warts, Psoriasis, Seborrheic Dermatitis
Acne
Definition: disease of pilosebaceous follicle
pathognomonic lesion: comedo
Pathophysiology
pilosebaceous follicle is a special type of hair
follicle that produces a tiny vellous (fine) hair
a big sebaceous gland is attached to the follicle
produces sebum (TGLs)
How acne happens
A: normal follicle
B: open comedo
(blackhead)
C: closed comedo
(whitehead)
D: papule
E: pustule
1) Microcomedo formation
At puberty, infundibular orifice of the
pilosebaceous follicle gets narrowed due to
retention hyperkeratosis, resulting in a
microcomedo
retention hyperkeratosis = accumulation of plates
of keratin inlumen
genetics and FFA in follicle promote this process
microcomedo = plug of keratin
If microcomedo enlarges
forms macrocomedo = open comedo =
blackhead
If microcomedo doesnt enlarge plug
allows sebaceous secretion in follicle
closed comedo = whitehead
2) sebaceous gland secretion ( by androgens)
3) Propionibacterium acnes: anaerobic, G+
P. acnes loves sebum makes FFA
further stimulation of retention
hyperkeratosis
P. acnes is chemoattractive to PMNs
4) Neutrophils
PMNs release proteolytic enzymes whole
mess is extruded into dermis
inflammatory papule pustule
(superficial abscess in dermis)
inflammatory nodule results when
inflammatory infiltrate and abscess in region
of sebaceous gland seen in nodulocystic
acne
Treatment
1) treat retention hyperkeratosis
tretinoin (retin-A) and adapalene (differin)
are vitamin A analogues: keratin
no microcomedo formation
most important (earliest in pathogenesis)
peeling agents (sulfur-salicylic acid) peel
retained keratin from follicle infundibulum
2) treat sebum secretion
isotretinoin (accutane) is systemic vit A
derivative (13-cis-retinoic acid)
causes irreversible squamous metaplasia of
sebaceous glands
turns off all sebum secretion
extremely teratogenic!
antiandrogens (estrogens, glucocorticoids,
flutamide, spironolactone)
ortho tricyclen was approved for treatment of acne
3) treat P. acnes
systemic antibiotics (erythromycin,
tetracycline, doxycycline, minocycline)
benzoyl peroxide: topical agent, suppresses
growth of P. acnes
4) treat PMNs
systemic agents that inhibit PMNs (steroids,
dapsone, colchicine) are not really used due
to side effects
Note that tetracycline and erythromycin also
seem to inhibit PMN chemotaxis
Warts
Etiology: HPV
Clinical
keratinocytes above granular layer are infected
transmission by direct contect
incubation 1-12 months
incidence in small children usually have
spontaneous involution
Findings: different appearance in different sites
extremities: common wart
face: filiform or flat
plantar surfaces: thickened plaques or punctate
hyperkeratoses
nether regions: cauliflower = condyloma
acuminata, spread by sex
Laboratory
clinical diagnosis, but sometimes warts can be
hard to distinguish from benign growths such as
seborrheic keratosis or precancers/cancerous
growths such as actinic keratoses or squamous
cell carcinoma biopsy!
characteristic histological finding is vacuolated
cells in upper dermis
Treatment
no single effective therapy: physically destroy
(laser, freeze, burn)
interferon may be helpful: imiquamod may
involve local release of endogenous interferon
Complications
infants born to mom with condyloma acuminata
may rarely develop laryngeal papillomas
cervical cancer!
