Академический Документы
Профессиональный Документы
Культура Документы
Tetanus 2
Загружено:
anoorfitriana0 оценок0% нашли этот документ полезным (0 голосов)
8 просмотров5 страницtetanus
Авторское право
© © All Rights Reserved
Доступные форматы
DOCX, PDF, TXT или читайте онлайн в Scribd
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документtetanus
Авторское право:
© All Rights Reserved
Доступные форматы
Скачайте в формате DOCX, PDF, TXT или читайте онлайн в Scribd
0 оценок0% нашли этот документ полезным (0 голосов)
8 просмотров5 страницTetanus 2
Загружено:
anoorfitrianatetanus
Авторское право:
© All Rights Reserved
Доступные форматы
Скачайте в формате DOCX, PDF, TXT или читайте онлайн в Scribd
Вы находитесь на странице: 1из 5
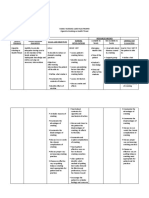
Tetanus
(Lock Jaw, Lockjaw, Clostridium tetani)
In this factsheet:
The Facts on Tetanus
Causes of Tetanus
Symptoms and Complications of Tetanus
Diagnosing Tetanus
Treating and Preventing Tetanus
The Facts on Tetanus
Tetanus is a condition caused by a nerve toxin that is produced by the bacterium Clostridium tetani,
a cousin of the bacteria that cause gangrene and botulism. It remains a serious worldwide public
health problem, killing over 500,000 people each year.
In developed countries, however, the introduction of a vaccine in the 1950s has all but eradicated
this disease. The cases of tetanus that do occur are often seen in those who either have not been
vaccinated or have failed to keep their immunizations up to date, as protection from the vaccine
declines over time.
Canada now averages about 4 cases a year. Only 5 people have died of tetanus in this country since
1980.
Causes of Tetanus
Clostridia are anaerobic bacteria, meaning they thrive best in the absence of oxygen. They're
commonly found in soil, but can also be found in the lower intestines of mammals. They can produce
spores that can survive for years.
Anyone who cuts himself or herself with a dirty object is at risk of getting Clostridium tetani in the
wound. The bacteria are only really dangerous if they're in wound tissue that's cut off from a good
oxygen supply. "Crush" wounds and deep puncture wounds are good candidates for such infections,
as are burns, surgical wounds, and punctures with dirty needles. Most cases of tetanus in North
America are found in older people following surgery and in intravenous drug users who reuse
unclean syringes.
There's also the occasional case of tetanus linked to childbirth. The mother can develop infection in
the uterus, and the baby in the stump of the umbilical cord.
As the bacteria grow and multiply, they produce a nerve toxin. As with botulism, it's the toxin that
does the damage, not the organisms themselves. The toxin binds to nerve endings that normally
serve to calm the muscles. In the absence of receiving such calming signals, the muscles contract and
become rigid and very sensitive to external input, leading to spasms.
Symptoms and Complications of Tetanus
Symptoms may appear anywhere from 2 days to 6 weeks after the wound has been infected, but the
typical incubation period (time between infection and symptoms) is 5 to 10 days. Symptoms can be
mild or severe and include:
chills
difficulty swallowing
headache
irritability
jaw and neck stiffness
low fever
restlessness
sore throat
stiff arms and legs
Symptoms soon progress to classic tetanus:
difficulty opening the jaw - that's why tetanus is sometimes called "lockjaw"
muscle spasms in the back, neck, or abdomen
People with tetanus often develop a fixed expression with a tight, stretched smile and arched
eyebrows. They often go into painful whole-body spasms when slightly disturbed, for example by
fluffing their pillow. They may sweat a great deal during these spasms. They may be unable to speak
because of spasms in the chest or throat - these can also make breathing difficult. Rigidity in the
bladder and bowels can cause retention of urine and constipation. Blue lips or nail beds are a sign of
depressed breathing, meaning theres too little oxygen or too much carbon dioxide in the blood.
People with tetanus are usually mentally alert. The pulse can be fast, but fever is rarely very high.
Sometimes the face is unaffected and the spasms are confined to muscles near the wound. In this
case, there is a better chance of a full recovery.
Sometimes the face is unaffected and the spasms are confined to muscles near the wound. In this
case, there is a better chance of a full recovery.
Complications of tetanus can include pneumonia, broken bones, skin sores, muscle tears, and low
blood pressure.
Diagnosing Tetanus
The bacteria can't always be detected in the wound, but the particular combination of symptoms
and a recent wound usually paints a clear picture of tetanus.
Meningitis and encephalitis (brain infections) can cause similar spasms and rigidity, but they usually
interfere with senses such as hearing, while tetanus doesn't. Taking a sample of cerebrospinal fluid
(CSF) allows the doctor to rule out both of these diseases.
Treating and Preventing Tetanus
People with tetanus need to be in an intensive care unit so they can receive treatment and
continuous monitoring.
