Академический Документы
Профессиональный Документы
Культура Документы
dc14-0018 Full
Загружено:
Lo RakИсходное описание:
Оригинальное название
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
dc14-0018 Full
Загружено:
Lo RakАвторское право:
Доступные форматы
Effects of Weight Loss, Weight
Cycling, and Weight Loss
Maintenance on Diabetes
Incidence and Change in
Cardiometabolic Traits in the
Diabetes Prevention Program
DOI: 10.2337/dc14-0018
OBJECTIVE
This study examined specic measures of weight loss in relation to incident di-
abetes and improvement in cardiometabolic risk factors.
RESEARCH DESIGN AND METHODS
This prospective, observational study analyzed nine weight measures, character-
izing baseline weight, short- versus long-termweight loss, short- versus long-term
weight regain, and weight cycling, within the Diabetes Prevention Program (DPP)
lifestyle intervention arm (n = 1,000) for predictors of incident diabetes and im-
provement in cardiometabolic risk factors over 2 years.
RESULTS
Although weight loss in the rst 6 months was protective of diabetes (hazard ratio
[HR] 0.94 per kg, 95% CI 0.90, 0.98; P < 0.01) and cardiometabolic risk factors (P <
0.01), weight loss from 0 to 2 years was the strongest predictor of reduced diabetes
incidence (HR 0.90 per kg, 95%CI 0.87, 0.93; P < 0.01) and cardiometabolic risk factor
improvement (e.g., fasting glucose: b = 20.57 mg/dL per kg, 95% CI 20.66, 20.48;
P < 0.01). Weight cycling (dened as number of 5-lb [2.25-kg] weight cycles) ranged
06 times per participant and was positively associated with incident diabetes (HR
1.33, 95%CI 1.12, 1.58; P < 0.01), fasting glucose (b = 0.91 mg/dL per cycle; P = 0.02),
HOMA-IR (b = 0.25 units per cycle; P = 0.04), and systolic blood pressure (b = 0.94
mmHg per cycle; P = 0.01). After adjustment for baseline weight, the effect of weight
cycling remained statistically signicant for diabetes risk (HR 1.22, 95% CI 1.02, 1.47;
P = 0.03) but not for cardiometabolic traits.
CONCLUSIONS
Two-year weight loss was the strongest predictor of reduced diabetes risk and
improvements in cardiometabolic traits.
Obesity is an established risk factor for a range of complex diseases, including type 2
diabetes, cardiovascular disease, several cancers, osteoarthritis, and periodontitis.
Intentional weight loss, on the other hand, reduces the risk of most of these dis-
eases. A persons body weight can vary considerably in both the short- and long-term.
1
Diabetes Research Center, Massachusetts
General Hospital, Boston, MA
2
Department of Medicine, Harvard Medical
School, Boston, MA
3
The Biostatistics Center, George Washington
University, Rockville, MD
4
MedStar Health Research Institute, Hyattsville,
MD, and Georgetown University School of Med-
icine, Washington, DC
5
The David Geffen School of Medicine, University
of California at Los Angeles, Los Angeles, CA
6
Pennington Biomedical Research Center, Louisi-
ana State University, Baton Rouge, LA
7
Veterans Affairs Puget Sound Health Care Sys-
tem and University of Washington, Seattle, WA
8
Center for Human Genetic Research, Depart-
ment of Medicine, Massachusetts General Hos-
pital, Boston, MA
9
Program in Medical and Population Genetics,
Broad Institute, Cambridge, MA
10
Department of Medicine, Division of Endocri-
nology, Metabolism and Diabetes, University of
Colorado Anschutz Medical Campus, Aurora, CO
11
Department of Clinical Sciences, Lund Univer-
sity, Malm o, Sweden
12
Department of Nutrition, Harvard School of
Public Health, Boston, MA
Corresponding author: Linda M. Delahanty,
dppmail@bsc.gwu.edu.
Received 3 January 2014 and accepted 19 June
2014.
Clinical trial reg. no. NCT00004992, clinicaltrials
.gov.
This article contains Supplementary Data online
at http://care.diabetesjournals.org/lookup/
suppl/doi:10.2337/dc14-0018/-/DC1.
*A list of Diabetes Prevention Program Research
Group investigators is provided in the Supple-
mentary Data online.
The opinions expressed are those of the investi-
gators and do not necessarily reect the views of
the funding agencies.
2014 by the American Diabetes Association.
Readers may use this article as long as the work
is properly cited, the use is educational and not
for prot, and the work is not altered.
Linda M. Delahanty,
1,2
Qing Pan,
3
Kathleen A. Jablonski,
3
Vanita R. Aroda,
4
Karol E. Watson,
5
George A. Bray,
6
Steven E. Kahn,
7
Jose C. Florez,
1,2,8,9
Leigh Perreault,
10
and Paul W. Franks,
11,12
for the Diabetes Prevention Program
Research Group*
Diabetes Care 1
E
P
I
D
E
M
I
O
L
O
G
Y
/
H
E
A
L
T
H
S
E
R
V
I
C
E
S
R
E
S
E
A
R
C
H
Diabetes Care Publish Ahead of Print, published online July 14, 2014
Factors associated with uctuations in
body weight include many biopsychoso-
cial processes, such as genetic predispo-
sition, thoughts, and emotions, and
barriers in a persons social or cultural
environment (13). Regaining weight
after intentional weight loss is common
(4,5). Although the extent and rate of
weight regain varies greatly from one
person to the next, few studies have
considered the dynamic nature of
changes in body weight in relation to
diabetes and cardiometabolic risk
(6,7). Studies that seek to determine
the dynamic relationships between var-
iations in body weight and susceptibility
to disease may yield novel insights into
the role of obesity in chronic disease
and thus give rise to tailored interven-
tions that seek to mitigate disease risk.
The purpose of this analysis was to
compare the effects of weight loss
variables on diabetes incidence and car-
diometabolic risk factor levels in partic-
ipants who received the Diabetes
Prevention Program (DPP) weight loss
intervention. We also sought to estab-
lish an optimized set of weight loss var-
iables that are most strongly related to
the risk of type 2 diabetes.
RESEARCH DESIGN AND METHODS
Participants
The design, methods, and main out-
comes of the DPP have been published
previously (4). In the DPP, 3,234 partic-
ipants aged 25 years or older with ele-
vated fasting glucose (5.36.9 mmol/L,
or #6.9 mmol/L for American Indians),
impaired glucose tolerance (glucose
7.811.0 mmol/L 2 h after a 75-g oral
glucose load), and elevated BMI ($22
kg/m
2
for Asian Americans, $24 kg/m
2
for others) were randomly assigned to
one of three treatments: intensive life-
style intervention, metformin, or pla-
cebo control (4). This analysis was
limited to participants randomized to
the intensive lifestyle intervention. Par-
ticipants included those who had com-
pleted at least 2 years of the lifestyle
intervention to allow sufcient time to
examine uctuations in body weight af-
ter the initial 6 months of weight loss
with the core curriculum. Of the 1,079
DPP participants originally randomized
to intensive lifestyle, 63 were excluded
due to less than 2 years of total partici-
pation and another 16 were excluded
due to missing measurements, leaving
1,000 participants in the current analy-
sis (93% of the total lifestyle cohort).
Measurements for fasting glucose,
HOMA-insulin resistance (IR), triglycer-
ides, and weight at baseline were not
systematically different between the
79 excluded subjects (Supplementary
Table 1) and the 1,000 participants in-
cluded in the analysis (Table 1).
Useof thiazidediuretics or b-adrenergic
antagonists was an exclusion criterion,
but other classes of antihypertensive
agents were permitted. New medical
therapies initiated by nonstudy physicians
after enrollment were not restricted.
Study procedures and documents were
approved by institutional review boards
at all participating sites. All participants
provided written informed consent for
their participation. The study was per-
formed in accordance with the Declara-
tion of Helsinki.
Intervention
The DPP lifestyle intervention has been
previously described in detail (8). In
brief, the lifestyle intervention had two
specic goals: to facilitate $7% of
body weight loss and to achieve $150
min/week of moderate intensity physical
activity. Participants were given calorie
goals to promote weight loss deter-
mined by initial body weight and fat
gram goals that were based on 25% of
calories from fat. Lifestyle coaches met
with participants individually over the
rst 24 weeks to review a 16-session
core curriculum that focused on diet,
physical activity, and strategies for be-
havioral modication. After the rst 6
months, lifestyle coaches offered tai-
lored individual sessions at least once
every 2 months and group classes/cam-
paigns three times per year to help im-
prove physical activity levels and sustain
weight loss.
