Академический Документы
Профессиональный Документы
Культура Документы
First Do No Harm: A Real Need To Deprescribe in Older Patients
Загружено:
caffyw0 оценок0% нашли этот документ полезным (0 голосов)
114 просмотров3 страницыDeliberate yet judicious deprescribing has considerable potential to relieve unnecessary medication-related suffering and disability in vulnerable older populations. A report by the Medical Journal of Australia.
Оригинальное название
First do no harm: a real need to deprescribe in older patients
Авторское право
© © All Rights Reserved
Доступные форматы
PDF, TXT или читайте онлайн в Scribd
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документDeliberate yet judicious deprescribing has considerable potential to relieve unnecessary medication-related suffering and disability in vulnerable older populations. A report by the Medical Journal of Australia.
Авторское право:
© All Rights Reserved
Доступные форматы
Скачайте в формате PDF, TXT или читайте онлайн в Scribd
0 оценок0% нашли этот документ полезным (0 голосов)
114 просмотров3 страницыFirst Do No Harm: A Real Need To Deprescribe in Older Patients
Загружено:
caffywDeliberate yet judicious deprescribing has considerable potential to relieve unnecessary medication-related suffering and disability in vulnerable older populations. A report by the Medical Journal of Australia.
Авторское право:
© All Rights Reserved
Доступные форматы
Скачайте в формате PDF, TXT или читайте онлайн в Scribd
Вы находитесь на странице: 1из 3
Clinical focus
1 MJA 201 (7) 6 October 2014
Clinical focus
Ian A Scott
FRACP, MHA, MEd
Director of Internal Medicine
and Clinical Epidemiology
1
Kristen Anderson
BPharm
PhD Scholar,
2
and
Advanced Primary Care
Pharmacist Fellow
3
Christopher R Freeman
BPharm, PhD, BCACP
Director of Pharmacy
3
Danielle A Stowasser
PhD, BPharm,
PGDipClinHospPharm
Associate Professor of
Pharmacy
4
1 Princess Alexandra Hospital,
Brisbane, QLD.
2 Centre of Research
Excellence in Quality
and Safety in Integrated
Primary/Secondary Care,
University of Queensland,
Brisbane, QLD.
3 CHARMING Institute,
Brisbane, QLD.
4 University of Queensland,
Brisbane, QLD.
ian.scott@
health.qld.gov.au
doi: 10.5694/mja14.00146
Summary
Inappropriate polypharmacy in older patients imposes
a significant burden of decreased physical functioning,
increased risk of falls, delirium and other geriatric
syndromes, hospital admissions and death.
The single most important predictor of inappropriate
prescribing and risk of adverse drug events in older
patients is the number of prescribed medications.
Deprescribing is the process of tapering or stopping
drugs, with the goal of minimising polypharmacy and
improving outcomes.
Barriers to deprescribing include underappreciation
of the scale of polypharmacy-related harm by both
patients and prescribers; multiple incentives to
overprescribe; a narrow focus on lists of potentially
inappropriate medications; reluctance of prescribers
and patients to discontinue medication for fear
of unfavourable sequelae; and uncertainty about
effectiveness of strategies to reduce polypharmacy.
Ways of countering such barriers comprise reframing
the issue to one of highest quality patient-centred
care; openly discussing benefitharm trade-offs with
patients and assessing their willingness to consider
deprescribing; targeting patients according to highest
risk of adverse drug events; targeting drugs more
likely to be non-beneficial; accessing field-tested
discontinuation regimens for specific drugs; fostering
shared education and training in deprescribing among
all members of the health care team; and undertaking
deprescribing over an extended time frame under the
supervision of a single generalist clinician.
D
eliberate yet judicious deprescribing has consid-
erable potential to relieve unnecessary medica-
tion-related suffering and disability in vulnerable
older populations. Polypharmacy variously defined
as more than five or up to 10 or more medications taken
regularly per individual is common among older
people (defined here as those aged 65 years or over).
Depending on the circumstances, including why and
how drugs are being administered, polypharmacy can
be appropriate (potential benefits outweigh potential
harms) or inappropriate (potential harms outweigh po-
tential benefits).
While many older people benefit immeasurably from
multiple drugs, many others suffer adverse drug events
(ADEs). In Australia, one in four community-living older
people are hospitalised for medication-related problems
over a 5-year period
1
and 15% of older patients attend-
ing general practice report an ADE over the previous 6
months.
