Академический Документы
Профессиональный Документы
Культура Документы
Chapter 10 Peritoneium, Omenta, and Internal
Загружено:
SMEY2040 оценок0% нашли этот документ полезным (0 голосов)
196 просмотров62 страницыAnatomic and surgical history of the peritoneum and omenta is found in Table 10-1. Omentum serves to warm intestines, lubricate peritoneal folds, and store fat. Theodoric of tyrone was the first surgeon to use omentium in hernia repair.
Исходное описание:
Оригинальное название
Chapter 10 Peritoneium, Omenta, And Internal
Авторское право
© © All Rights Reserved
Доступные форматы
PDF, TXT или читайте онлайн в Scribd
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документAnatomic and surgical history of the peritoneum and omenta is found in Table 10-1. Omentum serves to warm intestines, lubricate peritoneal folds, and store fat. Theodoric of tyrone was the first surgeon to use omentium in hernia repair.
Авторское право:
© All Rights Reserved
Доступные форматы
Скачайте в формате PDF, TXT или читайте онлайн в Scribd
0 оценок0% нашли этот документ полезным (0 голосов)
196 просмотров62 страницыChapter 10 Peritoneium, Omenta, and Internal
Загружено:
SMEY204Anatomic and surgical history of the peritoneum and omenta is found in Table 10-1. Omentum serves to warm intestines, lubricate peritoneal folds, and store fat. Theodoric of tyrone was the first surgeon to use omentium in hernia repair.
Авторское право:
© All Rights Reserved
Доступные форматы
Скачайте в формате PDF, TXT или читайте онлайн в Scribd
Вы находитесь на странице: 1из 62
5/23/2014 Print: Chapter 10.
Peritoneum, Omenta, and Internal Hernias
http://web.uni-plovdiv.bg/stu1104541018/docs/res/skandalakis' %20surgical%20anatomy%20-%202004/Chapter%2010_%20Peritoneum,%20Omenta,%20and%2 1/62
Print | Close Window
Note: Large images and tables on this page may necessitate printing in landscape mode.
Skandalakis' Surgical Anatomy > Chapter 10. Peritoneum, Omenta, and Internal Hernias >
HISTORY
The anatomic and surgical history of the peritoneum and omenta is found in Table 10-1.
Table 10-1. Anatomic and Surgical History of the Peritoneum and Omenta
Egypt 1500
B.C.
Ebers Papyrus contains first description of the peritoneum
Homer (fl. 8th cent. B.C.) "Dertron" (omentum) mentioned in The Odyssey
Hippocrates of Cos (460-370
B.C.)
Case reports of abdominal injuries in which the omentum became extruded and gangrenous
Aristotle (384-322 B.C.) Omentum composed of "warm fatty material" attached to the stomach; speeds digestion by its warmth
Eristratos (304-250 B.C.) Stated that omentum has no special function
Celsus (fl. ca. 25 A.D.) Described surgery on extruded omentum and various hernias
Galen (128-199) Anatomy of omental vasculature and peritoneal folds. Omentum serves to warm intestines, lubricate peritoneum, and store
fat
Paul of Aegina (625-690) Detailed treatment of abdominal wounds involving the omentum
Avicenna (980-1037) Detailed anatomic description of the omentum
Frugardi (12th cent.) Stressed importance of omentum in hernia repair
William of Saliceto (12th
cent.)
