Академический Документы
Профессиональный Документы
Культура Документы
Mulluscum Contagiosum Cantharone Article
Загружено:
RakaArdiansyah0 оценок0% нашли этот документ полезным (0 голосов)
66 просмотров6 страницasep
Авторское право
© © All Rights Reserved
Доступные форматы
PDF, TXT или читайте онлайн в Scribd
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документasep
Авторское право:
© All Rights Reserved
Доступные форматы
Скачайте в формате PDF, TXT или читайте онлайн в Scribd
0 оценок0% нашли этот документ полезным (0 голосов)
66 просмотров6 страницMulluscum Contagiosum Cantharone Article
Загружено:
RakaArdiansyahasep
Авторское право:
© All Rights Reserved
Доступные форматы
Скачайте в формате PDF, TXT или читайте онлайн в Scribd
Вы находитесь на странице: 1из 6
124 | www.PediatricSuperSite.
com PEDIATRIC ANNALS 39:3 | MARCH 2010
case challenges: dermatology
case challenges case challenges
Treatment of Molluscum Contagiosum
with Cantharidin: A Practical Approach
Erin F.D. Mathes, MD; and Ilona J. Frieden, MD
M
olluscum contagiosum is very com-
mon. In this article we discuss the
use of cantharidin as a treatment
option for molluscum contagiosum and give
detailed information about distribution sources,
how to apply it, and caveats regarding its use.
Molluscum contagiosum is a common vi-
ral disease of childhood caused by a poxvirus,
which presents with small, rm, dome-shaped,
umbilicated papules. It is generally benign and
self-limited, with spontaneous resolution within
6 months to several years. Watchful waiting can
often be an appropriate management strategy;
however, some patients either desire or require
treatment. Reasons for actively treating mol-
luscum contagiosum may include alleviation of
discomfort and itching (particularly in patients
where an eczematous eruption the so-called
molluscum eczema is seen in association)
or in patients with ongoing atopic dermatitis
where more lesions are likely to be present.
Other reasons for treatment include limitation
of spread to other areas and people, prevention
of scarring and superinfection, and elimination
of the social stigma of visible lesions. No one
treatment is uniformly effective.
Treatment options include destructive
therapies (curettage, cryotherapy, canthari-
din, and keratolytics, among others), immu-
nomodulators (imiquimod, cimetidine, and
Candida antigen), and antivirals (cidofovir).
In this article we discuss and describe our rst-
line treatment approach for those molluscum
needing treatment cantharidin.
Erin F. Mathes, MD, is Pediatric Dermatology
Fellow, Department of Dermatology University of
California, San Francisco. Ilona J. Frieden, MD, is
Professor of Dermatology and Pediatrics, Depart-
ments of Dermatology and Pediatrics University of
California, San Francisco.
Address correspondence to: Erin F. Mathes, MD,
1701 Divisadero St., Box 0316, San Francisco, CA
94143-0316; fax 415-353-7850; e-mail mathese@
derm.ucsf.edu.
Dr. Mathes and Dr. Frieden have disclosed no rel-
evant nancial relationships.
doi: 10.3928/00904481-20100223-03
For treatment, see page 125.
Editors note: Each month, this department features a discussion of an unusual diagnosis in genetics, radiology,
or dermatology. A description and images are presented, with the diagnosis and an explanation of how the diagnosis
was determined following. As always, your comments are welcome. E-mail pedann@slackinc.com.
ABSTRACT
3903CaseChallenges.indd 124 3/3/2010 3:20:07 PM
PEDIATRIC ANNALS 39:3 | MARCH 2010 www.PediatricSuperSite.com | 125
A recent review of evidence sup-
porting various treatment options
concluded that cantharidin may be the
treatment of choice in young children
because it is painless and effective.
1
Cantharidin, a phosphodiesterase
inhibitor that causes vesiculation of
the skin, was originally derived from
the blister beetle, but now is synthe-
sized commercially.
2
Careful appli-
cation to the skin typically results in
a small vesicle. Because molluscum
are very supercial skin lesions, ap-
plication causes skin vesiculation,
with extrusion of the molluscum
body, leading to the resolution of the
lesion.
2
Although the evidence for
the efcacy of cantharidin is mainly
limited to retrospective case series,
many physicians use cantharidin as
a treatment, and its use has a high
rate of parental (60% to 90%) and
physician (92%) satisfaction.
