Академический Документы
Профессиональный Документы
Культура Документы
Efectos Relativos de La Inmersión y Aumento de La Presión Sobre La Mecánica Respiratoria, El Trabajo y El Costo de Energía de La Respiración en Personas
Загружено:
Rorschach77Исходное описание:
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Efectos Relativos de La Inmersión y Aumento de La Presión Sobre La Mecánica Respiratoria, El Trabajo y El Costo de Energía de La Respiración en Personas
Загружено:
Rorschach77Авторское право:
Доступные форматы
Relative effects of submersion and increased pressure on respiratory
mechanics, work, and energy cost of breathing
Heather E. Held and David R. Pendergast
Center for Research and Education in Special Environments, Department of Physiology and Biophysics, State University of
New York at Buffalo, Buffalo, New York
Submitted 10 May 2012; accepted in nal form 7 January 2013
Held HE, Pendergast DR. Relative effects of submersion and
increased pressure on respiratory mechanics, work, and energy cost of
breathing. J Appl Physiol 114: 578591, 2013. First published Janu-
ary 10, 2013; doi:10.1152/japplphysiol.00584.2012.Submersion
and increased pressure (depth) characterize the diving environment
and may independently increase demand on the respiratory system. To
quantify changes in respiratory mechanics, this study employed a
unique protocol and techniques to measure, in a hyperbaric chamber,
inspiratory and expiratory alveolar pressures (interrupter technique),
inspiratory and expiratory resistance in the airways (Raw
I
and Raw
E
,
esophageal balloon technique), nitric oxide elimination (thought to
correlate with Raw), inspiratory and expiratory mechanical power of
breathing, and the total energy cost of ventilation. Eight healthy adult
men underwent experiments at 1, 2.7, and 4.6 atmospheres absolute
(ATA) in dry and fully submersed conditions. Subjects rested, cycled
on an ergometer at 100 W, and rested while voluntarily matching their
ventilation to their own exercise hyperpnea (isocapnic simulated
exercise ventilation). During isocapnic simulated exercise ventilation,
increased O
2
uptake (above rest values) resulted from increased
expired ventilation. Raw
I
decreased with submersion (mean 43%
during rest and 20% during exercise) but increased from 1 to 4.6 ATA
(19% during rest and 75% during exercise), as did Raw
E
(53%
decrease with submersion during rest and 10% during exercise; 9%
increase from 1 to 4.6 ATA during rest and 66% during exercise).
Nitric oxide elimination did not correlate with Raw. Depth increased
inspiratory mechanical power of breathing during rest (40%) and
exercise (20%). Expiratory mechanical power of breathing was
largely unchanged. These results suggest that the diving environment
affects ventilatory mechanics primarily by increasing Raw, secondary
to increased gas density. This necessitates increased alveolar pressure
and increases the work and energy cost of breathing as the diver
descends. These ndings can inform physician assessment of diver
tness and the pulmonary risks of hyperbaric O
2
therapy.
alveolar pressure; airway resistance; nitric oxide; exercise; diving
THE DIVING ENVIRONMENT demands more of the ventilatory system
than the terrestrial environment because static lung loading (SLL)
is often imposed during submersion, and breathing gas density
increases as a function of depth. These factors increase the work
of breathing and may limit exercise performance in healthy divers
or present unexpected risks in patients undergoing hyperbaric O
2
therapy (HBOT).
Many studies have assessed the effects of the diving environ-
ment on the work of breathing and outlined changes imposed on
ventilation by diving. SLL is imposed when the source of breath-
ing gas is at a hydrostatic pressure different from that of the chest
centroid (54). Negative SLL is typical and is encountered by
divers in a head-up orientation (36), when the breathing gas is at
less pressure than the chest. Negative SLL places greater demand
on the inspiratory muscles. In addition, when the body is im-
mersed, blood that normally pools in the extremities translocates
to the thorax (17), decreasing total lung capacity, residual volume
(17, 41, 53), and lung compliance (17). These changes increase
the elastic work of breathing. Additional blood in the thorax may
confer a small benet, however, by increasing the ability to
generate pressure in the airways. Since blood is essentially incom-
pressible, less work may be lost to compression during maximal
expiratory pressure (P
Emax
) maneuvers. The effects of submersion
on respiratory muscle efciency, however, remain unknown.
Increased depth affects respiratory mechanics in several ways.
Work of breathing increases as a function of depth, primarily due
to increased airway resistance (Raw) secondary to increased gas
density (38). Historically, Raw was measured using the pressure
differential between the mouth and an air-lled balloon placed
within the lower third of the esophagus (46). Recently, clinical
practice has shifted to measuring Raw by modifying the P
0.1
technique, which was rst developed by Otis and Proctor (45).
Use of this technique involves brief interruption of airow, and
pressure in the system is taken to approximate alveolar pressure
(PA). This indicates the degree of respiratory muscle activation
(26) and central nervous system respiratory drive (60). Raw can
be calculated by dividing the pressure differential between the
alveoli and the mouth by the ow rate immediately prior to
occlusion. Raw values at sea level assessed by the P
0.1
technique
are comparable to those obtained by the traditional esophageal
balloon technique (30, 40), and the P
0.1
technique has been used
to assess Raw during simulated dives at depths up to 45 atmo-
spheres absolute (ATA) (12). To our knowledge, however, the
P
0.1
and esophageal balloon techniques have not been compared
during wet simulated dives.
Another recent development in pulmonary mechanics is a
more thorough understanding of the role of nitric oxide (NO),
a free radical that induces smooth muscle relaxation. Raw may
be reduced by NO production (V
NO) (2), and animal studies
have shown that production or administration of NO decreases
Rawin a dose-dependent manner (21, 27). However, the effects of
diving on V
NO in human divers have not been reported, and the
relationship between Raw and V
NO has not been examined. It is
particularly important to study the effect of depth on V
NO, because
there is evidence that V
NO is associated with maintenance of tissue
normoxia (6), and it has been observed that V
NO in the cerebral
vasculature decreases with depth as PO
2
rises (20). If V
NO is
similarly regulated in airway smooth muscle, the decrease in V
NO
could result in bronchoconstriction and could be expected to
exacerbate the increase in Rawwith increasing depth. To maintain
alveolar ventilation, it is likely that increases in Raw demand
concurrent increases in PA. Thus it is important to measure the
Address for reprint requests and other correspondence: H. E. Held, Hyper-
baric Biomedical Research Laboratory, Molecular Pharmacology & Physiol-
ogy, College of Medicine, Univ. of South Florida, 12901 Bruce B. Downs
Blvd., MDC 8, Tampa, FL 33612 (e-mail: hheld1@health.usf.edu).
J Appl Physiol 114: 578591, 2013.
First published January 10, 2013; doi:10.1152/japplphysiol.00584.2012.
8750-7587/13 Copyright 2013 the American Physiological Society http://www.jappl.org 578
effect of depth on V
NO to form a more complete understanding of
how respiratory mechanics change in the diving environment.
Interestingly, depth may provide some benet to respiratory
muscle function. Because gas in the lungs at depth is com-
pressed relative to gas at sea level, less work may be lost to
compression of the gas during P
Emax
maneuvers, and higher
pressures may be generated.
Many early studies sought to maximize the depth at which
humans could operate, but more recent studies have attempted
to improve diver performance at more moderate depths. To do
so, it is important to clearly dene the effects of the diving
environment on respiratory mechanics.
The purpose of this study was to describe the effects of sub-
mersion and increased gas density (depth) on respiratory mechan-
ics, with a particular emphasis on correlating newer methods (e.g.,
P
0.1
measurement and V
NO calculation) with established measures
of pulmonary mechanics during diving. These ndings will create
a more complete picture of the effects of submersion and depth on
ventilation, which is important not only for improving diver
performance, but also for making a more thorough medical
assessment of tness to dive and determination of whether HBOT
is appropriate for patients with respiratory systems compromised
by disease or injury.
We hypothesized that submersion would increase P
Emax
while increased pressure would 1) decrease V
NO, 2) increase
Raw because of the increase in gas density and the decrease in
V
NO, 3) increase PA and, thereby, increase the respiratory work
rate, 4) increase the O
2
cost of breathing, and 5) increase P
Emax
.
Glossary
ATA Atmospheres absolute
FEV
1
Forced expiratory volume in 1 s
FI
CO
2
Fraction of CO
2
in inspired gas
FVC Forced vital capacity
HBOT Hyperbaric O
2
therapy
ISEV Isocapnic simulated exercise ventilation
MVV
15
Maximum voluntary ventilation in 15 s (l/min)
NO Nitric oxide
NOA NO analyzer
PA Alveolar pressure
PA
E
Expiratory PA
PA
I
Inspiratory PA
P
Emax
Maximal expiratory pressure at the mouth
P
es
Pleural pressure measured by esophageal balloon
P
mouth
Pressure at the mouth
Q
Cardiac output
Raw Resistance in the airways
Raw
E
Expiratory Raw measured at peak ow using the
esophageal balloon technique
Raw
I
Inspiratory Raw measured at peak ow using the
esophageal balloon technique
R
int
Raw measured by the P
0.1
technique
R
intE
Expiratory R
int
R
intI
Inspiratory R
int
SVC Slow vital capacity
V
CO
2
CO
2
production
VC Vital capacity
V
E Minute ventilation
V
NO NO elimination
V
O
2
O
2
consumption
V
O
2B
O
2
cost of breathing
V
O
2peak
Peak V
O
2
W
Respiratory work rate (power)
W
E
Expiratory W
(power)
W
I
Inspiratory W
(power)
METHODS
The study protocol was approved by the Universitys Health
Sciences Institutional Review Board, and the volunteer subjects pro-
vided written informed consent before participating in the study.
Subjects. Eight male certied SCUBA divers were recruited from
the local diving population. At the start of the study, they were 28
8 (SD) yr old with an average weight of 81 12 kg and height of
179 4 cm. A physical examination, including a chest X-ray and
pulmonary function tests, was performed (Table 1). A medical history
was obtained to exclude current or previous illness of consequence.
Volunteers with abnormal pulmonary function tests were excluded
from the study. All subjects were nonsmokers, but subject 10 had a
history of smoking (1 pack/day for 9 yr) ending 2 yr prior to
enrollment in the study and subsequently chewed tobacco.
Experimental procedure. Six experiments were performed in each
subject: in dry and submersed conditions, at three simulated depths (1,
2.7, and 4.6 ATA). The order of the experiments was randomized,
with the exception that each subjects rst experiment was performed
in the dry condition to allow familiarization with the protocol and
techniques. Prior to the start of each experiment, each subject was
outtted with a three-lead ECG and a thin balloon-tipped catheter
[100-mm balloon (Nolato, Torekov, Sweden) attached to 0.034-in. ID
polyethylene tubing]. The balloon was passed through a nostril until
it sat within the lower third of the esophagus (42 cm from the nostril
to the tip of the balloon) and was inated with 0.5 cm
3
of air upon
reaching the designated pressure. Proper placement was veried by
Table 1. Anthropometrics and pulmonary function test results
Subj No. Age, yr Height, cm Weight, kg SVC, liters
Submersed
SVC, liters
FVC,
liters
FEV1,
liters FEV1/FVC, %
MVV15,
l/min
V
O2peak,
ml min
1
kg
1
Submersed
V
O2peak,
ml min
1
kg
1
1 45 178 104 4.99 3.8 4.84 3.75 77 119 30 25
4 26 183 75 6.77 5.5 5.88 5.42 92 225 38 32
5 27 178 70 6.00 4.2 6.00 5.37 90 181 47 44
6 23 180 79 5.50 4.5 5.38 4.72 88 204 37 35
7 36 181 86 5.02 4.0 4.86 4.33 89 104 31 31
10 26 170 66 4.82 4.4 4.85 4.30 89 198 38 31
11 24 180 89 5.21 4.6 5.21 4.34 83 179 31 28
12 20 178 77 5.69 4.4 5.69 5.14 90 213 36 33
SVC, slow vital capacity; FVC, forced vital capacity; FEV1, forced expiratory volume in 1 s; MVV15, maximum voluntary ventilation in 15 s; V
O2peak, peak
O2 consumption. All values are in the dry condition, except where noted as submersed.
