Академический Документы
Профессиональный Документы
Культура Документы
New England Journal Medicine: The of
Загружено:
BrilliantIbnuSinaИсходное описание:
Оригинальное название
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
New England Journal Medicine: The of
Загружено:
BrilliantIbnuSinaАвторское право:
Доступные форматы
n engl j med 363;19 nejm.
org november 4, 2010
1791
The new england
journal of medicine
established in 1812 november 4, 2010 vol. 363 no. 19
Safety of Recombinant Activated Factor VII
in Randomized Clinical Trials
Marcel Levi, M.D., Jerrold H. Levy, M.D., Henning Friis Andersen, M.Sc., and David Truloff, D.V.M.
Abstract
From the Academic Medical Center, Uni-
versity of Amsterdam, Amsterdam (M.L.);
the Emory University School of Medi-
cine, Atlanta (J.H.L.); and Novo Nordisk,
Bagsvrd, Denmark (H.F.A., D.T.). Ad-
dress reprint requests to Dr. Levi at the
Department of Medicine (F-4), Academic
Medical Center, University of Amsterdam,
Meibergdreef 9, 1105 AZ Amsterdam, the
Netherlands, or at m.m.levi@amc.uva.nl.
N Engl J Med 2010;363:1791-800.
Copyright 2010 Massachusetts Medical Society.
Background
The use of recombinant activated factor VII (rFVIIa) on an off-label basis to treat
life-threatening bleeding has been associated with a perceived increased risk of throm-
boembolic complications. However, data from placebo-controlled trials are needed
to properly assess the thromboembolic risk. To address this issue, we evaluated the
rate of thromboembolic events in all published randomized, placebo-controlled
trials of rFVIIa used on an off-label basis.
Methods
We analyzed data from 35 randomized clinical trials (26 studies involving patients
and 9 studies involving healthy volunteers) to determine the frequency of thrombo-
embolic events. The data were pooled with the use of random-effects models to cal-
culate the odds ratios and 95% confidence intervals.
Results
Among 4468 subjects (4119 patients and 349 healthy volunteers), 498 had thrombo-
embolic events (11.1%). Rates of arterial thromboembolic events among all 4468
subjects were higher among those who received rFVIIa than among those who re-
ceived placebo (5.5% vs. 3.2%, P = 0.003). Rates of venous thromboembolic events
were similar among subjects who received rFVIIa and those who received placebo
(5.3% vs. 5.7%). Among subjects who received rFVIIa, 2.9% had coronary arterial
thromboembolic events, as compared with 1.1% of those who received placebo
(P = 0.002). Rates of arterial thromboembolic events were higher among subjects
who received rFVIIa than among subjects who received placebo, particularly among
those who were 65 years of age or older (9.0% vs. 3.8%, P = 0.003); the rates were
especially high among subjects 75 years of age or older (10.8% vs. 4.1%, P = 0.02).
Conclusions
In a large and comprehensive cohort of persons in placebo-controlled trials of rFVIIa,
treatment with high doses of rFVIIa on an off-label basis significantly increased the
risk of arterial but not venous thromboembolic events, especially among the elderly.
(Funded by Novo Nordisk.)
The New England Journal of Medicine
Downloaded from nejm.org on January 8, 2011. For personal use only. No other uses without permission.
Copyright 2010 Massachusetts Medical Society. All rights reserved.
T h e new engl and journal o f medicine
n engl j med 363;19 nejm.org november 4, 2010
1792
R
ecombinant activated coagulation
factor VII (rFVIIa) (NovoSeven, Novo Nor-
disk) is approved for the treatment of bleed-
ing in patients with hemophilia A or B who have
inhibiting antibodies to coagulation factor VIII
or IX. Indications have been broadened to include
the treatment of episodes of bleeding and the
prevention of episodes of bleeding related to sur-
gical or invasive procedures in patients with con-
genital and acquired hemophilia, factor VII defi-
ciency, or Glanzmanns thrombasthenia (the last
indication is approved only in Europe).
The mechanism of action of rFVIIa may offer
the potential for its use in preventing or treating
severe or life-threatening bleeding in patients with
other clinical conditions.
1
A growing number of
case reports and small, controlled or uncontrolled
studies have shown the successful use of rFVIIa
for various clinical indications other than the
treatment of hemophilia, including management
of severe traumatic injury, control of bleeding dur-
ing surgery and transplantation, treatment of in-
tracerebral hemorrhage, and management of
bleeding due to anticoagulation therapy.
2
Many
of the patients who have received rFVIIa for these
indications have been at high risk for death be-
cause of frank hemorrhaging, which was a pre-
requisite for the clinical trials.
The primary concern surrounding the use of
rFVIIa is its potential as a hemostatic agent to in-
duce thromboembolic events. It is administered
at doses that are up to 1000 times the physiologic
level and has a half-life of approximately 2.5
hours.
3
Although rFVIIa acts by generation of
thrombin on thrombin-activated platelets and is
theoretically localized to the site of vessel-wall
injury, systemic activation of coagulation may
occur.
4
An evaluation of 483 published studies (most-
ly uncontrolled and retrospective) of the use of
rFVIIa in patients with hemophilia, liver disease,
trauma or a condition requiring surgery, antico-
agulation reversal, and coagulation disorders
showed an incidence rate of thromboembolic
events of 1 to 2%.
2
OConnell et al.
5
described
168 reports of 185 rFVIIa-associated thromboem-
bolic events in the Adverse Event Reporting Sys-
tem of the Food and Drug Administration (FDA),
involving both approved and off-label uses of
rFVIIa. In 38% of these reported cases, however,
other hemostatic agents were used concomitantly
with rFVIIa. Most of the safety data on off-label
indications are retrospective and involve subjects
with a relatively high risk of adverse events, in-
cluding thrombosis, making interpretation of
these findings difficult.
We systematically analyzed rates of thrombo-
embolic events in 35 placebo-controlled trials (in-
volving 4468 persons) of off-label indications for
rFVIIa, including various coagulopathic states,
coexisting conditions, and dosing algorithms. In
all these trials, rFVIIa was administered for the
treatment or prevention of bleeding.
Methods
Identification of Safety Data
To evaluate the profile of thromboembolic events
associated with the off-label use of rFVIIa, we used
data from two main types of clinical trials: 26 ran-
domized, placebo-controlled trials involving 4119
patients with various clinical conditions, and
9 randomized, placebo-controlled trials involv-
ing 349 healthy volunteers. These trials included
both Novo Nordisk-sponsored trials (29 trials in-
volving 4064 patients and 263 healthy volunteers)
and investigator-initiated trials (6 trials involving
55 patients and 86 healthy volunteers). The inves-
tigator-initiated trials were identified through a
Medline search of randomized clinical trials (span-
ning the period from 1996 through 2008) with
the use of the terms rFVIIa, factor VIIa, ep-
tacog alfa, activated, or NovoSeven. The data
from the investigator-initiated trials were obtained
from the published studies, through direct con-
tact with the authors of the studies, or both (for
more details, see the Supplementary Appendix,
available with the full text of this article at NEJM
.org). These randomized, controlled clinical trials
were broadly categorized according to the under-
lying diagnosis. The resultant seven major catego-
ries of bleeding were spontaneous central nervous
system bleeding and bleeding due to advanced liver
disease, trauma, cardiac surgery, traumatic brain
injury, spinal surgery, and other conditions.
The study was designed by the first author, and
the data were collected by all the authors. Data
analysis was performed by the first, second, and
last authors, and the statistical analysis was per-
formed by the third author. All authors vouch for
the data and the analysis. The first two authors
wrote the first draft of the manuscript and made
the decision to submit the manuscript for publi-
cation with the approval of all the authors.
The New England Journal of Medicine
Downloaded from nejm.org on January 8, 2011. For personal use only. No other uses without permission.
Copyright 2010 Massachusetts Medical Society. All rights reserved.
