Академический Документы
Профессиональный Документы
Культура Документы
Factor VIII Inhibitors Complicating Treatment of Postoperative Bleeding in A Dog With Hemophilia A
Загружено:
soledadDC3290 оценок0% нашли этот документ полезным (0 голосов)
22 просмотров5 страницThis case report describes a 7-year-old Japanese Chin dog with moderate hemophilia A (Factor VIII deficiency) that developed circulating Factor VIII inhibitors complicating treatment after dental surgery. Despite presurgical administration of cryoprecipitate, the dog experienced continuous oral bleeding postoperatively. Testing confirmed the presence of Factor VIII inhibitors in the dog's blood. The postoperative hemorrhage was managed with extensive and prolonged blood component transfusions including fresh frozen plasma, cryoprecipitate, and packed red blood cells. The dog had a full clinical recovery after treatment. This report discusses the development and management of Factor VIII inhibitors in canine and human patients with hemophilia A.
Исходное описание:
Оригинальное название
9
Авторское право
© © All Rights Reserved
Доступные форматы
PDF, TXT или читайте онлайн в Scribd
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документThis case report describes a 7-year-old Japanese Chin dog with moderate hemophilia A (Factor VIII deficiency) that developed circulating Factor VIII inhibitors complicating treatment after dental surgery. Despite presurgical administration of cryoprecipitate, the dog experienced continuous oral bleeding postoperatively. Testing confirmed the presence of Factor VIII inhibitors in the dog's blood. The postoperative hemorrhage was managed with extensive and prolonged blood component transfusions including fresh frozen plasma, cryoprecipitate, and packed red blood cells. The dog had a full clinical recovery after treatment. This report discusses the development and management of Factor VIII inhibitors in canine and human patients with hemophilia A.
Авторское право:
© All Rights Reserved
Доступные форматы
Скачайте в формате PDF, TXT или читайте онлайн в Scribd
0 оценок0% нашли этот документ полезным (0 голосов)
22 просмотров5 страницFactor VIII Inhibitors Complicating Treatment of Postoperative Bleeding in A Dog With Hemophilia A
Загружено:
soledadDC329This case report describes a 7-year-old Japanese Chin dog with moderate hemophilia A (Factor VIII deficiency) that developed circulating Factor VIII inhibitors complicating treatment after dental surgery. Despite presurgical administration of cryoprecipitate, the dog experienced continuous oral bleeding postoperatively. Testing confirmed the presence of Factor VIII inhibitors in the dog's blood. The postoperative hemorrhage was managed with extensive and prolonged blood component transfusions including fresh frozen plasma, cryoprecipitate, and packed red blood cells. The dog had a full clinical recovery after treatment. This report discusses the development and management of Factor VIII inhibitors in canine and human patients with hemophilia A.
Авторское право:
© All Rights Reserved
Доступные форматы
Скачайте в формате PDF, TXT или читайте онлайн в Scribd
Вы находитесь на странице: 1из 5
Case Report
Factor VIII inhibitors complicating treatment of
postoperative bleeding in a dog with hemophilia A
Benjamin M. OKelley, DVM, Megan F. Whelan, DVM, DACVECC and Marjory B. Brooks, DVM,
DACVIM
Abstract
Objective To describe the clinical course of a dog with hemophilia A and circulating factor VIII inhibitors
complicating the treatment of postoperative hemorrhage.
Case Summary A 7-year-old castrated male Japanese Chin with hemophilia A, weighing 6 kg, was presented
for dental cleaning, polishing, and extractions. Despite presurgical administration of cryoprecipitate,
continuous oral bleeding occurred. Circulating factor VIII inhibitors were detected, and the postoperative
hemorrhage was subsequently managed with extensive and prolonged blood component transfusion. The dog
was discharged after a full clinical recovery.
New or Unique Information Provided This case report describes the clinical consequences and successful
treatment of postoperative hemorrhage in a dog with hemophilia A and circulating factor VIII inhibitors. A
relevant discussion of the management of human patients with circulating factor VIII inhibitors is included.
(J Vet Emerg Crit Care 2009; 19(4): 381385) doi: 10.1111/j.1476-4431.2009.00437.x
Keywords: coagulopathy, cryoprecipitate, hemostasis, transfusion medicine
Introduction
Hemophilia A is a common X-linked recessive bleeding
disorder caused by a specic deciency of coagulation
factor VIII (FVIII).
1,2
In canine and human patients,
disease severity is classied based on residual FVIII
coagulant activity (FVIII:C).
3,4
Human patients with se-
vere hemophilia (FVIII:Co2%) are at risk for frequent
spontaneous hemorrhage and often require FVIII re-
placement therapy, whereas clinically milder forms are
seen in patients with moderate (FVIII:C525%) or
mild (FVIII:C5620%) hemophilia.
1
The development of inhibitory alloantibodies di-
rected against FVIII represents the most severe compli-
cation of FVIII replacement therapy in humans. Such
antibodies, known as circulating inhibitors, develop in
approximately 2035% of transfusion-dependent pa-
tients with severe hemophilia A.
57
Although less com-
mon, circulating FVIII inhibitors have been described in
humans with mild to moderate hemophilia A.
5
Post-
transfusion alloantibody formation is not unique to
human patients. Inhibitory antibody formation has
been described in a research colony of dogs with se-
vere hemophilia A after transfusion of canine- (and
human-) origin FVIII therapy.
3
Inhibitory alloantibody
formation posttransfusion has also been described in a
Labrador Retriever with severe hemophilia B (factor IX
deciency).
8
In the following report, we describe the
clinical management of high-titer FVIII inhibitors in a
dog with moderate hemophilia A.
Case Summary
A 7-year-old castrated male Japanese Chin, weighing
6 kg, was diagnosed with moderate hemophilia A at a
referral hospital when the dog experienced prolonged
oral bleeding following a dental cleaning. Factor assays
from a coagulation laboratory
a
revealed FVIII de-
ciency (FVIII:C54%; reference interval, 50200%) and
normal Factor IX coagulant activity (FIX:C557%; ref-
erence interval, 50150%). The dogs oral bleeding was
severe enough that his PCV dropped to 22%. He was
treated with canine fresh frozen plasma (FFP) and
packed red blood cell (PRBC) transfusions. Medical re-
cords indicate that the oral bleeding initially stopped
Address correspondence and reprint requests to
Dr. Benjamin M. OKelley, Department of Emergency and Critical Care,
Angell Animal Medical Center, 350 South Huntington Avenue, Jamaica
Plain, Boston, MA 02130, USA.