579 Effects of Submersion and Pressure on Respiratory Mechanics Held HE et al.
J Appl Physiol doi:10.1152/japplphysiol.00584.2012 www.jappl.org
observation of increasingly negative pressure during a deep, slow
inspiration.
During experiments, subjects sat on a cycle ergometer behind a
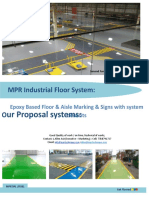
Lanphier-Morin barrier system (54) in the hyperbaric chamber (Fig. 1).
During submersion, water was 30.9 0.1C, which is critical water
temperature for resting subjects (16). Thus, subjects likely experienced
near-maximal vasoconstriction of the skin and subcutaneous tissue with-
out increases in metabolic rate while at rest but were thermoneutral
during exercise. The water level was adjusted at the start of the experi-
ment to impose a 15-cmH
2
O SLL.
B
C
D
F
H
N
P
Q
A
R
S
J
G
T
K
O
U
V
L,E
M
W
Mass spectrometer
Gasometer
Collins ergometer
Validyne transducer (Pesophageal)
Validyne transducer (Pmouth)
Solenoid valve
Ohio spirometer
Douglas bag
Bag in barrel
Gas sample line
Mouthpiece
Esophageal catheter
Temperature gauge
NO analyzer
Pressure regulator
Metering valve
Solenoid controller
Barrel
Potentiometer
Humidifier
Mixed Gas
Computer Monitor
A
B
C
D
E
F
G
H
J
K
L
M
N
O
P
Q
R
S
T
U
V
W
-
-
-
-
-
-
-
-
-
-
-
-
-
-
-
-
-
-
-
-
-
-
B
A
b
c
f
e
d
a
Fig. 1. Experimental setup. A: subjects were seated behind the dual-barrier system in the hyperbaric chamber and breathed from a large bag-in-box system. The
half of the chamber occupied by subjects could be ooded and the static lung load (SLL) adjusted by altering the height of the water between the 2 barrier
surfaces. B: expanded view of the subjects body position and relevant pressures: alveolar pressure (estimated by the P0.1 method, a), pleural pressure (estimated
using the esophageal balloon method, b), height of the chest centroid (c), height of the water level (d), distance across which SLL was imposed (15 cmH2O, e),
and ambient (chamber) pressure (f).
580 Effects of Submersion and Pressure on Respiratory Mechanics Held HE et al.
J Appl Physiol doi:10.1152/japplphysiol.00584.2012 www.jappl.org
Each experiment consisted of four 10-min periods of activity: rest,
exercise, recovery, and isocapnic simulated exercise ventilation (ISEV).
During exercise, the subject pedaled the cycle ergometer at 60 5 rpm,
against a work rate of 100 W [O
2
consumption (V
O
2
) 1.80 0.39
l/min, i.e., 59% of subjects peak V
O
2
(V
O
2peak
) determined at 1.0 ATA].
The ergometer controller was set to 25 W less when the subject pedaled
in water to account for the added hydrodynamic drag of pedaling in water
(54). During ISEV, the subject watched a computer screen, which
allowed him to mimic a replay of the ventilation pattern recorded during
his earlier exercise.
Determination of minute ventilation, V
O
2
, and V
NO. Subjects wore
a nose clip and breathed through a mouthpiece connected to two
large-bore (5.1-cm-diameter) hoses, which were part of a bag-in-box
spirometer system. Breathing gas was humidied before reaching a
vinyl reservoir bag. A 55-gallon drum containing a second (Douglas)
bag functioned as the bag-in-box. A spirometer and potentiometer
(Ohio Medical Products, Houston, TX) in the system continuously
recorded volume changes [tidal volumes (VT)]. A mass spectrometer
(MGA 1100, Perkin-Elmer, Pomona, CA) and a NO analyzer (NOA;
Sievers 280i, GE Water and Process Technologies Analytical Instru-
ments, Boulder, CO) continuously sampled gas for composition at the
subjects mouth. The mass spectrometer and the NOA were calibrated
prior to each test. The NOA was calibrated using ltered room air (0
parts per billion NO) and a mixture of known gas concentration (45
parts per million NO). The mass spectrometer was calibrated to O
2
,
CO
2
, and N
2
concentrations using room air (21% O
2
and 78% N
2
) and
two commercially available gas compositions: 100% O
2
and 9% CO
2
in O
2
.
After each collection, exhalate was vented through a dry gas meter
(750 Meter, Rockwell International Meter Division, Pittsburgh, PA)
outside the chamber. A thermocouple (DP-80 Series, Omega Engi-
neering, Stamford, CT) displayed the temperature inside the gas
meter, and the mass spectrometer and NOA sampled a small volume
of gas before it passed through the gas meter.
During experiments at the surface, the gas expelled from the
Douglas bag was sampled through a gas meter (model 506164,
Harvard Apparatus, Holliston, MA). A second mass spectrometer
(MGA 1100, Perkin-Elmer) sampled the gas for composition just
before it entered the gas meter, and a thermistor (Yellow Springs
Instrument, Yellow Springs, OH) measured the temperature. There
was no practical way to sample NO directly with this setup, so a
60-cm
3
syringe was used to draw a gas sample for analysis by the
NOA. Dry and submersed experiments were conducted in exactly the
same manner, with the addition of a tight-tting oronasal mask (as
used in recreational SCUBA diving) with a pass-through port in the
nose for the esophageal balloon tubing during submersion.
Measurement of pressure at the mouth and esophageal pressure. A
pressure transducer (model DP15-28, Validyne Engineering, Northridge,
CA) connected directly to the mouthpiece continuously measured pres-
sure at the mouth (P
mouth
). The transducer sat within a third wide-bore
hose, which allowed its reference port to remain open to ambient pressure
(chamber pressure), even during submersion. A second pressure trans-
ducer (model DP15-30, Validyne Engineering) continuously measured
esophageal pressure (P
es
).
Measurement of PA. PA was measured by a modication of the P
0.1
technique. The subjects mouthpiece was connected to a custom-made
breathing interrupter device, which was designed and built in-house.
The interrupter consisted of a thin metal plate seated in a slotted
plastic housing, which served as a guillotine valve that occluded
airow through the mouthpiece. The plate was driven by a pneumatic
piston (model MRS-012-5DBFGUEE1JJ, Bimba Manufacturing,
Monee, IL) connected by two pressurized air lines to a solenoid valve
(model 125-4E1, Humphrey Products, Kalamazoo, MI). A computer-
ized controller, designed and built in-house, directed the timing of
guillotine valve operation by activating the solenoid valve. The piston
housing held a magnet, which signaled when the piston was fully
extended (occlusion complete). This signal was recorded by the data
acquisition system for verication of occlusion during data analysis.
Occlusion began 100 ms after the onset of inhalation or exhalation,
occurred in 2 ms, and lasted 150 ms. These characteristics were
chosen because they are similar to the closure characteristics of
commercially available devices (48). Pressure excursions were mea-
sured by the P
mouth
transducer and recorded as described below (see
Data collection).
ISEV pacing. During exercise gas collection, a software program
(written in-house) recorded the spirometer volume signal. At 30 s
after the start of the collection, the subject performed a vital capacity
(VC) maneuver, which provided volume reference values for use dur-
ing ISEV.
The gas mixtures for ISEV were designed to maintain normocapnia
and contained 4.20 0.17% (mean SE) CO
2
at 1 ATA, 1.67
0.04% CO
2
at 2.7 ATA, and 0.95 0.01% CO
2
at 4.6 ATA. The gas
mixtures also included 21% O
2
, and the remaining fraction was N
2
.
The computer software that was used to record the subjects breathing
pattern during exercise simultaneously displayed, on a computer
screen in front of the subject, the earlier recording and the current
breath-to-breath volume changes of the spirometer. This allowed the
subject to mimic the earlier recording and, thereby, simulate his own
exercise breathing. The subject directly followed the pace on the
computer screen while an investigator outside the chamber visually
conrmed that he adhered to the recorded pattern. The subject per-
formed a VC maneuver at the same time as the recorded tracing
displayed VC, which allowed the investigator to adjust the baseline of
the real-time spirometer display so that it and, therefore, the subjects
end-expiratory lung volume were the same as during exercise.
Cardiac output. Cardiac output (Q
) was measured using a portable
cardiac measurement device (Finometer model 1, Finapres Medical
Systems, Amsterdam, The Netherlands). Because there was no way to
render the device safe for hyperbaric exposure or the presence of
water, the device was used only in the dry condition at 1 ATA.
Furthermore, only the nal four subjects were tested with the device.
Data collection. A data acquisition system (MP150, BIOPAC
Systems, Goleta, CA) recorded data for analysis. The signal from the
spirometer, the P
mouth
transducer, P
es
transducer, ECG signal, frac-
tions of O
2
and CO
2
, concentration of NO, and interrupter signal were
continuously output to the data acquisition system. Phase differences
among the recorded variables (e.g., between P
mouth
and P
es
or between
P
mouth
and O
2
concentration) were identied and corrected during
data analysis.
Compression and decompression schedules. US Navy compression
and decompression schedules (42) were used conservatively in the
dives. No decompression-related health problems were encountered.
V
O
2peak
testing. V
O
2peak
was determined at 1 ATA on the same
cycle ergometer (pedaling rate 60 rpm) used for the experiments
described above. The mouthpiece for determination of V
O
2peak
was
the same as that described above, except it did not include the
interrupter device or pressure transducers. Subjects wore heart rate
monitors (model 810i T61, Polar, Kempele, Finland). Before and after
the test, blood drawn from a nger prick was analyzed for lactate
(Accutrend Lactate, Roche Diagnostics, Mannheim, Germany).
Subjects initially pedaled at 50 W for 3 min and then at 100 and
150 W for 2 min each. The work rate was subsequently increased by
25 W every 2 min until the subject reached exhaustion. Frequency of
breathing (f) and maximum heart rate were recorded at each work rate.
Exhalate from the last minute of each work rate was collected and
analyzed for volume, temperature, and gas composition using the
equipment described above.
Subjects performed the test once in the dry condition and once
while fully submersed in water. As described above, the ergometer
was set to a work rate that was 25 W less than the corresponding dry
work rate. Subjects wore diving face masks and nose clips while
submersed.
Subjects were considered to have reached maximum V
O
2
if at least
two of the following three criteria were met: 1) the increase in V
O
2
581 Effects of Submersion and Pressure on Respiratory Mechanics Held HE et al.
J Appl Physiol doi:10.1152/japplphysiol.00584.2012 www.jappl.org
between the last gas collection and the gas collection preceding it
was 150 ml O
2
; 2) the concentration of blood lactate following
exercise was 4.0 mmol/l; and 3) the respiratory exchange ratio [CO
2
production (V
CO
2
)/V
O
2
] for the last collection was 1.15. Most
subjects did not fulll these criteria and, thus, were considered to have
reached V
O
2peak
under these conditions, as opposed to a true maxi-
mum.
Calculations. Minute ventilation (V
E) and V
O
2
were calculated
using standard equations (13) and are presented in liters at standard
temperature dry at ambient (chamber) pressure. V
NO was calcu-
lated using an equation adapted from that for V
CO
2
(13). PA was
calculated from the P
mouth
interruption data as described by Pao et al.
(48), because this method of calculation generates reproducible values
and is similar to calculations performed by commercially available
devices (48). Briey, PA was determined by application of a linear
regression to the region of increasing pressure in the P
mouth
signal
following the initial upstroke (expiration) or downstroke (inspiration).
A second line was drawn perpendicular to the x-axis (time) at the time
of closure [assumed to be complete at 25% of the overall rise (50)],
and the slope from the linear regression was used to extrapolate back
to the time of closure. The value of the regression at the time of
closure was taken as PA. Interrupter pressure curves that displayed
reduced pressures prior to reopening of the interrupter were discarded,
because leakage at the mouth could not be ruled out. Raw (P
0.1
method) was calculated using the standard equation [R
int
(PA
P
mouth
)/ow]. Flow was the time derivative of volume at the onset of
occlusion, and P
mouth
was the pressure immediately prior to occlusion.
Raw (esophageal balloon method) was calculated using the standard
equation (13) [R
aw
(P
mouth
P
es
)/ow] at the time of peak ow
during each breath.