1,3-8
In 1997, President Clinton ap-
proved an amendment to the Food,
Drug and Cosmetic Act of 1962 that
provides that certain drug products
may be compounded by a physician
or pharmacist for individual patients.
The Food and Drug Administration
(FDA) has included cantharidin in
the proposed list of bulk substances
that physicians and pharmacists are
permitted to compound for use in in-
dividual patients.
5
APPLICATION
Treating molluscum with canthari-
din is not technically difcult. Although
there is a small risk for adverse effects,
such as excessive blistering and scar-
ring, we (and others) believe the safety
prole is sufciently favorable to con-
tinue using it for this purpose.
1,3-5,7,8
A major advantage over certain treat-
ments, such as cryotherapy and curet-
tage, is that application of cantharidin
is painless. Although pain (typically
very minor) may occur several hours
to a day later, children rarely associate
this with their recent doctor visit, and
SIDEBAR 1.
Application Instructions
(also see Figure 1 and Figure 2)
Treat only a few lesions (no more than four to ve) at the rst visit. In subsequent
visits, treat no more than 12 to 15 lesions.
Try to get the childs cooperation, explaining that the medication will not hurt. If the
child is fearful and moving, assistance will be needed to apply without accidentally
getting the medication on normal, unaffected skin.
Use the wooden end of a cotton applicator to apply a small drop of cantharidin
directly to each lesion, taking care not to apply to the surrounding skin. If medication
accidentally is applied to normal skin (as may happen in a moving infant), immedi-
ately wash off the medication.
Allow the cantharidin to dry for at least 5 to 10 minutes to minimize the risk of spread
to adjacent unaffected skin.
Attempting to wash off the medication is controversial. Some authors recommend
doing so after 2 to 6 hours, but the polymer created by the collodion makes this dif-
cult. Another option is leaving the medication on overnight, only attempting to wash
it off if visible blisters are noted a few hours later, although it is doubtful that this will
actually halt the blistering effects.
SIDEBAR 2.
Helpful Hints
Gently shake the bottle, then stir with the applicator before applying to ensure an even
concentration of cantharidin.
Do not treat intertriginous areas, or the face, initially. After determining typical response to
medication, treatment in these areas can be considered:
For facial lesions, warn parents about the possibility of pigmentary alteration.
Do not treat lesions that are directly adjacent to the eye.
For intertriginous areas, warn parents about the greater risk of excessive blistering, especial-
ly in hot weather. If the weather is very hot, limit the number of lesions treated to just a few.
Do not treat inamed molluscum, at least initially, as they may resolve spontaneously.
If there was little or no response after the rst treatment, at the next visit, advise the patient
to leave the cantharidin on for longer, or not to wash it off at all.
Over-the-counter oral analgesics, such as ibuprofen or acetaminophen, may help
with discomfort.
Topical petrolatum may help soothe irritated skin. Before applying petrolatum, make sure
that the cantharidin has been thoroughly washed off. Liberal petrolatum application to
areas with active cantharidin can cause spread of cantharidin and widespread blisters.
10
If surrounding dermatitis is present, treat it with 1% hydrocortisone ointment
(over-the-counter).
case challenges
Cantharidin
T R E A T M E N T
3903CaseChallenges.indd 125 3/3/2010 3:20:08 PM
126 | www.PediatricSuperSite.com PEDIATRIC ANNALS 39:3 | MARCH 2010
are usually willing to have the medica-
tion applied on subsequent visits.
We disagree with a recent review
by Silverberg that suggested that can-
tharidin should not be applied by pedi-
atricians in their ofces.
9
Pediatricians
and family physicians perform many
procedures that are more complicated
than cantharidin application, such as
splinting, venipuncture, lumbar punc-
ture, intramuscular injection, lacera-
tion repair, and incision and drainage.
In this article, we give detailed instruc-
tions regarding the use of cantharidin,
including sources for purchasing,
techniques for application, potential
pitfalls and adverse effects, and billing
codes for in-ofce treatment with this
medication. We believe that with the
following information and guidance,
cantharidin can become a very useful
tool for treating molluscum in the pri-
mary physicians ofce.
Cantharidin is commercially avail-
able in a 0.7% concentration, in a
collodion base (see Table, page 127,
for sources). This 0.7% formulation
is strongly preferred for molluscum
treatment over a more potent formu-
lation, which combines a higher con-
centration of cantharidin (1%) mixed
with podophyllin and salycilic acid,
and has a much greater risk for caus-
ing excessive blistering, scarring, and
even chemical cellulitis.
