Академический Документы
Профессиональный Документы
Культура Документы
Impaired Physical Mobility NCP
Загружено:
MeljonesDaan100%(1)100% нашли этот документ полезным (1 голос)
12K просмотров3 страницыimpaired physical mobility ncp
Оригинальное название
impaired physical mobility ncp
Авторское право
© © All Rights Reserved
Доступные форматы
DOCX, PDF, TXT или читайте онлайн в Scribd
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документimpaired physical mobility ncp
Авторское право:
© All Rights Reserved
Доступные форматы
Скачайте в формате DOCX, PDF, TXT или читайте онлайн в Scribd
100%(1)100% нашли этот документ полезным (1 голос)
12K просмотров3 страницыImpaired Physical Mobility NCP
Загружено:
MeljonesDaanimpaired physical mobility ncp
Авторское право:
© All Rights Reserved
Доступные форматы
Скачайте в формате DOCX, PDF, TXT или читайте онлайн в Scribd
Вы находитесь на странице: 1из 3
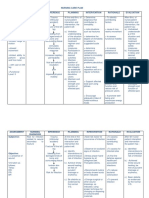
Impaired Physical Mobility
Assessment Nursing Diagnosis Objective Intervention Rationale Evaluation
S> dli nako mabuhat
akong gusto buhaton
sama sa pag kaon,
pag-areglar sa akong
kaugalingon as
verbalized.
O>
Weakness
Slowed
movement
Limited range
of motion
Impaired
Physical
mobility r/t
Neuromuscular
skeletal
impairment;
pain/discomfort
; restrictive
therapies (limb
immobilization)
as evidenced by
Reluctance to
attempt
movement;
limited ROM
and Decreased
muscle
strength/control
Regain/maintai
n mobility at
the highest
possible level.
Maintain
position of
function.
Increase
strength/functio
n of affected
and
compensatory
body parts.
Demonstrate
techniques that
enable
resumption of
activities.
Assess degree of
immobility produced by
injury/treatment and
note patients
perception of
immobility.
Encourage participation
in
diversional/recreational
activities. Maintain
stimulating
environment, e.g.,
radio, TV, newspapers,
personal
possessions/pictures,
clock, calendar, visits
from family/friends.
Instruct patient
in/assist with
active/passive ROM
exercises of affected
and unaffected
extremities.
Encourage use of
isometric exercises
starting with the
unaffected limb.
Patient may be restricted
by self-view/self-
perception out of
proportion with actual
physical limitations,
requiring
information/interventions
to promote progress
toward wellness.
Provides opportunity for
release of energy,
refocuses attention,
enhances patients sense
of self-control/self-worth,
and aids in reducing
social isolation.
Increases blood flow to
muscles and bone to
improve muscle tone,
maintain joint mobility;
prevent
contractures/atrophy and
calcium resorption from
disuse
Isometrics contract
muscles without bending
joints or moving limbs
and help maintain muscle
STE:
The client was
able rest at
intervals.
LTE:
After 3 days
nursing
intervention,
goal is met
through the
regaining of
patients
previous range
of motion.
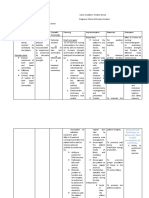
Provide footboard,
wrist splints,
trochanter/hand rolls
as appropriate.
Place in supine
position periodically if
possible, when traction
is used to stabilize
lower limb fractures.
Instruct in/encourage
use of trapeze and
post position for
lower limb fractures.
Assist with/encourage
self-care activities (e.g.,
bathing, shaving).
Provide/assist with
mobility by means of
wheelchair, walker,
crutches, canes as soon
as possible. Instruct in
safe use of mobility
aids.
Monitor blood pressure
(BP) with resumption of
activity. Note reports of
dizziness.
Reposition periodically
strength and mass. Note:
These exercises are
contraindicated while
acute bleeding/edema is
present.
Useful in maintaining
functional position of
extremities, hands/feet,
and preventing
complications (e.g.,
contractures/footdrop).
Reduces risk of flexion
contracture of hip.
Facilitates movement
during hygiene/skin care
and linen changes;
reduces discomfort of
remaining flat in bed.
Post position involves
placing the uninjured foot
flat on the bed with the
knee bent while grasping
the trapeze and lifting the
body off the bed.
Improves muscle
strength and circulation,
enhances patient control
in situation, and
promotes self-directed
wellness.
and encourage
coughing/deep-
breathing exercises.
Auscultate bowel
sounds. Monitor
elimination habits and
provide for regular
bowel routine. Place on
bedside commode, if
feasible, or use fracture
pan. Provide privacy.