Calculation of the work of breathing was based on long-established
methods where the work of breathing is taken as the area within the
pleural pressure-VT loop (46). Here, the work of breathing per minute
(power) was calculated from the product of ow and the pressure
differential between P
es
and P
mouth
. This product was plotted vs. time,
and the area was taken to provide work per breath. This was multi-
plied by f to provide work per minute (W
). One limitation of this
technique is that a portion of the work of breathing falls outside the
loop, which leads to a slight underestimation of the work of breathing
and prohibits separation of work into elastic and resistive components.
O
2
cost of breathing and respiratory muscle efciency. The abso-
lute O
2
cost of breathing (V
O
2B
) was calculated in two steps. 1) The
increase in V
O
2
from rest to ISEV was calculated: it was equal to the
difference in V
O
2
from rest to ISEV divided by the difference in V
E
from rest to ISEV. 2) This value was multiplied by V
E during ISEV,
which resulted in the total absolute V
O
2B
for the ventilation pattern
employed during exercise and ISEV. Respiratory muscle efciency
was the work of breathing per minute divided by the absolute V
O
2B
.
Maximal P
mouth
. After the V
O
2
and work of breathing experiment
but prior to decompression, P
Emax
was determined at several different
lung volumes (20, 40, 60, 80, and 100% of VC). Dry (i.e., nonsub-
mersed) VC was determined from the pulmonary function screening
test. VC for submersed experiments was determined by having the
subject perform several VC maneuvers while on the mouthpiece-
spirometer system during rest in the previously described experiment.
The largest peak-to-minimum value recorded from the spirometer was
taken as submersed VC. To perform P
Emax
maneuvers in the wet, the
subject was brought to the barrier interface and seated with the water
level 1 in. above the suprasternal notch, which generated the same
SLL as during the rest of the experiment. Pressures were measured by
a pressure transducer (model DP15-28, Validyne Engineering) and
recorded using the BIOPAC data acquisition system.
Analysis and statistics. Data were analyzed using SigmaPlot 11.0
and SigmaStat 3.5 and are presented as means SE. A two- or
three-way ANOVA was used to determine whether experimental
variables, such as depth, submersion, and effort (i.e., rest, exercise,
and ISEV), interacted or were independent of one another in their
effects on the physiological variables. Differences between groups
were assessed using paired t-tests. If normality and equal variance
tests failed, a signed-rank test was used instead. Statistical signi-
cance was set at P 0.05 for all tests.
RESULTS
Methodological validation. The ISEV phase of the protocol
used in this study was designed to determine the energy cost of
ventilation by quantifying the difference in V
O
2
from rest to
normocapnic hyperpnea at rest. To our knowledge, this is a
unique technique for measuring the O
2
cost of exercise hyper-
pnea. The protocol required six experiments, which in most
cases were conducted over a 6-wk period. This ostensibly
could have produced learning and training effects. Repeated
exercise bouts during the experiments did not, however, affect
V
O
2peak
in the dry or submersed condition (36 2 and 32 2
mlkg
1
min
1
, respectively). Repeated bouts of ISEV within
the same experiment separated by 10 min did not affect V
O
2
during ISEV, which was 308 54 ml/min during the rst
ISEV and 297 38 ml/min during the second ISEV. Similarly,
Q
was not signicantly affected by ISEV (7.3 0.2 l/min vs.
7.2 0.4 l/min at rest), although it increased signicantly
during exercise (17.0 1.2 l/min), as was expected. From
these results, it was concluded that V
E and V
O
2
during ISEV
were not inuenced by learning or training effects and that the
increase in V
O
2
was not due to increased cardiac metabolism
but, rather, to increased V
E alone.
Ventilation and duty cycle. During rest, V
E was unaffected
by submersion (compared with the dry condition) at all depths
tested. In the dry condition, resting V
E increased with increas-
ing depth (20% increase from 1 to 4.6 ATA; Table 2).
During exercise, the effects of submersion and depth were
markedly different from the effects observed at rest: V
E in-
creased with submersion and decreased with depth. Submer-
sion induced a 14% increase in V
E from dry to submersed
conditions at 1 ATA (P 0.033) and a 6% increase from dry
to submersed conditions at 4.6 ATA (P 0.018). As a result
of increasing depth, V
E decreased 11% from 1 to 4.6 ATA
(P 0.015) in the dry condition and 18% from 1 to 4.6 ATA
during submersion (P 0.006).
During ISEV, subjects were successfully paced at exercise
ventilation, as indicated by the absence of signicant differ-
ences in V
E between exercise and ISEV. Therefore, by design,
the effects of submersion and depth on V
E during ISEV
followed the same trends as during exercise: increases with
submersion and decreases with depth.
Changes in V
E resulted from changes in VT and f (Table 2).
At rest, there were no statistically signicant differences in VT
between the dry and submersed conditions; however, VT in-
creased as a function of depth during submersion (26% from 1
to 4.6 ATA, P 0.007). Similarly, during rest, f was unaf-
fected by submersion. Depth had no effect on f, with the
exception of a 16% decrease from 1 to 4.6 ATA during
submersion (P 0.008).
During exercise, trends in VT were similar to those observed
during rest: no change with submersion but an increase with depth
[18% from 1 to 4.6 ATA in the dry condition (P 0.024) and
13% in the submersed condition (P 0.008)]. On the other hand,
the effects of submersion and depth on f during exercise were very
different from the effects observed during rest. During exercise, f
increased with submersion (20% at 1 ATA, P 0.020) and
582 Effects of Submersion and Pressure on Respiratory Mechanics Held HE et al.
J Appl Physiol doi:10.1152/japplphysiol.00584.2012 www.jappl.org
T
a
b
l
e
2
.
R
e
s
p
i
r
a
t
o
r
y
m
e
c
h
a
n
i
c
s
R
e
s
t
E
x
e
r
c
i
s
e
I
S
E
V
D
r
y
S
u
b
m
e
r
s
e
d
D
r
y
S
u
b
m
e
r
s
e
d
D
r
y
S
u
b
m
e
r
s
e
d
1
A
T
A
2
.
7
A
T
A
4
.
6
A
T
A
1
A
T
A
2
.
7
A
T
A
4
.
6
A
T
A
1
A
T
A
2
.
7
A
T
A
4
.
6
A
T
A
1
A
T
A
2
.
7
A
T
A
4
.
6
A
T
A
1
A
T
A
2
.
7
A
T
A
4
.
6
A
T
A
1
A
T
A
2
.
7
A
T
A
4
.
6
A
T
A
V
T
,
l
i
t
e
r
s
0
.
8
6
0
.
1
0
0
.
9
6
0
.
1
3
1
.
0
5
0
.
1
0
0
.
9
3
0
.
1
5
1
.
0
6
0
.
1
3
1
.
1
7
0
.
4
1
1
.
9
3
0
.
1
0
2
.
0
7
0
.
0
9
2
.
2
7
0
.
1
8
2
.
0
5
0
.
0
8
2
.
2
3
0
.
1
7
2
.
3
2
0
.
1
4
2
.
0
1
0
.
0
8
2
.
2
3
0
.
0
8
2
.
3
8
0
.
1
6
2
.
0
9
0
.
1
2
2
.
3
7
0
.
1
8
2
.
4
3
0
.
1
5
f
,
r
e
s
p
i
r
a
t
i
o
n
s
/
m
i
n
1
2
.
4
1
.
7
1
1
.
9
1
.
0
1
3
.
5
1
.
8
1
4
.
7
2
.
6
1
4
.
2
3
.
2
1
2
.
4
2
.
2
*
2
6
.
5
2
.
1
2
5
.
1
2
.
5
2
1
.
2
2
.
4
3
1
.
7
3
.
2
*
2
4
.
4
2
.
9
2
3
.
1
2
.
0
2
6
.
5
2
.
1
2
4
.
6
2
.
8
2
0
.
9
2
.
6
3
1
.
4
3
.
0
*
2
5
.
2
2
.
6
2
3
.
0
2
.
0
E
,
l
/
m
i
n
1
0
.
5
0
.
8
1
1
.
0
0
.
9
1
2
.
7
0
.
9
1
2
.
4
1
.
1
1
1
.
7
1
.
0
1
1
.
8
0
.
5
4
6
.
2
2
.
6
4
2
.
9
3
.
5
4
1
.
0
2
.
3
5
2
.
6
3
.
5
*
4
6
.
6
2
.
4
4
3
.
4
2
.
3
*
4
6
.
1
2
.
2
4
5
.
7
3
.
7
4
0
.
5
3
.
6
5
2
.
9
3
.
3
*
4
7
.
1
2
.
9
4
5
.
2
3
.
0
*
D
u
t
y
c
y
c
l
e
0
.
4
2
0
.
0
1
0
.
4
3
0
.
0
1
0
.
4
1
0
.
0
2
0
.
4
2
0
.
0
2
0
.
4
1
0
.
0
1
0
.
4
0
0
.
0
2
0
.
4
6
0
.
0
1
0
.
4
7
0
.
0
1
0
.
4
7
0
.
0
1
0
.
4
9
0
.
0
1
*
0
.
4
9
0
.
0
1
0
.
4
9
0
.
0
1
0
.
4
8
0
.
0
1
0
.
4
9
0
.
0
1
0
.
4
9
0
.
0
1
0
.
4
9
0
.
0
1
0
.
5
0
0
.
0
1
0
.
5
1
0
.
0
1
V
O
2
,
l
/
m
i
n
0
.
2
4
0
.
0
1
0
.
2
6
0
.
0
1
0
.
2
7
0
.
0
1
0
.
3
0
0
.
0
2
0
.
2
9
0
.
0
2
0
.
2
7
0
.
0
2
1
.
6
9
0
.
0
7
1
.
6
7
0
.
0
8
1
.
6
5
0
.
0
9
1
.
8
3
0
.
0
8
2
.
0
0
0
.
2
0
1
.
9
6
0
.
2
1
*
0
.
3
4
0
.
0
3
0
.
3
6
0
.
0
1
0
.
3
6
0
.
0
1
0
.
4
4
0
.
0
4
*
0
.
4
2
0
.
0
3
0
.
4
0
0
.
0
1
*
C
O
2
,
l
/
m
i
n
0
.
2
3
0
.
0
2
0
.
2
3
0
.
0
1
0
.
2
6
0
.
0
1
0
.
3
0
0
.
0
3
0
.
2
5
0
.
0
1
0
.
2
6
0
.
0
2
1
.
6
2
0
.
0
3
1
.
5
2
0
.
0
7
1
.
5
2
0
.
0
4
1
.
7
3
0
.
0
7
1
.
6
2
0
.
0
6
1
.
5
8
0
.
0
5
0
.
3
2
0
.
0
2
0
.
3
0
0
.
0
1
0
.
3
0
0
.
0
1
0
.
3
7
0
.
0
3
0
.
3
4
0
.
0
1
0
.
3
0
0
.
0
1
N
O
,
n
l
/
m
i
n
8
5
.
7
3
3
.
7
5
0
.
8
3
2
4
.
0
4
6
.
5
6
4
.
9
7
7
.
5
1
8
.
6
6
8
.
4
8
.
5
3
2
.
5
6
4
.
3
1
2
2
.
3
3
6
.
5
2
5
.
0
5
2
.
6
7
0
.
0
4
7
.
8
1
8
7
.
3
4
7
.
5
1
.
6
1
5
0
.
0
2
2
1
.
6
9
9
.
2
1
8
5
.
6
6
1
.
8
1
5
.
8
3
7
.
0
8
0
.
4
1
9
.
2
1
3
8
.
1
2
9
.
0
8
1
.
5
2
4
.
1
2
0
.
9
4
9
.
7
R
i
n
t
I
,
c
m
H
2
O
1
3
5
.
0
4
1
1
.
3
4
2
3
.
9
1
3
.
4
9
4
1
.
7
2
1
9
.
1
2
4
4
.
0
1
3
1
.
9
7
5
5
.
4
1
2
6
.
7
6
4
7
.
4
1
2
2
.
6
4
9
.
9
2
1
.
2
9
1
8
.
0
2
1
.
7
0
5
4
.
4
4
2
4
.
8
7
1
2
.
7
8
3
.
2
7
2
6
.
7
5
7
.
5
7
3
2
.
3
9
5
.
