Академический Документы
Профессиональный Документы
Культура Документы
Surgical Intensive Care
Загружено:
lizzy5960 оценок0% нашли этот документ полезным (0 голосов)
103 просмотров95 страницReview of the SICU
Авторское право
© © All Rights Reserved
Доступные форматы
PDF, TXT или читайте онлайн в Scribd
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документReview of the SICU
Авторское право:
© All Rights Reserved
Доступные форматы
Скачайте в формате PDF, TXT или читайте онлайн в Scribd
0 оценок0% нашли этот документ полезным (0 голосов)
103 просмотров95 страницSurgical Intensive Care
Загружено:
lizzy596Review of the SICU
Авторское право:
© All Rights Reserved
Доступные форматы
Скачайте в формате PDF, TXT или читайте онлайн в Scribd
Вы находитесь на странице: 1из 95
1
Surgical Intensive Care
JUNYI LI, MD
Board certified in Anesthesiology
Board certified in Critical Care Medicine
Board certified in Transesophageal
Echocardiography
lijunyiutmb@yahoo.com
March 31, 2009
2
Subspecialty ICU
Medical Intensive Care Unit (MICU)
Coronary Care Unit (CCU)
Surgical I ntensive Care Unit (SI CU)
Neurological Intensive Care Unit (NICU)
Cardiovascular Intensive Care Unit (CVICU)
Pediatric Intensive Care Unit (PICU)
Neonatal Intensive Care Unit (NICU)
3
SICU Admission Criteria
Preoperative status
Major trauma
Surgical Procedure
Pts preexisting disease
Intraoperative event
Large volume shift
Unexpected surgical complication
Unexpected anesthesia complication
Postoperative status
Unexpected postop complication
Pts status
4
SICU Management
Respiratory care
Hemodynamic monitoring and management
Noninvasive
Invasive
Infection in SICU
Acid-base disorders
Fluid and electrolyte disorders
Blood component therapy
Nutrition support
5
Who need to be admitted to SICU ?
18 y/o health male presented for right inguinal hernia repair
under spinal anesthesia and uneventful intraop and postop.
50 y/o female with controlled HTN and DM for lumbar
laminectomy under general anesthesia with EBL 500 ml.
75 y/o male with stable angina, COPD required home oxygen
for TURP under spinal anesthesia
60 y/o male presented for AAA repair
54 y/o female with esophageal cancer presented for
esophagectomy
95 y/o female presented for right hip arthroplasty
6
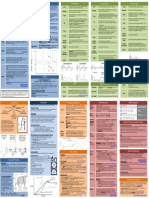
Respiratory care basic monitor
Respiratory rate
Chest movement
Breath sound
Color
7
Respiratory care lung volume
Tidal volume (VT)
Minute ventilation (Vm)
Functional residual capacity (FRC)
Vital capacity (VC)
8
Respiratory care - ventilation
Ventilation-perfusion (V/Q) ratio:
normal V/Q=4L/5L=0.8
Dead space ventilation: V/Q>1
anatomic dead space & physiologic dead space
Intrapulmonary shunt: V/Q<0.8
true shunt (V/Q=0) and venous admixture
9
V/Q relationship and associated blood gas
10
Effect of shunt fraction on PAO2
11
Effect of shunt fraction on PAO2 and PACO2
12
Ventilation-perfusion
Quantitative determinations
Dead space (Vd/Vt) = (PACO2 PECO2)/PACO2
Shunt fraction (Qs/Qt) =
(CCO2 CAO2)/(CCO2 CVO2)
A-a gradient (PAO2 PaO2)
PAO2 = PIO2 (Paco2/RQ)
PAO2 = FIO2(PB PH2O) (PaCO2/RQ)
PAO2 = 0.21(760 47) (40 /0.8) = 100 mmHg
PAO2/FIO2<200, Qs/Qt>20%
PAO2/FIO2>200, Qs/Qt<20%
13
Hypoxemia
Disorder A-a PO2 PVO2
Hypoventilation Normal Normal
Pulmonary disorder Increased Normal
DO2/VO2 imbalance Increased Decreased
DO2/VO2 oxygen deliver and uptake ratio
A-a PO2 PO2 difference between alveolar gas and arterial blood
PVO2 Mixed venous PO2
14
Evaluation of hypoxemia
15
Hypercapnia
Hypercapnia is PACO2>45 mm Hg, due to
Increased CO2 production
Hypoventilation
Increased dead space ventilation
16
Evaluation of hypercapnia
High
17
Oximetry
Oximetry detects arterial blood HbO2 and Hb
ratio
Ear oximetry
Pulse oximetry
Co-Oximeters can detect Met Hb and CO Hb
Mixed venous oximetry measured O2 sat in PA
blood
18
CO2 detector and capnometry
CO2 detector is a method for determining the
success or failure of ET intubation.