Treatment of tetanus usually includes:
supportive care
medications to control muscle spasms
antibiotics and tetanus immune globulin to manage the infection
wound treatment
vaccination
Supportive care: The biggest threat is to breathing. People who get tetanus usually have
mechanically assisted ventilation through a breathing tube. This may involve a tracheostomy, which
is a tube inserted directly through a hole cut in the throat.
Because people with tetanus may not be able to swallow, they are usually given nourishment either
intravenously or through a nasogastric (NG) tube, which is inserted through the nose, past the
throat, and into the stomach. A catheter (tube) may also be inserted in the bladder to drain it.
Medications to control muscle spasms: Medications such as benzodiazepines (e.g., midazolam,
diazepam), dantrolene, or baclofen are given to reduce muscle spasms*.
Antibiotics and tetanus immune globulin: As the consequences of tetanus are due to a toxin
produced by the bacteria, an injection of antitoxin is given to the patient. This antitoxin is an
antibody preparation that will bind any remaining toxin and prevent it from binding to the nerve
cells. They may also need tetanus immune globulin (a blood product from an immune person).
Antibiotics (e.g., metronidazole, penicillin) are used to kill the tetanus bacteria, the source of the
toxin, but they are too slow-acting to be the only treatment. If there is an open wound where the
tetanus bacteria are thriving, then that wound is surgically cleaned to physically remove any tetanus
bacteria.
Vaccination: In people who develop tetanus, the amount of bacteria causing the disease is too small
to lead to an effective immune response. This means that these people could get tetanus again. All
people who have had tetanus should also receive a tetanus vaccination as part of treatment.
Tetanus is a preventable disease, thanks to the development of a vaccine. When you see a doctor for
a cut that might be dirty or infected, the preventive treatment you get depends on your vaccination
status. The tetanus vaccine provides good protection for 5 years. Its effectiveness then slowly tails
off.
For clean, minor wounds, people who have been vaccinated in the last 10 years don't need any
treatment. People who were vaccinated more than 10 years ago get a booster shot of the vaccine,
which consists of a weakened form of the tetanus toxin. For deep or dirty wounds, people who
received their last tetanus booster more than 5 years ago will need another booster shot.
Those who have never been vaccinated, or have an uncertain vaccination history, need tetanus
immune globulin. They also need to be vaccinated against tetanus. People with deep, dirty wounds
who have a suppressed immune system (e.g., people with HIV or other immune system problems)
will be given tetanus immune globulin.
Children today are normally vaccinated at 2, 4, and 6 months, then again at 18 months and once
more around age 4 to 6. Most children will receive a vaccine that protects against tetanus,
diphtheria, pertussis, polio, and Hib (Haemophilus influenzae type b) for the doses given at 2, 4, 6,
and 18 months of age. A vaccine that protects against tetanus, diphtheria, pertussis (whooping
cough), and polio is usually given at 4 to 6 years of age. A further shot, with the adult diphtheria-
tetanus-pertussis vaccine, is recommended around age 14 to 16. Adults should continue to get
booster shots every 10 years to minimize the risk of tetanus.
Other vaccination schedules may be used for adults or children over 7 years of age who have not
been previously vaccinated. Talk to your health care provider for more information.
You can also reduce your risk of tetanus by cleaning all wounds thoroughly, rinsing them with clean
water and washing the area around the wound with soap and water. If the wound is deep and dirty,
see your doctor.
You might consider wearing knee and elbow pads during sports that are likely to involve violent
contact with the ground. Avoid going barefoot while outside of your house. This will help to prevent
infection from accidentally stepping on sharp, dirty objects.
*All medications have both common (generic) and brand names. The brand name is what a specific
manufacturer calls the product (e.g., Tylenol). The common name is the medical name for the
medication (e.g., acetaminophen). A medication may have many brand names, but only one
common name. This article lists medications by their common names. For more information on
brand names, speak with your doctor or pharmacist.