7
7
1
6
.
3
3
4
.
1
1
1
9
.
4
1
2
.
7
0
7
6
.
1
1
1
6
.
2
4
7
.
7
4
1
.
6
9
3
6
.
9
9
1
3
.
7
7
4
1
.
9
3
2
0
.
5
1
R
i
n
t
E
,
c
m
H
2
O
1
3
0
.
7
4
9
.
0
5
1
4
.
6
2
3
.
4
1
3
8
.
5
3
1
0
.
1
3
2
8
.
8
3
8
.
2
2
5
2
.
0
0
1
1
.
4
0
3
5
.
7
9
1
4
.
0
9
1
4
.
1
6
4
.
9
1
1
5
.
9
9
6
.
0
1
3
0
.
2
6
7
.
5
0
2
6
.
3
6
8
.
9
9
5
9
.
5
3
2
4
.
5
5
*
2
3
.
7
8
7
.
5
4
1
8
.
3
4
3
.
0
0
3
1
.
8
1
7
.
5
1
2
5
.
8
5
7
.
9
9
2
1
.
6
1
5
.
0
0
3
7
.
9
3
1
2
.
8
7
4
7
.
5
8
9
.
2
0
V
a
l
u
e
s
a
r
e
m
e
a
n
s
S
E
.
T
i
d
a
l
v
o
l
u
m
e
(
V
T
)
i
n
c
r
e
a
s
e
d
w
i
t
h
d
e
p
t
h
d
u
r
i
n
g
r
e
s
t
a
n
d
e
x
e
r
c
i
s
e
,
b
u
t
o
n
l
y
c
h
a
n
g
e
s
d
u
r
i
n
g
s
u
b
m
e
r
s
i
o
n
r
e
a
c
h
e
d
s
i
g
n
i
c
a
n
c
e
.
S
u
b
m
e
r
s
i
o
n
t
e
n
d
e
d
t
o
i
n
c
r
e
a
s
e
b
r
e
a
t
h
i
n
g
f
r
e
q
u
e
n
c
y
(
f
)
,
w
h
i
l
e
d
e
p
t
h
d
e
c
r
e
a
s
e
d
i
t
.
D
u
r
i
n
g
r
e
s
t
,
m
i
n
u
t
e
v
e
n
t
i
l
a
t
i
o
n
(
V
E
)
w
a
s
u
n
a
f
f
e
c
t
e
d
b
y
s
u
b
m
e
r
s
i
o
n
b
u
t
i
n
c
r
e
a
s
e
d
a
s
a
f
u
n
c
t
i
o
n
o
f
d
e
p
t
h
;
d
u
r
i
n
g
e
x
e
r
c
i
s
e
,
V
E
i
n
c
r
e
a
s
e
d
a
s
a
f
u
n
c
t
i
o
n
o
f
s
u
b
m
e
r
s
i
o
n
b
u
t
d
e
c
r
e
a
s
e
d
w
i
t
h
i
n
c
r
e
a
s
i
n
g
d
e
p
t
h
.
D
u
t
y
c
y
c
l
e
w
a
s
u
n
a
f
f
e
c
t
e
d
b
y
d
e
p
t
h
a
n
d
s
u
b
m
e
r
s
i
o
n
d
u
r
i
n
g
r
e
s
t
b
u
t
i
n
c
r
e
a
s
e
d
w
i
t
h
s
u
b
m
e
r
s
i
o
n
d
u
r
i
n
g
e
x
e
r
c
i
s
e
.
N
i
t
r
i
c
o
x
i
d
e
e
l
i
m
i
n
a
t
i
o
n
(
V
N
O
)
w
a
s
u
n
a
f
f
e
c
t
e
d
b
y
s
u
b
m
e
r
s
i
o
n
.
D
e
p
t
h
-
d
e
p
e
n
d
e
n
t
e
f
f
e
c
t
s
p
r
o
d
u
c
e
d
a
n
a
d
i
r
a
t
2
.
7
a
t
m
o
s
p
h
e
r
e
s
a
b
s
o
l
u
t
e
(
A
T
A
)
i
n
t
h
e
s
u
b
m
e
r
s
e
d
c
o
n
d
i
t
i
o
n
s
.
I
n
s
p
i
r
a
t
o
r
y
R
a
w
m
e
a
s
u
r
e
d
b
y
t
h
e
P
0
.
1
t
e
c
h
n
i
q
u
e
(
R
i
n
t
I
)
w
a
s
u
n
a
f
f
e
c
t
e
d
b
y
d
e
p
t
h
a
n
d
s
u
b
m
e
r
s
i
o
n
a
t
r
e
s
t
b
u
t
i
n
c
r
e
a
s
e
d
w
i
t
h
d
e
p
t
h
d
u
r
i
n
g
e
x
e
r
c
i
s
e
.
E
x
p
i
r
a
t
o
r
y
R
a
w
m
e
a
s
u
r
e
d
b
y
t
h
e
P
0
.
1
t
e
c
h
n
i
q
u
e
(
R
i
n
t
E
)
w
a
s
u
n
a
f
f
e
c
t
e
d
b
y
d
e
p
t
h
a
n
d
s
u
b
m
e
r
s
i
o
n
a
t
r
e
s
t
b
u
t
i
n
c
r
e
a
s
e
d
a
s
a
r
e
s
u
l
t
o
f
s
u
b
m
e
r
s
i
o
n
a
t
2
.
7
A
T
A
d
u
r
i
n
g
e
x
e
r
c
i
s
e
.
O
2
c
o
n
s
u
m
p
t
i
o
n
(
V
O
2
)
a
n
d
C
O
2
p
r
o
d
u
c
t
i
o
n
(
V
C
O
2
)
i
n
c
r
e
a
s
e
d
f
r
o
m
r
e
s
t
t
o
e
x
e
r
c
i
s
e
a
n
d
f
r
o
m
r
e
s
t
t
o
i
s
o
c
a
p
n
i
c
s
i
m
u
l
a
t
e
d
e
x
e
r
c
i
s
e
v
e
n
t
i
l
a
t
i
o
n
(
I
S
E
V
)
b
u
t
w
e
r
e
l
a
r
g
e
l
y
u
n
a
f
f
e
c
t
e
d
b
y
d
e
p
t
h
o
r
s
u
b
m
e
r
s
i
o
n
.
*
S
i
g
n
i
c
a
n
t
l
y
d
i
f
f
e
r
e
n
t
f
r
o
m
d
r
y
(
P
0
.
0
5
)
.
S
i
g
n
i
c
a
n
t
l
y
d
i
f
f
e
r
e
n
t
f
r
o
m
1
A
T
A
(
P
0
.
0
5
)
.
I
S
E
V
s
i
g
n
i
c
a
n
t
l
y
d
i
f
f
e
r
e
n
t
f
r
o
m
e
x
e
r
c
i
s
e
(
P
0
.
0
5
)
.
583 Effects of Submersion and Pressure on Respiratory Mechanics Held HE et al.
J Appl Physiol doi:10.1152/japplphysiol.00584.2012 www.jappl.org
decreased with depth [27% from 1 to 4.6 ATA during submersion
(P 0.004) and 20% from 1 to 4.6 ATA in the dry condition
(P 0.029)].
Since subjects were paced during ISEV, the effects of submer-
sion and depth on VT and f, as could be expected, followed the
same trends as during exercise. Thus, VT was unchanged by
submersion but tended to increase with increasing depth; simi-
larly, f increased with submersion and decreased with depth.
During rest, submersion and depth had no effect on duty
cycle, which is the duration of inspiration as a fraction of the
total breath. During exercise, depth had no effect, but duty
cycle increased 7% due to submersion at 1 ATA (P 0.007).
During ISEV, there were no statistically signicant effects of
depth or submersion on duty cycle.
Raw and V
NO. Raw
I
and Raw
E
decreased from rest to exer-
cise under all conditions tested. Raw
E
did not differ between
exercise and ISEV, nor did Raw
I
, except at 2.7 ATA in the dry
condition, where the value of Raw
I
was slightly higher during
ISEV than exercise (8.97 vs. 8.01 cmH
2
Ol
1
s, P 0.031).
For Raw
I
and Raw
E
, the effects of depth were independent, but
the effects of submersion (dry and submersed) and effort (rest,
exercise, and ISEV) were interrelated.
During rest, Raw
I
decreased with submersion and increased
with depth (Fig. 2A). The decrease in Raw
I
with submersion
was signicant at 2.7 ATA (46% decrease, P 0.009) and 4.6
ATA (34% decrease, P 0.008). The increase in Raw
I
with
depth was not surprising, given the concurrent increase in gas
density, and it reached signicance at 4.6 ATA during submer-
sion, where there was a 42% increase compared with 1 ATA
(P 0.013). Similarly, Raw
E
decreased with submersion and
increased with depth (Fig. 2B). Submersion decreased Raw
E
59% compared with the dry condition at 1 ATA (P 0.016)
and 68% compared with the dry condition at 2.7 ATA (P
0.013). As a result of increasing depth, Raw
E
increased 62%
from 1 to 4.6 ATA during submersion (P 0.023).
During exercise, Raw
I
and Raw
E
increased as a function of
depth (Fig. 2, C and D), but only Raw
I
decreased with sub-
mersion. The effect of submersion on Raw
I
during exercise
only reached signicance at 1 ATA, where there was a 30%
decrease (P 0.008). Depth, on the other hand, produced a
Pressure (ATA)
6 . 4 7 . 2 0 . 1
R
a
w
I
(
c
m
H
2
O
*
s
*
L
-
1
)
0
2
4
6
8
10
12
14
16
Dry ISEV
Submersed ISEV
Pressure (ATA)
6 . 4 7 . 2 0 . 1
R
a
w
E
(
c
m
H
2
O
*
s
*
L
-
1
)
0
2
4
6
8
10
12
14
16
Dry Exercise
Submersed Exercise
Pressure (ATA)
6 . 4 7 . 2 0 . 1
R
a
w
I
(
c
m
H
2
O
*
s
*
L
-
1
)
0
5
10
15
20
25
30
35
Dry Rest
Submersed Rest
Pressure (ATA)
6 . 4 7 . 2 0 . 1
R
a
w
E
(
c
m
H
2
O
*
s
*
L
-
1
)
0
5
10
15
20
25
30
35
Dry Rest
Submersed Rest
Pressure (ATA)
6 . 4 7 . 2 0 . 1
R
a
w
I
(
c
m
H
2
O
*
s
*
L
-
1
)
0
2
4
6
8
10
12
14
16
Dry Exercise
Submersed Exercise
Pressure (ATA)
6 . 4 7 . 2 0 . 1
R
a
w
E
(
c
m
H
2
O
*
s
*
L
-
1
)
0
2
4
6
8
10
12
14
16
Dry Exercise
Submersed Exercise
*
*
*
*
*
A
C
B
D
E F
Fig. 2. Resistance in the airways (Raw). A: during rest,
inspiratory Raw(RawI) decreased with submersion but
increased with depth [only during submersion, dry
slope 0.34 (cmH2Osl
1
)/ATA (r
2
0.11), sub-
mersed slope 0.96 (cmH2Osl
1
)/ATA (r
2
0.88)]. B: during rest, expiratory Raw (RawE) also
decreased with submersion and increased with depth
[submersion only, dry slope 0.60 (cmH2O
sl
1
)/ATA (r
2
0.10), submersed slope 1.07
(cmH2Osl
1
)/ATA (r
2
0.80)]. C: during exer-
cise, RawI decreased with submersion but increased
with depth [dry slope 1.02 (cmH2Osl
1
)/ATA
(r
2
0.99), submersed slope 1.09
(cmH2Osl
1
)/ATA (r
2
0.97)]. D: during exer-
cise, RawE was unaffected by submersion but in-
creased with depth [submersed only, dry slope
0.22 (cmH2Osl
1
)/ATA (r
2
0.70), submersed
slope 0.68 (cmH2Osl
1
)/ATA (r
2
0.83)].
E: during isocapnic simulated exercise ventilation
(ISEV), RawI tended to decrease with submersion
but increased as a function of depth [dry slope
1.15 (cmH2Osl
1
)/ATA (r
2
0.84), submersed
slope 1.36 (cmH2Osl
1
)/ATA (r
2
0.99)].