Cantharidin can only be applied
in a physicians ofce and should
never be dispensed to patients for
self-application (see Sidebar 1, page
125, and Figure 1, and Figure 2,
page 127, for application instruc-
tions). Most patients improve after
one or two visits.
3,4,8
Complications
include excessive blistering, pain,
pruritis, and burning (see Figure 3,
page 128, and Figure 4, page 128).
Although some authors estimate that
these adverse effects occur in ap-
proximately 6% to 46% of patients,
in our experience, the rate is at the
low end of this range.
3,4,8
Temporary
erythema can occur in up to 37% of
patients.
4,5
Care should be taken to
avoid spreading the cantharidin to
unaffected areas or to the eyes. There
may be temporary pigment alteration
that should resolve without scarring.
Several helpful hints to use the
medication effectively and minimize
size effects are summarized in Sidebar
2 (see page 125). The rst time can-
tharidin is used, it is prudent to treat
only three or four lesions to assess the
individual patients response. Warn
parents that although the medication is
applied sparingly, there is a 1% to 5%
chance of a larger blister developing.
There is controversy regarding wheth-
er the medication should be washed
off a few hours after application. Some
authors recommend this practice, but
because cantharidin is dissolved in
collodion, it forms a lm upon drying,
which is probably not easily removed
with soap and water.
7
Follow-up visits
to assess efcacy and perform further
SIDEBAR 3.
Anticipatory Guidance
11
Several hours after application, mild discomfort at the site of application occasionally
occurs. This can be treated by using cool compresses and by administering over-the-
counter analgesics, although, in our experience, this is rarely necessary.
One day after application, a small blister often forms, although, in some cases, only
redness or mild crusting is noted. If the blister is tense and uncomfortable, draining
with a sterilized needle may help diminish pain, although this is also rarely necessary.
Two to 4 days after application, the blister will crust or drain, leaving a supercial ero-
sion. Apply an antibiotic ointment or sterile petrolatum to the eroded area to encour-
age re-epithelialization.
Within 1 week, the area is typically healed, although postinammatory erythema may
persist for a week or two. In darker skin types, postinammatory hyper- or hypopig-
mentation may persist, at times for several months.
Scarring is rare. Occasionally, even untreated molluscum leave tiny pitted scars.
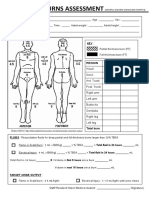
Figure 1. Cantharadin bottle with applicators.
case challenges
Cantharidin can only be
applied in a physicians
ofce and should never be
dispense to patients for
self-application.
3903CaseChallenges.indd 126 3/3/2010 3:20:08 PM
PEDIATRIC ANNALS 39:3 | MARCH 2010 www.PediatricSuperSite.com | 127
treatments are typically scheduled ev-
ery 2 to 4 weeks. If patients have not
had any adverse reactions, more le-
sions can be treated than at the initial
visit. Individual lesions of molluscum
typically resolve after one treatment
but occasionally require retreatment,
particularly if they are large. In many
cases, after two to three treatments, the
molluscum will diminish in number
and gradually resolve. Sidebar 3 (see
page 126) outlines recommendations
for anticipatory guidance.
OTHER CONSIDERATIONS
Another problem that often
arises is the presence of so-called
molluscum eczema, a dermatitis
virtually identical to atopic derma-
titis, which preferentially occurs in
areas of skin where molluscum are
present. Although the individual
molluscum can be treated with can-
tharidin, even in sites of dermati-
tis, the dermatitis itself should be
treated with a low to mid-potency
topical steroid to alleviate it and
prevent autoinnoculation with fur-
ther spread of the virus.
TABLE.
Distribution Sources: How to Purchase for Medical Ofces*
Company
Product
Name
Formulation Address/phone E-mail/Website
Dormer
Laboratories
Cantharone
0.7% canthari-
din in a col-
lodion base
91 Keleld, Suite 5, Rexdale, On-
tario, Canada M9W 5A3; (416)
242 6167; fax: 877 436 7637
www.dormer.ca
Pharmscience/
Omniderm
Canthacur
0.7% cantharidin
in a collodion
base
997 Seguin, Hudson, Quebec,
Canada J0P 1H0; 450-458-0158;
fax: 450-458-7499
CustomerServicePaladin@pharmascience.com
Delasco Cantharidin
Cantharidin
crystals and
collodion base
sold separately
for in-ofce
compounding
608 13th Ave., Council Bluffs,
IA 51501-6401; (800) 831-6273;
fax: (800) 320-9612
questions@delasco.com
College
Pharmacy
Cantharidin
Compounded to
order
3505 Austin Bluffs Parkway,
Suite 101, Colorado Springs, CO
80918
info@collegepharmacy.com**
*Cantharidins use is limited to in-ofce treatment by a physician. Please contact the suppliers for ordering requirements.