Differential diagnosis of omental (called "rete" or net) and intestinal hernias
Theodoric de Mondeville
(1260-1320)
1267 Described anatomy of omentum and its vasculature
Omentum serves to aid digestion
Mondino da Luzzi (1275-
1326)
Omentum arises at peritoneal reflection in diaphragmatic region; it is attached to stomach, spleen, and colon
Brunschwig (1450-1533) Detailed description of traumatic abdominal injury
da Vinci 1504 Accurate annotated drawings of dissected omenta; not published until 18th century
da Carpi 1523 Claimed to have performed resection without ligature or cautery; suggested that exposure to air causes gangrene
Vesalius 1543 Described innervation, vasculature, and deep and superficial layers of omentum
Franco (1500-1561) Repaired hernias with adherent tissue
Par (1510-1590) Described rupture of peritoneum with extrusion of omentum; recommended use of trusses
Fabricius ab Aquapendente
(1537-1590)
Omentum recipient of wastes from stomach, liver, and spleen
Riolan (1580-1657) Omentum "ruler of the whole abdomen," but not heat-regulating organ
Sennert 1628 Survey of omental diseases
van den Spiegel 1632 Described omentum and structure later named the spigelian lobe
Ruysch (1638-1731) Omentum not a perforated net between vessels
Wharton 1659 "Confirmed" existence of omental lymph vessels
Dionis 18th
cent
First diagnosis and resection of strangulated omentum in a hernia
Douglas 1730 Best detailed description of the peritoneum
Winslow 1732 Described greater and lesser omentum, lesser sac, and foramen (of Winslow)
von Haller 1743 Described colic omentum
Meckel (1781-1833) Omental embryology
Froriep 1812 Anatomy of peritoneum and omentum
Jobert de Lamballe 1829 Omentum will form adhesions with injured bowel
Cruveilhier 1829 Published pathology atlas; described omental shrinkage in tuberculous peritonitis
Hennecke 1836 Anatomy, pathology, embryology, and function of omentum
Ranvier 1874 "Milky spots" of omentum combat disease
Wegner 1877 First to perform experimental peritoneal lavage
von Leyden 1879 First description of subphrenic abscess
Oberst 1882 Reported omental torsion
Senn 1888 Recommended free omental grafts to protect unsafe suture lines in intestinal and kidney surgery
Morison 1894 Described the right infrahepatic space (subhepatic, hepatorenal space) and vascular regenerative capacity of omentum
Starling and Tubby 1894 Studied the transference of substances from the peritoneal cavity to the blood and from the blood to the peritoneum
5/23/2014 Print: Chapter 10. Peritoneum, Omenta, and Internal Hernias
http://web.uni-plovdiv.bg/stu1104541018/docs/res/skandalakis' %20surgical%20anatomy%20-%202004/Chapter%2010_%20Peritoneum,%20Omenta,%20and%2 2/62
Starling and Tubby 1894 Studied the transference of substances from the peritoneal cavity to the blood and from the blood to the peritoneum
Milian 1899 Foreign organic material injected into peritoneal cavity absorbed by omentum
Putnam 1922 Studied the properties of the peritoneal membrane
Ganter 1923 Evaluated peritoneal dialysis for the treatment of uremia
Seligman 1946 Successful treatment of nephrectomized dogs by continuous flow dialysis
Doolan & Lewis 1960 Patient maintained on continuous ambulatory peritoneal dialysis (CAPD)
Kiricuta 1963 Pedicled omentum used for chest wall repair in breast cancer surgery
Tenckhoff et al. 1964,
1972
Advances in peritoneal dialysis equipment
Turner-Walker et al. 1967 Omentum used in urogenital surgery
McLean, Buncke 1972 Autotransplantation of omentum to scalp
Goldsmith 1973 Pedicled omentum used for vascular supply of brain
Lichtenstein et al. 1989 Lichtenstein repair with prosthetic screen onlay technique ("tension-free hernioplasty")
Arregui 1991 Reported the transabdominal preperitoneal (TAPP) repair
Phillips et al. 1993 Performed laparoscopic Stoppa preperitoneal prosthetic mesh repair
McKernan & Laws 1993 Performed laparoscopic repair of inguinal hernia without peritoneoscopy, totally avoiding abdominal cavity
Robbins & Rutkow 1993 Reported results of hand-rolled "umbrella" plug hernioplasty
Fitzgibbons et al. 1995 Compared transabdominal preperitoneal, intraperitoneal onlay mesh, and total extraperitoneal laparoscopic inguinal
herniorrhaphies and found them to be equally effective
History table compiled by David A. McClusky III and John E. Skandalakis.
