Академический Документы
Профессиональный Документы
Культура Документы
Risk of Malignancy Index Is Not Accurate As A Triage Tool For Ovarian Cancer
Загружено:
BrilliantIbnuSina0 оценок0% нашли этот документ полезным (0 голосов)
10 просмотров5 страницOvarian cancer is the second most common gynecological cancer in western women and also in indonesia. Risk of Malignancy Index (RMI) is not accurate as a Triage Tool for ovarian cancer in Dr. Cipto Mangunkusumo Hospital. Most of the patients were nully-parity (28.3%), non-menopausal women (60.6%), normal body mass index (40.4%) and with stage IIIC ova
Исходное описание:
Оригинальное название
Risk of Malignancy Index is Not Accurate as a Triage Tool for Ovarian Cancer
Авторское право
© © All Rights Reserved
Доступные форматы
PDF, TXT или читайте онлайн в Scribd
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документOvarian cancer is the second most common gynecological cancer in western women and also in indonesia. Risk of Malignancy Index (RMI) is not accurate as a Triage Tool for ovarian cancer in Dr. Cipto Mangunkusumo Hospital. Most of the patients were nully-parity (28.3%), non-menopausal women (60.6%), normal body mass index (40.4%) and with stage IIIC ova
Авторское право:
© All Rights Reserved
Доступные форматы
Скачайте в формате PDF, TXT или читайте онлайн в Scribd
0 оценок0% нашли этот документ полезным (0 голосов)
10 просмотров5 страницRisk of Malignancy Index Is Not Accurate As A Triage Tool For Ovarian Cancer
Загружено:
BrilliantIbnuSinaOvarian cancer is the second most common gynecological cancer in western women and also in indonesia. Risk of Malignancy Index (RMI) is not accurate as a Triage Tool for ovarian cancer in Dr. Cipto Mangunkusumo Hospital. Most of the patients were nully-parity (28.3%), non-menopausal women (60.6%), normal body mass index (40.4%) and with stage IIIC ova
Авторское право:
© All Rights Reserved
Доступные форматы
Скачайте в формате PDF, TXT или читайте онлайн в Scribd
Вы находитесь на странице: 1из 5
Research Article
Risk of Malignancy Index is not accurate as a
Triage Tool for Ovarian Cancer
Risiko Indeks Keganasan tidak akurat sebagai
Alat Triage untuk Kanker Ovarium
Gregorius Tanamas, Jasmine Iskandar, Tofan W Utami,
Tricia D Anggraeni, Kartiwa H Nuryanto
Division of Oncology Gynecology
Department of Obstetrics and Gynecology
Faculty of Medicine University of Indonesia/
Dr. Cipto Mangunkusumo Hospital
Jakarta
INTRODUCTION
Ovarian cancer is the second most common gyne-
cological cancer in western women and also in In-
donesia.
1,2
It varies widely in frequency among dif-
ferent geographic regions and ethnic groups. The
majority of cases are sporadic, and only 5% to 10%
of ovarian cancers are familial.
3
Ovarian cancer,
rare before age 40, increases steeply there after
and peaks at ages 65-75. Incidence and mortality
rates are higher among white women than among
Abstract
Objective: To evaluate Risk of Malignancy Index (RMI) as a triage
tool for ovarian cancer in Dr. Cipto Mangunkusumo Hospital.
Method: This is a retrospective study conducted from January 2008-
December 2012 in patients diagnosed with ovarian mass. Patients
admitted for surgery due to ovarian masses were included to this
study. RMI 3 score was calculated based on ultrasonography exami-
nation in Dr. Cipto Mangunkusumo Hospital, CA-125 test and meno-
pausal status. Patients without final pathological report and incom-
plete data were excluded from study. Data were analysed using SPSS
20 to evaluate RMI result and final pathlogical report in benign and
malignant case.
Result: From 882 patients identified with ovarian masses from can-
cer registry, only 99 patients aged 17-70 y.o were included in this
study. Most of the patients were nully-parity (28.3%), non-meno-
pausal women (60.6%), normal body mass index (40.4%), and with
stage IIIC ovarian cancer (33.3%). Ultrasonography examination
showed that most of patients had solid mass and ascites (19.2%).