F: during ISEV, RawE was unaffected by submersion
but increased as a function of depth [dry slope 0.44
(cmH2Osl
1
)/ATA (r
2
0.70), submersed slope
0.73 (cmH2Osl
1
)/ATA (r
2
0.87)]. Values are
means SE. *Signicantly different from dry (P
0.05). Signicantly different from 1 ATA (P
0.05). ISEV signicantly different from exercise
(P 0.05).
584 Effects of Submersion and Pressure on Respiratory Mechanics Held HE et al.
J Appl Physiol doi:10.1152/japplphysiol.00584.2012 www.jappl.org
larger and more consistent increase in Raw
I
during exercise
than at rest: a 62% increase from 1 to 4.6 ATA in the dry
condition (P 0.008) and a 94% increase from 1 to 4.6 ATA
during submersion (P 0.007). Raw
E
was unaffected by
submersion but, like Raw
I
, increased with depth to a greater
degree than at rest: during submersion, there was a 139%
increase in Raw
E
from 1 to 4.6 ATA (P 0.017).
R
int
values were signicantly higher than Raw values and
were not as responsive to changes in submersion, depth, and
effort as Raw. Neither R
intI
nor R
intE
was different from rest to
exercise, and the effects of depth (1, 2.7, and 4.6 ATA),
submersion (dry and submersed), and effort (rest, exercise, and
ISEV) were independent of one another in their effects on R
intI
and R
intE
.
During rest, neither R
intI
nor R
intE
was affected by depth or
submersion (Table 2). During exercise, submersion still had no
effect on R
intI
, but depth increased it. There was a 449%
increase in R
intI
from 1 to 4.6 ATA in the dry condition (P
0.023) and a 153% increase from 1 to 4.6 ATA during
submersion (P 0.008). It is worth noting that these increases
are substantially larger than the increases in Raw
I
for the same
conditions, perhaps due to greater inertial effects and less
uniform ow at the start of the breath. R
intE
tended to increase
with submersion during exercise, which was signicant at 2.7
ATA (48% increase from the dry condition, P 0.047). R
intE
also increased with depth, which was signicant from 2.7 to
4.6 ATA in the dry condition, where there was an 89% increase
(P 0.049), a similar magnitude to the increase in Raw
E
.
V
NO was studied for its reported relationship with Raw and
was expected to correlate negatively with Raw as a function of
depth (i.e., as depth increased, V
NO would decrease due to the
higher PO
2
and Raw would increase due to increased gas
density and reduced V
NO). In fact, there was no correlation
between Raw or R
int
and V
NO as a function of depth or within
individual test conditions (e.g., surface dry). At rest, V
NO was
unaffected by depth and submersion (mean 60.2 9.3 l/min).
Submersion had no effect on V
NO during exercise. The effect
of depth on V
NO during exercise was also minimal, except at
2.7 ATA during submersion, when V
NO reached a nadir (99%
less than at 1 and 4.6 ATA, P 0.023 and 0.016, respectively).
Additionally, V
NO was not different from rest to exercise,
except at 4.6 ATA during submersion, when it was 582%
greater than the resting value (P 0.008).
PA. The magnitudes of PA
I
and PA
E
increased from rest to
exercise for all conditions, as expected. The effects of depth (1,
2.7, and 4.6 ATA), submersion (dry and submersed), and effort
(rest, exercise, and ISEV) were independent of one another in
their effects on PA
I
and PA
E
.
During rest, PA
I
was more negative as a result of submersion
and depth (Fig. 3A). The effect of submersion reached signif-
icance at 2.7 ATA: PA
I
was 25% more negative than in the dry
condition (P 0.020). PA
I
was also more negative with in-
creasing depth: 166% more negative at 4.6 than 1 ATA in the
dry condition (P 0.008) and 115% more negative at 4.6 than
1 ATA during submersion (P 0.001). In contrast to PA
I
,
resting PA
E
was largely unaffected by depth and submersion
(Fig. 3B). Depth had an effect only in the dry condition, when
PA
E
increased 99% from 1 to 4.6 ATA (P 0.001).
During exercise, the effects of depth and submersion on PA
I
were similar to those during rest (Fig. 3C). PA
I
was more
negative with increasing depth and tended to be more negative
with submersion, although the effect of submersion did not
reach signicance. PA
I
was 23% more negative at 2.7 than 1
ATA in the dry condition (P 0.026) and 72% more negative
at 4.6 than 1 ATA during submersion (P 0.001). In contrast,
during exercise, PA
E
increased with submersion but was unaf-
fected by depth (Fig. 3D). Submersion caused an 81% increase
in PA
E
compared with the dry condition at 1 ATA (P 0.004)
and a 90% increase from the dry condition at 2.7 ATA (P
0.008).
Power of breathing. W
I
and W
E
increased from rest to exercise
under all conditions, as expected, and the effects of submersion
(dry and submersed), depth (1, 2.7, and 4.6 ATA), and effort (rest,
exercise, and ISEV) were independent of one another in their
effects on W
I
and W
E
.
During rest, W
I
decreased with submersion and increased
with depth (Fig. 4A). The decrease from submersion was
statistically signicant at 2.7 ATA, where there was a 26%
decrease compared with the dry condition (P 0.031). The
increase in W
I
with depth was 53% from 1 to 4.6 ATA in the
dry condition (P 0.001) and 35% from 1 to 2.7 ATA during
submersion (P 0.043). In contrast to W
I
, W
E
was unaffected
by submersion but increased with depth during rest (Fig. 4B).
There was a 62% increase in W
E
from 1 to 4.6 ATA in the dry
condition (P 0.007) and a 72% increase from 1 to 4.6 ATA
during submersion (P 0.021).
During exercise, W
I
tended to increase with submersion and
depth (Fig. 4C). The effect of submersion reached signicance
at 4.6 ATA, where there was a 19% increase in W
I
from the dry
condition (P 0.020). Increasing depth resulted in an increase
of 20% from 1 to 4.6 ATA in the dry condition (P 0.022).
In contrast, W
E
was unaffected by submersion and depth (mean
639 305 mW; Fig. 4D).
O
2
cost and efciency of breathing. It was hypothesized that
V
O
2B
would increase as a function of depth due to the increased
work of breathing and would increase with submersion due to
the mechanical disadvantages imposed by blood redistribution
to the lungs and the presence of the SLL; however, there were
no signicant effects of submersion on V
O
2B
. Depth tended to
increase V
O
2B
during submersion, but this effect did not reach
statistical signicance (Fig. 5A).
Respiratory efciency decreased with submersion (49% de-
crease from dry condition to submersion at 2.7 ATA, P
0.023) but was unaffected by depth (Fig. 5B).
Maximal P
mouth
. As expected, P
Emax
increased with increas-
ing lung volume and with increasing depth (Fig. 6). Submer-
sion had no effect on P
Emax
at any depth, so wet and dry data
have been pooled. P
Emax
increased from 20% of VC to total
lung capacity at all depths [14% increase at 1 ATA (P
0.030), 19% increase at 2.7 ATA (P 0.003), and 17%
increase at 4.6 ATA (P 0.002)].
P
Emax
also increased as a function of depth, although the
increase only reached signicance at the higher lung volumes.
At a lung volume of 80% of VC, there was a 17% increase
from 1 to 2.7 ATA (P 0.035). At total lung capacity, there
was an increase of 15% from 1 to 4.6 ATA (P 0.033).
DISCUSSION
V
E and its components. During rest, VT was the primary
determinant ofV
E: as VT increased with depth, so did V
E. Such
an increase has been documented previously (43, 57) and may
585 Effects of Submersion and Pressure on Respiratory Mechanics Held HE et al.
J Appl Physiol doi:10.1152/japplphysiol.00584.2012 www.jappl.org
be explained by several processes. The most recent hypothesis
is hyperoxic hyperventilation, which may occur following
blunting of the peripheral chemoreceptor response by the high
PO
2
of the hyperbaric environment. After 510 min at depth,
reactive oxygen species accumulate in brain tissue and stimu-
late central chemoreceptors in the caudal solitary complex
(19), which should stimulate hyperventilation, although this
effect is likely dampened by feedback within the system and
has only been observed in vivo following carotid body dener-
vation (15, 24). It should also be noted that this mechanism
would lead to a decrease in arterial PCO
2
, and the majority of
studies have not produced this result (23). Another mechanism
that may contribute to the hyperventilation observed during
rest is the Haldane effect, whereby incomplete O
2
unloading
from hemoglobin interferes with CO
2
transport and leads to
CO
2
retention, which in turn raises PCO
2
and increases respi-
ratory drive (59). As discussed by Lambertsen et al. (34), this
may be particularly deleterious to the brain and could further
stimulate central chemoreceptors. It should be noted, however,
that modeling based on quantitative studies indicates that the
resulting increase in arterial PCO
2
would be 1 mmHg and is
therefore likely insignicant (23). Finally, it has been reported
that as gas density increases, respiratory dead space and the
dead space-to-VT ratio increase, most likely as a result of
decreased gas mixing in the lungs (41). Thus, V
E and VT would
have to increase to maintain alveolar ventilation at depth. This
is the most likely explanation for the increase in VT and V
E
with depth during rest.
In contrast to rest, V
E increased with submersion but de-
creased as a function of depth during exercise. The increase in
V
E during submersion was most likely due to a slightly higher
metabolic rate (as evidenced by increased V
O
2
and V
CO
2
),
despite an attempt to set the work rate equivalent to the dry
condition. Although increases in V
O
2
and V
CO
2
during submer-
sion generally were not statistically signicant, they may have
been sufcient to elevate V
E. An alternative explanation is the
effect of submersion in resting critical water temperature,
which is cool enough to cause an effect (18); however, during
exercise, this water temperature is thermoneutral and may not
have had an effect (10).
It is interesting to note that there was a concurrent increase
in duty cycle with submersion, which may reect the greater
Pressure (ATA)
6 . 4 7 . 2 0 . 1
R
e
s
t
P
A
E
(
c
m
H
2
O
)
0
1
2
3
4
Dry Rest
Submersed Rest
Pressure (ATA)
6 . 4 7 . 2 0 . 1
R
e
s
t
P
A
I
(
c
m
H
2
O
)
-6
-5
-4
-3
-2
-1
0
Dry Rest
Submersed Rest
A
Pressure (ATA)
6 . 4 7 . 2 0 . 1
E
x
e
r
c
i
s
e
P
A
I
(
c
m
H
2
O
)
-16
-14
-12
-10
-8
-6
-4
-2
0
Dry Exercise
Submersed Exercise
B
C
Pressure (ATA)
6 . 4 7 . 2 0 . 1
E
x
e
r
c
i
s
e
P
A
E
(
c
m
H
2
O
)
0
2
4
6
8
10
12
14
16
Dry Exercise
Submersed Exercise
D
*
*
*
Pressure (ATA)
6 . 4 7 . 2 0 . 1
I
S
E
V
P
A
I
(
c
m
H
2
O
)
-16
-14
-12
-10
-8
-6
-4
-2
0
Dry ISEV
Submersed ISEV
E F
Pressure (ATA)
6 . 4 7 . 2 0 . 1
I
S
E
V
P
A
E
(
c
m
H
2
O
)
0
2
4
6
8
10
12
14
16
Dry ISEV
Submersed ISEV
Fig. 3. Inspiratory and expiratory alveolar pressures
(PAI and PAE, respectively) during rest and exercise.
A: PAI during rest was more negative during submer-
sion and more negative as a function of depth [slope
0.81 cmH2O/ATA (r
2
0.92) in dry condition,
slope 0.69 cmH2O/ATA (r
2
0.97) during sub-
mersion]. B: PAE during rest was unaffected by sub-
mersion but tended to increase with depth [slope
0.42 cmH2O/ATA (r
2
0.92) in dry condition].
C: PAI during exercise was unaffected by submersion
but was more negative with depth [slope 0.61
cmH2O/ATA (r
2
0.91) in dry condition, slope
1.55 cmH2O/ATA (r
2
0.73) during submersion].
