Академический Документы
Профессиональный Документы
Культура Документы
Stroke
Загружено:
cgarci0 оценок0% нашли этот документ полезным (0 голосов)
26 просмотров13 страницThe technical term for stroke is cerebrovascular accident or CVA. Without warning, it seems to appear out of nowhere. The majority of those who experience a CVA episode survive.
Исходное описание:
Авторское право
© © All Rights Reserved
Доступные форматы
DOCX, PDF, TXT или читайте онлайн в Scribd
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документThe technical term for stroke is cerebrovascular accident or CVA. Without warning, it seems to appear out of nowhere. The majority of those who experience a CVA episode survive.
Авторское право:
© All Rights Reserved
Доступные форматы
Скачайте в формате DOCX, PDF, TXT или читайте онлайн в Scribd
0 оценок0% нашли этот документ полезным (0 голосов)
26 просмотров13 страницStroke
Загружено:
cgarciThe technical term for stroke is cerebrovascular accident or CVA. Without warning, it seems to appear out of nowhere. The majority of those who experience a CVA episode survive.
Авторское право:
© All Rights Reserved
Доступные форматы
Скачайте в формате DOCX, PDF, TXT или читайте онлайн в Scribd
Вы находитесь на странице: 1из 13
Stroke, what happens during a
Mzagzoug (in hubpages.com)
A man finds himself in familiar surroundings. He goes about his usual business doing what he
typically does, whether it is completing work, chores, or playing some golf, when all of a
sudden; the world around him no longer makes sense. His surroundings appear as if they have
been cut in half. He begins to experience a severe pounding headache. His vision becomes
blurry and he is disoriented. He has no movement. No feeling. No sensation. He experiences
numbness and loses complete control over one side of his body. He falls to the ground. His
arms and legs are paralyzed and no matter how hard he struggles to get up, it seems
impossible. He makes an attempt to call for help but the words coming out of his mouth sound
like gibberish. He tires to scream but his voice sounds distant because his mouth is too dry and
he cannot move his lips. If he is alone, fear and hopelessness might overwhelm him and he will
wonder if anyone will ever find him in his helpless state. This is the nightmare that stroke
victims face, a frightening scenario that leaves a person wondering whether or not they will live.
The technical term for stroke is cerebrovascular accident or CVA. The name for this condition
is most fitting since it is sudden and violent. Without warning, it seems to appear out of
nowhere. One minute, a person can be perfectly healthy and then, out of the blue, the
individual is left devastated by the paralyzing effects of CVA. Contrary to popular belief that it is
a condition commonly seen among the elderly, it is important to note that it can happen at any
age. The majority of those who experience a CVA episode survive, but many are left with
varying degrees of physical incapacities. The effects can range from mild to severe and can
include paralysis, problems with thinking, problems with speaking, and emotional problems
(Wiebers, p. 14). In fact, CVA is the main cause of serious disability. Not only do CVA patients
have to contend with physical problems but the shock of what has happened to them only adds
to their anger and frustration. Fortunately, it is one of the most preventable neurological
disorders. Many forms of CVA can be prevented by learning the risk factors and incorporating
healthy lifestyle changes.
Pathology of CVA:
Cerebrovascular accident (CVA) is a brain attack that results the same way a heart attack
does due to blockage of blood flow. The only difference is that instead of dealing with blood
flow problems to the heart, CVA deals with blood flow problems to the brain (Burkman, p. 4).
More specifically, it is the destruction of brain tissue caused by the lack of blood supply. When
blood flow to the brain is impeded, oxygen and vital nutrients cannot be delivered to the brain,
causing brain cells to suffocate and die from oxygen starvation within minutes. This sudden
disruption of blood supply to a part of the brain triggers disruption of certain body functions
controlled by that area of the brain.
In order to understand the cause and impact CVA has on the brain, it is necessary to
understand how the brain functions and how blood flows to the brain. The brain operates in a
holistic manner. Although certain parts of the brain perform certain functions, all of these parts
are interconnected and thus no specific area works alone (Tanner, p. 24). It is noted that the
brain utilizes 20 percent of the total blood supply to get the oxygen and nutrients that it needs
(Senelick, Rossi, & Dougherty, p. 27). When blood moves from the heart to the brain, it does
so by passing through the carotid arteries. The carotid arteries are located at the neck traveling
up along the windpipe. Upon reaching the skull the arteries divide and branch out in various
areas of the brain where they supply oxygen and nutrients to those areas (Burkman, p. 11).
Different regions of the brain work to control high mental functions as well as sensory and
motor skills. These regions are composed of nerve cells, or neurons, that have specific
functions. Each neuron consists of three parts: dendrites, cell body, and axon. These three
components work together to receive and relay messages to the rest of the body. In a CVA
episode, if this mechanism gets interrupted due to lack of oxygen, then the entire
electrochemical process fails and the functions these brain regions control no longer work
properly (Buckman, p.11). The individual would lose consciousness within five to ten seconds
and if persisted long enough, brain damage will occur (Senelick, Rossi, & Dougherty, p. 26).
What Happens in a CVA Episode?