Meanwhile, CA-125 showed that patients with <35 U/ml were
10.1% and 35 U/ml were 89.9%. Patients with RMI scores <200
(benign cases) were 19 cases (19.2%) and 200 (malignant cases)
were 80 cases (80.8%). Meanwhile, patients with benign final patho-
logical report were 23 cases (23.2%) and malignant cases were 76
cases (76.8%). There was no statistical difference in RMI between
benign and malignant cases based on final pathological report.
Conclusion: Our study showed that RMI was not accurate as triage
tool for ovarian cancer in our hospital. Further investigation and
more patients are needed to confirm this study.
[Indones J Obstet Gynecol 2014; 2-1: 50-54]
Keywords: CA-125, menopausal status, ovarian cancer, risk of ma-
lignancy index (RMI), ultrasonography.
Abstrak
Tujuan: Untuk mengevaluasi Risk of Malignancy Index (RMI) sebagai
alat triase kanker ovarium di Rumah Sakit Dr. Cipto Mangunkusumo.
Metode: Penelitian retrospektif ini dilaksanakan dari Januari 2008
sampai Desember 2012 pada pasien yang didiagnosa dengan massa
pada ovarium. Nilai RMI 3 dihitung berdasarkan pemeriksaan ultra-
sonografi di Rumah Sakit Dr. Cipto Mangunkusumo, nilai CA-125 dan
status menopause. Data dianalisis dengan menggunakan SPSS 20 un-
tuk mengevaluasi hasil RMI dan penilaian patologi akhir pada kasus
jinak dan ganas.
Hasil: Dari 882 pasien yang teridentifikasi dengan massa ovarium
dari registrasi kanker, hanya terdapat 99 pasien yang berusia 17-70
tahun yang memenuhi kriteria inklusi. Sebagian besar pasien adalah
pasien bukan nuliparitas (28,3%), belum menopause (60,6%), Indeks
Massa Tubuh normal (40,4%), dan dengan stadium IIIC (33,3%). Pe-
meriksaan ultrasonografi menunjukkan sebagian besar pasien mem-
punyai massa padat dan asites (19,2%). Sementara itu, terdapat
10,1% pasien dengan kadar CA-125 <35 U/ml dan 89,9% dengan CA-
125 35 U/ml. Terdapat 19 kasus (19,2%) dengan RMI <200 (jinak)
dan 80 kasus (80,8%) dengan RMI 200 (ganas). Pemeriksaan pa-
tologi akhir menunjukkan 23 kasus jinak (23,2%) dan 76 kasus ganas
(76,8%). Tidak terdapat perbedaan yang bermakna secara statistik
pada nilai RMI untuk kasus jinak ataupun ganas berdasarkan peme-
riksaan patologi akhir.
Kesimpulan: Penelitian kami menunjukkan bahwa RMI tidak akurat
sebagai alat triase untuk kanker ovarium di rumah sakit kami. Inves-
tigasi lebih lanjut dan lebih banyak pasien diperlukan untuk meng-
konfirmasi penelitian ini.
[Maj Obstet Ginekol Indones 2014; 2-1: 50-54]
Kata kunci: CA-125, Risk of Malignancy Index (RMI), status meno-
pause, kanker ovarium, ultrasonografi.
Correspondence: Gregorius Tanamas. Department of Obstetrics and Gynecology, Faculty of Medicine University of Indonesia, Jakarta.
Telephone: 085693179775, Email: gregor_7588@yahoo.com
Indones J
50 Tanamas et al Obstet Gynecol
African-American women. Over the last three de-
cades, ovarian cancer incidence has remained sta-
ble in high-risk countries, while an increasing trend
has been reported in low-risk countries.
1,4
Factors associated with an increased risk for in-
vasive epithelial ovarian cancer include age, race,
nulliparity, family history of ovarian cancer, and
history of endometrial or breast cancer.