Email: bokelley@mspca.org
From the Department of Emergency and Critical Care, Angell Animal
Medical Center, Boston, MA 02130 (OKelley, Whelan) and the Department
of Population Medicine and Diagnostic Sciences, College of Veterinary
Medicine, Cornell University, Ithaca, NY 14853, USA (Brooks).
Journal of Veterinary Emergency and Critical Care 19(4) 2009, pp 381385
doi:10.1111/j.1476-4431.2009.00437.x
& Veterinary Emergency and Critical Care Society 2009 381
following a single 20 mL/kg FFP transfusion, but the
dog had to be readmitted 72 hours later for recurrent
bleeding and symptomatic anemia; PCV was 13% at
that time. He was given PRBCs and approximately
40 mL/kg canine FFP; the oral bleeding stopped, with
no rebleeding at that time.
Nearly 2 years later, the dog presented to a different
referral hospital for a second dental evaluation and treat-
ment of periodontal disease. The clients perspective was
that the periodontal disease was severe enough that it
adversely affected the dogs quality of life. Physical ex-
amination was normal with the exception of severe den-
tal abnormalities. The prothrombin time was 6.7 seconds
(reference, 7.311.8 s); the activated partial thromboplas-
tin time (APTT) was 25.1 seconds (reference, o14.8 s).
Platelet count and brin split products were within nor-
mal limits. The PCV was 51%; total protein (TP) was
82 g/L (8.2 g/dL). Blood type was dog erythrocyte anti-
gen (DEA) 1.1 positive. Because of the dogs known his-
tory of hemophilia A and an anticipated need for dental
surgery, 1U (8mL/kg) of canine cryoprecipitate obtained
from a commercial blood bank
b
was administered.
An anesthetized oral examination revealed that gingi-
vitis, gingival recession, dental calculus, and periodontal
pocketing were present in varying degrees in all remain-
ing teeth. Several teeth showed abnormal mobility. A total
of 15 teeth were extracted; the remaining teeth were
scaled and polished. Postoperatively, a cold compress was
applied to the gingival incisions and an absorbable gelatin
sponge
c
was packed into an area of the gums where slight
bleeding had occurred intraoperatively. The dogs initial
recovery from anesthesia was without complication.
The following day, minimal oral bleeding was noted;
PCV initially dropped to 36%. Twelve hours later, the
PCV was 38% and the dog was bright, alert, and re-
sponsive with a normal heart rate. APTT, measured on
a point-of-care coagulation monitor,
d
was 110 seconds
(reference, 8797 s). The dog was discharged from the
hospital, but developed oral bleeding at home 48 hours
later, and was readmitted to the hospital. Mucosal su-
tures were observed to be intact, but a large soft blood
clot was present surrounding the right upper canine,
and blood was slowly but continuously oozing from
this area of the gums. One unit of FFP (45 mL/kg), col-
lected from a DEA 1.1 positive donor, was given over 4
hours. When the oral bleeding was still present the fol-
lowing morning, APTT was rechecked; it was severely
prolonged at 128 seconds (reference, o14.8 s). PCV was
24%; TP was 58 g/L (5.8 g/dL). One unit of cryopre-
cipitate (11 mL/kg) was given over 3 hours.
The next morning, the APTT was 21.3 seconds, and
PCV was 15%. One unit of cryoprecipitate (10 mL/kg)
was given over 3 hours, and DEA 1.1 positive, cross-
matched PRBCs (10 mL/kg) were administered over 3
hours. When oral bleeding continued, more FFP (20 mL/
kg) and DEA 1.1 positive, cross-matched PRBCs (10 mL/
kg) were administered. APTT, measured on a point-of-
care monitor,
d
was 127 seconds (reference, o97 s). After
another unit of cryoprecipitate (11 mL/kg) was given
over 4 hours, the oral bleeding nally subsided. PCV
was 33% and the dogs heart rate, mucous membrane
color, and capillary rell time were all within normal
limits. He was discharged from the hospital at that time.
Because of the unexpectedly high transfusion re-
quirements and extended time interval required to stop
the bleeding, the development of FVIII inhibitors was
suspected. A citrated plasma sample (prepared from
blood drawn into 1/10th volume of 3.8% sodium ci-
trate) was shipped overnight on cold packs to a referral
laboratory
a
for coagulation inhibitor testing. Factor VIII
coagulant activity was measured in a modied 1-stage
APTT assay, as described previously.
9
A screening test
to detect FVIII inhibition
10
was performed by measur-
ing the FVIII:C of an incubation mixture consisting of
equal parts patient plasma and pooled canine control
plasma (prepared from 20 healthy dogs). The results of
these analyses revealed severe FVIII deciency in the
patients baseline sample (FVIII:C51.5%) and a lack of
detectable FVIII activity (FVIII:Co1%) in the patient/
control plasma mixture. These ndings were compat-
ible with the presence of FVIII inhibitory activity in the
patient plasma. The activity was quantied using the
Bethesda assay method.
11
In brief, serial dilutions of the
patient plasma were combined in a 1:1 ratio with
pooled canine control plasma and incubated at 371C.
The residual FVIII:C of the incubation mixtures were
assayed and compared with the FVIII:C of pooled con-
trol plasma combined 1:1 with saline. In this assay, the
dilution of patient plasma containing residual FVIII:C
of 50% represents 1 Bethesda Unit (BU) per milliliter of
inhibitory activity. The Bethesda assay results revealed
a high titer inhibitor of 4256 BU/mL in the dogs
plasma at the time of his discharge.
Two weeks later, a recheck physical examination in-
dicated the oral surgery sites were healed; no oral
bleeding was observed. The client reported that the dog
was eating well at home and had regained a normal
energy and activity level. PCV was 42%, TP was 70 g/L
(7.0 g/dL). Citrated plasma was again submitted for
FVIII:C and Bethesda inhibitory activity determina-
tions. Assay results of the newly drawn sample re-
vealed severe FVIII deciency (FVIII:C51.5%) and
persistent high-titer FVIII inhibitors (4256 BU/mL).
