Академический Документы
Профессиональный Документы
Культура Документы
NP1 Notes
Загружено:
BrianMarBeltranОригинальное название
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
NP1 Notes
Загружено:
BrianMarBeltranАвторское право:
Доступные форматы
Blood transfusion therapy involves transfusing whole blood or blood components (specific portion
or fraction of blood lacking in patient). One unit of whole blood consists of 450 mL of blood collected into
60 to 70 mL of preservative or anticoagulant. Whole blood stored for more than 6 hours does not provide
therapeutic platelet transfusion, nor does it contain therapeutic amounts of labile coagulation factors
(factors V and VIII).
Blood components include:
1. Packed RBCs (100% of erythrocyte, 100% of leukocytes, and 20% of plasma originally present in
one unit of whole blood), indicated to increase the oxygen-carrying capacity of blood with minimal
expansion of blood.
2. Leukocyte-poor packed RBCs, indicated for patients who have experience previous febrile no
hemolytic reactions.
3. Platelets, either HLA (human leukocyte antigen) matched or unmatched.
4. Granulocytes ( basophils, eosinophils, and neutrophils )
5. Fresh frozen plasma, containing all coagulation factors, including factors V and VIII (the labile
factors).
6. Single donor plasma, containing all stable coagulation factors but reduced levels of factors V and
VIII; the preferred product for reversal of Coumadin-induced anticoagulation.
7. Albumin, a plasma protein.
8. Cryoprecipitate, a plasma derivative rich in factor VIII, fibrinogen, factor XIII, and fibronectin.
9. Factor IX concentrate, a concentrated form of factor IX prepared by pooling, fractionating, and
freeze-drying large volumes of plasma.
10. Factor VIII concentrate, a concentrated form of factor IX prepared by pooling, fractionating, and
freeze-drying large volumes of plasma.
11. Prothrombin complex, containing prothrombin and factors VII, IX, X, and some factor XI.
Advantages of blood component therapy
1. Avoids the risk of sensitizing the patients to other blood components.
2. Provides optimal therapeutic benefit while reducing risk of volume overload.
3. Increases availability of needed blood products to larger population.
Principles of blood transfusion therapy
1. Whole blood transfusion
o Generally indicated only for patients who need both increased oxygen-carrying capacity and
restoration of blood volume when there is no time to prepare or obtain the specific blood
components needed.
2. Packed RBCs
o Should be transfused over 2 to 3 hours; if patient cannot tolerate volume over a maximum
of 4 hours, it may be necessary for the blood bank to divide a unit into smaller volumes,
providing proper refrigeration of remaining blood until needed. One unit of packed red cells
should raise hemoglobin approximately 1%, hemactocrit 3%.
3. Platelets
o Administer as rapidly as tolerated (usually 4 units every 30 to 60 minutes). Each unit of
platelets should raise the recipients platelet count by 6000 to 10,000/mm3: however, poor
incremental increases occur with alloimmunization from previous transfusions, bleeding,
fever, infection, autoimmune destruction, and hypertension.
4. Granulocytes
o May be beneficial in selected population of infected, severely granulocytopenic patients (less
than 500/mm3) not responding to antibiotic therapy and who are expected to experienced
prolonged suppressed granulocyte production.
5. Plasma
o Because plasma carries a risk of hepatitis equal to that of whole blood, if only volume
expansion is required, other colloids (e.g., albumin) or electrolyte solutions (e.g., Ringers
lactate) are preferred. Fresh frozen plasma should be administered as rapidly as tolerated
because coagulation factors become unstable after thawing.
6. Albumin
o Indicated to expand to blood volume of patients in hypovolemic shock and to elevate level
of circulating albumin in patients with hypoalbuminemia. The large protein molecule is a
major contributor to plasma oncotic pressure.
7. Cryoprecipitate
o Indicated for treatment of hemophilia A, Von Willebrands disease, disseminated
intravascular coagulation (DIC), and uremic bleeding.
8. Factor IX concentrate
o Indicated for treatment of hemophilia B; carries a high risk of hepatitis because it requires
pooling from many donors.
9. Factor VIII concentrate
o Indicated for treatment of hemophilia A; heat-treated product decreases the risk of hepatitis
and HIV transmission.
10. Prothrombin complex-Indicated in congenital or acquired deficiencies of these factors.
Objectives
1. To increase circulating blood volume after surgery, trauma, or hemorrhage
2. To increase the number of RBCs and to maintain hemoglobin levels in clients with severe anemia
3. To provide selected cellular components as replacements therapy (e.g. clotting factors, platelets,
albumin)
Nursing Interventions
1. Verify doctors order. Inform the client and explain the purpose of the procedure.
2. Check for cross matching and typing. To ensure compatibility
3. Obtain and record baseline vital signs
4. Practice strict Asepsis
5. At least 2 licensed nurse check the label of the blood transfusion
o Check the following:
Serial number
Blood component
Blood type
Rh factor
Expiration date
Screening test (VDRL, HBsAg, malarial smear) - *this is to ensure that the blood is
free from blood-carried diseases and therefore, safe from transfusion.
6. Warm blood at room temperature before transfusion to prevent chills.
7. Identify client properly. Two Nurses check the clients identification.
8. Use needle gauge 18 to 19. This allows easy flow of blood.
9. Use BT set with special micron mesh filter. To prevent administration of blood clots and particles.
10. Start infusion slowly at 10 gtts/min. Remain at bedside for 15 to 30 minutes. Adverse reaction
usually occurs during the first 15 to 20 minutes.
11. Monitor vital signs. Altered vital signs indicate adverse reaction.
12. Do not mix medications with blood transfusion. To prevent adverse effects
o Do not incorporate medication into the blood transfusion
o Do not use blood transfusion lines for IV push of medication.
13. Administer 0.9% NaCl before; during or after BT. Never administer IV fluids with dextrose.
Dextrose causes hemolysis.
14. Administer BT for 4 hours (whole blood, packed RBC). For plasma, platelets, cryoprecipitate,
transfuse quickly (20 minutes) clotting factor can easily be destroyed.
15. Observe for potential complications. Notify physician.
Complications of Blood Transfusion
1. Allergic Reaction it is caused by sensitivity to plasma protein of donor antibody, which reacts
with recipient antigen.
o Assessments:
Flushing
Rush, hives
Pruritus
Laryngeal edema, difficulty of breathing
2. Febrile, Non-Hemolytic it is caused by hypersensitivity to donor white cells, platelets or plasma
proteins. This is the most symptomatic complication of blood transfusion
o Assessments:
Sudden chills and fever
Flushing
Headache
Anxiety
3. Septic Reaction it is caused by the transfusion of blood or components contaminated with
bacteria.
o Assessment:
Rapid onset of chills
Vomiting
Marked Hypotension
High fever
4. Circulatory Overload it is caused by administration of blood volume at a rate greater than the
circulatory system can accommodate.
o Assessment:
Rise in venous pressure
Dyspnea
Crackles or rales
Distended neck vein
Cough
Elevated BP
5. Hemolytic reaction. It is caused by infusion of incompatible blood products.
o Assessment:
Low back pain (first sign). This is due to inflammatory response of the kidneys to
incompatible blood.
Chills
Feeling of fullness
Tachycardia
Flushing
Tachypnea
Hypotension
Bleeding
Vascular collapse
Acute renal failure
Assessment findings
1. Clinical manifestations of transfusions complications vary depending on the precipitating factor.
2. Signs and symptoms of hemolytic transfusion reaction include:
o Fever
o Chills
o low back pain
o flank pain
o headache
o nausea
o flushing
o tachycardia
o tachypnea
o hypotension
o hemoglobinuria (cola-colored urine)
3. Clinical signs and laboratory findings in delayed hemolytic reaction include:
o fever
o mild jaundice
o gradual fall of hemoglobin
o positive Coombs test
4. Febrile non-hemolytic reaction is marked by:
o Temperature rise during or shortly after transfusion
o Chills
o headache
o flushing
o anxiety
5. Signs and symptoms of septic reaction include;
o Rapid onset of high fever and chills
o vomiting
o diarrhea
o marked hypotension
6. Allergic reactions may produce:
o hives
o generalized pruritus
o wheezing or anaphylaxis (rarely)
7. Signs and symptoms of circulatory overload include:
o Dyspnea
o cough
o rales
o jugular vein distention
8. Manifestations of infectious disease transmitted through transfusion may develop rapidly or
insidiously, depending on the disease.
9. Characteristics of GVH disease include:
o skin changes (e.g. erythema, ulcerations, scaling)
o edema
o hair loss
o hemolytic anemia
10. Reactions associated with massive transfusion produce varying manifestations
Possible Nursing Diagnosis
1. Ineffective breathing pattern
2. Decreased Cardiac Output
3. Fluid Volume Deficit
4. Fluid Volume Excess
5. Impaired Gas Exchange
6. Hyperthermia
7. Hypothermia
8. High Risk for Infection
9. High Risk for Injury
10. Pain
11. Impaired Skin Integrity
12. Altered Tissue Perfusion
Planning and Implementation
1. Help prevent transfusion reaction by:
o Meticulously verifying patient identification beginning with type and cross match sample
collection and labeling to double check blood product and patient identification prior to
transfusion.
o Inspecting the blood product for any gas bubbles, clothing, or abnormal color before
administration.
o Beginning transfusion slowly ( 1 to 2 mL/min) and observing the patient closely, particularly
during the first 15 minutes (severe reactions usually manifest within 15 minutes after the
start of transfusion).
o Transfusing blood within 4 hours, and changing blood tubing every 4 hours to minimize the
risk of bacterial growth at warm room temperatures.
o Preventing infectious disease transmission through careful donor screening or performing
pretest available to identify selected infectious agents.
o Preventing GVH disease by ensuring irradiation of blood products containing viable WBCs
(i.e., whole blood, platelets, packed RBCs and granulocytes) before transfusion; irradiation
alters ability of donor lymphocytes to engraft and divide.
o Preventing hypothermia by warming blood unit to 37 C before transfusion.
o Removing leukocytes and platelets aggregates from donor blood by installing a
microaggregate filter (20-40-um size) in the blood line to remove these aggregates during
transfusion.
2. On detecting any signs or symptoms of reaction:
o Stop the transfusion immediately, and notify the physician.
o Disconnect the transfusion set-but keep the IV line open with 0.9% saline to provide access
for possible IV drug infusion.
o Send the blood bag and tubing to the blood bank for repeat typing and culture.
o Draw another blood sample for plasma hemoglobin, culture, and retyping.
o Collect a urine sample as soon as possible for hemoglobin determination.
3. Intervene as appropriate to address symptoms of the specific reaction:
o Treatment for hemolytic reaction is directed at correcting hypotension, DIC, and renal
failure associated with RBC hemolysis and hemoglobinuria.
o Febrile, nonhemolytic transfusion reactions are treated symptomatically with antipyretics;
leukocyte-poor blood products may be recommended for subsequent transfusions.
o In septic reaction, treat septicemia with antibiotics, increased hydration, steroids and
vasopressors as prescribed.
o Intervene for allergic reaction by administering antihistamines, steroids and epinephrine as
indicated by the severity of the reaction. (If hives are the only manifestation, transfusion
can sometimes continue but at a slower rate.)
o For circulatory overload, immediate treatment includes positioning the patient upright with
feet dependent; diuretics, oxygen and aminophylline may be prescribed.
Nursing Interventions when complications occurs in Blood transfusion
1. If blood transfusion reaction occurs. STOP THE TRANSFUSION.
2. Start IV line (0.9% Na Cl)
3. Place the client in fowlers position if with SOB and administer O2 therapy.
4. The nurse remains with the client, observing signs and symptoms and monitoring vital signs as
often as every 5 minutes.
5. Notify the physician immediately.
6. The nurse prepares to administer emergency drugs such as antihistamines, vasopressor, fluids,
and steroids as per physicians order or protocol.
7. Obtain a urine specimen and send to the laboratory to determine presence of hemoglobin as a
result of RBC hemolysis.
8. Blood container, tubing, attached label, and transfusion record are saved and returned to the
laboratory for analysis.
Evaluation
1. The patient maintains normal breathing pattern.
2. The patient demonstrates adequate cardiac output.
3. The patient reports minimal or no discomfort.
4. The patient maintains good fluid balance.
5. The patient remains normothermic.
6. The patient remains free of infection.
7. The patient maintains good skin integrity, with no lesions or pruritus.
8. The patient maintains or returns to normal electrolyte and blood chemistry values.
References:
J.Q. Udan, RN, MAN 2004. Mastering Fundamentals of Nursing 2nd ed. Educational Publishing House
Image courtesy of : http://www.beltina.org/pics/blood_transfusion.jpg
The Large Intestine
Primary organ of bowel elimination
Extends from the ileocecal valve to the anus
Functions
Completion of absorption of H2O, Nutrients (chyme from sm. intest. - 1-1.5 L)
Manufacture of some vitamins
Formation of feces
Expulsion of feces from the body
The Small and Large Intestines
Process of Peristalsis
Peristalsis is under control of nervous system
Contractions occur every 3 to 12 minutes
Mass peristalsis sweeps occur 1 to 4 times each 24-hour period
One-third to one-half of food waste is excreted in stool within 24 hours
Peristalic Movements in the Intestine Colonic peristalsis is slow. Mass peristalsis is strong, few
waves per day, stimulated by food in small intestine.