References:
Arregui ME. Laparoscopic preperitoneal herniorrhaphy. Presented at the Society of American Endoscopic Surgeons Annual Meeting, Monterrey CA, April 1991.
Blumenkrantz MJ, Roberts M. Progress in peritoneal dialysis: a historical perspective. Contr Nephrol 1979;17:101-110.
Fitzgibbons RJ, Camps J, Cornet DA, Ngugen NX, Litke BS, Annibali R, Salerno GM. Laparoscopic inguinal herniorrhaphy: results of a multicenter trial. Ann Surg
1995;221:3-13.
Halliday P. The surgical management of subphrenic abscess: a historical study. Aust NZ J Surg 1975;45:235-244.
Lichtenstein IL, Shulman AG, Amid PK, Montllor MM. The tension-free hernioplasty. Am J Surg 1989;157:188-93.
Liebermann-Meffert D, White H (eds). The Greater Omentum. New York: Springer-Verlag, 1983.
Mattocks AM, El-Bassiouni EA. Peritoneal dialysis: a review. J Pharmaceut Sci 1971;60:1761-1782.
McKernan JB, Laws HL. Laparoscopic repair of inguinal hernias using a totally extraperitoneal prosthetic approach. Surg Endosc 1993;7:26-28.
Meyers MA. Morison pouch (letter; comment). Radiology 1995;195:578.
Phillips EH, Carroll BJ, Fallas MJ. Laparoscopic preperitoneal inguinal hernia repair without peritoneal incision. Surg Endosc 1993;7:159-62.
Robbins AW, Rutkow IM. The mesh-plug hernioplasty. Surg Clin North Am 1993;73:501.
Skandalakis JE, Gray SW. Embryology for Surgeons (2nd ed). Baltimore: Williams & Wilkins, 1994.
EMBRYOGENESIS
Normal Development
The gastrointestinal tract starts as a closed structure, fixed with the dorsal and ventral mesenteries. It can be envisioned as a downward-facing open
book (Fig. 10-1).
Fig. 10-1.
5/23/2014 Print: Chapter 10. Peritoneum, Omenta, and Internal Hernias
http://web.uni-plovdiv.bg/stu1104541018/docs/res/skandalakis' %20surgical%20anatomy%20-%202004/Chapter%2010_%20Peritoneum,%20Omenta,%20and%2 3/62
Relationship of various organs with embryonic ventral and dorsal mesenteries. (Modified from Brantigan OC. Clinical Anatomy. New York: McGraw-Hill, 1963; with
permission.)
The embryogenesis of the peritoneum derives from the mesoderm. Around the third week, the mesoderm differentiates into lateral plate mesoderm,
intermediate mesoderm, and paraxial mesoderm (Fig. 10-2). As differentiation continues, the lateral plate divides into somatic and splanchnic mesoderm.
These envelop the intraembryonic coelom on each side of the midline. Later, the right and left intraembryonic coelom will unite to form a single cavity.
This single cavity will subdivide again into pleural, pericardial, and peritoneal cavities and into the processus (tunica) vaginalis. Differentiation continues by
the formation of parietal and visceral layers of the serous membranes of the peritoneum, and by the formation of omenta, mesenteries, ligaments, and
fossae.
Fig. 10-2.
5/23/2014 Print: Chapter 10. Peritoneum, Omenta, and Internal Hernias
http://web.uni-plovdiv.bg/stu1104541018/docs/res/skandalakis' %20surgical%20anatomy%20-%202004/Chapter%2010_%20Peritoneum,%20Omenta,%20and%2 4/62
Embryogenesis of omenta, mesenteries, ligaments, and fossae.
The development of the omentum is controversial. The theory that an independent area (recess or cleft) was the start of the lesser sac found support
around the turn of the century.