Discussion
Factor VIII is a nonenzymatic glycoprotein coagulation
factor that circulates in plasma bound noncovalently to
& Veterinary Emergency and Critical Care Society 2009, doi: 10.1111/j.1476-4431.2009.00437.x 382
B.M. OKelley et al.
von Willebrand factor (vWf).
12,13
This association with
vWf both stabilizes the procoagulant activity of FVIII
and prolongs its circulation by decreasing the rate of
clearance of FVIII from the plasma and protecting it
from proteolysis by factors IIa, Xa, and activated pro-
tein C.
7,12,13
Patients with hemophilia A have genetic
mutations resulting in signicantly decreased or absent
FVIII:C. These mutations display genetic heterogeneity
that translates into phenotypic heterogeneity. For ex-
ample, humans with FVIII gene inversion produce no
FVIII and are severely affected, while those with point
mutations typically have quantitative or functional pro-
tein defects that result in relatively mild to moderate
forms of hemophilia.
1
The variability in FVIII gene
mutations has also been shown to inuence the likeli-
hood of circulating FVIII inhibitor development.
7
While the exact mechanisms of alloimmunization in
response to FVIII administration have not been fully
dened, FVIII inhibitors develop most frequently in
patients with severe hemophilia A.
57
Patients with se-
vere hemophilia typically require repeated administra-
tion of exogenous FVIII to prevent or control recurrent
hemorrhage. In most of these patients, the lack of func-
tional FVIII results from inactivating mutations that
abolish FVIII protein synthesis. In the absence of circu-
lating endogenous FVIII antigen, transfused FVIII is
presumably recognized by the patients immune sys-
tem as a foreign protein.
57
There also appears to be a
genetic component of inhibitor development unrelated
to the severity of hemophilia. A familial predisposition
is supported by an observed increase in alloimmuni-
zation among rst- and second-degree relatives of hu-
man patients with mild to moderate hemophilia who
have developed FVIII inhibitors.
5
The degree of hemostatic dysfunction resulting from
the formation of FVIII alloantibodies depends on a
number of factors, including epitope specicity and
antibody titer.
6
Many inhibitory antibodies bind to
functionally important domains of FVIII, interfering
with its interaction with other coagulation factors or
platelet phospholipids.
7
Other antibodies accelerate
FVIII clearance (due to impaired vWF-binding) or en-
hance its proteolysis. Although clinically silent, many
human hemophiliac patients develop non-neutralizing
FVIII alloantibodies after transfusion.
6
The medical management of FVIII inhibitors consists
of short-term measures to control bleeding episodes
and long-term approaches to modulate the immune re-
sponse. Potential treatments for active hemorrhage in-
clude high-volume plasma-derived or recombinant
FVIII concentrates, porcine FVIII, FVIII bypassing
agents, antibrinolytics, local hemostatic agents (such
as absorbable gelatin sponges), and cold compresses.
Human patients with posttransfusion antibody titers of
5 BU/mL are considered low responders and suitable
candidates for high-volume FVIII administration strat-
egies.
7,14,15
In these patients, administration of larger or
more frequent amounts of exogenous FVIII may satu-
rate existing antibodies, providing sufcient free FVIII
for adequate hemostasis. The amino acid sequence of
porcine FVIII is sufciently different from the human
protein to reduce its immunoreactivity, thereby pro-
longing the half-life of transfused porcine FVIII. Porcine
FVIII is currently unavailable, however, due to con-
tamination of plasma-derived products with endo-
genous porcine viruses.
16
Clinical trials are evaluating
recombinant porcine FVIII as an alternative with no risk
of pathogen transmission.
Acceptable sources of plasma-derived FVIII for the
treatment of hemophilia A include FFP and cryoprecip-
itate. Cryoprecipitate is the treatment of choice because
adverse reactions to cryoprecipitate appear to be less
common than similar reactions to FFP.
2
The volume of
FFP necessary to provide adequate exogenous FVIII
may be very large, adding a risk for uid overload. The
patient of this report received both FFP and cryopre-
cipitate; optimally, only cryoprecipitate would have
been used to decrease the risk of uid overload.
Antibrinolytic agents such as the lysine analogs ep-
silon-aminocaproic acid and tranexamic acid (TEA)
bind plasminogen, preventing its activation to plasmin
and resulting in reduced brinolysis. These agents can
be administered systemically or applied locally, and can
be especially useful following dental procedures. TEA
mouthwash, for example, has proven to be as effective
as FVIII replacement in controlling gingival hemor-
rhage in hemophiliac humans following dental scal-
ing.
17
Although epsilon-aminocaproic acid and TEA
have been used in dogs, their efcacy in controlling
hemorrhage in canine hemophiliac patients with inhib-
itors remains unknown.
Some human patients with mild hemophilia develop
FVIII inhibitors that react only with exogenous FVIII,
sparing endogenous FVIII. Desmopressin (1desamino-
8-arginine vasopressin, DDAVP) may be effective in
these patients by stimulating release of stored FVIII.
16
While the effects of DDAVP administration to dogs
with FVIII inhibitors have not been described, admin-
istration of 0.45.0 mg/kg DDAVP subcutaneously to
dogs with hemophilia A produced no substantial
changes in FVIII activity in 1 study.
18
If high-dose FVIII replacement is ineffective or not
feasible, so-called bypass therapy may be used. Bypass
therapy involves administering agents that allow for
successful clot formation in the absence of properly
functioning FVIII. The rst available bypass agents
were plasma-derived, activated prothrombin complex
concentrates. More recently, recombinant activated
& Veterinary Emergency and Critical Care Society 2009, doi: 10.1111/j.1476-4431.2009.00437.x 383
FVIII inhibitors in a dog with hemophilia A
human factor VII (rhFVIIa) has proven effective as a
bypass agent for controlling hemorrhage in human hemo-
philiacs with high-titer inhibitors.
