Академический Документы
Профессиональный Документы
Культура Документы
03 Marmor New AAPGuidelines For Pediatric UTIMgmt
Загружено:
hafidzz1Оригинальное название
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
03 Marmor New AAPGuidelines For Pediatric UTIMgmt
Загружено:
hafidzz1Авторское право:
Доступные форматы
1
Andi Marmor, MD
December, 2012
Recognize infants who should be tested for UTI
Choose the best method of collecting urine in a
febrile infant
Interpret the results of a UA/urine culture
Apply newest recommendations for imaging
after first febrile UTI in your practice
Most common bacterial infection in infants
<24 months with fever without a source (FWS)
Diagnostic challenge!
Pyelonephritis (upper tract) common
Bacteremia/urosepsis in young infants
May herald presence of UT abnormalities
Predispose to recurrent UTI, kidney damage
2011 AAP Guidelines were long-awaited
Committee on QI and Management
Gen peds, epi, ID, nephrology, radiology, urology
No financial conflicts of interest
Reviewed by multiple groups
2 searches of literature over the last 10 years
Systematic review on prophylactic abx
Authors contacted to provide raw data
2
1. Who should be tested for UTI?
2. How should urine be obtained for testing?
3. How should we make the diagnosis?
4. How should we treat UTI in young children?
5. When is imaging needed?
1. Who should be tested for UTI?
2. How should urine be obtained for testing?
3. How should we make the diagnosis?
4. How should we treat UTI in young children?
5. When is imaging needed?
Updated in 2011 AAP Guidelines
1. Who should be tested for UTI?
2. How should urine be obtained for testing?
3. How should we make the diagnosis?
4. How should we treat UTI in young children?
5. When is imaging needed?
Most common question
Bruno is a 5 month old boy who has felt hot
at home for 3 days, vomited once this
morning
Temp 39.1 in clinic, remaining VS are normal
Non-toxic and only mildly dehydrated
No source for fever found on history or PE
PMH: generally healthy, has received 3 doses
of PCV-13. Uncircumcised
Question 1: Should we test him for UTI?
3
1999 GUIDELINE
Collect urine in all girls and
uncircumcised boys <2 +
circ boys <1 with FWS
Various thresholds for +
culture (10-100K)
2011 GUIDELINE
Use clinical factors to
decide if risk of UTI is >1-
2%
+UA and + culture (>50 K)
necessary for dx of UTI
1. In infant requires abx, get cath urine (A)
2. If abx not required, assess likelihood of UTI (A)
a. If low*, observation OK
b. If not low, then obtain urine (cath or bag)
1. In infant requires abx, get cath urine (A)
2. If abx not required, assess likelihood of UTI (A)
a. If low*, observation OK
b. If not low, then obtain urine (cath or bag)
*low = < 2%?
All uncircumcised boys with FWS have risk >2%
Girls with FWS and 2 other risk factors have risk > 2%
Circumcised boys with FWS and all 3 risk factors have risk > 2%
AAP Table of Probabilities of UTI in Febrile Infants
4
Infants <3 months of age:
Overall risk is 10-15%
Uncirc boys highest risk group
Bacteremia in 15-20%
Infants and children >3 months of age:
Girls 3-24 mo ~10%
Uncirc boys 3-6 mo: 5-10%->2% by 1 year
Circ boys <1%
Low/moderate baseline probabilities should be
modified based on other risk factors!
Height of fever
Duration of fever
Ethnicity?
Girls: white
Boys: non-black
Latino boys at higher risk, even when controlled for
circumcision status
I think that ~ 5% is a reasonable threshold,
unless infant is at high risk for severe illness
<3 months of age (T>38)
All infants
3 -24months of age (T>39)
Girls: with fever for 2 days
Boys:
Uncircumcised <6 months of age (< 12 if other risk fx)
Circ boys: consider only if other risk factors present
What is Brunos approximate risk of UTI?
Based on age (5 mo), circumcision status
(uncircumcised) and duration of fever (3
days): best estimate ~5-10%
You decide to test for UTI
Question 2: How do you want to collect
Brunos urine?