4
There is
a weak association between ovarian cancer and age
at natural menopause and among women with
early onset disease. Factors associated with a re-
duced risk are history of one or more full-term
pregnancies, use of oral contraceptives, history of
breast feeding, tubal ligation, and hysterectomy.
5
Risk decreased with the number of pregnancies
and sterilization. Use of oral contraceptives signi-
ficantly reduced risk of ovarian cancer and reduced
slightly with duration of use.
6-8
Characterization of adnexal masses to identify
patients with malignant ovarian mass preopera-
tively for referral to a cancer center for treatment
has been extensively studied.
9,10
The accuracy of
ultrasonography in differentiating between benign
and malignant adnexal masses is proportional to
the expertise of the operator.
11,12
Findings sugges-
tive of malignancy in an adnexal mass include a
solid component, thick septations (greater than 2
to 3 mm), bilaterality, Doppler flow to the solid
component of the mass, and presence of ascites.
13
CA-125 (MUC16) has provided a useful serum
tumor marker for monitoring response to chemo-
therapy, detecting disease recurrence, distinguish-
ing malignant from benign pelvic masses, and po-
tentially improving clinical trial design.
14-16
The
normal value for a CA-125 depend on the lab run-
ning the test. In general, a level above 35 U/ml are
considered abnormal.
17
The aims of this study were to evaluate the risk
of malignancy index (RMI) incorporating meno-
pausal status, serum CA-125 levels, and ultrasound
features for discriminating benign from malignant
pelvic masses and to evaluate the performance of
the three different risk of malignancy indices Dr.
Cipto Mangunkusumo Hospital.
METHODS
This is a retrospective study conducted from Ja-
nuary 2008-December 2012 in patients diagnosed
with ovarian mass. Patients admitted for surgery
due to ovarian masses were included to this study.
RMI 3 score was calculated based on ultrasono-
graphy (U) examination in Dr. Cipto Mangunku-
sumo hospital, CA-125 (measured in U/ml) test
and menopausal status (M). Patients without final
pa-thological report and incomplete data were ex-
cluded from study. Data were analyzed using SPSS
20 to evaluate RMI result and final pathological re-
port in benign and malignant case.
Ultrasonography is scored based on five attri-
butes suggestive of malignancy. These attributes
are the presence of solid parts, multilocular cyst,
ascites, bilateral lesions, and intra-abdominal me-
tastases. One point is given for one or no presence
of the attributes, and three points for more than
one attributes. Menopausal woman is given three
points, and non-menopausal woman is given one
point. CA-125 is scored equal to the blood level of
CA-125 (U/ml). RMI score 200 is considered to
be high is of malignancy, and RMI score <200 is
considered to be low risk of malignancy. RMI score
was evaluated based on final pathologic report as
benign or malignant case. When ovarian mass was
malignant, it was staged based on Federation of Gy-
necology and Obstetrics (FIGO) classification.
RESULT
From 882 patients identified with ovarian masses
from cancer registry, only 99 patients aged 17-70
y.o were included in this study. Most of the patients
were nullyparity (28.3%), non-menopausal women
(60.6%), normal body mass index (40.4%), and
with stage IIIC ovarian cancer (33.3%). There were
no significant difference between benign and ma-
lignant case based on age (p = 0.82), parity (p =
0.09), menopausal status (p = 0.6), and CA-125
mean (p = 0.162). Body Mass Index (BMI) showed
significant difference between benign and malig-
nant case (p = 0.011). See Table 1 and 2.
RMI and CA-125 showed good sensitivity (84.2
and 90.8), but Area Under Curve showed low per-
formance (0.57 and 0.51). Our study showed that
RMI, ultrasonography score, CA-125, and meno-
pausal status has poor performance as triage tool.
RMI3=UxMxCA-125
Vol 2, No 1
January 2014 Risk of malignancy index 51
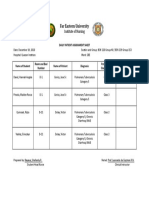
Table 1. Patients Characteristics.