When CVA strikes, after about 4 minutes without blood and oxygen the brain cells become
damaged. The damage spreads during the following hours. The body tries to restore blood and
oxygen to the cells by enlarging other blood vessels or arteries near the area. If the blockage is
in a large blood vessel, such as the carotid artery, the body may be able to supply blood to the
affected area through other blood vessels. If blood supply is not restored within one hour,
permanent brain damage usually occurs (Rogers, 2003). When brain cells are damaged or die,
the body parts controlled by those cells lose their ability to function. The loss of function may
be mild or severe, temporary or permanent. This all depends on where and how much of the
brain is damaged, the age and general health of the patient, what part of the brain the CVA
occurred in, and how fast the blood supply can be returned to the affected cells. Consequently,
this is why every minute counts when someone is experiencing a CVA. While every CVA
occurrence has different consequences, the longer blood flow is cut off to the brain, the greater
the damage. In any case of CVA, immediate treatment is crucial since not only can it save the
persons life but it can also enhance their chances for successful recovery (Wiebers, p. 222).
Causes of CVA:
There is no single cause of CVA; it is brought on by a combination of factors. However, there
are some commonly associated conditions which include high blood pressure, smoking,
diabetes, irregular heartbeat, arterial disease, and ageing. These conditions can lead to the
pathologic causes of CVA. The chains of events that occur in a CVA episode are commonly
caused by blood clots found in the artery. This blockage is medically referred to as thrombosis.
Typically, clots in the blood vessels form due to long-term, damaging effects of high blood
pressure, which are referred to as hypertension. In other situations, CVA occurs as a result of
artherosclerosis, commonly known as hardening of the arteries. This is due to the accumulated
deposit of fat into the walls of the arteries, eventually becoming large enough to obstruct blood
flow. Alternatively, in some instances, the accumulation of fat deposits, known as plaque, can
break off in a large artery, such as the carotid artery found in the neck, and travel down to a
smaller vessel in the brain where they get lodged. This process is called embolism and when
that happens; the flow of oxygen-rich blood is hindered leading to CVA (Cicala, p. 67).
Cerebral hemorrhage, bleeding within the brain, is a different cause of CVA. It takes place
when a blood vessel in the brain ruptures, causing bleeding inside the skull. Aneurysm, or
abnormal ballooning out of the wall of the vessels, take place and the bleeding can tear
through the delicate connections within the brain, eventually compressing brain cells to the
point where they die (Cicala, p. 71).
Furthermore, hypotension is an another major cause of CVA. It occurs when blood pressure
falls to dangerously low levels because an insufficient amount of blood is pumped to the brain.
The brain damage which results from this condition is referred to as anoxic encephalopathy.
Patients with this condition differ from all other CVA patients in that all, not just part, of the
brain may lose its blood supply. This can happen in cases of severe heart failure, certain
abnormal heart rhythms, and in some heart attacks when the heart fails to adequately pump
blood (Burkman, p. 7).
Types of CVA:
About 80 percent of all CVA occurrences are ischemic strokes. If the blood supply is
interrupted only briefly and the symptoms vanish within twenty-four hours, the CVA is
referred to as a transient ischemic attack or TIA. These types of CVA are often referred to
as short-term strokes or mini-strokes (Wiebers, p. 18-19). TIAs leave no permanent brain
tissue damage. The oxygen supply to the brain is restored quickly, and symptoms disappear
completely. However, TIAs are often a red flag warning of serious risk of a major stroke and
thus prompt medical attention is essential. Without treatment, about 30 percent of those who
suffer a TIA are at high risk of having a major CVA episode within the next three years
(Buckman, p. 14).
Cerebral thrombosis is another type of CVA. It occurs when cholesterol build-up causes a
blood clot to form in an artery or blood vessel supplying blood to the brain. This form of CVA is
commonly due to the accumulation of fat deposits into the arterial walls. The clot interrupts the
blood supply and brain cells are starved of oxygen (McMurdo, 2003).
The third type of CVA is cerebral embolism. It is a blood clot that forms in larger, open
blood vessels before traveling through the smaller blood vessels and lodging in the brain. The
middle cerebral artery, located in the middle portion of the brain, is most often affected by
emboli. When a clot is lodged in a blood vessel, it causes the brain cells to become starved of
oxygen. Sometimes clots will break up into smaller pieces quickly enough to restore the blood
flow (Burkman, p. 5). In diagnosis, a physician may perform a transthoracic or transeophageal
echocardiogram to help determine whether an abnormality inside the heart is responsible for
emboli (Burkman, p. 6).
Cerebral hemorrhage, a dangerous type of CVA, occurs when a weakened blood vessel
ruptures inside the brain and bleeds or hemorrhages. Hemorrhages can be caused by
aneurysms in which weakened blood vessels form bubble-shaped projections then break.
Usually, this event takes place without warning, except an acute or severe headache (Senelick,
Rossi, & Dougherty, p. 50). Hemorrhagic CVA can either be a subarachnoid hemorrhage or
intercerebral hemorhage. A subarachnoid hemorrhage results from bleeding in the deeper
cavities of the brain. An intracerebral hemorrhage occurs when a blood vessel bursts. With a
hemorrhage, the force of blood that escapes from the blood vessel can damage surrounding
brain tissue by the blood that seeps into it (Cleveland Clinic Health System, 2003). Pressure
from the bleeding can pinch blood vessels, shutting off more blood flow and producing further
stroke effects.