2
At least a quarter of these ADEs are potentially
preventable.
2
Up to 30% of hospital admissions for pa-
tients over 75 years of age are medication related, and
up to three-quarters are potentially preventable.
3
Up
to 40% of people living in either residential care
4
or the
community
5
are prescribed potentially inappropriate
medications. In both hospital and primary care settings,
about one in five prescriptions issued for older adults are
deemed inappropriate.
6
Polypharmacy in older people is associated with de-
creased physical and social functioning; increased risk
of falls, delirium and other geriatric syndromes, hospital
admissions, and death; and reduced adherence by patients
to essential medicines. The financial costs are substantial,
with ADEs accounting for more than 10% of all direct
health care costs among affected individuals.
7
The single most important predictor of inappropriate
prescribing and risk of ADEs is the number of medica-
tions a person is taking; one report estimated the risk
as 13% for two drugs, 38% for four drugs, and 82% for
seven drugs or more.
8
One in five older Australians are
receiving more than 10 prescription or over-the-counter
medicines.
9
People in residential aged care facilities are
prescribed, on average, seven drugs,
10
while hospitalised
patients average eight.
11
While hospitalisation might
provide an opportunity to review medication use, on
average, while two to three drugs are ceased, three to
four are added.
12
In responding to polypharmacy-related harm, a new
term has entered the medical lexicon: deprescribing.
This is the process of tapering or stopping drugs using
a systematic approach (Box).
13
Inculcating a culture of
deprescribing will be challenging for several reasons.
Barriers to deprescribing
Underappreciation of the scale of polypharmacy-
related harm
Clinicians easily recognise clinically evident ADEs with
clear-cut causality. In contrast, ADEs mimicking syn-
dromes prevalent in older patients falls, delirium,
lethargy and depression account for 20% of ADEs
in hospitalised older patients but go unrecognised by
clinical teams.
14
Increasing intensity of medical care
The drivers of polypharmacy are multiple: disease-spe cific
clinical guideline recommendations, quality indicators
and performance incentives;
15
a focus on pharmacological
versus non-pharmacological options; and prescribing
cascades, when more drugs are added in response to
onset of new illnesses, including ADEs misinterpreted
as new disease.
First do no harm: a real need to
deprescribe in older patients
Online first 22/09/14
EMBARGO: 12:01am Monday 22 September 2014
Clinical focus
2 MJA 201 (7) 6 October 2014
Narrow focus on lists of potentially inappropriate
medications
Lists of potentially inappropriate medications (such as
the Beers, McLeod and STOPP [Screening Tool of Older
Persons Potentially Inappropriate Prescriptions] criteria)
16
comprise drugs whose benefits are outweighed by harm
in most circumstances. Examples include potent opioids
used non-palliatively, non-steroidal anti-inflammatory
agents, anticholinergic drugs and benzodiazepines.
However, such drugs account for relatively few ADEs in
Australian practice.
17
In contrast, commonly prescribed
drugs with proven benefits in many older people, such
as cardiovascular drugs, anticoagulants, hypoglycaemic
agents, steroids and antibiotics, are more frequently im-
plicated as a result of misuse.
18
Reluctance of prescribers and ambivalence of patients
Many prescribers feel uneasy about ceasing drugs for
several reasons:
19,20
going against opinion of other doctors
(particularly specialists) who initiated a specific drug and
which patients appear to tolerate; fear of precipitating
disease relapse or drug withdrawal syndromes or patient
approbation at having their care downgraded; paucity
of precise benefitharm data for specific medications to
guide selection for discontinuation; apprehension around
discussing life expectancy versus quality of life in ration-
alising drug regimens; limited time and remuneration for
reappraising chronic medications, discussing pros and
cons with patients, and coordinating views and actions
of multiple prescribers.
While agreeing in principle to minimising polyphar-
macy, patients simultaneously express gratitude that their
drugs may prolong life, abate symptoms and improve
function. Fear of relapsing disease lessens patients de-
sire to discontinue a drug, especially if combined with
negative past experiences. Inability to see the personal
relevance of harmbenefit trade-offs or lack of trust
in their doctors advice about drug inappropriateness
and the safety of discontinuation plans also act against
deprescribing.
21
Possible solutions
Ultimately, deprescribing is a highly individualised and
time-consuming process, but several facilitative strat egies
are offered.