Clinical application of capnometry in ICU:
- Cardiac output monitor
- Ventilator-related mishap detection
- Early detection of nosocomial disorders
- Ventilator weaning
- Controlled hyperventilation
19
Acute respiratory distress syndrome
(ARDS)
A leading cause of acute respiratory failure
with high mortality
A diffuse inflammatory injury in the lung
Not an accumulation of watery edema fluid
Not a primary disease, but a complication
20
Common conditions that predispose to ARDS
21
ARDS microscopic changes and CXR
22
Diagnostic criteria for ALI and ARDS
Acute onset
Presence of predisposing condition
PaO2/FiO2 < 200 mm Hg for ARDS,
< 300 mm Hg for ALI
CXR bilateral infiltrates
PAOP < 18 mm Hg or no clinical evidence of
high LA pressure
23
Management of ARDS
No real treatment for ARDS, only supportive
Mechanical ventilation:
low-volume ventilation
permissive hypercapnia
positive end-expiratory pressure
Fluid management reducing extravascular
lung water
Pharmacotherapy uncertain effect
24
Respiratory therapy
Oxygen inhalation therapy
Chest physical therapy
Respiratory pharmacotherapy
Mechanical ventilation
25
Oxygen inhalation therapy
Arterial hypoxemia:
PaO2 < 60 mm Hg (SaO2 < 90 %)
Tissue hypoxia:
blood lactate > 4 mmHg
Endpoint of O2 therapy is tissue oxygenation
Tissue hypoxia may not consistent with arterial
hypoxemia
26
Effect of Oxygen on blood flow
Oxygen tends to reduce systemic blood flow
due to:
1. vasoconstrction in all vascular bed except
the pulmonary circulation
2. decrease in cardiac output
3. negative inotropic effect
27
Method of oxygen inhalation
Low-flow oxygen delivery system with
variable FiO2
High-flow oxygen delivery system with
constant FiO2
28
Device Reservoir Oxygen flow FiO2
capacity (L/min)
Nasal cannula 50 ml 1 0.21-0.24
2 0.24-0.28
3 0.28-0.34
4 0.34-0.38
5 0.38-0.42
6 0.42-0.46
Oxygen face mask 150-250 ml 5-10 0.40-0.60
Mask-reservoir bag 750-1250 ml
Partial rebreather 5-7 0.35-0.75
Nonrebreather 5-10 0.40-1.0
Low-flow oxygen delivery systems
FiO2 = 20 + 4 X oxygen flow (L/ml)
29
Respiratory pharmacotherapy
Bronchodilators
Corticosteroids
Mucokinetic therapy
30
Mechanical Ventilation
31
Mechanical ventilation
Mechanical ventilation is positive pressure
ventilation
Indications of mechanical ventilation
Rate
ABG: hypoxia and hypercapnia
Mechanical parameter: MV, VC and NIP
Dead space and shunt
Contraindication of mechanical ventilation
32
Normal lung
Noncompliant lung
Effect of positive pressure ventilation
33
Effect of positive pressure ventilation
34
Respiratory parameter
Rate: 10 20/min
VT: 6 10/kg
FiO2: 40 100%
PEEP: 5 10 cm H2O
PS: 5 10 cm H2O
I:E ratio: 1:2
35
Patterns of mechanical ventilation
Control mode ventilation
Assist-control ventilation
36
Pattern of mechanical ventilation
Volume-controlled ventilation
ACV (assist control ventilation)
IMV (intermittent mandatory ventilation)
SIMV (synchronized IMV)
Pressure-controlled ventilation
Pressure support ventilation
Special pattern:
37
Functional mode of ventilator
PEEP (positive end expiratory pressure)
PS (pressure support)
I:E reversal ratio
38
Ventilatory mode of mechanical ventilation
39
Volume-controlled ventilation
40
Pressure-controlled & Pressure support
41
PEEP and CPAP
42
Effect of PEEP on arterial oxygenation and CI
43
Discontinuing mechanical ventilation
Ventilator required for brainstem respiratory
depression (e.g.,GA in OR or drug overdose) is
easy to discontinue
Ventilator required for cardiopulmonary
insufficiency is weaning in gradual process
44
Discontinuing mechanical ventilation
Clinical evaluation:
Awake
Spontaneous breathing
Ability of airway protection
Stable hemodynamics
45
Discontinuing mechanical ventilation
Sequence of weaning:
FiO2 to 50% or less