Вам также может понравиться
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeОт EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeРейтинг: 4 из 5 звезд4/5 (5783)
- The Yellow House: A Memoir (2019 National Book Award Winner)От EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Рейтинг: 4 из 5 звезд4/5 (98)
- Never Split the Difference: Negotiating As If Your Life Depended On ItОт EverandNever Split the Difference: Negotiating As If Your Life Depended On ItРейтинг: 4.5 из 5 звезд4.5/5 (838)
- The Emperor of All Maladies: A Biography of CancerОт EverandThe Emperor of All Maladies: A Biography of CancerРейтинг: 4.5 из 5 звезд4.5/5 (271)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceОт EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceРейтинг: 4 из 5 звезд4/5 (890)
- The Little Book of Hygge: Danish Secrets to Happy LivingОт EverandThe Little Book of Hygge: Danish Secrets to Happy LivingРейтинг: 3.5 из 5 звезд3.5/5 (399)
- Team of Rivals: The Political Genius of Abraham LincolnОт EverandTeam of Rivals: The Political Genius of Abraham LincolnРейтинг: 4.5 из 5 звезд4.5/5 (234)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaОт EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaРейтинг: 4.5 из 5 звезд4.5/5 (265)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryОт EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryРейтинг: 3.5 из 5 звезд3.5/5 (231)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureОт EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureРейтинг: 4.5 из 5 звезд4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersОт EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersРейтинг: 4.5 из 5 звезд4.5/5 (344)
- The Unwinding: An Inner History of the New AmericaОт EverandThe Unwinding: An Inner History of the New AmericaРейтинг: 4 из 5 звезд4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyОт EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyРейтинг: 3.5 из 5 звезд3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreОт EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreРейтинг: 4 из 5 звезд4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)От EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Рейтинг: 4.5 из 5 звезд4.5/5 (119)
- Clinical Pharmacy PHR 405: Chapter 1: General ConsiderationsДокумент24 страницыClinical Pharmacy PHR 405: Chapter 1: General ConsiderationsSamiul Alam Rajib100% (1)
- Arterial Puncture ArmДокумент1 страницаArterial Puncture ArmD M Shawkot HossainОценок пока нет
- Sean Barnett-Nurs362resumeДокумент2 страницыSean Barnett-Nurs362resumeapi-252467227Оценок пока нет
- Carmarthen in SpotlightДокумент1 страницаCarmarthen in SpotlightDigital MediaОценок пока нет
- Bio StatisticsДокумент21 страницаBio StatisticsanaeshklОценок пока нет
- Authorization Letter RaviДокумент1 страницаAuthorization Letter RaviTanmoy Pal ChowdhuryОценок пока нет
- Bimbingan Dokter Hari - CKDДокумент24 страницыBimbingan Dokter Hari - CKDVicky LumalessilОценок пока нет
- Pregnancy Terms ExplainedДокумент4 страницыPregnancy Terms Explainedعبدالرحمن الزيودОценок пока нет
- Understanding Bipolar II DisorderДокумент49 страницUnderstanding Bipolar II DisorderJalishia Mae Dumduma100% (1)
- Family Nursing Care Plan Proper Cigarette Smoking As Health ThreatДокумент2 страницыFamily Nursing Care Plan Proper Cigarette Smoking As Health ThreatWishley Ann PiñedaОценок пока нет
- GVP Annex V AbbreviationsДокумент5 страницGVP Annex V AbbreviationsSilvia PeroniОценок пока нет
- White Lesions of The Oral MucosaДокумент213 страницWhite Lesions of The Oral MucosaJunaid Ramzan100% (1)
- Antiprotozoal DrugsДокумент37 страницAntiprotozoal DrugsMoneto CasaganОценок пока нет
- CCPVДокумент16 страницCCPVdastgirrajaОценок пока нет
- Disseminated Intravascular CoagulationДокумент4 страницыDisseminated Intravascular CoagulationHendra SshОценок пока нет
- New Method For Healing A Pathologic Fracture Using The BioChem Bracing SystemДокумент13 страницNew Method For Healing A Pathologic Fracture Using The BioChem Bracing SystemBioChemBracingОценок пока нет
- Multiple SclerosisДокумент35 страницMultiple SclerosisJc SeguiОценок пока нет
- Chapter 66 - ShockДокумент9 страницChapter 66 - ShockCrysta Venice Tapoc100% (1)
- Glasgow Coma Scale. GCS.Документ3 страницыGlasgow Coma Scale. GCS.Amanda Rodriguez TejedaОценок пока нет
- First Aid Multiple Choice QuestionsДокумент5 страницFirst Aid Multiple Choice QuestionsArunkumar Rangaswamy100% (2)
- Occlusal Considerations in Implant Therapy Clinical Guidelines With Biomechanical Rationale PDFДокумент10 страницOcclusal Considerations in Implant Therapy Clinical Guidelines With Biomechanical Rationale PDFSoares MirandaОценок пока нет
- Esthetic Analysis of The SmileДокумент7 страницEsthetic Analysis of The SmileNitin H.c.Оценок пока нет
- Circumcision Photo Guide: What To Expect After Surgery: Patient and Family EducationДокумент2 страницыCircumcision Photo Guide: What To Expect After Surgery: Patient and Family EducationJashanjot SinghОценок пока нет
- Management of UTIДокумент46 страницManagement of UTIninaguilaОценок пока нет
- Principles of Management of Poisoned Patient: 09/09/1440 DR Abdelmonem G. Madboly 1Документ19 страницPrinciples of Management of Poisoned Patient: 09/09/1440 DR Abdelmonem G. Madboly 1JyotiОценок пока нет
- Managing Hemophilia Care ComprehensivelyДокумент33 страницыManaging Hemophilia Care ComprehensivelyZuna QaziОценок пока нет
- Day 1 BacteriaДокумент251 страницаDay 1 BacteriaLisa NetherlandОценок пока нет
- Necessary Elements of A Dermatologic History and Physical Evaluation PDFДокумент9 страницNecessary Elements of A Dermatologic History and Physical Evaluation PDFkyle31Оценок пока нет
- Case Presentation On Rheumatoid ArthritisДокумент36 страницCase Presentation On Rheumatoid ArthritisGADDAM TEJASWINIОценок пока нет
- Contracted Pelvis Definition, Causes, Diagnosis & ManagementДокумент32 страницыContracted Pelvis Definition, Causes, Diagnosis & ManagementNirupama KsОценок пока нет