Академический Документы
Профессиональный Документы
Культура Документы
Alopesia Guideline
Загружено:
Ismail Bin Rahmat0 оценок0% нашли этот документ полезным (0 голосов)
45 просмотров5 страницAlopesia
Авторское право
© © All Rights Reserved
Доступные форматы
PDF, TXT или читайте онлайн в Scribd
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документAlopesia
Авторское право:
© All Rights Reserved
Доступные форматы
Скачайте в формате PDF, TXT или читайте онлайн в Scribd
0 оценок0% нашли этот документ полезным (0 голосов)
45 просмотров5 страницAlopesia Guideline
Загружено:
Ismail Bin RahmatAlopesia
Авторское право:
© All Rights Reserved
Доступные форматы
Скачайте в формате PDF, TXT или читайте онлайн в Scribd
Вы находитесь на странице: 1из 5
242
From Duke University Medical Center, Durham
a
; University of Minnesota,
Minneapolis
b
; Pontefract General Infirmary
c
; University of California
at San Francisco
d
; Northwest Cutaneous Research Specialists,
Portland
e
; The University of British Columbia, Vancouver
f
; and
Johnson & Johnson, Skin Biology Research Center, Skillman.
g
Reprint requests: Elise A. Olsen, MD, Professor of Medicine, Duke
University Medical Center, Box 3294, Durham, NC 27710.
J Am Acad Dermatol 1999;40:242-6.
*Developed from the Alopecia Areata Consensus meeting sponsored by
the National Alopecia Areata Foundation at the First Tricontinental
Meeting of the Hair Research Societies, Brussels, Belgium, Oct 8,
1995. Participants are listed at the end of the guidelines.
Copyright 1999 by the American Academy of Dermatology, Inc.
0190-9622/99/$8.00 + 0 16/1/95940
I. PURPOSE
To establish criteria for selecting and assessing subjects for both clinical and laboratory studies of
alopecia areata, thereby facilitating collaboration, comparison of data, and the sharing of patient-derived tissue
II. DEFINITION OF ALOPECIA AREATA
Alopecia areata is a dermatologic disease characterized in its limited form by circumscribed round
or oval patches of alopecia with well-demarcated borders between normal and affected scalp. There
is no scale or induration of the scalp and no loss of follicular markings. Disease extent may progress
from this limited form to complete loss of hair on the scalp and/or body.
III. INCLUSION CRITERIA
These guidelines apply only to terminal hair loss or growth on the scalp.
These guidelines focus on the major forms of alopecia areata (patchy alopecia areata, alopecia totalis,
and alopecia universalis) and their expression on the scalp. The terms alopecia totalis and alopecia
universalis imply 100% scalp hair loss.
Areas of hair loss other than on the scalp may be assessed and documented in the data collected on
each patient. (See Section IV. B)
IV. CRITERIA FOR MEASURING EXTENT OF INVOLVEMENT
Those data items in boldface type should be filled out in toto. Those data items not in bold are option-
al and can be filled out as desired by the investigator.
A. The proportion of scalp involvement is determined by dividing the scalp into 4 quadrants and
estimating the percentage of the scalp surface that all the alopecic areas would occupy if placed
together. The following groups will be used:
S: Scalp hair loss
_____S
0
= No hair loss _____S
4
= 76%-99% hair loss
_____S
1
= 25% hair loss _____a = 76%-95% hair loss
_____S
2
= 26%-50% hair loss _____b = 96%-99% hair loss
_____S
3
= 51%-75% hair loss _____S
5
= 100% hair loss
B. Other areas of alopecia or involvement by alopecia areata may be noted:
B: Body hair loss
_____B
0
= No body hair loss _____B
2
= 100% body (excluding scalp) hair loss
_____B
1
= Some body hair loss
N: Nail involvement
_____N
0
= No nail involvement
_____N
1
= Some nail involvement
_____a. Twenty-nail dystrophy/trachyonychia (must be all 20 nails)
SPECIAL ARTICLE
Alopecia areata investigational assessment
guidelines*
Elise Olsen, MD,
a
Maria Hordinsky, MD,
b
Susan McDonald-Hull, MB, FRCP,
c
Vera Price, MD,
d
Janet Roberts, MD,
e
Jerry Shapiro, MD,
f
and Kurt Stenn, MD
g
Durham, North Carolina; Minneapolis, Minnesota; Pontefract, United Kingdom;
San Francisco, California; Portland, Oregon; Vancouver, British Columbia, Canada;
Skillman, New Jersey
Journal of the American Academy of Dermatology
Volume 40, Number 2, Part 1 Olsen et al 243
C. Terminology
The term alopecia totalis is S
5
B
0
only and is 100% scalp terminal hair loss.