Cerebral hemorrhagic strokes are the most deadly, due to the pressure they can produce on
vital parts of the brain. They are typically brought on by hypertension as a result of poorly
controlled high blood pressure.
Signs & Symptoms of CVA:
The symptoms of CVA vary depending on the type and severity. The effects of a CVA are
primarily based on the location where the obstruction occurs and the extent of damage
incurred on the brain tissue. When blood flow is obstructed to a particular region of the brain,
that part of the brain will malfunction. In other words, since the right side of the brain controls
the left side of the body and the left side of the brain controls the right side of the body, a CVA
that occurs on one side of the brain will result in neurological complications on the side of the
body it affects (American Stroke Association: Effects of Stroke, 2004). Generally, the most
common symptoms include:
Numbness, weakness, or paralysis of the face, arm, or leg, especially on one side of the
body; depending on which side of the brain is afflicted.
Vision problems such as dimness, blurring, double vision, or loss of vision.
Difficulty with walking, dizziness, loss of balance or coordination.
Sudden severe headache with no known cause.
Confusion, speech, and language problems. Aphasia is a condition that results when the
individual has trouble understanding what is being said to them or, they may understand what
is being said but may not be able to think of the words to respond. On the other hand, a person
with dysarthria has speech problems in which the person knows the right words but has trouble
with articulation and cannot speak clearly (Burkman, p. 28-31).
The right hemisphere of the brain controls visual organization, perception, and attention. It is
also responsible for non-verbal communication, ability to perceive space, understand where we
are, what we are doing, and why various objects are placed where they are. If an individual
suffers from a CVA occurrence in the brain's right side of the brain, the left side of the face and
body could produce any or all of the following: Paralysis on the left side of the body, difficulty in
performing daily tasks, perception difficulties, neglect of left side, visual impairment, excessive
talking, short attention span, poor judgment, time disorientation, loss of left visual field,
Impaired abstract thinking, extreme emotional highs and lows, lethargy, and impulsiveness
(Senelick, Rossi, & Dougherty, p. 67).
The left hemisphere of the brain controls language skills. If the CVA occurs in the left side of
the brain, the right side of the face and body could produce any or all of the following: Paralysis
on the right side of the body, partial or complete loss of speaking or understanding language
due to aphasia or dysarthria, confusion between left and right, loss of visual field on the right,
decreased memory, slowness, and depression (Senelick, Rossi, & Dougherty, p. 77).
Not every CVA is found in the right or left hemisphere of the brain. Although most CVA
episodes happen in the right or left, there are less common occurrences of CVA that are
localized in the brain stem or in the cerebellum. These CVA occurrences may affect
movement, balance, and basic body functions, such as swallowing and breathing (Senelick,
Rossi, & Dougherty, p. 64). Of course not every symptom is manifested in every person who
suffers a CVA. Nor are every persons symptoms the same. In spite of this, when a CVA strikes
a specific area, there are enough similarities to make pinpointing the location a help in
diagnosis and, ultimately, in the rehabilitation outcome.
Epidemiology of CVA:
Every 45 seconds someone in America experiences a CVA episode, while every three
minutes, someone dies from CVA (American Stroke Association: Impact of Stroke, 2004). It is
the third leading cause of death in the United States, ranking behind diseases of the heart and
all forms of cancer. It is also the leading cause of serious, long-term disability in adults. About
700,000 CVA incidents are reported in the U.S. each year. 500,000 of them are new attacks
while 200,000 are recurrent (Internet Stroke Center, 2004). Today, there are about 4.8 million
CVA survivors in the U.S. (American Stroke Association: Impact of Stroke, 2004).
Based on medical statistics and research, the most common risk factors that most frequently
cause CVA include hypertension, diabetes, smoking, carotid or other artery diseases, certain
blood disorders such as sickle cell disease, heart diseases such as atrial fibrillation, high blood
cholesterol, physical inactivity, obesity, and excessive alcohol and drug use. For the most part,
some of these are factors result from lifestyle choices which can be appropriately changed to
reduce the risk of CVA. Factors which are not controlled by lifestyle choices include increasing
age, sex, and heredity or family history. Most who suffer CVA are over the age of sixty-five
(Burkman, p.105). Out of every 5 deaths from CVA, 2 are men while 3 are women (American
Stroke Association: Stroke Facts 2004) and for those who have a family member who suffered
from CVA, their chances of getting CVA increases. The risk also increases for those who had a
previous episode of CVA to experience a recurrent one (American Stroke Association: Impact
of Stroke, 2004).
As the third leading cause of death in the United States, CVA kills nearly 164,000 people each
year (American Stroke Association: Stroke Facts, 2004). An individual who experiences CVA
loses thousands of dollars in revenue per year. It costs the healthcare system thousands of
dollars to care for each individual CVA patient. For the families of CVA patients, the loss of
revenue is even more overwhelming. Each year, several billion dollars in revenue is lost as a
result of families having to change their lifestyles in order to care for a family member who has
suffered from CVA (Harris, 2002).
Psychosocial Aspects of CVA:
For patients of CVA, the quality of life is never really the same as it was before the stroke
episode. Their lives are changed drastically and the methods they use to cope with the change
can either make or break their rehabilitation. According to one study, although many CVA
survivors eventually gained back 76 percent of their past physical functioning skills, they were
only able to regain 33 percent of their past social functioning skills (Senelick, Rossi, &
Dougherty, p. 173).