Outcomes Measures
Subjects were weighed in light clothing
without shoes at each intervention and
outcome visit. Diabetes incidence was de-
termined by fasting plasma glucose levels
every 6 months and 2-h glucose levels
from 75-g oral glucose tolerance tests
performed annually. Diabetes events
through the 1.5-year check-up (before
the 2-year follow-up) are excluded from
our analysis for the diabetes outcome (n =
48), and only those between year 2 and
the end of DPP (July 31, 2001) are consid-
ered (n = 952). Therefore, the risk of
diabetes conditional on the fact that a
participant was diabetes-free before the
2-year follow-up is modeled. Cardiometa-
bolic risk factor assessments were done
for fasting glucose (mg/dL), insulin resis-
tance (HOMA-IR) (9,10), fasting triglycer-
ides (mg/dL), and systolic blood pressure
(SBP; mmHg). Cardiometabolic outcome
measures were madeat the 2-year follow-
up assessment.
Weight Loss Variables
To determine which aspects of weight
loss were most strongly related to the
incidence of diabetes and levels of car-
diometabolic risk factors, nine separate
variables for weight or weight loss over
specic time intervals were examined.
These included:
c Baseline weight (kg)
c Weight loss (kg) from baseline (im-
mediate loss) to:
+ 1 month
+ 3 months
+
6 months
+
2 years
c Weight loss (kg) up to 24 months (de-
layed loss):
+ From 6 to 24 months
+
From 18 to 24 months
c Weight cycling: A complete weight
cycle is dened as a 5-lb (2.25-kg) or
more weight loss from the highest
weight since last cycle and then a
5-lb (2.25-kg) or more weight regain
from the lowest weight since the
last cycle. Weight cycling for a given
participant is the number of such
cycles in the 2-year period starting
from the DPP baseline.
c Average weight in the rst 2 years:
The weighted average of the avail-
able weight measures from baseline
to year 2, where each weight obser-
vation is weighted by the time dura-
tion between this measure and its
previous measure.
Statistical Methods
The relationships of the weight variables
with diabetes incidence and cardiome-
tabolic risk factor levels were estimated
using Cox proportional hazards and lin-
ear regression models, respectively. Co-
variates included age at randomization
(years), race, sex, and the corresponding
baseline measure of glucose, HOMA-IR,
SBP, and triglyceride level. The Pearson
correlation coefcient between the
baseline weight and weight loss from
2 Weight Change Affects Diabetes Incidence Diabetes Care
1, 3, and 6 months and 2 years to base-
line, weight cycles, and average weight
in the rst 2 years were signicantly dif-
ferent from zero (P , 0.01; Table 2).
Therefore, baseline weight was not con-
trolled for due to the moderate-to-high
degree of correlations between baseline
weight and some of the other measures
of weight.
To assess the effects of weight cycling
beyond baseline weight, 2-year weight
loss, and average weight, we performed
secondary analyses where baseline
weight, 2-year weight loss, and average
weight were adjusted in addition to num-
ber of 5-lb weight cycles. Assessments of
weight loss from 18 to 24 months were
replaced in the Cox models by a variable
quantifying weight loss in the most re-
cent 6 months, which was treated as a
time-varying coefcient. Outliers in the
cardiometabolic outcomes (one in fasting
glucose, one in HOMA-IR, and one in
SBP) were deleted before linear regres-
sion analyses were performed for the
corresponding outcomes.
One model was tted for each combi-
nation of outcome and weight measure.
For the same outcome, we compared
the size of the coefcients correspond-
ing to different standardized weight
measures. For example, we tted nine
models for the same fasting glucose
Table 1Weight variables and cardiometabolic risk factors of the study cohort
Mean SD Minimum 25th percentile Median 75th percentile Maximum
Baseline
Fasting glucose (mg/dL) 106.27 8.15 76.00 100.00 105.00 112.00 139.00
HOMA-IR 6.99 4.33 0.56 4.15 6.05 8.89 54.46
Triglyceride (mg/dL) 163.42 97.38 31.00 98.00 139.00 198.00 796.00
SBP (mmHg) 123.42 14.63 84.00 112.00 122.00 132.00 175.00
At year 2
Fasting glucose (mg/dL) 104.92 14.78 74.00 97.00 103.00 110.00 331.00
HOMA-IR 5.97 4.67 0.46 3.20 4.87 7.31 60.03
Triglyceride (mg/dL) 140.95 84.00 31.00 86.00 118.00 169.00 672.00
SBP (mmHg) 120.12 14.72 84.00 110.00 119.00 129.00 209.00
Baseline weight (kg) 93.70 20.29 48.60 79.00 90.90 104.58 192.20
Weight loss from baseline to (kg)
1 month 1.38 2.66 217.17 20.18 1.27 2.83 15.85
3 months 4.40 3.87 29.62 1.79 4.13 6.51 25.27
6 months 6.84 5.62 213.25 3.20 6.45 9.60 35.55
2 years 5.39 7.56 219.15 1.05 4.50 8.50 77.50
Weight loss from (kg)
18 months to 2 years 21.38 5.73 227.60 24.35 21.20 1.13 49.20
6 months to 2 years 20.61 3.18 217.95 22.25 20.60 0.90 33.60
5-lb weight cycles (n) 1.45 0.99 0 1 1 2 6
Average weight (kg) 83.03 19.87 44.93 74.02 84.57 98.66 188.68
All body composition variables are raw weight loss values in the units of kilograms. The study sample consisted of 1,000 intensive lifestyle participants
with at least 2 years of follow-up and excluded participants who developed diabetes during those 2 years (n = 952).
Table 2Pearson partial correlation coefcients between the nine weight metrics conditional on age at enrollment
BL
weight
BL to 1
month
BL to 3
months
BL to 6
months
18 months to 2
years
BL to 2
years
6 months to 2
years
5-lb cycles
(n)
Avg
weight
BL weight 1 0.10 0.26 0.33 0.01 0.20 20.06 0.35 0.96
0.00 ,0.01 ,0.01 0.78 ,0.01 0.10 ,0.01 ,0.01
BL to 1 month 1 0.80 0.60 20.07 0.38 20.10 0.05 20.06
,0.01 ,0.01 0.03 ,0.01 0.00 0.13 0.08
BL to 3 months 1 0.86 20.08 0.56 20.12 0.06 0.04
,0.01 0.02 ,0.01 0.00 0.09 0.24
BL to 6 months 1 20.10 0.67 20.12 0.05 0.08
,0.01 ,0.01 0.00 0.14 0.02
18 months to
2 years
1 0.26 0.45 20.11 0.03
,0.01 ,0.01 0.00 0.39
BL to 2 years 1 0.66 20.10 20.06
,0.01 0.00 0.09
6 months to
2 years
1 20.19 20.16
,0.01 ,0.01
No. of 5-lb cycles 1 0.38
,0.01
BL, baseline.
care.diabetesjournals.org Delahanty and Associates 3
outcome and obtained nine coefcient
estimates for the nine standardized
weight measures. Weight measures
were standardized by the corresponding
ethnic- and sex-specic SDs, which yield
directly comparable regression coef-
cient estimates. Therefore, the regres-
sion coefcient of each measure of
weight is the difference in the outcome
corresponding to 1 SD change in the
given weight measure. Pairwise com-
parisons among the nine coefcients
were made. We then tested whether
the difference between a pair of coef-
cients varied from zero.
The most predictive single weight var-
iable was selected, whose model was
called the core model. To determine
whether a combination of the weight
variables could be dened that im-
proved the predictive accuracy for inci-
dent diabetes of the core model,
expanded models that included addi-
tional weight variables besides the co-
variates in the core model were
selected, and the predictive ability of
different models was assessed consider-
ing both statistical signicance and clin-
ical importance. Statistical selection of
candidate weight measures was done
by stepwise model selections, with a sig-
nicance level for variable entry of P =
0.25 and a signicance level for variable
removal of P = 0.15. The three strongest
predictors of diabetes identied
through the stepwise model selection
ranked by effect sizes, are 1) weight
loss from baseline to year 2, 2) average
weight in the rst 2 years, and 3) weight
loss in the rst month after randomiza-
tion. None of these variables was collin-
ear (variance ination factor ,2).
