Академический Документы
Профессиональный Документы
Культура Документы
Role AEDs in Migraine Prevention
Загружено:
Surat TanprawateОригинальное название
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Role AEDs in Migraine Prevention
Загружено:
Surat TanprawateАвторское право:
Доступные форматы
A Role of AEDs drug
in migraine
Surat Tanprawate, MD, MSc(Lond.), FRCPT
Headache clinic, Chiangmai University
Principle of migraine prevention
Role of anti-epileptic drug for
migraine
Topic
PART 1. Principle of
migraine prevention
A young female student with episodic headache for
1 years
Headache characters: throbbing, alternate side,
temper, eye, occiput, lasting for 4-6 hours
Frequency: 3 attacks / week
Associated symptom: nausea, photophobia
Severity: 7/10
Migraine is considered as a chronic
disorder with episodic attacks (CDEA)
No
migraine
LFEM
0-9 days of
headache/month
HFEM
10-14 days of
headache/month
Chronic
Migraine
Chronic migraine associated with
Conceptualized of clinical course of migraine
Poor quality of life
Highly associated with psychiatric disorder
Risk of medication overused
Risk of stroke? (MwA)
Bigal and Lipton Neurology 2008;71;848-855
2.5%/yr EM to CM
6%/yr HFEM to CM
26% 2-yrs transition rate CM to EM
Rate of transition
Migraine treatment
Give the information of migraine
Life style modication
Acute medication
Preventive medication
Risk factor for migraine
progression
Bigal ME et al. Current Opinion in Neurology 2009, 22:269276
Issue on preventive
medication?
Start
When should we start?
What should we start?
Evaluation
When should we
evaluate?
What should we
evaluate?
Stop
When should we
stop?
How to stop?
Drug titration Duration
When to use preventive
medication?
Migraine signicantly interfere with patients daily routine,
despite acute Rx
Acute medication contraindicated, ineffective, intolerable
AEs, or overused
Frequency of acute medication use > 2 / week
How often of migraine attack should
we start preventive medication?
Dodick DW, Siberstein SD Pract Neurol 2007;7:383-393
Estimated 1-year incidence rate of: (a) chronic daily headache (180+ HA day/
year); or (b) increased HA (105-179) in an episodic headache population
Headache frequency associated with onset of CDH:
a study on episodic headache (2-104 day/year)
Scher A.I. et al. Pain 106 (2003) 8189
4.33 / month
n=798
Frequency of migraine attacks > 1 / wk
Migraine condition that
needs preventive med
Hemiplegic migraine
Basilar migraine
Migraine with prolonged, disabling or
frequent aura
Migrainous cerebral infarction
The major group of
preventive medication
Anticonvulsants
Antidepressants
B-adrenergic blockers
Calcium channel antagonists
NSAIDs
Serotonin antagonists
Other (including riboavin, minerals, herbs, botulinum toxin)
Drug choice?
1. Migraine condition
(EM, CM, RM, MOH)
2. Efcacy
3. Adverse events
4. Comorbidity
5. Cost
Titration regimen
Start low, go slow: recommend every week titration
reach target dose within 1 month
Target dose
dose recommend in clinical trials
stop when reach efcacy / or side effects
Dodick DW, Siberstein SD Pract Neurol 2007;7:383-393
Maintenance regime
There have no evidence on the optimal length of prophylactic
treatment
Duration
6 weeks should appear clinical efcacy
3 months is usually considered sufcient to assess
prophylactic efcacy
6 months may be need to reach maximum effect
Treatment length may be continue to 3-6 months if there there
was some improvement during the rst 3 months
Dodick DW, Siberstein SD Pract Neurol 2007;7:383-393
Assessing improvements
with migraine prevention
Common endpoints used in preventive studies
Reduction in attack frequency
Reduction in attack intensity/severity
Decrease in migraine induced disability
% of patients with > 50% reduction in attack
frequency
Headache
follow up form
Headache day
Acute med used
HIT-6 scale
Treatment response
Headache Impact
Test (HIT-6)
!"# (< 49)
$%&'(%) (50-55)
*%' (56-59)
*%'+,- (>60)
Issue on preventive
medication?
Start
When should we start?
What should we start?
Evaluation
When should we
evaluate?
What should we
evaluate?
Stop
When should we
stop?
How to stop?