After a CVA, both the CVA survivor and the family often are uneasy about being on their own
at home. They have many apprehensions and anxieties for what the future holds. They fear
that another CVA incident might happen again. They worry that the CVA survivor may be
unable to accept the disabilities or that the survivor might be placed in a nursing home. They
have concerns that the caregiver may not be prepared to face the responsibility of caring for
the CVA survivor. There are also fears that friends and family will abandon the CVA survivor
(National Stroke Association 2002).
It is very difficult for many CVA patients to come to terms with the change in their abilities and
personal appearance. Their intellect is lowered. They can no longer go to the bathroom by
themselves. They have problems controlling their bladder and bowel movements. They have
difficulty swallowing foods and have trouble speaking due to slurred speech. They also face
sexual dysfunction which leads to feelings of inadequacy (Senelick, Rossi, & Dougherty, p.
181). Because of the devastating change and sudden loss of skills that were once second
nature to them, the quality of life for survivors of CVA is severely deteriorated. They constantly
feel tired and lose interest in hobbies and activities they once enjoyed.
The major emotional impact that CVA has on a person can also cause them to cry easily, often
for no apparent reason. It could be the sight of a grandchild or even something on the TV such
as the news for example. Slightly less common is uncontrollable laughter. Either way, these
displays of exaggerated emotions appear as if the CVA patient has a lower emotional threshold
than normal, in which almost anything can trigger an amplified emotional response (Tanner, p.
80). This is possibly due to damage to the parts of the brain that control emotions, which can
lead to personality changes. When the ability to control emotions is lost, patients may display
emotionally extreme behaviors. Naturally, this together with certain physical disabilities and
communication difficulties can lead to irritability, anxiety, frustration, and sometimes deep
sadness. A typical manifestation seen with CVA survivors is depression. They suffer from
intense feelings of hopelessness and helplessness (Burkman, p. 25).
It is important to remember that the inability to button a blouse or the inability to use a fork and
knife does not mean low intelligence. It is simply a loss of function. Unfortunately, the loss of
function is often associated with low intelligence. Society tends to falsely depreciate the value
of those who are not physically whole. Thus, it is common for CVA survivors to experience
feelings of guilt and worthlessness, shame, significant reduction in self-esteem and self-value,
and an unwillingness to be seen by others (Tanner, p.121-127). However, humans are social
beings and the sooner a CVA patient starts to socialize, the faster they will start to recover.
This is the most crucial time where the husband or wife, family, and friends are so important in
assuring the patient that he or she is still loved and wanted, and that there are those who care
and want to help. Some friends and family members may start to grow distant either because
they do not know how to cope or they no longer have any mutual interest. The best solution in
this case is simply to move on and form new friends (Buckman, p. 52-53).
For the survivors, family members, friends, and caregivers, everyone is affected by CVA both
directly and indirectly, and the impact can be devastating. It causes a great deal of anxiety for
everyone involved with the CVA survivor. The financial impacts also play an important role in
regards to the level of care available and affordable for the CVA patient. For patients who were
previously responsible for looking after the familys finances, the problem is even more
detrimental. If the patients were previously employed, they must face the possible reality that
their jobs are at risk. They must ask themselves how long it will be before they can get back to
work again, or if they will even have a job to go back to (Buckman, p. 66).
There are many issues that family members must consider in regards to their employment
while caring for the CVA patient. They must ask themselves whether or not they can take a
prolonged leave of absence or if they must completely give up their jobs. On the other hand, do
their jobs pay well sufficiently or do they have insurance that can allow them to hire a full time
care-giver? Depending on the degree of disability on the CVA patient, the family member
looking after the patient may or may not be able to take over the care-giving by the time they
get back home from work. The demands of full-time work and overnight care-giving may take a
huge toll on them (Buckman, p. 66).
Economic Impacts of CVA:
CVA is an expensive problem. On the national scale, the direct and indirect costs of CVA in the
United States are estimated at $53.6 billion a year (American Stroke Association: Stroke Facts
2004). In a population study of stroke costs within 30 days of an acute event, the average cost
for mild ischemic strokes was $13,019 and $20,346 for severe ischemic strokes (American
Heart Association: Heart Disease and Stroke Statistics, 2004). These figures should not come
as a surprise when taking into the consideration the affect that CVA has on the grand scale.
This is a condition that leaves many patients with disabilities that prohibit them from resuming
their previous lifestyle or employment. Plus, the financial cost for the care, diagnosis, and
treatment of CVA patients at home and in hospitals is quite alarming.
The cost of cardiovascular diseases and stroke in the United States in 2004 is estimated at
$368.4 billion. This figure comprise health expenditures which include the cost of physicians
and other professionals, hospital and nursing home services, the cost of medications, home
health care and other medical durables; plus the lost productivity resulting from morbidity and
mortality. By comparison, in 2003 the estimated cost of all cancers was $189 billion. That is
$64 billion in direct costs, $16 billion in morbidity indirect costs and $109 billion in mortality
indirect costs). In 1999 the estimated cost of HIV infections was $28.9 billion. That is $13.4
billion in direct costs and $15.5 billion in indirect costs (American Heart Association 2004). This
makes the social and economic impact of CVA one of the most devastating in medicine.