We also estimated the predictive ac-
curacy of the logistic model including
the top three weight measures (11). Fur-
thermore, three sets of sensitivity anal-
yses were tested to determine the
prognostic power of weight loss from
baseline to year 2 on diabetes risk by
adding dietary and physical activity
measurements to the model. In the rst
sensitivity analysis, the average daily ca-
loric intake calculated from food fre-
quency questionnaires at baseline and
year 1 was added to the Cox model of
2-year weight loss and demographic var-
iables. In the second sensitivity analysis,
average physical activity measured in
metabolic hours per week at baseline
and year 1 was added in addition to
the same core model. In the third sensi-
tivity analysis, average daily caloric in-
take and weekly physical activity in
metabolic hours per week were both
added. All calculations were done using
SAS 9.2 software (SAS Institute, Cary,
NC).
RESULTS
At baseline, this subgroup of lifestyle
participants was 51 (SD 11) years old
on average, 68% were women, and
54% were white, 18% African American,
16%, Hispanic American 5% Native
American, and 6% Asian American by
self-reported ethnicity. Participants
mean BMI was 33.77 (SD 6.56) kg/m
2
.
Other weight measures and cardiometa-
bolic risk factors are outlined in Table 1.
The cohort achieved a mean weight loss
of 6.84 (SD 5.62) kg at 6 months and
sustained a mean weight loss of 5.39
(SD 7.56) kg at 2 years. After completion
of the core curriculum at 6 months,
there was a modest mean weight regain
of 0.61 (SD 3.18) kg over the ensuing 18
months, with more rapid weight gain
(mean 1.38 [SD 5.73] kg) between 18
months and 24 months. From baseline
to 2 years, there were small changes in
fasting glucose and systolic blood pres-
sure, with greater changes in HOMA-IR
and triglyceride levels. The average
number of 5-lb (2.25-kg) weight cycles
was 1.45, with a range of 06 weight
cycles over 2 years. Weight cycling was
more frequent in men than in women
(1.59 vs. 1.39 cycles/year, P , 0.01),
younger participants (1.60 cycles/year
for age ,45 years vs. 1.40 for 4559
years, and 1.35 for $60 years, P =
0.01), and in African Americans than
other ethnic groups (1.68 vs. 1.001.44
cycles/year, P , 0.01).
Table 2 summarizes the pairwise par-
tial correlation coefcients between
weight variables conditional on age at
enrollment. Baseline body weight and
several weight loss variables were sig-
nicantly correlated with one another.
Higher baseline weight correlated
with a larger number of weight cycles
(r = 0.35, P , 0.01), weight loss (6
months: r = 0.33, P , 0.01; 2 years: r =
0.2, P , 0.01), and a larger average
weight in the rst 2 years (r = 0.96, P ,
0.01), but not weight regain between 6
and 24 months (P = 0.10) or from 18 to
24 months (P = 0.78). More initial weight
loss (e.g., baseline to 1 month weight
loss) was associated with greater subse-
quent weight loss from baseline to 24
months (r = 0.38, P , 0.01) and less
weight loss/greater weight regain be-
tween 6 and 24 months (r = 20.10,
P , 0.01) but not with more weight cy-
cling (number of 5-lb (2.27-kg) weight
cycles; P = 0.13). Weight cycling was cor-
related with average weight in the rst 2
years (r = 0.38, P , 0.001), less weight
loss/greater weight regain between 6
and 24 months (r = 0.19, P , 0.01) and
between 18 and 24 months (r = 20.11,
P ,0.01), and less long-termweight loss
at 2 years (r = 20.10, P , 0.01).
There were 99 incident diabetes
events ascertained during a median
follow-up of 3 years (range 24.5 years).
Table 3 reports the estimated effects
of a 1-unit (kg or weight cycle) change
in the weight loss variable on diabetes
incidence and glucose concentrations,
HOMA-IR, SBP, and triglyceride concen-
trations at 2 years. Figure 1 shows the
comparative effects of 1-SD change spe-
cic to ethnic/gender of the various
body weight variables on diabetes inci-
dence, and cardiometabolic outcomes
at 2 years. Greater weight loss in the
rst 6 months and from 6 months to 2
years were both predictive of reduced
diabetes incidence; however, overall
weight loss from baseline to 2 years
was the strongest single predictor of
lower diabetes incidence. The effects
of 2-year weight loss on diabetes risk
were not affected by further adjusting
for covariates measuring caloric intake
and physical activity (data not shown).
Weight cycling (dened as number of
5-lb weight cycles) was predictive of an
increased incidence of diabetes. More-
over, the effect of weight cycling on di-
abetes risk remained statistically
signicant in models adjusted for base-
line weight (hazard ratio [HR] 1.22, 95%
CI 1.02, 1.48; P = 0.03) or 2-year weight
loss (HR 1.22, 95% CI 1.02, 1.47; P =
0.03). The effect of the number of 5-lb
weight cycles was no longer signicant
when baseline weight and 2-year weight
loss were both included in the same
model (HR 1.11, 95% CI 0.91, 1.35; P =
0.29) or when average weight over 2
years was included in the model (HR
1.15, 95% CI 0.95, 1.39; P = 0.15).
The expanded model including demo-
graphic variables, 2-year weight loss,
1-month weight loss, and average weight
adds signicant predictive power to the
4 Weight Change Affects Diabetes Incidence Diabetes Care
core model (P , 0.01 compared with
the core model). The areas under the
curve (AUCs) of the core model (demo-
graphics and 2-year weight loss) and the
expanded models described above were
0.72 and 0.76, respectively. The AUC in
the model including the top three
weight measures was 0.76, which was
essentially the same as the logistic
model including all candidate weight
measures (AUC 0.76; P = 0.90 for differ-
ence between AUCs). Weight cycling
raised the risk of diabetes (HR 1.33,
95% CI 1.12, 1.58; P = 0.001) but did
not signicantly add to the predictive
accuracy of the core model (P = 0.28).
Cardiometabolic Outcomes
Weight loss was predictive of improved
cardiometabolic outcomes in both the
rst 6 months and from 6 months to 2
years, but again, was not as predictive as
total weight loss from baseline to 2
years. Weight loss from 18 months to
2 years was a signicant predictor of im-
proved triglyceride levels and insulin
sensitivity at 2 years but was not a sig-
nicant predictor of the other cardiome-
tabolic traits or diabetes incidence.
Weight cycling was associated with
worsening of most cardiometabolic risk
factor levels except for fasting triglycer-
ides: fasting glucose (b = 0.91, 95% CI
0.17, 1.65 mg/dL per kg; P = 0.02),
HOMA-IR (b = 0.25, 95% CI 0.01, 0.49
per kg; P = 0.04), and SBP (b = 0.94,
95% CI 0.19, 1.68 mmHg per kg; P =
0.01); however, these effects were no
longer statistically signicant when ad-
justed for baseline weight or 2-year
weight loss.
CONCLUSIONS
This study expands on previous research
by examining the relative importance of
several measures of body weight as pre-
dictors of diabetes and changes in car-
diometabolic risk factors and identifying
an optimized set of weight loss variables
associated with diabetes risk. We com-
pared the strength and magnitude of
the associations for various weight loss
variables with the change in cardiome-
tabolic levels and diabetes incidence to
quantify the short- and long-term time-
dependent effects of weight loss, recent
weight loss, degree of exposure to ex-
cess weight, and weight cycling in the
rst 2 years of the DPP trial. Although
weight loss during the rst 6 months of
T
a
b
l
e
3
E
s
t
i
m
a
t
e
d
e
f
f
e
c
t
s
(
H
R
o
r
c
o
e
f
c
i
e
n
t
)
o
f
t
h
e
b
o
d
y
w
e
i
g
h
t
d
y
n
a
m
i
c
s
o
n
d
i
a
b
e
t
e
s
i
n
c
i
d
e
n
c
e
a
n
d
c
a
r
d
i
o
m
e
t
a
b
o
l
i
c
o
u
t
c
o
m
e
s
D
i
a
b
e
t
e
s
i
n
c
i
d
e
n
c
e
F
a
s
t
i
n
g
g
l
u
c
o
s
e
(
m
g
/
d
L
)
H
O
M
A
-
I
R
T
r
i
g
l
y
c
e
r
i
d
e
s
(
m
g
/
d
L
)
S
B
P
(
m
m
H
g
)
H
R
9
5
%
C
I
P
b
9
5
%
C
I
P
b
9
5
%
C
I
P
b
9
5
%
C
I
P
b
9
5
%
C
I
P
B
L
w
e
i
g
h
t
1
.
0
2
1
.
0
1
,
1
.
0
3
,
0
.
0
1
0
.