Recombinant Activated Factor VII in Clinical Trials
n engl j med 363;19 nejm.org november 4, 2010
1793
Definition of Terms
All reported adverse events that were considered
to be possibly or probably thrombotic or embolic
in nature (on the basis of the use of standardized
terms in the Medical Dictionary for Regulatory Ac-
tivities [MedDRA]) were reviewed by the industry
authors and categorized as an arterial thrombo-
embolic event, a venous thromboembolic event, or
an event that was not thromboembolic. Reports
of adverse events that used broad terms that may
have been suggestive of thromboembolic events
were reviewed. Cases in which clear evidence
showed that the event was not thrombotic in na-
ture were excluded. All thrombotic events were
confirmed by means of objective tests. Arterial
thromboembolic events were classified as coro-
nary, cerebrovascular, or other events. Coronary
events (MedDRA terms: [acute] myocardial infarc-
tion, silent myocardial infarction, unstable angina,
and increased troponin) were confirmed by means
of electrocardiographic studies, laboratory tests,
echocardiographic studies, or a combination of
these tests. Cerebrovascular events (MedDRA
terms: cerebral infarction, cerebellar infarction,
ischemic stroke, cerebrovascular accident, hemipa-
resis, lacunar infarction, thromboembolic stroke,
or ischemic cerebral infarction) were confirmed
by means of computed tomography (thereby ex-
cluding cerebral hemorrhage as a cause of the
symptoms). Other arterial thromboembolic events
(MedDRA terms: arterial thrombosis of the legs,
embolism, graft thrombosis, hepatic-artery occlu-
sion, hepatic-artery thrombosis, iliac-artery throm-
bosis, intestinal infarction, intestinal ischemia,
intracardiac thrombus, peripheral arterial occlu-
sive disease, renal-artery thrombosis, retinal-artery
embolism, splenic infarction, and vascular-graft
occlusion) were confirmed by means of vascular
imaging.
Venous thromboembolic events (MedDRA
terms: deep-vein thrombosis, graft thrombosis,
jugular-vein thrombosis, mesenteric-vein throm-
bosis, pelvic venous thrombosis, phlebitis, portal-
vein thrombosis, pulmonary embolism, renal-vein
thrombosis, retinal-vein thrombosis, shunt occlu-
sion, subclavian-vein thrombosis, thrombophle-
bitis, superficial thrombophlebitis, thrombosis,
transverse sinus thrombosis, vena cava thrombo-
sis, venous thrombosis, and venous thrombosis of
the legs) were also confirmed by means of vascu-
lar imaging.
Dose Categories
A range of rFVIIa doses was administered across
the 35 trials. The data were categorized into one
of three dose groups: less than 80 g per kilogram
of body weight (low), 80 to 120 g per kilogram
(medium), or more than 120 g per kilogram
(high). This categorization of doses was chosen
because 80 to 120 g per kilogram approximates
the 90-g-per-kilogram-dose recommended in the
prescribing information for treating episodes of
bleeding in patients with hemophilia A or B who
have inhibiting antibodies to coagulation factors
VIII or IX. In trials with crossover or multiple-dose
designs, the subject was assigned to the group ac-
cording to the highest dose received.
Statistical Analysis
The statistical analyses focused on the propor-
tion of subjects who had thromboembolic events,
arterial thromboembolic events, or venous throm-
boembolic events. The statistical analyses were
primarily performed on data collected from ran-
domized, controlled clinical trials involving pa-
tients. The data from clinical trials involving
healthy volunteers are presented separately, with
the exception of Table 1, which shows rates of
thromboembolic events among all persons in the
35 trials.
For descriptive statistics, the rate of thrombo-
embolic events was defined as the number of pa-
tients with events as a proportion of the number
of patients who received a study drug. P values,
odds ratios, and 95% confidence intervals were
calculated with the use of logistic regression and
SAS software (version 9.2), with adjustment for
the type of bleeding, age, and rFVIIa treatment.
The type of bleeding and age were included be-
cause it was known that they are both predictors
of thromboembolic events.
33-36
If a statistically
significant difference was observed between the
event rate among patients who received rFVIIa and
the rate among patients who received placebo,
additional analyses were performed according to
the type of adverse event, the type of bleeding,
and the age group. In addition, P values, model-
based odds ratios, and confidence intervals were
calculated only in subgroups in which there were
enough events (>10 events in total) for the analy-
sis to be meaningful.
The association of dose with the risk of a
thromboembolic event was also evaluated by
The New England Journal of Medicine
Downloaded from nejm.org on January 8, 2011. For personal use only. No other uses without permission.
Copyright 2010 Massachusetts Medical Society. All rights reserved.
T h e new engl and journal o f medicine
n engl j med 363;19 nejm.org november 4, 2010
1794
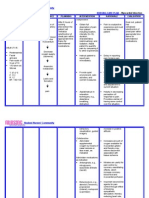
T
a
b
l
e
1
.
P
o
p
u
l
a
t
i
o
n
a
n
d
D
o
s
e
-
G
r
o
u
p
D
i
s
t
r
i
b
u
t
i
o
n
i
n
P
l
a
c
e
b
o
-
C
o
n
t
r
o
l
l
e
d
T
r
i
a
l
s
o
f
r
F
V
I
I
a
.
*
P
o
p
u
l
a
t
i
o
n
a
n
d
C
a
u
s
e
o
f
B
l
e
e
d
i
n
g
N
o
.
o
f
S
t
u
d
i
e
s
M
e
a
n
A
g
e
P
l
a
c
e
b
o
(
N
=
1
6
5
3
)
r
F
V
I
I
a
(
N
=
2
8
1
5
)
T
o
t
a
l
(
N
=
4
4
6
8
)
r
F
V
I
I
a
,
<
8
0
g
/
k
g
(
N
=
9
4
0
)
r
F
V
I
I
a
,
8
0
1
2
0
g
/
k
g
(
N
=
1
0
8
6
)
r
F
V
I
I
a
,
>
1
2
0
g
/
k
g
(
N
=
7
8
9
)
R
e
f
e
r
e
n
c
e
y
r
n
o
.
o
f
s
u
b
j
e
c
t
s
n
o
.
o
f
s
u
b
j
e
c
t
s
(
%
)
n
o
.
o
f
s
u
b
j
e
c
t
s
P
a
t
i
e
n
t
s
1
5
3
6
2
5
8
3
4
1
1
9
(
9
2
.
2
)
8
5
0
9
8
4
7
4
9
S
p
o
n
t
a
n
e
o
u
s
c
e
n
t
r
a
l
n
e
r
v
o
u
s
s
y
s
t
e
m
b
l
e
e
d
i
n
g
5
6
5
.
0
4
2
3
9
7
4
1
3
9
7
(
3
1
.
3
)
4
3
0
4
3
5
1
0
9
M
a
y
e
r
e
t
a
l
.
6
-
9
L
i
v
e
r
d
i
s
e
a
s
e
7
5
4
.
0
4
4
9
7
9
5
1
2
4
4
(
2
7
.
8
)
2
5
9
3
6
0
1
7
6
B
o
s
c
h
e
t
a
l
.
,
1
0
,
1
1
C
a
r
r
e
n
o
e
t
a
l
.
,
1
2
L
o
d
g
e
e
t
a
l
.
,
1
3
,
1
4
P
l
a
n
i
n
s
i
c
e
t
a
l
.
,
1
5
S
h
a
o
e
t
a
l
.
1
6
T
r
a
u
m
a
3
3
6
.
5
4
2
8
4
0
9
8
3
7
(
1
8
.
7
)
0
0
4
0
9
B
o
f
f
a
r
d
e
t
a
l
.
1
7
C
a
r
d
i
a
c
s
u
r
g
e
r
y
3
4
5
.
4
1
1
4
1
5
3
2
6
7
(
6
.
0
)
7
5
7
8
0
D
i
p
r
o
s
e
e
t
a
l
.
,
1
8
E
k
e
r
t
e
t
a
l
.
,
1
9
G
i
l
l
e
t
a
l
.
2
0
T
r
a
u
m
a
t
i
c
b
r
a
i
n
i
n
j
u
r
y
1
5
0
.
9
3
6
6
1
9
7
(
2
.
2
)
1
2
2
5
2
4
N
a
r
a
y
a
n
e
t
a
l
.
2
1
S
p
i
n
a
l
s
u
r
g
e
r
y
1
4
6
.
6
1
3
3
6
4
9
(
1
.