15
Experimentally, infu-
sion of rhFVIIa normalized the bleeding tendency of dogs
with hemophilia A (measured by a secondary toenail
bleeding time previously demonstrated to be abnormally
prolonged in these patients).
19
Recombinant rhFVIIa ad-
ministration was, however, highly immunogenic; it trig-
gered an immediate urticarial response in 4 of the 5 dogs
who received it, and all 5 dogs developed measureable
antibodies against FVIIa.
An obvious concern with the use of bypass therapies
is thromboembolic events caused by excessive proco-
agulant activity, but the incidence of such thrombotic
events post-rhFVIIa administration in human hemo-
philia patients is low.
15
The risk of thromboembolic
complications may be higher when bypass therapy and
antibrinolytic agents are used concurrently; this risk
must be weighed when considering coadministration of
these therapies to treat severe hemorrhage.
20
Immunomodulatory approaches to the long-term
management of coagulation inhibitors aim to eliminate
antibodies using immunoadsorbtion or chemotherapy
and immune tolerance induction (ITI) through sus-
tained exposure to high-dose FVIII. ITI may be suc-
cessful in eradicating inhibitors up to 80% of human
patients with severe hemophilia A,
7
but the exceedingly
high costs and limited availability of recombinant FVIII
products prohibit ITI from being a realistic option for
veterinary patients at this time.
While the development and clinical management of
FVIII inhibitory antibodies is well characterized in the
human medical literature, FVIII inhibitors have only
been described in a single research colony of dogs with
severe hemophilia A.
3
These dogs were all derived
from 1 hemophilic Schnauzer sire, with inhibitor for-
mation noted in the descendents of a single outcross
female. Inhibitory antibodies in the affected dogs were
classied as IgG, and cross-reacted with human and
canine FVIII. When the affected dogs and their relatives
were observed over a 10-year period, they demon-
strated similar clinical features as human patients with
inhibitors: transfusion resistance, heterogeneity of in-
hibitor expression between individuals and for a single
individual over time, and initial response to porcine
FVIII followed by development of anti-porcine cross-
reactive antibodies.
21
The development of FVIII inhibitory antibodies was
suspected in the Japanese Chin reported here because
of his failure to respond to appropriate transfusion
therapy. Recommended FFP dosages for treating canine
hemophiliac patients typically begin at 610 mL/kg,
and recommended cryoprecipitate doses start at 1
2 mL/kg for such patients.
2,22
The volume of FFP
needed to stop clinically relevant hemorrhage varies
greatly among patients due to varying disease severity
(FVIII:C levels) among patients and varying FVIII:C
activity per unit volume of FFP.
2,22
In 1 study, FFP was
administered to 4 dogs with mild to moderate hemo-
philia A.
2
The plasma was given at a volume of 1 U
(250300 mL)/15 kg body weight, and FVIII:C activity
was tracked over time. Only 3 of the 4 dogs reached
FVIII:C activities deemed likely to stop clinical hemor-
rhage based on previous studies correlating FVIII:C ac-
tivity with cuticle bleeding time. The dog who did not
reach an ideal FVIII:C was not screened for FVIII in-
hibitors, but the authors hypothesized that the presence
of low-titer anti-FVIII antibodies could have been re-
sponsible for this dogs lack of response to FFP.
During the period of hospitalization described in this
report, the Japanese Chin required a larger cumulative
volume and more prolonged course of transfusion to
control hemorrhage than after his initial dentistry. It is
possible that re-exposure to canine FVIII induced an
anamnestic response in this dog. The medical classica-
tion of high responder describes hemophilic patients
that mount a robust immune response and rapid rise in
FVIII inhibitor titer after FVIII replacement therapy. This
patients high-titer inhibitor (4256 BU/mL) posttrans-
fusion is compatible with a high-responder classication.
The large volume of blood products (65 mL/kg of
FFP and 40 mL/kg of cryoprecipitate) required to stop
hemorrhage in this dog parallels reports in the human
literature and highlights the difculty of controlling
active hemorrhage in high-responder hemophiliacs. In-
fusion of porcine FVIII or rhFVIIa was considered for
this patient but the high cost, immunogenicity, and rel-
ative unavailability of these products lead to the deci-
sion to attempt high-volume transfusion. The goal of
this approach was to administer enough exogenous
FVIII to neutralize existing antibodies long enough to
allow the patients oral wounds to heal. The patients
small body size made it possible to give him large
amounts of cryoprecipitate and FFP (on a mL/kg basis)
without being cost prohibitive to his owners or deplet-
ing the hospitals supply of these blood products. Re-
peated application of a cold compress or local
hemostatic agents (such as epinephrine or gelatin
sponges) to the bleeding gums would have been use-
ful for controlling hemorrhage in this patient, but se-
dation would have been needed because the patient
was intolerant of these procedures. If bleeding contin-
ued despite these treatments, local or systemic anti-
brinolytic administration may have been useful.
Bypass therapy with rhFVIIa could have been consid-
ered if the bleeding became life threatening.
While apparently uncommon, canine hemophilia pa-
tients are at risk for immunologic transfusion reactions.
& Veterinary Emergency and Critical Care Society 2009, doi: 10.1111/j.1476-4431.2009.00437.x 384
B.M. OKelley et al.
In addition to reports of coagulation inhibitors, alloanti-
bodies directed against platelet antigens have been de-
scribed in a German Shepherd with hemophilia A.
23
Hemophilic dogs that experience continuing hemorrhage
despite cryoprecipitate or FFP transfusion should be
screened to detect thrombocytopenia or FVIII inhibitors.
It is possible that the hemorrhage and subsequent
need for PRBC transfusions could have been avoided in
the dog of this report if the inhibitors had been detected
by appropriate preoperative screening. Before elective
surgery, dogs with known hemophilia and a history of
exogenous FVIII administration should be tested to as-
sess their present FVIII:C level and check for the pres-
ence of coagulation inhibitors. Clear endpoints to
transfusion therapy should be met before any surgical
procedure; normalization of the APTT or normalization
of a modied toenail bleeding time should occur in re-
sponse to adequate FVIII replacement. If clotting times
do not normalize, or if inhibitors are detected before
surgery, the necessity of the procedure should be care-
fully evaluated. Appropriate treatments, including anti-
brinolytics, large volumes of cryoprecipitate, and
bypass therapies should be available before proceed-
ing with an elective procedure in these patients.