Impacts of CVA on the Medical System:
Like any other severe disease, CVA is a major problem and has serious impacts on the
medical system. Consequently, todays technological advancements in medicine have enabled
physicians to utilize more sophisticated methods of evaluation for early diagnosis. Initially, the
physician will promptly review the patients medical history and run a computed tomography
(CT) scan. The CT scan allows the physician to determine if the cerebrovascular disease is a
cerebral hemorrhage or a transient ischemic attack. It also helps to determine the best course
of action for treatment and provides the location of where the damage is (Petrossian, 2001).
Other technological instruments physicians use for diagnosing CVA include:
Carotid ultrasound: used to detect the presence of plaque.
Magnetic resonance angiography (MRA): used to assess the degree of blockage in the
carotid arteries. The MRA is a variation of the magnetic resonance imaging (MRI) scan,
which is also very important in diagnosing CVA.
Electrocardiogram (EKG): used to identify any cardiac problems that may have led to the
CVA, such as a prior heart attack (Petrossian, 2001).
Tests used to assess overall brain function include:
Electroencephalogram (EEG): uses small metal devices (electrodes) that are attached to
the scalp. The electrodes are connected by wires to an electroencephalograph machine
that charts the electrical activity of the brain.
Evoked-potential study: used to test and measure the brains response to sight, hearing
and touch.
In the aspects of CVA treatment, the future looks bright. Scientists are continuously exploring
new methods of treating CVA and preventing recurrent cases of CVA. Current research is
ongoing in several areas. Studies are being done on additional drugs that dissolve clots. These
drugs are administered either in the veins or directly into the clogged artery. The goal of these
studies is to determine which CVA patients might benefit from this new and aggressive form of
treatment (MedicineNet.com, 2002). New medications are also being tested that help slow the
degeneration of the nerve cells that are deprived of oxygen during a CVA episode. These
drugs are referred to as "neuroprotective" agents. These agents attempt to rescue brain cells
from injury caused by an ischemic stroke. Some agents attempt to increase the flow of blood to
the region of brain experiencing CVA. Other agents may prevent damage caused by blood
returning to the affected area of the brain. One example of a neuroprotective agent is
sipatrigine. Another example is chlormethiazole, which works by modifying the expression of
genes within the brain (Petrossian, 2001).
Studies have found that atherosclerotic plaque can harbor bacteria, which, in turn, may
increase the tendency for plaquerupture. Researchers are investigating whether antibiotics,
specifically penicillin, can exert any effects against such bacteria. This would lead to an
increase in the stability of the plaque and reduce the risk of it breaking off and causing a CVA
(Petrossian, 2001).
Mechanical thrombolysis is also being investigated in its use to treat CVA. It involves devices
that use catheter-delivered tools to break up or remove blood clots. Currently, clot-busting
drugs are currently the only method available to break up an existing blood clot in the brain.
However, they can take up to an hour to be effective. Devices currently being tested use
lasers, sound waves, suction, spinning blades and snares to remove clots (Petrossian, 2001).
Some evidence suggests that transcranial magnetic stimulation or TMS, in which a small
magnetic current is delivered to an area of the brain, may possibly increase brain plasticity and
speed up recover of function after CVA (Pharma-Help, 2003).
Another concept that scientists are exploring is hypothermia or cool therapy. Researchers are
currently studying whether lowering a patients body temperature can decrease the amount of
damage that occurs during a severe CVA. Interesteingly enough, one study found that lowering
a person's body temperature by about one degree within a few hours of a CVA can significantly
reduce brain damage and risk of death (Rogers, 2003).
Finally, stem cells, which have the potential to develop into a variety of different organs, are
being used in attempts to replace brain cells damaged by a previous CVA. Stem cells are basic
cells that have the ability to develop into many different types of cells. They start out very
similar to each other, but depending on where they develop, the cells become highly
specialized to their individual functions. Researchers are investigating a variety of methods in
which stem cell transplants could be used as a treatment for CVA damage and other conditions
involving damaged brain cells (MedicineNet.com, 2002). In many academic medical centers,
some of these experimental agents are offered in the setting of a clinical trial.
While new therapies for the treatment of patients after CVA are on the horizon, they are not yet
perfect and may not restore complete function to a CVA patient. More investigation is needed
to determine the safety and effectiveness of these potential treatments, and to determine the
best method of administering these treatments to patients.
Recovery & Rehabilitation:
In the first twenty-four hours, recovery is much faster following a CVA when immediate damage
to the brain is repaired. Unfortunately, after the twenty-four hours the rate of recovery begins to
slow down dramatically, becoming less rapid afterwards. There is usually further improvement
over time, but not at the same pace as before. It is important to understand this process and
not get disheartened as recovery apparently slows down. Recovery from CVA depends on the
extent and location of the brain injury, the person's general health, his or her personality and
emotional state, the support and cooperation of family and friends, and the care the person
receives.