0
8
0
.
0
4
,
0
.
1
2
0
.
0
1
0
.
0
4
0
.
0
2
,
0
.
0
5
,
0
.
0
1
0
.
1
0
2
0
.
1
1
,
0
.
3
0
0
.
3
6
0
.
0
9
0
.
0
5
,
0
.
1
2
,
0
.
0
1
B
L
t
o
1
m
o
n
t
h
0
.
9
3
0
.
8
6
,
1
.
0
0
0
.
0
5
2
0
.
4
7
2
0
.
7
5
,
0
.
2
0
,
0
.
0
1
2
0
.
2
8
2
0
.
3
7
,
0
.
1
9
,
0
.
0
1
2
1
.
3
4
2
2
.
8
3
,
0
.
1
4
0
.
0
8
2
0
.
3
5
2
0
.
6
4
,
0
.
0
7
0
.
0
1
B
L
t
o
3
m
o
n
t
h
s
0
.
9
1
0
.
8
6
,
0
.
9
7
,
0
.
0
1
2
0
.
6
7
2
0
.
8
6
,
2
0
.
4
7
,
0
.
0
1
2
0
.
2
7
2
0
.
3
3
,
2
0
.
2
1
,
0
.
0
1
2
1
.
7
7
2
2
.
8
1
,
2
0
.
7
3
,
0
.
0
1
2
0
.
3
7
2
0
.
5
6
,
2
0
.
1
7
,
0
.
0
1
B
L
t
o
6
m
o
n
t
h
s
0
.
9
4
0
.
9
0
,
0
.
9
8
,
0
.
0
1
2
0
.
5
9
2
0
.
7
2
,
2
0
.
4
6
,
0
.
0
1
2
0
.
2
2
2
0
.
2
6
,
2
0
.
1
8
,
0
.
0
1
2
1
.
6
8
2
2
.
3
8
,
2
0
.
9
9
,
0
.
0
1
2
0
.
3
5
2
0
.
4
8
,
2
0
.
2
1
,
0
.
0
1
B
L
t
o
2
y
e
a
r
s
0
.
9
0
0
.
8
7
,
0
.
9
3
,
0
.
0
1
2
0
.
5
7
2
0
.
6
6
,
2
0
.
4
8
,
0
.
0
1
2
0
.
2
0
2
0
.
2
3
,
2
0
.
1
7
,
0
.
0
1
2
2
.
2
7
2
2
.
7
6
,
2
1
.
7
8
,
0
.
0
1
2
0
.
3
0
2
0
.
4
0
,
2
0
.
2
1
,
0
.
0
1
L
a
s
t
6
m
o
n
t
h
s
0
.
9
5
0
.
8
9
,
1
.
0
1
0
.
1
2
2
0
.
2
2
2
0
.
4
5
,
0
.
0
1
0
.
0
6
2
0
.
1
1
2
0
.
1
8
,
2
0
.
0
4
,
0
.
0
1
2
1
.
8
5
2
3
.
0
7
,
2
0
.
6
4
,
0
.
0
1
2
0
.
1
5
2
0
.
3
9
,
0
.
0
8
0
.
1
9
6
m
o
n
t
h
s
t
o
2
y
e
a
r
s
0
.
9
1
0
.
8
8
,
0
.
9
5
,
0
.
0
1
2
0
.
4
6
2
0
.
5
8
,
2
0
.
3
3
,
0
.
0
1
2
0
.
1
5
2
0
.
1
9
,
2
0
.
1
1
,
0
.
0
1
2
2
.
3
8
2
3
.
0
3
,
2
1
.
7
2
,
0
.
0
1
2
0
.
2
0
2
0
.
3
3
,
2
0
.
0
7
,
0
.
0
1
5
-
l
b
c
y
c
l
e
s
(
n
)
1
.
3
3
1
.
1
2
,
1
.
5
8
,
0
.
0
1
0
.
9
1
0
.
1
7
,
1
.
6
5
0
.
0
2
0
.
2
5
0
.
0
1
,
0
.
4
9
0
.
0
4
2
.
5
7
2
1
.
3
5
,
6
.
5
0
0
.
2
0
0
.
9
4
0
.
1
9
,
1
.
6
8
0
.
0
1
A
v
g
w
e
i
g
h
t
i
n
2
y
e
a
r
s
1
.
0
5
1
.
0
3
,
1
.
0
7
,
0
.
0
1
0
.
3
0
0
.
2
2
,
0
.
3
8
,
0
.
0
1
0
.
1
4
0
.
1
0
,
0
.
1
6
,
0
.
0
1
0
.
6
8
0
.
2
6
,
1
.
1
0
,
0
.
0
1
0
.
2
6
0
.
1
8
,
0
.
3
4
,
0
.
0
1
B
L
,
b
a
s
e
l
i
n
e
.
T
h
e
P
v
a
l
u
e
s
a
r
e
o
u
t
p
u
t
f
r
o
m
i
n
d
i
v
i
d
u
a
l
r
e
g
r
e
s
s
i
o
n
s
f
o
r
t
h
e
s
p
e
c
i
c
o
u
t
c
o
m
e
a
n
d
w
e
i
g
h
t
m
e
t
r
i
c
c
o
m
b
i
n
a
t
i
o
n
w
i
t
h
o
u
t
a
d
j
u
s
t
m
e
n
t
s
f
o
r
m
u
l
t
i
p
l
e
t
e
s
t
s
.
A
l
l
w
e
i
g
h
t
m
e
a
s
u
r
e
s
a
r
e
i
n
k
i
l
o
g
r
a
m
s
e
x
c
e
p
t
f
o
r
n
u
m
b
e
r
o
f
5
-
l
b
w
e
i
g
h
t
c
y
c
l
e
s
.
care.diabetesjournals.org Delahanty and Associates 5
the lifestyle intervention was a major
predictor of reduced incidence of diabe-
tes, the strongest predictor of reduced
diabetes risk and improvements in car-
diometabolic traits was the overall 2-
year weight loss: every kilogram of
weight loss in the rst 6 months of the
trial corresponded with a 6% reduction
in risk of diabetes, whereas every kilo-
gram of weight loss from baseline to 2
years corresponded with a 10% de-
crease in the risk of diabetes. Our results
differ fromthose previously reported by
Hamman et al. (12) because we exam-
ined the development of diabetes from
year 2 until study end and excluded
those who had less than 2 years of
follow-up and those who developed di-
abetes within the rst 1.5 years of the
intervention.
For all cardiometabolic traits, the
overall weight loss at 2 years was a bet-
ter predictor than average weight in
the rst 2 years. Interestingly, the initial
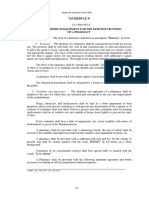
Figure 1Estimated effects (HR or coefcient) and the corresponding 95% condence intervals of body weight dynamics on diabetes risks (A),
fasting glucose (B), HOMA-IR (C), triglyceride levels (D), and SBP (E).
6 Weight Change Affects Diabetes Incidence Diabetes Care
6-month weight loss appears to be a bet-
ter predictor for the reduction in fasting
blood glucose, SBP and HOMA-IR than
the most recent 6-month weight loss,
whereas the most recent 6-month
weight loss was a predictor of both lower
triglyceride levels and improved insulin
sensitivity.
We also identied an optimized set of
weight loss variables for predicting inci-
dent diabetes in the DPP, which includes
1-month weight loss, 2-year weight loss,
and either initial body weight or expo-
sure to excess body weight over 2 years.
These results suggest that there are
added benets to early rapid weight
loss in the rst month in the context of
successful 2-year weight loss results,
particularly for those who have higher
initial body weights.
Our results are consistent with previ-
ous reports that have shown that weight
losses that are not maintained are not as
effective in reducing the risk of diabetes
as those that are maintained (12). Our
ndings regarding the importance of the
pattern of weight loss are also consis-
tent with ndings from the Look AHEAD
(Action for Health in Diabetes) trial, an-
other long-term intentional weight loss
study in people with diabetes. In Look
AHEAD, greater overall weight losses
had the strongest relationship with im-
proved cardiovascular disease risk fac-
tors at 4 years; however, a pattern of
larger month-to-month weight loss dur-
ing the rst year was also predictive of
greater improvements in glycated he-
moglobin, HDL cholesterol, and SBP at
4 years, independent of total weight
loss (6). These studies and our data em-
phasize that early larger weight losses
that are sustained seemto confer added
benets for reducing the risk of diabetes
and improving cardiometabolic out-
comes in the medium-term.