Encourage increased
fluid intake to 2000
3000 mL/day (within
cardiac tolerance),
including acid/ash
juices.
Provide diet high in
proteins,
carbohydrates,
vitamins, and minerals,
limiting protein content
until after first bowel
movement.
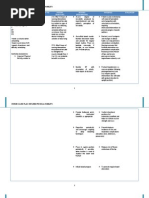
Early mobility reduces
complications of bed rest
(e.g., phlebitis) and
promotes healing and
normalization of organ
function. Learning the
correct way to use aids is
important to maintain
optimal mobility and
patient safety.
Postural hypotension is a
common problem
following prolonged bed
rest and may require
specific interventions
(e.g., tilt table with
gradual elevation to
upright position).
Prevents/reduces
incidence of skin and
respiratory complications
(e.g., decubitus,
atelectasis, pneumonia).
Вам также может понравиться
- Impaired Physical Mobility - FractureДокумент10 страницImpaired Physical Mobility - FractureLea TanОценок пока нет
- Impaired Physical MobilityДокумент11 страницImpaired Physical MobilityAgronaSlaughter100% (1)
- Impaired Physical Mobility NCPДокумент3 страницыImpaired Physical Mobility NCPYan ReyesОценок пока нет
- NCP-Impaired Physical Mobility - E+ ImbalanceДокумент3 страницыNCP-Impaired Physical Mobility - E+ ImbalanceRene John FranciscoОценок пока нет
- Impaired Physical MobilityДокумент3 страницыImpaired Physical MobilityCharmaine ChuaОценок пока нет
- NCP OsteomyelitisДокумент3 страницыNCP OsteomyelitisClariss Alota100% (2)
- NCP-Impaired Physical MobilityДокумент6 страницNCP-Impaired Physical MobilityRowell Zaragoza91% (11)
- Nursing Care Plan - Impaired Physical MobilityДокумент2 страницыNursing Care Plan - Impaired Physical MobilitySusan Croce57% (7)
- Impaired Physical Mobility. NCPДокумент1 страницаImpaired Physical Mobility. NCPwguino100% (3)
- NCP Risk For Fall DHFДокумент3 страницыNCP Risk For Fall DHFfortuneaya80% (5)
- NCP (Impaired Physical Mobility)Документ1 страницаNCP (Impaired Physical Mobility)soclose0488% (26)
- Impaired Physical MobilityДокумент1 страницаImpaired Physical Mobilityrozj0781% (21)
- NCP - Risk For FallsДокумент5 страницNCP - Risk For FallsMae CeaesarОценок пока нет
- NCP Impaired Physical MobilityДокумент6 страницNCP Impaired Physical MobilityRene John Francisco100% (1)
- DM NCPДокумент8 страницDM NCPCaress Mae Gubaton CabudoyОценок пока нет
- NCP Impaired Physical MobilityДокумент2 страницыNCP Impaired Physical MobilityKate Charnhattasin63% (8)
- XIII. NCP Risk For FallsДокумент1 страницаXIII. NCP Risk For FallsMartin T Manuel100% (2)
- Risk For Fall NCPДокумент8 страницRisk For Fall NCPVianah Eve EscobidoОценок пока нет
- IMPAIRED PHYSICAL MOBILITY RT Neuromuscular Involvement (Right Sided Paresthesia Aeb Inability To Purposefully Move Body Parts.Документ2 страницыIMPAIRED PHYSICAL MOBILITY RT Neuromuscular Involvement (Right Sided Paresthesia Aeb Inability To Purposefully Move Body Parts.Senyorita KHaye67% (3)
- NCP Impaired Skin IntegrityДокумент3 страницыNCP Impaired Skin IntegrityFlauros Ryu Jabien83% (6)
- NCP For Impaired Physical MobilityДокумент2 страницыNCP For Impaired Physical MobilityFielMendoza0% (1)
- NCP Acute PainДокумент3 страницыNCP Acute PainSatchiko Riko SakuraОценок пока нет
- Nursing Care Plan Assessment Nursing Diagnosis Inference Planning Intervention Rationale Evaluation SubjectiveДокумент2 страницыNursing Care Plan Assessment Nursing Diagnosis Inference Planning Intervention Rationale Evaluation SubjectiveDat boiОценок пока нет
- NCP: Patient With A Pressure UlcerДокумент2 страницыNCP: Patient With A Pressure UlcerICa MarlinaОценок пока нет
- NCP-Impaired Physical MobilityДокумент3 страницыNCP-Impaired Physical MobilityradarsoulОценок пока нет