D: PAE during exercise increased with submersion but
was unaffected by depth. E: PAI during ISEV was
unaffected by submersion but increased with depth
[slope 1.08 cmH2O/ATA (r
2
0.95) in dry
condition, slope 1.21 cmH2O/ATA (r
2
0.93)
during submersion]. F: PAE was unaffected by sub-
mersion and depth during ISEV [slope 0.11
cmH2O/ATA (r
2
0.23) in dry condition, slope
0.47 cmH2O/ATA (r
2
0.23) during submersion].
Values are means SE. *Signicantly different from
dry (P 0.05). Signicantly different from 1 ATA
(P 0.05). ISEV signicantly different from exer-
cise (P 0.05).
586 Effects of Submersion and Pressure on Respiratory Mechanics Held HE et al.
J Appl Physiol doi:10.1152/japplphysiol.00584.2012 www.jappl.org
inspiratory effort required to overcome the SLL. The decrease
in V
E as a function of depth occurred despite increasing VT at
depth and may reect a shift to a ventilation pattern that
increased elastic work. This would help offset the increase in
resistive work experienced at greater gas densities and may
also help maintain alveolar ventilation in spite of increasing
dead space, as discussed above. The alterations in V
E may
therefore reect a rebalancing of respiratory drive toward a
more efcient breathing pattern, a notion that is supported by
the observation that human subjects at sea level spontaneously
breathe at a frequency and VT that closely approximate the
most efcient pattern (39, 47).
Raw, PA, and the work of breathing. The overall trends in
V
NO were surprising, given the established role of NO as a
bronchodilator (5). During rest and exercise, V
NO was unaf-
fected by submersion. The nadir in V
NO that was observed at
2.7 ATA during exercise is puzzling but likely results from the
interaction of more than one variable. It is possible that V
NO
decreased as a result of hyperoxia, as previously proposed (20),
but this effect may have competed with increases in V
NO
typically seen during exercise (11, 29). The balance of these
two effects produced a nonuniform trend as depth increased but
exercise intensity remained constant. This is also the most
likely explanation for the lack of increase in V
NO from rest to
exercise that has typically been observed (11, 29, 37). Our
subjects exhibited a high degree of variability, which is most
likely due to the fact that V
NO varies between trained and
untrained subjects (11, 37) and as a function of height and age
(44). Given that our cohort was small and encompassed indi-
viduals with a broad age range and varying heights and levels
of physical tness, it is not surprising that our results exhibit a
wide standard error. The absence of correlation between V
NO
and Raw, even within a single condition, suggests that
control of airway caliber and, therefore, resistance was
multifactorial and not primarily determined by V
NO, at least
under the conditions tested. Several studies have shown,
under normobaric conditions, that V
NO uctuates according
to PO
2
in the surrounding tissue and have implicated NO in
maintenance of tissue normoxia (6, 22). The observation
that V
NO decreases with depth (i.e., increased PO
2
) is con-
sistent with this understanding and suggests that the altera-
tions in V
NO observed in this study were dictated more
heavily by demands to maintain tissue normoxia than by
other factors, such as Raw.
Pressure (ATA)
6 . 4 7 . 2 0 . 1
I
S
E
V
W
I
(
m
W
)
0
200
400
600
800
1000
1200
1400
1600
Dry ISEV
Submersed ISEV
Pressure (ATA)
6 . 4 7 . 2 0 . 1
R
e
s
t
W
I
(
m
W
)
0
50
100
150
200
250
300
Dry Rest
Submersed Rest
Pressure (ATA)
6 . 4 7 . 2 0 . 1
E
x
e
r
c
i
s
e
W
I
(
m
W
)
0
200
400
600
800
1000
1200
1400
1600
Dry Exercise
Submersed Exercise
Pressure (ATA)
6 . 4 7 . 2 0 . 1
R
e
s
t
W
E
(
m
W
)
0
50
100
150
200
250
300
Dry Rest
Submersed Rest
A
Pressure (ATA)
6 . 4 7 . 2 0 . 1
E
x
e
r
c
i
s
e
W
E
(
m
W
)
0
200
400
600
800
1000
1200
1400
1600
Dry Exercise
Submersed Exercise
C
B
D
*
Pressure (ATA)
6 . 4 7 . 2 0 . 1
I
S
E
V
W
E
(
m
W
)
0
200
400
600
800
1000
1200
1400
1600
Dry ISEV
Submersed ISEV
E F
*
Fig. 4. Work of breathing per minute (W
). A: during
rest, inspiratory W
(W
I) increased with submersion
and as a function of depth [slope 20.9 mW/ATA
(r
2
0.78) in dry condition, slope 13.4 mW/ATA
(r
2
0.84) during submersion]. B: during rest, ex-
piratory W
(W
E) was unaffected by submersion but
increased as a function of depth [slope 15.1
mW/ATA (r
2
0.62) in dry condition, slope 16.8
mW/ATA (r
2
0.91) during submersion]. C: during
exercise, W
I increased with submersion and as a
function of depth [slope 51.6 mW/ATA (r
2
0.99) in dry condition, slope 61.2 mW/ATA (r
2
0.73) during submersion]. D: during exercise, W
E
was not affected by depth or submersion. E: during
ISEV, W
I increased with submersion and as a func-
tion of depth [slope 61.7 mW/ATA (r
2
0.65) in
dry condition, slope 99.3 mW/ATA (r
2
0.97)
during submersion]. F: during ISEV, neither depth
nor submersion induced trends in W
E. Values are
means SE. *Signicantly different from dry con-
dition (P 0.05). Signicantly different from 1
ATA (P 0.05). ISEV signicantly different from
exercise (P 0.05).
587 Effects of Submersion and Pressure on Respiratory Mechanics Held HE et al.
J Appl Physiol doi:10.1152/japplphysiol.00584.2012 www.jappl.org
We chose to compare the traditional, esophageal balloon-
based method of calculating Raw with the newer P
0.1
method
(R
int
), as the P
0.1
method may more closely reect PA, and its
use has become more prevalent. If the two methods were found
to produce similar values and were equally sensitive to alter-
ations in Raw, the P
0.1
method would be desirable for future
studies because of the ease of use of the devices and improved
subject comfort from elimination of the esophageal balloon.
However, the commercially available devices make this mea-
surement 100 ms after the onset of the breath, which may not
reect the same pressures and resistances observed during the
portion of the breath with uniform ow (as in the esophageal
balloon method). While both measurements of airway resis-
tance (Raw and R
int
) detected increased resistance as a function
of depth, the values given by the P
0.1
technique differed
substantially from those of the esophageal balloon method. The
P
0.1
technique used in this study measured the initial portion of
the breath and, thus, did not detect any effect of depth or
submersion during rest. Furthermore, the values obtained using
this method were substantially higher than those obtained using
the esophageal balloon method. One possible explanation for
this discrepancy is that PA, used in the R
int
calculations, de-
scribes the pressure differential between the lung and ambient
pressure and, thus, includes the hydrostatic pressure exerted on
the chest during submersion, while pleural pressure (approxi-
mated by the esophageal balloon and used for Raw calcula-
tions) only describes the pressure differential generated be-
tween the lung and the chest wall and, thus, does not account
for hydrostatic pressure on the chest. It is not surprising, then,
that Raw and R
int
measurements differed during submersion.
The discord between the two methods in the dry condition is
puzzling, although it probably results from the difference in the
timing of the measurement (midbreath vs. early breath). R
int
measurements were made at the very start of the breath, when
little air was owing (which would increase the inertial com-
ponent) and airway diameter was likely to be smaller (which
would directly increase ow resistance). These effects appar-
ently contributed to a signicantly increased R
int
compared
with Raw and were so substantial that they overshadowed
many of the smaller changes that were detected using the
esophageal balloon method. For these reasons, we do not
recommend the P
0.1
method for assessment of Raw in the
diving environment unless the measurement can be made
during peak ow.
Overall, our measurements of Raw were in agreement with
some published values (38) but were higher than those that are
typically reported (56, 62), even in studies of asthma (25, 27,
32, 55). We propose that the elevated values we observed
derived from the subjects ventilation and rates, which were
somewhat higher than normal during rest and would have
proportionally increased resistance according to Poiseuilles
law. Elevated ventilation may have occurred if subjects were
anxious at the beginning of each experiment or as subjects
adjusted to breathing through the mouthpiece (4).
As expected, PA and Raw increased as a function of depth,
most likely due to increased gas density, which has been shown
to increase Raw by the square root of the increase in density
Lung Volume (% VC)
0 20 40 60 80 100 120
P
m
a
x
(
m
m
H
g
)
0
60
70
80
90
100
110
1 ATA
2.7 ATA
4.6 ATA
Fig. 6. Maximal expiratory pressure at the mouth (PEmax) as a function of lung
volume and depth. PEmax increased as a function of increasing lung volume [at
1 ATA, slope 0.11 mmHg/%vital capacity (VC) (r
2
0.84); at 2.7 ATA,
slope 0.20 mmHg/%VC (r
2
0.91); at 4.6 ATA, slope 0.15 mmHg/%VC
(r
2
0.78)] and depth. Values are mean SE. Signicantly different from
1 ATA (P 0.05). Signicantly different from the lowest lung volume (P
0.05).
Pressure (ATA)
6 . 4 7 . 2 0 . 1
V
O
2
B
(
m
L
/
m
i
n
)
100
150
200
Dry
Submersed
Pressure (ATA)
6 . 4 7 . 2 0 . 1
R
e
s
p
i
r
a
t
o
r
y
E
f
f
i
c
i
e
n
c
y
(
W
*
m
i
n
*
L
O
2
-
1
)
0
20
40
60
80
Dry
Submersed
A
B
*
Fig. 5. A: absolute O2 cost of breathing (V
O2B) tended to increase with depth
under submersed conditions [slope 17.2 ml/(minATA) (r
2
0.96)] but
decreased with depth in dry condition [slope 2.60 ml/(minATA) (r
2
0.99)]. B: respiratory efciency decreased with submersion but was unaffected
by depth. Values are means SE. *Signicantly different from dry condition
(P 0.05).
588 Effects of Submersion and Pressure on Respiratory Mechanics Held HE et al.
J Appl Physiol doi:10.1152/japplphysiol.00584.2012 www.jappl.org
(49). PA increased from rest to exercise, probably due to
increased demand and airow, while Raw decreased during
exercise, most likely due to increased airway caliber. These
ndings are in accordance with the works of others (31), and it
is generally well accepted that exercise-induced bronchodila-
tion stems from a combination of neural control, primarily via
the vagus nerve (61), and increases in circulating cat-
echolamines, such as epinephrine (52, 58).
On the basis of the literature, we expected that submersion
would not alter Raw (7) or would increase it secondary to
decreased functional residual capacity (9, 35), which immer-
sion and negative SLL have been shown to produce (54). Thus
we were surprised to observe decreases in Raw
I
and Raw
E
with
submersion during rest. The decrease in Raw
E
occurred, de-
spite the fact that related variables (f, VT, V
E, PA
E
, and W
E
)
were almost entirely unchanged as a result of submersion. Thus
we can only assume that airway caliber must have been larger
than in the dry condition. This is also unexpected, given that
we observed a decrease in VC, consistent with the observations
of others (3, 33), and such a decrease in lung volume is usually
associated with increases in Raw (8). We can only surmise that
immersion of the whole body, as opposed to head-out submer-
sion, may have played a role. For instance, in attempting to
prevent air from escaping around the mouth or through the
nostrils, which experienced positive static loading, it is possi-
ble that subjects recruited accessory muscles in the neck and
shoulders, which may have increased airway caliber. Raw
I
also
decreased with submersion during exercise. This occurred
despite increased V
E and f (greater ow). Again, the simplest
conclusion is that the airways were more open during submer-
sion than in the dry condition. The more-negative PA
I
observed
during submersion ostensibly reects the effect of SLL, and
not submersion per se, which would increase chest wall elastic
recoil at the start of inspiration (54); however, this cannot be
stated with certainty, since functional residual capacity was not
measured.
As might be expected, changes in W
paralleled changes in
Raw and PA. In general, W
increased as a function of depth.
We surmise that this was due to the increased PA required to
move denser air against the increased Raw, although the effect
of altered PA cannot be stated for certain, since pressure was
measured only at the beginning of inspiration and expiration,
and not in the middle of the breath when ow was greater.