1
)
2
4
1
2
0
S
a
c
h
s
e
t
a
l
.
2
2
O
t
h
e
r
c
a
u
s
e
s
6
3
8
.
5
7
3
1
5
5
2
2
8
(
5
.
1
)
5
0
7
4
3
1
C
h
u
a
n
s
u
m
r
i
t
e
t
a
l
.
,
2
3
F
r
i
e
d
e
r
i
c
h
e
t
a
l
.
,
2
4
P
i
h
u
s
c
h
e
t
a
l
.
,
2
5
R
a
o
b
a
i
k
a
d
y
e
t
a
l
.
2
6
H
e
a
l
t
h
y
v
o
l
u
n
t
e
e
r
s
9
2
7
.
2
1
1
7
2
3
2
3
4
9
(
7
.
8
)
9
0
1
0
2
4
0
B
i
j
s
t
e
r
v
e
l
d
e
t
a
l
.
,
2
7
,
2
8
E
r
h
a
r
d
t
s
e
n
e
t
a
l
.
,
2
9
F
r
i
d
b
e
r
g
e
t
a
l
.
,
3
0
F
r
i
e
d
e
r
i
c
h
e
t
a
l
.
,
3
1
W
o
l
z
t
e
t
a
l
.
3
2
*
R
e
f
e
r
e
n
c
e
s
a
r
e
p
r
o
v
i
d
e
d
f
o
r
t
h
e
t
r
i
a
l
s
t
h
a
t
h
a
v
e
b
e
e
n
p
u
b
l
i
s
h
e
d
.
T
h
e
r
e
m
a
i
n
i
n
g
d
a
t
a
a
r
e
p
r
o
v
i
d
e
d
i
n
t
h
e
S
u
p
p
l
e
m
e
n
t
a
r
y
A
p
p
e
n
d
i
x
.
O
n
e
s
t
u
d
y
i
n
c
l
u
d
e
d
c
h
i
l
d
r
e
n
y
o
u
n
g
e
r
t
h
a
n
1
y
e
a
r
o
f
a
g
e
.
S
t
u
d
i
e
s
i
n
c
l
u
d
e
d
p
a
t
i
e
n
t
s
w
i
t
h
p
r
o
s
t
a
t
e
c
t
o
m
y
,
p
e
l
v
i
c
o
r
p
e
l
v
i
c
a
c
e
t
a
b
u
l
a
r
f
r
a
c
t
u
r
e
r
e
c
o
n
s
t
r
u
c
t
i
o
n
,
d
e
n
g
u
e
h
e
m
o
r
r
h
a
g
i
c
f
e
v
e
r
,
b
l
e
e
d
i
n
g
a
f
t
e
r
h
e
m
a
t
o
p
o
i
e
t
i
c
s
t
e
m
-
c
e
l
l
t
r
a
n
s
p
l
a
n
t
a
t
i
o
n
(
t
w
o
p
a
t
i
e
n
t
s
)
,
a
n
d
s
e
v
e
r
e
b
l
e
e
d
i
n
g
a
s
s
o
c
i
a
t
e
d
w
i
t
h
v
i
t
a
m
i
n
K
a
n
t
a
g
o
n
i
s
t
t
h
e
r
a
p
y
.
F
o
u
r
s
t
u
d
i
e
s
i
n
v
o
l
v
e
d
h
e
a
l
t
h
y
v
o
l
u
n
t
e
e
r
s
w
h
o
r
e
c
e
i
v
e
d
a
n
t
i
c
o
a
g
u
l
a
n
t
s
(
f
o
n
d
a
p
a
r
i
n
u
x
,
2
7
i
d
r
a
p
a
r
i
n
u
x
,
2
8
a
c
e
n
o
c
o
u
m
a
r
o
l
,
2
9
a
n
d
w
a
r
f
a
r
i
n
3
0
)
.
O
n
e
s
t
u
d
y
i
n
v
o
l
v
e
d
p
e
r
s
o
n
s
w
h
o
h
a
d
r
e
c
e
i
v
e
d
t
h
e
a
n
t
i
p
l
a
t
e
l
e
t
a
g
e
n
t
c
l
o
p
i
d
o
g
r
e
l
,
o
n
e
s
t
u
d
y
i
n
v
o
l
v
e
d
p
e
r
s
o
n
s
w
h
o
h
a
d
r
e
c
e
i
v
e
d
t
i
s
s
u
e
f
a
c
t
o
r
i
n
h
i
b
i
t
o
r
(
n
e
m
a
t
o
d
e
a
n
t
i
c
o
a
g
u
l
a
n
t
p
r
o
t
e
i
n
c
2
)
,
3
1
o
n
e
s
t
u
d
y
i
n
v
o
l
v
e
d
p
e
r
s
o
n
s
w
h
o
h
a
d
r
e
c
e
i
v
e
d
a
t
h
r
o
m
b
i
n
i
n
h
i
b
i
t
o
r
(
m
e
l
a
g
a
t
r
a
n
)
,
3
2
o
n
e
s
t
u
d
y
w
a
s
a
p
h
a
r
m
a
c
o
k
i
n
e
t
i
c
s
s
t
u
d
y
,
3
1
a
n
d
o
n
e
s
t
u
d
y
i
n
v
o
l
v
e
d
p
e
r
s
o
n
s
w
h
o
h
a
d
u
n
d
e
r
g
o
n
e
p
u
n
c
h
b
i
o
p
s
y
.
The New England Journal of Medicine
Downloaded from nejm.org on January 8, 2011. For personal use only. No other uses without permission.
Copyright 2010 Massachusetts Medical Society. All rights reserved.
Recombinant Activated Factor VII in Clinical Trials
n engl j med 363;19 nejm.org november 4, 2010
1795
means of logistic regression. Statistical analyses
were performed by means of logistic regression
with dose as a covariate. Since the administered
dose of rFVIIa varies according to the type of
bleeding being treated (with some types of bleed-
ing, such as trauma-related bleeding, requiring the
use of higher doses than other types, such as
spontaneous central nervous system bleeding), the
dose given is confounded by the type of bleeding.
To minimize this problem, the analyses included
only studies in which patients had received a study
drug in at least two of the dose categories. Most
of the studies in which patients were randomly
assigned to at least two of the dose categories in-
volved spontaneous central nervous system bleed-
ing, which was associated with a higher event rate
than other indications. Therefore, the effect of the
dose was examined only among patients with this
type of bleeding.
Results
Demographic Characteristics of the Subjects
A total of 4468 subjects (1653 subjects who re-
ceived placebo and 2815 subjects who received
rFVIIa) were enrolled in 35 randomized clinical
trials encompassing various clinical scenarios.
Most of the subjects were patients with sponta-
neous central nervous system bleeding (31.3%),
advanced liver disease (27.8%), or trauma (18.7%)
(Table 1). Approximately 45% (2026) of the sub-
jects received either low doses of rFVIIa (<80 g
per kilogram) or medium doses (80 to 120 g per
kilogram). Healthy volunteers and patients with
bleeding from trauma or cardiac surgery were
younger than patients with other causes of bleed-
ing. However, regardless of the type of trial or the
cause of bleeding, the mean (SD) age was simi-
lar in the placebo groups (5019 years) and the
rFVIIa-treated groups (5319 years).
Thromboembolic Events in Patients
Age and disease state are known indicators of
thrombotic risk.
33-36
The odds ratios for throm-
boembolic events among patients who received
rFVIIa as compared with patients who received
placebo were calculated by adjusting for age and
the type of bleeding. The rate of thromboembol-
ic events was 10.2% among patients who received
rFVIIa as compared with 8.7% among patients who
received placebo (odds ratio, 1.17; 95% confidence
interval [CI], 0.94 to 1.47; P = 0.16) (Table 2). When
we evaluated the rates of thromboembolic events
according to type (i.e., arterial thromboembolic
events vs. venous thromboembolic events), we
found a significantly higher proportion of arte-
rial thromboembolic events in the rFVIIa-treated
groups than in the placebo groups (5.5% vs. 3.2%;
odds ratio, 1.68; 95% CI, 1.20 to 2.36; P = 0.003).