PEEP to 5 cm H2O or less
PS to 10 cm H2O or less
46
Discontinuing mechanical ventilation
Bedside weaning parameters:
Parameter Normal range Threshold for weaning
PaO2/FiO2 >400 200
VT 5-7 ml/kg 5 ml/kg
Rate 10-20/min <40/min
VC 65-75 ml/kg 10 ml/kg
VE 5-7 L/min <10 L/min
Pi max >-90 cm H2O (F) -24 cm H2O
>-120 cm H2O (M)
Rate/VT <50/min/L <100/min/L
47
Predictive value of selected weaning parameters
48
Discontinuing mechanical ventilation
Methods of weaning:
T-piece weaning
IMV weaning
CPAP weaning
49
Diagram of T-shaped circuit
50
Hemodynamic monitoring
Noninvasive
ECG: heart rate, rhythm, ischemia (ST-T)
Noninvasive BP
Echocardiography: TTE, TEE, color-doppler
Contractility
Volume status
EF
Ischemia (RWMA)
Noninvasive cardiac output (through A-line)
51
Hemodynamic monitoring
Invasive
Arterial blood pressure
Central venous pressure
Pulmonary artery catheter and wedge pressure
Cardiac output
52
Invasive arterial blood pressure
Major CV surgery
Surgery with great hemodynamic change
Surgery with large volume shift and bleeding
Shock and other critical ill patients
Surgery requiring hemodilution and control
hypotension
Frequent ABG
Indication
53
Invasive arterial blood pressure
Contraindication:
only relative contraindication except for
puncture site infection
54
Invasive arterial blood pressure
Selection of artery for cannulation
Radial artery
Ulnar artery
Brachial artery
Femoral artery
Dorsalis pedis and posterior tibial arteries
Axillary artery
Carotid artery do not use
55
Invasive arterial blood pressure
Complication
Bleeding and hematoma
Vasospam
Thrombosis and thrombi
Aneurysm
Infection
Nerve damage
Necrosis of skin overlying the catheter
56
Invasive arterial blood pressure
Waveform
SBP gradually increases
MBP remains unchanged
57
Invasive arterial blood pressure
Waveform distortion
Normal test
underdamped
overdamped
58
Central venous pressure
Indication
Fluid administration for severe hypovolemia
and shock
Infusion of cardiac drugs
Aspiration of air emboli in craniotomy
Insertion of transcutaneous pacing leads
Total parenteral nutrition (TPN)
Venous access for patients with poor
peripheral veins
59
Central venous pressure
Contraindication
Renal cell Ca extension into RA, RA myxoma,
or fungating tricuspid valve vegetations
Skin infection at cannulation site
Severe coagulopathy
Ipsilateral carotid endarterectomy (IJ),
pneumothorax and hemothorax are relative
contraindication
60
Central venous pressure
Selective sites of cannulation
Internal jugular veins
Subclavian veins
Femoral veins
External veins
Basilic veins
61
Central venous pressure
Measurement
Catheters tip lies above or the junction of SVC
and RA
CVP is measured with cm H2O
CVP should be measured during end expiration
62
Central venous pressure
Waveform
a wave atrial contraction, absent in A fib and
exaggearted in JR (cannon wave)
c wave TV elevation@early ventricular contraction
v wave venous return against to closed TV
x descent downward displacement of TV (systole)
y descent TV opening during diastole
63
Central venous pressure
Complication
Bleeding and hemotoma
Pneumothorax and hemothorax
Pleural effusion and chylothorax
Line-related infection
Air thrombi
64
Pulmonary artery catheterization
Length 110 cm
OD 2.3 mm
Distal port
Proximal port
Balloon at tip
Themistor
65
It Is Time To Pull The PAC
PAC dose not improve outcome
in critically ill patients
66
Background
Pulmonary artery catheter(PAC) has been used in
critical care practice for three decades
Majority of PAC are inserted to aid in
management of critically ill pts in ICU and high
risk surgical pts in OR
Observational studies & small randomized
controlled trials (RCT) showed variable results:
Worse outcome
No difference in outcome
Some benefit