Submersion decreased W
I
at rest but increased it during exer-
cise. The decrease in W
I
during submersion at rest was due to
less work per breath (data not shown) and correlated with the
decrease in Raw
I
. During exercise, f was elevated during
submersed experiments, but the work per breath was un-
changed between dry and submersed conditions (data not
shown). The result was a higher W
I
during submersed exercise
than in the dry condition. Finally, W
E
was largely unaffected
by submersion. This probably results from the negative SLL,
which assisted exhalation. Interestingly, depth increased W
E
during rest, but not exercise. The increase during rest was
expected, given the increase in gas density, but the lack of
increase during exercise is surprising. It is possible that expi-
ratory assistance from the negative SLL overshadowed any
hindrance as a function of depth.
V
O
2B
and respiratory efciency. Accurate measurement of
efciency and V
O
2B
hinged on three factors: 1) subjects ability
during ISEV to accurately duplicate the recorded breathing
pattern, 2) the necessity that increases in V
O
2
from rest to ISEV
were due solely to increased ventilatory effort, and 3) the
assumption that respiratory and accessory muscle recruitment
was similar between exercise and ISEV. On the basis of the
data obtained, subjects reliably reproduced the exercise venti-
lation pattern, as there were almost no differences between
exercise and ISEV ventilation (with regard to V
E, VT, f, etc.).
Similarly, Q
was not different from rest to ISEV, which
suggests that the increased V
O
2
was due solely to respiratory
effort. While we cannot rule out the possibility that subjects
recruited muscle groups differently during ISEV than during
exercise, subjects were monitored during the experiment, and
use of their arms for postural support during ISEV was dis-
couraged. We thus believe that the calculated V
O
2B
is repre-
sentative of O
2
use by the respiratory muscles during exercise.
Finally, V
O
2B
for our subjects was similar to that described by
others (1), and any difference probably is due to the fact that
our study subjects were less physically t than those in the
study by Aaron et al. (1).
For submersed conditions, V
O
2B
tended to increase with depth
due to an increase in the work of breathing and a concurrent
tendency for respiratory muscle efciency to decrease. Efciency
decreased slightly with submersion, so, overall, V
O
2B
paralleled
changes in W
.
P
Emax
. P
Emax
increased with lung volume and increasing
depth. The increases in lung volume are consistent with pre-
viously published observations (14) and probably reect more
optimal respiratory muscle length at higher lung volumes (51).
Additionally, preservation of a favorable muscle length during
expiratory and inspiratory efforts is sustained by the reduced
compressibility of gas in the lungs during the maneuver. These
ndings are not surprising for several reasons. It is difcult to
generate pressure against a small volume of air in the lungs,
because the elastic recoil of the chest prevents the ribcage from
contracting to a small enough volume to exert signicant
pressure. At higher lung volumes, the elastic recoil of the chest
wall is diminished, and past its relaxation volume, the elastic
recoil of the chest wall inward supplements contraction of the
expiratory muscles. Since subjects VCs were measured in dry
(i.e., normal perfusion) and submersed (when more blood is
present in the subjects lungs) conditions and these values were
used to calculate the amount of air subjects inhaled, the
volumes during submersion were normalized compared with
the dry volumes. For this reason, it is not surprising that there
were no differences in P
Emax
between dry and submersed
conditions. It is possible that the presence of additional blood
could have served to elevate P
Emax
by serving as an incom-
pressible substrate (much as the dense air at increased depth),
but either this was not signicant or venous return decreased in
response to the high pressures in the thorax and prevented the
presence of a sufcient amount of blood to have an effect.
Conclusions. In summary, submersion did not have an effect
on P
Emax
. Increased pressure did not reliably decrease V
NO or
increase the work of breathing in the dry condition, although it
did increase Raw, PA, respiratory work during submersion, and
P
Emax
. These changes should be considered when assessing the
impact of submersion and depth on divers who are undertaking
rigorous physical activity, when assessing tness to dive, and
when providing HBOT to patients with compromised ventila-
tion.
589 Effects of Submersion and Pressure on Respiratory Mechanics Held HE et al.
J Appl Physiol doi:10.1152/japplphysiol.00584.2012 www.jappl.org
ACKNOWLEDGMENTS
We acknowledge the involvement of Claes Lundgren. We thank the staff of
the Center for Research and Education in Special Environments, Andrew
Barth, Lukas Eckhardt, Michael Fletcher, Ron Okupski, Curtis Senf, Amber
Simpson, Eric Stimson, and Matthew Vargo, for assistance in data collection.
We also thank Nancy Niedermayer for organizational work.
GRANTS
This research was sponsored by Ofce of Naval Research Grant N00014-
08-1-0255. H. E. Helds doctoral position is supported by the Ofce of Naval
Research.
DISCLOSURES
No conicts of interest, nancial or otherwise, are declared by the authors.
AUTHOR CONTRIBUTIONS
H.E.H. and D.R.P. are responsible for conception and design of the research;
H.E.H. performed the experiments; H.E.H. analyzed the data; H.E.H. and D.R.P.
interpreted the results of the experiments; H.E.H. prepared the gures; H.E.H.
drafted the manuscript; H.E.H. and D.R.P. edited and revised the manuscript;
H.E.H. and D.R.P. approved the nal version of the manuscript.
REFERENCES
1. Aaron E, Seow K, Johnson B, Dempsey J. Oxygen cost of exercise
hyperpnea: implications for performance. J Appl Physiol 72: 18181825,
1992.
2. Adnot S, Raffestin B, Eddahibi S. NO in the lung. Respir Physiol 101:
109120, 1995.
3. Agostoni E, Gurtner G, Torri G, Rahn H. Respiratory mechanics during
submersion and negative-pressure breathing. J Appl Physiol 21: 251258,
1966.
4. Askanazi J, Silverberg P, Foster R, Hyman A, Milic-Emili J, Kinney
J. Effects of respiratory apparatus on breathing pattern. J Appl Physiol 48:
577580, 1980.
5. Belvisi MG, Stretton CD, Yacoub M, Barnes PJ. Nitric oxide is the
endogenous neurotransmitter of bronchodilator nerves in humans. Eur J
Pharmacol 210: 221222, 1992.
6. Blitzer M, Loh E, Roddy M, Stamler J, Creager M. Endothelium-
derived nitric oxide regulates systemic and pulmonary vascular resistance
during acute hypoxia in humans. J Am Coll Cardiol 28: 591596, 1996.
7. Bondurant S, Hickam JB, Isley JK. Pulmonary and circulatory effects of
acute pulmonary vascular engorgement in normal subjects. J Clin Invest
36: 5966, 1957.
8. Briscoe WA, DuBois AB. The relationship between airway resistance,
airway conductance and lung volume in subjects of different age and body
size. J Clin Invest 37: 12791285, 1958.
9. Butler J, Caro CG, Alcala R, DuBois AB. Physiological factors affecting
airway resistance in normal subjects and in patients with obstructive
respiratory disease. J Clin Invest 39: 584591, 1960.
10. Cherry AD, Forkner IF, Frederick HJ, Natoli MJ, Schinazi EA,
Longphre JP, Conard JL, White WD, Freiberger JJ, Stolp BW.
Predictors of increased PaCO
2
during immersed prone exercise at 4.7 ATA.
J Appl Physiol 106: 316325, 2009.
11. Chirpaz-Oddou M, Favre-Juvin A, Flore P, Eterradossi J, Delaire M,
Grimbert F, Therminarias A. Nitric oxide response in exhaled air during
an incremental exhaustive exercise. J Appl Physiol 82: 13111318, 1997.
12. Clarke JR, Jaeger MJ, Zumrick JL, OBryan R, Spaur WH. Respi-
ratory resistance from 1 to 46 ATA measured with the interrupter tech-
nique. J Appl Physiol 52: 549555, 1982.
13. Comroe JH, Dubois AB, Briscoe WA, Carlsen E. The Lung. Chicago:
Year Book Medical Publishers, 1962, p. 390.
14. Cook CD, Mead J, Orzalesi MM. Static volume-pressure characteristics
of the respiratory system during maximal efforts. J Appl Physiol 19:
10161021, 1964.
15. Cragg P, Drysdale D, Hamilton J. Ventilation in intact and glossopha-
ryngeal nerve sectioned anaesthetized rats exposed to oxygen at high
pressure. J Physiol 370: 489499, 1986.
16. Craig A Jr, Dvorak M. Thermal regulation during water immersion. J
Appl Physiol 21: 15771585, 1966.
17. Dahlbck G, Jnsson E, Liner M. Inuence of hydrostatic compression
of the chest and intrathoracic blood pooling on static lung mechanics
during head-out immersion. Undersea Biomed Res 5: 7185, 1978.
18. Datta A, Tipton M. Respiratory responses to cold water immersion:
neural pathways, interactions, and clinical consequences awake and
asleep. J Appl Physiol 100: 20572064, 2006.
19. Dean J, Mulkey D, Henderson R 3rd, Potter S, Putnam R. Hyperoxia,
reactive oxygen species, and hyperventilation: oxygen sensitivity of brain
stem neurons. J Appl Physiol 96: 784791, 2004.
20. Demchenko IT, Boso AE, Bennett PB, Whorton AR, Piantadosi CA.
Hyperbaric oxygen reduces cerebral blood ow by inactivating nitric
oxide. J Appl Physiol 4: 597608, 2000.
21. Dupuy P, Shore S, Drazen J, Frostell C, Hill W, Zapol W. Broncho-
dilator action of inhaled nitric oxide in guinea pigs. J Clin Invest 90:
421428, 1992.
22. Dweik R, Laskowski D, Abu-Soud H, Kaneko F, Hutte R, Stuehr D,
Erzurum S. Nitric oxide synthesis in the lung. Regulation by oxygen
through a kinetic mechanism. J Clin Invest 101: 660666, 1998.
23. Forkner IF, Piantadosi CA, Scafetta N, Moon RE. Hyperoxia-induced
tissue hypoxia: a danger? Anesthesiology 106: 10511055, 2007.
24. Gautier H, Bonora M, Gaudy J. Ventilatory response of the conscious or
anesthetized cat to oxygen breathing. Respir Physiol 65: 181196, 1986.
25. Haverkamp HC, Dempsey J, Miller J, Romer L, Pegelow D, Lovering
A, Eldridge M. Repeat exercise normalizes the gas-exchange impairment
induced by a previous exercise bout in asthmatic subjects. J Appl Physiol
99: 18431852, 2005.
26. Hayot M, Ramonatxo M, Matecki S, Milic-Emili J, Prefaut C. Non-
invasive assessment of inspiratory muscle function during exercise. Am J
Respir Crit Care 162: 22012207, 2000.
27. Hjoberg J, Shore S, Kobzik L, Okinaga S, Hallock A, Vallone J,
Subramaniam V, De Sanctis GT, Elias JA, Drazen JM. Expression of
nitric oxide synthase-2 in the lungs decreases airway resistance and
responsiveness. J Appl Physiol 97: 249259, 2004.
29. Iwamoto J, Pendergast D, Suzuki H, Krasney J. Effect of graded
exercise on nitric oxide in expired air in humans. Respir Physiol 97:
333345, 1994.
30. Jackson AC, Milhorn HT, Norman JR. A reevaluation of the interrupter
technique for airway resistance measurement. J Appl Physiol 36: 264
268, 1974.
31. Kagawa J, Kerr HD. Effects of brief graded exercise on specic airway
conductance in normal subjects. J Appl Physiol 28: 138144, 1970.
32. Kaminsky DA. What does airway resistance tell us about lung function?
Respir Care 57: 8599, 2012.
33. Kurss DI, Lundgren CE, Pasche AJ. Effect of water temperature on vital
capacity in head-out immersion. In: Underwater Physiology VII: Proceed-
ings of the 7th Symposium on Underwater Physiology, edited by Bachrach
AJ, Matzen MM. Bethesda, MD: Undersea Med. Soc., 1981, p. 297301.
34. Lambertsen C, Kough R, Cooper D, Emmel GL, Loeschcke H,
Schmidt C. Oxygen toxicity. Effects in man of oxygen inhalation at 1 and
3.5 atmospheres upon blood gas transport, cerebral circulation and cere-
bral metabolism. J Appl Physiol 5: 471486, 1953.
35. Linderholm H. Lung mechanics in sitting and horizontal postures studied
by body plethysmographic methods. Am J Physiol 204: 8591, 1963.