5
A. Urethral catheter
B. Supra-pubic bladder aspiration
C. Clean catch
D. Diaper pad
1. In infant requiring abx, get cath urine (A)
2. If abx not required, assess likelihood of UTI (A)
a. If low, observation OK
b. If not low, then obtain urine (cath or bag)*
*AAP Recs: bag OK for UA, but if +, cath for culture
Suprapubic aspiration
(SPA)
Catheter
Urine bag
Surprise clean catch
6
Suprapubic aspiration
(SPA)
Catheter
Urine bag
Surprise clean catch
Specificity of LE lower in bag
62-84% vs 91-94% for cath
1
But sensitivity is similar
This makes a negative bag
UA more helpful than a
positive one
Especially in a low-risk pt
1
Schroeder 2005; McGillivray, 2005
Since the culture is our gold standard we need
to minimize false positives AND false negatives
False POSITIVES with bag culture
Depend on the gender, technique, and + threshold
False NEGATIVES
Depend on the threshold chosen for positive test
Higher threshold = false pos, false negs
Since the culture is our gold standard we need
to minimize false positives AND false negatives
False POSITIVES with bag culture
Depend on the gender, technique, and + threshold
False NEGATIVES
Depend on the threshold chosen for positive test
Higher threshold = false pos, false negs
Usual + threshold is >100,000 orgs
Rate of FP and FN both ~15% at this threshold
7
Does bag culture (using 100,000K threshold)
change PP enough to be useful?
Prior Prob PPV NPV
5% 23% 1%
10% 40% 2%
20% 60% 4%
Does bag culture (using 100,000K threshold)
change PP enough to be useful?
Prior Prob PPV NPV
5% 23% 1%
10% 40% 2%
20% 60% 4%
The best use of the bag culture is to rule OUT UTI in
the low prior probability patient
High Risk
Infant < 6 mo of age
Systemically ill
Further workup if +UTI
Low/Mod Risk
> 6 mo of age
Well-appearing
First time UTI
Cath urine preferred
Treat if +
Bag urine OK
Good NPV
If UA+, consider sending
cath specimen for culture
Since Bruno is uncircumcised, <6 mo of age,
and he has had a high fever for several days,
you decide to get a cath urine
The UA is positive for LE
Question 3: What would you do next?
8
1. In infant requiring abx, get cath urine (A)
2. If abx not required, assess likelihood of UTI (A)
a. If low, observation OK
b. If not low, then obtain urine (cath or bag)
3. Diagnosis requires + UA and + culture of at
least 50K of a uropathogen (C)
Committee on QI and Management
Gen peds, epi,, ID, nephrology, radiology, urology
No financial conflicts of interest
Reviewed by multiple groups
2 searches of literature over the last 10 years
Systematic review on prophylactic abx
Authors contacted to provide raw data
2 assumptions:
1. Low sensitivity of LE is due to false + cultures
False negatives occur in pts with asymptomatic bacteriuria
True sensitivity is higher, so infection unlikely if LE negative
2. Diagnosing infants with asymptomatic bacteriuria
as having UTI does more harm than good
The number of true UTIs missed will be small
Benefits of not over-treating > risk of missing a UTI
2 assumptions:
1. Low sensitivity of LE is due to false + cultures
False negatives occur in pts with asymptomatic bacteriuria
True sensitivity is higher, so infection unlikely if LE negative
2. Diagnosing infants with asymptomatic bacteriuria
as having UTI does more harm than good
The number of true UTIs missed will be small
Benefits of not over-treating > risk of missing a UTI
Both true in low-risk infants
9
High risk = Young infants, or those sick
enough to require IV antibiotics/admission:
Obtain a catheter specimen for UA and
culture
Negative UA: confirm with culture
Positive UA: start treatment, confirm with culture
Positive culture = > 10,000 CFU/HPF
If desired, collect bag specimen for UA
Negative UA: UTI is unlikely
Positive UA: confirm with a culture
Preferred: send a cath specimen for culture
If you send a clean bag sample for culture
Use >100,000 for + threshold
Consider clinical implications before sending!
1. Who should be tested for UTI?
2. How should urine be obtained for testing?
3. How should we make the diagnosis?
4. How should we treat UTI in young children?
5. When is imaging needed?
PO antibiotics for 10 days for most infants
IV if ill-appearing, < 2 months of age, or poor PO
Local
microbiology/sensitivit
ies should determine
treatment
E.Coli
10
Bruno is treated with oral cephalexin for 10
days, and is afebrile after 24 hours
His urine culture grows >100,000 colonies of
E. Coli
Question 4: Does he need imaging to exclude
a urinary tract abnormality?