Factors that influence Bowel Elimination
1. Age
2. Diet
3. Position
4. Pregnancy
5. Fluid Intake
6. Activity
7. Psychological
8. Personal Habits
9. Pain
10. Medications
11. Surgery/Anesthesia
Developmental Considerations
Infantscharacteristics of stool and frequency depend on formula or breast feedings
Toddler physiologic maturity is first priority for bowel training (1 2 yrs)
Child, adolescent, adultdefecation patterns vary in quantity, frequency, and rhythmicity
Older adultconstipation is often a chronic problem
Foods Affecting Bowel Elimination
Constipating foods cheese, lean meat, eggs, & pasta
Foods with laxative effectfruits and vegetables, bran, chocolate, alcohol, coffee
Gas-producing foodsonions, cabbage, beans, cauliflower
Effect of Medications on Stool
Aspirin, anticoagulants pink, red, or black stool
Iron saltsblack stool
Antacids white discoloration or speckling in stool
Antibioticsgreen-gray color
Physical Assessment of the Abdomen
Inspectionobserve contour, any masses, scars, or distension
Auscultationlisten for bowel sounds in all quadrants
Note frequency and character, audible clicks, and flatus
Describe bowel sounds as audible, hyperactive, hypoactive, or inaudible Percussionexpect
resonant sound or tympany
Areas of increased dullness may be caused by fluid, a mass, or tumor
Palpationnote any muscular resistance, tenderness, enlargement of organs, masses
Physical Assessment of the Anus and Rectum
Inspection and palpation
Examine anal area for cracks, nodules, distended veins, masses or polyps, fecal mass
Insert gloved finger into anus to assess sphincter tone & smoothness of mucosal lining
Inspect perineal area for skin irritation secondary to diarrhea
Stool Collection
Medical aseptic technique is imperative
Wear disposable gloves
Wash hands before and after glove use
Do not contaminate outside of container with stool
Obtain stool and package, label, and transport according to agency policy
Patient Guidelines for Stool Collection
Void first so urine is not in stool sample
Defecate into the container rather than toilet bowl
Do not place toilet tissue in bedpan or specimen container
Notify nurse when specimen is available
get to lab quickly (30 min) if anything viable in sample ie. parasites, C-diff. etc
Types of Direct Visualization Studies
Esophagogastroduodenoscopy (EGD)
Colonoscopy
Sigmoidoscopy
Wireless capsule endoscopy
Indirect Visualization Studies
Upper gastrointestinal (UGI)
Small bowel series
Barium enema
Scheduling Diagnostic Tests
1 fecal occult blood test
2 barium studies (should precede UGI) make sure ALL barium is removed*
3 endoscopic examinations
Noninvasive procedures take precedence over invasive procedures
Patient Outcomes for Normal Bowel Elimination
Patient has a soft-formed bowel movement every 1-3 days without discomfort
The relationship between bowel elimination and diet, fluid, and exercise is explained
Patient should seek medical evaluation if changes in stool color or consistency persist
Promoting Regular Bowel Habits
Timing -attend to urges promptly
Positioning have pt. sit up, gravity aids in BM
Privacy close door & pull curtain
Nutrition
Exercise abdominal muscles & thighs
Abdominal settings
Thigh strengthening
Individuals at High Risk for Constipation
Patients on bed rest taking constipating medications
Patients with reduced fluids or bulk in their diet
Patients who are depressed
Patients with central nervous system disease or local lesions that cause pain
*Valsalva maneuver (straining & holding breath) intrathoracic / intracranial pressure possible brain
injury
Nursing Measures for the Patient With Diarrhea
Answer call lights immediately
Remove the cause of diarrhea whenever possible (e.g., medication)
If there is impaction, obtain physician order for rectal examination
Give special care to the region around the anus
After diarrhea stops, suggest the intake of fermented dairy products
Fecal seepage may indicate impaction
Preventing Food Poisoning
Never buy food with damaged packaging
Never use raw eggs in any form
Do not eat ground meat uncooked
Never cut meat on a wooden surface
Do not eat seafood that is raw or has unpleasant odor
Clean all vegetables and fruits before eating
Refrigerate leftovers within 2 hours of eating them
Give only pasteurized fruit juices to small children
Methods of Emptying the Colon of Feces
Enemas
Rectal suppositories
Rectal catheters
Digital removal of stool
Types of Enemas
Cleansing high volume
Retention - oil
Return-flow bag of solution taken in (100-300 ml fluid) for pt with gas
Retention Enemas
Oil-retentionlubricate the stool and intestinal mucosa easing defecation
Carminativehelp expel flatus from rectum
Medicatedprovide medications absorbed through rectal mucosa
Anthelminticdestroy intestinal parasites
Nutritiveadminister fluids and nutrition rectally
Bowel Training Programs
Manipulate factors within the patient's control
Food and fluid intake, exercise, time for defecation
Eliminate a soft, formed stool at regular intervals without laxatives
When achieved, discontinue use of suppository if one was used
Types of Colostomies each has different stool consistency
Sigmoid colostomy
Descending colostomy
Transverse colostomy
Ascending colostomy
Ileostomy
Location of (A) a Sigmoid Colostomy and (B) a Descending Colostomy
Location of (C) a Transverse Colostomy and (D) an Ascending Colostomy
Location of an Ileostomy
Colostomy Care
Keep patient as free of odors as possible; empty appliance frequently
Inspect the patient's stoma regularly
Note the size, which should stabilize within 6 to 8 weeks
Keep the skin around the stoma site clean and dry
Measure the patient's fluid intake & output
Explain each aspect of care to the patient and self-care role
Encourage patient to care for and look at ostomy
Normal-Appearing Stoma
Patient Teaching for Colostomies
Community resources are available for assistance
Initially encourage patients to avoid foods high in fiber
Avoid foods that cause diarrhea or flatus
Drink two quarts of water daily
Teach about medications
Teach about odor control (intake of dark green vegetables helps control odor)
Resume normal activity including work and sexual relations
Comfort Measures
Encourage recommended diet and exercise
Use medications only as needed
Apply ointments or astringent (witch hazel)
Use suppositories that contain anesthetics
Characteristics of Normal Stool
1. Color varies from light to dark brown foods & medications may affect color
2. Odor aromatic, affected by ingested food and persons bacterial flora
3. Consistency formed, soft, semi-solid; moist
4. Frequency varies with diet (about 100 to 400 g/day)
5. Constituents small amount of undigested roughage, sloughed dead bacteria and epithelial cells,
fat, protein, dried constituents of digestive juices (bile pigments); inorganic matter (calcium,
phosphates)
Common Bowel Elimination Problems
1. Constipation abnormal frequency of defecation and abnormal hardening of stools
2. Impaction accumulated mass of dry feces that cannot be expelled
3. Diarrhea increased frequency of bowel movements (more than 3 times a day) as well as liquid
consistency and increased amount; accompanied by urgency, discomfort and possibly incontinence
4. Incontinence involuntary elimination of feces
5. Flatulence expulsion of gas from the rectum
6. Hemorrhoids dilated portions of veins in the anal canal causing itching and pain and bright red
bleeding upon defecation.
Cleansing Enemas
Stimulate peristalsis through irrigation of colon and rectum and by distention
1. Soap Suds: Mild soap solutions stimulate and irritate intestinal mucosa. Dilute 5 ml of castile soap
in 1000 ml of water
2. Tap water: Give caution o infants or to adults with altered cardiac and renal reserve
3. Saline: For normal saline enemas, use smaller volume of solution
4. Prepackaged disposable enema (Fleet): Approximately 125 cc, tip is pre-lubricate and does not
require further preparation
Oil-Retention Enemas
Lubricates the rectum and colon; the feces absorb the oil and become softer and easier to pass
Carminative Enema
Provides relief from gaseous distention
Astringent Enema
Contracts tissue to control bleeding
Key Points: Administering Enema
1. Fill water container with 750 to 1000 cc of lukewarm solution, (500 cc or less for children, 250 cc
or less fro an infant), 99 degrees F to 102 degrees F. Solutions that are too hot or too cold, or
solutions that are instilled too quickly, can cause cramping and damage to rectal tissues
2. Allow solution to run through the tubing so that air is removed
3. Place client on left side in Sims position
4. Lubricate the tip of the tubing with water-soluble lubricant
5. Gently insert tubing into clients rectum (3 to 4 inches for adult, 1 inch for infants, 2 to 3 inches for
children), past the external and internal sphincters
6. Raise the water container no more than 12 to 18 inches above the client
7. Allow solution to flow slowly. If the flow is slow, the client will experience fewer cramps. The client
will also be able to tolerate and retain a greater volume of solution
8. After you have instilled the solution, instruct client to hold solution for about 10 to 15 minutes
9. Oil retention: enemas should be retained at least 1 hour. Cleansing enemas are retained 10 to 15
minutes.
References:
FEU In House Review Handout PPD test
1. Read result 48 72 hours after injection.
2. For HIV positive clients, in duration of 5 mm is considered positive
Bronchography
1. Secure consent
2. Check for allergies to seafood or iodine or anesthesia
3. NPO 6-8 hours before the test
4. NPO until gag reflex return to prevent aspiration
Thoracentesis (Aspiration of fluid in the pleural space.)
1. Secure consent, take V/S
2. Position upright leaning on over bed table
3. Avoid cough during insertion to prevent pleural perforation
4. Turn to unaffected side after the procedure to prevent leakage of fluid in the thoracic cavity
5. Check for expectoration of blood. This indicate trauma and should be reported to MD immediately.
Holter Monitor
1. It is continuous ECG monitoring, over 24 hours period
2. The portable monitoring is called telemetry unit
Echocardiogram
1. Ultrasound to assess cardiac structure and mobility
2. Client should remain still, in supine position slightly turned to the left side, with HOB elevated 15-
20 degrees
Electrocardiography
1. If the patients skin is oily, scaly, or diaphoretic, rub the electrode with a dry 4x4 gauze to enhance
electrode contact.
2. If the area is excessively hairy, clip it
3. Remove client`s jewelry, coins, belt or any metal
4. Tell client to remain still during the procedure
Cardiac Catheterization
1. Secure consent
2. Assess allergy to iodine, shellfish
3. V/S, weight for baseline information
4. Have client void before the procedure
5. Monitor PT, PTT, and ECG prior to test
6. NPO for 4-6 hours before the test
7. Shave the groin or brachial area
8. After the procedure : bed rest to prevent bleeding on the site, do not flex extremity
9. Elevate the affected extremities on extended position to promote blood supply back to the heart
and prevent thrombophlebitis
10. Monitor V/S especially peripheral pulses
11. Apply pressure dressing over the puncture site
12. Monitor extremity for color, temperature, tingling to assess for impaired circulation.
MRI
1. Secure consent,
2. The procedure will last 45-60 minute
3. Assess client for claustrophobia
4. Remove all metal items
5. Client should remain still
6. Tell client that he will feel nothing but may hear noises
7. Client with pacemaker, prosthetic valves, implanted clips, wires are not eligible for MRI.
8. Client with cardiac and respiratory complication may be excluded
9. Instruct client on feeling of warmth or shortness of breath if contrast medium is used during the
procedure
UGIS Barium Swallow
1. Instruct client on low-residue diet 1-3 days before the procedure
2. Administer laxative evening before the procedure
3. NPO after midnight
4. Instruct client to drink a cup of flavored barium
5. X-rays are taken every 30 minutes until barium advances through the small bowel
6. Film can be taken as long as 24 hours later
7. Force fluid after the test to prevent constipation/barium impaction
LGIS Barium Enema
1. Instruct client on low-residue diet 1-3 days before the procedure
2. Administer laxative evening before the procedure
3. NPO after midnight
4. Administer suppository in AM
5. Enema until clear
6. Force fluid after the test to prevent constipation/barium impaction
Liver Biopsy
1. Secure consent,
2. NPO 2-4 hrs before the test
3. Monitor PT, Vitamin K at bedside
4. Place the client in supine at the right side of the bed
5. Instruct client to inhale and exhale deeply for several times and then exhale and hold breath while
the MD insert the needle
6. Right lateral post procedure for 4 hours to apply pressure and prevent bleeding
7. Bed rest for 24 hours
8. Observe for S/S of peritonitis
Paracentesis
1. Secure consent, check V/S
2. Let the patient void before the procedure to prevent puncture of the bladder
3. Check for serum protein. Excessive loss of plasma protein may lead to hypovolemic shock.
Lumbar Puncture
1. Obtain consent
2. Instruct client to empty the bladder and bowel
3. Position the client in lateral recumbent with back at the edge of the examining table
4. Instruct client to remain still
5. Obtain specimen per MDs order
References:
J.Q. Udan, RN, MAN 2004. Mastering Fundamentals of Nursing 2nd ed. Educational Publishing House
Ethos - comes from Greek work w/c means character/culture
- Branch of Philosophy w/c determines right and wrong
Moral - personal/private interpretation from what is good and bad.
