Академический Документы
Профессиональный Документы
Культура Документы
Pulmonary Edema
Загружено:
KailaashBaabuИсходное описание:
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Pulmonary Edema
Загружено:
KailaashBaabuАвторское право:
Доступные форматы
Pulmonary edema is a condition associated with increased loss of fuid from the
pulmonary capillaries into the pulmonary interstitium and alveoli. Pulmonary edema
of cardiac origin most commonly results from an increase in pulmonary capillary
pressure caused by an elevation of left atrial pressure (pulmonary capillary wedge
pressure) associated with left ventricular failure or valve disease (e.g., mitral or
aortic regurgitation, mitral or aortic stenosis). Pulmonary hypertension can also
lead to elevated capillary pressures and pulmonary edema. The physical factors and
dynamics of edema formation are discussed elsewhere.
Pulmonary edema, a medical emergency, is an accumulation of fluid in the lungs. Most often
a consequence of congestive heart failure, pulmonary edema typically occurs when the heart is
unable to pump blood out through the arteries as quickly as it is returned to the heart through the
veins.
Failure of the left side of the heart (left ventricle) causes blood to accumulate in the veins of the
lungs (pulmonary veins), producing a dangerous rise in blood pressure within these veins.
Sustained high pressure in the pulmonary veins eventually forces some fluid from the blood into
the surrounding microscopic air sacs (alveoli), which transfer oygen to the bloodstream. !s the
alveoli fill with fluid, they can no longer provide adequate amounts of oygen to the body.
Symptoms, especially severe breathing difficulty, develop over the course of a few hours and
may be life"threatening. !lthough the outlook for pulmonary edema is favorable if the
underlying disorder is treated in a timely fashion, the overall outcome for the patient depends
upon the nature of the underlying disorder. !dults at high risk for heart failure are most
commonly affected.
! less common form of the disease, high-altitude pulmonary edema (which may occur while
mountain"climbing, for instance), is also life"threatening if not treated quickly. Strenuous activity
upon arrival at high altitudes may cause a dangerous rise in the pressure in the pulmonary veins,
forcing fluid out of the veins into the alveoli. !fter people become acclimated to the altitude,
strenuous activity does not pose such a risk.
#igh"altitude pulmonary edema most often affects young adults under age $% who are
unacclimati&ed to the altitude but otherwise in good health. Symptoms appear within $' to ($
hours and necessitate immediate descent to a lower altitude for treatment. (!ir travelers are
generally not at risk for this disorder because commercial airplane cabins are pressuri&ed.)
What Causes Pulmonary Edema?
)ongestive heart failure due to high blood pressure, aortic or mitral valve disease, or
cardiomyopathy is a common cause of pulmonary edema.
! heart attack may cause pulmonary edema.
! variety of other conditions, such as lung infections, etensive burns, liver or kidney
disease, #odgkin*s disease, pneumothora or nutritional deficiencies, may lead to
pulmonary edema in some cases.
+verdoses of heroin, morphine and other narcotics may lead to pulmonary edema.
,apid ascent to high altitudes followed immediately by heavy eertion may cause high"
altitude pulmonary edema.
Pulmonary edema is acute, severe left ventricular failure with pulmonary venous
hypertension and alveolar flooding. Findings are severe dyspnea, diaphoresis, whee&ing, and
sometimes blood"tinged frothy sputum. -iagnosis is clinical and by chest "ray. .reatment
is with +$, /0 nitrates, diuretics, and sometimes morphine and short"term /0 positive
inotropes, endotracheal intubation, and mechanical ventilation.
/f left ventricular (10) filling pressure increases suddenly, plasma fluid moves rapidly from
pulmonary capillaries into interstitial spaces and alveoli, causing pulmonary edema.
!lthough precipitating causes vary by age and country, about one half of cases result from
acute coronary ischemia2 some from decompensation of significant underlying heart failure
(#F), including diastolic dysfunction #F due to hypertension2 and the rest from
arrhythmia, an acute valvular disorder, or acute volume overload often due to /0 fluids.
-rug or dietary nonadherence is often involved.
Symptoms and Signs
3atients present with etreme dyspnea, restlessness, and aniety with a sense of suffocation.