**Shipping to selected states only
Figure 2. Application of cantharadin to molluscum.
case challenges
3903CaseChallenges.indd 127 3/3/2010 3:20:09 PM
128 | www.PediatricSuperSite.com PEDIATRIC ANNALS 39:3 | MARCH 2010
Although there are few, random-
ized, prospective trials on treatments
for molluscum, a recent large retro-
spective study on cantharidin by Sil-
verberg et al found that 90% of 300
patients cleared and an additional
8% improved in an average of 2.1
treatments. Parental satisfaction was
95%.
4,6
In their retrospective study
of 110 patients, Cathcart et al found
a 96% efcacy after approximately
two treatments and a parental satis-
faction rate of 78%.
8
In contrast, in
their prospective randomized trial
of four treatment modalities, Hanna
et al found that 36.7% of patients in
the cantharidin group were cured af-
ter one visit, an additional 43% after
two visits, and the remaining 20%
after three or more visits. The paren-
tal satisfaction rate for cantharidin
was 60%. The parental satisfaction
for curettage (the preferred treat-
ment modality in Hannas study)
was almost 90%.
3
The practice envi-
ronment in Hannas study is signi-
cantly different than most U.S. prac-
tices because phamacologic sedation
is available as needed for curettage.
In our experience, curettage is an ef-
fective and acceptable treatment for
older children, especially when it is
difcult for the family to return for
several more visits.
The Current Procedural Termi-
nology (CPT) codes for billing for
destruction of molluscum are well-
established: CPT: 17110 (destruction
of up to 14 lesions) and 17111 (de-
struction of 15 or more lesions).
CONCLUSIONS
With appropriate precautions and
information provided, we believe
that the use of this medication by
pediatricians and other primary care
Figure 3. Chemical irritation from cantharidin application; this response is very unusual.
Figure 4. Blisters following cantharidin application; the amount of blistering is more than
typically occurs.
case challenges
Figure 5. Verruca vulgaris ring wart from cantharadin application.
3903CaseChallenges.indd 128 3/3/2010 3:20:11 PM
case challenges
providers is safe and well within
the technical expertise of any well-
trained practitioner.
Finally, although cantharidin is an
excellent treatment option for mollus-
cum, we do not recommend its use for
common warts. For unknown reasons,
the noninammatory blisters caused
by the medication can result in so-
called ring warts (see Figure 5, page
128), leading to wart spread, rather
than improvement.
REFERENCES
1. Brown J, Janniger CK, Schwartz CZ, Sil-
verberg NB. Childhood molluscum conta-
giosum. Int J Dermatol. 2006;45(2):93-99.
2. Wolverton SE. Comprehensive Derma-
tologic Drug Therapy. Philadelphia, PA:
Saunders; 2001;532.
3. Hanna D, Hatami A, Powell J, et al. A
prospective randomized trial comparing
the efcacy and adverse effects of four
recognized treatments of molluscum con-
tagiosum in children. Pediatr Dermatol.
2006;23(6):574-579.
4. Silverberg NB, Sidbury R, Mancini AJ.
Childhood molluscum contagiosum:
experience with cantharidin therapy
in 300 patients. J Am Acad Dermatol.
2000;43(3):503-507.
5. Moed L, Shwayder TA, Chang MW.
Cantharidin revisited: a blistering defense
of an ancient medicine. Arch Dermatol.
2001;137(10):1357-1360.
6. Van der Wouden JC, et al. Interventions
for cutaneous molluscum contagiosum.
Cochrane Database of Systematic Re-
views 2006, Issue 2. Art. No.: CD004767.
DOI:10.1002/14651858.CD004767.pub2.
7. Coloe J, Morrell DS. Cantharadin use
among pediatric dermatologists in the treat-
ment of molluscum contagiosum. Pediatr
Dermatol. 2009;26(4):405-408.
8. Cathcart S, Coloe J, Morrell DS. Parental
satisfaction, efcacy, and adverse events
in 54 patients treated with cantharidin for
molluscum contagiosum infection. Clin
Pediatr (Phila). 2008;48(2):161-165.