With neurological recovery, it is difficult to determine with precision how long the recovery
process will take because of the uncertainty of how much neurological damage might have
resulted from the CVA. There is still a great deal that remains to be a mystery in regards to
how the brain compensates for the damage caused by CVA. Some brain cells may be only
temporarily damaged, not killed, and may resume functioning. In some cases, the brain can
reorganize its own functioning. Sometimes, a region of the brain "takes over" for a region
damaged by the CVA (National Stroke Association, 2004). In this process, undamaged brain
tissue assumes some of the functions of the dead tissue. The potential of these living nerves is
unveiled to help with recovery. Another process also used by nerves in healing is what could
be referred to as sprouting. When nerve connection is lost, nerve cells may send out new
signals in search of new connections. Still, some connections may not be able to reestablish
old ones if large portions of the brain are damaged or in the old nerve pathways are trapped in
scar tissue (Burkman, p. 73).
In the case of functional recovery, it is affected by both neurological recovery and rehabilitation.
Rehabilitation actually starts in the hospital as soon as possible after the CVA. In patients who
are stable, rehabilitation may begin within two days after the CVA has occurred, and should be
continued as necessary after release from the hospital. Although some people recover from a
CVA spontaneously, most people need rehabilitation to relearn previous skills and learn new
skills (Burkman, p. 79). The goal of rehabilitation is to help the person who has suffered from
CVA make the most of his or her physical and mental capabilities while adapting to any
limitations resulting from the CVA. This must be accomplished in a way that preserves dignity
and promotes motivation in the patient.
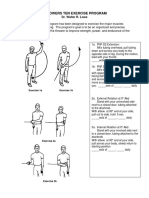
Rehabilitation consists of physical therapy, occupational therapy, and speech and language
pathology. For the CVA patient, the physical therapist's aim is to get back as much movement
as possible by means of a range of exercises, and to prevent complications arising as a result
of the way in which limbs are positioned. Occupational therapists, on the other hand, are
concerned with helping individuals to achieve as much independence as possible. They help
the patient find ways to do again what used to be the simplest of things from everyday tasks
like brushing teeth to taking up new leisure activities as well as rediscovering old ones
(Burkman, p.83). Finally, with speech and language therapists they understand how CVA often
leaves people with communication difficulties and problems with swallowing. That is why
speech and language therapists assess the problems, work with the patient on the best ways
to overcome them and improve communication skills (Burkman, p. 84).
Reducing the Risk of CVA:
Preventive measures achieved by adopting a healthier lifestyle are the best way to reduce the
risks of CVA and promote better circulation of blood flow to the brain. Although preventive
measures may not fully protect an individual against having a CVA, they can still go far to
reduce the risks of such an event. Many of the preventive measures involve lifestyle changes
that are similar to those that can help prevent heart disease. One of the lifestyle measures
includes controlling high blood pressure or hypertension. Blood pressure abnormalities must be
continually monitored and controlled because they are a chief contributor to CVA. Getting
treatment for atrial fibrillation or atrial flutter is another preventive measure. Irregular heart
beats can affect heart function and allow blood to collect in the chambers of your heart. The
blood which collects there can clot and most likely lead to CVA. Additionally, reducing
cholesterol levels, perhaps by taking cholesterol-reducing drugs also helps. Periodic blood
cholesterol tests can help monitor the risk of artherosclerosis.
Other preventive measures that should be considered as well are increasing ones level of
exercise, maintaining an ideal weight, refraining from or quitting smoking, limit use of alcohol to
about one glass of wine or one beer per day, which may help in the prevention of strokes, and
controlling diabetes (Wiebers, p. 90). These small changes can greatly reduce the risks of CVA
and decrease its damages making them less severe.
Personal Reflections on CVA:
The team of health care professionals including nurses, physical therapists, occupational
therapists, and speech and language therapists are there to devise a program designed for the
needs of the CVA survivor. They are there every step of the way to help them cope and start to
learn new ways of carrying out everyday tasks. However, there is no doubt that the
determination of the person who has experienced the CVA episode, along with a positive
attitude, plays a great part in their recovery, though of course they will have help from their
caregiver, family, friends and health care professionals.
After the initial shock of a CVA comes adjustment. He or she is going to face many new
challenges, and a positive outlook certainly helps. The best approach is to take each day as it
comes, and live it to the fullest extent possible. Setting small achievable goals can help. For
example, relearning to do something as simple as tying a shoelace can be the first step to a
greater goal such as learning how to drive. Independence is the ultimate aim and self-
sufficiency brings enormous rewards. Nevertheless, what is equally important is to be realistic.
The extent and rate of recovery from CVA is different for everyone and learning new ways to
cope is tiring both physically and mentally. The best way to handle it is to do things at a
comfortable pace, take adequate amounts of rest, and to keep a regular routine.
People who have had CVA say that no matter how much they improve, they always feel the
stroke with them. As the months progress they begin to learn just how much recovery is
possible, and how to get the most out of life within those restrictions. Someone who has just
been stricken with CVA is entering a new phase of life. With a positive attitude it is possible for
them and for their loved ones to face the challenges and go on to live fully satisfying lives.
References
American Heart Association (2004). Heart Disease and Stroke Statistics 2004 Update.
Retrieved on April 8, 2004 from
website:http://www.americanheart.org/downloadable/heart/1075102824882HDSStats2004Upd
ateREV1-23-04.pdf
American Stroke Association (2004). Impact of Stroke. Retrieved on April 8, 2004 from
website: http://www.strokeassociation.org/presenter.jhtml?identifier=1033
American Stroke Association (2004). Stroke Risk Factors. Retrieved on April 8, 2004 from
website: http://www.strokeassociation.org/presenter.jhtml?identifier=4716
American Stroke Association (2004). Stroke Facts 2004: All Americans. Retrieved on April 8,
2004 from
website:http://www.americanheart.org/downloadable/heart/1073974411867Stroke%20Facts%2
02004.pdf
Buckman, R. (2000). What You Really Need to Know About Caring for Someone After a
Stroke. New York: Lebhar-Friedman Books.