Variable
Benign
(n= 23)
Malignant
(n=76)
p
Age 0.82
a
Median 44 47
Minimum 18 17
Maximum 70 68
Parity 0.09
a
Mean 3 2
Minimum 0 0
Maximum 9 10
Menopause 0.6
b
Yes 8 (8.1%) 31 (31.3%)
No 15 (15.2%) 45 (45.4%)
BMI 0.011
b
Underweight 4 (4%) 20 (20.2%)
Normal 16 (16.2%) 24 (24.2%)
Overweight 1 (1%) 10 (10.2%)
Obese I 2 (2%) 19 (19.2%)
Obese II 0 (0%) 3 (3%)
CA-125 0.162
a
Mean 1662.4 775.9
Minimum 16.6 13.3
Maximum 23566.0 9537.0
a
Mann-Whitney U test
b
Pearson X2 test
Table 2. FIGO Stage
FIGO n = 76
IA 9 (11.8%)
IB 2 (2.7%)
IC 15 (19.8%)
IIA 1 (1.4%)
IIB 5 (6.5%)
IIC 6 (7.9%)
IIIC 33 (43.4%)
IV 5 (6.5%)
Figure 1. Receiver Operator Characteristic (ROC) Curve
Shows the Relationship between Sensitivity and Specificity
for RMI, CA 125, Menopausal Status, USG Score.
Table 3. Area Under Curve, Sensitivity, Specificity, Positive Predictive Value, Negative Predictive Value for RMI, CA-125,
Menopausal Status, USG Score.
Variable
Histopathological result (n = 99)
AUC Sensitivity Specificity
Positive predic-
tive value
Negative predic-
tive value
Malignant Benign
RMI 200 64 16
0.57 84.2 30.4 80.0 36.8
RMI <200 12 7
CA-125 35 U/ml 69 20
0.51 90.8 13.0 77.5 30.0
CA-125 <35 U/ml 7 3
Menopause 31 8
0.53 40.8 65.2 79.4 25.0
Non-menopause 45 15
USG score 3 55 13
0.59 72.4 43.5 80.8 32.2
USG score 1 21 10
Indones J
52 Tanamas et al Obstet Gynecol
DISCUSSION
Many studies showed that Risk of malignancy in-
dex (RMI) is a valuable tool to differ benign from
malignant ovarian mass. It has been used widely
to help clinician in daily practice encountering
adnexal masses.
9,18
RMI is non-invasive and simple
to apply in daily clinical practice.
19
RMI has been
through 4 times modification since it was first in-
troduced in 1990 by Jacob et al.
20
The last modifi-
cation (RMI 4) was introduced in 2009 by
Yamamoto et al, which is added tumor size in cal-
culation.
21
In our study, RMI had good sensitivity (84.2) but
poor specificity (30.4). RMI showed good perfor-
mance as screening tool but poor performance as
triage tool to differ benign from malignant ovarian
mass. Moreover, Area Under Curve of RMI showed
low significance level (0.57). Other study conduc-
ted by Ong C et al in Singapore showed similar re-
sult with our study. Ong C et al concluded that RMI
1, RMI 2, RMI 3, RMI 4 showed no statistical dif-
ference to differ benign from malignant cases in
Southeast Asian population.
19
The components of RMI also showed no statis-
tical difference between benign and malignant
case. CA-125 showed the higher sensitivity (90.8)
with the lowest specificity (13.0). This finding is
consistent with other studies. Metaanalysis study
showed that CA-125 has good sensitivity for de-
tection malignant ovarian mass, but poor specifi-
city.
22,23
CA-125 level was influenced by several
factors, including age, smoking status, ethnicity,
and history of breast cancer. Meanwhile, history of
previous gynecological operation and obesity lo-
wer the CA-125 level.
23
Evaluation of ovarian mass based on ultrasono-
graphy depends on examiners experience. Experi-
enced ultrasonography examiner can determine
benign or malignant adnexal mass accurately.
24
Van Calster et al showed that 93% of tumor were
correctly categorized as benign of malignant by
pattern recognition.
25
Moreover, pattern recogni-
tion was superior than CA-125 to differ benign
from malignant ovarian case.