9. Silverberg NB. A practical approach to
molluscum contagiosum. Part 2. Contem-
porary Pediatrics. 2007;24(9):63-72.
10. Shah A, Treat J, Yan AC. Spread of can-
tharidin after petrolatum use resulting
in a varicelliform vesicular dermatitis.
J Am Acad Dermatol. 2008;59(2 Suppl
1):S54-S55.
11. Cantharone brochure. www.dormer.ca.
Dormer Laboratories, Canada.
3903CaseChallenges.indd 130 3/3/2010 3:20:14 PM
Вам также может понравиться
- Moluskum in HivДокумент3 страницыMoluskum in HivRakaArdiansyahОценок пока нет
- Insidensi AmerikaindianДокумент6 страницInsidensi AmerikaindianRakaArdiansyahОценок пока нет
- Book 1Документ6 страницBook 1RakaArdiansyahОценок пока нет
- Ekspression MolluscumДокумент8 страницEkspression MolluscumRakaArdiansyahОценок пока нет
- Pone 0005255Документ8 страницPone 0005255RakaArdiansyahОценок пока нет
- Terapi British SeksДокумент5 страницTerapi British SeksRakaArdiansyahОценок пока нет
- Us HealtcareДокумент10 страницUs HealtcareRakaArdiansyahОценок пока нет
- Pembagian JurnalДокумент11 страницPembagian JurnalRakaArdiansyahОценок пока нет
- Sampah 03Документ1 страницаSampah 03RakaArdiansyahОценок пока нет
- Sampah 03Документ1 страницаSampah 03RakaArdiansyahОценок пока нет
- Sampah 03Документ1 страницаSampah 03RakaArdiansyahОценок пока нет
- Sampah 02Документ1 страницаSampah 02RakaArdiansyahОценок пока нет
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceОт EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceРейтинг: 4 из 5 звезд4/5 (895)
- Never Split the Difference: Negotiating As If Your Life Depended On ItОт EverandNever Split the Difference: Negotiating As If Your Life Depended On ItРейтинг: 4.5 из 5 звезд4.5/5 (838)
- The Yellow House: A Memoir (2019 National Book Award Winner)От EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Рейтинг: 4 из 5 звезд4/5 (98)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeОт EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeРейтинг: 4 из 5 звезд4/5 (5794)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaОт EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaРейтинг: 4.5 из 5 звезд4.5/5 (266)
- The Little Book of Hygge: Danish Secrets to Happy LivingОт EverandThe Little Book of Hygge: Danish Secrets to Happy LivingРейтинг: 3.5 из 5 звезд3.5/5 (400)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureОт EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureРейтинг: 4.5 из 5 звезд4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryОт EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryРейтинг: 3.5 из 5 звезд3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerОт EverandThe Emperor of All Maladies: A Biography of CancerРейтинг: 4.5 из 5 звезд4.5/5 (271)
- The Unwinding: An Inner History of the New AmericaОт EverandThe Unwinding: An Inner History of the New AmericaРейтинг: 4 из 5 звезд4/5 (45)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersОт EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersРейтинг: 4.5 из 5 звезд4.5/5 (345)
- Team of Rivals: The Political Genius of Abraham LincolnОт EverandTeam of Rivals: The Political Genius of Abraham LincolnРейтинг: 4.5 из 5 звезд4.5/5 (234)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreОт EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreРейтинг: 4 из 5 звезд4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyОт EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyРейтинг: 3.5 из 5 звезд3.5/5 (2259)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)От EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Рейтинг: 4.5 из 5 звезд4.5/5 (121)
- Influenza Vaccine (Influvac) Consent Form: Title: Name: Age: GenderДокумент1 страницаInfluenza Vaccine (Influvac) Consent Form: Title: Name: Age: GenderIan BondocОценок пока нет
