Академический Документы
Профессиональный Документы
Культура Документы
Chinese Medicine Gu Parasites
Загружено:
nepretip100%(2)100% нашли этот документ полезным (2 голоса)
323 просмотров8 страницgu parasites
Авторское право
© © All Rights Reserved
Доступные форматы
PDF, TXT или читайте онлайн в Scribd
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документgu parasites
Авторское право:
© All Rights Reserved
Доступные форматы
Скачайте в формате PDF, TXT или читайте онлайн в Scribd
100%(2)100% нашли этот документ полезным (2 голоса)
323 просмотров8 страницChinese Medicine Gu Parasites
Загружено:
nepretipgu parasites
Авторское право:
© All Rights Reserved
Доступные форматы
Скачайте в формате PDF, TXT или читайте онлайн в Scribd
Вы находитесь на странице: 1из 8
10
JOURNAL OF CHINESE MEDICINE NUMBER 57 MAY 1998
DRIVING OUT DEMONS AND SNAKES
A FORGOTTEN CLINICAL APPROACH
TO CHRONIC PARASITISM
by Heiner Fruehauf
A
s the field of Oriental medicine matures in a
modern environment, we are beginning to be-
come aware of the enormous dimensions that this
field encompasses. While ten years ago the Western public
still thought of Oriental medicine as a synonym for acupunc-
ture, most practitioners have now broadened their under-
standing of the term to something that includes acupuncture,
moxibustion, herbs, dietetics and qigong exercises. Although
other clinical approaches that once shaped the face of Chinese
medicine, such as Daoist psychotherapy or the application of
herbs to acupuncture points, remain forgotten, there is good
reason to believe that in time they will be unearthed and put
to use in a modern clinical context.
This presentation is an attempt to participate in the proc-
ess of 'medical archaeology' by exploring one of the sub-
merged areas of Oriental medicine, namely the complex
and variegated clinical approach to the diagnosis and treat-
ment of Gu syndrome (gu
zheng). A review of the mod-
ern research literature shows
that this topic has remained
virtually unexplored in both
China and the West
1
. Al-
though there are too many
classical references to en-
tirely ignore the phenom-
enon of Gu syndrome, mainland Chinese scholars gener-
ally dismiss it as an ancient, feudalist and superstitious
belief in demons and exorcist practices that has little or no
value in modern clinical practice. However, a close exami-
nation of the original texts illuminates the mysterious con-
cept of Gu syndrome as a valid clinical approach that may
potentially provide an answer to the many invisible de-
mons that plague patients in a modem age, namely sys-
temic funguses, parasites, viruses and other hidden patho-
gens.
Cultural and Medical Concepts of Gu
Historically, the term Gu was first introduced as a metaphor
for stagnancy, debauchery, degeneration and hidden evil.
The words gudao (the way of Gu) and wugu (shamanic Gu
practice) are mentioned in one of Chinas earliest historical
records as a reference to black magic used to kill or confuse
others, Shamanic Gu practice entails the administration of
poison to people, causing them to forget who they are
2
.
The Book of Records (Shiji), moreover reports that in 91 BCE
a Gu incident resulted in the annihilation of tens of thousands
of people. The unsuspecting victims were reportedly killed
by the black magic practice of putting spell-cast wooden
puppets into the ground close to them
3
. In this context, the
term Gu describes a situation where the attackers were in
the dark, while the victims did not know what was
happening to them. It was this original meaning - a type of
yin (hidden) evil that is doing harm to peoples mental and
physical well being - that
became the trademark of all
other Gu phenomena in
Chinese cultural history,
including the medical concept
discussed in this essay.
It is the mother matrix of
Chinese civilisation, the Yijing
(Book of Change), that pro-
vides the earliest clues for an understanding of the medical
connotations that were originally associated with the term
Gu. Hexagram eighteen is entitled Gu, here most often
translated as 'Degeneration'. It is formed by the trigram xun
(wind) below and the trigram geng (mountain) above.
Classical commentators have remarked that this particular
hexagram describes an energetic situation where a feeble
wind cannot penetrate the dense area at the mountains
base, creating a place that does not receive air and thus
becomes decayed and rotten. According to the movement
GU SYNDROME
A close examination of the original texts illuminates
the mysterious concept of Gu syndrome as a valid
clinical approach that may potentially provide an
answer to the many invisible demons that plague
patients in a modem age, namely systemic funguses,
parasites, viruses and other hidden pathogens.
11
JOURNAL OF CHINESE MEDICINE NUMBER 57 MAY 1998
oriented philosophy of the Yijing that laid the foundation of
all Daoist sciences, including Chinese medicine, movement
means life and health, stagnation means death and disease.
In the broad cultural context of the Yijing, Gu thus marks a
state of extreme stagnation where corruption and decay
have already manifested and can no longer be ignored.
Whether this occurs in society as a whole or in the micro-
cosm of the human body, the oracle advises that only
drastic (albeit thoughtful) action can turn this serious situ-
ation around. Gu, in short, is the ancient Chinese symbol for
extreme pathological yin - the dark side of life, the worst
nightmare of any human being. It represents darkness,
rottenness, slithering vermin, poisonous snakes, betrayal,
black magic, backstabbing murder and in medical terms,
progressive organ decay accompanied by torturous pain
and insanity.
The Chinese pictogram for Gu yields similar information.
Brilliantly exemplifying the multidimensional quality of
the symbolist mode of expression, the character Gu cap-
tures both the concept of decay as well as its most pertinent
cultural and medical manifestations. Since the beginning of
Chinese writing approximately 3,500 years ago, it has por-
trayed either two or three worms squirming in a vessel. In
the words of a traditional commentator Gu is if a cooking
vessel remains unused for a long time and worms start to
grow in it
4
.
This symbol also reflects a bizarre yet widespread practice
of black alchemy. Many traditional medical texts define
Gu as the verminous manifestation of evil that appears
when a wide variety of toxic worms and insects are locked
into a vessel, where they naturally become each others prey.
After a period ranging from three to twelve months, only
one snake-like worm remains, which is said to contain the
vicious and toxic potential of all the others. The seed of the
Gu worm (gu chong), in a procedure of which the technical
details remain unclear but which nevertheless can be clas-
sified as an early example of biological warfare, was then
used to poison other people. The victim of these uncanny
machinations appeared to die from a chronic disease and
Gu poisoning was thus regarded as a popular way to kill
without exposing the attacker - a scenario similar to Napo-
leons sickbed death induced by small but regular doses of
arsenic, the true nature of which came to light only after the
advent of hair analysis.
As in other occult practices, the details of the production
and application of Gu poison were kept secret by the
communities that commanded them. Although primarily
designed to empower their guileful masters by appropriat-
ing the victims wealth and source energy on both a material
and a magical dimension, some practitioners apparently
used it to further their political goals. Zhang Jiao for in-
stance, the Daoist wizard and co-architect of the Yellow
Turban uprising that toppled the powerful Han dynasty
1800 years ago, is said to have been a master of Gu, the
highly destructive and disorienting effects of which have
often been confused with magic
5
.
Reminiscent of homeopathic reasoning, the ground-up
Gu worm was also renowned as one of the most effective
remedies against Gu poisoning. So widespread was the
production of Gu and anti-Gu substances that entire re-
gions in Southern China became known as commercial Gu
centres, similar to villages that base their livelihood on the
cultivation of herbs. A host of textual references indicates,
moreover, that the Gu phenomenon was deeply entrenched
in the habitual texture of Chinese everyday life. Ancient
travellers routinely carried rhino horn powder, said to
make contaminated food foam, or other anti-evil sub-
stances such as musk, realgar and garlic. The repercussions
of Gu hysteria finally reached a state of intensity that caused
the government to intervene. In 598 CE, according to the
official dynastic annals, an imperial decree was issued that
explicitly forbade the manufacture of Gu worms
6
. Although
the widespread application of this misguided alchemical
practice has since disappeared, it reportedly survives until
the present day among the mountain tribes of Southwest
China
7
.
In medical texts, the character Gu most often describes a
situation where the vessel of the human body is filled with
thriving parasite populations that eventually bring about a
state of extreme stagnation and mental and physical decay.