The term alopecia totalis/alopecia universalis (AT/AU) is S
5
B
0
-B
2
and implies 100% scalp
terminal hair loss with variable body hair loss.
The term alopecia universalis is S
5
B
2
and is 100% scalp terminal hair and 100% body hair loss.
V. ALOPECIA AREATA DATABASE
A. Essential background data
Patients initials__________
Date of intake___________
Age__________
Date of birth__________
Age at onset of first episode of alopecia areata__________
First episode of alopecia areata (month/year of onset)__________
Current episode alopecia areata
Age of onset__________
Month/year of onset__________
Duration of current episode (months)__________
Extent of hair loss__________(S
0
-S
5
, B
0
-B
2
: as defined in IVA and IVB)
Sex
Male_____
Female_____
Racial group
American Indian or Alaskan native_____
Asian or Pacific Islander_____
Black, not of Hispanic origin_____
Hispanic_____
White, not of Hispanic origin_____
Predominant hair color
Black_____
Brown_____
Red_____
Blond_____
Gray_____
White_____
B. Prior history of alopecia areata
Number of prior episodes of alopecia areata_____
History of alopecia totalis or alopecia totalis/alopecia universalis at any time
1. > 2 years duration_____
2. 2 years duration_____
C. Pertinent immediate past history
History of infections within 6 months before onset of hair loss
a. Initial episode of alopecia areata
Site of infection__________
Type of infection__________
b. Current episode of alopecia areata
Site of infection__________
Type of infection__________
History of vaccination within 6 months before onset of hair loss
a. Initial episode of alopecia areata
Type of vaccination__________
b. Current episode of alopecia areata
Type of vaccination__________
Patients or parents perception of trigger for hair loss
Initial episode__________
Current episode__________
Journal of the American Academy of Dermatology
February 1999 244 Olsen et al
D. Patient and family medical history
Patient and family
medical history
Atopic dermatitis
Allergic rhinitis
Asthma
Thyroid disease
Hashimoto's thyroiditis
Graves' disease
Vitiligo
Diabetes
Insulin-dependent diabetes
Non-insulin-dependent diabetes
Unknown type
Lupus erythematosus
Pernicious anemia
Rheumatoid arthritis
Ulcerative colitis
Celiac disease
Psoriasis
Other autoimmune disease
Type
Down syndrome
Immunodeficiency
Type
Other
P
a
t
i
e
n
t
M
o
t
h
e
r
F
a
t
h
e
r
S
o
n
D
a
u
g
h
t
e
r
B
r
o
t
h
e
r
S
i
s
t
e
r
M
a
t
e
r
n
a
l
G
r
a
n
d
m
o
t
h
e
r
M
a
t
e
r
n
a
l
G
r
a
n
d
f
a
t
h
e
r
P
a
t
e
r
n
a
l
G
r
a
n
d
m
o
t
h
e
r
P
a
t
e
r
n
a
l
G
r
a
n
d
f
a
t
h
e
r
M
a
t
e
r
n
a
l
A
u
n
t
M
a
t
e
r
n
a
l
U
n
c
l
e
P
a
t
e
r
n
a
l
A
u
n
t
P
a
t
e
r
n
a
l
U
n
c
l
e
In attendance were Sam Alaiti, MD, Brigitte Almond, MD, Ulrike Blume-Peytavi, MD, Jean-Claude Bystryn, MD,
Nigel Hibberts, MD, Maria Hordinsky, MD, Satoshi Itami, MD, Vicki Kalabokes, Ulrike Lichti, PhD,
Takashi Masuai, MD, Andrew McDonagh, MD, Susan McDonald-Hull, MB, FRCP, Andrew Messenger, MD, Kazoo
Murato, MD, Michael Nutbrown, PhD, Roy Oliver, PhD, Elise Olsen, MD, Giovanni Orrechia, MD, Ralf Paus, MD,
Vera Price, MD, Valerie Randall, PhD, Janet Roberts, MD, Marty Sawaya, MD, PhD, Jerry Shapiro, MD,
Kurt Stenn, MD, John Sundberg, DVM, PhD, Susan Takayasu, MD, Julie Thornton, PhD, Dominique Van Neste, MD,
and David Whiting, MD.