Acknowledgements
The authors thank Dr. Bill Rosenblad for performing
the dental assessment, cleaning, polishing, and extrac-
tions. The authors also thank Dr. Tamara Kremer-
Mecabell and Dr. Chris Rollings for their clinical input
and assistance with case management.
Footnotes
a
Comparative Coagulation Section, Animal Health Diagnostic Center,
Cornell University, Ithaca, NY.
b
Midwest Animal Blood Services, Stockbridge, MI.
c
Gelfoam. Pzer, New York, NY.
d
SCA 2000. Synbiotics Corporation, San Diego, CA.
References
1. Brooks MB, Barnas JL, Fremont J, et al. Cosegregation of a factor
VIII microsatellite marker with mild hemophilia A in Golden
Retriever dogs. J Vet Intern Med 2005; 19(2):205210.
2. Stokol T, Parry BW. Efcacy of fresh-frozen plasma and cryopre-
cipitate in dogs with von Willebrands disease or hemophilia
A. J Vet Intern Med 1998; 12(2):8492.
3. Giles AR, Tinlin S, Hoogendoorn H, et al. Development of factor
VIII: C antibodies in dogs with hemophilia A (factor VIII:C de-
ciency). Blood 1984; 63:451456.
4. Giles AR, Tinlin S, Hoogendoorn H, et al. In vivo characterization
of recombinant factor VIII in a canine model of hemophilia A
(factor VIII deciency). Blood 1988; 72:335339.
5. Hay CRM, Ludlam CA, Colvin BT, et al. Factor VIII inhibitors in
mild and moderate-severity haemophilia A. Thromb Haemost
1998; 79:762766.
6. Reding MT. Immunological aspects of inhibitor development.
Haemophilia 2006; 12(suppl 6):3036.
7. Reipert BM, van den Helden PMW, Schwarz H-P, et al. Mecha-
nisms of action of immune tolerance induction against factor VIII
in patients with congenital haemophilia A and factor VIII inhib-
itors. Br J Haematol 2006; 136(1):1225.
8. Brooks MB, Gu W, Ray K. Complete deletion of factor IX gene and
inhibition of factor IX activity in a Labrador retriever with hemo-
philia B. J Am Vet Med Assoc 1997; 211(11):14181421.
9. Stokol T, Brooks MB, Erb HN. Effect of citrate concentration on
coagulation test results in dogs. J Am Vet Med Assoc 2000;
217(11):16721677.
10. Triplett DA, Harms CS. Factor assays, In: Triplett DA. ed. Proce-
dures for the Coagulation Laboratory. Chicago: American Society
of Clinical Pathologists Press; 1981, pp. 3857.
11. Kasper CK, Aledort L, Aronson D, et al. Proceedings: a more uni-
form measurement of factor VIII inhibitors. Thromb Diath Ha-
emorrh 1975; 34(2):612.
12. Rock G, Adamkiewicz T, Blanchette V, et al. Acquired von Wille-
brand factor deciency during high-dose infusion of recombinant
factor VIII. Br J Haematol 1996; 93(3):684687.
13. Topper MJ, Welles EG. Hemostasis, In: Latimer KS, Mahaffey EA,
Prasse KW. eds. Veterinary Laboratory Medicine: Clinical Pathol-
ogy, 4th ed. Ames: Iowa State Press; 2003, pp. 99135.
14. Morni M, Auerswald G, Kobelt RA, et al. Prophylactic treatment
of haemophilia patients with inhibitors: clinical experience with
recombinant factor VIIa in European Haemophilia Centres. Hae-
mophilia 2007; 13(5):502507.
15. Kraut EH, Aledort LM, Arkin S, et al. Surgical interventions in
a cohort of patients with haemophilia A and inhibitors: an
experiential retrospective chart review. Haemophilia 2007; 13(5):
508517.
16. Haya S, Moret A, Cid AR, et al. Inhibitors in haemophilia A: cur-
rent management and open issues. Haemophilia 2007; 13(suppl 5):
5260.
17. Lee AP, Boyle CE, Savidge GF, et al. Effectiveness in controlling
haemorrhage after dental scaling in people with haemophilia by
using tranexamic acid mouthwash. Br Dent J 2005; 198(1):3338.
18. Mansell PD, Parry BW. Changes in factor VIII: coagulant activity
and von Willebrand factor antigen concentration after subcutane-
ous injection of desmopressin in dogs with mild hemophilia A.
J Vet Int Med 1991; 5(3):191194.
19. Brinkhous KM, Hedner U, Garris JB, et al. Effect of recombinant
factor VIIa on the hemostatic defect in dogs with hemophilia A,
hemophilia B, and von Willebrand disease. Proc Natl Acad Sci U S
A 1989; 86(4):13821386.
20. Teitel J, Berntorp E, Collins P, et al. A systematic approach to
controlling problem bleeds in patients with severe congenital hae-
mophilia and high-titre inhibitors. Haemophilia 2007; 13(3):256
263.
21. Tinlin S, Webster S, Giles AR. The development of homologous
(canine/anti-canine) antibodies in dogs with haemophilia A (fac-
tor VIII deciency): a ten-year longitudinal study. Thromb Hae-
most 1993; 69(1):214.
22. Giger Urs. Transfusion medicine, In: Silverstein DC, Hopper K.
eds. Small Animal Critical Care Medicine. St Louis: Saunders
Elsevier; 2009, pp. 281287.
23. Wardrop KJ, Lewis D, Marks S, et al. Posttransfusion purpura in a
dog with hemophilia A. J Vet Int Med 1997; 11(4):261263.