Reframe the issue
Both the patient and clinician should regard deprescrib-
ing as an attempt to alleviate symptoms (of drug toxicity),
improve quality of life (from drug-induced disability) and
lessen the risk of morbid events (ADEs) in the future. Its
objective is not simply to reduce the burden, inconveni-
ence or costs of complex drug regimens, although these
too are potential benefits. Deprescribing should not be
seen by patients as an act of abandonment but one of
affirmation for highest quality care and shared decision
making. Compelling evidence that identifies circum-
stances in which medications can be safely withdrawn
while reducing the risk of ADEs and death needs to be
emphasised.
22-25
Discuss benefitharm trade-offs and assess
willingness
In consenting to a trial of withdrawal, patients need to
know the benefitharm trade-offs specific to them of
continuing or discontinuing a particular drug. Patient
education initiatives providing such personalised infor-
mation can substantially alter perceptions of risk and
change attitudes towards discontinuation.
26
Target patients according to highest ADE risk
In addition to medication count, other ADE predictors
include past history of ADEs, presence of major comor-
bidities, marked frailty, residential care settings and
multiple prescribers.
Target drugs more likely to be non-beneficial
Such drugs, as initial targets for deprescribing, consist
of five types.
Drugs to avoid if at all possible (comprising those
previously cited in drugs to avoid lists
16
).
Drugs lacking therapeutic effect for substantiated
indications despite optimal adherence over a reason-
able period of time.
Drugs that patients are unwilling to take for vari-
ous reasons, including occult drug toxicity, difficulty
handling medications, costs and little faith in drug
efficacy.
Drugs lacking a substantiated indication, either be-
cause the original disease diagnosis was incorrect as
often occurs with regard to heart failure, Parkinson
disease and depression or because the stated di-
agnosis-specific indication is invalid owing to evi-
dence of harm or no benefit. Importantly, indications
Core themes in deprescribing
13
Ascertain all current medications (medication reconciliation)
Identify patients at high risk of adverse drug events
number and type of drugs
patient characteristics (physical, mental, social impairments)
multiple prescribers
Estimate life expectancy in high-risk patients
with focus on patients with prognosis equal to or less than 12 months
Define overall care goals and patient values and preferences in the context of life
expectancy
relativity of symptom control and quality of life v cure or prevention
patient preference for aggressive v conservative care; willingness to consider
deprescribing
Define and validate current indications for ongoing treatment
medicationdiagnosis reconciliation
drugs lacking valid indications are candidates for discontinuation
Determine time until benefit for preventive or disease-modifying medications
drugs whose time until benefit exceeds expected life span are candidates for
discontinuation
Estimate magnitude of benefit v harm in absolute terms for individual patient
drugs with little likelihood of benefit and/or significant risk of harm are candidates for
discontinuation
Implement and monitor a drug deprescribing plan
ongoing reappraisal for illness relapse or deterioration or withdrawal syndromes
communication of plan and shared responsibility among all prescribers
supervision of drug discontinuation by single generalist clinician
EMBARGO: 12:01am Monday 22 September 2014
3 MJA 201 (7) 6 October 2014
Clinical focus
or treatment targets derived from studies involving
younger patients or highly selected, older individuals
with a single disease may be inappropriate for older,
frail patients with multimorbidity.
Drugs that are unlikely to prevent disease events
within the patients remaining life span. The ques-
tion here is not how much benefit drugs aimed at
preventing future disease events (such as statins and
bisphosphonates) may confer, but when. If the time
until benefit exceeds the patients estimated life span,
no benefit will result, while the ADE risk is constant
and immediate. Undertaking such reconciliations is
facilitated by accurate estimation of longevity using
easy-to-use web-based mortality indices (eg, see http://
eprognosis.ucsf.edu) and drug-specific time until ben-
efit using trial-based time-to-event data.
27
Access and apply specific discontinuation regimens
Detailed descriptions of how clinicians can safely with-
draw specific drugs and monitor for adverse effects can
be found within various articles and websites.
28,29
Foster shared education and training
Interactive, case-based, interdisciplinary meetings involv-
ing multiple prescribers, combined with deprescribing
advice from clinical pharmacologists or appropriately
trained pharmacists have been shown to be beneficial
with regard to doctors deprescribing practice.