36. Lundgren CE. Immersion effects. In: The Lung at Depth, edited by
Lundgren CE, Miller J. New York: Dekker, 1999, p. 91128.
37. Maroun MJ, Mehta S, Turcotte R, Cosio MG, Hussain SN. Effects of
physical conditioning on endogenous nitric oxide output during exercise.
J Appl Physiol 79: 12191225, 1995.
38. Marshall R, Lanphier EH, DuBois AB. Resistance to breathing in
normal subjects during simulated dives. J Appl Physiol 9: 510, 1956.
39. Mead J. Control of respiratory frequency. J Appl Physiol 15: 325336, 1960.
40. Mead J, Whittenberger JL. Evaluation of airway interruption technique
as a method for measuring pulmonary air-ow resistance. J Appl Physiol
6: 408416, 1954.
41. Moon R, Cherry A, Stolp B, Camporesi E. Pulmonary gas exchange in
diving. J Appl Physiol 106: 668677, 2009.
42. NAVSEA. US Navy Diving Manual Revision 6. Washington, DC: Naval
Sea Systems Command, 2008, p. 992. (Publ. no. 0910-LP-106-0957).
43. Noreet W, Hickey D, Lundgren C. A comparison of respiratory
function in divers breathing with a mouthpiece or a full face mask.
Undersea Biomed Res 14: 503526, 1987.
44. Olin AC, Rosengren A, Thelle DS, Lissner L, Bake B, Torn K. Height,
age, and atopy are associated with fraction of exhaled nitric oxide in a
large adult general population sample. Chest 130: 13191325, 2006.
45. Otis A, Proctor D. Measurement of alveolar pressure in human subjects.
Am J Physiol 152: 106, 1947.
46. Otis AB. The work of breathing. Physiol Rev 34: 449458, 1954.
590 Effects of Submersion and Pressure on Respiratory Mechanics Held HE et al.
J Appl Physiol doi:10.1152/japplphysiol.00584.2012 www.jappl.org
47. Otis AB, Fenn WO, Rahn H. Mechanics of breathing in man. J Appl
Physiol 2: 592607, 1950.
48. Pao CS, Healy MJ, McKenzie SA. Airway resistance by the interrupter
technique: which algorithm for measuring pressure? Pediatr Pulmonol 37:
3136, 2004.
49. Pedley T, Schroter R, Sudlow M. The prediction of pressure drop and
variation of resistance within the human bronchial airways. Respir Physiol
9: 387405, 1970.
50. Phagoo S, Wilson N, Silverman M. Evaluation of a new interrupter
device for measuring bronchial responsiveness and the response to bron-
chodilator in 3 year old children. Eur Respir J 9: 1374, 1996.
51. Rassier D, MacIntosh B, Herzog W. Length dependence of active force
production in skeletal muscle. J Appl Physiol 86: 14451457, 1999.
52. Sarpeshkar V, Bentley DJ. Adrenergic-2 receptor polymorphism and
athletic performance. J Hum Genet 55: 479485, 2010.
53. Taylor N, Morrison J. Lung volume changes in response to altered
breathing gas pressure during upright immersion. Eur J Appl Physiol 62:
122129, 1991.
54. Thalmann E, Sponholtz D, Lundgren C. Effects of immersion and static
lung loading on submerged exercise at depth. Undersea Biomed Res 6:
259290, 1979.
55. Veiga J, Lopes AJ, Jansen JM, Melo PL. Airow pattern complexity
and airway obstruction in asthma. J Appl Physiol 111: 412419, 2011.
56. Vorosmarti J, Bradley M, Anthonisen N. The effects of increased gas
density on pulmonary mechanics. Undersea Biomed Res 2: 110, 1975.
57. Warkander DE, Noreet WT, Nagasawa GK, Lundgren CE. Physio-
logically and subjectively acceptable breathing resistance in divers
breathing gear. Undersea Biomed Res 19: 427445, 1992.
58. Warren J, Dalton N. A comparison of the bronchodilator and vasopressor
effects of exercise levels of adrenaline in man. Clin Sci (Lond) 64:
475479, 1983.
59. Whalen RE, Saltzman HA, Holloway DH Jr, McIntosh HD, Sieker
HO, Brown IW Jr. Cardiovascular and blood gas responses to hyperbaric
oxygenation. Am J Cardiol 15: 638646, 1965.
60. Whitelaw W, Derenne JP, Milic-Emili J. Occlusion pressure as a
measure of respiratory center output in conscious man. Respir Physiol 23:
181199, 1957.
61. Widdicombe J. Neuroanatomy of the airways. In: Allergy Frontiers:
Classication and Pathomechanisms, edited by Pawankar R, Holgate ST,
Rosenwasser LJ. Tokyo: Springer, 2009, p. 457468.
62. Wood L, Bryan A. Exercise ventilatory mechanics at increased ambient
pressure. J Appl Physiol 44: 231237, 1978.
591 Effects of Submersion and Pressure on Respiratory Mechanics Held HE et al.
J Appl Physiol doi:10.1152/japplphysiol.00584.2012 www.jappl.org
Вам также может понравиться
- Parkinson'sДокумент3 страницыParkinson'sRorschach77Оценок пока нет
- Exp Physiol-2004-Bazán-Perkins-623-8 (Cambios Espontáneos en Cobaya Patrón Respiratorio Durante La Pletismografía Barométrica Papel de Las Catecolaminas y Los Óxidos de Nitrógeno)Документ6 страницExp Physiol-2004-Bazán-Perkins-623-8 (Cambios Espontáneos en Cobaya Patrón Respiratorio Durante La Pletismografía Barométrica Papel de Las Catecolaminas y Los Óxidos de Nitrógeno)Rorschach77Оценок пока нет
- CO2Документ6 страницCO2Rorschach77Оценок пока нет
- Comparison of Glycerol Lactamide Acetmide and DMSO As Cryoprotectants of Japanese White Rabbit SpermatozoaДокумент6 страницComparison of Glycerol Lactamide Acetmide and DMSO As Cryoprotectants of Japanese White Rabbit SpermatozoaRorschach77Оценок пока нет
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeОт EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeРейтинг: 4 из 5 звезд4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingОт EverandThe Little Book of Hygge: Danish Secrets to Happy LivingРейтинг: 3.5 из 5 звезд3.5/5 (399)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryОт EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryРейтинг: 3.5 из 5 звезд3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceОт EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceРейтинг: 4 из 5 звезд4/5 (894)
- The Yellow House: A Memoir (2019 National Book Award Winner)От EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Рейтинг: 4 из 5 звезд4/5 (98)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureОт EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureРейтинг: 4.5 из 5 звезд4.5/5 (474)
- Never Split the Difference: Negotiating As If Your Life Depended On ItОт EverandNever Split the Difference: Negotiating As If Your Life Depended On ItРейтинг: 4.5 из 5 звезд4.5/5 (838)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaОт EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaРейтинг: 4.5 из 5 звезд4.5/5 (265)
- The Emperor of All Maladies: A Biography of CancerОт EverandThe Emperor of All Maladies: A Biography of CancerРейтинг: 4.5 из 5 звезд4.5/5 (271)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersОт EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersРейтинг: 4.5 из 5 звезд4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnОт EverandTeam of Rivals: The Political Genius of Abraham LincolnРейтинг: 4.5 из 5 звезд4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaОт EverandThe Unwinding: An Inner History of the New AmericaРейтинг: 4 из 5 звезд4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyОт EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyРейтинг: 3.5 из 5 звезд3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreОт EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreРейтинг: 4 из 5 звезд4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)От EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Рейтинг: 4.5 из 5 звезд4.5/5 (119)
- Arts9 q4 Mod1 Theatricalforms v5Документ30 страницArts9 q4 Mod1 Theatricalforms v5Harold RicafortОценок пока нет
- New Company Profile.Документ8 страницNew Company Profile.Allen AsirОценок пока нет
- Activities/Assessments 2:: Determine The Type of Sampling. (Ex. Simple Random Sampling, Purposive Sampling)Документ2 страницыActivities/Assessments 2:: Determine The Type of Sampling. (Ex. Simple Random Sampling, Purposive Sampling)John Philip Echevarria0% (2)
- Process of Producting High Carbon Ferro ChromeДокумент5 страницProcess of Producting High Carbon Ferro ChromeSantosh Kumar MahtoОценок пока нет
- Monthly Business ReviewДокумент36 страницMonthly Business Reviewmdipu5_948971128Оценок пока нет
- EMarketer Time Spent With Media SnapshotДокумент13 страницEMarketer Time Spent With Media SnapshotWei ShingОценок пока нет
- Dental System SoftwareДокумент4 страницыDental System SoftwareHahaОценок пока нет
- Short Answers Class 9thДокумент14 страницShort Answers Class 9thRizwan AliОценок пока нет
- Snorkeling: A Brief History and Guide to This Underwater AdventureДокумент3 страницыSnorkeling: A Brief History and Guide to This Underwater AdventureBernadette PerezОценок пока нет
- Grade 4 DLL Quarter 2 Week 2 Sir Bien CruzДокумент47 страницGrade 4 DLL Quarter 2 Week 2 Sir Bien CruzRonel Fillomena0% (1)
- Powers of Central Govt under Environment Protection ActДокумент13 страницPowers of Central Govt under Environment Protection Actsirajudeen IОценок пока нет
- APM200 Outdoor Power Supply System User Manual-20060628-B-1.0Документ52 страницыAPM200 Outdoor Power Supply System User Manual-20060628-B-1.0Andrés MarroquínОценок пока нет
- Beyond VaR OfficialДокумент76 страницBeyond VaR OfficialmaleckicoaОценок пока нет
- HUMAN RIGHTS, RATIONALITY, AND SENTIMENTALITYДокумент13 страницHUMAN RIGHTS, RATIONALITY, AND SENTIMENTALITYJohn HunterОценок пока нет
- STS Syllabus 2020Документ27 страницSTS Syllabus 2020AndreaDimaculangan100% (1)
- Electronics Foundations - Basic CircuitsДокумент20 страницElectronics Foundations - Basic Circuitsccorp0089Оценок пока нет
- PPC2000 Association of Consultant Architects Standard Form of Project Partnering ContractДокумент5 страницPPC2000 Association of Consultant Architects Standard Form of Project Partnering ContractJoy CeeОценок пока нет
- Business Plan1Документ38 страницBusiness Plan1Gwendolyn PansoyОценок пока нет
- Neural Network For PLC PDFДокумент7 страницNeural Network For PLC PDFMarcelo Moya CajasОценок пока нет
- Intraoperative Nursing Care GuideДокумент12 страницIntraoperative Nursing Care GuideDarlyn AmplayoОценок пока нет
- The Pathogenic Basis of Malaria: InsightДокумент7 страницThe Pathogenic Basis of Malaria: InsightRaena SepryanaОценок пока нет
- The Case of Ataraxia and Apraxia in The Development of Skeptic THДокумент11 страницThe Case of Ataraxia and Apraxia in The Development of Skeptic THeweОценок пока нет
- Bahasa InggrisДокумент8 страницBahasa InggrisArintaChairaniBanurea33% (3)
- Download 12,000 Shed PlansДокумент27 страницDownload 12,000 Shed PlansRadu_IS100% (2)
- ProSteel Connect EditionДокумент2 страницыProSteel Connect EditionInfrasys StructuralОценок пока нет
- Design of Self - Supporting Dome RoofsДокумент6 страницDesign of Self - Supporting Dome RoofszatenneОценок пока нет
- So You Want To Be A NeurosugeonДокумент10 страницSo You Want To Be A NeurosugeonColby TimmОценок пока нет
- Department of Education Doña Asuncion Lee Integrated School: Division of Mabalacat CityДокумент2 страницыDepartment of Education Doña Asuncion Lee Integrated School: Division of Mabalacat CityRica Tano50% (2)
- Loverpreet Chapterv 1Документ16 страницLoverpreet Chapterv 1Sheikh SiddiquiОценок пока нет
- Marketing Budget: Expenses Q1 Q2 Q3 Q4 Totals Budget %Документ20 страницMarketing Budget: Expenses Q1 Q2 Q3 Q4 Totals Budget %Miaow MiaowОценок пока нет