Burkman, K. (1998, May). The Stroke Recovery Book. Independent Publishers Group.
Cicala, R. S. (1999). The Brain Disorders Sourcebook. Los Angeles: Lowell House.
Cleveland Clinic Health System (2003). Understanding Stroke. Retrieved on April 8, 2004 from
website: http://www.cchs.net/health/health-info/docs/0900/0992.asp?index=5601
Senelick, R. C., Rossi, P. W., & Dougherty, K. (1999, June 1). Living with Stroke: A Guide For
Families: Help and New Hope for All Those Touched by Stroke (1
st
ed.). New York: McGraw-
Hill.
Harris, J. T. (2002). Epidemiology of Stroke. Retrieved on April 8, 2004 from
website: http://www.hcstrokefoundation.org/epidemiology.html
Internet Stroke Center (2003). Stroke Statistics. Retrieved on April 8, 2004 from
website: http://www.strokecenter.org/pat/stats.htm
McMurdo, M. (2003). Stroke (Cerebrovascular accident). Retrieved on April 8, 2004 from
website: http://www.netdoctor.co.uk/diseases/facts/stroke.htm
MedicineNet.com (2002, April 15). Stroke. Retrieved on April 8, 2004 from
website:http://www.medicinenet.com/script/main/art.asp?articlekey=489&pf=3&track=qpa489
National Stroke Association (2002). Life After Stroke: Survivor and Caregiver. Retrieved on
April 8, 2004 from
website:http://209.107.44.93/NationalStroke/HadAStroke/Life+After+Stroke+-
+Survivor+and+Caregiver.htm
Petrossian, G. A. (eds.) (2001, May 14). Stroke. Retrieved on April 8, 2004 from
website: http://www.heartcenteronline.com/Stroke.html
Pharma-Help.com (2003). Cerebrovascular Accident. Retrieved on April 8, 2004 from
website: http://pharma-help.com/cerebrovascular-accident
Rodgers, E. (2003, May 30). Stroke (Cerebrovascular accident). Retrieved on April 8, 2004
from website:http://www.peacehealth.org/kbase/topic/major/hw224638/descrip.htm
Вам также может понравиться
- Ten Personality Disorders - Neel Burton MDДокумент11 страницTen Personality Disorders - Neel Burton MDcgarciОценок пока нет
- ProfJutte Lowpotencies PDFДокумент6 страницProfJutte Lowpotencies PDFcgarciОценок пока нет
- Asafoetida AsafДокумент49 страницAsafoetida AsafcgarciОценок пока нет
- Natrum Mur FarringtonДокумент16 страницNatrum Mur FarringtoncgarciОценок пока нет
- Relationship of Remedies DR Rgibson Miller PDFДокумент9 страницRelationship of Remedies DR Rgibson Miller PDFcgarci100% (3)
- Arsenicum Alb - Holistic LookДокумент3 страницыArsenicum Alb - Holistic LookcgarciОценок пока нет
- Immune SuppressionДокумент1 страницаImmune SuppressioncgarciОценок пока нет
- Cerebral ParesisCase Berridge.Документ3 страницыCerebral ParesisCase Berridge.cgarciОценок пока нет
- Plant Kingdom EssentHomoeopДокумент40 страницPlant Kingdom EssentHomoeopcgarciОценок пока нет
- Gwillim, Linda & Biggs, Kathy - Placenta HumanumДокумент90 страницGwillim, Linda & Biggs, Kathy - Placenta HumanumLeonard MichlinОценок пока нет
- Matridonal Remedies LGraystonДокумент9 страницMatridonal Remedies LGraystonaruen79100% (1)
- Endocrino and HomeopathyДокумент24 страницыEndocrino and HomeopathycgarciОценок пока нет
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceОт EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceРейтинг: 4 из 5 звезд4/5 (895)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeОт EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeРейтинг: 4 из 5 звезд4/5 (5794)
- The Yellow House: A Memoir (2019 National Book Award Winner)От EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Рейтинг: 4 из 5 звезд4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingОт EverandThe Little Book of Hygge: Danish Secrets to Happy LivingРейтинг: 3.5 из 5 звезд3.5/5 (400)
- Never Split the Difference: Negotiating As If Your Life Depended On ItОт EverandNever Split the Difference: Negotiating As If Your Life Depended On ItРейтинг: 4.5 из 5 звезд4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureОт EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureРейтинг: 4.5 из 5 звезд4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryОт EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryРейтинг: 3.5 из 5 звезд3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerОт EverandThe Emperor of All Maladies: A Biography of CancerРейтинг: 4.5 из 5 звезд4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaОт EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaРейтинг: 4.5 из 5 звезд4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersОт EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersРейтинг: 4.5 из 5 звезд4.5/5 (345)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyОт EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyРейтинг: 3.5 из 5 звезд3.5/5 (2259)