30
Extend the time frame with the same clinician
Several patient encounters with the same overseeing
generalist clinician, focused on one drug at a time, can
provide repeated opportunities to discuss and assuage
a patients fear of discontinuing a drug and to adjust the
deprescribing plan according to changes in clinical cir-
cumstances and revised treatment goals. Deprescribing
can be remunerated under extended care or medication
review items, with patients full awareness that such
consultations are expressly for reviewing medications.
Conclusion
Inappropriate polypharmacy and its associated harm
is a growing threat among older patients that requires
deliberate yet judicious deprescribing using a systematic
approach. Widespread adoption of this strategy has its
challenges, but also considerable potential to relieve un-
necessary suffering and disability, as embodied in that
basic Hippocratic dictum first do no harm.
Acknowledgements: Ian Scott and Kristen Anderson were assisted in this research by a
program grant from the National Health and Medical Research Council (grant 1001157).
Competing interests: No relevant disclosures.
Provenance: Not commissioned; externally peer reviewed.
1 Kalisch LM, Caughey GE, Barratt JD, et al. Prevalence of preventable
medication-related hospitalizations in Australia: an opportunity to reduce
harm. Int J Qual Health Care 2012; 24: 239-249.
2 Miller GC, Britt HC, Valenti L. Adverse drug events in general practice
patients in Australia. Med J Aust 2006; 184: 321-324.
3 Runciman WB, Roughead EE, Semple SJ, Adams RJ. Adverse drug events
and medication errors in Australia. Int J Qual Health Care 2003; 15 Suppl 1:
i49-i59.
4 Staford AC, Alswayan MS, Tenni PC. Inappropriate prescribing in older
residents of Australian care homes. J Clin Pharm Ther 2011; 36: 33-44.
5 Byles JE, Heinze R, Nair BK, Parkinson L. Medication use among older
Australian veterans and war widows. Intern Med J 2003; 33: 388-392.
6 Roughead EE, Anderson B, Gilbert AL. Potentially inappropriate prescribing
among Australian veterans and war widows/widowers. Intern Med J 2007; 37:
402-405.
7 Gyllensten H, Rehnberg C, Jnsson AK, et al. Cost of illness of patient-
reported adverse drug events: a population-based cross-sectional survey.
BMJ Open 2013; 3: e002574.
8 Atkin PA, Veitch PC, Veitch EM, Ogle SJ. The epidemiology of serious adverse
drug reactions among the elderly. Drugs Aging 1999; 14: 141-152.
9 Parkes AJ, Coper LC. Inappropriate use of medications in the veteran
community: how much do doctors and pharmacists contribute? Aust N Z J
Public Health 1997; 21: 469-476.
10 Elliott RA, Thomson A. Assessment of a nursing home medication review
service provided by hospital-based clinical pharmacists. Aust J Hosp Pharm
1998; 29: 255-260.
11 Woodward MC, Elliott RA, Oborne CA. Quality of prescribing for elderly
inpatients at nine hospitals in Victoria, Australia. J Pharm Pract Res 2003; 33:
101-105.
12 Crotty M, Rowett D, Spurling L, et al. Does the addition of a pharmacist
transition coordinator improve evidence-based medication management and
health outcomes in older adults moving from the hospital to a long-term care
facility? Results of a randomized, controlled trial. Am J Geriatr Pharmacother
2004; 2: 257-264.
13 Scott IA, Gray LC, Martin JH, et al. Deciding when to stop: towards evidence-
based deprescribing of drugs in older populations. Evid Based Med 2013; 18:
121-124.
14 Klopotowska JE, Wierenga PC, Smorenburg SM, et al. Recognition of adverse
drug events in older hospitalized medical patients. Eur J Clin Pharmacol 2013;
69: 75-85.
15 Boyd CM, Darer J, Boult C, et al. Clinical practice guidelines and quality of care
for older patients with multiple comorbid diseases: implications for pay for
performance. JAMA 2005; 294: 716-724.
16 Spinewine A, Schmader KE, Barber N, et al. Appropriate prescribing in elderly
people: how well can it be measured and optimised? Lancet 2007; 370:
173-184.
17 Miller GC, Valenti L, Britt H, Bayram C. Drugs causing adverse events in
patients aged 45 or older: a randomised survey of Australian general practice
patients. BMJ Open 2013; 3: e003701.
18 Budnitz DS, Lovegrove MC, Shehab N, Richards CL. Emergency
hospitalizations for adverse drug events in older Americans. N Engl J Med 2011;
365: 2002-2012.