& Veterinary Emergency and Critical Care Society 2009, doi: 10.1111/j.1476-4431.2009.00437.x 385
FVIII inhibitors in a dog with hemophilia A
Вам также может понравиться
- Blood ProductsДокумент41 страницаBlood ProductsrijjorajooОценок пока нет
- Diabetes InsipidusДокумент10 страницDiabetes InsipidussoniaОценок пока нет
- Canine and Feline Endocrinology PDFДокумент685 страницCanine and Feline Endocrinology PDFSandra Solano100% (8)
- NBME 1 RatioДокумент87 страницNBME 1 RatioBugs Caslib100% (1)
- Practical Guide to Equine ColicОт EverandPractical Guide to Equine ColicLouise L. SouthwoodОценок пока нет
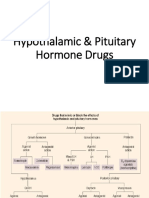
- Hypothalamic & Pituitary Hormone DrugsДокумент29 страницHypothalamic & Pituitary Hormone DrugsDylan MansillaОценок пока нет
- HemophiliaДокумент20 страницHemophiliamuhirwa SamuelОценок пока нет
- NCM 116 Endocrine DisordersДокумент106 страницNCM 116 Endocrine DisordersAnthony Seth AguilandoОценок пока нет
- Bed WettingДокумент5 страницBed WettingLeah ValenciaОценок пока нет
- Blood DisordersДокумент75 страницBlood DisordersmatrixtrinityОценок пока нет
- Diabetes InsipidusДокумент8 страницDiabetes InsipidusNader Smadi100% (5)
- Veterinary Internal Medicne - 2008 - Buechner Maxwell - Neonatal Alloimmune Thrombocytopenia in A Quarter Horse FoalДокумент5 страницVeterinary Internal Medicne - 2008 - Buechner Maxwell - Neonatal Alloimmune Thrombocytopenia in A Quarter Horse FoallucascotaОценок пока нет
- 10 Transfusion GatosДокумент4 страницы10 Transfusion GatosJoce MaripanguiОценок пока нет
- Xenotransfusion of Canine Blood To A CatДокумент3 страницыXenotransfusion of Canine Blood To A CatFelipe GonzalezОценок пока нет
- Cardiovascular Parameter in A Mixed-Sex Swine Study of Severe Dcs Sickness Treated With The Emulsified Perfluorocarbon OxycyteДокумент9 страницCardiovascular Parameter in A Mixed-Sex Swine Study of Severe Dcs Sickness Treated With The Emulsified Perfluorocarbon OxycyteVenansius Ratno KurniawanОценок пока нет
- Acute Isovolemic Anemia Impairs Central Processing As Determined by P300 LatencyДокумент5 страницAcute Isovolemic Anemia Impairs Central Processing As Determined by P300 LatencyNanggala Putra RahandaОценок пока нет
- Extraction of FourДокумент3 страницыExtraction of FourBulfendri DoniОценок пока нет
- Suspected Relative Adrenal Insufficiency in A Critically Ill CatДокумент5 страницSuspected Relative Adrenal Insufficiency in A Critically Ill CatdenisegmeloОценок пока нет
- Fluir Ressuscitation Dogs 21-02-2013Документ8 страницFluir Ressuscitation Dogs 21-02-2013Líria HiranoОценок пока нет
- Jurnalreading PDFДокумент4 страницыJurnalreading PDFninja satuОценок пока нет
- Aronson 2016Документ26 страницAronson 2016Alba Rocio Zavala MoyaОценок пока нет
- Vet Record Case Reports - 2022 - Crosby - Severe Thrombocytopenia Due To Subinvolution of Placental Sites in A MalteseДокумент4 страницыVet Record Case Reports - 2022 - Crosby - Severe Thrombocytopenia Due To Subinvolution of Placental Sites in A MalteseDeana Laura SanchezОценок пока нет
- Sobrecarga de Fluidos RetrospectivoДокумент9 страницSobrecarga de Fluidos RetrospectivoFelipe GonzalezОценок пока нет
- Blood Transfusions in Small Animal MedicineДокумент15 страницBlood Transfusions in Small Animal MedicineMirel YdianОценок пока нет
- Haemophilia: Diana S PurwantoДокумент6 страницHaemophilia: Diana S Purwantofadia nauraОценок пока нет
- Acquired Hemophilia A Presenting in An Elderly Man: Teaching Case ReportДокумент2 страницыAcquired Hemophilia A Presenting in An Elderly Man: Teaching Case ReportvishnupgiОценок пока нет
- Xenotransfusion of Canine Blood To Cats: A Review of 49 Cases and Their OutcomeДокумент7 страницXenotransfusion of Canine Blood To Cats: A Review of 49 Cases and Their OutcomeManuel DiazОценок пока нет
- UntitledДокумент15 страницUntitledMirel YdianОценок пока нет
- J Clin Apher 2020 Sep 17 Chuliber FaДокумент8 страницJ Clin Apher 2020 Sep 17 Chuliber FaFernando SousaОценок пока нет
- Small Animal Transfusion Medicine - 2020 - VSPДокумент12 страницSmall Animal Transfusion Medicine - 2020 - VSPTactvisОценок пока нет
- Out 2Документ9 страницOut 2mokhamad rizkiОценок пока нет
- Small Volume Resuscitation With 20 Albumin in Intensive Care Physiological EffectsДокумент10 страницSmall Volume Resuscitation With 20 Albumin in Intensive Care Physiological EffectsDr. Prashant KumarОценок пока нет
- Amylase and Lipase Detection in Hemorrhaged Animals Treated With HBOC-201Документ8 страницAmylase and Lipase Detection in Hemorrhaged Animals Treated With HBOC-201István PortörőОценок пока нет
- Red Cell Transfusion: Blood Transfusion and The AnaesthetistДокумент20 страницRed Cell Transfusion: Blood Transfusion and The AnaesthetistDesi OktarianaОценок пока нет
- Crim Em2013-948071Документ2 страницыCrim Em2013-948071m.fahimsharifiОценок пока нет
- Criopp 2014 BJAДокумент13 страницCriopp 2014 BJARaluca GoiceaОценок пока нет