Journal of the American Academy of Dermatology
Volume 40, Number 2, Part 1 Olsen et al 245
COMMENTARY
Alopecia areata is a disorder with many clinical
presentations, from a single patch of hair loss on
the scalp or body to complete scalp and/or body
hair loss to diffuse scalp hair thinning without dis-
crete patches of loss. The hair loss may be the sin-
gle obvious clinical abnormality or there may be
associated nail abnormalities. Less commonly,
there may be evidence of associated conditions
(primarily categorized as autoimmune) such as
Hashimotos thyroiditis and vitiligo. Alopecia
areata clearly has a genetic component, but the
specific genetic linkage may vary with the hair
loss phenotype. Other potentially hereditary fac-
tors such as atopy may be linked to severity of dis-
ease and refractoriness to therapy. The importance
of environmental factors in triggering hair loss or
modifying the subsequent course is uncertain.
Previously, variable attention was paid to the
clinical aspects of patients with alopecia areata
whose tissue or blood was used for clinical inves-
tigation. However, the type, extent, and duration of
hair loss, presence of other clinical abnormalities,
genetic factors, and other concurrent or preceding
immunologic events may greatly (and without tak-
ing these into account, unknowingly) influence the
test results. Moreover, clinical studies that have
attempted to track the clinical course of alopecia
areata in relation to a variety of factors or to deter-
mine a response to treatment have been hampered
by the lack of a method to clearly depict the type
and extent of hair loss that would, in turn, facilitate
pooling of data. The guidelines developed and pre-
sented herein are a studied attempt to correct this
situation for clinical and bench researchers alike
by providing a means by which to communicate
the specifics of the clinical, genetic, and pertinent
environmental factors specific to a study patient
with alopecia areata. It is also a first step toward
establishing a fruitful alopecia areata database.
To facilitate usage of the aforementioned guide-
lines, the following clarifications are offered:
1. There are several ways to determine the per-
centage of scalp hair loss and whichever way is
easiest for a particular investigator is fine.
However, whatever method is chosen, it should be
used uniformly for all patients at a given site. If
repetitive assessments are done over time in a
given patient, the same investigator should do all
of the assessments or if two or more investigators
are rating a patients hair loss at different time
points, then there must previously have been found
a good reproducibility of assessments between
investigators.
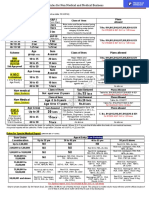
To determine percentage scalp hair loss, one
can:
a. Mentally divide the scalp into 4 quadrants
(Fig 1) and estimate the percentage of the scalp
surface that all the alopecic areas would occupy if
placed together.
b. Use the visual aid provided for determin-
ing percentage hair loss (Fig 2), which gives the
investigator a graphic representation of the percent-
age surface area of the scalp covered by the quad-
rants demarcated which, taken together, equal
100% of the scalp. One can then determine the
percentage of scalp hair lost in a given quadrant and
multiply this by the total scalp area delineated by
that quadrant and add the resultant numbers for each
quadrant. For example, if one fourth (25%) of the
back area of the scalp was devoid of hair, then 0.25
24% = 6% scalp hair loss in this quadrant. In this
same patient, if the top of the scalp had 40% loss,
then 0.4 40% = 16% scalp hair loss in this
section. If the sides of the scalp in this patient had
no loss, the total scalp hair loss for this person
would thus be 6% + 16% = 22%, or S
1
by the
guidelines classification.
c. Where scalp hair loss is extensive (ie,
where > 90% of the scalp hair is lost), it is often
easier to reverse this procedure and to determine
the amount of hair remaining versus lost on the
scalp. If one determines that 8% of scalp hair
remains, obviously this is also 92% loss or S
4
(S
4a
,
to be more specific) according to the guidelines
classification.
d. The investigator may also draw the
alopecic areas directly on the diagrams for a gen-
eral means of documenting location and extent of
loss or, if the areas of loss are very discrete, to
determine percentage of loss by an image analyz-
er. Drawing the lesions directly on the diagrams is
not necessary to determine percentage of hair loss
using methods a-c, as given above.