- Team of Rivals: The Political Genius of Abraham LincolnОт EverandTeam of Rivals: The Political Genius of Abraham LincolnРейтинг: 4.5 из 5 звезд4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaОт EverandThe Unwinding: An Inner History of the New AmericaРейтинг: 4 из 5 звезд4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreОт EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreРейтинг: 4 из 5 звезд4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)От EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Рейтинг: 4.5 из 5 звезд4.5/5 (121)
- Pidato Bahasa Inggris NurulДокумент2 страницыPidato Bahasa Inggris NurulAna Defita SariОценок пока нет
- Synthesis of DHA Rich PUFA From Cod Liver Fish OilДокумент7 страницSynthesis of DHA Rich PUFA From Cod Liver Fish OilS Bharadwaj ReddyОценок пока нет
- Tnation CardioДокумент8 страницTnation Cardiojegreen3Оценок пока нет
- Additional Activity: Fitness Self-Assessment: Masbate National Comprehensive High SchoolДокумент2 страницыAdditional Activity: Fitness Self-Assessment: Masbate National Comprehensive High SchoolEmerich VelascoОценок пока нет
- Dose Ordered Dose Available X Volume Available: O Calculate Rate Using MinutesДокумент27 страницDose Ordered Dose Available X Volume Available: O Calculate Rate Using Minutesmaryhiromi10Оценок пока нет
- Muscle Maximum Growth IIДокумент116 страницMuscle Maximum Growth IIAlex Antoniou88% (16)
- Sarcopenia and Osteoporosis-Terkunci PDFДокумент33 страницыSarcopenia and Osteoporosis-Terkunci PDFNur AisyahОценок пока нет
- Basic Life Support CPRДокумент38 страницBasic Life Support CPRSamsonОценок пока нет
- Harrymodule 2 Lesson 2 PECHДокумент17 страницHarrymodule 2 Lesson 2 PECHHarvs MonforteОценок пока нет
- case study حنانДокумент35 страницcase study حنانMera Abo ElhassanОценок пока нет
- Pe 1. LectureДокумент6 страницPe 1. LectureJopieОценок пока нет
- Tropical PancreatitisДокумент26 страницTropical PancreatitisHarsha VardhanОценок пока нет
- DR Physique Lean Bulking Series II 2015Документ121 страницаDR Physique Lean Bulking Series II 2015Vlad Alexandru50% (2)
- LP 1throwers - Ten - Exercises - 2010 PDFДокумент5 страницLP 1throwers - Ten - Exercises - 2010 PDFClaudiaОценок пока нет
- Name: Reycel Ann L. Ilawan Section: F Reference: Puhl, R., Rubino, F., Cummings, D., Eckel, R., & Ryan, D. (2020) - Joint InternationalДокумент3 страницыName: Reycel Ann L. Ilawan Section: F Reference: Puhl, R., Rubino, F., Cummings, D., Eckel, R., & Ryan, D. (2020) - Joint InternationalReycel IlawanОценок пока нет
- Case Questions: I. Understanding The Disease and PathophysiologyДокумент8 страницCase Questions: I. Understanding The Disease and Pathophysiologyapi-532124328Оценок пока нет
- 5 Altered Nutrition Less Than Body Requirements Chronic Renal Failure Nursing Care PlansДокумент3 страницы5 Altered Nutrition Less Than Body Requirements Chronic Renal Failure Nursing Care Plansjustin_sane40% (5)
- Faculty of Medicine: Kafr El-Sheikh UniversityДокумент11 страницFaculty of Medicine: Kafr El-Sheikh UniversityjayОценок пока нет
- Basic Strenght StandardsДокумент6 страницBasic Strenght StandardsЂорђеОценок пока нет
- Bodyweight Chaos FinishersДокумент22 страницыBodyweight Chaos FinishersBoonyarit SikhonwitОценок пока нет
- PCOSДокумент15 страницPCOSAndyan Adlu PrasetyajiОценок пока нет
- Grant ProposalДокумент6 страницGrant Proposalapi-280793093100% (1)
- Diabetic BookДокумент317 страницDiabetic BookRajanbabuОценок пока нет
- Terry 24th March Part 2Документ3 страницыTerry 24th March Part 2mr_singapore2010Оценок пока нет
- Analysis: Dietary and Nutritional Approaches For Prevention and Management of Type 2 DiabetesДокумент9 страницAnalysis: Dietary and Nutritional Approaches For Prevention and Management of Type 2 DiabetesMr. LОценок пока нет
- Protein Requirements and Supplementation in Strength Sports: Nutrition July 2004Документ8 страницProtein Requirements and Supplementation in Strength Sports: Nutrition July 2004Andrei ChirilaОценок пока нет
- AtorvastatinДокумент2 страницыAtorvastatinKasandra Dawn Moquia BerisoОценок пока нет
- Nutrition Perspectives Research Paper Tyler LundquistДокумент6 страницNutrition Perspectives Research Paper Tyler Lundquistapi-489129243Оценок пока нет
- FAQ Always HungryДокумент17 страницFAQ Always HungryRadu DiaconuОценок пока нет
- Made To Crave Devotional: 60 Days To Craving God, Not Food by Lysa TerKeurstДокумент24 страницыMade To Crave Devotional: 60 Days To Craving God, Not Food by Lysa TerKeurstZondervan78% (9)