- Case Report: Surgical Removal of A Canine Aortic Thromboembolism Secondary To PancreatitisДокумент8 страницCase Report: Surgical Removal of A Canine Aortic Thromboembolism Secondary To PancreatitisIvan RisnaОценок пока нет
- Blood TransfusionДокумент4 страницыBlood TransfusionSherineBelzaОценок пока нет
- A Woman With Sporadic Hemophilia-B Die Because of Cerebral Bleeding: A Rare Case in Bali-IndonesiaДокумент7 страницA Woman With Sporadic Hemophilia-B Die Because of Cerebral Bleeding: A Rare Case in Bali-IndonesiaKholifatur RohmaОценок пока нет
- Up-Regulation of Platelet Activation in Hemophilia AДокумент8 страницUp-Regulation of Platelet Activation in Hemophilia AUtari UbОценок пока нет
- Buhles 1974Документ12 страницBuhles 1974Paula Andrea Castro MartinezОценок пока нет
- Characteristics of Hemostasis During Experimental Ehrlichia Canis InfectionДокумент9 страницCharacteristics of Hemostasis During Experimental Ehrlichia Canis InfectionDiana Granada100% (1)
- Case Report: Hyperhemolysis Syndrome Without Underlying Hematologic DiseaseДокумент4 страницыCase Report: Hyperhemolysis Syndrome Without Underlying Hematologic DiseaseEliana LopezОценок пока нет
- Anes MNGMT Ped TraumaДокумент5 страницAnes MNGMT Ped Traumaramzi MohamedОценок пока нет
- Hipertensión PortalДокумент5 страницHipertensión PortalJose Manuel Garcia RuedaОценок пока нет
- Livnat 2009Документ6 страницLivnat 2009Eugenio Daniel Martinez HurtadoОценок пока нет
- New England Journal Medicine: The ofДокумент12 страницNew England Journal Medicine: The ofNut RonakritОценок пока нет
- V. Oral PresentationsДокумент29 страницV. Oral PresentationsIstván PortörőОценок пока нет
- Javma 237 3 299Документ5 страницJavma 237 3 299tcvhОценок пока нет
- Hypokalemic Paralysis PDFДокумент4 страницыHypokalemic Paralysis PDFAndhy IndriyonoОценок пока нет
- Hypovitaminosis D Is Associated With Negative Outcome in Dogs With Protein Losing Enteropathy: A Retrospective Study of 43 Cases - Allenspach 2017Документ6 страницHypovitaminosis D Is Associated With Negative Outcome in Dogs With Protein Losing Enteropathy: A Retrospective Study of 43 Cases - Allenspach 2017acolpoОценок пока нет
- Rapid Publication: Sickle CellДокумент5 страницRapid Publication: Sickle CellVibhav SinghОценок пока нет
- Hyperbaric Oxygen Therapy For Cyclophosphamide-Induced Intractable Refractory Hemorrhagic Cystitis in A Systemic Lupus Erythematosus PatientДокумент3 страницыHyperbaric Oxygen Therapy For Cyclophosphamide-Induced Intractable Refractory Hemorrhagic Cystitis in A Systemic Lupus Erythematosus PatientFahmee MujaheedОценок пока нет
- Jha2 2 118Документ3 страницыJha2 2 118Renato DantasОценок пока нет
- A Case Report - A Dog With Acute Onset of Hepatozoon Canis InfectionДокумент4 страницыA Case Report - A Dog With Acute Onset of Hepatozoon Canis InfectionSivapong VsmuОценок пока нет
- ACVIM Consensus Statement On The Diagnosis and TreatmentДокумент28 страницACVIM Consensus Statement On The Diagnosis and TreatmentBê LagoОценок пока нет
- Ariculo MauДокумент2 страницыAriculo MauMerpi Alvarez GorisОценок пока нет
- Hemoperitoneum in CAPD, A Red FlagДокумент6 страницHemoperitoneum in CAPD, A Red FlagBhanu KumarОценок пока нет
- The Effect of Hetastarch (670/0.75) in Vivo On Platelet Closure Time in The DogДокумент6 страницThe Effect of Hetastarch (670/0.75) in Vivo On Platelet Closure Time in The DogsoledadDC329Оценок пока нет
- VetSurg - 2021 Simpson - Cholecystectomy in 23 Cats 2005-2021Документ8 страницVetSurg - 2021 Simpson - Cholecystectomy in 23 Cats 2005-2021Silvia RoseОценок пока нет
- J Physiol-2006-Bletsa-225-36Документ12 страницJ Physiol-2006-Bletsa-225-36Nadya PurwantyОценок пока нет
- Case ReportДокумент3 страницыCase ReportDario Mendoza RodriguezОценок пока нет
- 17TOHJДокумент4 страницы17TOHJAriffa DiazОценок пока нет
- Article Casey LIVER Hepatic CirrhosisДокумент8 страницArticle Casey LIVER Hepatic CirrhosisMaría José Muñoz PalaciosОценок пока нет
- Case Report: Acute Warfarin Toxicity As Initial Manifestation of Metastatic Liver DiseaseДокумент7 страницCase Report: Acute Warfarin Toxicity As Initial Manifestation of Metastatic Liver DiseaseAndrexixОценок пока нет
- Pandemic H1N1 Influenza A Viral Infection Complicated by Atypical Hemolytic Uremic Syndrome and Diffuse Alveolar HemorrhageДокумент5 страницPandemic H1N1 Influenza A Viral Infection Complicated by Atypical Hemolytic Uremic Syndrome and Diffuse Alveolar HemorrhageDavidОценок пока нет
- Use of Thromboelastography in Dogs With Immune-Mediated Hemolytic Anemia: 39 Cases (2000 2008)Документ5 страницUse of Thromboelastography in Dogs With Immune-Mediated Hemolytic Anemia: 39 Cases (2000 2008)soledadDC329Оценок пока нет
- The Effect of Hetastarch (670/0.75) in Vivo On Platelet Closure Time in The DogДокумент6 страницThe Effect of Hetastarch (670/0.75) in Vivo On Platelet Closure Time in The DogsoledadDC329Оценок пока нет
- Noninvasive Ventilation in Cats: Original StudyДокумент10 страницNoninvasive Ventilation in Cats: Original StudysoledadDC329Оценок пока нет
- 6Документ8 страниц6soledadDC329Оценок пока нет