2. Vellus hair is not taken into account in this
system, only terminal hair. A fine downy hair
growth on the scalp that is otherwise devoid of ter-
minal hair would be characterized as alopecia total-
is (AT) or S
5
.
3. We encourage investigators to examine all of
the alopecia areata patients body for hair and nail
abnormalities so that body hair loss and nail
Journal of the American Academy of Dermatology
February 1999 246 Olsen et al
involvement can be most accurately determined
and recorded. Determination of body hair loss and
nail involvement can be done without examining
the patient in toto; a patient who only exposes his
or her arms, face, and scalp to examination can be
determined to have B
1
and N
1
classification (ie,
some body hair loss and some nail involvement).
However, this same patient, if undressed, may
more accurately have B
2
and N
1a
(total body hair
loss and 20-nail dystrophy) classification. In this
case, B
1
and N
1
rating, although not totally accu-
rate, is still correct and is superior to not answer-
ing these questions at all. Please note that a patient
must be checked for total body hair loss to desig-
nate that person as having alopecia universalis
(S
5
B
2
).
4. For reporting purposes, the terms alopecia
totalis (AT) and alopecia universalis (AU) may
still be used, but they are defined narrowly (ie, AT
is 100% terminal scalp hair loss without any body
hair loss and AU is 100% terminal scalp hair and
body hair loss). Alopecia totalis/alopecia univer-
salis (AT/AU) is the term now recommended to use
to define AT with variable amounts of body hair
loss. A patient with extensive, but not complete,
terminal scalp hair loss and extensive orcomplete
body hair loss is not defined by AT, AU, or AT/AU.
Elise A. Olsen, MD
Duke University Medical Center
Fig 1. Visual aid for estimating percentage scalp hair
loss. (Described by Price VH. In: Khoury EL, Price
VH, Abdel-Salam MM, Stern M, Greenspan JS.
Topical minoxidil in alopecia areata: no effect on the
perifollicular lymphoid infiltration. J Invest Dermatol
1992;99:40-7.)
Fig 2. Visual aid for estimating percentage scalp hair
loss. (Olsen EA, Canfield DC. Canfield Scientific;
Fairfield, NJ.)
% = percentage of scalp surface area in region outlined.
Вам также может понравиться
- Science in The Art of Osteopathy PDFДокумент378 страницScience in The Art of Osteopathy PDFPetru Acozmei100% (5)
- Urethral Trauma: Sub Bagian Urologi Bagian / SMF Bedah FK Uns/Rsud Dr. MoewardiДокумент19 страницUrethral Trauma: Sub Bagian Urologi Bagian / SMF Bedah FK Uns/Rsud Dr. MoewardiAtika SugiartoОценок пока нет
- CH 04Документ14 страницCH 04Fernando MoralesОценок пока нет
- Ansi+asse+z359 13-2013Документ54 страницыAnsi+asse+z359 13-2013Oscar Casso100% (1)
- Pi Is 0190962223009799Документ6 страницPi Is 0190962223009799Stefano HeringerОценок пока нет
- Alopecia AreataДокумент8 страницAlopecia AreataPedro López CastroОценок пока нет
- Review of Quality of Life Studies in Women With AlДокумент5 страницReview of Quality of Life Studies in Women With AlLouie MercadoОценок пока нет
- Akshay ProtocolДокумент22 страницыAkshay Protocolakshay9610meenaОценок пока нет
- An Open Clinical Study To Evaluate Safety and Efficacy of Hairzone Solution in The Management of Diffuse Hair LossДокумент4 страницыAn Open Clinical Study To Evaluate Safety and Efficacy of Hairzone Solution in The Management of Diffuse Hair LossShrinivas PrabhuОценок пока нет