Ethical Principles:
1. Autonomy the right/freedom to decide (the patient has the right to refuse despite the explanation
of the nurse) Example: surgery, or any procedure
2. Nonmaleficence the duty not to harm/cause harm or inflict harm to others (harm maybe physical,
financial or social)
3. Beneficence- for the goodness and welfare of the clients
4. Justice equality/fairness in terms of resources/personnel
5. Veracity - the act of truthfulness
6. Fidelity faithfulness/loyalty to clients
Moral Principles:
1. Golden Rule
2. The principle of Totality The whole is greater than its parts
3. Epikia There is always an exemption to the rule
4. One who acts through as agent is herself responsible (instrument to the crime)
5. No one is obliged to betray herself You cannot betray yourself
6. The end does not justify the means
7. Defects of nature maybe corrected
8. If one is willing to cooperate in the act, no justice is done to him
9. A little more or a little less does not change the substance of an act.
10. No one is held to impossible
Law - Rule of conduct commanding what is right and what is wrong. Derived from an Anglo-Saxon term
that meansthat which is laid down or fixed
Court - Body/agency in government wherein the administration of justice is delegated.
Plaintiff - Complainant or person who files the case (accuser)
Defendant - Accused/respondent or person who is the subject of complaint
Witness- Individual held upon to testify in reference to a case either for the accused or against the
accused.
Written orders of court
Writ legal notes from the court
1. Subpoena
a. Subpoena Testificandum a writ/notice to an individual/ordering him to appear in court at a
specific time and date as witness.
b. Subpoena Duces Tecum- notice given to a witness to appear in court to testify including all
important documents
Summon notice to a defendant/accused ordering him to appear in court to answer the complaint
against him
Warrant of Arrest - court order to arrest or detain a person
Search warrant - court order to search for properties.
Private/Civil Law - body of law that deals with relationships among private individuals
Public law - body of law that deals with relationship between individuals and the State/government and
government agencies. Laws for the welfare of the general public.
Private/Civil Law :
1. Contract law involves the enforcement of agreements among private individuals or the payment
of compensation for failure to fulfill the agreements
o Ex. Nurse and client nurse and insurance
o Nurse and employer client and health agency
An agreement between 2 or more competent person to do or not to do some lawful
act.
It maybe written or oral= both equally binding
Types of Contract:
1. Expressed when 2 parties discuss and agree orally or in writing the terms and conditions during the
creation of the contract.
Example: nurse will work at a hospital for only a stated length of time (6 months),under stated
conditions (as volunteer, straight AM shift, with food/transportation allowance)
2. Implied one that has not been explicitly agreed to by the parties, but that the law considers to exist.
Example: Nurse newly employed in a hospital is expected to be competent and to follow hospital
policies and procedures even though these expectations were not written or discussed.
Likewise: the hospital is expected to provide the necessary supplies, equipment needed to provide
competent, quality nursing care.
Feature/Characteristics/Elements of a lawful contract:
1. Promise or agreement between 2 or more persons for the performance of an action or restraint from
certain actions.
2. Mutual understanding of the terms and meaning of the contract by all.
3. A lawful purpose activity must be legal
4. Compensation in the form of something of value-monetary
Persons who may not enter into a contract: minor, insane, deaf, mute and ignorant
Tort law
Is a civil wrong committed against a person or a persons property.
Person/persons responsible for the tort are sued for damages
Is based on:
o ACT OF COMMISSION something that was done incorrectly
o ACT OF OMMISION something that should have been done but was not.
Classification of Tort
Unintentional Tort
1. Negligence
Misconduct or practice that is below the standard expected of ordinary, reasonable and prudent
person
Failure to do something due to lack of foresight or prudence
Failure of an individual to provide care that a reasonable person would ordinarily use in a similar
circumstance.
An act of omission or commission wherein a nurse fails to act in accordance with the standard of
care.
Doctrines of Negligence:
a. Res ipsa loquitor the thing speaks for itself the injury is enough proof of negligence
b. Respondeat Superior let the master answer command responsibility
c. Force majuere unforeseen event, irresistible force
2. Malpractice
stepping beyond ones authority
6 elements of nursing malpractice:
a. Duty the nurse must have a relationship with the client that involves providing care and following
an acceptable standard of care.
b. Breach of duty
the standard of care expected in a situation was not observed by the nurse
is the failure to act as a reasonable, prudent nurse under the circumstances
something was done that should not have been done or nothing was done when it should have
been done
c. Foreseeability a link must exist between the nurses act and the injury suffered
d. Causation it must be proved that the harm occurred as a direct result of the nurses failure to
follow the standard of care and the nurse should or could have known that the failure to
follow the standard of care could result in such harm.
e. harm/injury physical, financial, emotional as a result of the breach of duty to the client Example:
physical injury, medical cost/expenses, loss of wages, pain and suffering
f. damages amount of money in payment of damage/harm/injury
Intentional Tort
Unintentional tort do not require intent bur do require the element of HARM
Intentional tort the act was done on PURPOSE or with INTENT
o No harm/injury/damage is needed to be liable
o No expert witnesses are needed
Assault
An attempt or threat to touch another person unjustifiably
Example:
o A person who threatens someone with a club or closed fist.
o Nurse threatens a client with an injection after refusing to take the meds orally.
Battery
Willful touching of a person, persons clothes or something the person is carrying that may or may
not cause harm but the touching was done without permission, without consent, is embarrassing or
causes injury.
Example:
o A nurse threatens the patient with injection if the patient refuses his meds orally. If the
nurse gave the injection without clients consent, the nurse would be committing battery
even if the client benefits from the nurses action.
False Imprisonment
Unjustifiable detention of a person without legal warrant to confine the person
Occurs when clients are made to wrongful believe that they cannot leave the place
Example:
o Telling a client no to leave the hospital until bill is paid
o Use of physical or chemical restraints
o False Imprisonment Forceful Restraint=Battery
Invasion of Privacy
intrusion into the clients private domain
right to be left alone
Types of Invasion the client must be protected from:
1. use of clients name for profit without consent using ones name, photograph for advertisements of
HC agency or provider without clients permission
2. Unreasonable intrusion observation or taking of photograph of the client for whatever purpose
without clients consent.
3. Public disclosure of private facts private information is given to others who have no legitimate
need for that.
4. Putting a person in a false/bad light publishing information that is normally considered offensive
but which is not true.
Defamation
communication that is false or made with a careless disregard for the truth and results in injury to
the reputation of a person
Types:
1. Libel defamation by means of print, writing or picture
o Example:
1. o writing in the chart/nurses notes that doctor A is incompetent because he didnt
respond immediately to a call
2. Slander defamation by the spoken word stating unprivileged (not legally protected) or false word
by which a reputation is damaged
o Example:
Nurse A telling a client that nurse B is incompetent
Person defamed may bring the lawsuit
The material (nurses notes) must be communicated to a 3rd party in order that the
persons reputation maybe harmed
Public Law:
Criminal Law deals with actions or offenses against the safety and welfare of the public.
1. homicide self-defense
2. arson- burning or property
3. theft stealing
4. sexual harassment
5. active euthanasia
6. illegal possession of controlled drugs
Homicide killing of any person without criminal intent may be done as self-defense
Arson willful burning of property
Theft act of stealing
Early Beliefs, Practices and Care of the sick
Early Filipinos subscribed to superstitious belief and practices in relation to health and sickness
Diseases, their causes and treatment were associated with mysticism and superstitions
Cause of disease was caused by another person (an enemy of witch) or evil spirits
Persons suffering from diseases without any identified cause were believed bewitched by
mangkukulam
Difficult childbirth were attributed to nonos
Evil spirits could be driven away by persons with powers to expel demons
Belief in special Gods of healing: priest-physician, word doctors, herbolarios/herb doctors
Early Hospitals during the Spanish Regime
Religious orders exerted efforts to care for the sick by building hospitals in different parts of the
Philippines:
1. Hospital Real de Manila San Juan de Dios Hospital
2. San Lazaro Hospital Hospital de Aguas Santas
3. Hospital de Indios
Prominent personages involved during the Philippine Revolution
1. Josephine Bracken wife of Jose Rizal installed a field hospital in an estate in Tejeros that
provided nursing care to the wounded night and day.
2. Rose Sevilla de Alvaro converted their house into quarters for Filipino soldiers during the Phil-
American War in 1899.
3. Hilaria de Aguinaldo wife of Emlio Aginaldo organized the Filipino Red Cross.
4. Melchora Aquino (Tandang Sora) nursed the wounded Filipino soldiers, gave them shelter and
food.
5. Captain Salomen a revolutionary leader in Nueva Ecija provided nursing care to the wounded
when not in combat.
6. Agueda Kahabagan revolutionary leader in Laguna also provided nursing services to her troops.
7. Trinidad Tecson (Ina ng Biak na Bato) stayed in the hospital at Biac na Bato to care for the
wounded soldiers.
School Of Nursing
1. St. Pauls Hospital School of Nursing, Intramuros Manila 1900
2. Iloilo Mission Hospital Training School of Nursing 1906
o 1909 Distinction of graduating the 1st trained nurses in the Phils. With no standard
requirements for admission of applicants except their willingness to work
o April 1946 a board exam was held outside of Manila. It was held in the Iloilo Mission
Hospital thru the request of Ms. Loreto Tupas, principal of the school.
3. St. Lukes Hospital School of Nursing 1907; opened after four years as a dispensary clinic.
4. Mary Johnston Hospital School of Nursing 1907
5. Philippines General Hospital school of Nursing 1910
College of Nursing
1. UST College of Nursing 1st College of Nursing in the Phils: 1877
2. MCU College of Nursing June 1947 (1st College who offered BSN 4 year program)
3. UP College of Nursing June 1948
4. FEU Institute of Nursing June 1955
5. UE College of Nursing Oct 1958
1909
3 female graduated as qualified medical-surgical nurses
1919
The 1st Nurses Law (Act#2808) was enacted regulating the practice of the nursing profession in
the Philippines Islands. It also provided the holding of exam for the practice of nursing on the 2nd
Monday of June and December of each year.
1920
1st board examination for nurses was conducted by the Board of Examiners, 93 candidates took
the exam, 68 passed with the highest rating of 93.5%-Anna Dahlgren
Theoretical exam was held at the UP Amphitheater of the College of Medicine and Surgery.
Practical exam at the PGH Library.
1921
Filipino Nurses Association was established (now PNA) as the National Organization Of Filipino
Nurses
PNA: 1st President Rosario Delgado
Founder Anastacia Giron-Tupas
1953
Republic Act 877, known as the Nursing Practice Law was approved.
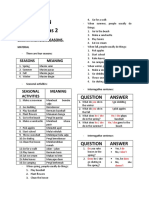
IV Fluid/Solution Quick Reference Guide
Intravenous Solutions are used in fluid replacement therapy by changing the composition of the serum by adding fluids and electrolytes.
Listed below is a table which may serve as your quick reference guide on the different intravenous solutions.
Type Description Osmolality Use Miscellaneous
Normal
Saline
(NS)
0.9% NaCl in
WaterCrystalloid
Solution
Isotonic
(308 mOsm)
Increases
circulating plasma
volume when red
cells are
adequate
Replaces losses
without altering
fluid concentrations.
Helpful for Na+
replacement
1/2
Normal
Saline
(1/2 NS)
0.45% NaCl in
WaterCrystalloid
Solution
Hypotonic
(154 mOsm)
Raises total fluid
volume
Useful for daily
maintenance of
body fluid, but is of
less value for
replacement
of NaCldeficit.
Helpful for
establishing renal
function.
Fluid replacement
for clients who dont
need extra glucose
(diabetics)
Lactated
Ringers
(LR)
Normal saline
with electrolytes
and buffer
Isotonic
(275 mOsm)
Replaces fluid
and buffers pH
Normal saline with
K+, Ca++, and
lactate (buffer)
Often seen with
surgery
D
5
W Dextrose 5% in
water
Crystalloid
solution
Isotonic (in the
bag)
*Physiologically
hypotonic
(260 mOsm)
Raises total fluid
volume.Helpful in
rehydrating and
excretory
purposes.
Provides 170-200
calories/1,000cc for
energy.
Physiologically
hypotonic -the
dextrose is
metabolized quickly
so that only water
remains a
hypotonic fluid
D
5
NS Dextrose 5% in
0.9% saline
Hypertonic
(560 mOsm)
Replaces fluid
sodium, chloride,
and calories.
Watch for fluid
volume overload
D
5
1/2 NS Dextrose 5% in
0.45% saline
Hypertonic
(406 mOsm)
Useful for daily
maintenance of
body fluids and
nutrition, and for
rehydration.
Most common
postoperative fluid
D
5
LR Dextrose 5% in
Lactated
Ringers
Hypertonic
(575 mOsm)
Same as LR plus
provides about
180 calories per
1000ccs.