)ough producing blood"tinged sputum, pallor, cyanosis, and marked diaphoresis are
common2 some patients froth at the mouth. Frank hemoptysis is uncommon. .he pulse is
rapid and low volume, and 43 is variable. Marked hypertension indicates significant cardiac
reserve2 hypotension with systolic 43 5 677 mg #g is ominous. /nspiratory fine crackles are
widely dispersed anteriorly and posteriorly over both lung fields. Marked whee&ing (cardiac
asthma) may occur. 8oisy respiratory efforts often make cardiac auscultation difficult2 a
summation gallop9merger of :rd (S:) and 'th (S') heart sounds9may be present. Signs of
right ventricular (,0) failure (eg, neck vein distention, peripheral edema) may be present.
Diagnosis
)linical evaluation showing severe dyspnea and pulmonary crackles
)hest "ray
Sometimes serum brain natriuretic peptide (483) or 8"terminal"pro 483 (8."pro"
483)
;)<, cardiac markers, and other tests for etiology as needed
! )+3- eacerbation can mimic pulmonary edema due to 10 failure or even that due to
biventricular failure if cor pulmonale (see )or 3ulmonale) is present. 3ulmonary edema
may be the presenting symptom in patients without a history of cardiac disorders, but )+3-
patients with such severe symptoms usually have a history of )+3-, although they may be
too dyspneic to relate it.
! chest "ray, done immediately, is usually diagnostic, showing marked interstitial edema.
4edside measurement of serum 483=8."pro483 levels (elevated in pulmonary edema2
normal in )+3- eacerbation) is helpful if the diagnosis is in doubt. ;)<, pulse oimetry,
and blood tests (cardiac markers, electrolytes, 4>8, creatinine and, for severely ill patients,
!4<s) are done. ;chocardiography may be helpful to determine the cause of the pulmonary
edema (eg, M/, valvular dysfunction, hypertensive heart disease, dilated cardiomyopathy)
and may influence the choice of therapies. Hypoemia can be severe. )+$ retention is a
late, ominous sign of secondary hypoventilation.
!reatment
!reatment of cause
+$
/0 diuretic
8itrates
/0 inotropes
Morphine
0entilatory assistance
/nitial treatment includes identifying the cause2 677? +$ by nonrebreather mask2 upright
position2 furosemide
7.% to 6.7 mg=kg /0 or by continuous infusion % to 67 mg=h2 nitroglycerin
7.' mg sublingually q % min, followed by an /0 drip at 67 to $7 mcg=min, titrated upward at
67 mcg=min q % min as needed to a maimum :77 mcg=min if systolic 43 is @ 677 mm #g.
Morphine
, 6 to % mg /0 once or twice, has long been used to reduce severe aniety and the work of
breathing but is decreasingly used, as noninvasive ventilatory assistance with bilevel
positive airway pressure (4i3!3) is helpful if hypoia is significant. /f )+$ retention is
present or the patient is obtunded, tracheal intubation and assisted ventilation are required
(see .racheal /ntubation).
Specific additional treatment depends on etiologyA
For acute M/ or another acute coronary syndrome, thrombolysis or direct
percutaneous coronary angioplasty with or without stent placement
For severe hypertension, an /0 vasodilator
For supraventricular or ventricular tachycardia, direct"current cardioversion
For rapid atrial fibrillation, cardioversion is preferred. .o slow the ventricular rate,
an /0 B"blocker, /0 digoin
, or cautious use of an /0 )a channel blocker
/n patients with acute M/, fluid status before onset of pulmonary edema is usually normal,
so diuretics are less useful than in patients with acute decompensation of chronic #F and
may precipitate hypotension. /f systolic 43 falls 5 677 mm #g or shock develops, /0
dobutamine
and an intra"aortic balloon pump (counterpulsation) may be required.
Some newer drugs, such as /0 483 (nesiritide
) and )a"sensiti&ing inotropic drugs (levosimendan, pimobendan), vesnarinone, and
ibopamine, may have initial beneficial effects but do not appear to improve outcomes
compared to standard therapy, and mortality may be increased.
+nce patients are stabili&ed, long"term #F treatment is begun (see see .reatment).
"ey Points
#cute pulmonary edema can result from acute coronary ischemia, decompensation
of underlying #F, arrhythmia, an acute valvular disorder, or acute volume overload.
3atients have severe dyspnea, diaphoresis, whee&ing, and sometimes blood"tinged
frothy sputum.
)linical eamination and chest "ray are usually sufficient for diagnosis2 ;)<,
cardiac markers, and sometimes echocardiography are done to identify cause.