- Efficacy of Low Level Laser Therapy in The Treatment of Alopecia AreataДокумент6 страницEfficacy of Low Level Laser Therapy in The Treatment of Alopecia AreataRo KohnОценок пока нет
- Alopecia Areata Na Barba Cervantes2017Документ8 страницAlopecia Areata Na Barba Cervantes2017Anderson FerreiraОценок пока нет
- Guidelines Acne VulgarisДокумент14 страницGuidelines Acne VulgarisKym DominguezОценок пока нет
- Comprehensive Overview and Treatment Update On Hair LossДокумент8 страницComprehensive Overview and Treatment Update On Hair LossmirafitrОценок пока нет
- Indian Journal of Dermatology, Venereology and Leprology (IJDVL)_ Diffuse alopecia areata is associated with intense inflammatory infiltration and CD8+ T cells in hair loss regions and an increase in serum IgE level _ _b_Ying Zhao_sup_1__sup_, Bin ZhaДокумент5 страницIndian Journal of Dermatology, Venereology and Leprology (IJDVL)_ Diffuse alopecia areata is associated with intense inflammatory infiltration and CD8+ T cells in hair loss regions and an increase in serum IgE level _ _b_Ying Zhao_sup_1__sup_, Bin ZhaBrayan Cabanillas MirandaОценок пока нет
- 88 Hair Growth DisordrДокумент24 страницы88 Hair Growth DisordrAlivia Soeraya100% (1)
- Comprehensive Overview and Treatment Update On Hair LossДокумент9 страницComprehensive Overview and Treatment Update On Hair LossZuldan KaramiОценок пока нет
- Alopecia Areata VOP ReportДокумент28 страницAlopecia Areata VOP ReportRo KohnОценок пока нет
- Alopecia AreataДокумент4 страницыAlopecia AreataMellisa Aslamia AslimОценок пока нет
- Alopecia AreataДокумент11 страницAlopecia AreataMuhammad Azhari Airlangga100% (1)
- Alopecia Areata: News On Diagnosis, Pathogenesis and TreatmentДокумент22 страницыAlopecia Areata: News On Diagnosis, Pathogenesis and TreatmentMariaAmeliaGoldieОценок пока нет
- HAIRLOSSДокумент16 страницHAIRLOSSIrawan Pandu Buditomo100% (1)
- Evaluation of CD4 and CD8 in Al-Diwaniyah Alopecia Patients by ELIZAДокумент8 страницEvaluation of CD4 and CD8 in Al-Diwaniyah Alopecia Patients by ELIZACentral Asian StudiesОценок пока нет
- AutoimmuneДокумент5 страницAutoimmuneTiara ArazsyОценок пока нет
- Hair and Scalp Evaluation: The Trichogram: Practical DermatologyДокумент10 страницHair and Scalp Evaluation: The Trichogram: Practical DermatologyFelipe NunesОценок пока нет
- Alopecia HandoutДокумент4 страницыAlopecia HandoutEmAlNourОценок пока нет
- JURNAL KulitДокумент10 страницJURNAL KulitDita TifaniadiОценок пока нет
- What's To Know About Alopecia Areata?Документ9 страницWhat's To Know About Alopecia Areata?anton deeОценок пока нет
- Innovative Method of Alopecia Treatment by Autologous Adipose-Derived SVFДокумент9 страницInnovative Method of Alopecia Treatment by Autologous Adipose-Derived SVFStefano HeringerОценок пока нет
- Macbeth Et Al-2016-British Journal of DermatologyДокумент13 страницMacbeth Et Al-2016-British Journal of DermatologyRo KohnОценок пока нет
- Hair Loss in WomenДокумент11 страницHair Loss in WomenLENINОценок пока нет
- Is Every Patient of Hair Loss A Candidate For Hair Transplant - Deciding Surgical Candidacy in Pattern Hair Loss - PMCДокумент12 страницIs Every Patient of Hair Loss A Candidate For Hair Transplant - Deciding Surgical Candidacy in Pattern Hair Loss - PMChi_its_ariОценок пока нет
- Hairloss Cream002Документ5 страницHairloss Cream002JaTi NurwigatiОценок пока нет
- Contents DetДокумент4 страницыContents DetNhật Nguyễn QuangОценок пока нет