25
There are several limitation in this study, such
as small number of cases. Eventhough, many cases
were identified, only few of them could be analy-
zed. The problems were medical record storage
system. Many medical records were not found to
be reviewed, and few of them with incomplete
data. Others limiting factors in our study included
its retrospecitve nature and limited time to do the
research.
CONCLUSION
Our study showed that RMI was not accurate as
triage tool for ovarian cancer in our hospital. Fur-
ther investigation and more patients are needed to
confirm this study.
REFERENCES
1. Tjindarbumi D, Mangunkusumo R. Cancer in Indonesia, Pre-
sent and Future. Japan J Clin Oncol 2002; 32(suppl 1): 17-
21.
2. Park B, Park S, Kim TJ, et al. Epidemiological characteristics
of ovarian cancer in Korea. J Gynecol Oncol 2010; 21(4):
241-7.
3. Holschneider CH, Berek JS. Ovarian cancer: epidemiology,
biology, and prognostic factors. Semin Surg Oncol 2000;
19(1): 3-10.
4. Tortolero-Luna G, Mitchell MF. The epidemiology of ovarian
cancer. J Cell Biochem Suppl 1995; 23: 200-7.
5. Modugno F, Ness RB, Wheeler JE. Reproductive risk factors
for epithelial ovarian cancer according to histologic type
and invasiveness. Ann Epidemiol 2001; 11(8): 568-74.
6. Booth M, Beral V, Smith P. Risk factors for ovarian cancer:
a case-control study. Br J Cancer 1989; 60(4): 592-8.
7. Schildkraut JM, Cooper GS, Halabi S, Calingaert B, Hartge P,
Whittemore AS. Age at natural menopause and the risk of
epithelial ovarian cancer. Obstet Gynecol 2001; 98(1): 85-
90.
8. Kurian AW, Balise RR, McGuire V, Whittemore AS. Histologic
types of epithelial ovarian cancer: have they different risk
factors? Gynecol Oncol 2005; 96(2): 520-30.
9. Bailey J, Tailor A, Naik R, et al. Int J Gynecol Cancer 2006;
16 Suppl 1: 30-4.
10. Manjunath AP, Pratapkumar, Sujatha K, Vani R. Comparison
of three risk of malignancy indices in evaluation of pelvic
masses. Gynecol Oncol 2001; 81(2): 225-9.
11. Yazbek J, Raju SK, Ben-Nagi J, Holland TK, Hillaby K, Jurkovic
D. Effect of quality of gynaecological ultrasonography on
management of patients with suspected ovarian cancer: a
randomised controlled trial. Lancet Oncol 2008; 9(2): 124-
31.
12. Van Gorp T, Veldman J, Van Calster B, et al. Subjective as-
sessment by ultrasound is superior to the risk of malig-
nancy index (RMI) or the risk of ovarian malignancy algo-
rithm (ROMA) in discriminating benign from malignant
adnexal masses. Eur J Cancer 2012; 48(11): 1649-56.
13. Givens V, Mitchell GE, Harraway-Smith C, Reddy A, Maness
DL. Diagnosis and management of adnexal masses. Am Fam
Physician 2009; 80(8): 815-20.
14. Vorgias G, Iavazzo C, Savvopoulos P, et al. Can the preope-
rative Ca-125 level predict optimal cytoreduction in pa-
tients with advanced ovarian carcinoma? A single institu-
tion cohort study. Gynecol Oncol 2009; 112(1): 11-5.
15. Bast RC, Jr., Badgwell D, Lu Z, et al. New tumor markers:
Vol 2, No 1
January 2014 Risk of malignancy index 53
CA125 and beyond. Int J Gynecol Cancer 2005; 15 Suppl 3:
274-81.
16. Scholler N, Urban N. CA125 in ovarian cancer. Biomark Med
2007; 1(4): 513-23.
17. Nguyen HN, Jacobson A, Patino-Paul R. New reference levels
for CA125 in pre- and postmenopausal women. Prim Care
Update Ob Gyns 1998; 5(4): 157.