.reat the cause and give +$ and /0 furosemide
and=or nitrates as needed2 try noninvasive ventilatory assistance initially but use
tracheal intubation and assisted ventilation if necessary.
Вам также может понравиться
- Medicine in Brief: Name the Disease in Haiku, Tanka and ArtОт EverandMedicine in Brief: Name the Disease in Haiku, Tanka and ArtРейтинг: 5 из 5 звезд5/5 (1)
- Cor Pulmonale (Pneumoconiosis)Документ23 страницыCor Pulmonale (Pneumoconiosis)Sai charithaОценок пока нет
- Cardiac TamponadeДокумент10 страницCardiac TamponadeRahmi Fatma SariОценок пока нет
- Angelina A Joho MSC in Critical Care and TraumaДокумент50 страницAngelina A Joho MSC in Critical Care and TraumaZabron LuhendeОценок пока нет
- Cardiac TamponadeДокумент6 страницCardiac TamponadeVicky XieОценок пока нет
- Sclerodactyly, and Telangiectasis) Syndrome Accompany-: Cor PulmonaleДокумент2 страницыSclerodactyly, and Telangiectasis) Syndrome Accompany-: Cor PulmonaledivinaОценок пока нет
- Obstructive ShockДокумент2 страницыObstructive ShockningshofieОценок пока нет
- Pulmonary ThromboembolismДокумент4 страницыPulmonary ThromboembolismValerrie NgenoОценок пока нет
- Casos Cardiológicos 1Документ12 страницCasos Cardiológicos 1Larissa SeabraОценок пока нет
- LME SelfДокумент5 страницLME SelfJM Mizraime Gallo Dela-peñaОценок пока нет
- Tamponade JantungДокумент5 страницTamponade JantungsyaviraОценок пока нет
- Pulmonary Embolus (PE)Документ3 страницыPulmonary Embolus (PE)Heidi M FischerОценок пока нет
- Cardiac AsthmaДокумент12 страницCardiac AsthmaNeupane KsabОценок пока нет
- USMLE General CardiologyДокумент72 страницыUSMLE General CardiologyWidyo MahargoОценок пока нет
- Cor Pulmonale IkaДокумент19 страницCor Pulmonale IkaIka Lukita SariОценок пока нет
- Under Supervision DR/ Mariam Sabry: Ulmonary DemaДокумент28 страницUnder Supervision DR/ Mariam Sabry: Ulmonary DemaMohamed ElsyaedОценок пока нет
- Pericarditis AbДокумент39 страницPericarditis AbAbnet WondimuОценок пока нет
- Acute Heart FailureДокумент9 страницAcute Heart FailureChen Briones100% (1)
- Rheumatic Heart Disease: Emmanuel Edafe Consultant Interventional Cardiologist, NduДокумент36 страницRheumatic Heart Disease: Emmanuel Edafe Consultant Interventional Cardiologist, NduPrincewill SeiyefaОценок пока нет
- Cor PulmonaleДокумент14 страницCor PulmonaleEvangelin MelvinОценок пока нет
- Cor PulmonaleДокумент24 страницыCor PulmonaleGungdeprawira NegaraОценок пока нет
- Lungs 3Документ60 страницLungs 3Surya L KОценок пока нет
- Pulmonary Edema Facts What Causes Pulmonary Edema?Документ23 страницыPulmonary Edema Facts What Causes Pulmonary Edema?Louella RamosОценок пока нет
- Lecture 4Документ4 страницыLecture 4Grafu Andreea AlexandraОценок пока нет
- Tit Bits in MedДокумент11 страницTit Bits in MedValerrie NgenoОценок пока нет
- Apasi Yg Ga Buat NisaДокумент20 страницApasi Yg Ga Buat Nisamuhammad iqbal mahfuzhОценок пока нет
- Pericardial DiseseasДокумент38 страницPericardial Diseseasmameekasim75Оценок пока нет
- Cor PulmonaleДокумент62 страницыCor PulmonaleAlbert NixonОценок пока нет
- Poster Presentation CCRA Malang 2014Документ3 страницыPoster Presentation CCRA Malang 2014alfarobi yogiОценок пока нет
- Cor PulmonaleДокумент15 страницCor PulmonaleRizky Zulfa Afrida100% (1)
- Infectious Disease of HeartДокумент11 страницInfectious Disease of HeartRina CebreroОценок пока нет
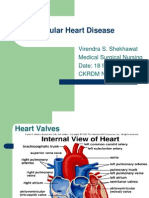
- Valvular Heart DiseaseДокумент41 страницаValvular Heart DiseaseVirendra Shekhawat100% (1)