- Impact of Scalp Cooling On Chemo Induced Alopecia Wig Use and Hair Growth in Patients With CancerДокумент5 страницImpact of Scalp Cooling On Chemo Induced Alopecia Wig Use and Hair Growth in Patients With CancerRo KohnОценок пока нет
- Choosing Wisely Master ListДокумент92 страницыChoosing Wisely Master ListrobertojosesanОценок пока нет
- 10 11648 J Ajcem 20160404 12Документ5 страниц10 11648 J Ajcem 20160404 12Ro KohnОценок пока нет
- AlopeciaДокумент11 страницAlopeciaAnonymous kltUTa100% (1)
- ACITIVITY 1 (Week 1) Preliminary Reading For Students 1. Health Assessment Chapter 30 Page 513 (Fundamentals of Nursing 10 Edition)Документ5 страницACITIVITY 1 (Week 1) Preliminary Reading For Students 1. Health Assessment Chapter 30 Page 513 (Fundamentals of Nursing 10 Edition)Lore Anne Mhae SantosОценок пока нет
- Actinic Cheilitis: Clinical Characteristics Observed in 75 Patients and A Summary of The Literature of This Often Neglected Premalignant DisorderДокумент9 страницActinic Cheilitis: Clinical Characteristics Observed in 75 Patients and A Summary of The Literature of This Often Neglected Premalignant DisorderYustisia CharissaОценок пока нет
- Alopecia Areata ManejoДокумент14 страницAlopecia Areata ManejoVar AndaОценок пока нет
- Guidelines Acne Vulgaris PDFДокумент14 страницGuidelines Acne Vulgaris PDFmonitamiftahОценок пока нет
- Examining The Potential For Koebnerization andДокумент10 страницExamining The Potential For Koebnerization and2vszgwndvtОценок пока нет
- Sumber 21Документ17 страницSumber 21Dita N HapsariОценок пока нет
- Alopecia Areata Zinc Copper SeleniumДокумент14 страницAlopecia Areata Zinc Copper SeleniumpomodoroОценок пока нет
- ACR EULAR 2016 Sjogrens Classification CriteriaДокумент11 страницACR EULAR 2016 Sjogrens Classification CriteriaFelipe Jaeger de BelliОценок пока нет
- Alopecia AreataДокумент12 страницAlopecia AreataJohnОценок пока нет
- Med 4 2Документ6 страницMed 4 2Zohaib HassanОценок пока нет
- Clinical Review - FullДокумент5 страницClinical Review - FullsandeepОценок пока нет
- Alopecia Areata: Amos Gilhar, M.D., Amos Etzioni, M.D., and Ralf Paus, M.DДокумент7 страницAlopecia Areata: Amos Gilhar, M.D., Amos Etzioni, M.D., and Ralf Paus, M.DSistaОценок пока нет
- Oftalmologi Ok 5Документ4 страницыOftalmologi Ok 5Jericho JeruzalemОценок пока нет
- Low-Dose Oral Minoxidil in The Treatment of Alopecia - Evidence and Experience-Based Consensus Statement of Indian Experts - PMCДокумент12 страницLow-Dose Oral Minoxidil in The Treatment of Alopecia - Evidence and Experience-Based Consensus Statement of Indian Experts - PMCAbhinav ChawlaОценок пока нет
- Epigenetics and DermatologyОт EverandEpigenetics and DermatologyQianjin LuРейтинг: 3 из 5 звезд3/5 (1)
- 1 s2.0 S019096222302399XДокумент5 страниц1 s2.0 S019096222302399Xsf2svj6t7hОценок пока нет
- Hair Loss and Its Management in ChildrenДокумент23 страницыHair Loss and Its Management in ChildrenDiana Sofia GonzalezОценок пока нет
- 5%minox Vs 5%minox and 0.05% BetamethasoneДокумент4 страницы5%minox Vs 5%minox and 0.05% BetamethasoneSopotsОценок пока нет
- Case of Alopecia Areata Originated From Dental Focus: Created By: Hafidhotussadiah Taufik RizalДокумент18 страницCase of Alopecia Areata Originated From Dental Focus: Created By: Hafidhotussadiah Taufik RizalhafodhotusadiahОценок пока нет
- Systematic Approach To Hair Loss in Women: Ralph M. TrüebДокумент15 страницSystematic Approach To Hair Loss in Women: Ralph M. TrüebErika Alvarez IbarraОценок пока нет
- Ethnic Hair Update Past and PresentДокумент7 страницEthnic Hair Update Past and PresentANGIE JULIETH BELLAIZAC RIASCOSОценок пока нет