67
Summary
PAC-directed management in high risk
surgical, severe sepsis, shock and RADS
pts is a safe procedure
PAC use dose not improve outcome
PAC use may not increase cost of care
68
Pulmonary artery catheterization
Indication
Cardiac disease: CAD with LV dysfunction, valvular
heart disease, heart failure
Pulmonary disease: ARDS, severe COPD, Pulmonary
hypertension
Complex fluid management: shock, acute burn ARF,
MOF
Specific surgical procedure: aortic cross clamp
pheochromocytoma, liver transplants,
Hemodynamic unstability required cardiovascular
drug therapy
High-risk obstetrics: severe toxemia
69
Pulmonary artery catheterization
Contraindication
Severe TV or PV stenosis
RA or RV tumor
Endocarditis with vegetation on TV or PV
Other contraindication related to central
venous cannulation
70
Pulmonary artery catheter
71
Pulmonary artery catheterization
Insertion of catheter
72
PCWP and CVP
73
Pulmonary artery catheter in chest x-ray
74
Pulmonary artery catheterization
Complication
Complication associated with CV cannulation
Bacteremia and endocarditis
Thrombogenesis and pulmonary infarction
Pulmonary artery rupture and hemorrhage
Arrhythmias and conduction abnormalities
Pulmonary valve damage
75
Pulmonary capillary wedge pressure
CVP = RAP = RVEDP
PCWP = LAP = LVEDP
76
Hemodynamic parameter
BSA = (Ht + Wt 60)/100, nl 1.6 to 1.9 m2
CO = HR x SV
CI = CO/BSA
DO2 = CI x 13.4 x Hb x SaO2
VO2 = CI x 13.4 x Hb x (SaO2 SvO2)
* SvO2 obtained from PAC distal port
77
Hemodynamic Profiles
Heart failure:
Right heart failure Left heart failure
High RAP High PCWP
Low CI Low CI
High PVRI High SVRI
78
Hemodynamic profiles
Hypotension:
Hypovolemic Cardiogenic Vasogenic
Low CVP High CVP Low CVP
Low CI Low CI High CI
High SVRI High SVRI Low SVRI
79
Cardiac output monitoring
Thermodilution methods
Pulmonary artery catheter
Peripheral artery catheter (Picco)
Dye dilution methods
Echocardiography
Thoracic bioimpedance
80
Cardiac output monitoring
Fick principle
CO =
Oxygen consumption
a v O2 content difference
=
VO2
CaO2 CvO2
Fick principle is the basis of all indicator
dilution methods of determining cardiac
output
81
Thermodilution method
82
Hemodynamic management
Preload
Afterload
Cardiac contractility
83
Hemodynamic management
Preload
Monitoring via CVP or PCWP
Increased preload by giving volume
Decreased preload by giving diuretics and/or
vasodilators (nitroglycerin)
84
Hemodynamic management
Afterload
Vascular resistance
Balance between cardiac work and organ
perfusion
Vasodilators:
Systemic vasodilators: nitroprusside,
calcium channel blockers, a1-blockers
Pulmonary vasodilators: PGE1, PGI, NO
Vasocontrictors: levophed, epinephrine,
vasopresin
85
Hemodynamic management
Inotropic agents
Positive inotropic agents: epinephrine,
dopamine, dobutamine, PDEI (milrinone)
Negative inotropic agents: beta blocker and
calcium channel blockers
86
Hemodynamic management
Mechanical support (IABP)
87
Hemodynamic effect of IABP
Decrease afterload and promote SV
Increased diastolic pressure and coronary
blood flow in hypotensive patients
Indication: AMI, cardiac shock, unstable
angina, acute MR
Contraindication: AI, aortic dissection and
aortic graft in thoracic aorta
Complication: leg ischemia, septicemia
88
Acute renal failure (ARF)
The hallmark of ARF is azotemia and oliguria
Lab: blood urea nitrogen(BUN), criatinine(Cr), blood
electrolytes, glumerular filtration rate
Etiology: prerenal, renal and postrenal
Renal ischemia (50%),
Nephrotoxines (35%),
Intrinsic renal disease (15%)
50% of ARF in SICU due to major trauma or surgery
89
Etiology of ARF
90
Treatment of ARF
Supportive management
Diuretics and mannitol to maintain urine
output in nonoliguric patients
Renal dose dopamine?