Watch for fluid
volume overload
Normosol-
R
Normosol Isotonic
(295 mOsm)
Replaces fluid
and buffers pH
pH 7.4
Contains sodium,
chloride,
calcium, potassi
um and magnesium
Common fluid for
OR and PACU
Urine Specimen
1. Clean-Catch mid-stream urine specimen for routine urinalysis, culture and sensitivity test
a. Best time to collect is in the morning, first voided urine
b. Provide sterile container
c. Do perineal care before collection of the urine
d. Discard the first flow of urine
e. Label the specimen properly
f. Send the specimen immediately to the laboratory
g. Document the time of specimen collection and transport to the lab.
h. Document the appearance, odor, and usual characteristics of the specimen.
2. 24-hour urine specimen
a. Discard the first voided urine.
b. Collect all specimens thereafter until the following day
c. Soak the specimen in a container with ice
d. Add preservative as ordered according to hospital policy
3. Second-Voided urine required to assess glucose level and for the presence of albumen in the urine.
a. Discard the first urine
b. Give the patient a glass of water to drink
c. After few minutes, ask the patient to void
4. Catheterized urine specimen
a. Clamp the catheter for 30 min to 1 hour to allow urine to accumulate in the bladder and adequate
specimen can be collected.
b. Clamping the drainage tube and emptying the urine into a container are contraindicated after a
genitourinary surgery.
Stool Specimen
1. Fecalysis to assess gross appearance of stool and presence of ova or parasite
a. Secure a sterile specimen container
b. Ask the pt. to defecate into a clean, dry bed pan or a portable commode.
c. Instruct client not to contaminate the specimen with urine or toilet paper (urine inhibits bacterial
growth and paper towel contain bismuth which interfere with the test result.
2. Stool culture and sensitivity test
To assess specific etiologic agent causing gastroenteritis and bacterial sensitivity to various
antibiotics.
3. Fecal Occult blood test
Are valuable test for detecting occult blood (hidden) which may be present in colo-rectal cancer,
detecting melena stool
a. Hematest- (an Orthotolidin reagent tablet)
b. Hemoccult slide- (filter paper impregnated with guaiac)
*Both test produces blue reaction id occult blood lost exceeds 5 ml in 24 hours.
c. Colocare a newer test, requires no smear
Instructions
1. Advise client to avoid ingestion of red meat for 3 days
2. Patient is advice on a high residue diet
3. Avoid dark food and bismuth compound
4. If client is on iron therapy, inform the MD
5. Make sure the stool in not contaminated with urine, soap solution or toilet paper
6. Test sample from several portion of the stool.
Venipuncture
Pointers
1. Never collect a venous sample from the arm or a leg that is already being use d for I.V therapy or
blood administration because it mat affect the result.
2. Never collect venous sample from an infectious site because it may introduce pathogens into the
vascular system
3. Never collect blood from an edematous area, AV shunt, site of previous hematoma, or vascular
injury.
4. Dont wipe off the povidine-iodine with alcohol because alcohol cancels the effect of povidine
iodine.
5. If the patient has a clotting disorder or is receiving anticoagulant coagulant therapy, maintain
pressure on the site for at least 5 min after withdrawing the needle.
Arterial puncture for ABG test
1. Before arterial puncture, perform Allens test first.
2. If the patient is receiving oxygen, make sure that the patients therapy has been underway for at
least 15 min before collecting arterial sample
3. Be sure to indicate on the laboratory request slip the amount and type of oxygen therapy the
patient is having.
4. If the patient has just received a nebulizer treatment, wait about 20 minutes before collecting the
sample.
Blood specimen
1. No fasting for the following tests:
o CBC, Hgb, Hct, clotting studies, enzyme studies, serum electrolytes
2. Fasting is required:
o FBS, BUN, Creatinine, serum lipid (cholesterol, triglyceride)
Sputum Specimen
1. Gross appearance of the sputum
a. Collect early in the morning
b. Use sterile container
c. Rinse the mount with plain water before collection of the specimen
d. Instruct the patient to hack-up sputum
2. Sputum culture and sensitivity test
a. Use sterile container
b. Collect specimen before the first dose of antibiotic
3. Acid-Fast Bacilli
a. To assess presence of active pulmonary tuberculosis
b. Collect sputum in three consecutive mornings
4. Cytologic sputum exam
a. To assess for presence of abnormal or cancer cells.
Leavell and Clarks Three Levels of Prevention
Primary Prevention
Seeks to prevent a disease or condition at a prepathologic state; to stop something from ever happening.
Health Promotion
health education
marriage counseling
genetic screening
good standard of nutrition adjusted to developmental phase of life
Specific Protection
use of specific immunization
attention to personal hygiene
use of environmental sanitation
protection against occupational hazards
protection from accidents
use of specific nutrients
protections from carcinogens
avoidance to allergens
Secondary Prevention
Also known as Health Maintenance. Seeks to identify specific illnesses or conditions at an early stage with prompt intervention to prevent or limit disability; to prevent
catastrophic effects that could occur if proper attention and treatment are not provided
Early Diagnosis and Prompt Treatment
case finding measures
individual and mass screening survey
prevent spread of communicable disease
prevent complication and sequelae
shorten period of disability
Disability Limitations
Adequate treatment to arrest disease process and prevent further complication and sequelae.
Provision of facilities to limit disability and prevent death.
Tertiary Prevention
Occurs after a disease or disability has occurred and the recovery process has begun; Intent is to halt the disease or injury process and assist the person in obtaining an optimal
health status. To establish a high-level wellness. To maximize use of remaining capacities
Restoration and Rehabilitation
Work therapy in hospital
Use of shelter colony
Maslows Hierarchy of Basic Human Needs
Definition
Each individual has unique characteristics, but certain needs are common to all people.
A need is something that is desirable, useful or necessary. Human needs are physiologic and psychological conditions that an individual must meet to achieve a state of
health or well-being.
Physiologic
1. Oxygen
2. Fluids
3. Nutrition
4. Body temperature
5. Elimination
6. Rest and sleep
7. Sex
Safety and Security
1. Physical safety
2. Psychological safety
3. The need for shelter and freedom from harm and danger
Love and belonging
1. The need to love and be loved
2. The need to care and to be cared for.
3. The need for affection: to associate or to belong
4. The need to establish fruitful and meaningful relationships with people, institution, or organization
Self-Esteem Needs
1. Self-worth
2. Self-identity
3. Self-respect
4. Body image
Self-Actualization Needs
1. The need to learn, create and understand or comprehend
2. The need for harmonious relationships
3. The need for beauty or aesthetics
4. The need for spiritual fulfillment
Characteristics of Basic Human Needs
1. Needs are universal.
2. Needs may be met in different ways
3. Needs may be stimulated by external and internal factor
4. Priorities may be deferred
5. Needs are interrelated
Maslows Characteristics of a Self-Actualized Person
1. Is realistic, sees life clearly and is objective about his or her observations
2. Judges people correctly
3. Has superior perception, is more decisive
4. Has a clear notion of right or wrong
5. Is usually accurate in predicting future events
6. Understands art, music, politics and philosophy
7. Possesses humility, listens to others carefully
8. Is dedicated to some work, task, duty or vocation
9. Is highly creative, flexible, spontaneous, courageous, and willing to make mistakes
10. Is open to new ideas
11. Is self-confident and has self-respect
12. Has low degree of self-conflict; personality is integrated
13. Respect self, does not need fame, and possesses a feeling of self-control
14. Is highly independent, desires privacy
15. Can appear remote or detached
16. Is friendly, loving and governed more by inner directives than by society
17. Can make decisions contrary to popular opinion
18. Is problem centered rather than self-centered
19. Accepts the world for what it is
Metro Manila Development Screening Test (MMDST)
Definition
Simple and clinically useful tool
To determine early serious developmental delays
Dr. William K. Frankenburg
Modified and standardized by Dr. Phoebe D. Williams DDST to MMDST
Developed for health professionals (MDs, RNs, etc) It is not an intelligence test
It is a screening instrument to determine if childs development is within normal
Children 6 years and below
Purposes
Measures developmental delays
Evaluates 4 aspects of development
Aspects of development
In the care of pediatric clients, growth and development are not in isolation. Nurses being competent in the aspects of growth and development particularly principles, theories
and milestones are in best position to counsel clients on these aspects. Having background knowledge on growth and development, nurses are equipped with assessment skills to
determine developmental delays through the aid of screening tests.
The Metro Manila Developmental Screening Test (MMDST) is a screening test to note for normalcy of the childs development and to determine any delays as well in children 6
years old and below. Modified and standardized by Dr. Phoebe Williams from the original Denver Developmental Screening Test (DDST) by Dr. William K. Frankenburg,
MMDST evaluates 4 sectors of development:
Personal-Social tasks which indicate the childs ability to get along with people and to take care of himself
Fine-Motor Adaptive tasks which indicate the childs ability to see and use his hands to pick up objects and to draw
Language tasks which indicate the childs ability to hear, follow directions and to speak
Gross-Motor tasks which indicate the childs ability to sit, walk and jump
MMDST KIT. Preparation for test administration involves the nurse ensuring the completeness of the test materials contained in the MMDST Kit. These materials should be
followed as specified:
MMDST manual
test Form
bright red yarn pom-pom
rattle with narrow handle
eight 1-inch colored wooden blocks (red, yellow, blue green)
small clear glass/bottle with 5/8 inch opening
small bell with 2 inch-diameter mouth
rubber ball 12 inches in circumference
cheese curls
pencil
EXPLAINING THE PROCEDURE. Once the materials are ready, the nurse explains the procedure to the parent or caregiver of the child. It has to be emphasized that this is
not a diagnostic test but rather a screening test only. When conducting the test, the parents or caregivers of the child under study should be informed that it is not an IQ test as it
may be misinterpreted by them. The nurse should also establish rapport with the parent and the child to ensure cooperation.
AGE & THE AGE LINE. To proceed in the administration of the test, the nurse is to compute for the exact age of the child, meaning the age of the child during the test date
itself. The age is the most crucial component of the test because it determines the test items that will be applicable/ administered to the child. The exact age is computing by
subtracting the childs birth date with the test date. After computing, draw the age line in the test form.
TEST ITEMS. There are 105 test items in MMDST but not all are administered. The examiner prioritizes items that the age line passes through. It is however imperative to
explain to the parent or caregiver that the child is not expected to perform all the tasks correctly. If the sequence were to be followed, the examiner should start with personal-
social then progressing to the other sectors. Items that are footnoted with R can be passed by report.
SCORING. The test items are scored as either Passed (P), Failed (F), Refused (R), or Nor Opportunity (NO). Failure of an item that is completely to the left of the childs age is
considered a developmental delay. Whereas, failure of an item that is completely to the right of the childs age line is acceptable and not a delay.
CONSIDERATIONS:
Manner in which each test is administered must be exactly the same as stated in the manual, words or direction may not be changed
If the child is premature, subtract the number of weeks of prematurity. But if the child is more than 2 years of age during the test, subtracting may not be necessary
If the child is shy or uncooperative, the caregiver may be asked to administer the test provided that the examiner instructs the caregiver to administer it exactly as directed
in the manual
If the child is very shy or uncooperative, the test may be deferred
Moral Theories
Freud (1961)
Believed that the mechanism for right and wrong within the individual is the superego, or conscience. He hypnotized that a child internalizes and adopts the moral
standards and character or character traits of the model parent through the process of identification.
The strength of the superego depends on the intensity of the childs feeling of aggression or attachment toward the model parent rather than on the actual standards of
the parent.
Erikson (1964)
Eriksons theory on the development of virtues or unifying strengths of the good man suggests that moral development continuous throughout life. He believed that if
the conflicts of each psychosocial developmental stages favorably resolved, then an egostrength or virtue emerges.
Kohlberg
Suggested three levels of moral development. He focused on the reason for the making of a decision, not on the morality of the decision itself.
1. At first level called the premolar or the preconventional level, children are responsive to cultural rules and labels of good and bad, right and wrong. However children
interpret these in terms of the physical consequences of the actions, i.e., punishment or reward.
2. At the second level, the conventional level, the individual is concerned about maintaining the expectations of the family, groups or nation and sees this as right.
3. At the third level, people make postconventional, autonomous, or principal level. At this level, people make an effort to define valid values and principles without
regard to outside authority or to the expectations of others. These involve respect for other human and belief that relationships are based on mutual trust.
Peter (1981)
Proposed a concept of rational morality based on principles. Moral development is usually considered to involve three separate components: moral emotion (what one
feels), moral judgment (how one reason), and moral behavior (how one act).
In addition, Peters believed that the development of character traits or virtues is an essential aspect or moral development. And that virtues or character traits can be
learned from others and encouraged by the example of others.
Also, Peters believed that some can be described as habits because they are in some sense automatic and therefore are performed habitually, such as politeness, chastity,
tidiness, thrift and honesty.
Gilligan (1982)
Included the concepts of caring and responsibility. She described three stages in the process of developing an Ethic of Care which are as follows.
1. Caring for oneself.
2. Caring for others.
3. Caring for self and others.
She believed the human see morality in the integrity of relationships and caring. For women, what is right is taking responsibility for others as self-chosen decision. On
the other hand, men consider what is right to be what is just.