- FSRH Clinical Guideline Intrauterine Contraception Mar23 Amended 11jul2023Документ163 страницыFSRH Clinical Guideline Intrauterine Contraception Mar23 Amended 11jul2023JULIANA DA SILVA NOGUEIRA CARVALHOОценок пока нет
- The Importance of Good PostureДокумент1 страницаThe Importance of Good Postureerica thapaОценок пока нет
- 3.4-Behar Anorexia y MadurezДокумент10 страниц3.4-Behar Anorexia y MadurezAlejandra CarmonaОценок пока нет
- 429 FT0 Physiotherapy in Obstetrics Gynaecology Mohd. JavedДокумент86 страниц429 FT0 Physiotherapy in Obstetrics Gynaecology Mohd. JavedRekha Satheesan100% (1)
- Pengaruh Massage Kaki Terhadap Penurunan Insomnia Pada Lansia Di Banjar Temesi Desa Temesi Kabupaten GianyarДокумент12 страницPengaruh Massage Kaki Terhadap Penurunan Insomnia Pada Lansia Di Banjar Temesi Desa Temesi Kabupaten Gianyar119 CIKOKOLОценок пока нет
- Silabus Rmo 2021Документ13 страницSilabus Rmo 2021Nuzlan NuariОценок пока нет
- Baichongwo (M-Le-34) : Hundred Insect BurrowДокумент1 страницаBaichongwo (M-Le-34) : Hundred Insect Burrowray72roОценок пока нет
- Clinical Psych BookletДокумент36 страницClinical Psych BookletNancy MohamedОценок пока нет
- Thunderbird Medication and Vaccination ProgramДокумент1 страницаThunderbird Medication and Vaccination ProgramIntsik R. DominadoОценок пока нет
- Nursing BulletsДокумент65 страницNursing BulletsMark Anthony Esmundo RN100% (1)
- Nursing Care To Promote Fetal and Maternal HealthДокумент4 страницыNursing Care To Promote Fetal and Maternal HealthKristine BartsОценок пока нет
- Scullard Shock and Infection PDFДокумент53 страницыScullard Shock and Infection PDFDave WilliamzОценок пока нет
- (PEDIA) 2.04 Pediatric Neurologic Exam - Dr. Rivera PDFДокумент15 страниц(PEDIA) 2.04 Pediatric Neurologic Exam - Dr. Rivera PDFJudith Dianne IgnacioОценок пока нет
- The Pearson Guide To GPAT and o Umang H Shah SRJ Ilovepdf CompressedДокумент5 страницThe Pearson Guide To GPAT and o Umang H Shah SRJ Ilovepdf CompressedDrSidharth MehanОценок пока нет
- Type 2 Diabetes MellitusДокумент4 страницыType 2 Diabetes MellitusMazhar WarisОценок пока нет
- Artikel 8 PDFДокумент8 страницArtikel 8 PDFapryani lumban gaolОценок пока нет
- Great Atlas of Dermatology IndexedДокумент73 страницыGreat Atlas of Dermatology Indexedjohn pauloОценок пока нет
- Chloe Ting - 2021 Summer Shred Challenge - Free Workout ProgramДокумент1 страницаChloe Ting - 2021 Summer Shred Challenge - Free Workout ProgramAnniie GuerreroОценок пока нет
- Encopresis in Children An Overview of Recent FindiДокумент5 страницEncopresis in Children An Overview of Recent FindiMaulana MalikОценок пока нет
- Patient Safety and The Informed ConsentДокумент13 страницPatient Safety and The Informed ConsentPatricia Elena ManaliliОценок пока нет
- Episiotomía Desgarro PerinealДокумент9 страницEpisiotomía Desgarro PerinealjigagomezОценок пока нет
- Adhesive Capsulitis of The ShoulderДокумент7 страницAdhesive Capsulitis of The ShoulderKemal TaufikОценок пока нет
- Perforasi Pada Penderita Apendisitis Di RSUD DR.H.Abdul Moeloek LampungДокумент7 страницPerforasi Pada Penderita Apendisitis Di RSUD DR.H.Abdul Moeloek LampungKikiОценок пока нет
- Redcord Medical Active Sport - v3 - 2013Документ12 страницRedcord Medical Active Sport - v3 - 2013Sang Ah YooОценок пока нет
- Cardiac Surgery MCQДокумент43 страницыCardiac Surgery MCQprofarmah100% (7)
- Homeopathic Detox Therapy (HDT) - Interview Ton Jansen - August 2014Документ21 страницаHomeopathic Detox Therapy (HDT) - Interview Ton Jansen - August 2014Yuldash100% (2)
- Drug StudyДокумент7 страницDrug Studyanne009Оценок пока нет
- Burn Assessment CMU PDFДокумент2 страницыBurn Assessment CMU PDFmegamindОценок пока нет
- Health Education For MothersДокумент17 страницHealth Education For MothersNina MoradaОценок пока нет