- Evaluation of Fresh Frozen Plasma Administration in Dogs With Pancreatitis: 77 Cases (1995 2005)Документ6 страницEvaluation of Fresh Frozen Plasma Administration in Dogs With Pancreatitis: 77 Cases (1995 2005)soledadDC329Оценок пока нет
- A Comparison of Total Calcium, Corrected Calcium, and Ionized Calcium Concentrations As Indicators of Calcium Homeostasis Among Hypoalbuminemic Dogs Requiring Intensive CareДокумент8 страницA Comparison of Total Calcium, Corrected Calcium, and Ionized Calcium Concentrations As Indicators of Calcium Homeostasis Among Hypoalbuminemic Dogs Requiring Intensive CaresoledadDC329Оценок пока нет
- 3Документ7 страниц3soledadDC329Оценок пока нет
- Brown Recluse Spider Envenomation in Small Animals: Loxosceles ReclusaДокумент8 страницBrown Recluse Spider Envenomation in Small Animals: Loxosceles ReclusasoledadDC329Оценок пока нет
- Nasogastric Tube Feeding in Cats With Suspected Acute Pancreatitis: 55 Cases (2001 2006)Документ10 страницNasogastric Tube Feeding in Cats With Suspected Acute Pancreatitis: 55 Cases (2001 2006)soledadDC329Оценок пока нет
- Endoscopically Guided Nasojejunal Tube Placement in Dogs For Short-Term Postduodenal FeedingДокумент10 страницEndoscopically Guided Nasojejunal Tube Placement in Dogs For Short-Term Postduodenal FeedingsoledadDC329Оценок пока нет
- Infectious Diseases of The Dog and Cat, 3rd Edition: CHAPTER 82 Cryptosporidiosis and CyclosporiasisДокумент16 страницInfectious Diseases of The Dog and Cat, 3rd Edition: CHAPTER 82 Cryptosporidiosis and CyclosporiasissoledadDC329Оценок пока нет
- Infectious Diseases of The Dog and Cat, 3rd Edition: CHAPTER 73 LeishmaniasesДокумент28 страницInfectious Diseases of The Dog and Cat, 3rd Edition: CHAPTER 73 LeishmaniasessoledadDC329Оценок пока нет
- Infectious Diseases of The Dog and Cat, 3rd Edition: CHAPTER 76 CytauxzoonosisДокумент13 страницInfectious Diseases of The Dog and Cat, 3rd Edition: CHAPTER 76 CytauxzoonosissoledadDC329Оценок пока нет
- Infectious Diseases of The Dog and Cat, 3rd Edition: CHAPTER 77 BabesiosisДокумент29 страницInfectious Diseases of The Dog and Cat, 3rd Edition: CHAPTER 77 BabesiosissoledadDC329Оценок пока нет
- Infectious Diseases of The Dog and Cat, 3rd Edition: CHAPTER 81 Enteric CoccidiosisДокумент21 страницаInfectious Diseases of The Dog and Cat, 3rd Edition: CHAPTER 81 Enteric CoccidiosissoledadDC329Оценок пока нет
- Diabetes Insipidus - NIDDKДокумент9 страницDiabetes Insipidus - NIDDKAnam MirОценок пока нет
- Acquired Coagulation DisordersДокумент12 страницAcquired Coagulation DisordersaymenОценок пока нет
- Pituitary Agents PharmaДокумент42 страницыPituitary Agents PharmaJayson Tom Briva CapazОценок пока нет
- Hematologic DisordersДокумент32 страницыHematologic DisordersQuolette ConstanteОценок пока нет
- Anti DiureticsДокумент16 страницAnti DiureticsPuneethgowda.G.K Puneeth50% (2)
- Hemophilia: Supervisor: Dr. H. Hakimi, Sp.A (K)Документ46 страницHemophilia: Supervisor: Dr. H. Hakimi, Sp.A (K)Bima DwiОценок пока нет
- Hyponatremia in Cirrhosis: An Update: Joseph J. Alukal, MD, Savio John, MD and Paul J. Thuluvath, MD, FRCPДокумент11 страницHyponatremia in Cirrhosis: An Update: Joseph J. Alukal, MD, Savio John, MD and Paul J. Thuluvath, MD, FRCPMuzaffar MehdiОценок пока нет
- Urinary Incontinence 335236 153 38333 v3Документ6 страницUrinary Incontinence 335236 153 38333 v3jermumОценок пока нет
- Diabetes Insipidus: Done By: Farah Suhimat Sereen MajaliДокумент23 страницыDiabetes Insipidus: Done By: Farah Suhimat Sereen Majaliraed faisalОценок пока нет
- Jurnal LUTS PDFДокумент8 страницJurnal LUTS PDFmitaОценок пока нет
- Hipofisis 3Документ23 страницыHipofisis 3RafaelPetitОценок пока нет
- Diabetes InsipidusДокумент48 страницDiabetes InsipidusAhmed Fraz MamoonОценок пока нет
- Diabetes InsipidusДокумент7 страницDiabetes Insipiduspaul_stefenson10Оценок пока нет
- Medicine & Surgery MCQs With Answers Feb 20Документ21 страницаMedicine & Surgery MCQs With Answers Feb 20sb medexОценок пока нет
- Diabetes InsipidusДокумент60 страницDiabetes Insipidusperie_md100% (1)
- Diabetes Insipidus (Agu Presentation)Документ15 страницDiabetes Insipidus (Agu Presentation)Um HamoOdОценок пока нет
- Central Diabetes InsipidusДокумент8 страницCentral Diabetes InsipidusasdwasdОценок пока нет
- Treatment of Hemophilia A and B PDFДокумент268 страницTreatment of Hemophilia A and B PDFYusry SuryawiraОценок пока нет
- (A) (B) (C) (D) : (A) Primary Polydipsia Is Not The Answer Here Because in Primary PolydipsiaДокумент1 страница(A) (B) (C) (D) : (A) Primary Polydipsia Is Not The Answer Here Because in Primary PolydipsiaAbdul QuyyumОценок пока нет
- EnuresisДокумент11 страницEnuresisAracelis Calzadilla NúñezОценок пока нет
- Hemophilia: Factor IX (Hemophilia B)Документ38 страницHemophilia: Factor IX (Hemophilia B)Jhvhjgj JhhgtyОценок пока нет
- Rapid Review AIPGMEE, 2011Документ44 страницыRapid Review AIPGMEE, 2011basic80% (5)
- ButlerДокумент9 страницButlerHepicentar NišaОценок пока нет