03:Common Skin Disorders: Acne, Warts, Psoriasis, Seborrheic Dermatitis
Psoriasis
Definition: chronic skin dz of unknown cause
affects ~1% of US/european population, but
uncommon in native americans and asians
M=F
Clinical presentation: can mix and match these types
Psoriasis Vulgaris
plaque-type, most common form
sharply-demarcated red plaques with silver-
white scale
elbows, knees, lower legs, scalp
chronic & stationary
Guttate Psoriasis ( drop-like )
papules with sharp borders and silver scale
usually erputs acutely in generalized fashion
triggered by GAS
Erythrodermic Psoriasis
a cause of exfoliative erythroderma
entire skin surface becomes red and scaly
may occur suddenly
Generalized Pustular Psoriasis
usualy acute and generalized
no scale, but surfaces of bright red plaques
are studded with pustules
Localized Pustular Psoriasis
planter & palmar aspects of hands, feet,
fingers, toes
pustules may occur in crops or waves on a
base of atrophic erythematous plaques
Histopathology: all forms have same pathology
1) psoriasiform epidermal hyperplasia with loss
of granular layer
2) elongated dermal papillae and enlarged
capillaries
3) PMNs in dermis and within epidermis
4) lymphocytes in dermis
5) parakeratotic scale
Associated diseases
psoriatic arthritis: destructive arthritis which may
accompany psoriasis
Pathogenesis: vicious cycle
1) rapidly growing epidermis
2) inflammatory cells in dermis and
epidermis
inflammation induces growth and vice
versa
genetic factors (B27)
environmental factors (trauma = Koebner
phenomenon), drugs, strep infections, stress,
can set the disease in motion
Treatment aimed at controlling, not curing
Antiinflammatory (AI), antiproliferative (AP), or
immunomodulatory (IM) treatments are used
mild/moderate disease: AI & AP
moderate/severe disease: AI, AP & IM
Seborrheic Dermatitis ( dandruff )
Definition
inflammatory disorder with erythematous scaly
plaques involving arreas of skin rich in
sebacaeous glands (scalp, face, chest)
Clinical
Who gets it?
common in infancy and adulthood
uncommon between age 6 and puberty
with HIV or Parkinsons (of all things)
In infants
scalp and diaper area
cradle cap = scalp covered with
erythematous scaly dermatitis
in children, its not pruritic, but may become
bacterially superinfected
Leiners disease = SD exfoliative
erythoderm
sepsis + diarrhea + wasting
In adults
involves scalp: pruritus and scaling
more severe with HIV or PD
only rarely progresses to exfoliative
erythroderm
bacterial superinfection pustules or
impetiginized crusting
can develop seborrheic
blepharoconjunctivitis if extensive facial
involvement
Histopathology
spongiotic dermatitis with moderate acanthosis,
intracellular edema and spongiosis
mounts of parakeratotic scale around ostia of
hair follicles
perivascular lymphocytic infiltrate in dermis
Pathogenesis
lipophilic yeast Pityrosporum ovale produces
inflammatory rxn
Treatment
inhibit growth of P. ovale, reduce inflammation,
remove scale
antiseborrheic shampoo
can use topical corticosteroids
is there any skin disease that is not treated
with topical corticosteroids?
04: Pathology of Inflammatory Skin Diseases
Terminology
Acantholysis
broken intercellular bridges between
keratinocytes normally polygonal cells
become round
Eczema/Eczematous
eruption with erythema, scale, and vesicles
histological correlated is spongiosis
Epidermotropism
random permeation of epidermis by atypical
lymphocytes
hallmark of mycosis fungoides
Exocytosis
entry of normal lymphocytes into epidermis
during inflammatory event
normally permeation at all levels with associated
spongiosis and scale formation
Interface
rxn affecting dermoepidermal junction (DEJ)
two main forms: lichenoid and vacuolar
Lichenoid
clinical meaning: flat-topped violaceous
papules with enhanced skin markings
pathological meaning: band-like
inflammatory infiltrate, with obscures DEJ
accoated with keratinocyte necrosis
Lichenification
palpable thickening of skin with accentuated
markings, a secondary change
Hyperkaratosis (Ortho- and Parakeratosis)