Weight cycling and the average
weight in the rst 2 years were both
among the top three predictors of in-
creased incidence of diabetes, implying
that continued efforts to reduce expo-
sure to excess body weight are impor-
tant in reducing the risk of diabetes. The
effect of weight cycling on diabetes risk
was still signicant even after adjusting
for baseline weight or 2-year weight
change, but not after adjusting for aver-
age weight in the rst 2 years. Impor-
tantly, however, in a translational
setting, one would not know the long-
term weight change before or during
the intervention period, and so focusing
on reducing weight cycling and prevent-
ing weight gain are logical and com-
plimentary objectives for diabetes
prevention. Moreover, a patients base-
line weight is clearly not the focus of an
intervention. Thus, in the context of
translation, the correlations among
baseline weight, average weight, and
weight cycling are important for a clini-
cian to consider, because heavier pa-
tients are more likely to weight cycle
and develop diabetes. Nevertheless,
this does not mean diabetes risk is not
affected by weight cycling in these pa-
tients or that one should not focus on
reducing weight cycling for diabetes
prevention. By contrast, we conclude
for the cardiometabolic traits that
weight cycling does not convey effects
that are independent of baseline weight
or 2-year weight change.
Our ndings generally agree with
those reported elsewhere that indicate
that weight cycling is associated with
weight regain, increased risk of hyper-
tension and diabetes, and elevations in
other cardiometabolic traits (2,1317).
In contrast to previous studies that
have categorized the magnitude and
frequency of weight cycling (13,15,17)
(e.g., 59, 1019, 2049, and $50 lb)
(13), we measured the effects of the
number of weight cycles (gain and
loss) of at least 5 lb because most DPP
participants did not have 10-lb weight
cycles over 2 years of follow-up. Al-
though our ndings show that overall
weight status is an important determi-
nant of diabetes and cardiometabolic
risk and that overall weight loss lowers
risk, avoiding weight regain of more
than 5 lb also appears to be clinically
important.
A strength of our study is that we ex-
amined and compared the relative impor-
tance of a variety of weight loss variables
in a well-characterized, ethnically diverse
cohort of people with impaired glucose
tolerance that was pursuing intentional
weight loss. We also used weight change
data from actual clinic visits rather than
from self-reported weights to assess
weight cycling.
However, these ndings must also be
interpreted with several limitations in
mind. Many estimated effects are statis-
tically signicant but may not be clinically
relevant due to the large sample size. The
results fromanalyses focused on estimat-
ing the HRs of each weight variable on
diabetes and cardiometabolic outcomes
are not adjusted for multiple testing.
This is because extensive existing evi-
dence supports an effect of body weight
change on diabetes risk; thus, the prior
probability of association is likely to be
greater than the null, which is not consid-
ered in conventional multiple test correc-
tion procedures. By clearly dening the
number of tests performed and present-
ing nominal P values, we provide the
necessary information for readers to de-
termine for themselves the possibility
that these associations represent true
positive effects. Potential confounding
factors include changes in diet or activity
that vary within the intervention and
could affect development or worsening
of cardiometabolic risk factors. Although
we measured changes in body weight,
weight cycling, and magnitude of expo-
sure to excess body weight, we did not
examine body fat distribution by waist cir-
cumference or visceral fat, andweight as a
proxy for change in adiposity may lack
precision. Because the DPP is a multieth-
nic cohort of people at high-risk for diabe-
tes, theseresults may not begeneralizable
to individuals at a lower risk of diabetes.
These ndings have several important
clinical implications. First, current pro-
grams that focus on translating the rst
months of the DPP lifestyle intervention
need to consider offering maintenance
programs to maximize sustainability of
weight loss, improvements in cardiome-
tabolic risk factors, and the potential to
prevent or delay diabetes. Early rapid
weight loss that is sustained may confer
additional benets for reducing the risk
of diabetes. Although lapses in eating
behavior may lead to weight regain
and some weight cycling, the ability to
refocus on weight loss behaviors and
achieve weight loss overall appears to
be most important for diabetes preven-
tion and improved cardiometabolic out-
comes. Nevertheless, minimizing weight
cycling is also important for reducing di-
abetes risk and for psychological well-
being and perceived self-efcacy related
to weight loss. Efforts to promote
weight loss should seek to achieve this
in a manner that is steady and consis-
tent over time.
In conclusion, the overall 2-year weight
loss among the DPP lifestyle intervention
participants was the strongest predictor
care.diabetesjournals.org Delahanty and Associates 7
of reduced risk for diabetes and improve-
ments in cardiometabolic traits com-
pared with eight other body weight
variables. Early rapid weight loss in the
context of successful 2-year weight loss
also provided added benet in diabetes
risk reduction. In the context of the DPPs
intentional weight loss program, weight
cycling was associatedwithoverall weight
regain, increased risk of diabetes, and el-
evations in SBP, insulin resistance, and
fasting glucose. Weight cycling conferred
an increased risk for diabetes indepen-
dent of baseline weight or 2-year weight
change but not when both were consid-
ered simultaneously or when average
weight over 2 years was considered. The
effects of weight cycling on the cardiome-
tabolic traits were not statistically signi-
cant when baseline weight or 2-year
weight were conditioned upon. Dening
the weight loss variables that are most
strongly associated with the reduced in-
cidence of diabetes and improvements
in cardiometabolic traits may have impli-
cations for the choice of approaches in
studies that examine genetic inuences
on weight loss and in the translation of
ndings from studies such as the DPP to
clinical practice.
Acknowledgments. The DPP investigators
gratefully acknowledge the commitment and
dedication of the participants of the DPP.
Funding Support. The National Institute of
Diabetes and Digestive and Kidney Diseases
(NIDDK) of the National Institutes of Health
(NIH) provided funding to the clinical centers
and the coordinating center for the design and
conduct of the study and the collection, man-
agement, analysis, and interpretation of the
data (U01-DK-048489). The Southwestern
American Indian Centers were supported di-
rectly by the NIDDK and the Indian Health
Service. The General Clinical Research Center
Program, National Center for Research Resources
and the Department of Veterans Affairs sup-
ported data collection at many of the clinical
centers. Funding for data collection and partic-
ipant support was also provided by the Ofce
of Research on Minority Health, the National
Institute of Child Health and Human Develop-
ment, the National Institute on Aging, the
Centers for Disease Control and Prevention,
the Ofce of Research on Womens Health, and
the American Diabetes Association. Bristol-
Myers Squibb and Parke-Davis provided medi-
cation. This research was also partly supported
by the intramural research program of the
NIDDK. LifeScan Inc., Health o meter, Hoechst
Marion Roussel, Inc., Merck-Medco Managed
Care, Inc., Merck and Co., Nike Sports Market-
ing, Slim Fast Foods Co., and Quaker Oats Co.
donated materials, equipment, or medicines for
concomitant conditions. McKesson BioServices
Corp., Matthews Media Group, Inc., and the
Henry M. Jackson Foundation provided support
services under subcontract with the coordi-
nating center. A complete list of centers, in-
vestigators, and staff can be found in the
Supplementary Data online. K.A.J. (the DPP Ge-
netics Program) has a research grant from NIH
(R01-DK072014). J.C.F. has received NIH grants
(R01-DK072041). P.W.F. is supported by the
Department of Clinical Sciences, Lund University
and the Department of Nutrition, Harvard Uni-
versity. P.W.F. has received speaking honoraria
from academic and nonprot organizations.
Duality of Interest. L.M.D. has a nancial
interest in Omada Health, a company that devel-
ops online behavior-change programs, with a
focus on diabetes. These interests were reviewed
and are managed by Massachusetts General
Hospital and Partners HealthCare in accordance
with their conict of interest policies. J.C.F. has
received consulting honoraria fromNovartis, Lilly,
and Pzer. P.W.F. has received speaking hono-
raria from Novo Nordisk and has research grants
from Novo Nordisk.
Author contributions. L.M.D., Q.P., and P.W.F.
researched the data and wrote the manu-
script. K.A.J., V.R.A., K.EW., G.A.B., S.E.K., and
J.C.F., and L.P. reviewed and edited the manu-
script. P.W.F. is the guarantor of this work and,
as such, had full access to all the data in the
study and takes responsibility for the integrity
of the data and the accuracy of the data
analysis.