Drug titration Duration
severity
frequency
acute med use
type of migraine
efcacy
comorbidity
1 month 3-6 months
6 wks-3 mo-6 mo
frequency
impact
3-6 months
slow tapering off with
maintain lowest dose if
headache occurs
PART2. Role of AEDs
in migraine
Evidence of neuronal
excitability in migraine
Co-morbid condition of migraine and epilepsy
Cortical spreading depression (CSD) in migraine
with aura
Mutation in Familial Hemiplegic Migraine (FHM)
Response of migraine with AEDs
Discovery of
anti-epileptic drugs
Old generation
1800s Bromide Solution
1912 Phenobarbital
1938 Phenytoin
1960 Ethosuximide
1973 Carbamazepine
1978 Valproate
New generation
1993 Felbamate
1993 Gabapentin
1994 Lamotrigine
1996 Fosphenytoin
1996 Topiramate
1997 Tiagabine
1999 Vigabatrin
2000 Oxcarbazepine
2000 Levetiracetam
2005 Pregabalin
Discovery of
anti-epileptic drugs
Old generation
1800s Bromide Solution
1912 Phenobarbital
1938 Phenytoin
1960 Ethosuximide
1973 Carbamazepine
1978 Valproate
New generation
1993 Felbamate
1993 Gabapentin
1994 Lamotrigine
1996 Fosphenytoin
1996 Topiramate
1997 Tiagabine
1999 Vigabatrin
2000 Oxcarbazepine
2000 Levetiracetam
2005 Pregabalin
Discovery of
anti-epileptic drugs
Old generation
1800s Bromide Solution
1912 Phenobarbital
1938 Phenytoin
1960 Ethosuximide
1973 Carbamazepine
1978 Valproate
New generation
1993 Felbamate
1993 Gabapentin
1994 Lamotrigine
1996 Fosphenytoin
1996 Topiramate
1997 Tiagabine
1999 Vigabatrin
2000 Oxcarbazepine
2000 Levetiracetam
2005 Pregabalin
Discovery of
anti-epileptic drugs
Calabresi P et al. Trends in Pharm Sci 2007; 28(4):188-195
Calabresi P et al. Trends in Pharm Sci 2007; 28(4):188-195
AEDs in migraine treatment
Type of treatment
prophylaxis
acute treatment
Type of Migraine
episodic vs chronic migraine
with/without aura
refractory migraine
CM with MOH
Migraine variant
Episodic vs Chronic vs Refractory
Episodic migraine
0-14 headache days per month
Chronic
15 or more headache days per month for 3 or more months
8 or more days meet criteria for migraine with our aura/or response to migraine
specic drug
Refractory (preventive medication)
Failed adequate trials of preventive med at least 2/4 drug classes (Beta-
blocker, Anti-convulsants, Tricyclic anti depressant, Calcium channel
blocker)
Medication overuse headache (MOH)
Overused acute medication > 10 / or 15 days per months more than 3 months
why 15 days cut-off point?
Schulman EA et al. Headache 2008;48:778-782)
AEDs used in
Episodic migraine
S.D. Silberstein, et al. Neurology 2012;78;1337
AAN/AHS 2012
Sodium valproate/Divalproex sodium
1975: Welch et al. reported change in CSF GABA levels
during migraine episodes in humans
Valproate enhances GABAergic transmission (highly
pleiotropic), blocks Na channels and
Early studies
1988; Sorensen et al. reported 11/22 pt. with migraine
become headache free during 1200 mg valproate
1992; Hering & Kurtzky: the rst D-B, P-C, valproate 800
mg/d for migraine prophylaxis
Approved by FDA for the management of migraine
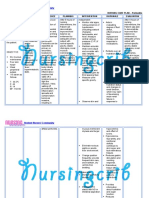
Clinical studies of AEDs for migraine prophylaxis
Study design and
period of treatment
N
Headache
type
Results Results
D-B, P-C (8 weeks)
(1992)
32
MwoA and
MwA
400 mg
Reduction in migraine freq., intensity and
duration in 80% of the treated group
Multicenter,
randomised, D-B,
P-C (8 weeks)
(1995))
107
Migraine
not specic
Adjust to
serum level of
70-120 mg/l
>50% reduction in migraine freq. No SEs
on headache intensity/duration
Multicenter,
randomised, D-B,
P-C, (8 weeks)
(1997)
171
MwoA and
MwA
500 mg;1000
mg;1500 mg
Reduction in freq/ greater in 1000 mg
Randomised, D-B,
P-C (2002)
237
MwoA and
MwA
500-1000 mg
extended
release