19 Anthierens S, Tansens A, Petrovic M, Christiaens T. Qualitative insights into
general practitioners views on polypharmacy. BMC Fam Pract 2010; 11: 65.
20 Schuling J, Gebben H, Veehof LJ, Haaijer-Ruskamp FM. Deprescribing
medication in very elderly patients with multimorbidity: the view of Dutch
GPs. A qualitative study. BMC Fam Pract 2012; 13: 56.
21 Reeve E, To J, Hendrix I, et al. Patient barriers to and enablers of deprescribing:
a systematic review. Drugs Aging 2013; 30: 793-807.
22 Iyer S, Naganathan V, McLachlan AJ, Le Couteur DG. Medication withdrawal
trials in people aged 65 years and older: a systematic review. Drugs Aging
2008; 25: 1021-1031.
23 Declercq T, Petrovic M, Azermai M, et al. Withdrawal versus continuation of
chronic antipsychotic drugs for behavioural and psychological symptoms in
older people with dementia. Cochrane Database Syst Rev 2013; (3): CD007726.
24 Gallagher PF, OConnor MN, OMahony D. Prevention of potentially
inappropriate prescribing for elderly patients: a randomized controlled trial
using STOPP/START criteria. Clin Pharmacol Ther 2011; 89: 845-854.
25 Garnkel D, Zur-Gil S, Ben-Israel J. The war against polypharmacy: a new cost-
efective geriatric-palliative approach for improving drug therapy in disabled
elderly people. Isr Med Assoc J 2007; 9: 430-434.
26 Martin P, Tamblyn R, Ahmed S, Tannenbaum C. A drug education tool
developed for older adults changes knowledge, beliefs and risk perceptions
about inappropriate benzodiazepine prescriptions in the elderly. Patient Educ
Couns 2013; 92: 81-87.
27 NHS Highland. Polypharmacy: guidance for prescribing in frail adults.
http://www.nhshighland.scot.nhs.uk/publications/documents/guidelines/
polypharmacy guidance for prescribing in frail adults.pdf (accessed Jun 2014).
28 Farrell B, Merkley VF, Thompson W. Managing polypharmacy in a 77-year-old
woman with multiple prescribers. CMAJ 2013; 185: 1240-1245.
29 Best Practice Advocacy Centre New Zealand. A practical guide to stopping
medicines in older people. Best Practice Journal 2010; 27 Apr. http://www.
bpac.org.nz/magazine/2010/april/stopGuide.asp (accessed Nov 2013).
30 Bregnhj L, Thirstrup S, Kristensen MB, et al. Combined intervention
programme reduces inappropriate prescribing in elderly patients exposed to
polypharmacy in primary care. Eur J Clin Pharmacol 2009; 65: 199-207.
EMBARGO: 12:01am Monday 22 September 2014
Вам также может понравиться
- Drowning Prevention Report, Sri Lanka 2014Документ21 страницаDrowning Prevention Report, Sri Lanka 2014caffyw100% (1)
- Reviving Ocean Economy: A Call For Action - 2015Документ60 страницReviving Ocean Economy: A Call For Action - 2015caffywОценок пока нет
- Oral Therapy Could Provide Treatment For Peanut AllergiesДокумент16 страницOral Therapy Could Provide Treatment For Peanut AllergiescaffywОценок пока нет
- Landscape of Violence Report Finds Rural and Regional Victorian Women More Likely To Experience ViolenceДокумент217 страницLandscape of Violence Report Finds Rural and Regional Victorian Women More Likely To Experience ViolencecaffywОценок пока нет
- Open Letter To The VCs of Australian UniversitiesДокумент6 страницOpen Letter To The VCs of Australian UniversitiescaffywОценок пока нет
- Tunnel Vision or World Class Public Transport?Документ16 страницTunnel Vision or World Class Public Transport?caffywОценок пока нет
- Can Broccoli Cure Autism?Документ3 страницыCan Broccoli Cure Autism?caffywОценок пока нет
- TWT East Timor Response Department, Foreign Affairs, Trade ResponseДокумент1 страницаTWT East Timor Response Department, Foreign Affairs, Trade ResponsecaffywОценок пока нет
- European Spine JournalДокумент1 страницаEuropean Spine JournalcaffywОценок пока нет
- The Benefits and Harms of DeprescribingДокумент4 страницыThe Benefits and Harms of DeprescribingcaffywОценок пока нет