2,3
Liebermann-Meffert and White
4
stated that the omentum does not develop as a fold of the dorsal mesogastrium, but
develops independently in close relation to the spleen; the organs do not rotate. According to Krutsiak and Voitiv,
5
the lesser peritoneal sac develops in
three sections: the vestibulum bursae omentalis, the bursa omentalis proper, and the cavity omentum majus.
The dorsal mesentery is responsible for the genesis of the greater omentum (Fig 10-3), a double-layered evagination of that part of the dorsal
mesogastrium located between the left gastric artery and the common hepatic artery. At the fifth week, the dorsal mesentery elongates downward after
the formation of the omental bursa (lesser sac). This process forms the inferior recess. A four-layered anatomic entity -the greater omentum or fat apron-
is created (Table 10-2).
Table 10-2. Development of the Greater Omentum from Birth to Adulthood
Age Premature Newborn Mature Newborn 3 to 4 mo 1 to 5 yr 5 to 10 yr Adult
Attachments Attached to the transverse
colon but does not reach the
colonic flexures
Further
attachment but
does not reach
the colonic
flexures
Distal to the
transverse colon
Extends beyond
the colonic
flexures; some
attachments to
the ascending and
descending colon
Resembles the
adult omentum;
insertion on the
ascending colon
and occasionally
on the cecum
Width, 20 to 46 cm
Downward
length
Just below the colon Covering approx.
of small bowel
Covering of small
bowel
Most of the
intestines are
covered by the
omentum
More downward
extension
7 to 10 cm or 14 to 35 cm
Network Fatless thin vascular membrane Fatless thin
vascular
membrane
Fat around the
vessels
More fat;
occasionally some
lymph nodes
More fat Volume depends on body
weight; may be fat or lean
Vascularization Vascular pattern can be seen Vascular pattern
can be seen
Vascular pattern can
be seen
Vascular pattern
can be seen
Vascular pattern
can be more
obviously seen
Wider range of varieties; no
standard pattern;
unpredictable
Observations Omentum is rudimentary fringe
and extends upward toward
the spleen. Its two posterior
layers fused to the transverse
colon and transverse
mesocolon
Splenic ligaments
developed;
omentum
reaches the
diaphragm
Splenic ligaments,
especially
gastrosplenic and
splenorenal, are
better developed;
better formation of
omentum
Omentum well
formed
Omentum and
omental derivation
almost with
normal limits
Typical omental formation, fat
or lean, voluminous or not,
according to body weight; all
parts well differentiated;
artery, veins, and lymph nodes
may be seen
Diagram
Data from Liebermann-Meffert D, White H, eds. Diseases of the Omentum: Congenital Abnormalities and Pediatric Disease. New York: Springer-Verlag, 1983.
Fig. 10-3.
5/23/2014 Print: Chapter 10. Peritoneum, Omenta, and Internal Hernias
http://web.uni-plovdiv.bg/stu1104541018/docs/res/skandalakis' %20surgical%20anatomy%20-%202004/Chapter%2010_%20Peritoneum,%20Omenta,%20and%2 5/62
Formation of greater omentum. A, Rotation of stomach and formation of omental bursa. B, Fusion of posterior wall of omental bursa to transverse colon and
mesocolon. C and D, Fusion of anterior and posterior walls of omental bursa to form adult omentum. S, Stomach; P, Pancreas; C, Colon.
The ventral mesentery is found only above the umbilicus. The formation of the liver divides the ventral mesentery into two sections: the lesser omentum
and the three peritoneal ligaments of the liver (falciform, coronary, and triangular).
As the stomach grows, bends, rotates, or augments around the greater curvature, it finally forms a large portion of the anterior wall of the lesser sac. By
definition, the greater omentum attaches to the greater curvature of the stomach. This represents the original dorsal surface of the stomach.
By continuing growth, the omental apron forms a double-layered sac. The sac of the greater omentum is closely related to the transverse mesocolon (Fig.
10-4). The adult transverse mesocolon is a fusion between the embryonic transverse mesocolon and the portion of the dorsal mesogastrium attaching to
the posterior abdominal wall.