Spiritual Theories
Fowler (1979)
Described the development of faith. He believed that faith, or the spiritual dimension is a force that gives meaning to a persons life.
He used the term faith as a form of knowing a way of being in relation to an ultimate environment. To Fowler, faith is a relational phenomenon: it is an active
made-of-being-in-relation to others in which we invest commitment, belief, love, risk and hope.
Nasogastric and Intestinal Tubes
Nasogastric Tubes
1. Levin Tube single lumen
a. Suctioning gastric contents
b. Administering tube feedings
2. Salem Sump Tube double lumen (smaller blue lumen vents the tube & prevents suction on the gastric mucosa, maintains intermittent suction regardless of suction
source)
a. Suctioning gastric contents
b. Maintaining gastric decompression
Key Points
1. Prior to insertion, position the client in High-Fowlers position if possible.
2. Use a water-soluble lubricant to facilitate insertion
3. Measure the tube from the tip of the clients nose to the earlobe and from the nose to the xiphoid process to determine the approximate amount of tube to insert to reach
the stomach
4. Flex the clients head slightly forward; this will decrease the chance of entry into the trachea
5. Insert the tube through the nose into the nasopharyngel area; ask the client to swallow, and as the swallow occurs, progress the tube past the area of the trachea and into
the esophagus and stomach. Withdraw tube immediately if client experiences respiratory distress
6. Secure the tube to the nose; do not allow the tube to exert pressure on the upper inner portion of the nares
7. Validating placement of tube.
o Aspirate gastric contents via a syringe to the end of the tube
o Measure ph of aspirate fluid
o Place the stethoscope over the gastric area and inject a small amount of air through the NGT. A characteristic sound of air entering the stomach from the tube
should be heard
8. Characteristics of nasogastric drainage:
o Normally is greenish-yellowish, with strands of mucous
o Coffee-ground drainage old blood that has been broken down in the stomach
o Bright red blood bleeding from the esophagus, the stomach or swallowed from the lungs
o Foul-smelling (fecal odor) occurs with reverse peristalsis in bowel obstruction; increase in amount of drainage with obstruction
Intestinal Tubes
Provide intestinal decompression proximal to a bowel obstruction. Prevent/decrease intestinal distention. Placement of a tube containing a mercury weight and allowing
normal peristalsis to propel tube through the stomach into the intestine to the point of obstruction where decompression will occur
1. Types of Intestinal Tubes
a. Cantor and Harris Tubes
i. Approximately 6-10 feet long
ii. Single lumen
iii. Mercury placed in rubber bag prior to tube insertion
b. Miller-Abbot Tubes
i. Approximately 10 feet long
ii. Double lumen
iii. One lumen utilized for aspiration of intestinal contents
iv. Second lumen utilized to instill mercury into the rubber bag after the tube has been inserted into the stomach
2. Nursing Implications
a. Maintain client on strict NPO
b. Initial insertion usually done by physician and progression of the tube may be monitored via an X-ray
c. After the tube has been placed in the stomach, position client on the right side to facilitae passage through the pyloric valve
d. Advance the tube 2 to 4 inches at regular intervals as indicated by the physician
e. Encourage activity, to facilitate movement of the tube through the intestine
f. Evaluate the type of gastric secretions being aspirated
g. Do not tape or secure the tube until it has reached the desired position
h. Tubes may attached to suction and left in place for several days
i. Offer the client frequent oral hygiene, if possible offer hard candy or gum to reduce thirst
j. Removal of the tube depends on the relief of the intestinal obstruction
k. May be removed by gradual pulling back (4-6 inches per hour) and eventual removal via the nose or mouth
l. May be allowed to progress through the intestines and expelled via the rectum.
How to Insert a Nasogastric (NG) Tube
Check physicians order.
Check clients identaband and if able have client state name.
Discuss procedure to client.
Provide privacy.
Gather equipment.
Position client at 45 degree angle or higher with head elevated.
Wash hands and don clean gloves.
Provide regular oral and nasal hygiene.
Remove gloves and wash hands.
Position client for comfort.
Document procedure.
Nasal Gavage
I. Definition:
In this method of feeding, liquid is introduced into the stomach through a rubber catheter which is passed through the anterior and posterior nose and the pharynx into
the esophagus. When forced feeding is necessary, this method is less exhausting as the mouth does not have to be forced or kept open.
II. Therapeutic Uses:
1. When a patient is weakened and cannot swallow food.
2. Sometimes in the operation of the mouth such as carcinoma of the tongue, a cleft palate or fracture of the jaw etc.
3. In the operation of the throat and sometimes after tracheotomy.
4. In tetanus or meningitis with a locked jaw.
5. In forced feeding for irrational and violet patients.
6. In very weak patient who cannot swallow food vary well.
III. Equipment:
Tray with:
Medium size rubber catheter
Sterile (No.2 French catheter for adult)
Sterile glass syringe or a small glass funnel attached
O.S
Kidney basin
Dressing rubber
Draw sheet
Lubricant
A flask containing the nourishment ordered at temperature of 104 to 105F
IV. Procedure
Food consists of any liquid for which will readily pass through the tube.
The temperature should be warm, not hot, as the lining of the nose is much sensitive than that of the mouth.
The danger of burning the patient is greater when feeding by this method
1. The position of the patient may be lying down with the head turned to one side or sitting up with the head titled forward. An Infant should lie across knees of the nurse
with head turned away from the nurse.
2. Expel the air and lubricate the tube.
3. Insert the curve thru the nose and backward inward the septum. Instruct the patient to make motion of swallowing till about 3 inches of the catheter is introduced.
4. Tell patient to open the mouth and look if the catheter has passed if patient coughs, wait before moving down the catheter.
5. Introduce 6 to 8 inches. Wait until the patient is accustomed to the presence of the tube.
6. Connect the funnel to the catheter; then pour the liquid slowly at the sides. Raise 3 to 4 inches above the nostril and release food slowly.
7. Wait for a few minutes then pinch the tube and withdraw. In some cases the tube is left and hold in place by adhesive.
VI. Precautionary Measures While Doing the Nasal Gavage
The following precautions should be strictly observe during a nasal gavage:
1. The catheter should first be lubricated and in inserting it should be directed toward the septum of the nose. If there is difficulty in passing it, the tube should be removed
and inserted again in the other nostril.
2. As the catheter is small, there is considerable danger of its passing into the larynx therefore the patients color and breathing should be observed closely before pouring
in the solution which if the tube should be in the larynx would down the patient.
3. Even a small amount of food in the lungs would cause a severe irritation, and dyspnea and if, allowed to remain (that is if not cough up) would decompose and probably
lead to a lung abscess or septic pneumonia, if the tube is in the trachea a whistling sound will be heard when the funnel is hold to ear, while if in the esophagus probably
a gurgling sound will be heard.
4. As the tube is soft it may become coiled upon itself in the mouth or in the throat. If the fluid, is poured in while the tube is in this position it will cause gagging,
checking and gasping. And will almost certainly enter the larynx causing dyspnea, cyanosis and later a possible abscess and septic pneumonia. Look in the mouth or
pass the finger to the back of the throat to sea the tube is in position.
5. Before pouring in the solution, wait until the patient is at rest, until all distress has subsided and normal breathing is established and to make sure that the tube is in the
esophagus.
6. Pour in only few drops at first, then pour the balance in very slowly, if there are not symptoms of checking
7. After all the fluid has left the funnel, pinch the catheter and quickly withdraw.
Nursing Jurisprudence
Jurisprudence
It embraces:
1. All laws enacted by the legislative body.
2. All regulations promulgated by those in authority.
3. Court decisions.
4. Formal principles upon which laws are based.
Nursing Jurisprudence
Defined as the department of law that comprises all the legal rules and principles affecting the practice of nursing. It includes not only the study but also the
interpretation of all these rules and principles and their application in the regulation of the practice of nursing.
It deals with:
1. All laws, rules and regulations.
2. Legal principles and doctrines governing and regulating the practice of nursing.
3. Legal opinions and decisions of competent authority in cases involving nursing practice.
Sources of Nursing Jurisprudence in the Philippines
The sources are the following:
1. The Constitution of the Republic of the Philippines, particularly the Bill of Rights.
2. Republic Act No. 7164 otherwise known as the Philippine Nursing Law of 1991.
3. Rules and regulations promulgated by the Board of Nursing and/or Professional Regulation Commission pertaining to nursing practice.
4. Decisions of the Board of Nursing and/or Professional Regulation Commission on nursing cases.
5. Decisions of the Supreme Court on matters relevant to nursing.
6. Opinions of the Secretary of Justice in like cases.
7. The Revised Penal Code.
8. The New Civil Code of the Philippines.
9. The Revised Rule of Courts.
10. The National Internal Revenue Code as amended
Nursing Theorist
Nursing
As defined by the INTERNATIONAL COUNCIL OF NURSES as written by Virginia Henderson.
The unique function of the nurse is to assist the individual, sick or well, in the performance of those activities contributing to health, its recovery, or to a peaceful death
the client would perform unaided if he had the necessary strength, will or knowledge.
Help the client gain independence as rapidly as possible.
Nursing Theory
Over the years, nursing has incorporated theories from non-nursing sources, including theories of systems, human needs, change, problem solving, and decision making.
Barnum defines theory as a construct that accounts for or organizes some phenomenon. A nursing theory, then, describes or explains nursing.
With the formulation of different theories, concepts, and ideas in nursing it:
It guides nurses in their practice knowing what is nursing and what is not nursing.
It helps in the formulations of standards, policies and laws.
It will help the people to understand the competencies and professional accountability of nurses.
It will help define the role of the nurse in the multidisciplinary health care team.
Four Major Concepts
Nurses have developed various theories that provide different explanations of the nursing discipline. All theories, however, share four central concepts: Person refers to all
human beings. People are the recipients of nursing care; they include individuals, families, communities, and groups. Environment includes factors that affect individuals
internally and externally. It means not only in the everyday surroundings but all setting where nursing care is provided. Health generally addresses the persons state of well-
being. The concept of Nursing is central to all nursing theories. Definitions of nursing describe what nursing is, what nurses do, and how nurses interact with clients. Most
nursing theories address each of the four central concepts implicitly or explicitly.
Betty Neuman
(1972, 1982, 1989, 1992)
Health Care System Model
The Neuman System Model or Health Care System Model
Stress reduction is a goal of system model of nursing practice. Nursing actions are in primary, secondary or tertiary level of prevention.
To address the effects of stress and reactions to it on the development and maintenance of health. The concern of nursing is to prevent stress invasion, to protect the
clients basic structure and to obtain or maintain a maximum level of wellness. The nurse helps the client, through primary, secondary, and tertiary prevention modes, to
adjust to environmental stressors and maintain client stability.
Metaparadigm
Person
A client system that is composed of physiologic, psychological, sociocultural, and environmental variables.
Environment
Internal and external forces surrounding humans at any time.
Health
Health or wellness exists if all parts and subparts are in harmony with the whole person.
Nursing
Nursing is a unique profession in that it is concerned with all the variables affecting an individuals response to stressors.
Dorothea Orem
(1970, 1985)
Self-Care Deficit Theory
Self-Care Deficit Theory
Defined Nursing: The act of assisting others in the provision and management of self-care to maintain/improve human functioning at home level of
effectiveness.
Focuses on activities that adult individuals perform on their own behalf to maintain life, health and well-being.
Has a strong health promotion and maintenance focus.
Identified 3 related concepts:
1. Self-care - activities an Individual performs independently throughout life to promote and maintain personal well-being.
2. Health - results when self-care agency (Individuals ability) is not adequate to meet the known self-care needs.
3. Nursing System - nursing interventions needed when Individual is unable to perform the necessary self-care activities:
Wholly compensatory - nurse provides entire self-care for the client.
Example: care of a new born, care of client recovering from surgery in a post-anesthesia care unit
Partial compensatory - nurse and client perform care; client can perform selected self-care activities, but also accepts care done by the nurse for needs
the client cannot meet independently.
Example: Nurse can assist post operative client to ambulate, Nurse can bring a meal tray for client who can feed himself
Supportive-educative - nurses actions are to help the client develop/learn their own self-care abilities through knowledge, support and encouragement.
Example: Nurse guides a mother how to breastfeed her baby, Counseling a psychiatric client on more adaptive coping strategies.
Dorothy E. Johnson
(1980)
Behavioral System Model
Behavioral System Model
Focuses on how the client adapts to illness; the goal of nursing is to reduce stress so that the client can move more easily through recovery.
Viewed the patients behavior as a system, which is a whole with interacting parts.
The nursing process is viewed as a major tool.
To reduce stress so the client can recover as quickly as possible. According to Johnson, each person as a behavioral system is composed of seven subsystems namely:
1. Ingestive. Taking in nourishment in socially and culturally acceptable ways.
2. Eliminated. Riddling the body of waste in socially and culturally acceptable ways.
3. Affiliative. Security seeking behavior.
4. Aggressive. Self protective behavior.
5. Dependence. Nurturance seeking behavior.
6. Achievement. Master of oneself and ones environment according to internalized standards of excellence.
7. Sexual role identity behavior
In addition, she viewed that each person strives to achieve balance and stability both internally and externally and to function effectively by adjusting and adapting to
environmental forces through learned pattern of response. Furthermore, She believed that the patient strives to become a person whose behavior is commensurate with
social demands; who is able to modify his behavior in ways that support biologic imperatives; who is able to benefit to the fullest extent during illness from the health
care professionals knowledge and skills; and whose behavior does not give evidence of unnecessary trauma as a consequence of illness.