No significant difference was observed between
patients who received rFVIIa and patients who
received placebo with respect to the incidence of
venous thromboembolic events (5.3% and 5.7%,
respectively; odds ratio with rFVIIa, 0.93; 95% CI,
0.70 to 1.23; P = 0.61). When the analyses were lim-
ited to data from industry-sponsored, placebo-
controlled trials, the results were similar (odds
ratio for arterial thromboembolic events, 1.72; 95%
CI, 1.22 to 2.43; P = 0.002; odds ratio for venous
thromboembolic events, 0.92; 95% CI, 0.70 to 1.22;
P = 0.58).
Further analysis of arterial thromboembolic
events in the rFVIIa-treated groups indicated that
76 of 141 events (53.9%) were coronary throm-
boembolic events, and the frequency of coro-
nary thromboembolic events in the rFVIIa-treated
groups was higher than that in the placebo groups
(odds ratio, 2.39; 95% CI, 1.39 to 4.09; P = 0.002).
There was also a trend toward an increased rate
of cerebrovascular thromboembolic events among
patients who received rFVIIa (Table 3).
Analysis of arterial thromboembolic events ac-
cording to age, with adjustment for the type of
bleeding, showed that patients who were 18 years
of age or older had more arterial thromboem-
bolic events than patients younger than 18 years of
age (Table 4). When we analyzed the treatment ef-
fect, we found that the rates of arterial thrombo-
embolic events were higher among patients who
received rFVIIa than among patients who received
placebo, particularly among patients who were 65
years of age or older (9.0% vs. 3.8%; odds ratio,
2.43; 95% CI, 1.34 to 4.41; P = 0.003) and were most
pronounced in the subgroup of rFVIIa-treated pa-
tients who were 75 years of age or older (odds ratio,
3.02; 95% CI, 1.22 to 7.48; P = 0.02) (Table 4).
Analysis of the rates of arterial thromboem-
bolic events according to the type of bleeding,
with adjustment for age, showed that among pa-
tients enrolled in trials of rFVIIa to mitigate spon-
taneous central nervous system bleeding, the rates
of arterial thromboembolic events were signifi-
cantly higher in the rFVIIa-treated groups than in
the placebo groups (8.6% vs. 5.4%; odds ratio,
1.67; 95% CI, 1.03 to 2.69; P = 0.04) (Table 5). The
odds ratios were similar and were higher than
The New England Journal of Medicine
Downloaded from nejm.org on January 8, 2011. For personal use only. No other uses without permission.
Copyright 2010 Massachusetts Medical Society. All rights reserved.
T h e new engl and journal o f medicine
n engl j med 363;19 nejm.org november 4, 2010
1796
1 for types of bleeding other than central nervous
system bleeding, but they were not significant,
possibly because of the lower numbers of patients
for most of the other types of bleeding, as well
as a lower incidence of arterial thromboembolic
events in the placebo group (Table 5).
These analyses, however, do not account for the
various doses of rFVIIa that were used, which may
have had an effect on the risk of thromboembolic
events, especially in studies involving patients with
central nervous system bleeding. The rates of ar-
terial thromboembolic events were 5.4% among
23 patients with spontaneous central nervous sys-
tem bleeding who received placebo, 6.0% among
26 patients who received less than 80 g of rFVIIa
per kilogram, 10.3% among 45 patients who re-
ceived 80 to 120 g of rFVIIa per kilogram, and
11.9% among 13 patients who received more than
120 g of rFVIIa per kilogram. When the dose
was considered as a covariate (adjusted for age) of
rates of arterial thromboembolic events among
patients with central nervous system bleeding who
received rFVIIa, this apparent dose-dependent ef-
fect of rFVIIa treatment was significant (P = 0.02).
Thromboembolic Events in Healthy Volunteers
Thromboembolic events were also analyzed in 349
healthy volunteers in five Novo Nordisk-sponsored
and four investigator-initiated placebo-controlled
trials. The rate of thromboembolic events was 0.9%
among both healthy volunteers who received
rFVIIa and healthy volunteers who received pla-
cebo. None of the thromboembolic events were
arterial in nature. All three venous thromboem-
bolic events (two in healthy volunteers who received
rFVIIa and one in a healthy volunteer who received
placebo) were cases of phlebitis.
Discussion
This comprehensive study of the safety profile of
rFVIIa for off-label treatment of episodes of bleed-
ing involved 4468 subjects enrolled in 35 placebo-
controlled clinical trials. We found an increased
Table 3. Arterial Thromboembolic Events with a Rate Greater Than 0.5%.
Variable
rFVIIa
(N = 2583)
Placebo
(N = 1536)
Odds Ratio
(95% CI)* P Value
number (percent)
All arterial thromboembolic events 141 (5.5) 49 (3.2) 1.68 (1.202.36) 0.003
Coronary events 76 (2.9) 17 (1.1) 2.39 (1.394.09) 0.002
Acute coronary syndromes 57 (2.2) 11 (0.7)
Increased troponin level 19 (0.7) 6 (0.4)
Cerebrovascular events 45 (1.7) 20 (1.3) 1.27 (0.742.17) 0.39
Cerebral infarction 44 (1.7) 19 (1.2)
Hemiparesis 1 (<0.1) 1(<0.1)
* Odds ratios were calculated by means of logistic regression with adjustment for age and type of bleeding.
Computed tomographic confirmation of thrombosis was not obtained for the two cases of hemiparesis.
Table 2. Odds Ratios for Thromboembolic Events.
Thromboembolic Event
rFVIIa
(N = 2583)
Placebo
(N = 1536)
Odds Ratio
(95% CI)* P Value
number (percent)
All events 264 (10.2) 134 (8.7) 1.17 (0.941.47) 0.16
Arterial events 141 (5.5) 49 (3.2) 1.68 (1.202.36) 0.003
Venous events 137 (5.3) 88 (5.7) 0.93 (0.701.23) 0.61
* Odds ratios were calculated by means of logistic regression with adjustment for age and type of bleeding.
The percentage of thromboembolic events was calculated as the number of patients with events as a proportion of the
number of patients who received the assigned study drug.
The New England Journal of Medicine
Downloaded from nejm.org on January 8, 2011. For personal use only. No other uses without permission.
Copyright 2010 Massachusetts Medical Society. All rights reserved.
Recombinant Activated Factor VII in Clinical Trials
n engl j med 363;19 nejm.org november 4, 2010
1797
risk of arterial thromboembolic events among pa-
tients who received off-label rFVIIa as compared
with patients who received placebo for bleeding
episodes. The rate of coronary arterial thrombo-
embolic events among the patients who received
rFVIIa was 2.6 times as high as the rate among
patients who received placebo. Age was also as-
sociated with an increase in the risk of arterial
thromboembolic events after rFVIIa treatment,
with an odds ratio of 2.4 among patients 65 years
of age or older and 3.0 among patients 75 years
of age or older. The rates of arterial thromboem-
bolic events were also higher among patients who
received higher doses of rFVIIa.
Abshire reviewed the efficacy and safety of
rFVIIa in patients with hemophilia who had con-
genital or acquired inhibitory antibodies against
factor VIII or IX; that study was based on data
from clinical trials and spontaneous postmarket-
ing surveillance reports.
37
With approximately
800,000 standard doses of rFVIIa administered
during the period from May 2003 through Decem-
ber 2006, a total of 30 thromboembolic events
were reported, 6 of which were fatal. Spontaneous
reports of 71 adverse events included 14 thrombo-
embolic events (20%), with 2 of 34 reported deaths
due to a thromboembolic event.
37
Solicited reports
of 40 adverse events included 5 thromboembolic
events 12%), with 1 of 32 deaths due to a throm-
boembolic event. A comprehensive overview of
thrombotic adverse events, based on the Med-
Watch pharmacovigilance program, also showed
a low incidence of thrombotic complications as-
sociated with the use of rFVIIa (24.6 events per
100,000 infusions), although the risk of thrombo-
sis was higher among patients treated with rFVIIa
than among those treated with other hemostatic
agents.
38
As the authors of the overview correctly
state, differences in adverse-event reporting prac-
tices among the various compounds may have
contributed to the observed difference in the rate
of thrombotic events. Taken together, the data
show that the use of rFVIIa for an approved in-
dication (i.e., the treatment of episodes of bleeding
in patients with hemophilia) is associated with a
rate of thromboembolic events of less than 1%.