Reduction in 4 week migraine rate
Sodium valproate/valproic acid
Divalproex sodium in migraine
prophylaxis
0
12.5
25
37.5
50
Placebo
Divalproex Na
P
a
t
i
e
n
t
s
(
%
)
P<0.001
P<0.05 (Dose 500
-1500 mg)
Methew NT et al. ARCH Neurol 1995 Klapper J Cephalalgia 1997
48%
14%
% pt. > 50% HA freq. reduction in 12 weeks
14%
44%
Caution in VA used
Child bearing age
Adverse events that can cause discontinuation from
long term safety study = 21%
alopecia (6%)
tremor (2%)
weight gain (2%)
vomiting (5%)
Divalproate vs Amitriptyline: RCT trial
300 migraine DVA-ER vs AMT
Kalita J et al. Acta Neurol Scand 2013: 128: 6572
Divalproate vs Amitriptyline: RCT trial
Kalita J et al. Acta Neurol Scand 2013: 128: 6572
Topiramate
Acts on AMPA receptors, blocking the glutamate
binding site, but also blocks kainate receptors
and Na+ channels, and enhances GABA
currents (highly pleiotropic*)
Studies of TPM in migraine
2001: double-blind placebo control trial
Storey JR et al. Headache 2001 41, 968-975
Clinical studies of AEDs for migraine prophylaxis
Study design and
period of treatment
N
Headache
type
Results Results
Single-center,
randomised, D-B,
P-C (8 weeks)
(2001)
35
MwoA and
MwA
100-200 mg
Reduction in mean 28 day HA freq. (36%
vs 14%)
Multicenter,
randomised, D-B,
P-C (18 weeks)
(2004)
483
MwoA and
MwA
50 mg;100 mg;
200 mg
Reduction in mean monthly migraine freq.
(TPM 100 and 200 mg)
Multicenter,
randomised, D-B,
P-C, parallel group
(18 weeks) (2004)
487
MwoA and
MwA
50 mg;100 mg;
200 mg
Reduction in mean monthly migraine freq.
(TPM 100 and 200 mg)
Multicenter,
randomised vs
propranolol or
placebo (18
weeks) (2004)
575
MwoA and
MwA
100 mg; 200
mg; vs
propranolol
Reduction freq., monthly migraine day
100 mg TPM vs PPN: similar efcacy
Topiramate
Topiramate in migraine prevention
(Large Controlled Trial)
26-weeks, double-blind, placebo controlled
487 EM patient, TPM 50, 100, 200 mg vs placebo
Silberstein SD. Arch Neurol. 2004;61:490-495
Topiramate in migraine prevention
(Large Controlled Trial)
Silberstein SD. Arch Neurol. 2004;61:490-495
331 subjects (172 TPM vs 159 AMT) dose titration
25 to 100 mg/d
Primary outcome: change from baseline in the
mean monthly no. of migraine episode: NS
Secondary outcome: functional ability, QoL: NS
Outcome: NS
DW Docick et al. Clinical therapeutic 2009;31(3):542-559
Percent weight change from baseline between
TPM vs AMT
Efcacy of Gabapentin in migraine
prevention (EM): D-B, P-C study
0
12.5
25
37.5
50
Gabapentin (n=56) Placebo (n=31)
46%
16%
P<0.05 ITT population
TID dosing
Gabapentin titrated to 2400 mg/d
% of patients with > 50% reduction
in attack frequency (4 weeks)
Mathew et al. Headache 2001
Conclusion EM prevention
1. Evidence based: AAN/AHS guideline
2. All Level A recommendation has similar efcacy,
but different side effect
3. Most DBPC studies evaluated efcacy 3-6 months
4. Long term used still save in some studies
Preventive medication
in chronic migraine
Brain change in chronic
migraine
Structural brain change
Periaqueductal grey
matter change (PAG): iron
deposition
Functional brain change
Central sensitisation
Central sensitization of
Trigeminal nucleus
caudalis(TNC)
Summary of evidence for prophylactic medications in
undifferentiated chronic daily headache and chronic migraine
Treatment Evidence for use in CDH/CM
Anticonvulsants
Topiramate Double-blind, placebo-controlled trial in CM
Gabapentin One double-blind, placebo-controlled trial in CDH
Valproate Double-blind, placebo-controlled in CDH including CM
Antidepressants
Amitriptyline Small open-labeled trial in TM
Fluoxetine Small double-blind, placebo-controlled trial in CDH
Tizanidine Small double-blind, placebo-controlled trial in CDH