Chinas earliest dictionary, the Shuowen Jiezi (An Explana-
tion of Symbolic Lines and Complex Pictograms), defined
Gu as a state of abdominal worm infestation 2000 years
ago
8
. It is important however, to point out that traditional
texts always use the term Gu syndrome (gu zheng) in con-
trast to worm syndrome (chong zheng). Whether initiated by
man-made Gu poisoning or by natural infection, a parasitic
situation labelled as Gu syndrome traditionally warrants
the presence of particularly vicious parasites, or a superin-
fection of many different kinds of parasites that combine
their toxic potential to gradually putrefy the patients body
and mind. From a modern perspective this definition of Gu
Hexagram 18: Gu/Degeneration
Ancient pictograms for Gu: worms in a pot
12
JOURNAL OF CHINESE MEDICINE NUMBER 57 MAY 1998
syndrome points to aggressive helminthic, protozoan, fun-
gal, spirochete or viral afflictions that have become sys-
temic in an immune-compromised patient. In ancient China,
schistosomiasis and chronic entamoeba infections may have
been the most common manifestations of Gu syndrome.
Physical and Mental Signs of Gu Syndrome
Traditional medical sources present varying accounts of the
aetiology and pathogenesis of Gu syndrome, but they all
agree on the devastating nature of the disorder, Gu ranks
second only to the viciousness of wild beasts when it comes
to harmful natural influences; although Gu unfolds its
harmful nature only long after the initial encounter, it kills
people just the same
9
.
Here are some of the clinical characteristics that are
frequently highlighted in the traditional Gu literature: i. Gu
pathogens are malicious and have life-threatening conse-
quences; ii. Gu pathogens primarily enter the body through
food; iii. Gu pathogens represent a type of toxin (gu du). This
makes reference to their virulent epidemic quality, but also
to the only recently corroborated fact that the metabolic by-
products of parasitic organisms have a toxic affect on the
body. Starting with the 7th century medical handbook,
Zhubing Yuanhou Lun (A Discussion of the Origins and
Symptomatology of All Disease), classical texts have stated
early on that Gu can transform itself into harmful toxins
10
;
iv. Gu pathogens are most likely to thrive in already defi-
cient organisms, and once established further harm the
bodys source qi; v. Gu pathogens operate in the dark. It is
often unclear when and how the pathogen was contracted,
making an accurate diagnosis extremely difficult. Due to
the multiplicity of potential symptoms moreover, most
doctors appear confused by Gu pathologies. Chinese mas-
ter physicians have continuously pointed out that Gu-
induced chronic diarrhoea, ascites, wasting syndrome,
mental symptoms, etc. must be diagnosed and treated
completely differently from the general occurrence of these
disorders. The coarse doctor treats the Gu type of diar-
rhoea just like regular diarrhoea, the Ming Dynasty ency-
clopaedia Puji Fang (Common Aid Formulas) emphasises,
and this is completely wrong
11
.
Some of the typical Gu symptoms cited in the literature
refer to the familiar picture of acute protozoan infection,
such as abdominal cramping and pain, vomiting, and the
excretion of bloody stools. Others paint the infinitely more
complex and variegated picture of systemic superinfection
by chronic parasites, funguses and viruses. There are
thousands of Gu toxins, all of which may potentially cause
different symptoms the authoritative 6th century encyclo-
paedia Beiji Qianjin Yaofang (Thousand Ducat Formulas)
explains, some of them will cause bloody stools, while
others initiate the desire to lay in a dark room; others may
bring about bouts of irregular emotions, such as depression
that alternates with periods of sudden happiness; others
again cause the extremities to feel heavy and ache all over;
and then there are myriads of other symptoms that we do
not have the space here to list in their entirety
12
.
Although it is one of the defining trademarks of Gu
syndrome as well as my own clinical experience that chronic
parasitism may involve virtually any symptom in virtually
any combination, for diagnostic purposes the indications
most consistently quoted in traditional texts can be
synopsised in the following way.
Digestive symptoms
Chronic diarrhoea, loose stools or alternating diarrhoea
and constipation; explosive bowel movements; abdominal
bloating or ascites; abdominal cramping and/or pain; nau-
sea; intestinal bleeding and/or pus; poor appetite or raven-
ous appetite, peculiar food cravings.
Neuromuscular symptoms
Muscle soreness, muscle heaviness, muscle weakness; wan-
dering body pains; physical heat sensations; cold night
sweats; aversion to bright light.
Mental symptoms
Depression, frequent suicidal thoughts; flaring anger, fits of
rage; unpredictable onset of strong yet volatile emotions;
inner restlessness, insomnia; general sense of muddledness
and confusion, chaotic thought patterns; visual and/or
auditory hallucinations; epileptic seizures; sensation of
feeling possessed.
Constitutional signs
Progressing state of mental and physical exhaustion, indi-
cations of source qi damage; dark circles underneath the
eyes; mystery symptoms that evade clear diagnosis; history
of acute protozoan infection; history of travel to tropical
regions; floating and big pulse or congested (choppy) pulse;
stagnation in sublingual veins; rooted damp tongue coat-
ing; red tongue tip or red parasite dots* on top of the
tongue.
Among this wide range of signs and symptoms, it is the
distinct presence of mental symptoms that (usually in com-
bination with digestive problems) is the most consistently
quoted element of Gu Syndrome. The Chunqiu Zuozhuan
(Spring and Autumn Annals), one of the earliest extant
Chinese texts, relates the story of an erotomanic marquis
who acted as if suffering from Gu disease when coming
close to the female quarters of his estate, and concludes that
Gu is a disease which catapults a persons mind and will
power into a state of chaos
13
. A later commentator points
out that the Chinese character for worm or parasite is
actually an integral building block in the pictogram feng
*Parasite dots (chong ban) are little red dots that generally cluster on
the front third of the tongue (shining through a greasy tongue coating),
sometimes extending to the middle. They are often said to be indicative
of worms and other parasites (especially when observed in children).
They are a sign of localised heat amidst the dampness, an energetic
environment that, while different from damp-heat, is typical for most
parasitic disorders.
13
JOURNAL OF CHINESE MEDICINE NUMBER 57 MAY 1998
(crazy)
14
. The Qing Dynasty publication Zhigu Xinfang (New
Approaches to Gu Therapy) even dedicated a whole chap-
ter to the mental ramifications of Gu syndrome
15
.
The distinct association of mental symptoms with sys-
temic parasitism is highly informative from both an anthro-
pological and a medical perspective. In most texts gu zheng
can be translated as demon syndrome equally as well as it
can be rendered as parasite syndrome. Traditional physi-
cians recognised that patients who acted possessed often
needed to be exorcised with
the application of demon
expelling substances such as
garlic and other herbs, most
of which have anti-parasitic
effects. This view represents
a highly advanced medical
insight into the complex way
in which parasites interface
with our hormonal system.
Modern medicine has long
rejected a connection between parasitic affliction and psy-
chopathology, and has only recently begun to acknowledge
that a) psychiatric disorders are more prevalent in less
developed countries where parasitic loads are more en-
demic; b) individual patients afflicted by parasites are more
likely to exhibit changes in mental status; and c) there is
generally an improvement in psychiatric patients follow-
ing parasite treatment
16
.
The Treatment of Gu Syndrome:
A Forgotten Approach
A multiplicity of therapeutic approaches has been sug-
gested in the traditional Gu literature. Some of them are
mantras and magical charms that reveal the influence of
Daoist medicine, but most of them are herbal formulas. In
the absence of modern clinical trials on systemic parasite
infections I found it extremely useful to examine both the
theoretical and practical aspects of these time honoured
approaches.
Master Ranxi (Ranxi Daoren), a Qing Dynasty Daoist
healer who specialised in the treatment of Gu syndrome,
pointed out that chronic parasite infections are very resil-
ient and hard to resolve thoroughly. Gu toxins that have
entered the core of a persons being can be compared to oil
seeping into flour - it is everywhere and cannot be separated
out
17
. He notes that although this disorder is serious and
affects the patient on all levels of existence, he or she may
well live with this situation forever without necessarily
dying from it. He compares the situation to a tree that hosts
birds and insects in various parts of its structure.
Depending on the general health of the tree, this condi-
tion may not necessarily cause the demise of the whole
organism. Traditional approaches, therefore, have always
taken into consideration the state of the patients source
(yuan) qi. Patients who have only recently contracted Gu
poison and are still strong can theoretically be treated with
purgatives, emetics, or other excess-removing methods.