- History and Physical Examination: EvaluationДокумент3 страницыHistory and Physical Examination: EvaluationDore NanОценок пока нет
- Modern Management of Cardiogenic Pulmonary Edema: Amal Mattu, MD, Joseph P. Martinez, MD, Brian S. Kelly, MDДокумент21 страницаModern Management of Cardiogenic Pulmonary Edema: Amal Mattu, MD, Joseph P. Martinez, MD, Brian S. Kelly, MDJoni MokodoОценок пока нет
- Inflammatory Disease of The HeartДокумент20 страницInflammatory Disease of The HeartmichaelurielОценок пока нет
- 1.3 Heart FailureДокумент30 страниц1.3 Heart Failuresn_b5Оценок пока нет
- Pulmonary EdemaДокумент32 страницыPulmonary EdemaAshraf Jonidee100% (1)
- HTN and CHFДокумент29 страницHTN and CHFkiflomОценок пока нет
- Acute Respiratory FailureДокумент17 страницAcute Respiratory FailurejulianajosОценок пока нет
- Uptodate Cor Pulmonale PDFДокумент13 страницUptodate Cor Pulmonale PDFcristianamihailaОценок пока нет
- Heart Valve DiseaseДокумент67 страницHeart Valve DiseaseSaba SivaОценок пока нет
- Pulmonary Embolism (PE) - Pulmonary Disorders - MSD Manual Professional EditionДокумент25 страницPulmonary Embolism (PE) - Pulmonary Disorders - MSD Manual Professional Editionpeterpavel112Оценок пока нет
- Pulmonary Edema - StatPearls - NCBI BookshelfДокумент7 страницPulmonary Edema - StatPearls - NCBI BookshelfriyanasirОценок пока нет
- Cor Pulmonale EmedicineДокумент16 страницCor Pulmonale EmedicineHengki Permana PutraОценок пока нет
- Pulmonary Thromboembolism: DR Olubunmi Ogunlade Consultant PulmonologistДокумент34 страницыPulmonary Thromboembolism: DR Olubunmi Ogunlade Consultant PulmonologistEmeka Chinedu Precious PetrousОценок пока нет
- Patho 1Документ153 страницыPatho 1ademabdellaaleОценок пока нет
- Wardclass-Venous Air EmbolismДокумент17 страницWardclass-Venous Air EmbolismDan Dan Soi TОценок пока нет
- Surgical Implications of Low Cardiac Output Syndrome After Myocardial InfarctionДокумент5 страницSurgical Implications of Low Cardiac Output Syndrome After Myocardial Infarctionrandomized1234Оценок пока нет
- Kardiogenik SyokДокумент43 страницыKardiogenik SyokGalih Arief Harimurti WawolumajaОценок пока нет
- Cor PulmonaleДокумент27 страницCor PulmonaleumapathisivanОценок пока нет
- Symptoms and Signs: Pulmonary Edema (American English), or Oedema (Документ4 страницыSymptoms and Signs: Pulmonary Edema (American English), or Oedema (contentseeker3401Оценок пока нет
- Kelompok 15 Skenario 3Документ42 страницыKelompok 15 Skenario 313calcitoninОценок пока нет
- Cardiac Tamponade, Also Known As Pericardial Tamponade, Is AnДокумент7 страницCardiac Tamponade, Also Known As Pericardial Tamponade, Is AnSimran Josan100% (1)
- Critical Care Management of Acute Stroke - ZazuliaДокумент15 страницCritical Care Management of Acute Stroke - ZazuliaIndah ManafОценок пока нет
- Acute Heart Failure Syndromes: Kelompok CДокумент29 страницAcute Heart Failure Syndromes: Kelompok CErwin BawonoОценок пока нет
- Heart FailureДокумент4 страницыHeart FailureFaizan AbbasiОценок пока нет
- Heart FailureДокумент20 страницHeart Failurelancer 89100% (1)
- Eisenmenger SyndromeДокумент9 страницEisenmenger SyndromesyifandikaОценок пока нет
- Endodontic Diagnostic Terminology UpdateДокумент3 страницыEndodontic Diagnostic Terminology UpdateAlyaefkageОценок пока нет
- Blood Anatomy and Physiology ReviewДокумент20 страницBlood Anatomy and Physiology ReviewStacey CamilleОценок пока нет