Metaparadigm
Person
A system of interdependent parts with patterned, repetitive, and purposeful ways of behaving.
Environment
All forces that affect the person and that influence the behavioral system
Health
Focus on person, not illness. Health is a dynamic state influenced by biologic, psychological, and social factors
Nursing
Promotion of behavioral system, balance and stability. An art and a science providing external assistance before and during balance disturbances
Ernestine Wiedenbach
(1964)
The Helping Art of Clinical Nursing
The Helping Art of Clinical Nursing
Developed the Clinical Nursing A Helping Art Model.
She advocated that the nurses individual philosophy or central purpose lends credence to nursing care.
She believed that nurses meet the individuals need for help through the identification of the needs, administration of help, and validation that actions were helpful.
Components of clinical practice: Philosophy, purpose, practice and an art.
Metaparadigm
Person
Any individual who is receiving help from a member of the health profession or from a worker in the field of health.
Environment
Not specifically addressed
Health
Concepts of nursing, client, and need for help and their relationships imply health-related concerns in the nurseclient relationship.
Nursing
The nurse is a functional human being who acts, thinks, and feels. All actions, thoughts, and feelings underlie what the nurse does.
Faye Glenn Abdellah
(1960)
Twenty One Nursing Problems
Twenty One Nursing Problems
Nursing is broadly grouped into 21 problem areas to guide care and promote the use of nursing judgement.
Introduced Patient Centered Approaches to Nursing Model She defined nursing as service to individual and families; therefore the society. Furthermore, she
conceptualized nursing as an art and a science that molds the attitudes, intellectual competencies and technical skills of the individual nurse into the desire and ability to
help people, sick or well, and cope with their health needs.
21 Nursing Problems
1. To maintain good hygiene.
2. To promote optimal activity; exercise, rest and sleep.
3. To promote safety.
4. To maintain good body mechanics
5. To facilitate the maintenance of a supply of oxygen
6. To facilitate maintenance of nutrition
7. To facilitate maintenance of elimination
8. To facilitate the maintenance of fluid and electrolyte balance
9. To recognize the physiologic response of the body to disease conditions
10. To facilitate the maintenance of regulatory mechanisms and functions
11. To facilitate the maintenance of sensory functions
12. To identify and accept positive and negative expressions, feelings and reactions
13. To identify and accept the interrelatedness of emotions and illness.
14. To facilitate the maintenance of effective verbal and non-verbal communication
15. To promote the development of productive interpersonal relationship
16. To facilitate progress toward achievement of personal spiritual goals
17. To create and maintain a therapeutic environment
18. To facilitate awareness of self as an individual with varying needs.
19. To accept the optimum possible goals
20. To use community resources as an aid in resolving problems arising from illness.
21. To understand the role of social problems as influencing factors
Metaparadigm
Person
The recipients of nursing care having physical, emotional, and sociologic needs that may be overt or covert.
Environment
Not clearly defined. Some discussion indicates that clients interact with their environment, of which nurse is a part.
Health
A state when the individual has no unmet needs and no anticipated or actual impairment.
Nursing
Broadly grouped in 21 nursing problems, which center around needs for hygiene, comfort, activity, rest, safety, oxygen, nutrition, elimination, hydration, physical
and emotional health promotion, interpersonal relationships, and development of self-awareness. Nursing care is doing something for an individual
Florence Nightingale
(1860)
Environmental Theory
Environmental Theory
Defined Nursing: The act of utilizing the environment of the patient to assist him in his recovery.
Focuses on changing and manipulating the environment in order to put the patient in the best possible conditions for nature to act.
Identified 5 environmental factors: fresh air, pure water, efficient drainage, cleanliness/sanitation and light/direct sunlight.
Considered a clean, well-ventilated, quiet environment essential for recovery.
Deficiencies in these 5 factors produce illness or lack of health, but with a nurturing environment, the body could repair itself.
Developed the described the first theory of nursing. Notes on Nursing: What It Is What It Is Not. She focused on changing and manipulating the environment in
order to put the patient in the best possible conditions for nature to act.
Metaparadigm
Person
An individual with vital reparative processes to deal with disease.
Environment
External conditions that affect life and individuals development.
Health
Focus is on the reparative process of getting well
Nursing
Goal is to place the individual in the best condition for good healthcare
Evelyn Tomlin, Helen Erickson, and Mary Ann Swain
(1983)
Modeling and Role Modeling Theory
Modeling and Role Modeling Theory
Developed Modeling and Role Modeling Theory. The focus of this theory is on the person. The nurse models (assesses), role models (plans), and intervenes in this
interpersonal and interactive theory.
They asserted that each individual unique, has some self-care knowledge, needs simultaneously to be attached to the separate from others, and has adaptive potential.
Nurses in this theory, facilitate, nurture and accept the person unconditionally.
Metaparadigm
Person
A differentiation is made between patients and clients in this theory. A patient is given treatment and instruction; a client participates in his or her own care. Our goal
is for nurses to work with clients. A client is one who is considered to be a legitimate member of the decision-making team, who always has some control over the
planned regimen, and who is incorporated into the planning and implementation of his or her own care as much as possible.
Environment
Environment is not identified in the theory as an entity of its own. The theorist see environment in the social subsystems as the interaction between self and others both
cultural and individual. Biophysical stressors are seen as part of the environment.
Health
Health is a state of physical, mental and social well-being, not merely the absence of disease or infirmity. It connotates a state of dynamic equilibrium among the
various subsystems [of a holistic person].
Nursing
The nurse is a facilitator, not an effector. Our nurse-client relationship is an interactive, interpersonal process that aids the individual to identify, mobilize, and develop
his or her own strengths.
Hildegard Peplau
(1951)
Interpersonal Relations Theory
Interpersonal Relations Theory
Defined Nursing: An interpersonal process of therapeutic interactions between an Individual who is sick or in need of health services and a nurse especially educated
to recognize, respond to the need for help.
Nursing is a maturing force and an educative instrument
Identified 4 phases of the Nurse - Patient relationship:
1. Orientation - individual/family has a felt need and seeks professional assistance from a nurse (who is a stranger). This is the problem identification phase.
2. Identification - where the patient begins to have feelings of belongingness and a capacity for dealing with the problem, creating an optimistic attitude from which inner
strength ensues. Here happens the selection of appropriate professional assistance.
3. Exploitation - the nurse uses communication tools to offer services to the patient, who is expected to take advantage of all services.
4. Resolution - where patients needs have already been met by the collaborative efforts between the patient and the nurse. Therapeutic relationship is terminated and the
links are dissolved, as patient drifts away from identifying with the nurse as the helping person.
Metaparadigm
Person
An organism striving to reduce tension generated by needs
Environment
The interpersonal process is always included, and psychodynamic milieu receives attention, with emphasis on the clients culture and mores.
Health
Ongoing human process that implies forward movement of personality and other ongoing human processes in the direction of creative, constructive, productive,
personal, and community living.
Nursing
Interpersonal therapeutic process that functions cooperatively with others human processes that make health possible for individuals in communities. Nursing is an
educative instrument, a maturing force that aims to promote forward movement of personality.
Ida Jean Orlando
(1961)
The Dynamic Nurse-Patient Relationship
The Dynamic Nurse-Patient Relationship
Conceptualized The Dynamic Nurse Patient Relationship Model.
She believed that the nurse helps patients meet a perceived need that the patient cannot meet for themselves. Orlando observed that the nurse provides direct assistance
to meet an immediate need for help in order to avoid or to alleviate distress or helplessness.
She emphasized the importance of validating the need and evaluating care based on observable outcomes.
To interact with clients to meet immediate needs by identifying client behaviors, nurses reactions, and nursing actions to take
Metaparadigm
Person
Unique individual behaving verbally nonverbally. Assumption is that individuals are at times able to meet their own needs and at other times unable to do so
Environment
Not defined
Health
Not defined. Assumption is that being without emotional or physical discomfort and having a sense of well-being contribute to a healthy state.
Nursing
Professional nursing is conceptualized as finding out and meeting the clients immediate need for help.
Imogene King
(1971, 1981)
Goal Attainment Theory
Goal Attainment Theory
Nursing process is defined as dynamic interpersonal process between nurse, client and health care system.
Postulated the Goal Attainment Theory. She described nursing as a helping profession that assists individuals and groups in society to attain, maintain, and restore
health. If is this not possible, nurses help individuals die with dignity.
In addition, King viewed nursing as an interaction process between client and nurse whereby during perceiving, setting goals, and acting on them transactions occurred
and goals are achieved.
Metaparadigm
Person
Biopsychosocial being
Environment
Internal and external environment continually interacts to assist in adjustments to change.
Health
A dynamic life experience with continued goal attainment and adjustment to stressors.
Nursing
Perceiving, thinking, relating, judging, and acting with an individual who comes to a nursing situations
Jean Watson
(1979)
The Philosophy and Science of Caring
The Philosophy and Science of Caring
Nursing is concerned with promotion health, preventing illness, caring for the sick, and restoring health.
Nursing is a human science of persons and human health-illness experiences that are mediated by professional, personal, scientific, esthetic and ethical human care
transactions
She defined caring as a nurturing way or responding to a valued client towards whom the nurse feels a personal sense of commitment and responsibility. It is only
demonstrated interpersonally that results in the satisfaction of certain human needs. Caring accepts the person as what he/she may become in a caring environment
Carative Factors:
1. The formation of a humanistic-altruistic system of values
2. Instillation of faith-hope
3. The cultivation of sensitivity to ones self and others
4. The development of a helping- trust relationship
5. The promotion and acceptance of the expression of positive and negative feelings.
6. The systemic use of the scientific problem-solving method for decision making
7. The promotion of interpersonal teaching-learning
8. The provision for supportive, protective and corrective mental, physical, socio-cultural and spiritual environment
9. Assistance with the gratification of human needs
10. The allowance for existential phenomenological forces
Metaparadigm
Person
A valued being to be cared for, respected, nurtured, understood, and assisted, a fully functional, integrated self
Environment
Social environment, caring and the culture of caring affect health
Health
Physical, mental, and social wellness
Nursing
A human science of people and human health; illness experiences that are mediated by professional, personal, scientific, aesthetic, and ethical human care transactions.
Joyce Travelbee
(1966, 1971)
Interpersonal Aspects of Nursing
Interpersonal Aspects of Nursing
She postulated the Interpersonal Aspects of Nursing Model. She advocated that the goal of nursing individual or family in preventing or coping with illness, regaining
health finding meaning in illness, or maintaining maximal degree of health.
She further viewed that interpersonal process is a human-to-human relationship formed during illness and experience of suffering
She believed that a person is a unique, irreplaceable individual who is in a continuous process of becoming, evolving and changing.
Metaparadigm
Person
A unique, irreplaceable individual who is in a continuous process of becoming, evolving, and changing.
Environment
Not defined
Health
Heath includes the individuals perceptions of health and the absence of disease.
Nursing
An interpersonal process whereby the professional nurse practitioner assists an individual, family, or community to prevent or cope with the experience of illness and
suffering, and if necessary, to find meaning in these experiences.
Lydia Hall
(1964)
Core, Care and Cure Model
Core, Care and Cure Model
The client is composed of the ff. overlapping parts: person (core), pathologic state and treatment (cure) and body (care).
Introduced the model of Nursing: What Is It? Focusing on the notion that centers around three components of Care, Core and Cure.
Care represents nurturance and is exclusive to nursing. Core involves the therapeutic use of self and emphasizes the use of reflection. Cure focuses on nursing related to
the physicians orders. Core and cure are shared with the other health care providers.
The major purpose of care is to achieve an interpersonal relationship with the individual that will facilitate the development of the core.
Metaparadigm
Person
Client is composed of body, pathology, and person. People set their own goals and are capable of learning and growing.
Environment
Should facilitate achievement of the clients personal goals.
Health
Development of a mature self-identity that assists in the conscious selection of actions that facilitate growth.
Nursing
Caring is the nurses primary function. Professional nursing is most important during the recuperative period.
Madeleine Leininger
(1978, 1984)
Transcultural Care Theory and Ethnonursing
Transcultural Care Theory and Ethnonursing
Developed the Transcultural Nursing Model. She advocated that nursing is a humanistic and scientific mode of helping a client through specific cultural caring
processes (cultural values, beliefs and practices) to improve or maintain a health condition.
Nursing is a learned humanistic and scientific profession and discipline which is focused on human care phenomena and activities in order to assist, support, facilitate,
or enable individuals or groups to maintain or regain their well being (or health) in culturally meaningful and beneficial ways, or to help people face handicaps or death.
Transcultural nursing as a learned subfield or branch of nursing which focuses upon the comparative study and analysis of cultures with respect to nursing and health-
illness caring practices, beliefs and values with the goal to provide meaningful and efficacious nursing care services to people according to their cultural values and
health-illness context.