The already weakened systemic type, however, most often
encountered in a Western context in the form of patients
suffering from chronic fungal, protozoan and/or viral dis-
eases, must be treated with a combination of anti-Gu medi-
cations and a special selection of tonics that boost the bodys
source qi. These tonics should serve the double purpose of
strengthening the patients defences while exhibiting an
anti-parasitic effect at the same time. Traditional Gu spe-
cialists agree that regular ton-
ics, especially ginseng,
should never be used, for
they enhance the life force
and activity of the Gu spir-
its. Some texts even regard a
persons violent reaction to
ginseng as one of the main
diagnostic features of the dis-
ease.
Many of the suggested for-
mulas follow up on the Yijing guideline that severe stagna-
tion must be shaken into action with bold measures, specifi-
cally by including toxic materials such as Xiong Huang
(Realgar), Fu Zi (Radix Aconiti Carmichaeli Praeparatae),
Liu Huang (Sulphur), Ba Dou (Semen Croton Tiglii) and
Wu Gong (Scolopendra Subspinipes). Other methods,
though not toxic, are just as impractical for use in a modern
Western setting, such as the oral administration of cart
wheel grease or ground up worms that have escaped from
the orifices of a freshly deceased person. Many formulas,
however, consist of herbs that are easily obtained in the West
and safe for long-term use.
A survey of the traditional literature yields the following
categories and representative herbs that are typically utilised
in Gu therapy.
1. Disperse Gu toxins (with diaphoretic herbs) (san du)
Zi Su Ye (Folium Perillae Frutescentis), Bo He (Herba
Menthae), Bai Zhi (Radix Angelicae), Lian Qiao (Fructus
Forsythiae Suspensae), Gao Ben (Rhizoma et Radix Ligustici
Sinensis), Sheng Ma (Rhizoma Cimicifugae) and Ju Hua
(Flos Chrysanthemi Morifolii).
This is the most crucial category in traditional Gu treat-
ment. In my opinion it is also the one that can potentially
benefit modern practitioners the most, since contemporary
approaches to parasites are generally devoid of this ele-
ment. Perilla (both leaf and seed - Zi Su Ye and Su Zi), Bo He
and Bai Zhi particularly are extremely visible in traditional
Gu formulas. Their sweat-inducing properties are much
weaker than standard diaphoretics like Ma Huang (Herba
Ephedrae) or Gui Zhi (Ramulus Cinnamomi Cassiae), and
they are imbued with a strong fragrance - a penetrating
yang energy that, like a diffusive light, is able to permeate
the darkest crevasses of the body where the Gu pathogens
hide out. For the same reason, acupressure with mint oil
was often recommended. Traditional Gu specialists hon-
Gu syndrome traditionally warrants the presence of
particularly vicious parasites, or a superinfection of
many different kinds of parasites that combine their
toxic potential to gradually putrefy the patients body
and mind. From a modern perspective this definition
of Gu syndrome points to aggressive helminthic, pro-
tozoan, fungal, spirochete or viral afflictions that have
become systemic in an immune-compromised patient.
14
JOURNAL OF CHINESE MEDICINE NUMBER 57 MAY 1998
oured this saturating effect by creating a new medicinal
category for this trio of herbs, namely open the exterior
with snake killing herbs (shashe fabiao).
2. Kill parasites (sha chong) and expel demons (qu gui)
Da Suan (Bulbus Alli Sativi), Yu Jin (Tuber Curcumae), Ku
Shen (Radix Sophorae Flavescentis), Huai Hua (Flos
Sophorae Japonicae Immaturus), She Chuang Zi (Fructus
Cnidii Monnieri), Jin Yin Hua (Flos Lonicerae Japonicae),
Qing Hao (Herba Artemisiae Apiaceae), Shi Chang Pu
(Rhizoma Acori Graminei), Ding Xiang (Flos Caryophylli),
He Zi (Fructus Terminaliae Chebulae), Lei Wan (Sclerotium
Omphaliae Lapidescens), Bing Lang (Semen Arecae Cat-
echu), Ku Gua (Momordica Charantia) and Chuan Shan Jia
(Squama Manitis Pentadactylae). Raw garlic (Da Suan), in
particular the single-clove purple garlic from Sichuan, is
often recommended as the most effective single remedy for
Gu syndrome. Peasants and travellers in modern China still
tend to consume a daily dose of raw garlic to ward of
intestinal distress. External treatment of Gu syndrome of-
ten involved the stimulation of all or some of the bodys
thirteen demon points (gui xie) by burning moxa on garlic
slivers. It is interesting to note that garlic was also consid-
ered to be the primary anti-evil medication in most Western
traditions. Many of us may remember scenes from movies
or novels where the terrified victim clutches a supply of
garlic to ward off approaching vampires.
3. Calm the spirit (by nourishing the qi and yin of the Lung and
Heart) (an shen)
Huang Jing (Rhizome Polygonati), Bai He (Bulbus Lilii), Bei
Sha Shen (Radix Glehniae Littoralis), Xuan Shen (Radix
Scrophulariae Ningpoensis), Sheng Di Huang (Radix
Rehmanniae Glutinosae), Xi Yang Shen (Radix Panacis
Quinquefolii), Fu Shen (Poriae Cocos Pararadicis Sclero-
tium) and Jiang Xiang (Lignum Dalbergiae Odoriferae).
Key elements in this category are Huang Jing and Bai He;
the former being affectionately revered as the Essence of the
Earth by traditional immortality seekers and Daoist practi-
tioners of external alchemy such as Hua Tuo, who regarded
it as both an energy tonic with a calming influence on
meditation and as an anti-parasitic herb; the other featuring
prominently in the defining primer for complex diseases,
the second century Jingui Yaolue (Essentials from the Golden
Cabinet), as the only effective herb for lily disease, i.e. a
certain type of hysteria/anxiety syndrome.
4. Tonify qi and blood (with pungent/detoxifying substances) (bu
qixue)
Dang Gui (Radix Angelicae Sinensis), Bai Shao (Radix
Paeoniae Lactiflorae), He Shou Wu (Radix Polygoni
Multiflori), Gan Cao (Radix Glycyrrhizae Uralensis), Huang
Qi (Radix Astragali) and Wu Jia Pi (Cortex Acanthopanacis
Radicis). Here, the pungent Dang Gui and the detoxifying
Gan Cao feature prominently. He Shou Wu is best left out
in cases with prominent diarrhoea.
5. Move qi and blood (with anti-parasitic herbs) (xingqi poju)
Chuan Xiong (Radix Ligustici Wallichii), Chai Hu (Radix
Bupleuri), E Zhu (Rhizoma Curcumae Zedoariae), San Leng
(Rhizoma Sparganii), Chen Pi (Pericarpium Citri
Reticulatae), Mu Xiang (Radix Saussureae seu Vladimirae),
Ze Lan (Herba Lycopi Lucidi) and San Qi (Radix
Notoginseng). While again displaying anti-parasitic quali-
ties, these herbs are crucial for symptom relief such as
bloating, swelling and pain. Furthermore, they address the
stagnation caused by internal scar formation and the ha-
bitual encystment of parasitic organisms, especially
protozoans.
A comprehensive formula that synthesises this multi-level
approach and, due to its available and non-toxic ingredi-
ents, holds particular promise in a modern clinical setting,
is Su He Tang (Perilla and Mentha Decoction) and its
modification Jia Jian Su He Tang (Modified Perilla and
Mentha Decoction) [for both prescriptions see Appendix 1]
recorded in Zhigu Xinfang (New Approaches to Gu
Therapy)
18
. This Qing Dynasty work also makes a number
of useful dietary recommendations [see Appendix 3] which
include the modern insight that the consumption of sugar,
fruit and other sweet foods boosts the development of yeast
and other types of parasitic organisms and should therefore
be avoided. It should be emphasised that, similar to the
necessary practice of food rotation in digestively compro-
mised patients, Su He Tang or similar prescriptions are best
modified every one to six weeks, depending on the patients
degree of sensitivity. Based on my personal clinical experi-
ence I recommend using the Gu herb categorisation out-
lined above as a standard outline. Typically, it is best to
always include at least two herbs from each category, and
to change at least one of them when the prescription is
modified.