18. Ma S, Shen K, Lang J. [Effect of a risk of malignancy index
in preoperative diagnosis of ovarian cancer]. Zhonghua Fu
Chan Ke Za Zhi 2001; 36(3): 162-4.
19. Ong C, Biswas A, Choolani M, Low JJ. Comparison of risk of
malignancy indices in evaluating ovarian masses in a South-
east Asian population. Sing Med J 2013; 54(3): 136-9.
20. Jacobs I, Oram D, Fairbanks J, Turner J, Frost C, Grudzinskas
JG. A risk of malignancy index incorporating CA-125, ultra-
sound and menopausal status for the accurate preoperative
diagnosis of ovarian cancer. Maturitas 1991; 13(2): 177.
21. Yamamoto Y, Yamada R, Oguri H, Maeda N, Fukaya T. Com-
parison of four malignancy risk indices in the preoperative
evaluation of patients with pelvic masses. Eur J Obstet Gy-
naecol Reprod Biol 2009; 144(2): 163-7.
22. Medeiros LR, Rosa DD, da Rosa MI, Bozzetti MC. Accuracy
of CA-125 in the diagnosis of ovarian tumors: A quantitative
systematic review. Eur J Obstet Gynaecol Reprod Biol 2009;
142(2): 99-105.
23. Johnson CC, Kessel B, Riley TL, et al. The epidemiology of
CA-125 in women without evidence of ovarian cancer in
the Prostate, Lung, Colorectal and Ovarian Cancer (PLCO)
Screening Trial. Gynecol Oncol 2008; 110(3): 383-9.
24. van den Akker PAJ, Aalders AL, Snijders MPLM, et al. Evalu-
ation of the risk of malignancy index in daily clinical man-
agement of adnexal masses. Gynecol Oncol 2010; 116(3):
384-8.
25. Van Calster B, Timmerman D, Bourne T, et al. Discrimina-
tion between benign and malignant adnexal masses by spe-
cialist ultrasound examination versus serum CA-125. J Natl
Cancer Inst 2007; 99(22): 1706-14.
Indones J
54 Tanamas et al Obstet Gynecol
Вам также может понравиться
- The Yellow House: A Memoir (2019 National Book Award Winner)От EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Рейтинг: 4 из 5 звезд4/5 (98)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeОт EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeРейтинг: 4 из 5 звезд4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingОт EverandThe Little Book of Hygge: Danish Secrets to Happy LivingРейтинг: 3.5 из 5 звезд3.5/5 (400)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureОт EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureРейтинг: 4.5 из 5 звезд4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryОт EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryРейтинг: 3.5 из 5 звезд3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceОт EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceРейтинг: 4 из 5 звезд4/5 (895)
- Team of Rivals: The Political Genius of Abraham LincolnОт EverandTeam of Rivals: The Political Genius of Abraham LincolnРейтинг: 4.5 из 5 звезд4.5/5 (234)
- Never Split the Difference: Negotiating As If Your Life Depended On ItОт EverandNever Split the Difference: Negotiating As If Your Life Depended On ItРейтинг: 4.5 из 5 звезд4.5/5 (838)
- The Emperor of All Maladies: A Biography of CancerОт EverandThe Emperor of All Maladies: A Biography of CancerРейтинг: 4.5 из 5 звезд4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaОт EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaРейтинг: 4.5 из 5 звезд4.5/5 (266)
- The Unwinding: An Inner History of the New AmericaОт EverandThe Unwinding: An Inner History of the New AmericaРейтинг: 4 из 5 звезд4/5 (45)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersОт EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersРейтинг: 4.5 из 5 звезд4.5/5 (345)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyОт EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyРейтинг: 3.5 из 5 звезд3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreОт EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreРейтинг: 4 из 5 звезд4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)От EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Рейтинг: 4.5 из 5 звезд4.5/5 (121)