A. Renal ultrasound
B. Voiding cysto-urethrogram(VCUG)
C. Renal DMSA scan
D. No imaging
1999 GUIDELINE
Ultrasound:
Earliest convenience
Urgent if poor response
VCUG:
Earliest convenient time
Prophylactic abx while
awaiting VCUG
2011 GUIDELINE
Ultrasound:
Earliest convenience
Urgent if poor response
VCUG:
If abnormal ultrasound
After 2
nd
UTI
Antibiotics not
recommended
1999 GUIDELINE
Ultrasound:
Earliest convenience
Urgent if poor response
VCUG:
Earliest convenient time
Prophylactic abx while
awaiting VCUG
2011 GUIDELINE
Ultrasound:
Earliest convenience
Urgent if poor response
VCUG:
If abnormal ultrasound
After 2
nd
UTI
Antibiotics not
recommended
11
1. Febrile infants with UTI should have renal US
(acutely if ill, or after resolution if well) (C)
2. VCUG
a. Should NOT be performed routinely (B)
b. Consider if highly abnUS or recurrent UTI (X)
Goals of imaging after
1
st
UTI are to
Identify significant
urinary tract
abnormalities
Prevent recurrent UTIs
and further renal
damage
What does this
baby have?
Tissue remnant in the male urethra
1 in 5-8,000 pregnancies
Majority identified prenatally
Presentation in infancy:
Distension, poor urine stream, renal failure, urosepsis
15-20% progress to ESRD despite surgical
management
Prognosis independent of UTI, age at presentation
1
Damage already done?
1
DeFoor, 2008
Retrograde flow of urine during voiding
Most common urinary tract abnormality
~30-50% of infants <3 years with 1
st
UTI
Most outgrown in childhood
Normal
Abnormal
12
Inexpensive and relatively non-invasive
Operator-dependent
Good for:
Obstruction, gross structural abnormalities
What about VUR?
Specificity for VUR is high, but sensitivity low
Sensitivity for high-gradeVUR ~85%
Good NPV in low-risk patients!
More sensitive and
specific
More invasive, involves
radiation
Necessary? IF
VUR predicted recurrent
UTIs and progressive renal
damage AND
Intervention were effective
at preventing these
consequences
More sensitive and
specific
More invasive, involves
radiation
Necessary? IF
VUR predicted recurrent
UTIs and progressive renal
damage AND
Intervention were effective
at preventing these
consequences
13
Recurrence rate similar between children
with/without VUR
UTIs recur despite repair of VUR
Scarring more likely to be found in infants
with hi-grade reflux AND recurrent UTI
BUT
Scarring does not seem to be directly related to
UTI recurrence or presence of VUR
Non-progressive, may occur without VUR and
without UTIs
Incidence of ESRD = 5/million
5-12% of patients with ESRD have reflux
nephropathy as a cause
Risk of ESRD after episode of pyelo?
Craig: 1/10,000
Blumenthal: < 1/million
Aggressive treatment of VUR in the last 30
years has not affected ESRD rates
More sensitive and
specific
More invasive, involves
radiation
Necessary? IF
VUR predicted recurrent
UTIs and progressive renal
damage AND
Intervention were effective
at preventing these
consequences
14
Retrospective: medical vs surgical management
No difference in scarring
Cochrane review (2004): medical vs medical +
surgical
Rates of recurrent UTI and scarring similar
Need RCT of surgical vs expectant management!
Multiple RCTs of kids with 1st time UTI, +/- VUR
None have shown significant difference between
groups in UTI recurrence or renal scarring
Trend towards:
Recurrence and resistance MORE likely in those
receiving antibiotics
More recurrences in those with higher grade VUR
Limitations:
Study sizes limited
Variable inclusion of children with high-grade reflux
Antibiotics do not seem to prevent recurrent
UTI or renal scarring in kids with/without VUR
Fixing VUR confers no additional benefit
2011 AAP Guideline:
If [antibiotic] prophylaxis is, in fact, not beneficial
then the rationale for performing VCUG
routinely after an initial febrile UTI must be
questioned
Schroeder, 2011
Retro review before/after new imaging policy
NO change in UTI recurrence, detection of hi-
grade VUR
Decrease in imaging, abx and low-grade VUR
Pennesi, 2012
Retrospective review of 406 kids with 1
st
UTI
Only those with abnormal U/S got VCUG
Of the 7% who had abnUS, 13% had scarring =
1.5% total
15
1. Febrile infants with UTI should have renal US
(acutely if ill, or after resolution if well) (C)
2. VCUG
a. Should NOT be performed routinely (B)
b. Consider if highly abnUS or recurrent UTI (X)
1. Febrile infants with UTI should have renal US
(acutely if ill, or after resolution if well) (C)
2. VCUG
a. Should NOT be performed routinely (B)
b. Consider if highly abnUS or recurrent UTI (X)
Committee on QI and Management
Gen peds, epi,, ID, nephrology, radiology, urology
No financial conflicts of interest
Reviewed by multiple groups
2 searches of literature over the last 10 years
Systematic review on prophylactic abx
Authors contacted to provide raw data
Nuclear isotope
Documents renal
scarring
Most useful for
research.