- PQCNC New Initiative Proposal CLABSIДокумент17 страницPQCNC New Initiative Proposal CLABSIkcochranОценок пока нет
- PneumothoraxДокумент14 страницPneumothoraxAsterlita WenasОценок пока нет
- Hospital Use CaseДокумент3 страницыHospital Use Caseprashant gauravОценок пока нет
- San Ma&no,: John Frush, and Roland FisherДокумент11 страницSan Ma&no,: John Frush, and Roland FisherAbhishek SharmaОценок пока нет
- Root Cause Analysis ToolsДокумент7 страницRoot Cause Analysis ToolsSofiane IdjerОценок пока нет
- PANCE Prep Pearls Valvular Disease PDFДокумент4 страницыPANCE Prep Pearls Valvular Disease PDFkatОценок пока нет
- Dysphagya Screening PDFДокумент67 страницDysphagya Screening PDFMagaly DonosoОценок пока нет
- Patient's Profile Name: S.T. Age: 3y/o SexДокумент3 страницыPatient's Profile Name: S.T. Age: 3y/o SexCharles_Guzman_1567Оценок пока нет
- Circulating SerotoninДокумент17 страницCirculating Serotoninnihilx27374Оценок пока нет
- Opi 1Документ2 страницыOpi 1medstudjokiОценок пока нет
- Daftar Pustaka: Universitas Sumatera UtaraДокумент4 страницыDaftar Pustaka: Universitas Sumatera UtaraDwita Setya FitrantiОценок пока нет
- Calcium Hydroxylapatite (Radiesse) For Correction of The Mid-And Lower Face: Consensus RecommendationsДокумент12 страницCalcium Hydroxylapatite (Radiesse) For Correction of The Mid-And Lower Face: Consensus RecommendationsMichele CarvalhoОценок пока нет
- 3.16.13-Letter To The Editor From Paul LiistroДокумент1 страница3.16.13-Letter To The Editor From Paul LiistroLisa BousquetОценок пока нет
- Classification and Management of Subcutaneous EmphysemaДокумент5 страницClassification and Management of Subcutaneous EmphysemaTaufik Gumilar WahyudinОценок пока нет
- Clinical Approach To Brainstem LesionsДокумент10 страницClinical Approach To Brainstem LesionsJosé SánchezОценок пока нет
- Medif FormДокумент2 страницыMedif FormyunhanieОценок пока нет
- CCA Final Exam Review 06 - 02Документ4 страницыCCA Final Exam Review 06 - 02Stephen_haslundОценок пока нет
- GuideToClinicalEndodontics v6 2019updateДокумент40 страницGuideToClinicalEndodontics v6 2019updateLorena MarinОценок пока нет
- Attachments For Removable Partial Dentures Prostho 6Документ10 страницAttachments For Removable Partial Dentures Prostho 6Melika DОценок пока нет
- 3 The Kaiser Permanente Northern California AdvanceДокумент6 страниц3 The Kaiser Permanente Northern California AdvanceBlanca LanderosОценок пока нет
- Fluid and ElectrolytesДокумент14 страницFluid and Electrolytesstring44100% (2)
- Challenges NabhДокумент24 страницыChallenges NabhEka BОценок пока нет
- TabletsДокумент6 страницTabletsRupesh Kumar DuttaОценок пока нет
- Operasi Monokular Recess Resect Dengan Teknik: Hangback Pada Exotropia Deviasi BesarДокумент10 страницOperasi Monokular Recess Resect Dengan Teknik: Hangback Pada Exotropia Deviasi BesarBlack Clover IdОценок пока нет
- Did You Know?: Nama: Alfa Innersia Zahada NIM: 1897194042 Prodi: Pend. Bahasa Inggris A Semester: 2Документ2 страницыDid You Know?: Nama: Alfa Innersia Zahada NIM: 1897194042 Prodi: Pend. Bahasa Inggris A Semester: 2Abu Bakar Ar-Rasa'ilОценок пока нет
- Nursing Assessment 1Документ70 страницNursing Assessment 1Amira AttyaОценок пока нет
- Epidemiology, Aetiology, and Management of IschaemicДокумент12 страницEpidemiology, Aetiology, and Management of IschaemicKhairunNisaОценок пока нет
- 1) KULLA, S. Lung Cancer Online VersionДокумент83 страницы1) KULLA, S. Lung Cancer Online VersionJosh SolisОценок пока нет