Onabotulinumtoxin A Double-blind, placebo controlled trial in CM
Randomized, placebo-controlled, parallel-group
16 weeks
Topiramate 100 mg/d vs placebo
306 pts included (153 topiramate vs 153 placebo)
SD Silberstein Headache 2007;47:170-180
17+/- 5.4 17+/- 5.0
Primary outcome
Topiramate Placebo
Migraine/Migraine days
Baseline+/- SD
-6.4+/- 5.8
-4.7+/- 6.1
P=0.01
-1
-2
-3
-4
-5
-6
-7
Change from baseline in monthly (28 day) rate of
migraine/migraine days
SD Silberstein Headache 2007;47:170-180
The effect of sodium valproate on
CDH, and its subgroups
Yurekli VA. J Headache Pain 2008; 9:3741
Double-blind, Placebo-controlled 70 CDH; 29 CM, and 41 CTTH
Sodium valproate 500 mg(1st wk) to 1000 mg ; 3 months f/u
Medication overuse
headache
(6) Topiramate 100 mg (up to 200 mg) per day is probably
effective in the treatment of MOH
(7) Corticosteroid (at least 60 mg prednisolone) and amitryptyline
(up to 50 mg) are possibly effective in treatment to withdrawal
symptoms
Conclusion: CM +/- MOH
Few strong evidence of preventive medication
used in CM/MOH
TPM -> CM/MOH, BTx->CM
In clinical practice, may use medication based on
EM evidence, comorbitity, cost, preference
Although widely use of combination therapy, the
strong evidence is still lacking
Migraine variants
Fact
Most of studied migraine prevention was done in
MwoA/MwA
Few studies done in migraine variant: only case
series/report
Recommended drug sometime can not be applied
in migraine variants prevent
Evidence of preventive drugs for FHM/SHM
Drug Standard dosage Study group Outcome
Flunarizine 10 mg daily FHM/SHM
Reduce attack
freq 85 %
Verapamil 120-240 mg/d FHM/SHM
Pain free/reduce
freq and severity
Sodium valproate 500-2,000 mg/d HM with epilepsy
Reduce attacks
freq.
Lamotrigine 100-500 mg/d
Migraine with
disabling aura
(incl. HM)
Reduce freq. after
3-6 months
Acetazolamide 250-1,000 mg/d HM
Reduce attack
freq.
Topiramate in HM
TPM in HM has not been described
AEDs for acute migraine
therapy
600 - 1200 mg can be used if oral
acute medication failed
Conclusion
Start Evaluation Stop
Migraine is a complex neurological disorder
Multimodality treatment is needed to prevent migraine
chronic transformation
AEDs is one of the effective migraine prevention
Thank you
FB: openneurons
Вам также может понравиться
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryОт EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryРейтинг: 3.5 из 5 звезд3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)От EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Рейтинг: 4.5 из 5 звезд4.5/5 (121)
- Never Split the Difference: Negotiating As If Your Life Depended On ItОт EverandNever Split the Difference: Negotiating As If Your Life Depended On ItРейтинг: 4.5 из 5 звезд4.5/5 (838)
- The Little Book of Hygge: Danish Secrets to Happy LivingОт EverandThe Little Book of Hygge: Danish Secrets to Happy LivingРейтинг: 3.5 из 5 звезд3.5/5 (400)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaОт EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaРейтинг: 4.5 из 5 звезд4.5/5 (266)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeОт EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeРейтинг: 4 из 5 звезд4/5 (5795)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreОт EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreРейтинг: 4 из 5 звезд4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyОт EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyРейтинг: 3.5 из 5 звезд3.5/5 (2259)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersОт EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersРейтинг: 4.5 из 5 звезд4.5/5 (345)