Glucocorticoids for ARF due to vasculitis or
glomerulonephritis
Other: restrict fluid, sodium, potassium, posph
Renal replacement therapy (dialysis)
91
Renal Replacement Therapy
92
Infection in SICU
Infections are leading cause of death in ICUs
Community acquired and hospital acquired infection
Strains of bacteria resistant to commonly used
antibiotics are common
Advanced age, prolonged use of invasive devices,
respiratory failure, renal failure and head trauma are
established risk factors for hospital acquired infection
Multiple antibiotics and broad spectrum antibiotics
are commonly used in SICU
93
Nutrition support in SICU
Maintaining adequate nutrition in critically ill
patients improves wound healing. Restore
immune competence and reduces morbidity
and mortality
Critically ill patients generally required 1.0-
1.5g/kg/day instead of 0.5g/kg/day for
nonstressed patients
Enteral nutrition and parenteral nutrition
94
Enteral Nutrition in SICU
GI tract is the route of choice for nutrition
support when its functional integrity is intact
Enteral nutrition is simpler, cheaper, less
complicated, and fewer complication
Enteral nutrition can better preserve GI
structure and function
Diarrhea is most common problem related to
hyperosmolarity of the solution or lactose
intolerance
95
Parenteral Nutrition in SICU
Total parenteral nutrition (TPN) is indicated if
the GI tract cannot be used of if absorption is
inadequate
Complications of TPN are catheter-related and
metabolic
The most common problem in TPN is
hyperglycermia
Вам также может понравиться
- Icu GuidebookДокумент43 страницыIcu Guidebookdrimran570100% (4)
- Critical Care Reviews Book 2017Документ356 страницCritical Care Reviews Book 2017Herbert Baquerizo VargasОценок пока нет
- Hemodynamics For The Bedside Nurse 1CEUДокумент7 страницHemodynamics For The Bedside Nurse 1CEURN333100% (1)
- Manual IcuДокумент217 страницManual IcuEmil Zatopek100% (3)
- Avinash B Kumar MD Assistant Professor Anesthesiology and Critical Care Dec 2006Документ29 страницAvinash B Kumar MD Assistant Professor Anesthesiology and Critical Care Dec 2006sgod34Оценок пока нет
- Interpret Blood Gas Analysis & Acid-Base ImbalancesДокумент3 страницыInterpret Blood Gas Analysis & Acid-Base ImbalancesChameera Bandara100% (2)
- ICU AlgorithmsДокумент45 страницICU AlgorithmsHashimIdreesОценок пока нет
- Memorial Healthcare System (Hollywood, Florida) Program: - Within 5 Years Is PreferredДокумент27 страницMemorial Healthcare System (Hollywood, Florida) Program: - Within 5 Years Is PreferredRamanpreet Kaur MaanОценок пока нет
- Cardiac SurgeryДокумент110 страницCardiac SurgeryChristopher McAndrew100% (1)
- Preop TemplateДокумент1 страницаPreop TemplateJoseph D WalchОценок пока нет
- Anesthesiology GuideДокумент4 страницыAnesthesiology GuideGeorge Wang100% (1)
- Mksap NotesДокумент64 страницыMksap NotesobishtОценок пока нет
- Ecg Tutorial PDFДокумент82 страницыEcg Tutorial PDFpacpacpac123Оценок пока нет
- 2 Approach To The Neuro Exam Feb 2011Документ35 страниц2 Approach To The Neuro Exam Feb 2011suaqaziОценок пока нет
- Megacode Testing Checklist Scenarios 4-7-10 Tachycardia, VF, PEA, PC...Документ1 страницаMegacode Testing Checklist Scenarios 4-7-10 Tachycardia, VF, PEA, PC...krgduraiОценок пока нет
- EMERGENCY MEDICINE IN-SERVICE EXAM REVIEW 2009Документ147 страницEMERGENCY MEDICINE IN-SERVICE EXAM REVIEW 2009iamo107501100% (1)
- Necrotizing Otitis 2022Документ20 страницNecrotizing Otitis 2022asmashОценок пока нет
- Data Interpretation For Medical StudentДокумент18 страницData Interpretation For Medical StudentWee K WeiОценок пока нет
- RFDS Western Operations HEA16 - V3.0 Clinical ManualДокумент28 страницRFDS Western Operations HEA16 - V3.0 Clinical ManualJoed BiasonОценок пока нет