- PM: Email From The Chief Minister of Sri LankaДокумент1 страницаPM: Email From The Chief Minister of Sri LankacaffywОценок пока нет
- Councils To Be Abolished PDFДокумент2 страницыCouncils To Be Abolished PDFLatika M BourkeОценок пока нет
- Letter To The High CommissionerДокумент2 страницыLetter To The High CommissionercaffywОценок пока нет
- FINAL DeprescribingДокумент2 страницыFINAL DeprescribingcaffywОценок пока нет
- Autism Spectrum Australia Summary ReportДокумент7 страницAutism Spectrum Australia Summary ReportcaffywОценок пока нет
- Compensation Claims Made by Asylum Seekers Between 1999 and 2011Документ2 страницыCompensation Claims Made by Asylum Seekers Between 1999 and 2011caffywОценок пока нет
- Newport Police Department Report On Aaron AlexisДокумент3 страницыNewport Police Department Report On Aaron AlexisEyder PeraltaОценок пока нет
- European Spine Journal 2Документ7 страницEuropean Spine Journal 2caffywОценок пока нет
- Reporting Racism ReportДокумент68 страницReporting Racism ReportcaffywОценок пока нет
- Facilitating Wolbachia Introductions Into Mosquito Populations Through Insecticide-Resistance SelectionДокумент9 страницFacilitating Wolbachia Introductions Into Mosquito Populations Through Insecticide-Resistance SelectioncaffywОценок пока нет
- European Spine JournalДокумент1 страницаEuropean Spine JournalcaffywОценок пока нет
- European Spine Journal 2Документ7 страницEuropean Spine Journal 2caffywОценок пока нет
- European Spine JournalДокумент1 страницаEuropean Spine JournalcaffywОценок пока нет
- Letter To UK - PMДокумент3 страницыLetter To UK - PMcaffywОценок пока нет
- Coding Letter To Canadian War MuseumДокумент2 страницыCoding Letter To Canadian War MuseumcaffywОценок пока нет
- Bishop Michael Kennedy's Letter To His ParishДокумент2 страницыBishop Michael Kennedy's Letter To His ParishcaffywОценок пока нет
- Lion Range State Ranking Dec 2012Документ12 страницLion Range State Ranking Dec 2012caffywОценок пока нет
- DNA Paper Smear Cancer Paper Science Translational MedicineДокумент11 страницDNA Paper Smear Cancer Paper Science Translational MedicinecaffywОценок пока нет
- Artillery MapДокумент1 страницаArtillery MapcaffywОценок пока нет
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeОт EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeРейтинг: 4 из 5 звезд4/5 (5794)
- The Yellow House: A Memoir (2019 National Book Award Winner)От EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Рейтинг: 4 из 5 звезд4/5 (98)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryОт EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryРейтинг: 3.5 из 5 звезд3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceОт EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceРейтинг: 4 из 5 звезд4/5 (895)
- The Little Book of Hygge: Danish Secrets to Happy LivingОт EverandThe Little Book of Hygge: Danish Secrets to Happy LivingРейтинг: 3.5 из 5 звезд3.5/5 (400)
- Never Split the Difference: Negotiating As If Your Life Depended On ItОт EverandNever Split the Difference: Negotiating As If Your Life Depended On ItРейтинг: 4.5 из 5 звезд4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureОт EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureРейтинг: 4.5 из 5 звезд4.5/5 (474)
- The Emperor of All Maladies: A Biography of CancerОт EverandThe Emperor of All Maladies: A Biography of CancerРейтинг: 4.5 из 5 звезд4.5/5 (271)
- Team of Rivals: The Political Genius of Abraham LincolnОт EverandTeam of Rivals: The Political Genius of Abraham LincolnРейтинг: 4.5 из 5 звезд4.5/5 (234)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaОт EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaРейтинг: 4.5 из 5 звезд4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersОт EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersРейтинг: 4.5 из 5 звезд4.5/5 (344)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyОт EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyРейтинг: 3.5 из 5 звезд3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreОт EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreРейтинг: 4 из 5 звезд4/5 (1090)