Gu Syndrome in Modern Clinical Practice
Transported into a modern clinical setting, this highly
refined yet forgotten type of Gu therapy has the potential to
become a valid approach to a wide variety of disorders.
Many Oriental medicine practitioners are commonly con-
fronted with mystery patients who suffer from a multi-
plicity of mental and physical symptoms that cannot be
clearly diagnosed either by allopathic medicine or standard
TCM. Many of these patients have tentatively been labelled
with dont know what to call it epithets, such as chronic
fatigue syndrome, fibromyalgia, Epstein-Barr syndrome,
leaky gut syndrome, lyme disease, and, in certain cases,
lupus and multiple sclerosis.
Similarly to the traditional Gu approach, many modern
researchers have claimed that this type of patient is in most
cases afflicted by systemic fungal infection (primarily can-
didiasis), systemic parasite infection, chronic viral infection
or a combination thereof. Modern treatments for systemic
fungal, parasite or viral affliction, however, do not have the
benefit of being designed against a backdrop of 2500 years
15
JOURNAL OF CHINESE MEDICINE NUMBER 57 MAY 1998
of clinical experience. Western therapies for these disorders
(and this tends to be true for both allopathic and alternative
medications) are generally based on the simplistic assump-
tion that parasitic micro-organisms represent a type of
excess that needs to be killed off. Drugs like Flagyl, Nystatin
and Diflukin, as well as alternative products based on
grapefruit seed extract, walnut skin extract, capryllic acid
and the like, may improve the situation temporarily but are
generally abrasive and thus cannot be tolerated by the
patients weakened constitution over long periods of time.
Another potential problem with the military approach is
that it may actually be partially responsible for the occur-
rence of Gu syndrome in modem times. Gu, by definition,
is not a regular parasitic infection, but a condition that
weakens the entire organism by having become systemic in
nature. Recent research has documented that strong anti-
parasitic drugs, although at first successful in eliminating
the bulk of invaders from the digestive tract, can force
yeasts and protozoan organisms to become systemic and
wreak havoc in the bodys more internal organ tissues
19
.
In this context, two elements of the ancient Gu approach
are most instructive for us. One is the early Chinese realisa-
tion that systemic conditions are like oil that has seeped
into flour and thus require a complex therapeutic regimen
that continues for months or even years. Modern research
is beginning to confirm that entrenched parasites form a
complex symbiotic bond with all aspects of our system, and
are generally keyed into vital pathways of our immunologi-
cal and hormonal response networks
20
. To undo this criti-
cally balanced equilibrium between maximum parasite
success and continuing host survival is difficult, because
the two systems move as one. Some of our food cravings, for
example, may actually reflect the nutritional needs of our
parasitic hitchhikers.
The other realisation is the truly holistic insight that
chronic parasitism always involves a combination of defi-
ciency and excess. This basic premise is stated in all Gu
texts, including the Jueyin Chapter of the Shanghan Lun
(Treatise on Disorders Caused by Cold). Chinese physi-
cians recognised early on that once a patient progresses
beyond the point of acute infection, excess-removing
modalities such as purging usually leave residual patho-
gens behind. If the light of the bodys own life force was
restored, however, it would necessarily reach the point of
effervescent vigilance again and be able to thoroughly drive
all murky organisms from their shady hideouts. Recent
research has fully corroborated the assumption that the
likelihood and severity of parasite affliction is directly
proportionate to the strength or weakness of our immune
system
21
.
At the same time, ancient doctors noticed that standard
energy tonics like Gui Pi Tang (Restore the Spleen Decoc-
tion) or Bu Zhong Yi Qi Tang (Tonify the Middle and
Augment the Qi Decoction) tend to aggravate symptoms
such as bloating or restlessness. The traditional Gu ap-
proach, therefore, is the result of a carefully crafted pro-
gram that utilises i. blood movers such Chuan Shan Jia
(Squama Manitis Pentadactylae) to push through barriers
of accumulated phlegm and blood, exposing the parasites
and making them vulnerable for attack
19
; ii. aromatic anti-
parasitic herbs that create an uninviting milieu for the
invaders; and finally iii. tonic substances that stimulate the
bodys own scavengers which feed on foreign organisms.
For each category, moreover, the Gu therapists encouraged
the use of herbs that were also anti-parasitic in one way or
another. Carefully orchestrated, Jia Jian Su He Tang and
other Gu formulas are thus able to address the difficult
condition of systemic parasitism or chronic viral syndrome
in its full complexity, and generally tend to be more effec-
tive than most monodirectional approaches known to date.
During the last four years, I have prescribed variations of
Su He Tang and especially Jia Jian Su He Tang to approxi-
mately 150 patients who either have been diagnosed with
chronic conditions of entamoeba histolytica, giardia,
blastocystis hominis, candida albicans and other parasitic
organisms, or who simply suffer from a multiplicity of
mental and physical symptoms that cannot be explained by
standard medical parameters. I can say without hesitation
that the clinical results obtained in these cases are promis-
ing. I can also say that elements of the Gu approach have
proven to be an inspiration for my therapy of other types of
difficult and recalcitrant diseases such as diverticulosis,
ulcerative colitis, cancer and AIDS. The frequent use of
strange ingredients like Huang Jing (Rhizome Polygonati),
Ku Shen (Radix Sophorae Flavescentis) and She Chuang Zi
(Fructus Cnidii Monnieri) has since become a trademark of
my herbal practice. It is my sincere hope that the wisdom of
the traditional Gu approach can also become inspiring for
other practitioners who specialise in the treatment of knotty
diseases.
Appendix 1: Herbal Prescriptions for
Gu Syndrome
1. Su He Tang (Perilla and Mentha Decoction)
Source: Lu Shunde, Zhi Gu Xinfang (New Methods for the
Treatment of Gu Syndrome), Qing Dynasty.
Indications: treats all types of Gu syndrome including vari-
ous expressions of snake Gu and emaciation Gu, and Gu-
related disorders involving bloating, swelling, madness,
depression and epilepsy. Secondary symptoms include
'flu-like symptoms, coughing or other signs of qi
counterflow, or a tight abdominal wall. Generally it can be
said that this decoction is designed for Gu syndrome in-
volving the internal sweltering of excess fire (important
signs: dark urine, patient usually gets worse after ingesting
tonics).
Ingredients and Administration
Bo He (Herba Menthae) 30g
Zi Su Ye (Folium Perillae Frutescentis) 30g
Tiao Shen/ Bei Sha Shen (Radix Glehniae Littoralis) 24g
16
JOURNAL OF CHINESE MEDICINE NUMBER 57 MAY 1998
Lian Qiao (Fructus Forsythiae Suspensae) 24g
Huang Qi (Radix Astragali) 21g
Dang Gui (Radix Angelicae Sinensis) 30g
Sheng He Shou Wu (Unprocessed Radix Polygoni Multiflori) 30g
Bai Zhi (Radix Angelicae) 30g
Chuan Xiong (Radix Ligustici Wallichii) 15g
Jue Ming Zi (Semen Cassiae Torae) 15g
Huai Hua (Flos Sophorae Japonicae Immaturus) 30g
Bai Shao (Radix Paeoniae Lactiflorae) 15g
Chai Hu (Radix Bupleuri) 18g
Qing Hao (Herba Artemisiae Apiaceae) 30g
Sheng Yuanban/Sheng Di Huang (Radix Rehmanniae
Glutinosae) 24g
Decoct in water. If San Qi (Radix Notoginseng) 6g is added,
the results will be enhanced. It is important to gradually
work up to the full daily amount over a period of 5-6 doses,
since otherwise the internal toxin might flare up and cause
restlessness, distress, vomiting or diarrhoea in the patient.