16
Goals: Find severe abnormalities that need to
be treated or followed
Ultrasound
After first infection if < 3 mo, recurrent if > 3 mo
In acute infection if unusual clinical course
VCUG only if
UT obstruction/abnormality on ultrasound
Recurrent UTI + VUR on U/S and surgical correction
considered
A. Renal ultrasound
B. Voiding cysto-urethrogram(VCUG)
C. Renal DMSA scan
D. No imaging
My practice: no imaging, if he responds to treatment
Consider pyelonephritis in all infants <24 mo
with FWS
Test for UTI in when probability >5%, or
concern is high
All infants <3 months of age with FWS (T>38)
3 -24months of age (T>39)
Girls with fever for 2 days
Uncircumcised boys <6 mo (< 12mo if other risk fx)
Circ boys: ONLY if other risk factors present
Obtain ultrasound
In complicated or recurrent UTI
Consider after 1
st
UTI in high risk or very young infants
Consider VCUG
If ultrasound shows high grade VUR or obstruction
and surgical correction is considered
Antibiotics are NOT recommended to prevent
recurrent UTIs, even in patients with known or
suspected VUR
Diagnose and treat recurrent febrile UTI in all
infants!
17
Вам также может понравиться
- ATP IV HandoutДокумент2 страницыATP IV Handouthafidzz1Оценок пока нет
- Nilai Normal LABДокумент5 страницNilai Normal LABhafidzz1Оценок пока нет
- Kaji Latih Ilmu BedahДокумент1 страницаKaji Latih Ilmu Bedahhafidzz1Оценок пока нет
- Treatment CA - Penis OkiДокумент12 страницTreatment CA - Penis Okihafidzz1Оценок пока нет
- Gestational Trophoblastic Disease (GTD) Part I: Molar PregnancyДокумент88 страницGestational Trophoblastic Disease (GTD) Part I: Molar Pregnancyhafidzz1100% (1)
- Cost and Resource Impact of SIGN 97: Risk Estimation and The Prevention of Cardiovascular DiseaseДокумент10 страницCost and Resource Impact of SIGN 97: Risk Estimation and The Prevention of Cardiovascular Diseasehafidzz1Оценок пока нет
- CVD Risk AssessmentДокумент5 страницCVD Risk Assessmenthafidzz1Оценок пока нет
- Management of Patients With High CVD RiskДокумент10 страницManagement of Patients With High CVD Riskhafidzz1Оценок пока нет
- The Yellow House: A Memoir (2019 National Book Award Winner)От EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Рейтинг: 4 из 5 звезд4/5 (98)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeОт EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeРейтинг: 4 из 5 звезд4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingОт EverandThe Little Book of Hygge: Danish Secrets to Happy LivingРейтинг: 3.5 из 5 звезд3.5/5 (400)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureОт EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureРейтинг: 4.5 из 5 звезд4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryОт EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryРейтинг: 3.5 из 5 звезд3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceОт EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceРейтинг: 4 из 5 звезд4/5 (895)
- Team of Rivals: The Political Genius of Abraham LincolnОт EverandTeam of Rivals: The Political Genius of Abraham LincolnРейтинг: 4.5 из 5 звезд4.5/5 (234)
- Never Split the Difference: Negotiating As If Your Life Depended On ItОт EverandNever Split the Difference: Negotiating As If Your Life Depended On ItРейтинг: 4.5 из 5 звезд4.5/5 (838)
- The Emperor of All Maladies: A Biography of CancerОт EverandThe Emperor of All Maladies: A Biography of CancerРейтинг: 4.5 из 5 звезд4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaОт EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaРейтинг: 4.5 из 5 звезд4.5/5 (266)
- The Unwinding: An Inner History of the New AmericaОт EverandThe Unwinding: An Inner History of the New AmericaРейтинг: 4 из 5 звезд4/5 (45)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersОт EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersРейтинг: 4.5 из 5 звезд4.5/5 (345)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyОт EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyРейтинг: 3.5 из 5 звезд3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreОт EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreРейтинг: 4 из 5 звезд4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)От EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Рейтинг: 4.5 из 5 звезд4.5/5 (121)