OConnell et al.
5
reviewed events from the
FDAs Adverse Event Reporting System during the
period from 1999 through 2005 and identified
185 thromboembolic events, the majority of which
occurred in patients with off-label indications for
rFVIIa. However, in this patient population, 38%
of the patients received other concomitant thera-
pies, and the study had the inherent limitations
of passive surveillance. In a systematic review of
all published and unpublished case reports, case
series, and clinical studies from 1996 through
2004 that focused on the efficacy and safety of
rFVIIa in patients with or without coagulation
disorders, including patients with trauma and
those who had undergone surgery, the incidence
rate of thrombosis was 1 to 2%.
2
The difference
between the rate of thromboembolic events re-
ported in that review and the results of the pooled
analysis presented here may be due to the fact
that the previous review included mostly patients
with congenital or acquired hemophilia or liver
failure, whereas the present review includes clini-
cal trials involving patients with other causes of
hemorrhage.
Our pooled analysis was conducted with a large
safety data set obtained from placebo-controlled
trials of rFVIIa. The inclusion of control groups
allowed for the proper evaluation of thromboem-
Table 4. All Arterial Thromboembolic Events, According to Age.
Age Group rFVIIa Placebo
Odds Ratio
(95% CI)* P Value
no./total no. (%)
<18 yr 1/70 (1.4) 1/51 (2.0)
1864 yr 73/1764 (4.1) 34/1107 (3.1) 1.36 (0.892.08) 0.15
65 yr 67/742 (9.0) 14/372 (3.8) 2.43 (1.344.41) 0.003
6574 yr 33/427 (7.7) 8/225 (3.6) 2.12 (0.954.71) 0.07
75 yr 34/315 (10.8) 6/147 (4.1) 3.02 (1.227.48) 0.02
* Odds ratios were calculated by means of logistic regression with adjustment for indication.
The P value was not calculated for the first age group because there were only two events.
The percentage of thromboembolic events was calculated as the number of patients with events as a proportion of the
number of patients who received a study drug.
The New England Journal of Medicine
Downloaded from nejm.org on January 8, 2011. For personal use only. No other uses without permission.
Copyright 2010 Massachusetts Medical Society. All rights reserved.
T h e new engl and journal o f medicine
n engl j med 363;19 nejm.org november 4, 2010
1798
bolic events after the administration of rFVIIa.
Furthermore, the data presented in our analysis
were obtained from clinical trials involving pa-
tients with bleeding disorders other than hemo-
philia in order to establish a clear understanding
of the safety of rFVIIa in patients with various
types of bleeding. This design is important, be-
cause many of these patients also received multiple
transfusions that may have contributed to adverse
outcomes, especially in observational studies.
39
In
a previous study, we evaluated safety data obtained
from 13 clinical trials of rFVIIa in patients with
coagulopathy due to anticoagulant therapy, cirrho-
sis, or severe traumatic injury, and we reported
thromboembolic events in 23 of 430 patients who
received placebo (5.3%) and in 45 of 748 patients
who received active treatment (6.0%). No signifi-
cant differences were noted between patients who
received placebo and patients who received rFVIIa,
on the basis of data from individual trials or
pooled data (P = 0.57).
40
The limitations of the current data set include
the relatively small individual study samples, dif-
ferences in indications (e.g., central nervous sys-
tem bleeding and bleeding from liver disease,
trauma, and other causes), and the fact that the
studies were conducted over a 12-year span. How-
ever, the wide scope of indications may be con-
sidered important, since subjects with or without
coagulopathies were evaluated. The variation in
dosing was taken into consideration by categoriz-
ing subjects into three dose groups. Confounding
factors such as age and sex were also taken into
consideration in the statistical analysis.
The data presented provide a systematic evalu-
ation of rates of thromboembolic events in place-
bo-controlled trials of rFVIIa. It is important to
note that central nervous system bleeding occurs
in an older population with an inherently in-
creased risk of thromboembolic events. Therefore,
risk-benefit considerations should be evaluated
before administering any hemostatic agent.
Supported by Novo Nordisk.
Dr. Levy reports serving on a steering committee for Novo
Nordisk, and Drs. Andersen and Truloff report being employees
of and having equity interest in Novo Nordisk. No other poten-
tial conflict of interest relevant to this article was reported.
Disclosure forms provided by the authors are available with
the full text of this article at NEJM.org.
We thank the following Novo Nordisk employees: Brett Skol-
nick, Ph.D., Sheba Mathew, Ph.D., and Abha Chandra, Ph.D., for
valuable contributions made during the development of an ear-
lier version of the manuscript, and Ming Ying Ching, M.S.,
Naum Khutoryansky, Ph.D., and Anders Rosholm, Ph.D., for
providing statistical support.
Table 5. All Arterial Thromboembolic Events, According to Cause of Bleeding.*
Cause of Bleeding
No. of
Studies rFVIIa Placebo
Odds Ratio
(95% CI) P Value Reference
no./total no. (%)
Spontaneous central nervous system
bleeding
5 84/974 (8.6) 23/423 (5.4) 1.67 (1.032.69) 0.04 Mayer et al.
6-9
Advanced liver disease 7 23/795 (2.9) 6/449 (1.3) 2.19 (0.895.42) 0.09 Bosch et al.,
10,11
Carreno et al.,
12
Lodge et al.,
13,14
Planinsic et al.,
15
Shao et al.
16
Trauma 3 19/409 (4.6) 15/428 (3.5) 1.39 (0.692.77) 0.36 Boffard et al.
17
Cardiac surgery 3 9/153 (5.9) 4/114 (3.5) 1.59 (0.475.34) 0.45 Diprose et al.,
18
Ekert
et al.,
19
Gill et al.
20
Traumatic brain injury 1 2/61 (3.3) 1/36 (2.8) Narayan et al.
21
Spinal surgery 1 1/36 (2.8) 0/13 Sachs et al.
22
Other causes 6 3/155 (1.9) 0/73 Chuansumrit et al.,
23
Friederich et al.,
24
Pihusch et al.,
25
Raobaikady et al.
26
* References are provided for the trials that have been published. The remaining data are provided in the Supplementary Appendix.
Odds ratios were calculated by means of logistic regression with adjustment for age. Odds ratios were not calculated in instances with very
few events.
The percentage of thromboembolic events was calculated as the number of patients with events as a proportion of the number of patients
who received a study drug.
The New England Journal of Medicine
Downloaded from nejm.org on January 8, 2011. For personal use only. No other uses without permission.
Copyright 2010 Massachusetts Medical Society. All rights reserved.
Recombinant Activated Factor VII in Clinical Trials
n engl j med 363;19 nejm.org november 4, 2010
1799
References
1. Hedner U. Factor VIIa and its poten-
tial therapeutic use in bleeding-associated
pathologies. Thromb Haemost 2008;100:
557-62.
2. Levi M, Peters M, Bller HR. Efficacy
and safety of recombinant factor VIIa for
treatment of severe bleeding: a systematic
review. Crit Care Med 2005;33:883-90.
3. Villar A, Aronis S, Morfini M, et al.
Pharmacokinetics of activated recombinant
coagulation factor VII (NovoSeven) in chil-
dren vs. adults with haemophilia A. Hae-
mophilia 2004;10:352-9.
4. Hedner U. Mechanism of action of
factor VIIa in the treatment of coagulopa-
thies. Semin Thromb Hemost 2006;32:
Suppl 1:77-85.
5. OConnell KA, Wood JJ, Wise RP,
Lozier JN, Braun MM. Thromboembolic
adverse events after use of recombinant hu-
man coagulation factor VIIa. JAMA 2006;
295:293-8.
6. Mayer SA, Brun NC, Begtrup K, et al.
Recombinant activated factor VII for acute
intracerebral hemorrhage. N Engl J Med
2005;352:777-85.
7. Mayer SA, Brun NC, Broderick J, et al.
Safety and feasibility of recombinant fac-
tor VIIa for acute intracerebral hemorrhage.
Stroke 2005;36:74-9.