too much stratum corneum clinically
manifests as scale
ortho: no nuclei
para: retained nuclei (always abnormal)
hallmark of eczematous (spongiotic)
dermatitis
Spongiosis
intercellular edema, evident by enhanced
visualization of spines (intercellular bridges)
Inflammatory reaction patterns
Spongiotic:
Characteristics
characteristic feature of eczematous
dermatitis
atopic dermatitis
nummular dermatitis
contact dermatitis
other spongiotic processes
seborrheic dermatitis
pityriasis rosea
04: Pathology of Inflammatory Skin Diseases
Phases may overlap (acute, subacute,
chronic)
Acute eczematous (spongiotic) dermatitis
minimal epidermal hyperplasia
spongiotic vesicles
langerhands cell-rich microvesiculation
dermal inflammatory infiltrate
scale has NOT yet formed
Subacute
hyperplasia
mild spongiosis
parakeratosis
Chronic
hyperplasia (may even be psoriasiform)
spongiosis
more hyperkeratosis
Psoriasiform
like psoriasis, duh
regular elongation of rete ridges, with bulbous
expansioon of tips
thinning of supra-papillary plates (portion of
epidermis above dermal papilla)
extensive parakeratosis
PMNs
munros microabscesses = PMN aggregates
layered within parakeratosis
Less commonly: spongiform pustules of Kogoj =
intercalation of PMNs between keratinocytes
Interface dermatitis
characteristics
these processes disrupt the DEJ
keratinocyte necrosis & pigment
incontenence
Lichenoid
band-like infiltrate obscures jxn
prototype: lichen planus
orthokeratosis
saw-toothed epidermal hyperplasia with
hypergranulosis
mononuclear inflammatory infiltrate (
eosinophils)
Note: in drug-induced lichenoid HSR,
see eosinophils
Vacuolar
presence of clear vacuoles on either side of
DEJ
seen in SLE, erythema multiforme, and
acute GVH disease
Erythema Multiforme
Herpes-associated: EM minor
Drug associated: EM major (Stevens-Johnson)
04: Pathology of Inflammatory Skin Diseases
Vesiculobullous
characteristics
divided into two categories depending on
where the skin splits in the blistering process
intra-epidermal
gross
flaccid bullae (blisters)
histology
acantholysis
primarily pemphigus disorders
rarely see in diseases of epidermal maturation &
keratinization:
grovers, darrier-white, hailey-hailey
sub-epidermal
tense blisters, less susceptible to rupture
non inflammatory:
epidermolysis bullosa acquisita
Eos:
bullous pemphigoid
PMNs:
dermatitis herpetiformis
bullous lupus
linear IgA dz
Hair follicle-based inflammation
Acne vulgaris
comedo = keratin-plugged follicule infected
with bacteria
inflammation papules, cysts, nodules
Rosacea
gross
erythematous facial rash with flushing triggered by
hot beverages, EtOH, stress
histology
follicular spongiosis
demodex mites within follicles
telanggiectasias
Granulomatous
characteristics
activated (epithelioid) macrophages
Sacoidal
non-necrotizing grandma-lomas
necrosis
inflammation
Necrobiotic granulomatous inflammation: living
dead (degenerative connective tissue
interspersed with macrophages)
Granuloma annulare
gross
papular eruption
may coalesce to form annular plaques on
extremities
histology
collagen degeneration with dermal mucin
surrounding palisaded granulomatous rxn
Necrobiosis lipoidica
gross
yellowish waxy plaques over shins
associated w/ DM
histology
pan-dermal granulomtous rxn
lymphplasmacytic inflammation
granulomas with giant cells
Necrotizing granulomas
infectious granulomas
caseating if TB or fungal
Vasculopathic
most common: leukocytoclastic (hypersensitivity
vasculitis)
necrotizing small vessel vasculitis
seen w/drug HSR rxns or w/CT dz
Вам также может понравиться
- JAUNDICE Internal Medicine PresentationДокумент34 страницыJAUNDICE Internal Medicine PresentationNano BaddourОценок пока нет
- 8 Steps To Solving Acid-Base ProblemsДокумент2 страницы8 Steps To Solving Acid-Base Problemslizzy596Оценок пока нет
- Uwise Gynecology and BreastДокумент24 страницыUwise Gynecology and Breastlizzy596Оценок пока нет
- Complications of LaborДокумент53 страницыComplications of Laborlizzy596Оценок пока нет