- The Intensive Care Unit MaualДокумент356 страницThe Intensive Care Unit MaualMariefel Villanueva AlejagaОценок пока нет
- Oral Board Exam AudioДокумент64 страницыOral Board Exam AudioMahjong SirenОценок пока нет
- ACLS Algorithms Adult 2010Документ12 страницACLS Algorithms Adult 2010anon_336736395Оценок пока нет
- Studying for the Cardiology BoardsДокумент20 страницStudying for the Cardiology BoardsDaniel Hans JayaОценок пока нет
- Critical Care Calculations Study GuideДокумент6 страницCritical Care Calculations Study GuideAja Blue100% (2)
- Respiratory Therapy Pocket Reference: Ifnopt TriggerДокумент2 страницыRespiratory Therapy Pocket Reference: Ifnopt TriggerJulieОценок пока нет
- Cardiac SurgeryДокумент101 страницаCardiac SurgeryHusein Fatih ArafatОценок пока нет
- Internal Medicine NotesДокумент54 страницыInternal Medicine NotesKiara Govender100% (1)
- The Red Book, 2022-23Документ189 страницThe Red Book, 2022-23Gringo Chan67% (3)
- Genetic and Environmental Factors Determine Natural Skin ColorДокумент113 страницGenetic and Environmental Factors Determine Natural Skin ColorNBMEmyselfandiОценок пока нет
- Critical Care: Past, Present and FutureДокумент81 страницаCritical Care: Past, Present and FuturehimanshuОценок пока нет
- 409 Pope, B. and Maillie, S. CCRN-PCCN Review Multisystem and Q and AДокумент21 страница409 Pope, B. and Maillie, S. CCRN-PCCN Review Multisystem and Q and Agliftan100% (2)
- Ccu Survival GuideДокумент10 страницCcu Survival Guideomegasauron0gmailcom100% (1)
- Anaesthesia For Renal TransplantationДокумент46 страницAnaesthesia For Renal TransplantationShehan WijayasiriwardanaОценок пока нет
- Advanced Medicine Recall A Must For MRCP PDFДокумент712 страницAdvanced Medicine Recall A Must For MRCP PDFKai Xin100% (2)
- 2017-2018 Intern GuideДокумент31 страница2017-2018 Intern GuideaskjagОценок пока нет
- Critical Care NotesДокумент18 страницCritical Care NotesjulieОценок пока нет
- Patient Rounding Format in SICU/CTICUДокумент4 страницыPatient Rounding Format in SICU/CTICUseigfried13Оценок пока нет
- List of 136 CCS cases from Feb 2020Документ4 страницыList of 136 CCS cases from Feb 2020Ramanpreet Kaur MaanОценок пока нет
- Test 3 OutlineДокумент3 страницыTest 3 Outlinemara5140Оценок пока нет
- ACC SAP 8 Exam1&2ACC SAP 8 Exam1&2Документ115 страницACC SAP 8 Exam1&2ACC SAP 8 Exam1&2Yahya Hassan Hussein El-tamaly100% (3)
- CardiacДокумент10 страницCardiacMarcus Reynolds100% (1)
- 10-Critical CareДокумент3 страницы10-Critical CareIbrahimFikryОценок пока нет
- Nephrotic and Nephritic Syndrome GuideДокумент3 страницыNephrotic and Nephritic Syndrome Guidewinston1234Оценок пока нет
- Respiratory SystemДокумент3 страницыRespiratory SystemAnna Dominique JimenezОценок пока нет
- Housestaff Manual 2023-2024 - MeadeДокумент267 страницHousestaff Manual 2023-2024 - MeadeMelchor Alcántara Barrera100% (2)
- Abnormal EcgДокумент8 страницAbnormal EcgM.DalaniОценок пока нет
- ACLS ECG Strip Interpretation and Study GuideДокумент12 страницACLS ECG Strip Interpretation and Study GuideMariana Berger100% (1)
- Intern Ward Survival Guide 2009Документ5 страницIntern Ward Survival Guide 2009mediquest100% (1)
- HemodynamicsДокумент2 страницыHemodynamicsbecksterbooОценок пока нет
- Caring For A Patient After Coronary Artery Bypass.6Документ6 страницCaring For A Patient After Coronary Artery Bypass.6Nadia BeadleОценок пока нет
- UCLA Intern Survival GuideДокумент57 страницUCLA Intern Survival GuideKevin Lewis100% (3)
- Cardiac Surgery Basic KnowledgeДокумент28 страницCardiac Surgery Basic KnowledgeGinwong100% (1)
- Hemodynamic MonitoringДокумент41 страницаHemodynamic MonitoringSuresh KumarОценок пока нет
- A Simple Guide to Hypovolemia, Diagnosis, Treatment and Related ConditionsОт EverandA Simple Guide to Hypovolemia, Diagnosis, Treatment and Related ConditionsОценок пока нет