8. Mayer SA, Brun NC, Broderick J, et al.
Recombinant activated factor VII for acute
intracerebral hemorrhage: US phase IIA
trial. Neurocrit Care 2006;4:206-14.
9. Mayer SA, Brun NC, Begtrup K, et al.
Efficacy and safety of recombinant activated
factor VII for acute intracerebral hemor-
rhage. N Engl J Med 2008;358:2127-37.
10. Bosch J, Thabut D, Bendtsen F, et al.
Recombinant factor VIIa for upper gastro-
intestinal bleeding in patients with cir-
rhosis: a randomized, double-blind trial.
Gastroenterology 2004;127:1123-30.
11. Bosch J, Thabut D, Albillos A, et al.
Recombinant factor VIIa for variceal bleed-
ing in patients with advanced cirrhosis:
a randomized, controlled trial. Hepatolo-
gy 2008;47:1604-14.
12. Carreno V, Messnern M, Arrieta J,
Berthier A, Schelde P, DeMello G. The ef-
fect of recombinant factor VIIa (Novo-
Seven) on haemorrhage following dental
surgery in patients with liver cirrhosis
a randomised placebo controlled study.
Presented at the XVIII Congress of the
International Society on Thrombosis and
Haemostasis, July 612, 2001:P2612.
13. Lodge JP, Jonas S, Jones RM, et al.
Efficacy and safety of repeated perioper-
ative doses of recombinant factor VIIa in
liver transplantation. Liver Transpl 2005;
11:973-9.
14. Lodge JP, Jonas S, Oussoultzoglou E,
et al. Recombinant coagulation factor VIIa
in major liver resection: a randomized,
placebo-controlled, double-blind clinical
trial. Anesthesiology 2005;102:269-75.
15. Planinsic RM, van der Meer J, Testa G,
et al. Safety and efficacy of a single bolus
administration of recombinant factor VIIa
in liver transplantation due to chronic liver
disease. Liver Transpl 2005;11:895-900.
16. Shao YF, Yang JM, Chau GY, et al. Safety
and hemostatic effect of recombinant acti-
vated factor VII in cirrhotic patients under-
going partial hepatectomy: a multicenter,
randomized, double-blind, placebo-con-
trolled trial. Am J Surg 2006;191:245-9.
17. Boffard KD, Riou B, Warren B, et al.
Recombinant factor VIIa as adjunctive
therapy for bleeding control in severely in-
jured trauma patients: two parallel ran-
domized, placebo-controlled, double-blind
clinical trials. J Trauma 2005;59:8-15.
18. Diprose P, Herbertson MJ, OShaugh-
nessy D, Gill RS. Activated recombinant fac-
tor VII after cardiopulmonary bypass re-
duces allogeneic transfusion in complex
non-coronary cardiac surgery: randomized
double-blind placebo-controlled pilot study.
Br J Anaesth 2005;95:596-602.
19. Ekert H, Brizard C, Eyers R, Cochrane
A, Henning R. Elective administration in
infants of low-dose recombinant activat-
ed factor VII (rFVIIa) in cardiopulmonary
bypass surgery for congenital heart dis-
ease does not shorten time to chest clo-
sure or reduce blood loss and need for
transfusions: a randomized, double-blind,
parallel group, placebo-controlled study of
rFVIIa and standard haemostatic replace-
ment therapy versus standard haemostatic
replacement therapy. Blood Coagul Fibri-
nolysis 2006;17:389-95.
20. Gill R, Herbertson M, Vuylsteke A, et al.
Safety and efficacy of recombinant activat-
ed factor VII: a randomized placebo-con-
trolled trial in the setting of bleeding after
cardiac surgery. Circulation 2009;120:21-7.
21. Narayan RK, Maas AI, Marshall LF,
Servadei F, Skolnick BE, Tillinger MN. Re-
combinant factor VIIA in traumatic intra-
cerebral hemorrhage: results of a dose-
escalation clinical trial. Neurosurgery
2008;62:776-86.
22. Sachs B, Delacy D, Green J, et al. Re-
combinant activated factor VII in spinal
surgery: a multicenter, randomized, dou-
ble-blind, placebo-controlled, dose-esca-
lation trial. Spine 2007;32:2285-93.
23. Chuansumrit A, Wangruangsatid S,
Lektrakul Y, Chua MN, Zeta Capeding MR,
Bech OM. Control of bleeding in children
with Dengue hemorrhagic fever using
recombinant activated factor VII: a ran-
domized, double-blind, placebo-controlled
study. Blood Coagul Fibrinolysis 2005;16:
549-55.
24. Friederich PW, Henny CP, Messelink
EJ, et al. Effect of recombinant activated
factor VII on perioperative blood loss in
patients undergoing retropubic prostatec-
tomy: a double-blind placebo-controlled
randomised trial. Lancet 2003;361:201-5.
[Erratum, Lancet 2003;361:1138.]
25. Pihusch M, Bacigalupo A, Szer J, et al.
Recombinant activated factor VII in treat-
ment of bleeding complications following
hematopoietic stem cell transplantation.
J Thromb Haemost 2005;3:1935-44.
26. Raobaikady R, Redman J, Ball JA, Ma-
loney G, Grounds RM. Use of activated
recombinant coagulation factor VII in pa-
tients undergoing reconstruction surgery
for traumatic fracture of pelvis or pelvis
and acetabulum: a double-blind, random-
ized, placebo-controlled trial. Br J Anaesth
2005;94:586-91.
27. Bijsterveld NR, Moons AH, Boekholdt
SM, et al. Ability of recombinant factor
VIIa to reverse the anticoagulant effect
of the pentasaccharide fondaparinux in
healthy volunteers. Circulation 2002;106:
2550-4.
28. Bijsterveld NR, Vink R, van Aken BE,
et al. Recombinant factor VIIa reverses
the anticoagulant effect of the long-acting
pentasaccharide idraparinux in healthy
volunteers. Br J Haematol 2004;124:653-8.
29. Erhardtsen E, Nony P, Dechavanne M,
French P, Biossel JP, Hedner U. The effect
of recombinant factor VIIa (NovoSeven) in
healthy volunteers receiving acenocouma-
rol to an International Normalized Ratio
above 2.0. Blood Coagul Fibrinolysis 1998;
9:741-8.
30. Fridberg MJ, Hedner U, Roberts HR,
Erhardtsen E. A study of the pharmacoki-
netics and safety of recombinant activated
factor VII in healthy Caucasian and Japa-
nese subjects. Blood Coagul Fibrinolysis
2005;16:259-66.
31. Friederich PW, Levi M, Bauer KA, et
al. Ability of recombinant factor VIIa to
generate thrombin during inhibition of
tissue factor in human subjects. Circula-
tion 2001;103:2555-9.
32. Wolzt M, Levi M, Sarich TC, et al. Effect
of recombinant factor VIIa on melagatran-
induced inhibition of thrombin generation
and platelet activation in healthy volunteers.
Thromb Haemost 2004;91:1090-6.
33. Abbott RD, Curb JD, Rodriguez BL, et
al. Age-related changes in risk factor ef-
fects on the incidence of thromboembolic
and hemorrhagic stroke. J Clin Epidemiol
2003;56:479-86.
34. Heit JA. Venous thromboembolism:
disease burden, outcomes and risk factors.
J Thromb Haemost 2005;3:1611-7.
35. Rosendaal FR. Risk factors for venous
thrombotic disease. Thromb Haemost
1999;82:610-9.
36. Samama MM. An epidemiologic study
of risk factors for deep vein thrombosis in
medical outpatients: the Sirius study.
Arch Intern Med 2000;160:3415-20.
37. Abshire T. Safety update on recombi-
nant factor VIIa in the treatment of con-
genital and acquired hemophilia. Semin
Hematol 2008;45:Suppl:S3-S6.
38. Aledort LM. Comparative thrombotic
event incidence after infusion of recombi-
nant factor VIIa versus factor VIII inhibi-
The New England Journal of Medicine
Downloaded from nejm.org on January 8, 2011. For personal use only. No other uses without permission.
Copyright 2010 Massachusetts Medical Society. All rights reserved.
n engl j med 363;19 nejm.org november 4, 2010
1800
Recombinant Activated Factor VII in Clinical Trials
tor bypass activity. J Thromb Haemost
2004;2:1700-8.