- Diabetes QuestionsДокумент6 страницDiabetes QuestionsLara B100% (3)
- 10 Bilateral Schwartze Sign, Decision-Making For Surgery. Iranian Journal of OtorhinolaryngologyДокумент1 страница10 Bilateral Schwartze Sign, Decision-Making For Surgery. Iranian Journal of OtorhinolaryngologyNurulSyaidahОценок пока нет
- Assessment of Knowledge of Public On Coronary Artery Disease, Hypertension and Diabetes MellitusДокумент5 страницAssessment of Knowledge of Public On Coronary Artery Disease, Hypertension and Diabetes MellitusMythili MuthappaОценок пока нет
- Inverted Nipple PaperДокумент7 страницInverted Nipple PaperFarisah Dewi Batari EmsilОценок пока нет
- P QuizletДокумент2 страницыP QuizletFgg FggОценок пока нет
- 9 The Post Anesthesia Care UnitДокумент77 страниц9 The Post Anesthesia Care Unitsanjivdas100% (1)
- RESUME For DentistДокумент2 страницыRESUME For Dentistvijay37010% (1)
- ADCHEM Percentage StohsДокумент18 страницADCHEM Percentage StohsMelvin CabonegroОценок пока нет
- (Journal Reading) A Randomized Trial of Adenotonsillectomy For Childhood Sleep ApneaДокумент27 страниц(Journal Reading) A Randomized Trial of Adenotonsillectomy For Childhood Sleep ApneaKharisma BimoОценок пока нет
- LWS101 Week 2 Ethics PPTslidesДокумент44 страницыLWS101 Week 2 Ethics PPTslidesJanet YauОценок пока нет
- Project Report NewДокумент48 страницProject Report NewPrincy Sony AntonyОценок пока нет
- Pnle CHNДокумент25 страницPnle CHNLrak Eed0% (1)
- Antibiotic Grouping by MechanismДокумент11 страницAntibiotic Grouping by MechanismalterОценок пока нет
- Diadynamic CurrentДокумент30 страницDiadynamic Currentpartizan_bl100% (2)
- Daily Patient Assignment SheetДокумент1 страницаDaily Patient Assignment SheetSheferely BayauaОценок пока нет
- CPR PresentationДокумент33 страницыCPR Presentationathar.shahОценок пока нет
- 2013 Skin and Wound Infections - StudentДокумент35 страниц2013 Skin and Wound Infections - Studentmicroperadeniya0% (1)
- Clinic Handbook of GastroenterologyДокумент285 страницClinic Handbook of Gastroenterologyansarijaved100% (1)
- IndianJRadiolImaging - Imaging in Laringeal CancerДокумент18 страницIndianJRadiolImaging - Imaging in Laringeal CancerMirela IordacheОценок пока нет
- Skripsi Full Tanpa Bab PembahasanДокумент53 страницыSkripsi Full Tanpa Bab Pembahasanfani akifaazriОценок пока нет
- Who en enДокумент307 страницWho en enAafreen ShaikhОценок пока нет
- Practical Work CA On DX 2012Документ26 страницPractical Work CA On DX 2012Nurul Aulia AbdullahОценок пока нет
- 05 N293 33108Документ23 страницы05 N293 33108Arjay G ParaniОценок пока нет
- Update Therapeutic CommunicationДокумент11 страницUpdate Therapeutic CommunicationSupriyatin AjjaОценок пока нет
- DR - Gold Created by SiraДокумент26 страницDR - Gold Created by SiraMohamed ElhabetОценок пока нет
- Countercoup Skull FracturesДокумент5 страницCountercoup Skull FracturesVinay KumarОценок пока нет
- Vitalograph - Hygiene Considerations For SpirometryДокумент4 страницыVitalograph - Hygiene Considerations For SpirometryEileenYingYeeОценок пока нет
- Validity of The Lateral Gliding Test As Tool ForДокумент7 страницValidity of The Lateral Gliding Test As Tool ForFelippe GuarigliaОценок пока нет
- AA Effectiveness - Faith Meets ScienceДокумент68 страницAA Effectiveness - Faith Meets SciencejgogekОценок пока нет
- 41 Prep GuideДокумент73 страницы41 Prep Guidedaljit chahalОценок пока нет