Fig. 10-4.
5/23/2014 Print: Chapter 10. Peritoneum, Omenta, and Internal Hernias
http://web.uni-plovdiv.bg/stu1104541018/docs/res/skandalakis' %20surgical%20anatomy%20-%202004/Chapter%2010_%20Peritoneum,%20Omenta,%20and%2 6/62
Vertical disposition of the peritoneum (abdominopelvic cavity).
For all practical purposes, embryogenesis stops here. However, the anatomic entities derived from the peritoneum further subdivide the peritoneal cavity
into several compartments. The peritoneal cavity consists of two principal spaces, the greater sac or general peritoneal cavity and the omental bursa or
lesser sac (Fig. 10-4). These are connected by the epiploic foramen of Winslow. In the male the peritoneal cavity is truly a closed sac. However, in the
female the minute openings of the uterine tubes provide continuity with the environment external to the body.
Congenital Anomalies
Greater Omentum
Congenital anomalies in this area are rare and case reports are sporadic. This renders difficult the anatomic and embryologic understanding of these
malformations.
Absence of the greater omentum and all or part of the ligaments and folds related to it is rarely described in the literature. A case of "hypoplasia of the
greater omentum," asplenia syndrome, and multiple other anomalies was presented by Kiuchi et al.,
6
who witnessed striking dysplasia of length, breadth,
and thickness in the laboratory and in the operating room.
The greater omentum itself may fail to form the gastrocolic ligament or to attach to the greater curvature. This failure can be partial or total. Omental
derivatives may also present failure of attachment or unexpected attachments.
Although most congenital omental defects are asymptomatic, internal obstruction may be produced if a loop of small bowel passes through the omentum.
The senior author of this chapter, John Skandalakis, has seen symptomatic defects at the greater omentum, and asymptomatic defects at the lesser
omentum.
Bifid omentum may occur, although Skandalakis found no references in the literature to support this. Also rare are congenital adhesions between the
omentum and the abdominal wall (anterior or posterior), or between the omentum and other organs.
Skandalakis
7
reported a case of idiopathic segmental infarction where the lesion involved the right lower border of the omentum. The etiology could have
been embryologic; the pathogenesis was confusing.
Although many benign solid tumors of the omentum have been found in children, a congenital origin is hard to support. Benign cysts, which may be
congenital or acquired, are either lined with epithelium or endothelium (true cysts) or are pseudocysts without this lining (false cysts). A rare case of
immature omental teratoma was reported by Spurney and McCormack.
8
A solid ovarian teratoma that metastasized to the omentum was studied by
Boehner.
9
Omental pregnancy and accessory spleens in the omentum have been documented.
10
Omentum can become incarcerated in congenital hernias (indirect
inguinal, diaphragmatic, etc); this can be observed in newborns and in children. Haider
11
reported omental herniation within the pericardium.
Lesser Omentum
Anomalies of the lesser omentum are rare; their variations are difficult to classify. Skandalakis has encountered holes of varying sizes. A male infant
lacking a lesser omentum, in conjunction with other anomalies, was reported by Hodach.
12
Mesenteries
The root of the mesentery extends from the upper left quadrant (1st or 2nd lumbar vertebra) to the right sacroiliac joint, and is fused to the
retroperitoneal space. Failure to fuse, or the presence of a hole in the mesentery, can allow the herniation of small bowel (symptomatic or asymptomatic
5/23/2014 Print: Chapter 10. Peritoneum, Omenta, and Internal Hernias
http://web.uni-plovdiv.bg/stu1104541018/docs/res/skandalakis' %20surgical%20anatomy%20-%202004/Chapter%2010_%20Peritoneum,%20Omenta,%20and%2 7/62
internal hernia). Nonfusion deformity produces a hernia of Waldeyer; this may occur in combination with nonfusion of colonic mesentery. Jejunal atresia
with agenesis of the dorsal mesentery is known as "apple peel syndrome,"
13
"Christmas tree deformity,"
14
or "maypole atresia."