39. Murphy GJ, Reeves BC, Rogers CA,
Rizvi SI, Culliford L, Angelini GD. In-
creased mortality, postoperative morbidi-
ty, and cost after red blood cell transfu-
sion in patients having cardiac surgery.
Circulation 2007;116:2544-52.
40. Levy JH, Fingerhut A, Brott T, Lang-
bakke IH, Erhardtsen E, Porte RJ. Recom-
binant factor VIIa in patients with coagu-
lopathy secondary to anticoagulant therapy,
cirrhosis, or severe traumatic injury: re-
view of safety profile. Transfusion 2006;
46:919-33.
Copyright 2010 Massachusetts Medical Society.
Paul Berman, M.D.
The New England Journal of Medicine
Downloaded from nejm.org on January 8, 2011. For personal use only. No other uses without permission.
Copyright 2010 Massachusetts Medical Society. All rights reserved.
Вам также может понравиться
- Nota 2Документ8 страницNota 2Hector GuzmanОценок пока нет
- Antiplatelet Drugs: Mechanisms and Risks of Bleeding Following Cardiac OperationsДокумент18 страницAntiplatelet Drugs: Mechanisms and Risks of Bleeding Following Cardiac OperationsViona PrasetyoОценок пока нет
- Risk Factors and Complications of Subconjunctival Hemorrhages in Patients Taking WarfarinДокумент5 страницRisk Factors and Complications of Subconjunctival Hemorrhages in Patients Taking WarfarinSyafar Agus Al-Fath MukminОценок пока нет
- Jurnal THTДокумент3 страницыJurnal THTValentina AdindaОценок пока нет
- THREAT Helps To Identify Epistaxis Patients Requiring Blood TransfusionsДокумент6 страницTHREAT Helps To Identify Epistaxis Patients Requiring Blood TransfusionswitariОценок пока нет
- Low Systemic Vascular ResistanceДокумент7 страницLow Systemic Vascular ResistanceMuhammad BadrushshalihОценок пока нет
- Salim 2009Документ6 страницSalim 2009raden chandrajaya listiandokoОценок пока нет
- STR6Документ12 страницSTR6ali akbar meccaОценок пока нет
- Lectura 3seminario Micosis ProfundaДокумент8 страницLectura 3seminario Micosis ProfundaSebastian CastroОценок пока нет
- Closure of Patent Foramen Ovale Versus Medical Therapy After Cryptogenic StrokeДокумент9 страницClosure of Patent Foramen Ovale Versus Medical Therapy After Cryptogenic StrokelaurasheerОценок пока нет
- Clinical Trials and Regulatory Science in CardiologyДокумент6 страницClinical Trials and Regulatory Science in Cardiologydianaerlita97Оценок пока нет
- Readmission and Other Adverse Events After Transsphenoidal Surgery: Prevalence, Timing, and Predictive FactorsДокумент9 страницReadmission and Other Adverse Events After Transsphenoidal Surgery: Prevalence, Timing, and Predictive FactorsbobОценок пока нет
- Transfusion-Related Acute Lung Injury: Pearl Toy,, and Ognjen GajicДокумент2 страницыTransfusion-Related Acute Lung Injury: Pearl Toy,, and Ognjen GajicMaulana Akbar LubisОценок пока нет
- Bleeding Risk Assessment and Management in Atrial Fibrillation PatientsДокумент15 страницBleeding Risk Assessment and Management in Atrial Fibrillation PatientsAlina SarbuОценок пока нет
- Concise Report: Efficacy and Tolerance of Infliximab in Refractory Takayasu Arteritis: French Multicentre StudyДокумент5 страницConcise Report: Efficacy and Tolerance of Infliximab in Refractory Takayasu Arteritis: French Multicentre StudyMikhail PisarevОценок пока нет
- F4.cyklo CrashДокумент10 страницF4.cyklo CrashSuresh KumarОценок пока нет
- Perioperative Management of Acquired Hemophilia A: A Case Report and Review of LiteratureДокумент3 страницыPerioperative Management of Acquired Hemophilia A: A Case Report and Review of LiteratureSiva SankarОценок пока нет
- Managementul Acut Al TVC La Cei in Tratament Cu AntiagregantДокумент21 страницаManagementul Acut Al TVC La Cei in Tratament Cu AntiagregantDrHellenОценок пока нет
- Anticoagulation AsraДокумент38 страницAnticoagulation AsratriadindaОценок пока нет
- Indications For Platelet Transfusion in Children With Acute LeukemiaДокумент10 страницIndications For Platelet Transfusion in Children With Acute LeukemiaAbidi HichemОценок пока нет
- Acquired Factor V Inhibitor RéviséДокумент7 страницAcquired Factor V Inhibitor RéviséImen KrichenОценок пока нет
- Frank 2019Документ15 страницFrank 2019Oliver ArteagaОценок пока нет
- GastroprofilaxisДокумент13 страницGastroprofilaxisDaniel Alejandro Lecaros BarríaОценок пока нет
- Casa Is 2000Документ5 страницCasa Is 2000Igor DemićОценок пока нет
- Bleeding in AFДокумент24 страницыBleeding in AFAlexandra RosaОценок пока нет
- Management of Epistaxis in Patients With Ventricular Assist Device: A Retrospective ReviewДокумент6 страницManagement of Epistaxis in Patients With Ventricular Assist Device: A Retrospective ReviewDenta HaritsaОценок пока нет
- WJH 3 130bacteremiaДокумент7 страницWJH 3 130bacteremiaLasiaf AlaskaОценок пока нет
- Periprocedural Heparin Bridging in Patients Receiving Vitamin K AntagonistsДокумент26 страницPeriprocedural Heparin Bridging in Patients Receiving Vitamin K AntagonistsWallnut StreetОценок пока нет
- Hospitalizations After Heart Failure Diagnosis: A Community PerspectiveДокумент8 страницHospitalizations After Heart Failure Diagnosis: A Community PerspectiveferanofiartikaОценок пока нет
- Uso de Plasmaféresis en Unidades de Pacientes CríticosДокумент8 страницUso de Plasmaféresis en Unidades de Pacientes CríticosElena Garcia LueizaОценок пока нет
- Efficacy of Red Blood Cell Transfusion in The Critically Ill (Original Article)Документ8 страницEfficacy of Red Blood Cell Transfusion in The Critically Ill (Original Article)Rayhan OemarОценок пока нет
- Argenta 2011Документ4 страницыArgenta 2011NYONGKERОценок пока нет
- Usefulness Associated With Antiarrhythmic Medicines ShortTerm Employ Soon After Catheter Ablation Regarding Atrial Fibrillation EASTAF Trialktjjz PDFДокумент1 страницаUsefulness Associated With Antiarrhythmic Medicines ShortTerm Employ Soon After Catheter Ablation Regarding Atrial Fibrillation EASTAF Trialktjjz PDFjohnhawk8Оценок пока нет
- Napolitano 2006Документ14 страницNapolitano 2006Olivia Alexandra DavidОценок пока нет
- The Use of Recombinant Factor Viia (Novoseven) For Treatment of Active or Impending Bleeding in Brain Injury: Broadening The IndicationsДокумент7 страницThe Use of Recombinant Factor Viia (Novoseven) For Treatment of Active or Impending Bleeding in Brain Injury: Broadening The IndicationsBig TexОценок пока нет
- Factor VIIДокумент7 страницFactor VIIsonia martinОценок пока нет
- Characteristics of Patients With Venous Thromboembolism and Atrial Fibrillation in VenezuelaДокумент5 страницCharacteristics of Patients With Venous Thromboembolism and Atrial Fibrillation in VenezuelaDhedy DheyzОценок пока нет
- Etiological Pattern and Outcome of Non-Variceal Upper G.I. BleedingДокумент5 страницEtiological Pattern and Outcome of Non-Variceal Upper G.I. BleedingJawad ZafarОценок пока нет