Focuses on the fact that different cultures have different caring behaviors and different health and illness values, beliefs, and patterns of behaviors.
Awareness of the differences allows the nurse to design culture-specific nursing interventions.
Martha Rogers
(1970)
Science of Unitary Man
Science of Unitary Man
Nursing is an art and science that is humanistic and humanitarian. It is directed toward the unitary human and is concerned with the nature and direction of human
development. The goal of nurses is to participate in the process of
Nursing interventions seek to promote harmonious interaction between persons and their environment, strengthen the wholeness of the Individual and redirect human
and environmental patterns or organization to achieve maximum health.
5 basic assumptions:
1. The human being is a unified whole, possessing individual integrity and manifesting characteristics that are more than and different from the sum of parts.
2. The individual and the environment are continuously exchanging matter and energy with each other
3. The life processes of human beings evolve irreversibly and unidirectionally along a space-time continuum
4. Patterns identify human being and reflect their innovative wholeness
5. The individual is characterized by the capacity for abstraction and imagery, language and thought, sensation and emotion
Metaparadigm
Person
Unitary man, a four-dimensional energy field.
Environment
Encompasses all that is outside any given human field. Person exchanging matter and energy.
Health
Not specifically addressed, but emerges out of interaction between human and environment, moves forward, and maximizes human potential.
Nursing
A learned profession that is both science and art. The professional practice of nursing is creative and imaginative and exists to serve people.
Myra Estrin Levine
(1973)
Conservation Model
Conservation Model
Believes nursing intervention is a conservation activity, with conservation of energy as a primary concern, four conservation principles of nursing: conservation of
client energy, conservation of structured integrity, conservation of personal integrity, conservation of social integrity.
Described the Four Conversation Principles. She advocated that nursing is a human interaction and proposed four conservation principles of nursing which are
concerned with the unity and integrity of the individual. The four conservation principles are as follows:
1. Conservation of energy. The human body functions by utilizing energy. The human body needs energy producing input (food, oxygen, fluids) to allow energy
utilization output.
2. Conservation of Structural Integrity. The human body has physical boundaries (skin and mucous membrane) that must be maintained to facilitate health
and prevent harmful agents from entering the body.
3. Conservation of Personal Integrity. The nursing interventions are based on the conservation of the individual clients personality. Every individual has sense
of identity, self worth and self esteem, which must be preserved and enhanced by nurses.
4. Conservation of Social integrity. The social integrity of the client reflects the family and the community in which the client functions. Health care institutions
may separate individuals from their family. It is important for nurses to consider the individual in the context of the family.
Metaparadigm
Person
A holistic being
Environment
Broadly, includes all the individuals experiences
Health
The maintenance of the clients unity and integrity
Nursing
A discipline rooted in the organic dependency of the individual human being on his or her relationship with others
Rosemarie Rizzo Parse
(1981)
Theory of Human Becoming
Theory of Human Becoming
Nursing is a scientific discipline, the practice of which is a performing art
Three assumption about Human Becoming
1. Human becoming is freely choosing personal meaning in situation in the intersubjective process of relating value priorities
2. Human becoming is co-creating rhythmic patterns or relating in mutual process in the universe
3. Human becoming is co-transcending multidimensionality with emerging possibilities.
Metaparadigm
Person
A major reason for nursing existence
Environment
Man and environment interchange energy to create what is in the world, and man chooses the meaning given to the situations he creates
Health
A lived experience that is a process of being and becoming
Nursing
Nursing Practice is directed toward illuminating and mobilizing family interrelationships in light of the meaning assigned to health and its possibilities as language in
the co created patterns of relating.
Sister Callista Roy
(1979)
Adaptation Model
Adaptation Model
Viewed humans as Biopsychosocial beings constantly interacting with a changing environment and who cope with their environment through Biopsychosocial
adaptation mechanisms.
Presented the Adaptation Model. She viewed each person as a unified biopsychosocial system in constant interaction with a changing environment. She contented
that the person as an adaptive system, functions as a whole through interdependence of its part. The system consists of input, control processes, output feedback.
Focuses on the ability of Individuals, families, groups, communities, or societies to adapt to change.
The degree of internal or external environmental change and the persons ability to cope with that change is likely to determine the persons health status.
Nursing interventions are aimed at promoting physiologic, psychologic, and social functioning or adaptation.
To identify the types and demands placed on a client and clients adaptation to the demands.
Metaparadigm
Person
Biopsychological being and the recipient of nursing care.
Environment
All conditions, circumstances, and influences surrounding and affecting the development of an organism or groups of organisms
Health
The person encounters adaptation problems in changing the environment.
Nursing
A theoretical system of knowledge that prescribes a process of analysis and action related to the care of the ill or potentially ill persons
Virginia Henderson
(1955)
The Nature of Nursing Model
The Nature of Nursing Model
Introduced The Nature of Nursing Model. She identified fourteen basic needs.
She postulated that the unique function of the nurse is to assist the clients, sick or well, in the performance of those activities contributing to health or its recovery, the
clients would perform unaided if they had the necessary strength, will or knowledge.
She further believed that nursing involves assisting the client in gaining independence as rapidly as possible, or assisting him achieves peaceful death if recovery is no
longer possible.
Defined Nursing: Assisting the individual, sick or well, in the performance of those activities contributing to health or its recovery (or to peaceful death) that an
individual would perform unaided if he had the necessary strength, will or knowledge.
Identified 14 basic needs :
1. Breathing normally
2. Eating and drinking adequately
3. Eliminating body wastes
4. Moving and maintaining desirable position
5. Sleeping and resting
6. Selecting suitable clothes
7. Maintaining body temperature within normal range
8. Keeping the body clean and well-groomed
9. Avoiding dangers in the environment
10. Communicating with others
11. Worshipping according to ones faith
12. Working in such a way that one feels a sense of accomplishment
13. Playing/participating in various forms of recreation
14. Learning, discovering or satisfying the curiosity that leads to normal development and health and using available health facilities.
Metaparadigm
Person
Individual requiring assistance to achieve health and independence or a peaceful death. Mind and body are inseparable.
Environment
All external conditions and influences that affect life and development
Health
Equated with independence, viewed in terms of the clients ability to perform 14 components of nursing care unaided: breathing, eating, drinking, maintaining comfort,
sleeping, resting clothing, maintaining body temperature, ensuring safety, communicating, worshiping, working, recreation, and continuing development.
Nursing
Assists and supports the individual in life activities and the attainment of independence.
Nutrition
Principles of Nutrition
1. Digestion process by which food substances are changed into forms that can be absorbed through cell membranes
2. Absorption the taking in of substance by cells or membranes
3. Metabolism sum of all physical and chemical processes by which a living organism is formed and maintained and by which energy is made available
4. Storage some nutrients are stored when not used to provide energy; e.g. carbohydrates are stored either as glycogen or as fat
5. Elimination process of discarding unnecessary substances through evaporation, excretion
Nutrients
1. Carbohydrates the primary sources are plant foods
Types of Carbohydrates
a. Simple (sugars) such as glucose, galactose, and fructose
b. Complex such as starches (which are polysaccharides) and fibers (supplies bulk or roughage to the diet)
2. Proteins organic substances made up of amino acids
3. Lipids organic substances that are insoluble in water but soluble in alcohol and ether.
o Fatty acids the basic structural units of all lipids and are either saturated (all the carbon atoms are filled with hydrogen) or unsaturated (could accommodate
more hydrogen than it presently contains)
o Food sources of lipids are animal products (milk, egg yolks and meat) and plants and plant products (seeds, nuts,oils)
4. Vitamins organic compounds not manufactured in the body and needed in small quantities to catalyze metabolic processes.
a. Water-soluble vitamins include C and B-complex vitamins
b. Fat-soluble vitamins include A, D, E, and K and these can be stored in limited amounts in the body
5. Minerals compounds that work with other nutrients in maintaining structure and function of the body
a. Macronutrients calcium, phosphate, sodium, potassium, chloride, magnesium and sulfur
b. Micronutrients (trace elements) iron, iodine, copper, zinc, manganese and fluoride The best sources are vegetables, legumes, milk and some meats
6. Water the bodys most basic nutrient need; it serves as a medium for metabolic reactions within cells and a transporter fro nutrients, waste products and other
substances
Roles and Function of a Nurse
1. Caregiver
The caregiver role has traditionally included those activities that assist the client physically and psychologically while preserving the clients dignity. Caregiving
encompasses the physical, psychosocial, developmental, cultural and spiritual levels.
2. Communicator
Communication is an integral to all nursing roles. Nurses communicate with the client, support persons, other health professionals, and people in the community. In
the role of communicator, nurses identify client problems and then communicate these verbally or in writing to other members of the health team. The quality of a
nurses communication is an important factor in nursing care.
3. Teacher
As a teacher, the nurse helps clients learn about their health and the health care procedures they need to perform to restore or maintain their health. The nurse
assesses the clients learning needs and readiness to learn, sets specific learning goals in conjunction with the client, enacts teaching strategies and measures
learning.
4. Client advocate
Client advocate acts to protect the client. In this role the nurse may represent the clients needs and wishes to other health professionals, such as relaying the clients
wishes for information to the physician. They also assist clients in exercising their rights and help them speak up for themselves.
5. Counselor
Counseling is a process of helping a client to recognize and cope with stressful psychologic or social problems, to developed improved interpersonal relationships, and
to promote personal growth. It involves providing emotional, intellectual, and psychologic support.
6. Change agent
The nurse acts as a change agent when assisting others, that is, clients, to make modifications in their own behavior. Nurses also often act to make changes in a
system such as clinical care, if it is not helping a client return to health.
7. Leader
A leader influences others to work together to accomplish a specific goal. The leader role can be employed at different levels; individual client, family, groups of
clients, colleagues, or the community. Effective leadership is a learned process requiring an understanding of the needs and goals that motivate people, the
knowledge to apply the leadership skills, and the interpersonal skills to influence others.
8. Manager
The nurse manages the nursing care of individuals, families, and communities. The nurse-manager also delegates nursing activities to ancillary workers and other
nurses, and supervises and evaluates their performance.
9. Case manager
Nurse case managers work with the multidisciplinary health care team to measure the effectiveness of the case management plan and to monitor outcomes.
10. Research consumer nurses often use research to improve client care. In a clinical area nurses need to:
Have some awareness of the process and language of research
Be sensitive to issues related to protecting the rights of human subjects
Participate in identification of significant researchable problems
Be a discriminating consumer of research findings
Expanded role of the nurse
1. Clinical Specialists
Is a nurse who has completed a masters degree in specialty and has considerable clinical expertise in that specialty. She provides expert care to individuals,
participates in educating health care professionals and ancillary, acts as a clinical consultant and participates in research.
2. Nurse Practitioner
Is a nurse who has completed either as certificate program or a masters degree in a specialty and is also certified by the appropriate specialty organization. She is
skilled at making nursing assessments, performing P. E., counseling, teaching and treating minor and self- limiting illness.
3. Nurse-midwife
A nurse who has completed a program in midwifery; provides prenatal and postnatal care and delivers babies to woman with uncomplicated pregnancies.
4. Nurse anesthetist
A nurse who completed the course of study in an anesthesia school and carries out pre-operative status of clients.
5. Nurse Educator
A nurse usually with advanced degree, who beaches in clinical or educational settings, teaches theoretical knowledge, clinical skills and conduct research.
6. Nurse Entrepreneur
A nurse who has an advanced degree, and manages health-related business.
7. Nurse administrator
A nurse who functions at various levels of management in health settings; responsible for the management and administration of resources and personnel involved in
giving patient care.