References
1. Papas MA, Alberg AJ, Ewing R, Helzlsouer KJ,
Gary TL, Klassen AC. The built environment and
obesity. Epidemiol Rev 2007;29:129143
2. Teixeira PJ, Going SB, Sardinha LB, Lohman
TG. A review of psychosocial pre-treatment pre-
dictors of weight control. Obes Rev 2005;6:43
65
3. Hill JO, Galloway JM, Goley A, et al. Scientic
statement: sociological determinants of predia-
betes and type 2 diabetes. Diabetes Care 2013;
36:110
4. Knowler WC, Barrett-Connor E, Fowler SE,
et al.; Diabetes Prevention Program Research
Group. Reduction in the incidence of type 2 di-
abetes with lifestyle intervention or metformin.
N Engl J Med 2002;346:393403
5. Wing RR; Look AHEADResearch Group. Long-
termeffects of a lifestyle intervention on weight
and cardiovascular risk factors in individuals
with type 2 diabetes mellitus: four-year results
of the Look AHEAD trial. Arch Intern Med 2010;
170:15661575
6. Neiberg RH, Wing RR, Bray GA, et al.; Look
AHEAD Research Group. Patterns of weight
change associated with long-term weight
change and cardiovascular disease risk factors
in the Look AHEADStudy. Obesity (Silver Spring)
2012;20:20482056
7. Maruthur NM, Ma Y, Delahanty LM, et al.; for
the Diabetes Prevention Research Group. Early
response to preventive strategies in the Diabe-
tes Prevention Program. J Gen Intern Med 2013;
28:16291636
8. Diabetes Prevention Program (DPP) Research
Group. The Diabetes Prevention Program (DPP):
description of lifestyle intervention. Diabetes
Care 2002;25:21652171
9. Matthews DR, Hosker JP, Rudenski AS, Naylor
BA, Treacher DF, Turner RC. Homeostasis model
assessment: insulin resistance and beta-cell
function fromfasting plasma glucose and insulin
concentrations in man. Diabetelogia 1985;28:
412419
10. Haffner S, Temprosa M, Crandall J, et al.;
Diabetes Prevention Program Research Group.
Intensive lifestyle intervention or metformin on
inammation and coagulation in participants
with impaired glucose tolerance. Diabetes
2005;54:15661572
11. DeLong ER, DeLong DM, Clarke-Pearson DL.
Comparing the areas under two or more corre-
lated receiver operating characteristic curves:
a nonparametric approach. Biometrics 1988;
44:837845
12. Hamman RF, Wing RR, Edelstein SL, et al.
Effect of weight loss with lifestyle intervention
on risk of diabetes. Diabetes Care 2006;29:
21022107
13. Field AE, Byers T, Hunter DJ, et al. Weight
cycling, weight gain, and risk of hypertension in
women. Am J Epidemiol 1999;150:573579
14. Guagnano MT, Pace-Palitti V, Carrabs C,
Merlitti D, Sensi S. Weight uctuations could
increase blood pressure in android obese
women. Clin Sci (Lond) 1999;96:677680
15. Guagnano MT, Ballone E, Pace-Palitti V,
et al. Risk factors for hypertension in obese
women. The role of weight cycling. Eur J Clin
Nutr 2000;54:356360
16. Waring ME, Eaton CB, Lasater TM, Lapane
KL. Incident diabetes in relation to weight pat-
terns during middle age. Am J Epidemiol 2010;
171:550556
17. French SA, Folsom AR, Jeffery RW, Zheng
W, Mink PJ, Baxter JE. Weight variability and
incident disease in older women: the Iowa
Womens Health Study. Int J Obes Relat Metab
Disord 1997;21:217223
8 Weight Change Affects Diabetes Incidence Diabetes Care
Вам также может понравиться
- Low Carb StudyДокумент15 страницLow Carb StudycphommalОценок пока нет
- ANNALS-Diabetes Tipo IIДокумент16 страницANNALS-Diabetes Tipo IIewb100% (2)
- Articulo Dislipidemias 2Документ18 страницArticulo Dislipidemias 2DANIELA CALDERON SAGAHONОценок пока нет
- Research: Cite This As: BMJ 2010 341:c3337Документ7 страницResearch: Cite This As: BMJ 2010 341:c3337Deepak DahiyaОценок пока нет
- Diabetes MellitusДокумент8 страницDiabetes Mellitusi_anitaОценок пока нет
- Articulo Dislipidemias 2Документ16 страницArticulo Dislipidemias 2DANIELA CALDERON SAGAHONОценок пока нет
- Out 11Документ7 страницOut 11AnamОценок пока нет
- Effects of A Three-Armed Randomised Controlled TriДокумент11 страницEffects of A Three-Armed Randomised Controlled TriGrigorina MitrofanОценок пока нет
- Dia Care 2002 Pastors 608 13Документ6 страницDia Care 2002 Pastors 608 13Isnar Nurul AlfiyahОценок пока нет
- Am J Clin Nutr 2016 Valsesia Ajcn.116.137646Документ10 страницAm J Clin Nutr 2016 Valsesia Ajcn.116.137646kasabeОценок пока нет
- 2 Year Paleo TrialДокумент8 страниц2 Year Paleo TrialOfer KulkaОценок пока нет
- Efficacy of Lifestyle Interventions in Patients With Type 2 Diabetes - A Systematic Review and Meta-AnalysisДокумент11 страницEfficacy of Lifestyle Interventions in Patients With Type 2 Diabetes - A Systematic Review and Meta-AnalysisDara Agusti MaulidyaОценок пока нет
- 1 s2.0 S0026049511003404 MainДокумент8 страниц1 s2.0 S0026049511003404 MainFrankis De Jesus Vanegas RomeroОценок пока нет
- Nutrients 12 00055 v2Документ27 страницNutrients 12 00055 v2Luciano MirianiОценок пока нет
- Lifestyle Behaviors and Physician Advice For Change Among Overweight and Obese Adults With Prediabetes and Diabetes in The United States, 2006Документ10 страницLifestyle Behaviors and Physician Advice For Change Among Overweight and Obese Adults With Prediabetes and Diabetes in The United States, 2006Agil SulistyonoОценок пока нет
- Richardson Synthesis Summative 280613Документ13 страницRichardson Synthesis Summative 280613api-217086261Оценок пока нет
- DessertДокумент12 страницDessertVijayavarman M SОценок пока нет
- The Effect of High-Protein, Low-Carbohydrate Diets in The Treatment of Type 2 Diabetes: A 12 Month Randomised Controlled TrialДокумент10 страницThe Effect of High-Protein, Low-Carbohydrate Diets in The Treatment of Type 2 Diabetes: A 12 Month Randomised Controlled TrialFirda Rizky KhoerunnissaОценок пока нет
- JurnalДокумент10 страницJurnalRima FerdillaIKPBОценок пока нет
- Effect of Diet On Type 2 Diabetes Mellitus: A Review.: Sami, W Ansari, T Butt, N.S Hamid, M.R. 2017Документ5 страницEffect of Diet On Type 2 Diabetes Mellitus: A Review.: Sami, W Ansari, T Butt, N.S Hamid, M.R. 2017Yayang SavitaОценок пока нет
- NIH Public Access: Author ManuscriptДокумент18 страницNIH Public Access: Author ManuscriptKevinJuliusTanadyОценок пока нет
- Nutrients 08 00073Документ9 страницNutrients 08 00073Irma RakhmawatiОценок пока нет
- New-Guthrie2015Документ10 страницNew-Guthrie2015Ser Eldrin GarciaОценок пока нет
- Research Article Perceived Stress and Adherence To The Dietary Recommendations and Blood Glucose Levels in Type 1 DiabetesДокумент8 страницResearch Article Perceived Stress and Adherence To The Dietary Recommendations and Blood Glucose Levels in Type 1 DiabetesAisiri RaoОценок пока нет
- Am J Clin Nutr 2015 Cespedes Ajcn.Документ4 страницыAm J Clin Nutr 2015 Cespedes Ajcn.Jhon Sahatma SinagaОценок пока нет
- A Very Low Carbohydrate, Low Saturated Fat Diet For Type 2 Diabetes Management: A Randomized TrialДокумент10 страницA Very Low Carbohydrate, Low Saturated Fat Diet For Type 2 Diabetes Management: A Randomized TrialvicenteОценок пока нет
- Order 5553454.editedДокумент5 страницOrder 5553454.editedonka melissaОценок пока нет