- A Case-Based Approach to Interventional Pulmonology: A Focus on Asian PerspectivesОт EverandA Case-Based Approach to Interventional Pulmonology: A Focus on Asian PerspectivesJamalul Azizi Abdul RahamanОценок пока нет
- Emergency Department Resuscitation of the Critically Ill, 2nd Edition: A Crash Course in Critical CareОт EverandEmergency Department Resuscitation of the Critically Ill, 2nd Edition: A Crash Course in Critical CareОценок пока нет
- Bilary TractДокумент32 страницыBilary Tractlizzy596Оценок пока нет
- JAUNDICE Internal Medicine PresentationДокумент34 страницыJAUNDICE Internal Medicine PresentationNano BaddourОценок пока нет
- Dr. Vodde Changes in Specific Diagnoses From DSM IV To 5Документ183 страницыDr. Vodde Changes in Specific Diagnoses From DSM IV To 5lizzy596Оценок пока нет
- Psychiatry For Medical Students and ResidentsДокумент80 страницPsychiatry For Medical Students and ResidentsNabeel Kouka, MD, DO, MBA, MPH100% (4)
- Uwise NeoplasiaДокумент17 страницUwise Neoplasializzy596Оценок пока нет
- Complications of LaborДокумент53 страницыComplications of Laborlizzy596Оценок пока нет
- 8 Steps To Solving Acid-Base ProblemsДокумент2 страницы8 Steps To Solving Acid-Base Problemslizzy596Оценок пока нет
- Gynecology and Contraception TopicsДокумент24 страницыGynecology and Contraception Topicslizzy596Оценок пока нет
- Surgical History DemonstrationДокумент2 страницыSurgical History Demonstrationlizzy596Оценок пока нет
- Conduct Disorders TreatmentДокумент9 страницConduct Disorders Treatmentlizzy596Оценок пока нет
- 2012-13 Psychiatry Board ReviewДокумент79 страниц2012-13 Psychiatry Board Reviewlizzy596100% (1)
- Nasogastric Tube InsertionДокумент1 страницаNasogastric Tube Insertionlizzy596Оценок пока нет
- Bladder CatheterizationДокумент1 страницаBladder Catheterizationlizzy596Оценок пока нет
- ReducingДокумент13 страницReducinglizzy596Оценок пока нет
- 2012-13 Psychiatry Board ReviewДокумент79 страниц2012-13 Psychiatry Board Reviewlizzy596100% (1)
- 2012 ECG HandoutДокумент40 страниц2012 ECG Handoutlizzy596Оценок пока нет
- B. Belingon - Notes From Case Session Slides, Becky's Notes (Dr. Nguyen)Документ14 страницB. Belingon - Notes From Case Session Slides, Becky's Notes (Dr. Nguyen)lizzy596Оценок пока нет
- Bladder BugsДокумент10 страницBladder Bugslizzy596Оценок пока нет
- Respiratory Therapy Formulas and Values GuideДокумент1 страницаRespiratory Therapy Formulas and Values Guidelizzy59683% (6)
- Trauma Patient with Chest and Possible Abdominal InjuriesДокумент11 страницTrauma Patient with Chest and Possible Abdominal Injurieslizzy596Оценок пока нет
- Micro InfectiousDiseaseДокумент17 страницMicro InfectiousDiseaselizzy596Оценок пока нет
- Esophagus and Stomach NotesДокумент15 страницEsophagus and Stomach Noteslizzy596Оценок пока нет
- B. Belingon - Notes From Case Session Slides, Anna's Notes (Dr. Esterl), Becky's Notes (Dr. Nguyen)Документ11 страницB. Belingon - Notes From Case Session Slides, Anna's Notes (Dr. Esterl), Becky's Notes (Dr. Nguyen)lizzy596Оценок пока нет
- Female Reproduction Pathology ReviewДокумент23 страницыFemale Reproduction Pathology Reviewlizzy596Оценок пока нет
- Liver and Biliary NotesДокумент16 страницLiver and Biliary Noteslizzy596Оценок пока нет
- Cardio NotesДокумент7 страницCardio Noteslizzy596Оценок пока нет
- GlomerulonephritisДокумент1 страницаGlomerulonephritismaleskunОценок пока нет
- Kidney SyndromesДокумент35 страницKidney Syndromeslizzy596Оценок пока нет
- Week 2 Critical CareДокумент8 страницWeek 2 Critical Carelizzy596Оценок пока нет
- Ethnic Conflicts and PeacekeepingДокумент2 страницыEthnic Conflicts and PeacekeepingAmna KhanОценок пока нет
- Full Discography List at Wrathem (Dot) ComДокумент38 страницFull Discography List at Wrathem (Dot) ComwrathemОценок пока нет