Вам также может понравиться
- Scope of Nle1116aДокумент413 страницScope of Nle1116aericОценок пока нет
- MGT of Care With Answer&RationalesДокумент5 страницMGT of Care With Answer&RationalesJay-Dee Evangelista PacionОценок пока нет
- CHN QuestionsДокумент52 страницыCHN QuestionsJustin VergaraОценок пока нет
- TTS For APOДокумент9 страницTTS For APOJan Joseph BanzuelaОценок пока нет
- Nursing Seminar 1 SAS Session 8Документ8 страницNursing Seminar 1 SAS Session 8ZiaОценок пока нет
- DOH PowerpointДокумент232 страницыDOH PowerpointEmmanuel ApuliОценок пока нет
- Scope of This Nursing Test I Is Parallel To The NP1 NLE CoverageДокумент15 страницScope of This Nursing Test I Is Parallel To The NP1 NLE CoverageHanah Kanashiro AlcoverОценок пока нет
- Top Q&A - Ms and FundaДокумент9 страницTop Q&A - Ms and FundaMarkglennPanganibanОценок пока нет
- Nursing Seminar 1 SAS Session 22Документ9 страницNursing Seminar 1 SAS Session 22ZiaОценок пока нет
- Nursing Leadership and Management: Ethicomoral/ Legal Aspects of Health Care and Nursing PracticeДокумент271 страницаNursing Leadership and Management: Ethicomoral/ Legal Aspects of Health Care and Nursing PracticeRonnie De Vera II100% (1)
- Medical Surgical ATI Proctored Exam 2019 Questions and Answers Verified 100Документ7 страницMedical Surgical ATI Proctored Exam 2019 Questions and Answers Verified 100ianshirow834Оценок пока нет
- Set A: NP1 Nursing Board Exam December 2006 Answer Key 'Foundation of Professional Nursing PracticeДокумент16 страницSet A: NP1 Nursing Board Exam December 2006 Answer Key 'Foundation of Professional Nursing PracticeElizabella Henrietta TanaquilОценок пока нет
- Fundamentals of Nursing - DX Exam 50 Items Without RatioДокумент3 страницыFundamentals of Nursing - DX Exam 50 Items Without RatioDennis Nabor Muñoz, RN,RM100% (1)
- Nle 2019Документ4 страницыNle 2019Jackie AbarraОценок пока нет
- Nurses Baguio 05-2024 (First Timer/Repeaters)Документ59 страницNurses Baguio 05-2024 (First Timer/Repeaters)PRC BaguioОценок пока нет
- Fundamentals of Nursing BulletsДокумент32 страницыFundamentals of Nursing BulletsCatherine G. BorrasОценок пока нет
- Practice QuestionsДокумент24 страницыPractice QuestionsMonique RapleyОценок пока нет
- Nursing Practice IДокумент9 страницNursing Practice IMonique Porcadilla SantiagoОценок пока нет
- Nursing Q and A (Volume 2)Документ7 страницNursing Q and A (Volume 2)Rem Yriz100% (1)
- Test 1Документ33 страницыTest 1julialeo67% (3)
- Community Health/Communicable Disease Nursing INSTRUCTIONS: Select The Correct Answer For Each of The Following Questions. Mark ONLYДокумент11 страницCommunity Health/Communicable Disease Nursing INSTRUCTIONS: Select The Correct Answer For Each of The Following Questions. Mark ONLYjcruzadaОценок пока нет
- Competency Appraisal - Diagnostic TestsДокумент7 страницCompetency Appraisal - Diagnostic TestsMj BrionesОценок пока нет
- Fabs and Onco Post TestДокумент20 страницFabs and Onco Post TestJe KirsteneОценок пока нет
- CHNДокумент14 страницCHNJoyVee Pillagara-De LeonОценок пока нет
- Chapter 6 CardiovascularДокумент10 страницChapter 6 CardiovascularMarie Charmaine100% (1)
- 43 Questions NLE Dec 2011Документ15 страниц43 Questions NLE Dec 2011Lyka Cuanan CorcueraОценок пока нет
- 09 Questions and Rationale On Psychotic DisordersДокумент25 страниц09 Questions and Rationale On Psychotic DisordersLot RositОценок пока нет
- Perioperative Nursing and Concept of Pain PretestДокумент3 страницыPerioperative Nursing and Concept of Pain PretestYucef Bahian-AbangОценок пока нет
- Nursing Practice 1 QuestionДокумент12 страницNursing Practice 1 QuestiongranfrancoОценок пока нет
- Endo QuizДокумент3 страницыEndo Quizمصطفى محمد جواد كاظمОценок пока нет
- Name: Glenda S, Casundo Date: Nov. 3, 2020 Course/Yr: BSN Iv Comp - Appraisal Quiz No.2Документ4 страницыName: Glenda S, Casundo Date: Nov. 3, 2020 Course/Yr: BSN Iv Comp - Appraisal Quiz No.2Joanne Bernadette AguilarОценок пока нет
- CHN Post Test1Документ13 страницCHN Post Test1Cstive ValenzuelaОценок пока нет
- Test 1 NUR 151Документ3 страницыTest 1 NUR 151davidvpnОценок пока нет
- HeheezjghДокумент7 страницHeheezjghDemiar Madlansacay QuintoОценок пока нет
- Chapter 19Документ16 страницChapter 19missy23pap100% (1)
- Flaccid BladderДокумент29 страницFlaccid BladderphotosaurusrapОценок пока нет
- Recalls 7 CompilationДокумент117 страницRecalls 7 CompilationReka LambinoОценок пока нет
- MedicalSurgical Nursing Exam 13 Burns 40 ItemsДокумент5 страницMedicalSurgical Nursing Exam 13 Burns 40 ItemscatneskaОценок пока нет
- Post Test - Emergency NursingДокумент5 страницPost Test - Emergency Nursingpapa.pradoОценок пока нет
- Pre-Board Exam For November 2009 NLEДокумент28 страницPre-Board Exam For November 2009 NLEFranz.thenurse6888100% (1)
- Compt - Appraisal Prelim 2 Glenda CasundoДокумент19 страницCompt - Appraisal Prelim 2 Glenda CasundoJoanne Bernadette AguilarОценок пока нет
- Chapter 2: Health Promotion in Middle-Aged AdultsДокумент10 страницChapter 2: Health Promotion in Middle-Aged AdultsTrixie AlvarezОценок пока нет
- Simu 20 Test 2Документ108 страницSimu 20 Test 2Profile Info100% (1)
- Siadh and Di QuestionsДокумент18 страницSiadh and Di QuestionsRegiever Salvante100% (1)
- Pruritus PRURITIS Pruritis (Itching) Is One of The Most CommonДокумент2 страницыPruritus PRURITIS Pruritis (Itching) Is One of The Most CommonFreeNursingNotesОценок пока нет
- Chapter 01: Professional Nursing Practice Lewis: Medical-Surgical Nursing, 10th EditionДокумент5 страницChapter 01: Professional Nursing Practice Lewis: Medical-Surgical Nursing, 10th EditionKenyia CheatumОценок пока нет
- Phenomena Cause-And-Effect: Brainhub Review: Session 1 Nursing ResearchДокумент22 страницыPhenomena Cause-And-Effect: Brainhub Review: Session 1 Nursing ResearchLynette JavaОценок пока нет
- 100 Item Exam On Fundamentals of Nursing - Pulse - Blood Pressure PDFДокумент12 страниц100 Item Exam On Fundamentals of Nursing - Pulse - Blood Pressure PDFJawad AkbarОценок пока нет
- Simu 20 Test 3Документ114 страницSimu 20 Test 3Profile Info100% (1)
- June 2008 Board Exam TipsДокумент5 страницJune 2008 Board Exam TipsOnil CallejoОценок пока нет
- Nur 111 Session 18 Sas 1Документ11 страницNur 111 Session 18 Sas 1Zzimply Tri Sha UmaliОценок пока нет
- Carl Rogers Erik Erikson Ivan Pavlov Albert Ellis B.F SkinnerДокумент3 страницыCarl Rogers Erik Erikson Ivan Pavlov Albert Ellis B.F Skinnermark OrpillaОценок пока нет
- Allan Ocampo Tutorials: Mobile:0920-5583476 Bus.:273-2245Документ55 страницAllan Ocampo Tutorials: Mobile:0920-5583476 Bus.:273-2245ocampotutorials100% (1)
- COMPREHENSIVE NURSING ACHIEVEMENT TEST (RN): Passbooks Study GuideОт EverandCOMPREHENSIVE NURSING ACHIEVEMENT TEST (RN): Passbooks Study GuideОценок пока нет
- NURSING CARE OF ADULTS II: Passbooks Study GuideОт EverandNURSING CARE OF ADULTS II: Passbooks Study GuideОценок пока нет
- Management of Tuberculosis: A guide for clinicians (eBook edition)От EverandManagement of Tuberculosis: A guide for clinicians (eBook edition)Оценок пока нет
- TFN NotesДокумент83 страницыTFN NotesBrianMarBeltranОценок пока нет
- Nursing Practice II - Community Health Nursing and Care of The Mother and Child - RNpediaДокумент13 страницNursing Practice II - Community Health Nursing and Care of The Mother and Child - RNpediaBrianMarBeltranОценок пока нет
- NURSING PRACTICE IV Care of Clients With Physiologic and Psychosocial Alterations - RNpediaДокумент14 страницNURSING PRACTICE IV Care of Clients With Physiologic and Psychosocial Alterations - RNpediaBrianMarBeltran100% (1)
- Lesson Three - Puberty and Body PartsДокумент6 страницLesson Three - Puberty and Body PartsBrianMarBeltranОценок пока нет
- Nursing Practice I - Foundation of Professional Nursing Practice - RNpediaДокумент2 страницыNursing Practice I - Foundation of Professional Nursing Practice - RNpediaBrianMarBeltranОценок пока нет
- S C 7 1 - Mixtures Worksheet and KEYДокумент4 страницыS C 7 1 - Mixtures Worksheet and KEYBrianMarBeltran33% (3)
- Separation Techniques WorksheetДокумент2 страницыSeparation Techniques WorksheetBrianMarBeltran100% (3)
- Psyche NotesДокумент64 страницыPsyche NotesBrianMarBeltranОценок пока нет
- TFN NotesДокумент83 страницыTFN NotesBrianMarBeltranОценок пока нет
- Three Words Eight LettersДокумент509 страницThree Words Eight Lettersericka_abaya100% (6)
- Step 1. Identify The Problem: Nursing ResearchДокумент2 страницыStep 1. Identify The Problem: Nursing ResearchBrianMarBeltranОценок пока нет
- CHN NotesДокумент50 страницCHN NotesBrianMarBeltranОценок пока нет
- Either or - Neither NorДокумент1 страницаEither or - Neither Norcatarinasilva8Оценок пока нет
- BHM 502atДокумент232 страницыBHM 502atRishabhОценок пока нет
- Observations of Chemical ChangeДокумент2 страницыObservations of Chemical ChangeJessica Loper100% (1)
- Daily Activities at HomeДокумент4 страницыDaily Activities at HomeSneider Rueda100% (1)
- Today's DieticianДокумент68 страницToday's DieticianPooja ManojОценок пока нет
- Max RubnerДокумент28 страницMax RubnerRuben Gutierrez-ArizacaОценок пока нет
- Future Will, Going To and Present Continuous Perfect ContinuousДокумент1 страницаFuture Will, Going To and Present Continuous Perfect ContinuousFelipe Lipe SteinerОценок пока нет
- Inglese SoluzioniДокумент111 страницInglese SoluzioniEmmanueleОценок пока нет
- Branding Handout - UpdatedДокумент31 страницаBranding Handout - UpdatedIBA PrepworksОценок пока нет
- Rogers' Magazine Media KitДокумент41 страницаRogers' Magazine Media KitLucifer PotatoОценок пока нет
- WLP English 4 Q3 WK 2Документ11 страницWLP English 4 Q3 WK 2Geraldine Ison ReyesОценок пока нет
- Causative Form (Part 1)Документ14 страницCausative Form (Part 1)Matheus ThoméОценок пока нет
- 4 Cucina FrescaДокумент3 страницы4 Cucina FrescaSubhadra HaribabuОценок пока нет
- Worktext (TCW) Chapter 11 Global Food Security and Global CitizenshipДокумент7 страницWorktext (TCW) Chapter 11 Global Food Security and Global CitizenshipMae Angelie GarciaОценок пока нет
- Lab Report Moisture ContentДокумент5 страницLab Report Moisture ContentHusna AtiqahОценок пока нет
- Yogini PDFДокумент15 страницYogini PDFMr-AdithyaaОценок пока нет
- Listening Activity March 26th 2021Документ27 страницListening Activity March 26th 2021Federico Plazas G.Оценок пока нет
- Agrarian Reform VS IndustrializationДокумент1 страницаAgrarian Reform VS IndustrializationalyssaОценок пока нет
- Đề cương Nam Trung Yên 2020-2021 đã làmДокумент8 страницĐề cương Nam Trung Yên 2020-2021 đã làmbop1427Оценок пока нет
- Life ExchangeДокумент38 страницLife Exchangepirozokmaks325Оценок пока нет
- Chocolate LasagnaДокумент1 страницаChocolate LasagnaLocksley Belicena AmernaОценок пока нет
- Anthropometric Measurements: Hameed LatifДокумент14 страницAnthropometric Measurements: Hameed LatifSyeda Zainab AbbasОценок пока нет
- Rangkuman English (Pas Sem 2)Документ5 страницRangkuman English (Pas Sem 2)Johanwi Penyuluh Kehutanan MilenialОценок пока нет
- Mapeh Module 2 Pe AnswersДокумент3 страницыMapeh Module 2 Pe AnswersF R N S SОценок пока нет
- Lesson 2: Tap or BottledДокумент8 страницLesson 2: Tap or BottledCarloss Mantilla GonzalesОценок пока нет
- Berlatih Bahasa InggrisДокумент72 страницыBerlatih Bahasa InggrisDewi MulyantiОценок пока нет
- Module 12 Tle 10Документ13 страницModule 12 Tle 10redox franciscoОценок пока нет
- Tasneem PDFДокумент10 страницTasneem PDFVishal MaddhesiyaОценок пока нет
- AWD IntroToWine Powerpoint 1Документ54 страницыAWD IntroToWine Powerpoint 1thành JvОценок пока нет
- Reiki and Essential OilsДокумент4 страницыReiki and Essential OilsPaula Martins50% (2)