- Uwise NeoplasiaДокумент17 страницUwise Neoplasializzy596Оценок пока нет
- Bilary TractДокумент32 страницыBilary Tractlizzy596Оценок пока нет
- Dr. Vodde Changes in Specific Diagnoses From DSM IV To 5Документ183 страницыDr. Vodde Changes in Specific Diagnoses From DSM IV To 5lizzy596Оценок пока нет
- Psychiatry For Medical Students and ResidentsДокумент80 страницPsychiatry For Medical Students and ResidentsNabeel Kouka, MD, DO, MBA, MPH100% (4)
- 2012-13 Psychiatry Board ReviewДокумент79 страниц2012-13 Psychiatry Board Reviewlizzy596100% (1)
- Nasogastric Tube InsertionДокумент1 страницаNasogastric Tube Insertionlizzy596Оценок пока нет
- ReducingДокумент13 страницReducinglizzy596Оценок пока нет
- Conduct Disorders TreatmentДокумент9 страницConduct Disorders Treatmentlizzy596Оценок пока нет
- 2012-13 Psychiatry Board ReviewДокумент79 страниц2012-13 Psychiatry Board Reviewlizzy596100% (1)
- Bladder CatheterizationДокумент1 страницаBladder Catheterizationlizzy596Оценок пока нет
- Liver and Biliary NotesДокумент16 страницLiver and Biliary Noteslizzy596Оценок пока нет
- Surgical History DemonstrationДокумент2 страницыSurgical History Demonstrationlizzy596Оценок пока нет
- Female Reproduction Pathology ReviewДокумент23 страницыFemale Reproduction Pathology Reviewlizzy596Оценок пока нет
- Ventilation Cheat SheetДокумент1 страницаVentilation Cheat Sheetlizzy59683% (6)
- Cardio NotesДокумент7 страницCardio Noteslizzy596Оценок пока нет
- 2012 ECG HandoutДокумент40 страниц2012 ECG Handoutlizzy596Оценок пока нет
- Week 1 - Trauma (BB)Документ11 страницWeek 1 - Trauma (BB)lizzy596Оценок пока нет
- Esophagus and Stomach NotesДокумент15 страницEsophagus and Stomach Noteslizzy596Оценок пока нет
- Surgical Intensive CareДокумент95 страницSurgical Intensive Carelizzy596Оценок пока нет
- B. Belingon - Notes From Case Session Slides, Anna's Notes (Dr. Esterl), Becky's Notes (Dr. Nguyen)Документ11 страницB. Belingon - Notes From Case Session Slides, Anna's Notes (Dr. Esterl), Becky's Notes (Dr. Nguyen)lizzy596Оценок пока нет
- Bladder BugsДокумент10 страницBladder Bugslizzy596Оценок пока нет
- GlomerulonephritisДокумент1 страницаGlomerulonephritismaleskunОценок пока нет
- Week 2 Critical CareДокумент8 страницWeek 2 Critical Carelizzy596Оценок пока нет
- B. Belingon - Notes From Case Session Slides, Becky's Notes (Dr. Nguyen)Документ14 страницB. Belingon - Notes From Case Session Slides, Becky's Notes (Dr. Nguyen)lizzy596Оценок пока нет
- Kidney SyndromesДокумент35 страницKidney Syndromeslizzy596Оценок пока нет
- Micro InfectiousDiseaseДокумент17 страницMicro InfectiousDiseaselizzy596Оценок пока нет
- The Yellow House: A Memoir (2019 National Book Award Winner)От EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Рейтинг: 4 из 5 звезд4/5 (98)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceОт EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceРейтинг: 4 из 5 звезд4/5 (895)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeОт EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeРейтинг: 4 из 5 звезд4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingОт EverandThe Little Book of Hygge: Danish Secrets to Happy LivingРейтинг: 3.5 из 5 звезд3.5/5 (399)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaОт EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaРейтинг: 4.5 из 5 звезд4.5/5 (266)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureОт EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureРейтинг: 4.5 из 5 звезд4.5/5 (474)