- Bismillah Fix Hba1c3Документ8 страницBismillah Fix Hba1c3NsafifahОценок пока нет
- Journal Medicine: The New EnglandДокумент11 страницJournal Medicine: The New EnglandYancy Erazo DoradoОценок пока нет
- MainДокумент16 страницMainTito AlhoОценок пока нет
- Diabetes Prevention ProgramДокумент12 страницDiabetes Prevention ProgramIrene JordanОценок пока нет
- Moderators and Mediators of Behaviour Change in A Lifestyle Program For Treated Hypertensives: A Randomized Controlled Trial (ADAPT)Документ9 страницModerators and Mediators of Behaviour Change in A Lifestyle Program For Treated Hypertensives: A Randomized Controlled Trial (ADAPT)Shayan AlPah DoWg KhalidОценок пока нет
- Lifestyle Behaviors and Physician Advice For Change Among Overweight and Obese Adults With Prediabetes and Diabetes in The United States, 2006Документ9 страницLifestyle Behaviors and Physician Advice For Change Among Overweight and Obese Adults With Prediabetes and Diabetes in The United States, 2006Agil SulistyonoОценок пока нет
- Dietary Counselling and Food Fortification in Stable COPD: A Randomised TrialДокумент7 страницDietary Counselling and Food Fortification in Stable COPD: A Randomised TrialJames Cojab SacalОценок пока нет
- Effect of Mediterranean Diet in Diabetes Control and Cardiovascular Risk Modification A Systematic ReviewДокумент8 страницEffect of Mediterranean Diet in Diabetes Control and Cardiovascular Risk Modification A Systematic Reviewgizi.mapsОценок пока нет
- Dia Care 2014 Espeland 2548 56Документ9 страницDia Care 2014 Espeland 2548 56Fikih Diah KusumasariОценок пока нет
- Intermittent Fasting Combined With Calorie Restriction Is Effective For Weight Loss and Cardio-Protection in Obese WomenДокумент9 страницIntermittent Fasting Combined With Calorie Restriction Is Effective For Weight Loss and Cardio-Protection in Obese Womenpriya1832Оценок пока нет
- Research ArticleДокумент93 страницыResearch Articlearyan batangОценок пока нет
- 1 s2.0 S0168822714003982 Main PDFДокумент7 страниц1 s2.0 S0168822714003982 Main PDFKhoirun S. NisaОценок пока нет
- Beachbody Ultimate Reset Clinical StudyДокумент12 страницBeachbody Ultimate Reset Clinical StudyChris ColottiОценок пока нет
- 2Документ51 страница2Madhavan YadhavanОценок пока нет
- Dietary Strategies For Weight Loss MaintenanceДокумент10 страницDietary Strategies For Weight Loss MaintenanceMARKETDIGITAL BNОценок пока нет
- A Randomized Trial of A Low-Carbohydrate Diet For Obesity - NEJMДокумент16 страницA Randomized Trial of A Low-Carbohydrate Diet For Obesity - NEJMMateo PeychauxОценок пока нет
- The Long-Term Effects of Lifestyle Change On Blood Pressure: One-Year Follow-Up of The ENCORE StudyДокумент8 страницThe Long-Term Effects of Lifestyle Change On Blood Pressure: One-Year Follow-Up of The ENCORE StudyMarlia NoveliaОценок пока нет
- Clinical Guideline: Annals of Internal MedicineДокумент8 страницClinical Guideline: Annals of Internal MedicineYulias YoweiОценок пока нет
- Effects of Laparoscopic Gastric Plication (LGP) in Patients With Type 2 Diabetes, One Year Follow-UpДокумент4 страницыEffects of Laparoscopic Gastric Plication (LGP) in Patients With Type 2 Diabetes, One Year Follow-UpAnras FajrulОценок пока нет
- Diabetes DietДокумент8 страницDiabetes DietkitchaaОценок пока нет
- Da QingДокумент18 страницDa QingAlina PopaОценок пока нет
- A Low-Fat Vegan Diet and A Conventional Diabetes Diet in The Treatment of Type 2 Diabetes: A Randomized, Controlled, 74-wk Clinical TrialДокумент9 страницA Low-Fat Vegan Diet and A Conventional Diabetes Diet in The Treatment of Type 2 Diabetes: A Randomized, Controlled, 74-wk Clinical TrialSheldon SilvaОценок пока нет
- Dr. Poon's Metabolic Diet Program Improves Clinical and Laboratory Outcomes in Obese Patients With Metabolic SyndromeДокумент5 страницDr. Poon's Metabolic Diet Program Improves Clinical and Laboratory Outcomes in Obese Patients With Metabolic SyndromeasclepiuspdfsОценок пока нет
- Nutritional Management and Dietary Guidelines For Cancer CachexiaДокумент3 страницыNutritional Management and Dietary Guidelines For Cancer CachexiaShalah Marie UbaldoОценок пока нет
- Weight Management Clinical TrialsДокумент7 страницWeight Management Clinical TrialschuariwapoohОценок пока нет
- Jurnal 2Документ9 страницJurnal 2Akhmadi 98Оценок пока нет
- Mindful Eating For Weight Loss in Women With Obesity A Randomized Controlled TrialДокумент28 страницMindful Eating For Weight Loss in Women With Obesity A Randomized Controlled TrialFilipe BritoОценок пока нет
- Example 6Документ4 страницыExample 6Tutor BlairОценок пока нет
- Lit ReviewДокумент19 страницLit Reviewapi-240895351Оценок пока нет
- HbA1C AS AN INDEX OF GLYCEMIC STATUS IN OBESE TYPE 2 DIABETICSДокумент6 страницHbA1C AS AN INDEX OF GLYCEMIC STATUS IN OBESE TYPE 2 DIABETICSInternational Journal of Clinical and Biomedical Research (IJCBR)Оценок пока нет
- The DASH Diet and Insulin SensitivityДокумент7 страницThe DASH Diet and Insulin SensitivityJosefina OrtegaОценок пока нет
- Macronutrients, Food Groups, and Eating Patterns in The Management of DiabetesДокумент12 страницMacronutrients, Food Groups, and Eating Patterns in The Management of Diabetesannaafia69969Оценок пока нет
- Debunking The Evergreening Patents MythДокумент3 страницыDebunking The Evergreening Patents Mythjns198Оценок пока нет
- Dryer Regenerative Blower Purge DBP 02250195 405 R00 PDFДокумент84 страницыDryer Regenerative Blower Purge DBP 02250195 405 R00 PDFjennyОценок пока нет
- Radproduction Chapter 2-9Документ276 страницRadproduction Chapter 2-9Christian DioОценок пока нет
- Geology Harn v1 2Документ17 страницGeology Harn v1 2vze100% (1)
- Schedule NДокумент3 страницыSchedule Nmittal kelaОценок пока нет
- Grand Hyatt Manila In-Room Dining MenuДокумент14 страницGrand Hyatt Manila In-Room Dining MenuMetroStaycation100% (1)
- Intentions and Results ASFA and Incarcerated ParentsДокумент10 страницIntentions and Results ASFA and Incarcerated Parentsaflee123Оценок пока нет
- Key ScientificДокумент4 страницыKey ScientificGarrettОценок пока нет
- Kingdom of AnimaliaДокумент6 страницKingdom of AnimaliaBen ZerepОценок пока нет
- Liebherr 2956 Manual de UsuarioДокумент27 страницLiebherr 2956 Manual de UsuarioCarona FeisОценок пока нет
- Biology 1st Term PaperДокумент2 страницыBiology 1st Term PapershrirahulambadkarОценок пока нет
- General Session Two - Work Life BalanceДокумент35 страницGeneral Session Two - Work Life BalanceHiba AfandiОценок пока нет
- Drawing Submssion Requirements - September - 2018Документ66 страницDrawing Submssion Requirements - September - 2018Suratman Blanck MandhoОценок пока нет
- E10b MERCHANT NAVY CODE OF CONDUCTДокумент1 страницаE10b MERCHANT NAVY CODE OF CONDUCTssabih75Оценок пока нет
- L04-課文單片填空 (題目) (Day of the Dead)Документ3 страницыL04-課文單片填空 (題目) (Day of the Dead)1020239korrnellОценок пока нет
- B - Cracked Tooth SyndromeДокумент8 страницB - Cracked Tooth SyndromeDavid TaylorОценок пока нет