- The Unwinding: An Inner History of the New AmericaОт EverandThe Unwinding: An Inner History of the New AmericaРейтинг: 4 из 5 звезд4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)От EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Рейтинг: 4.5 из 5 звезд4.5/5 (121)
- Guidelines For Doing Business in Grenada & OECSДокумент14 страницGuidelines For Doing Business in Grenada & OECSCharcoals Caribbean GrillОценок пока нет
- CHN Nutri LabДокумент4 страницыCHN Nutri LabMushy_ayaОценок пока нет
- PDF BrochureДокумент50 страницPDF BrochureAnees RanaОценок пока нет
- Present Tenses ExercisesДокумент4 страницыPresent Tenses Exercisesmonkeynotes100% (1)
- PM 50 Service ManualДокумент60 страницPM 50 Service ManualLeoni AnjosОценок пока нет
- Electronics 11 02566Документ13 страницElectronics 11 02566卓七越Оценок пока нет
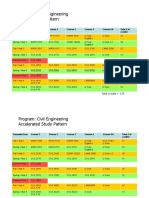
- HKUST 4Y Curriculum Diagram CIVLДокумент4 страницыHKUST 4Y Curriculum Diagram CIVLfrevОценок пока нет
- Investigation Data FormДокумент1 страницаInvestigation Data Formnildin danaОценок пока нет
- Abas Drug Study Nicu PDFДокумент4 страницыAbas Drug Study Nicu PDFAlexander Miguel M. AbasОценок пока нет
- The Marriage of Figaro LibrettoДокумент64 страницыThe Marriage of Figaro LibrettoTristan BartonОценок пока нет
- Bill of Quantities 16FI0009Документ1 страницаBill of Quantities 16FI0009AJothamChristianОценок пока нет
- SPFL Monitoring ToolДокумент3 страницыSPFL Monitoring ToolAnalyn EnriquezОценок пока нет
- Vq40de Service ManualДокумент257 страницVq40de Service Manualjaumegus100% (4)
- Agenda - 2 - Presentation - MS - IUT - Thesis Proposal PPT Muhaiminul 171051001Документ13 страницAgenda - 2 - Presentation - MS - IUT - Thesis Proposal PPT Muhaiminul 171051001Tanvir AhmadОценок пока нет
- Formato MultimodalДокумент1 страницаFormato MultimodalcelsoОценок пока нет
- Kortz Center GTA Wiki FandomДокумент1 страницаKortz Center GTA Wiki FandomsamОценок пока нет
- Pediatric Fever of Unknown Origin: Educational GapДокумент14 страницPediatric Fever of Unknown Origin: Educational GapPiegl-Gulácsy VeraОценок пока нет
- Revenue Memorandum Circular No. 55-2016: For ExampleДокумент2 страницыRevenue Memorandum Circular No. 55-2016: For ExampleFedsОценок пока нет
- API RP 7C-11F Installation, Maintenance and Operation of Internal Combustion Engines.Документ3 страницыAPI RP 7C-11F Installation, Maintenance and Operation of Internal Combustion Engines.Rashid Ghani100% (1)
- Saudi Methanol Company (Ar-Razi) : Job Safety AnalysisДокумент7 страницSaudi Methanol Company (Ar-Razi) : Job Safety AnalysisAnonymous voA5Tb0Оценок пока нет
- Managing Errors and ExceptionДокумент12 страницManaging Errors and ExceptionShanmuka Sreenivas100% (1)
- Concise Selina Solutions Class 9 Maths Chapter 15 Construction of PolygonsДокумент31 страницаConcise Selina Solutions Class 9 Maths Chapter 15 Construction of Polygonsbhaskar51178Оценок пока нет
- FluteДокумент13 страницFlutefisher3910% (1)
- Chapter1 Intro To Basic FinanceДокумент28 страницChapter1 Intro To Basic FinanceRazel GopezОценок пока нет
- Dependent ClauseДокумент28 страницDependent ClauseAndi Febryan RamadhaniОценок пока нет
- Institutions and StrategyДокумент28 страницInstitutions and StrategyFatin Fatin Atiqah100% (1)
- Properties of WaterДокумент23 страницыProperties of WaterNiken Rumani100% (1)
- Oil List: Audi Front Axle DriveДокумент35 страницOil List: Audi Front Axle DriveAska QianОценок пока нет
- Subeeka Akbar Advance NutritionДокумент11 страницSubeeka Akbar Advance NutritionSubeeka AkbarОценок пока нет
- E-CRM Analytics The Role of Data Integra PDFДокумент310 страницE-CRM Analytics The Role of Data Integra PDFJohn JiménezОценок пока нет