- Nursing Care Plan CholecystectomyДокумент2 страницыNursing Care Plan Cholecystectomyderic87% (23)
- Background of The StudyДокумент3 страницыBackground of The StudyKraeОценок пока нет
- Activity Sheet For Health 2Документ15 страницActivity Sheet For Health 2Marites Espino MaonОценок пока нет
- Diabetic Emergencies PDFДокумент11 страницDiabetic Emergencies PDFJuan C. Salazar PajaresОценок пока нет
- Prescribing For The ElderlyДокумент8 страницPrescribing For The ElderlykarladeyОценок пока нет
- Lyons Et Al-2017-Periodontology 2000Документ4 страницыLyons Et Al-2017-Periodontology 2000Julio César PlataОценок пока нет
- Health & Family Welfare Department: Government of West BengalДокумент2 страницыHealth & Family Welfare Department: Government of West BengalAnkit JhaОценок пока нет
- Productos Cataloguo Tappa PDFДокумент10 страницProductos Cataloguo Tappa PDFjavier jimenezОценок пока нет
- English Course Guide Ws 2017Документ165 страницEnglish Course Guide Ws 2017César TapiaОценок пока нет
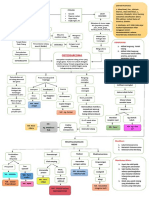
- Woc Osteosarcoma WidyaДокумент1 страницаWoc Osteosarcoma WidyaWidya Agustiani0% (1)
- Oral and Maxillofacial Manifestations in Patients With Drug AddictionДокумент8 страницOral and Maxillofacial Manifestations in Patients With Drug AddictionDiana Mihaela IlieОценок пока нет
- PhysioEx Exercise 7 Activity 1 Damagel)Документ3 страницыPhysioEx Exercise 7 Activity 1 Damagel)CLAUDIA ELISABET BECERRA GONZALESОценок пока нет
- Meniscus Injuries: Uhuebor David Mbbs (Lagos)Документ23 страницыMeniscus Injuries: Uhuebor David Mbbs (Lagos)Uhuebor DavidОценок пока нет
- 0708 How Investments PatientSurveyДокумент10 страниц0708 How Investments PatientSurveyRishi jainОценок пока нет
- NCP Inactivity ToleranceДокумент16 страницNCP Inactivity ToleranceChrisTine M. MoralesОценок пока нет
- Dapus SkripsiДокумент3 страницыDapus SkripsiGaluh MahardikaОценок пока нет
- Malignant Diseases of The CervixДокумент128 страницMalignant Diseases of The Cervixnicewan0% (1)
- Death Wish ListДокумент6 страницDeath Wish ListphilippatstonОценок пока нет
- TrepДокумент50 страницTrepMiguel Adrian GaonaОценок пока нет
- Relapse PreventionДокумент1 страницаRelapse PreventionAnonymous nYp4sSОценок пока нет
- Here's Your Coronavirus Insurance: You Have Made A Wise ChoiceДокумент3 страницыHere's Your Coronavirus Insurance: You Have Made A Wise ChoiceAjay Kumar GumithiОценок пока нет
- Pulmonary Catheter Learning Package PDFДокумент36 страницPulmonary Catheter Learning Package PDFnisar khanОценок пока нет
- Presentation Resuscitation - Power PointДокумент45 страницPresentation Resuscitation - Power PointRouquia ManzoorОценок пока нет
- Ak Sharma Pharmacy Final SIF ReportДокумент10 страницAk Sharma Pharmacy Final SIF ReportAmit ChaudharyОценок пока нет
- NCMA113 FUNDA SKILL 1 Performing Medical HandwashingДокумент3 страницыNCMA113 FUNDA SKILL 1 Performing Medical HandwashingJessoliver GalvezОценок пока нет
- The Scoop On Brain Healt Dietary Supplement Products Containing Huperzine AДокумент7 страницThe Scoop On Brain Healt Dietary Supplement Products Containing Huperzine Avasilyi IvanenkoОценок пока нет
- Orahex Oral SolutionДокумент1 страницаOrahex Oral SolutionconanmarcОценок пока нет
- FFMedicalDevicesRules2017Notifiedon16 01 2018Документ93 страницыFFMedicalDevicesRules2017Notifiedon16 01 2018Anonymous dukfCrCBdnОценок пока нет
- National Guideline For Kala-Azar Case Management Bangladesh 2013Документ72 страницыNational Guideline For Kala-Azar Case Management Bangladesh 2013Kutu MiaОценок пока нет
- SDMS ID: P2010/0496-001 2.9/09WACS Title: Management of Postpartum HaemorrhageДокумент11 страницSDMS ID: P2010/0496-001 2.9/09WACS Title: Management of Postpartum HaemorrhageYwagar YwagarОценок пока нет