- The Emperor of All Maladies: A Biography of CancerОт EverandThe Emperor of All Maladies: A Biography of CancerРейтинг: 4.5 из 5 звезд4.5/5 (271)
- Team of Rivals: The Political Genius of Abraham LincolnОт EverandTeam of Rivals: The Political Genius of Abraham LincolnРейтинг: 4.5 из 5 звезд4.5/5 (234)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceОт EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceРейтинг: 4 из 5 звезд4/5 (895)
- Basic Movement Disorder ApproachДокумент96 страницBasic Movement Disorder ApproachSurat Tanprawate100% (18)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureОт EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureРейтинг: 4.5 из 5 звезд4.5/5 (474)
- The Yellow House: A Memoir (2019 National Book Award Winner)От EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Рейтинг: 4 из 5 звезд4/5 (98)
- The Unwinding: An Inner History of the New AmericaОт EverandThe Unwinding: An Inner History of the New AmericaРейтинг: 4 из 5 звезд4/5 (45)
- Acute Migraine Management, Chiangmai 2015Документ60 страницAcute Migraine Management, Chiangmai 2015Surat Tanprawate100% (1)
- Neurological Examination - Pre-Med - 401Документ73 страницыNeurological Examination - Pre-Med - 401Surat Tanprawate100% (4)
- Bonus BTR CompiledДокумент373 страницыBonus BTR Compiledbhaskarjya58Оценок пока нет
- Headache Tutorial - Neuro Essential CMU2020Документ66 страницHeadache Tutorial - Neuro Essential CMU2020Surat Tanprawate100% (4)
- Approach To Movement DisorderДокумент12 страницApproach To Movement DisorderSurat Tanprawate100% (1)
- NCLEX Strategy QuestionsДокумент9 страницNCLEX Strategy QuestionsPaulo de Jesus100% (1)
- Neuro Ophthalmology For Med Student - 2016Документ120 страницNeuro Ophthalmology For Med Student - 2016Surat Tanprawate100% (3)
- Physical Exam For DiagnosisДокумент61 страницаPhysical Exam For DiagnosisSurat Tanprawate100% (3)
- Physical Exam For DiagnosisДокумент61 страницаPhysical Exam For DiagnosisSurat Tanprawate100% (3)
- Neuro OphthalmologyДокумент114 страницNeuro OphthalmologySurat TanprawateОценок пока нет
- Von Willebrand DiseaseДокумент9 страницVon Willebrand DiseaserandyОценок пока нет
- Piriformis SyndromeДокумент8 страницPiriformis SyndromelewienОценок пока нет
- New Era in Migraine Management - 2019 - HatYaiДокумент77 страницNew Era in Migraine Management - 2019 - HatYaiSurat Tanprawate100% (3)
- Lecture 1 - Principles of Newborn ResuscitationДокумент29 страницLecture 1 - Principles of Newborn ResuscitationShane Lim GarciaОценок пока нет
- Cycloid Psychosis An Examination of The Validy of The ConceptДокумент9 страницCycloid Psychosis An Examination of The Validy of The ConceptjoaogarcesОценок пока нет
- Headache Case Seminar - RCPTДокумент25 страницHeadache Case Seminar - RCPTSurat TanprawateОценок пока нет
- Headache Case Seminar - RCPTДокумент25 страницHeadache Case Seminar - RCPTSurat TanprawateОценок пока нет
- Principle of ElectroDx by Dr. Angkana Nudsasarn, Chiang Mai UniversityДокумент113 страницPrinciple of ElectroDx by Dr. Angkana Nudsasarn, Chiang Mai UniversitySurat Tanprawate100% (3)
- NCP Ineffective Breathing ActualДокумент3 страницыNCP Ineffective Breathing ActualArian May Marcos100% (1)
- Headache in Emergency ConditionДокумент34 страницыHeadache in Emergency ConditionSurat TanprawateОценок пока нет
- Nursing Care Plan For Peritonitis NCPДокумент2 страницыNursing Care Plan For Peritonitis NCPderic86% (7)
- RAPDДокумент2 страницыRAPDAlpascaFirdausОценок пока нет
- Neuro-Ophthalmology - Third Year Student - 2018Документ126 страницNeuro-Ophthalmology - Third Year Student - 2018Surat TanprawateОценок пока нет
- Headche:Dizzy Med Stud - 2016Документ51 страницаHeadche:Dizzy Med Stud - 2016Surat TanprawateОценок пока нет