15
Internal hernia can result if the transverse mesocolon fails to attach to the second part of the duodenum, the anterior border of the pancreas, or the
lower pole of the left kidney. Any defect producing a hole can have similar results. The intersigmoid fossa can be the site of an internal hernia, as can any
site on the sigmoid mesocolon.
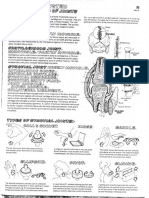
Congenital mesenteric cysts can be categorized by origin (Fig. 10-5):
Endodermal: enteric cysts, cystic intestinal duplications
Multiple: retroperitoneal teratoma
Mesodermal: lymphatic cysts, retroperitoneal cysts of urogenital origin
Fig. 10-5.
5/23/2014 Print: Chapter 10. Peritoneum, Omenta, and Internal Hernias
http://web.uni-plovdiv.bg/stu1104541018/docs/res/skandalakis' %20surgical%20anatomy%20-%202004/Chapter%2010_%20Peritoneum,%20Omenta,%20and%2 8/62
Topographic anatomy showing 5 omental and mesenteric cysts (dotted). (Modified from Skandalakis JE, Gray SW (Eds). Embryology for Surgeons, 2nd Ed.
Baltimore: Williams & Wilkins, 1994; with permission.)
Mesenteric cysts are discussed in more detail in the chapter on the small intestine, under "Surgical Applications to the Jejunum and Ileum."
Ligaments
Failure of the falciform ligament to fuse with the anterior abdominal wall causes a defect that can lead to internal herniation.
16
The broad ligament, being
thin and almost avascular, is also a possible site for an internal hernia.
Fossae
Moynihan
17
described nine paraduodenal fossae, which he theorized were "fusion folds" caused by "physiologic adhesions." We consider five (each bearing
the name of its original investigator) to be of clinical importance and consistent enough for study (Table 10-3, Fig. 10-6).
18,19,20
Table 10-3. The Paraduodenal Fossae
Fossa and Eponym Anatomic Boundaries Incidence
(%)
Surgical
Significance
1. Superior fossa of
Treitz
Behind the superior duodenal fold at the left of the fourth part of the duodenum; the cavity extends upward,
approaching the pancreas; the hernial sac is directed to the right
30-50 May contain a
right
paraduodenal
hernia
2. Inferior fossa of
Treitz
Behind the inferior duodenal fold at the left of the fourth part of the duodenum; a thumb-like cavity extending
downward, parallel to the duodenum; the hernial sac is directed to the right
50-75 May contain a
right
paraduodenal
hernia
3.
Mesentericoparietal
fossa of Waldeyer
At the base of the mesentery of the first part of the jejunum, behind the superior mesenteric artery and below the
duodenum; more common in fetuses than in adults; the hernial sac is directed to the right
1
(Parsons,
1953)
May contain a
right
paraduodenal
hernia
4. Intermesocolic
fossa of Brsike
At the base of the transverse mesocolon which together with the pancreas forms the upper wall of the fossa; the
lower wall is formed by the duodenojejunal junction and fourth part of the duodenum; the anterior wall is formed
by a peritoneal fold between the transverse mesocolon and mesentery of the upper jejunum; the middle colic
artery lies to the right of the orifice; the hernial sac is directed to the right
Rare May contain a
right
paraduodenal
hernia
5. Paraduodenal
fossa of Landzert
Under the fold, bridging the left end of the superior and inferior fossae (Treitz); the fold contains the inferior
mesenteric vein and left colic artery; psoas muscle and hilum of left kidney lie posterior; the hernial sac is directed
to the left
2
(Parsons,
1953)
May contain a
left
paraduodenal
hernia
Source: Skandalakis JE, Gray SW. Embryology for Surgeons, 2nd Ed. Baltimore: Williams & Wilkins, 1994.
Fig. 10-6.