Traditional notes: The original annotation to the formula
includes the traditional euphemism that it works 100 out
of 100 times when used for patients that suffer from a
combination of chronic mental and digestive symptoms,
provided that Gu toxins are at the root of them. Other
instructions emphasise that the formula needs to be admin-
istered in unusually high amounts to be fully effective, but
that the patient should work him/herself up to the listed
amount only gradually (while such unusually high amounts
may have been commendable for a schistosomiasis patient,
much less will suffice in a modern Western setting; I usually
prescribe about 50 to 120g of crude herbs or the equivalent
thereof in herbal granules per day). Treatment should be
sustained over a period of 3-9 months, during which it
should be modified at regular intervals, although it may be
interrupted by brief intermissions. For a person with a
constitutional Spleen/Stomach cold condition who has
contracted Gu for the second or third time, or for someone
who has taken Su He Tang for a long time and has already
cleared all of the Gu poison, the use of Su He Tang is
contraindicated. In this case, materials that warm the centre
and move qi must be prescribed. For constitutionally weak
people, Jia Jian Su He Tang or a combination of Su He Tang
and Jia Jian Su He Tang is recommended.
2. Jia Jian Su He Tang (Modified Perilla and Mentha
Decoction)
Indications: Suitable for all kinds of Gu disorders provided
that the patients blood and qi are fragile and cannot tolerate
cold materials like Sheng Di Huang (Radix Rehmanniae
Glutinosae), Xuan Shen (Radix Scrophulariae Ningpoensis),
Huang Bai (Cortex Phellodendri), Lian Qiao (Fructus
Forsythiae Suspensae), Huai Hua (Flos Sophorae Japonicae
Immaturus), Qing Hao (Herba Artemisiae Apiaceae), Bai
Shao (Radix Paeoniae Lactiflorae), Chai Hu (Radix Bupleuri)
etc., or hot materials like Rou Gui (Cortex Cinnamomi
Cassiae) or Fu Zi (Radix Aconiti Carmichaeli Praeparatae).
Ingredients and Administration:
Zi Su Ye (Folium Perillae Frutescentis) 15g
Bo He (Herba Menthae) 15g
Dang Gui (Radix Angelicae Sinensis) 21g
Chuan Xiong (Radix Ligustici Wallichii) 15g
Gan Cao (Radix Glycyrrhizae Uralensis) 15g
Ze Lan (Herba Lycopi Lucidi) 6g
Bai Zhi (Radix Angelicae) 15g
He Shou Wu (Radix Polygoni Multiflori) 15g
Huang Qi (Radix Astragali) 15g
Bai He (Bulbus Lilii) 15g
Chen Pi (Pericarpium Citri Reticulatae) 6g
San Leng (Rhizoma Sparganii) 6g
E Zhu (Rhizoma Curcumae Zedoariae) 6g
Yu Jin (Tuber Curcumae) 3g
Mu Xiang (Radix Saussureae seu Vladimirae) 3g
Ding Xiang (Flos Caryophylli) 3g
Wu Jia Pi (Cortex Acanthopanacis Radicis) 15g.
Add 3 slices of Sheng Jiang (Rhizoma Zingiberis Officinalis
Recens).
If patient becomes constipated after taking Jia Jian Su He
Tang, switch to Su He Tang.
Appendix 2: Acupuncture/moxibustion
Instructions for Gu Syndrome
Source: Qugu Ranxi Lu (Master Ranxis Treatise on Expelling
Gu Toxins), 1893.
apply vigorous garlic moxibustion to Gaohuangshu
BL-43
apply moxibustion to Feishu BL-13, Zusanli ST-36 and
Guikuxie (Demon Wailing Point)*.
also highly recommended is frequent acupressure with
menthol preparations, especially on the Thirteen Demon
(or Ghost) Points (shisan guixie); it is also possible to selec-
tively needle the Thirteen Demon Points:
Guigong (Demon Palace): Renzhong DU-26
Guixin (Demon Evidence) Shaoshang LU-11
Guilei (Demon Pile) Yinbai SP-1
Guixin (Demon Centre) Daling P-7
Guilu (Demon Path) Shenmai BL-62
Guizhen (Demon Pillow) Fengfu DU-16
*This point is not listed in modern Chinese texts. It first appeared in
Sun Simiaos Thousand Ducat Formulas in the chapter on epilepsy
along with the 13 Ghost or Demon points, and was ascribed the
name Guikuxie (Demon Wailing Point) in the 16th century primer
Entering Medicine. Descriptions of its location are not exact. It is said
that the thumbs should be tied together so that the nails face each
other and that the point is found at the crease between the nails
half on the nail and half on the flesh. One opinion is that it is
located at the mid level of the thumb nails just distal to Shaoshang
LU-11. Another is that it corresponds to Shaoshang LU-11 when
this point is used for mental disturbance and treated by
moxibustion with the thumbs facing each other so one cone treats
both thumbs. One source says of this point If moxibusted, the
demon will come forth wailing, revealing its name.
17
JOURNAL OF CHINESE MEDICINE NUMBER 57 MAY 1998
Guichuang (Demon Bed) Jiache ST-6
Guishi (Demon Market) Chengqiang REN-24
Guiku (Demon Hole) Laogong P-8
Guitang (Demon Hall) Shangxing DU-23
Guicang (Demon Hideout) Huiyin REN-1 in males;
extra point Yumen (head of the clitoris) in females
Guitui (Demon Leg) Quchi L.I.-11
Guifeng (Demon Envelope) extra point Haiquan (under
tongue)
Appendix 3: Dietary Instructions for
Gu Syndrome
Source: Zhigu Xinfang (New Approaches to Gu Therapy),
1823.
Avoid (during or after the Gu treatment): chicken, duck, fish,
shrimp, snails, gecko, snakes, insects of all kinds. Also food
items that easily breed worms should be avoided, espe-
cially all forms of sugar, honey, jujube dates and other sweet
substances.
Consume in increased amounts: tofu, celery, cabbage, spinach,
lotus root, shiso (perilla) leaves, peppermint, garlic, horse-
radish, ginger, bitter melon, black muer fungus, lychee,
longan, oranges, tangerines, grapefruit, plums, pomegran-
ates, watermelon, vinegar, green tea, lamb and pork. How-
ever, if any of these items should aggravate the condition,
it should also be avoided.
Appendix 4: Qigong Exercise
for Gu Syndrome
Name and Source: Yangsheng Fang Daoyin Fa (Energy Guid-
ing Method to Nourish Life), in Zhubing Yuanhou Lun
(Discussion on the Origins and Symptomatology of All
Disease), early 7th century.
Instructions: Find a comfortable position, either sitting up or
lying down. Place your internal focus on the abdomen,
feeling it expand as you breathe in and collapse as you
breathe out. Keep swallowing the saliva that accumulates
in your mouth, imagining that it is thunder and lightning
that permeate every corner of the abdomen. Gu is a yin
pathogen, hidden and stagnant, and it takes a constant
inundation with yang energy to drive it out. Thunder and
lightning represent the most yang phenomena in nature.
References
1 With the exception of an academic study by Paul Unschuld that
examines some of the historical and cultural, but not the clinical
ramifications of Gu. See Paul Unschuld, Medicine in China: A
History of Ideas, University of California Press, 1988.
2 Chunqiu Zuo Zhuan Zhu Shu (A Detailed Annotation of the
Spring and Autumn Annals), in Shisan Jing Zhu Shu (A Detailed
Annotation of the Thirteen Classics), Zhonghua Shuju, Beijing
1982, vol.2, p.1781.
3 Quoted in Qi Hao, Yi, wu yu qigong (Medicine, Shamanism and
Qigong), Renmin Tiyu, Beijing 1990, p.110.
4 Su Shi Yi Zhuan (Master Sus Yijing Commentary), quoted in
Qugu Ranxi Lu (Master Ranxis Treatise On Expelling Gu
Toxins), in Miben Yixue Congshu (Compendium of Secret
Medical Texts), vol.1, Shanghai Shudian, Shanghai 1988, p.3.
5 Qugu Ranxi Lu, p.1
6 Beishi: Sui Benji (Histories of the Northern Kingdoms: The Sui),
vol.1/11, quoted in ibid., p.9.
7 See the anthropologist Ma Xueliangs report on the customs of
the Miao people, a shamanic matriarchal society residing at the
shores of Lake Luogu in Yunnan: Guozu de zhaohun yu
fanggu (Spirit Seances and Gu Poisoning Practised by the Luo
People), in Yunnan Yizu Lisu Yanjiu Wenji (A Collection of
Research Articles on the Customs and Rituals of the Yi Tribes),
Chengdu, Sichuan Renmin, 1983.