- 9801 Low-Shrinkage Camera Module Epoxy With LED and Heat-Cure CapabilityДокумент3 страницы9801 Low-Shrinkage Camera Module Epoxy With LED and Heat-Cure CapabilityAchraf BouraОценок пока нет
- Tiếng AnhДокумент250 страницTiếng AnhĐinh TrangОценок пока нет
- (Cô Vũ Mai Phương) Tài liệu LIVESTREAM - Chuyên đề thi THPT - Câu hỏi giao tiếp xã hội (Buổi 1)Документ4 страницы(Cô Vũ Mai Phương) Tài liệu LIVESTREAM - Chuyên đề thi THPT - Câu hỏi giao tiếp xã hội (Buổi 1)nguyen duong trungОценок пока нет
- Chapter 03Документ35 страницChapter 03david jenil nabuaОценок пока нет
- Mdx-40a Use en R1 PDFДокумент100 страницMdx-40a Use en R1 PDFMarcos BustamanteОценок пока нет
- Method Statement For Installation of Chilled Water Pump & Condenser Water PumpДокумент14 страницMethod Statement For Installation of Chilled Water Pump & Condenser Water Pump721917114 47Оценок пока нет
- Biology - Cell City AnswersДокумент5 страницBiology - Cell City AnswersDaisy be100% (1)
- Chapter FourДокумент9 страницChapter FourSayp dОценок пока нет
- Schindler 3100: Cost-Effective MRL Traction Elevator For Two-And Three-Story BuildingsДокумент20 страницSchindler 3100: Cost-Effective MRL Traction Elevator For Two-And Three-Story BuildingsHakim BgОценок пока нет
- Variance AnalysisДокумент22 страницыVariance AnalysisFrederick GbliОценок пока нет
- Aplikasi Metode Geomagnet Dalam Eksplorasi Panas BumiДокумент10 страницAplikasi Metode Geomagnet Dalam Eksplorasi Panas Bumijalu sri nugrahaОценок пока нет
- Tri-Partite Agreement AssociationДокумент9 страницTri-Partite Agreement AssociationThiyagarjanОценок пока нет
- Cyber Safety PP Presentation For Class 11Документ16 страницCyber Safety PP Presentation For Class 11WAZ CHANNEL100% (1)
- Legg Calve Perthes Disease: SynonymsДокумент35 страницLegg Calve Perthes Disease: SynonymsAsad ChaudharyОценок пока нет
- Instant Loss On a Budget: Super-Affordable Recipes for the Health-Conscious CookОт EverandInstant Loss On a Budget: Super-Affordable Recipes for the Health-Conscious CookРейтинг: 3.5 из 5 звезд3.5/5 (2)
- Glucose Revolution: The Life-Changing Power of Balancing Your Blood SugarОт EverandGlucose Revolution: The Life-Changing Power of Balancing Your Blood SugarРейтинг: 5 из 5 звезд5/5 (351)
- The Beck Diet Solution Weight Loss Workbook: The 6-Week Plan to Train Your Brain to Think Like a Thin PersonОт EverandThe Beck Diet Solution Weight Loss Workbook: The 6-Week Plan to Train Your Brain to Think Like a Thin PersonРейтинг: 3.5 из 5 звезд3.5/5 (33)
- The End of Craving: Recovering the Lost Wisdom of Eating WellОт EverandThe End of Craving: Recovering the Lost Wisdom of Eating WellРейтинг: 4.5 из 5 звезд4.5/5 (82)
- The Diabetes Code: Prevent and Reverse Type 2 Diabetes NaturallyОт EverandThe Diabetes Code: Prevent and Reverse Type 2 Diabetes NaturallyРейтинг: 4.5 из 5 звезд4.5/5 (3)
- The Arm: Inside the Billion-Dollar Mystery of the Most Valuable Commodity in SportsОт EverandThe Arm: Inside the Billion-Dollar Mystery of the Most Valuable Commodity in SportsРейтинг: 4 из 5 звезд4/5 (49)
- Find Your Path: Honor Your Body, Fuel Your Soul, and Get Strong with the Fit52 LifeОт EverandFind Your Path: Honor Your Body, Fuel Your Soul, and Get Strong with the Fit52 LifeРейтинг: 4 из 5 звезд4/5 (3)
- Sugar Crush: How to Reduce Inflammation, Reverse Nerve Damage, and Reclaim Good HealthОт EverandSugar Crush: How to Reduce Inflammation, Reverse Nerve Damage, and Reclaim Good HealthРейтинг: 4 из 5 звезд4/5 (6)
- Metabolism Revolution: Lose 14 Pounds in 14 Days and Keep It Off for LifeОт EverandMetabolism Revolution: Lose 14 Pounds in 14 Days and Keep It Off for LifeОценок пока нет
- Body Love Every Day: Choose Your Life-Changing 21-Day Path to Food FreedomОт EverandBody Love Every Day: Choose Your Life-Changing 21-Day Path to Food FreedomРейтинг: 4 из 5 звезд4/5 (1)
- The Diet Trap Solution: Train Your Brain to Lose Weight and Keep It Off for GoodОт EverandThe Diet Trap Solution: Train Your Brain to Lose Weight and Keep It Off for GoodОценок пока нет
- Glucose Goddess Method: A 4-Week Guide to Cutting Cravings, Getting Your Energy Back, and Feeling AmazingОт EverandGlucose Goddess Method: A 4-Week Guide to Cutting Cravings, Getting Your Energy Back, and Feeling AmazingРейтинг: 5 из 5 звезд5/5 (61)
- Eat to Lose, Eat to Win: Your Grab-n-Go Action Plan for a Slimmer, Healthier YouОт EverandEat to Lose, Eat to Win: Your Grab-n-Go Action Plan for a Slimmer, Healthier YouОценок пока нет
- Grit & Grace: Train the Mind, Train the Body, Own Your LifeОт EverandGrit & Grace: Train the Mind, Train the Body, Own Your LifeРейтинг: 4 из 5 звезд4/5 (3)
- Ultrametabolism: The Simple Plan for Automatic Weight LossОт EverandUltrametabolism: The Simple Plan for Automatic Weight LossРейтинг: 4.5 из 5 звезд4.5/5 (28)
- The Body Book: The Law of Hunger, the Science of Strength, and Other Ways to Love Your Amazing BodyОт EverandThe Body Book: The Law of Hunger, the Science of Strength, and Other Ways to Love Your Amazing BodyОценок пока нет
- Hungry for Change: Ditch the Diets, Conquer the Cravings, and Eat Your Way to Lifelong HealthОт EverandHungry for Change: Ditch the Diets, Conquer the Cravings, and Eat Your Way to Lifelong HealthРейтинг: 4 из 5 звезд4/5 (7)
- The Food Lover's Cleanse: 140 Delicious, Nourishing Recipes That Will Tempt You Back into Healthful EatingОт EverandThe Food Lover's Cleanse: 140 Delicious, Nourishing Recipes That Will Tempt You Back into Healthful EatingРейтинг: 4 из 5 звезд4/5 (3)
- Foods That Cause You to Lose Weight: The Negative Calorie EffectОт EverandFoods That Cause You to Lose Weight: The Negative Calorie EffectРейтинг: 3 из 5 звезд3/5 (5)
- How to Be Well: The 6 Keys to a Happy and Healthy LifeОт EverandHow to Be Well: The 6 Keys to a Happy and Healthy LifeРейтинг: 5 из 5 звезд5/5 (1)
- Keto Friendly Recipes: Easy Keto For Busy PeopleОт EverandKeto Friendly Recipes: Easy Keto For Busy PeopleРейтинг: 3.5 из 5 звезд3.5/5 (2)
- Summary: Fast Like a Girl: A Woman’s Guide to Using the Healing Power of Fasting to Burn Fat, Boost Energy, and Balance Hormones: Key Takeaways, Summary and AnalysisОт EverandSummary: Fast Like a Girl: A Woman’s Guide to Using the Healing Power of Fasting to Burn Fat, Boost Energy, and Balance Hormones: Key Takeaways, Summary and AnalysisРейтинг: 3 из 5 звезд3/5 (2)
- Secrets From the Eating Lab: The Science of Weight Loss, the Myth of Willpower, and Why You Should Never Diet AgainОт EverandSecrets From the Eating Lab: The Science of Weight Loss, the Myth of Willpower, and Why You Should Never Diet AgainРейтинг: 3.5 из 5 звезд3.5/5 (38)
- The Candida Cure: The 90-Day Program to Balance Your Gut, Beat Candida, and Restore Vibrant HealthОт EverandThe Candida Cure: The 90-Day Program to Balance Your Gut, Beat Candida, and Restore Vibrant HealthОценок пока нет
- Summary of Mary Claire Haver's The Galveston DietОт EverandSummary of Mary Claire Haver's The Galveston DietРейтинг: 5 из 5 звезд5/5 (2)