- PATIENT: Remedios Garma ROOM: 408Документ2 страницыPATIENT: Remedios Garma ROOM: 408andreaОценок пока нет
- NURSING CARE PLAN Problem Body Weakness Nursing Diagnosis Impaired PhysicalДокумент1 страницаNURSING CARE PLAN Problem Body Weakness Nursing Diagnosis Impaired Physicalmitchie riveraОценок пока нет
- NCP - Acute Pain - FractureДокумент1 страницаNCP - Acute Pain - Fracturemawel73% (22)
- NCP For Impaired Physical MobilityДокумент1 страницаNCP For Impaired Physical Mobilityitzme_andreaОценок пока нет
- NCP For Impaired Physical MobilityДокумент2 страницыNCP For Impaired Physical MobilityPrincess Averin NavarroОценок пока нет
- NCP Impaired Physical MobilityДокумент2 страницыNCP Impaired Physical MobilityJohn Michael FernandezОценок пока нет
- NCP: Impaired Physical Immobility Related To Loss of A Limb (Amputation)Документ5 страницNCP: Impaired Physical Immobility Related To Loss of A Limb (Amputation)RazelAnneValinoОценок пока нет
- Activity Intolerance NCPДокумент7 страницActivity Intolerance NCPMariquita BuenafeОценок пока нет
- NCP Risk For InjuryДокумент2 страницыNCP Risk For InjuryAbigail Joy Tabones75% (4)
- Acute Pain NCPДокумент3 страницыAcute Pain NCPMjhay Montemayor100% (1)
- NCP Impaired Physical Mobility Acute PainДокумент8 страницNCP Impaired Physical Mobility Acute PainAi RouОценок пока нет
- Risk For FallsДокумент1 страницаRisk For FallsEugene UC100% (1)
- NCP Delayed Wound RecoveryДокумент5 страницNCP Delayed Wound RecoveryDarkCeades100% (2)
- NCP Impaired Physical MobilityДокумент2 страницыNCP Impaired Physical MobilityDante Sales67% (6)
- NCP Impaired Physical Mobility-2Документ4 страницыNCP Impaired Physical Mobility-2ejoanbОценок пока нет
- NCP FractureДокумент7 страницNCP FractureMacris BondocОценок пока нет
- NCP of Impaired MobilityДокумент3 страницыNCP of Impaired MobilityHazel Cabrera0% (1)
- 217 RF Peripheral Neurovascular DysfunctionДокумент8 страниц217 RF Peripheral Neurovascular Dysfunctionapi-271775750Оценок пока нет
- Clinical Instructor: Mrs. Ramon A. Galicia, RN: Krystlle Lyre G. Cordero 4Bcn San Beda College Nursing Care PlanДокумент4 страницыClinical Instructor: Mrs. Ramon A. Galicia, RN: Krystlle Lyre G. Cordero 4Bcn San Beda College Nursing Care Planstarcordero100% (2)
- Immobility Care Plan For NursesДокумент3 страницыImmobility Care Plan For NursesColleen Murray67% (9)
- NCP Cva Impaired Physical MobilityДокумент2 страницыNCP Cva Impaired Physical MobilityMaricar Azolae Mascual100% (1)
- NCP Activity Intolerance Related To Decreased in Oxygen SupplyДокумент3 страницыNCP Activity Intolerance Related To Decreased in Oxygen SupplyKyle Stephen TancioОценок пока нет
- NCP For Impaired Physical MobilityДокумент2 страницыNCP For Impaired Physical MobilityPrincess Averin Navarro50% (2)
- Impaired Physical Mobility Related To Pain and DiscomfortДокумент2 страницыImpaired Physical Mobility Related To Pain and DiscomfortRis NapolisОценок пока нет
- NCP Activity IntoleranceДокумент2 страницыNCP Activity Intolerancea22hous0% (1)
- NCP FractureДокумент2 страницыNCP Fracturemawel50% (2)
- NCP FractureДокумент1 страницаNCP FractureJonathan Bermundo Barba0% (1)
- NCP For FractureДокумент2 страницыNCP For FractureArnie Jude Carido100% (1)
- Self Care DeficitДокумент2 страницыSelf Care DeficitSj 斗力上75% (4)
- NCP (Actual)Документ2 страницыNCP (Actual)Silinna May Lee SanicoОценок пока нет
- Impaired Physical MobilityДокумент3 страницыImpaired Physical MobilityCalimlim Kim100% (1)
- NCP For Impaired MobilityДокумент4 страницыNCP For Impaired MobilityBettinaFernandoОценок пока нет
- Nursing Care PlanДокумент4 страницыNursing Care Planssairej06100% (3)