5/23/2014 Print: Chapter 10. Peritoneum, Omenta, and Internal Hernias
http://web.uni-plovdiv.bg/stu1104541018/docs/res/skandalakis' %20surgical%20anatomy%20-%202004/Chapter%2010_%20Peritoneum,%20Omenta,%20and%2 9/62
Major paraduodenal fossae (transverse colon reflected upward; duodenum reflected to right). Numbers refer to Table 10-3. (Modified from Skandalakis LJ, Gadacz
TR, Mansberger AR Jr, Mitchell WE Jr, Colborn GL, Skandalakis JE. Modern Hernia Repair: The Embryological and Anatomical Basis of Surgery. New York: Parthenon,
1996; with permission.)
These fossae seem to be of congenital origin. The paraduodenal fossae may form during the 10th week when the mesenteries of the ascending and
descending colon fuse to the parietal peritoneum of the posterior abdominal wall. With the peritoneum and duodenojejunal junction as co-conspirators, a
congenital hernia may result at the time of formation of the fossae, or an acquired hernia may occur later. When internal herniation takes place, the sac is
directed to the right or to the left; hence, the identification of right or left hernia.
There are a number of intraperitoneal fossae and apertures through which peritoneal contents may protrude. These internal hernias account for less than
1%
21
of intestinal obstructions; of these, paraduodenal hernias account for more than 50%.
Congenital hernial sacs open at the sites of the fossae, but there is no evidence that a congenital fossa becomes a hernial sac later in life. A
paraduodenal fossa is not the site of a potential acquired hernia; instead, it marks the location where a congenital hernia might have occurred, but failed
to do so.
In a left paraduodenal hernia, an intestinal loop enters a pocket of yet-unfused descending mesocolon during the return of the intestines to the abdomen
in the 10th week; during subsequent fusion of the mesocolon, a hernial sac is produced. The same process under the ascending mesocolon produces a
right paraduodenal hernia.
Laslie et al.
22
suggested that the hernial sac is not formed by the mesocolon, but represents the lining of the extraembryonic coelom, which envelops the
intestinal loops while they are in the umbilical cord and which entered the abdomen with them. This avascular coelomic sac fuses secondarily with the
ascending or descending mesocolon to form a right or left paraduodenal hernia. In some cases, this fusion does not take place and the anomalous sac
remains more evident. This condition has been called internal omphalocele.
SURGICAL ANATOMY OF THE PERITONEUM
The peritoneum is the largest serous membrane in the body, with a surface area of about 22,000 cm
2
. It can be divided into parietal and visceral portions.
The parietal layer lines the abdominal and pelvic cavities and the abdominal surface of the diaphragm. The visceral layer covers the abdominal and pelvic
viscera and includes the mesenteries.
The parietal peritoneum is only loosely connected with the body wall, separated from it by an adipose layer, the tela subserosa; whereas the visceral
peritoneum is usually tightly attached to the organs it covers. The peritoneum consists of a fibrous layer (the tunica subserosa) and a surface layer of
mesothelium (the tunica serosa).
The peritoneal cavity is a potential space. It normally contains only a thin film of fluid which lubricates the surfaces, allowing frictionless movements of the
gastrointestinal tract. Under the effects of certain pathologic conditions, great quantities of fluid can occupy the peritoneal cavity.
Peritoneum does not line the entirety of the abdominopelvic cavity. It is lifted from the body wall, especially posteriorly, by organs located against the wall
during embryologic development. This chain of events causes the formation of a retroperitoneal space between the peritoneum and the body wall, with
5/23/2014 Print: Chapter 10. Peritoneum, Omenta, and Internal Hernias
http://web.uni-plovdiv.bg/stu1104541018/docs/res/skandalakis' %20surgical%20anatomy%20-%202004/Chapter%2010_%20Peritoneum,%20Omenta,%20and% 10/62
organs situated within the space. An organ that is covered only in part by the peritoneum is referred to as a retroperitoneal organ. An organ that is
covered by peritoneum essentially everywhere except for the site of entrance of vessels is referred to as an intraperitoneal organ.