- Status Epilepticus PathophysiologyДокумент22 страницыStatus Epilepticus PathophysiologySurat TanprawateОценок пока нет
- Migraine SubtypeДокумент55 страницMigraine SubtypeSurat Tanprawate100% (1)
- Pre-Extern Tutorial, 14Документ68 страницPre-Extern Tutorial, 14Surat Tanprawate100% (2)
- Headache You Should Know - SuratДокумент33 страницыHeadache You Should Know - SuratSurat Tanprawate100% (2)
- MS and NMO Update From ECTRIMS - Boston 2014 PDFДокумент43 страницыMS and NMO Update From ECTRIMS - Boston 2014 PDFSurat TanprawateОценок пока нет
- HIV Neurology, 2014Документ62 страницыHIV Neurology, 2014Surat Tanprawate100% (2)
- Neuro Ophthalmology PDFДокумент70 страницNeuro Ophthalmology PDFSurat Tanprawate100% (4)
- Neurologic Examination PDFДокумент90 страницNeurologic Examination PDFhirsi200518Оценок пока нет
- Migraine Management, Songkra Hospital 13Документ53 страницыMigraine Management, Songkra Hospital 13Surat Tanprawate50% (2)
- Carcinoma Uterus - Amita MaheshwariДокумент42 страницыCarcinoma Uterus - Amita MaheshwariMochammad Rizal AttamimiОценок пока нет
- Pericarditis: Dr. Alfredo Gonzales SaavedraДокумент38 страницPericarditis: Dr. Alfredo Gonzales SaavedraSandy Burgos CabanillasОценок пока нет
- Research Proposal DoneДокумент8 страницResearch Proposal DoneLoveu GoОценок пока нет
- Heterogeneity of Cardio-Facio-Cutaneous Syndrome: Editorial CommentДокумент1 страницаHeterogeneity of Cardio-Facio-Cutaneous Syndrome: Editorial CommentSarly FebrianaОценок пока нет
- Hormonal Imbalance and Its Causes in Young Females: January 2015Документ6 страницHormonal Imbalance and Its Causes in Young Females: January 2015figgernaggotОценок пока нет
- IMUNOterapi HCCДокумент12 страницIMUNOterapi HCCAri Dwi PrasetyoОценок пока нет
- AtaxiaДокумент10 страницAtaxiaosakaОценок пока нет
- Guillain-Barré Syndrome (GBS) : Prepared by Dr. Madiha Anees PT Asst. Prof/VP RCRS MS-PT, BS-PTДокумент26 страницGuillain-Barré Syndrome (GBS) : Prepared by Dr. Madiha Anees PT Asst. Prof/VP RCRS MS-PT, BS-PTaneelala kanwal kanwalОценок пока нет
- ScriptДокумент1 страницаScriptSherlyn Miranda GarcesОценок пока нет
- Maternal and ChildДокумент6 страницMaternal and Childgunn twothingОценок пока нет
- Assignment OneДокумент2 страницыAssignment OnefulcaОценок пока нет
- Guidelines TX of HPNДокумент3 страницыGuidelines TX of HPNjheyfteeОценок пока нет
- Lombok Immunizationand Traveller231017-Dr - Agus SomiaДокумент63 страницыLombok Immunizationand Traveller231017-Dr - Agus Somiarinaldy IX9Оценок пока нет
- FFFFFFF: Health Declaration Form Health Declaration Form Health Declaration FormДокумент1 страницаFFFFFFF: Health Declaration Form Health Declaration Form Health Declaration FormLeny Goyo LaurenteОценок пока нет
- Hypocalcemia: Author: Christopher B Beach, MD, FACEP, FAAEM, Associate Professor and ViceДокумент65 страницHypocalcemia: Author: Christopher B Beach, MD, FACEP, FAAEM, Associate Professor and ViceronelnОценок пока нет
- Anticoagulants and Antiplatelet AgentsДокумент4 страницыAnticoagulants and Antiplatelet AgentsMark Russel Sean LealОценок пока нет
- CCFRG Second Batch Module Ii Dec1 2 L03 FinalДокумент4 страницыCCFRG Second Batch Module Ii Dec1 2 L03 FinalShivya MollyОценок пока нет
- Lips Diseases and Its Management: Classification of Lip DisordersДокумент17 страницLips Diseases and Its Management: Classification of Lip DisordersSubhash VermaОценок пока нет
- V 5 N 1Документ190 страницV 5 N 1Jorge RodriguezОценок пока нет
- Gosssypiboma: Dr. B.V AmruthavalliДокумент3 страницыGosssypiboma: Dr. B.V AmruthavalliInternational Organization of Scientific Research (IOSR)Оценок пока нет
- ECG NotesДокумент7 страницECG NotesShams NabeelОценок пока нет