8 Duan Yuzai, ea., Shuowen Jiezi Zhu (An Annotated Text of the
Explanation of Symbolic Lines and Complex Pictograms),
Shanghai Guji, Shanghai 1995, p.676.
9 Qugu Ranxi Lu, p.4.
10 Ding Guangdi, ed., Zhubing Yuanhou Lun Jiao Zhu (An Edited
and Annotated Text of the Discussion On the Origins and
Symptomatology of All Disease), Renmin Weisheng, Beijing
1992, vol.1, p.723.
11 Puji Fang (Common Aid Formulas), Shanghai Guji, Shanghai
1991, vol.5, p. 359.
12 Sun Simiao, Qianjin Fang (Thousand Ducat Formulas), Jilin
Renmin, Jilin 1994, vol.2, p.808.
13 Chunqiu Zuo Zhuan Zhu Shu, in Shisan Jing Zhu Shu, vol.2,
p.1874.
14 Qugu Ranxi Lu, p.3.
15 Zhigu Xinfang (New Approaches to Gu Therapy), chapter Dian
Kuang Gu Lun (Depression and Craziness as Manifestations
of Gu Syndrome), in Lidai Zhongyi Zhenben Jicheng (A Collection
of Precious Historical Texts in Chinese Medicine), vol.23, p.15.
16 See J. Pachman and S.A. Belanger, Parasitic Infections and
Psychopathology: A Preliminary Hypothesis, Journal of
Biosocial Sciences, 4/1994, pp.179-184; and N.H. Mohamed et.al.,
Parasitic Infections Associated With Mental Retardation in
Egypt, Journal of the Egyptian Society for Parasitology, 8/1991,
pp.319-331.
17 Qugu Ranxi Lu, p.25.
18 Zhigu Xinfang, p.4.
19 See Thomas J. Brooks, The Essentials of Medical Parasitology,
publisher and date unknown.
20 See, for instance, N.E. Beckage, Endocrine and Neuro-
endocrine Host-Parasite Relationships, Receptor, Fall 1993,
pp.233-245; G.F. Mitchell, Co-Evolution of Parasites and
Adaptive Immune responses, Immunology Today, 3/1991,
pp.A2-A5; and Felipe Kierszenbaum, ed., Parasitic Infections
and the Immune System, Academic Press, 1994.
21 See, for instance, P. Scott and G. Trinchieri, The Role of
Natural Killer Cells in Host-Parasite Interactions, Current
Opinions in Immunology, 2/1995, pp.34-40; Peter D. Walzer and
Robert M. Genta, eds., Parasitic Infections in the Compromised
Host, Marcel Dekker, 1988; and Derek Wakelin, Immunity to
Parasites: How Parasitic Infections Are Controlled, Cambridge
University Press, 1996.
Heiner Fruehauf has researched topics related to East Asian civilisation
and Chinese medicine for 17 years. He has studied at the Universities
of Tubingen, Fudan, Hamburg, Chicago and Waseda, and holds a
Ph.D. from the Dept. of East Asian Languages and Civilisation at the
University of Chicago and a post-doctoral degree from Chengdu
College of TCM. He has published widely in the fields of Chinese and
Japanese culture and Chinese medicine.
Вам также может понравиться
- Secrets of the Hidden Vessels: Explains how Chinese acupuncture works in terms Western readers can understandОт EverandSecrets of the Hidden Vessels: Explains how Chinese acupuncture works in terms Western readers can understandРейтинг: 5 из 5 звезд5/5 (1)
- Gu SyndromДокумент3 страницыGu SyndromAlvaro ToledoОценок пока нет
- Acupuncture Today and in Ancient China: Explains How Chinese Acupuncture Works in Terms Western Readers Can UnderstandОт EverandAcupuncture Today and in Ancient China: Explains How Chinese Acupuncture Works in Terms Western Readers Can UnderstandОценок пока нет
- Syndrome: An In-Depth Interview With Heiner FruehaufДокумент11 страницSyndrome: An In-Depth Interview With Heiner Fruehaufrashax100% (1)
- Six Strands of the Web: An In-Depth Study of the Six Stages of Disease in Traditional Chinese MedicineОт EverandSix Strands of the Web: An In-Depth Study of the Six Stages of Disease in Traditional Chinese MedicineОценок пока нет
- Pearls-Cancer HerbalДокумент4 страницыPearls-Cancer HerbalDonna100% (1)
- The clinical application of Shang Han Lun: 76 fomula anaysis with case studiesОт EverandThe clinical application of Shang Han Lun: 76 fomula anaysis with case studiesРейтинг: 5 из 5 звезд5/5 (1)
- The 5 Organs Network of Chinese Medicine - IntroductionДокумент5 страницThe 5 Organs Network of Chinese Medicine - IntroductionAdam HooverОценок пока нет
- On the Theory and Practical Application of Channels and CollateralsОт EverandOn the Theory and Practical Application of Channels and CollateralsОценок пока нет
- TCM Diagnostics Applied To Parasite-Related Disease by Laraine Crampton, MATCM, L. Ac ... PDFДокумент102 страницыTCM Diagnostics Applied To Parasite-Related Disease by Laraine Crampton, MATCM, L. Ac ... PDFMaya PelinОценок пока нет
- Classic FormulasДокумент26 страницClassic Formulasgiovanna2004Оценок пока нет
- (Sabine Wilms) Nurturing Life in Classical Chinese Medicine by Sun Si MiaoДокумент9 страниц(Sabine Wilms) Nurturing Life in Classical Chinese Medicine by Sun Si MiaoAlexandre Henriques100% (1)
- The Role of The Qi Mechanism in The Treatment of Knotty DiseasesДокумент6 страницThe Role of The Qi Mechanism in The Treatment of Knotty DiseasesInfohogg100% (2)
- Formula GuaДокумент10 страницFormula GuarendaoОценок пока нет
- Z'ev Rosenberg InterviewДокумент7 страницZ'ev Rosenberg InterviewZ'ev Rosenberg100% (1)
- Important Combination Tonic Formulas - Dr. Jake Fratkin - Boulder, COДокумент4 страницыImportant Combination Tonic Formulas - Dr. Jake Fratkin - Boulder, COVera Gardasevic MitrovicОценок пока нет
- WHO Intl Standard Terminologies On TCMДокумент366 страницWHO Intl Standard Terminologies On TCManlme7899Оценок пока нет
- Chinese Herbal Dose in Ancient and Modern Times: A Comparative StudyДокумент4 страницыChinese Herbal Dose in Ancient and Modern Times: A Comparative StudyNguyễn TiếnОценок пока нет
- TCM Foundations, Extraordinary Vessels, Gynecology, Tongue DiagnosisДокумент527 страницTCM Foundations, Extraordinary Vessels, Gynecology, Tongue DiagnosisAndreas Papazachariou100% (3)
- Chang Zhang-Fu - Chinese Materia Medica (2014) PDFДокумент727 страницChang Zhang-Fu - Chinese Materia Medica (2014) PDFAntonella Ercolani100% (17)
- Herbs Visual Materia Medica - SACRED LOTUS ARTSДокумент103 страницыHerbs Visual Materia Medica - SACRED LOTUS ARTSthiagovieiracosta100% (5)
- Herb Comps Review QuizletДокумент6 страницHerb Comps Review Quizletpeter911cmОценок пока нет
- Wen Bing2 PDFДокумент9 страницWen Bing2 PDFJiayiОценок пока нет
- Introduction To Chinese Herbology: Created by Bob Damone, M.S., L.Ac. and Todd Luger, B.S., M.Ac.O.M., L.AcДокумент108 страницIntroduction To Chinese Herbology: Created by Bob Damone, M.S., L.Ac. and Todd Luger, B.S., M.Ac.O.M., L.AcnaburaОценок пока нет
- Deng2014 Tesis - Chinese Herbal Medicine For PsoriasisДокумент495 страницDeng2014 Tesis - Chinese Herbal Medicine For PsoriasisanascopelОценок пока нет
- NCCAOM Exam Review in Chinese Herbology-2015Документ9 страницNCCAOM Exam Review in Chinese Herbology-2015Edison HlmОценок пока нет