- Restrictive or Liberal Red-Cell Transfusion For Cardiac SurgeryДокумент11 страницRestrictive or Liberal Red-Cell Transfusion For Cardiac SurgeryRadmila KaranОценок пока нет
- Restrictive or Liberal Red-Cell Transfusion For Cardiac SurgeryДокумент12 страницRestrictive or Liberal Red-Cell Transfusion For Cardiac SurgeryFredy Alcides Ramos VelasquezОценок пока нет
- Art:10.1186/s13054 016 1252 2Документ9 страницArt:10.1186/s13054 016 1252 2IsnaОценок пока нет
- Diastolic Function Is A Strong Predictor of Mortality in Patients With Chronic Kidney DiseaseДокумент6 страницDiastolic Function Is A Strong Predictor of Mortality in Patients With Chronic Kidney DiseasehanifahrafaОценок пока нет
- A Double-Blind, Placebo-Controlled Trial of Ruxolitinib For MyelofibrosisДокумент9 страницA Double-Blind, Placebo-Controlled Trial of Ruxolitinib For MyelofibrosisharlessitompulОценок пока нет
- Arrhytmia in ICUДокумент2 страницыArrhytmia in ICUEvita FebriyantiОценок пока нет
- Plasma Exchange For Heparin-Induced Thrombocytopenia: Is There Enough Evidence?Документ4 страницыPlasma Exchange For Heparin-Induced Thrombocytopenia: Is There Enough Evidence?sayednourОценок пока нет
- Acute Fungal Sinusitis Natural History and The Role of Frozen SectionДокумент8 страницAcute Fungal Sinusitis Natural History and The Role of Frozen SectionwitariОценок пока нет
- Burden of Sodium Abnormalities in Patients Hospitalized For Heart FailureДокумент7 страницBurden of Sodium Abnormalities in Patients Hospitalized For Heart FailureVincent ReyesОценок пока нет
- 3144.full MoyamoyaДокумент8 страниц3144.full MoyamoyaDarren ZytkiewiczОценок пока нет
- Corticosteroid Side-Effects and Risk For Bleeding in ImmuneДокумент8 страницCorticosteroid Side-Effects and Risk For Bleeding in ImmuneDini BerlianaОценок пока нет
- Vox SanguinisДокумент179 страницVox SanguinistristanmunarОценок пока нет
- Annsurg00186 0127Документ14 страницAnnsurg00186 0127Muhammad NomanОценок пока нет
- Amal Et AlДокумент3 страницыAmal Et AlInternational Journal of Clinical and Biomedical Research (IJCBR)Оценок пока нет
- Research Article: Elevated Heparin-Induced Antibodies Are More Common in Diabetic Patients With Vascular DiseaseДокумент6 страницResearch Article: Elevated Heparin-Induced Antibodies Are More Common in Diabetic Patients With Vascular DiseaseAntony Boston MichaelОценок пока нет
- Komplikasi Stroke PDFДокумент7 страницKomplikasi Stroke PDFJose Hady PuteraОценок пока нет
- Original ContributionsДокумент10 страницOriginal ContributionsMarisol MartinezОценок пока нет
- Ying Li 2016Документ8 страницYing Li 2016Bogdan TrandafirОценок пока нет
- Treatment of Venous Thromboembolism: ReviewДокумент12 страницTreatment of Venous Thromboembolism: ReviewMayra Alejandra Prada SerranoОценок пока нет
- Guias ASRA 2010 Anestesia Regional en Paciente AnticoaguladoДокумент38 страницGuias ASRA 2010 Anestesia Regional en Paciente AnticoaguladoJonathan Tipon Galvis100% (1)
- Poise-3 (Nejm 2022)Документ12 страницPoise-3 (Nejm 2022)Jesus MujicaОценок пока нет
- Prospectus PDFДокумент68 страницProspectus PDFPrince Digital ComputersОценок пока нет
- XareltofinalДокумент2 страницыXareltofinalMuniba NasimОценок пока нет
- Carcinoma StomachДокумент54 страницыCarcinoma StomachDn Ezrinah Dn EshamОценок пока нет
- PATHology Questions MGR Medical UniversityДокумент40 страницPATHology Questions MGR Medical UniversityPONNUSAMY P50% (2)
- Angelman Syndrome - Identification and ManagementДокумент10 страницAngelman Syndrome - Identification and ManagementFajar YuniftiadiОценок пока нет
- Machupo VirusДокумент15 страницMachupo VirusiggyОценок пока нет
- Human Biology Laboratory 4: Body Tissues and Organization List The 4 Tissue Types and Give A General Function: Pg. 40Документ4 страницыHuman Biology Laboratory 4: Body Tissues and Organization List The 4 Tissue Types and Give A General Function: Pg. 40bugyourselfОценок пока нет
- Dental ChartingДокумент51 страницаDental ChartingXuan5550% (1)
- Contents (Continued) : Chapter 5. Nondestructive Inspection (Ndi)Документ3 страницыContents (Continued) : Chapter 5. Nondestructive Inspection (Ndi)blackhawkОценок пока нет
- Goc Marina Reviewer PDFДокумент57 страницGoc Marina Reviewer PDFAl Jhem Geronimo60% (5)
- Chapter 15 - Autonomic Nervous System Course OutlineДокумент9 страницChapter 15 - Autonomic Nervous System Course OutlineleoОценок пока нет
- Legal MedДокумент42 страницыLegal Medaisajane_rmt100% (6)
- At-Risk and Runaway Youth in Washington State: Outcomes For Youth Admitted To Secure Crisis Residential Centers and Mandatory Chemical Dependency TreatmentДокумент45 страницAt-Risk and Runaway Youth in Washington State: Outcomes For Youth Admitted To Secure Crisis Residential Centers and Mandatory Chemical Dependency TreatmentWashington State Institute for Public PolicyОценок пока нет
- Sds Methode LimitationsДокумент8 страницSds Methode LimitationsorinadeesfuerzoОценок пока нет
- Smear Layer Final2Документ10 страницSmear Layer Final2bhudentОценок пока нет
- Kosmetik BatalДокумент5 страницKosmetik BatalNurul AtikОценок пока нет
- Case Study Breast CancerДокумент3 страницыCase Study Breast CancerJustin Joshua Derilo OrdoñaОценок пока нет
- Biochemistry and Histocytochemistry Research DevelopmentsДокумент377 страницBiochemistry and Histocytochemistry Research Developmentsfenrisulven2010100% (1)
- Limfoma Kutis Pada Pasien Yang Semula Di DiagnosisДокумент34 страницыLimfoma Kutis Pada Pasien Yang Semula Di DiagnosisChris MulyoОценок пока нет
- Part 1 - Bernal Safety - Intro and Emergencies - Powerpoint - 29mar21Документ34 страницыPart 1 - Bernal Safety - Intro and Emergencies - Powerpoint - 29mar21John TorrezОценок пока нет
- Fluids and Electrolytes Study GuideДокумент13 страницFluids and Electrolytes Study GuideElizabeth McKeeОценок пока нет
- Endocrine PathologyДокумент13 страницEndocrine Pathologysarguss14100% (1)
- Neck Pain and Lower Back Pain. Med Clin N Am. 2019.Документ14 страницNeck Pain and Lower Back Pain. Med Clin N Am. 2019.Jose Fernando Diez100% (1)
- Quantitative Analysis of The Lifting Effect Of.10Документ12 страницQuantitative Analysis of The Lifting Effect Of.10Arcelino FariasОценок пока нет
- Acute Limb Ischemia: Clinical PracticeДокумент9 страницAcute Limb Ischemia: Clinical PracticeIndah MaulidawatiОценок пока нет
- Nursing Care Plan Myocardia InfarctionДокумент3 страницыNursing Care Plan Myocardia Infarctionaldrin1920Оценок пока нет
- Colorectal CA With Type 2 Diabetes MellitusДокумент62 страницыColorectal CA With Type 2 Diabetes MellitusJoan Rae TanОценок пока нет
- Drug Education NotesДокумент75 страницDrug Education NotesJoshua D None-NoneОценок пока нет
- V Jttu/: Prices ChangeДокумент179 страницV Jttu/: Prices ChangeKarpincho3Оценок пока нет
- Maternal and Child Health Nursing TestДокумент21 страницаMaternal and Child Health Nursing TestAt Day's Ward50% (2)