- Jurnal IkkДокумент4 страницыJurnal IkkOsdatilla Esa PutriОценок пока нет
- Alopecia Areata Is A Medical Disease: OmmentaryДокумент3 страницыAlopecia Areata Is A Medical Disease: OmmentaryNurfadillah Putri Septiani PattinsonОценок пока нет
- UntitledДокумент334 страницыUntitledLocalVet TunariОценок пока нет
- Lesser Known Homoeopathic Medicines of Alopecia Areata.20200718115446Документ9 страницLesser Known Homoeopathic Medicines of Alopecia Areata.20200718115446BruntОценок пока нет
- Portfolio In: Morong National High SchoolДокумент5 страницPortfolio In: Morong National High SchoolSophrina Jazmynrose CruzОценок пока нет
- 157-Article Text-621-1-10-20120514Документ7 страниц157-Article Text-621-1-10-20120514loОценок пока нет
- Recruit HandbookДокумент72 страницыRecruit HandbookJUAN RAMON0% (1)
- Risk Assessment: Severity (1, 2 or 3)Документ1 страницаRisk Assessment: Severity (1, 2 or 3)Ulviyye ElesgerovaОценок пока нет
- The Amazing DeclineДокумент26 страницThe Amazing DeclineSuzanne HumphriesОценок пока нет
- Chest Drains Al-WPS OfficeДокумент16 страницChest Drains Al-WPS OfficeisnainiviaОценок пока нет
- Cosmetic Surgery EssayДокумент7 страницCosmetic Surgery Essayalisharenee0550% (2)
- hsg261 Health and Safety in Motor Vehicle Repair and Associated Industries PDFДокумент101 страницаhsg261 Health and Safety in Motor Vehicle Repair and Associated Industries PDFpranksterboyОценок пока нет
- Basic Nutrition: Lesson 2Документ13 страницBasic Nutrition: Lesson 2Shaina DaquilОценок пока нет
- Factors Affecting Demand For Soft DrinksДокумент8 страницFactors Affecting Demand For Soft Drinksخلود البطاحОценок пока нет
- Freedom From DistractibilityДокумент4 страницыFreedom From DistractibilityΚων/να ΠαπОценок пока нет
- Overconfidence As A Cause of Diagnostic Error in Medicine PDFДокумент22 страницыOverconfidence As A Cause of Diagnostic Error in Medicine PDFIulianZaharescuОценок пока нет
- Complicated GrievingДокумент117 страницComplicated GrievingEra Galuh100% (1)
- P.E & Health G11-Q1-M7Документ13 страницP.E & Health G11-Q1-M7John Gerald CantancioОценок пока нет
- Rules For Non Medical BusinessДокумент1 страницаRules For Non Medical BusinessAbhijit AminpurОценок пока нет
- Harga Obat Generik E-KatalogueДокумент4 страницыHarga Obat Generik E-KatalogueMuhammad FarilОценок пока нет
- Aira Noreen Leyva - Resume ReviewДокумент2 страницыAira Noreen Leyva - Resume Reviewapi-447475293Оценок пока нет
- Ob MidtermДокумент5 страницOb MidtermSheila Tolentino-BelanioОценок пока нет
- Worksheet Normal Distribution PDFДокумент3 страницыWorksheet Normal Distribution PDFJustin Eduard MarzanОценок пока нет
- American Soc. of Addiction Medicine Naloxone StatementДокумент5 страницAmerican Soc. of Addiction Medicine Naloxone Statementwebmaster@drugpolicy.orgОценок пока нет
- Mobil™ Dexron-VI ATF: Product DescriptionДокумент2 страницыMobil™ Dexron-VI ATF: Product DescriptionOscar GonzálezОценок пока нет
- Restobar FSДокумент58 страницRestobar FSGabrielle Alonzo100% (1)
- PAT, CGMP For The 21st Century and ICH Q8, Q9, Q10Документ28 страницPAT, CGMP For The 21st Century and ICH Q8, Q9, Q10Narendrakumar100% (2)
- Paramedical 1Документ156 страницParamedical 1Iswarya MohanОценок пока нет
- Nutritional Assessement Anthropometric MethodsДокумент77 страницNutritional Assessement Anthropometric MethodsElias Libay100% (1)
- Hospital Income Benefit Plan HIBДокумент2 страницыHospital Income Benefit Plan HIBIngrid SastrilloОценок пока нет