- Java Interview Questions: Interfaces, Abstract Classes, Overloading, OverridingДокумент2 страницыJava Interview Questions: Interfaces, Abstract Classes, Overloading, OverridingGopal JoshiОценок пока нет
- Introduction To Computing (COMP-01102) Telecom 1 Semester: Lab Experiment No.05Документ7 страницIntroduction To Computing (COMP-01102) Telecom 1 Semester: Lab Experiment No.05ASISОценок пока нет
- 1 - Nature and Dev - Intl LawДокумент20 страниц1 - Nature and Dev - Intl Lawaditya singhОценок пока нет
- Online Statement of Marks For: B.A. (CBCS) PART 1 SEM 1 (Semester - 1) Examination: Oct-2020Документ1 страницаOnline Statement of Marks For: B.A. (CBCS) PART 1 SEM 1 (Semester - 1) Examination: Oct-2020Omkar ShewaleОценок пока нет
- (Class 8) MicroorganismsДокумент3 страницы(Class 8) MicroorganismsSnigdha GoelОценок пока нет
- Classification of Boreal Forest Ecosystem Goods and Services in FinlandДокумент197 страницClassification of Boreal Forest Ecosystem Goods and Services in FinlandSivamani SelvarajuОценок пока нет
- 2013 Gerber CatalogДокумент84 страницы2013 Gerber CatalogMario LopezОценок пока нет
- Javascript The Web Warrior Series 6Th Edition Vodnik Test Bank Full Chapter PDFДокумент31 страницаJavascript The Web Warrior Series 6Th Edition Vodnik Test Bank Full Chapter PDFtina.bobbitt231100% (10)
- La TraviataДокумент12 страницLa TraviataEljona YzellariОценок пока нет
- FCE Listening Test 1-5Документ20 страницFCE Listening Test 1-5Nguyễn Tâm Như Ý100% (2)
- Compound SentenceДокумент31 страницаCompound Sentencerosemarie ricoОценок пока нет
- Digi-Notes-Maths - Number-System-14-04-2017 PDFДокумент9 страницDigi-Notes-Maths - Number-System-14-04-2017 PDFMayank kumarОценок пока нет
- Art 1780280905 PDFДокумент8 страницArt 1780280905 PDFIesna NaОценок пока нет
- Popular Restaurant Types & London's Top EateriesДокумент6 страницPopular Restaurant Types & London's Top EateriesMisic MaximОценок пока нет
- PIA Project Final PDFДокумент45 страницPIA Project Final PDFFahim UddinОценок пока нет
- EAPP Q2 Module 2Документ24 страницыEAPP Q2 Module 2archiviansfilesОценок пока нет
- Canine Guided Occlusion and Group FuntionДокумент1 страницаCanine Guided Occlusion and Group Funtionlittlestar35100% (3)
- Comal ISD ReportДокумент26 страницComal ISD ReportMariah MedinaОценок пока нет
- Vegan Banana Bread Pancakes With Chocolate Chunks Recipe + VideoДокумент33 страницыVegan Banana Bread Pancakes With Chocolate Chunks Recipe + VideoGiuliana FloresОценок пока нет
- Professional Ethics AssignmentДокумент12 страницProfessional Ethics AssignmentNOBINОценок пока нет
- Sample Letter of Intent To PurchaseДокумент2 страницыSample Letter of Intent To PurchaseChairmanОценок пока нет
- Mayflower Compact - WikipediaДокумент4 страницыMayflower Compact - WikipediaHeaven2012Оценок пока нет
- Statement of The Problem: Notre Dame of Marbel University Integrated Basic EducationДокумент6 страницStatement of The Problem: Notre Dame of Marbel University Integrated Basic Educationgab rielleОценок пока нет
- AI Capstone Project Report for Image Captioning and Digital AssistantДокумент28 страницAI Capstone Project Report for Image Captioning and Digital Assistantakg29950% (2)
- Obtaining Workplace InformationДокумент4 страницыObtaining Workplace InformationJessica CarismaОценок пока нет
- A Review On Translation Strategies of Little Prince' by Ahmad Shamlou and Abolhasan NajafiДокумент9 страницA Review On Translation Strategies of Little Prince' by Ahmad Shamlou and Abolhasan Najafiinfo3814Оценок пока нет
- Codilla Vs MartinezДокумент3 страницыCodilla Vs MartinezMaria Recheille Banac KinazoОценок пока нет
- Marrickville DCP 2011 - 2.3 Site and Context AnalysisДокумент9 страницMarrickville DCP 2011 - 2.3 Site and Context AnalysiskiranjiОценок пока нет