- Flavors and Nature of Herbs - Chinese MedicineДокумент7 страницFlavors and Nature of Herbs - Chinese MedicinescumsОценок пока нет
- TCM Diagnosis by AskingДокумент15 страницTCM Diagnosis by AskingGloria Aleman-GarzaОценок пока нет
- Chapter 22Документ40 страницChapter 22JiayiОценок пока нет
- AJACM 2012 7 1 Emotions & Desires Part Two - M GarveyДокумент7 страницAJACM 2012 7 1 Emotions & Desires Part Two - M GarveyRicardo TeixeiraОценок пока нет
- The Kidney Heart in CM Part 1Документ5 страницThe Kidney Heart in CM Part 1davidg2012100% (1)
- Chapter 3Документ37 страницChapter 3JiayiОценок пока нет
- Aaaom Course TextbooksДокумент2 страницыAaaom Course Textbooksferry7765Оценок пока нет
- Demystifying Traditional Herbal Medicine With Modern ApproachДокумент7 страницDemystifying Traditional Herbal Medicine With Modern ApproachOswaldo EncisoОценок пока нет
- Chapter 6Документ64 страницыChapter 6Jiayi100% (1)
- Treatise On Febrile Diseases Caused by C - Zhang ZhongjingДокумент580 страницTreatise On Febrile Diseases Caused by C - Zhang ZhongjingLiliana Ponte100% (20)
- Sun Simiao and Dietetics FinalДокумент7 страницSun Simiao and Dietetics Finalgaetanscribd100% (1)
- Jin Gui Yao Lue (Acupuncture)Документ2 страницыJin Gui Yao Lue (Acupuncture)Tim SchlankОценок пока нет
- Zang Fu IiДокумент16 страницZang Fu Iimd_corona62Оценок пока нет
- Traditional Chinese Medicine/Usage of Single Herbs: Name English Name Category UsageДокумент10 страницTraditional Chinese Medicine/Usage of Single Herbs: Name English Name Category UsageNatОценок пока нет
- TCM Cases - PainДокумент671 страницаTCM Cases - PainGeander G. Bacheti100% (5)
- Blood DeficiencyДокумент7 страницBlood Deficiencypeter911cmОценок пока нет
- Mental Disorders: by Heiner FruehaufДокумент14 страницMental Disorders: by Heiner Fruehaufitsik12886Оценок пока нет
- Nan JingДокумент300 страницNan JingPierre Chen100% (6)
- Shang Han Lun Cold DamageДокумент1 страницаShang Han Lun Cold DamageDandhi FirmansyahОценок пока нет
- EssentialFormulas (Tony Reid)Документ23 страницыEssentialFormulas (Tony Reid)Tim Schlank100% (1)
- Just The Beginning of An Ending:: Menopausal Management by Chinese Herbal MedicineДокумент36 страницJust The Beginning of An Ending:: Menopausal Management by Chinese Herbal MedicineNadja VossОценок пока нет
- The Mother of All Diseases-StagnationДокумент12 страницThe Mother of All Diseases-StagnationAndri Ferdian100% (2)
- Nutrition For Kidney YinДокумент6 страницNutrition For Kidney Yinbaskars39Оценок пока нет
- 59Документ115 страниц59James Driscoll100% (1)
- AJACM 2010 5 2 Wen Bing Xue and 2009 H1N1 - KohДокумент7 страницAJACM 2010 5 2 Wen Bing Xue and 2009 H1N1 - KohPedro MaiaОценок пока нет
- Chinese Herbology Damone Luger PDFДокумент108 страницChinese Herbology Damone Luger PDFTera100% (1)
- Sun Simiao - Recipes Worth A Thousand GoldДокумент56 страницSun Simiao - Recipes Worth A Thousand Goldnqngestion100% (3)
- Heart Shock: Diagnosis and Treatment of Trauma With Shen-Hammer and Classical Chinese Medicine - NeuropsychologyДокумент4 страницыHeart Shock: Diagnosis and Treatment of Trauma With Shen-Hammer and Classical Chinese Medicine - Neuropsychologycutyjimi0% (1)
- ASA08 S6 MazinAlKhafaji PRESДокумент22 страницыASA08 S6 MazinAlKhafaji PRESYagtaliОценок пока нет
- Ling Shu Vol 1Документ169 страницLing Shu Vol 1Paco Ladera100% (2)
- Differential DiagnosisДокумент7 страницDifferential DiagnosisCarleta Stan100% (1)
- Emotions FruehaufДокумент15 страницEmotions FruehaufRomi BrenerОценок пока нет
- (Peter Holmes) Jade Remedies A Chinese Herbal Ref (B-Ok - CC) PDFДокумент438 страниц(Peter Holmes) Jade Remedies A Chinese Herbal Ref (B-Ok - CC) PDFLM_S_S100% (6)
- A Payments-Based Cryptocurrency and Incentivization NetworkДокумент12 страницA Payments-Based Cryptocurrency and Incentivization NetworknepretipОценок пока нет
- The Bitcoin Backbone Protocol: Analysis and ApplicationsДокумент44 страницыThe Bitcoin Backbone Protocol: Analysis and ApplicationsnepretipОценок пока нет
- Bitcoins: Illegal Tender' or Currency of The Future?: Expert AnalysisДокумент3 страницыBitcoins: Illegal Tender' or Currency of The Future?: Expert AnalysisnepretipОценок пока нет
- IRS Targets BitcoinДокумент4 страницыIRS Targets BitcoinnepretipОценок пока нет
- 21.1 Alberts Final WebДокумент21 страница21.1 Alberts Final WebnepretipОценок пока нет
- Bitcoin Unlimited: Articles of FederationДокумент12 страницBitcoin Unlimited: Articles of FederationnepretipОценок пока нет
- Bitcoin: Questions, Answers, and Analysis of Legal Issues: Edward V. MurphyДокумент36 страницBitcoin: Questions, Answers, and Analysis of Legal Issues: Edward V. MurphynepretipОценок пока нет
- The Treatment of Cancer With Chinese MedicineДокумент6 страницThe Treatment of Cancer With Chinese Medicinenepretip100% (2)
- 27HarvJLTech587 PDFДокумент22 страницы27HarvJLTech587 PDFnepretipОценок пока нет
- Cryptocurrency: Technical OverviewДокумент10 страницCryptocurrency: Technical OverviewnepretipОценок пока нет
- Acupuncture HypothyroidismДокумент4 страницыAcupuncture Hypothyroidismnepretip100% (1)
- Ethics Part2 - BBColl2021Документ26 страницEthics Part2 - BBColl2021Michael MatshonaОценок пока нет
- Lam Kam Chuen - Master Lam's Walking Chi Kung PDFДокумент146 страницLam Kam Chuen - Master Lam's Walking Chi Kung PDFSergej100% (4)
- Practice Test 3Документ8 страницPractice Test 3Hồng NgọcОценок пока нет
- DLL Mathematics 6 Whole YearДокумент241 страницаDLL Mathematics 6 Whole YearHazel Jane Fabrigas - BaguioОценок пока нет
- Ammonium Nitrate ExplosivesДокумент24 страницыAmmonium Nitrate ExplosivesManh Loc PhanОценок пока нет
- Seven Ways To Identify HistoryДокумент4 страницыSeven Ways To Identify HistoryMiaClarissaОценок пока нет
- Reading and Writing NewДокумент32 страницыReading and Writing NewrashmiОценок пока нет
- Kami Export - End of Semester Assessment - Study GuideДокумент14 страницKami Export - End of Semester Assessment - Study GuideBarbz BitnickiОценок пока нет
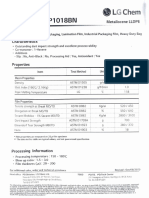
- Metaloceno Leucene HP1018BNДокумент1 страницаMetaloceno Leucene HP1018BNAngel Ramás Saint SeiyaОценок пока нет
- KPK SST PD PDFДокумент1 страницаKPK SST PD PDFArshad AliОценок пока нет
- Working Efficiently and Effectively in EngineeringДокумент8 страницWorking Efficiently and Effectively in EngineeringJordan Leah50% (2)
- Ch2 Small Scale Fading and MultipathДокумент30 страницCh2 Small Scale Fading and MultipathaqilahОценок пока нет
- Image-Based On-Line Measurement of Crepe Structure: White PaperДокумент12 страницImage-Based On-Line Measurement of Crepe Structure: White PaperAhmed AsforaОценок пока нет
- Case Wx145 165 185 Hydraulic Excavator Service ManualДокумент20 страницCase Wx145 165 185 Hydraulic Excavator Service ManualBrenda100% (49)