- Never Split the Difference: Negotiating As If Your Life Depended On ItОт EverandNever Split the Difference: Negotiating As If Your Life Depended On ItРейтинг: 4.5 из 5 звезд4.5/5 (838)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryОт EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryРейтинг: 3.5 из 5 звезд3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerОт EverandThe Emperor of All Maladies: A Biography of CancerРейтинг: 4.5 из 5 звезд4.5/5 (271)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyОт EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyРейтинг: 3.5 из 5 звезд3.5/5 (2259)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersОт EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersРейтинг: 4.5 из 5 звезд4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnОт EverandTeam of Rivals: The Political Genius of Abraham LincolnРейтинг: 4.5 из 5 звезд4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaОт EverandThe Unwinding: An Inner History of the New AmericaРейтинг: 4 из 5 звезд4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreОт EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreРейтинг: 4 из 5 звезд4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)От EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Рейтинг: 4.5 из 5 звезд4.5/5 (121)
- ScabiesДокумент5 страницScabiespakemainmainОценок пока нет
- 01 - Onsite Sanitation TechnologiesДокумент80 страниц01 - Onsite Sanitation TechnologiesDivyam ShreevatsalОценок пока нет
- The Sober Truth: Debunking The Bad Science Behind 12-Step Programs and The Rehab IndustryДокумент3 страницыThe Sober Truth: Debunking The Bad Science Behind 12-Step Programs and The Rehab IndustryEmma-Jean Weinstein100% (3)
- 7.hematology SummaryДокумент91 страница7.hematology SummaryPeter Shirima100% (1)
- Mcguire 1991Документ8 страницMcguire 1991Angela RamirezОценок пока нет
- ,previewДокумент57 страниц,previewhoàng đình sơn60% (5)
- Neuropsychologia: Jade Dignam, David Copland, Alicia Rawlings, Kate O 'Brien, Penni Burfein, Amy D. RodriguezДокумент12 страницNeuropsychologia: Jade Dignam, David Copland, Alicia Rawlings, Kate O 'Brien, Penni Burfein, Amy D. RodriguezFrancisco Beltrán NavarroОценок пока нет
- Anemia PPT 3 Nov 2014Документ60 страницAnemia PPT 3 Nov 2014Susi DesmaryaniОценок пока нет
- SCAI Shock Classification DeckДокумент22 страницыSCAI Shock Classification DeckJimmy JimmyОценок пока нет
- MHFW OrderДокумент4 страницыMHFW OrderNavjivan IndiaОценок пока нет
- Caregiving Final 2nd Sem ExamДокумент3 страницыCaregiving Final 2nd Sem ExamRichard CortezОценок пока нет
- Airway Clearance TechniquesДокумент14 страницAirway Clearance TechniquesKhushboo DurejaОценок пока нет
- Poster ISCP10 Final Daft CWCДокумент1 страницаPoster ISCP10 Final Daft CWCVizaОценок пока нет
- The Case of Dora and Her DreamsДокумент5 страницThe Case of Dora and Her DreamsHardik Motsara100% (1)
- Punjab Drugs Rules 2007Документ33 страницыPunjab Drugs Rules 2007RphNaeemMalik75% (12)
- Antiaritmice Clasa I A MedicamentДокумент3 страницыAntiaritmice Clasa I A MedicamentAndreea ElenaОценок пока нет
- How - . - I Train Others in Dysphagia.Документ5 страницHow - . - I Train Others in Dysphagia.Speech & Language Therapy in PracticeОценок пока нет
- Youstina Khalaf Exam 26-5Документ6 страницYoustina Khalaf Exam 26-5M Usman KhanОценок пока нет
- Problem-Solution Essay FinalДокумент8 страницProblem-Solution Essay FinalNoriko May ManarinОценок пока нет
- Chapter 1 Developmental Disorders of The Oral CavityДокумент6 страницChapter 1 Developmental Disorders of The Oral CavityArafat Masud NiloyОценок пока нет
- Typhon Cases 2Документ7 страницTyphon Cases 2api-483865455Оценок пока нет
- ANAESTHESIA FOR GASTROINTESTINAL CANCER SURGERIES AutosavedДокумент40 страницANAESTHESIA FOR GASTROINTESTINAL CANCER SURGERIES AutosavedKavyasree KatamОценок пока нет
- Cell WallДокумент43 страницыCell WallRao KashifОценок пока нет
- NBME Practice TestДокумент13 страницNBME Practice TestZoë IndigoОценок пока нет
- Trastorno de Ansiedad Artículo en Ingles: CursoДокумент11 страницTrastorno de Ansiedad Artículo en Ingles: CursocamilaОценок пока нет
- Ati Communication NR 341 PDFДокумент3 страницыAti Communication NR 341 PDFmp1757Оценок пока нет
- Pediatric DisordersДокумент182 страницыPediatric DisordersErnesto Trinidad Jr RN83% (6)
- UroflowДокумент41 страницаUroflowSri HariОценок пока нет
- Hijamah (Cupping)Документ18 страницHijamah (Cupping)Nabeel HassanОценок пока нет
- SDJ 2020-06 Research-2Документ9 страницSDJ 2020-06 Research-2Yeraldin EspañaОценок пока нет