- NCP (Ideal) Nursing DiagnosisДокумент2 страницыNCP (Ideal) Nursing DiagnosisSilinna May Lee SanicoОценок пока нет
- Impaired Physical MobilityДокумент2 страницыImpaired Physical MobilityAl-Qadry NurОценок пока нет
- LLB IV Sem GST Unit I Levy and Collection Tax by DR Nisha SharmaДокумент7 страницLLB IV Sem GST Unit I Levy and Collection Tax by DR Nisha Sharmad. CОценок пока нет
- Research Article: Dynamic Modelling of A Solar Water Pumping System With Energy StorageДокумент13 страницResearch Article: Dynamic Modelling of A Solar Water Pumping System With Energy Storagehabtamu melsewОценок пока нет
- ROBONIK - Prietest EasylabДокумент2 страницыROBONIK - Prietest EasylabAlexis Armando Ramos C.Оценок пока нет
- Trandsend 2Документ3 страницыTrandsend 2dadiОценок пока нет
- Portfolio Sandwich Game Lesson PlanДокумент2 страницыPortfolio Sandwich Game Lesson Planapi-252005239Оценок пока нет
- Strategi Meningkatkan Kapasitas Penangkar Benih Padi Sawah (Oriza Sativa L) Dengan Optimalisasi Peran Kelompok TaniДокумент24 страницыStrategi Meningkatkan Kapasitas Penangkar Benih Padi Sawah (Oriza Sativa L) Dengan Optimalisasi Peran Kelompok TaniHilmyTafantoОценок пока нет
- Esp 1904 A - 70 TPH o & M ManualДокумент50 страницEsp 1904 A - 70 TPH o & M Manualpulakjaiswal85Оценок пока нет
- WP05 - ACT 01 - Development 1909Документ53 страницыWP05 - ACT 01 - Development 1909ramesh9966Оценок пока нет
- MBF100 Subject OutlineДокумент2 страницыMBF100 Subject OutlineMARUTI JEWELSОценок пока нет
- DGA Furan AnalysisДокумент42 страницыDGA Furan AnalysisShefian Md Dom100% (10)
- Shape It! SB 1Документ13 страницShape It! SB 1Ass of Fire50% (6)
- VISCOLAM202 D20 Acrylic 20 Thickeners 202017Документ33 страницыVISCOLAM202 D20 Acrylic 20 Thickeners 202017Oswaldo Manuel Ramirez MarinОценок пока нет
- RISO RZ User GuideДокумент112 страницRISO RZ User GuideJojo AritallaОценок пока нет
- S L Dixon Fluid Mechanics and Thermodynamics of TurbomachineryДокумент4 страницыS L Dixon Fluid Mechanics and Thermodynamics of Turbomachinerykuma alemayehuОценок пока нет
- IFE Level 4 Certificate in Fire InvestigationДокумент16 страницIFE Level 4 Certificate in Fire InvestigationMarlon FordeОценок пока нет
- Takeover Strategies and DefencesДокумент20 страницTakeover Strategies and DefencesJithu JoseОценок пока нет
- RELATIVE CLAUSES 1º Bachillerato and KeyДокумент3 страницыRELATIVE CLAUSES 1º Bachillerato and Keyrapitanoroel0% (2)
- France 10-Day ItineraryДокумент3 страницыFrance 10-Day ItineraryYou goabroadОценок пока нет
- AppendixA LaplaceДокумент12 страницAppendixA LaplaceSunny SunОценок пока нет
- CAKUTДокумент50 страницCAKUTsantosh subediОценок пока нет
- Luigi Cherubini Requiem in C MinorДокумент8 страницLuigi Cherubini Requiem in C MinorBen RutjesОценок пока нет
- Trading Book - AGДокумент7 страницTrading Book - AGAnilkumarGopinathanNairОценок пока нет
- Val Ed SyllabusДокумент25 страницVal Ed Syllabusroy piamonteОценок пока нет
- Checklist Code ReviewДокумент2 страницыChecklist Code ReviewTrang Đỗ Thu100% (1)
- PET Formal Letter SamplesДокумент7 страницPET Formal Letter SamplesLe Anh ThuОценок пока нет
- OpenGL in JitterДокумент19 страницOpenGL in JitterjcpsimmonsОценок пока нет
- GP 43-45-DRAFT - Site RestorationДокумент48 страницGP 43-45-DRAFT - Site Restorationmengelito almonte100% (1)
- ALA - Assignment 3 2Документ2 страницыALA - Assignment 3 2Ravi VedicОценок пока нет
- Module No.3 Prepare Architectual Job Requirements Architectural Working DrawingДокумент23 страницыModule No.3 Prepare Architectual Job Requirements Architectural Working DrawingJay S. On100% (1)
- My Report in Assessment 1Документ67 страницMy Report in Assessment 1Eddie Wilson BroquezaОценок пока нет