- Adopting and Adapting Arbitration For Climate ChangeRelated DisputesДокумент9 страницAdopting and Adapting Arbitration For Climate ChangeRelated DisputescontestantlauОценок пока нет
- Sports PsychologyДокумент26 страницSports PsychologyHabiya TauseefОценок пока нет
- Heat Capacities and Latent Heats 'O' Level 0625 2019Документ10 страницHeat Capacities and Latent Heats 'O' Level 0625 2019DanielОценок пока нет
- GulfSea Synth Gear Oil PG220Документ2 страницыGulfSea Synth Gear Oil PG220Md.Obydur RahmanОценок пока нет
- TDS Kaloty en V1.2020Документ4 страницыTDS Kaloty en V1.2020Alex Rivas RamírezОценок пока нет
- Appendix 3Документ34 страницыAppendix 3tcc.arshadОценок пока нет
- Proceeding of The 3rd Annul National Conference On Agriculture and Environmental Management For Sustainable Development From June 17-18, 2016Документ277 страницProceeding of The 3rd Annul National Conference On Agriculture and Environmental Management For Sustainable Development From June 17-18, 2016Tolasa RegasaОценок пока нет
- CV - Elchin SalimovДокумент3 страницыCV - Elchin SalimovMicRoToneОценок пока нет
- Crack-Free Growth and Transfer of Continuous Monolayer Graphene Grown On Melted CopperДокумент8 страницCrack-Free Growth and Transfer of Continuous Monolayer Graphene Grown On Melted CopperMassi MussibatОценок пока нет
- Gcse Travel Writing CourseworkДокумент4 страницыGcse Travel Writing Courseworkafiwgxldd100% (2)
- Score Booster For All Bank Prelims Exams - Day 6Документ24 страницыScore Booster For All Bank Prelims Exams - Day 6bofeniОценок пока нет
- Monitoring and ImplimentationДокумент2 страницыMonitoring and Implimentationpranav shuklaОценок пока нет
- Hardener K-12 MSDSДокумент12 страницHardener K-12 MSDSrehanОценок пока нет
- Civil Engineering Multiple Choice Questions and AnswersДокумент1 страницаCivil Engineering Multiple Choice Questions and Answersengineeringmcqs100% (7)
- Tugas Bahasa IndonesiaДокумент4 страницыTugas Bahasa IndonesiaNABIL ABDILLAHОценок пока нет
- Soal B. Inggris Kelas X Semester 2Документ5 страницSoal B. Inggris Kelas X Semester 2Aliyah Al-IhsaniyahОценок пока нет
- Summary: The Myth of Normal: Trauma, Illness, and Healing in a Toxic Culture By Gabor Maté MD & Daniel Maté: Key Takeaways, Summary & AnalysisОт EverandSummary: The Myth of Normal: Trauma, Illness, and Healing in a Toxic Culture By Gabor Maté MD & Daniel Maté: Key Takeaways, Summary & AnalysisРейтинг: 4 из 5 звезд4/5 (9)
- Uncontrolled Spread: Why COVID-19 Crushed Us and How We Can Defeat the Next PandemicОт EverandUncontrolled Spread: Why COVID-19 Crushed Us and How We Can Defeat the Next PandemicОценок пока нет
- The Wisdom of Plagues: Lessons from 25 Years of Covering PandemicsОт EverandThe Wisdom of Plagues: Lessons from 25 Years of Covering PandemicsРейтинг: 4.5 из 5 звезд4.5/5 (6)
- Profiles of the Vaccine-Injured: "A Lifetime Price to Pay"От EverandProfiles of the Vaccine-Injured: "A Lifetime Price to Pay"Рейтинг: 3.5 из 5 звезд3.5/5 (3)
- Do You Believe in Magic?: The Sense and Nonsense of Alternative MedicineОт EverandDo You Believe in Magic?: The Sense and Nonsense of Alternative MedicineОценок пока нет
- Fatal Conveniences: The Toxic Products and Harmful Habits That Are Making You Sick—and the Simple Changes That Will Save Your HealthОт EverandFatal Conveniences: The Toxic Products and Harmful Habits That Are Making You Sick—and the Simple Changes That Will Save Your HealthРейтинг: 4 из 5 звезд4/5 (7)
- The Truth about Wuhan: How I Uncovered the Biggest Lie in HistoryОт EverandThe Truth about Wuhan: How I Uncovered the Biggest Lie in HistoryРейтинг: 4 из 5 звезд4/5 (6)
- The Gut-Immune Connection: How Understanding the Connection Between Food and Immunity Can Help Us Regain Our HealthОт EverandThe Gut-Immune Connection: How Understanding the Connection Between Food and Immunity Can Help Us Regain Our HealthОценок пока нет
- The Inescapable Immune Escape PandemicОт EverandThe Inescapable Immune Escape PandemicРейтинг: 5 из 5 звезд5/5 (1)
- There Are No Accidents: The Deadly Rise of Injury and Disaster—Who Profits and Who Pays the PriceОт EverandThere Are No Accidents: The Deadly Rise of Injury and Disaster—Who Profits and Who Pays the PriceРейтинг: 4.5 из 5 звезд4.5/5 (15)
- War on Ivermectin: The Medicine that Saved Millions and Could Have Ended the PandemicОт EverandWar on Ivermectin: The Medicine that Saved Millions and Could Have Ended the PandemicРейтинг: 4 из 5 звезд4/5 (7)
- The Hair Color Mix Book: More Than 150 Recipes for Salon-Perfect Color at HomeОт EverandThe Hair Color Mix Book: More Than 150 Recipes for Salon-Perfect Color at HomeРейтинг: 3.5 из 5 звезд3.5/5 (7)
- There Are No Accidents: The Deadly Rise of Injury and Disaster—Who Profits and Who Pays the PriceОт EverandThere Are No Accidents: The Deadly Rise of Injury and Disaster—Who Profits and Who Pays the PriceРейтинг: 4.5 из 5 звезд4.5/5 (11)
- Summary: The Real Anthony Fauci: Bill Gates, Big Pharma, and the Global War on Democracy and Public Health by Robert F. Kennedy Jr: Key Takeaways, Summary & Analysis IncludedОт EverandSummary: The Real Anthony Fauci: Bill Gates, Big Pharma, and the Global War on Democracy and Public Health by Robert F. Kennedy Jr: Key Takeaways, Summary & Analysis IncludedОценок пока нет
- Epic Measures: One Doctor. Seven Billion Patients.От EverandEpic Measures: One Doctor. Seven Billion Patients.Рейтинг: 4 из 5 звезд4/5 (13)
- Mama Might Be Better Off Dead: The Failure of Health Care in Urban AmericaОт EverandMama Might Be Better Off Dead: The Failure of Health Care in Urban AmericaОценок пока нет
- Sickening: How Big Pharma Broke American Health Care and How We Can Repair ItОт EverandSickening: How Big Pharma Broke American Health Care and How We Can Repair ItРейтинг: 4 из 5 звезд4/5 (9)
- Breaking out of the Health Care Abyss: Transformational Tips for Agents of ChangeОт EverandBreaking out of the Health Care Abyss: Transformational Tips for Agents of ChangeОценок пока нет
- Healthy Buildings: How Indoor Spaces Drive Performance and ProductivityОт EverandHealthy Buildings: How Indoor Spaces Drive Performance and ProductivityРейтинг: 5 из 5 звезд5/5 (2)
- Get Well Soon: History's Worst Plagues and the Heroes Who Fought ThemОт EverandGet Well Soon: History's Worst Plagues and the Heroes Who Fought ThemРейтинг: 4 из 5 звезд4/5 (234)
- Environmental Health and Occupational Health & SafetyОт EverandEnvironmental Health and Occupational Health & SafetyРейтинг: 3.5 из 5 звезд3.5/5 (9)
- The Wuhan Cover-Up: And the Terrifying Bioweapons Arms RaceОт EverandThe Wuhan Cover-Up: And the Terrifying Bioweapons Arms RaceОценок пока нет