The purpose of this chapter is to remind surgeons of the anatomy of the peritoneal compartments (Fig. 10-7) and to emphasize some of the newer
concepts, with the hope that this will help in the agonizing treatment of peritoneal collections. In spite of sonograms, CAT scans, fluoroscopic
localizations, MRIs, laparoscopies, etc., which are tremendously helpful, an anatomic knowledge of the spaces is necessary to reduce morbidity, or even
catastrophe, in the operating room.
Fig. 10-7.
Arbitrary compartments of abdominal cavity. (Modified from Skandalakis JE, Gray SW, Rowe JS Jr. Anatomical Complications in General Surgery. New York: McGraw-
Hill, 1983; with permission.)
The abdominal surgeon must understand the development of the peritoneum and its peculiar attachments. The formation of the omentum and its various
folds and ligaments must be studied if anatomic complications are to be avoided (Table 10-4).
Table 10-4. Parts of the Peritoneum
Omenta Great omentum
Lesser omentum
Mesenteries Mesentery of the small bowel
Mesoappendix
Transverse mesocolon
Pelvic mesocolon
Ligaments Of liver
Of urinary bladder
Of uterus
Fossae Duodenal
Cecal
Intersigmoid
Source: Skandalakis JE, Gray SW. Embryology for Surgeons, 2nd Ed. Baltimore: Williams & Wilkins, 1994.
Peritoneal Dispositions
Vertical Disposition in the Abdominopelvic Cavity
In most anatomy books, the starting point for the study of the vertical disposition of the peritoneum is the umbilical area (Fig. 10-4). On its way up, the
5/23/2014 Print: Chapter 10. Peritoneum, Omenta, and Internal Hernias
http://web.uni-plovdiv.bg/stu1104541018/docs/res/skandalakis' %20surgical%20anatomy%20-%202004/Chapter%2010_%20Peritoneum,%20Omenta,%20and% 11/62
parietal peritoneum forms the falciform ligament. This is a roughly triangular, bilaminar structure, which passes from the posterior surface of the abdominal
wall and inferior surface of the diaphragm to the anterosuperior surface of the liver. The ligament is not oriented strictly in an anterior-posterior direction;
rather, as can be seen easily in transverse sectional images, it is inclined to the right in a nearly coronal plane as it passes upward from the umbilicus.
The falciform ligament is a thin, bilaminar peritoneal membrane with loose connective tissue separating the two layers and conveying the ligamentum teres
hepatis in its free inferior edge. At the liver, the two peritoneal laminae are continuous with the visceral peritoneum covering the liver. Upon reaching the
intersection of the diaphragm and liver, the two layers separate. The right layer passes across the hepatic surface to the right forming the anterior
(superior) lamina of the coronary ligament (Fig. 10-8); the left layer passes to the left over the lateral segment of the left lobe, forming the anterior layer
of the left triangular ligament.
Fig. 10-8.
Peritoneal reflections of diaphragm showing bare area, coronary, triangular, and falciform ligaments. Arrow represents pathway behind abdominal esophagus
where surgeon may pass finger through posterior layer of coronary ligament. (From Gray SW, Rowe JS Jr, Skandalakis JE. Surgical anatomy of the
gastroesophageal junction. Am Surg 45(9):575-587, 1979; redrawn from Hollinshead. Anatomy for Surgeons. Hoeber-Harper, 1956; with permission.)
The free, crescentic, inferior margin of the falciform ligament is characterized by the firm, cordlike thickening caused by the presence of the ligamentum
teres hepatis (round ligament) of the liver. This structure is the remnant of the left umbilical vein of intrauterine development, the right umbilical vein
having disappeared early in embryonic development. The round ligament passes from the umbilicus to the inferior border and inferior surface of the liver,
where it ends at the umbilical segment of the left portal vein. Also within the falciform ligament, the paraumbilical veins (of Sappey) pass from the liver to
the integument surrounding the umbilicus.
Continuing upward from the left portal vein to the inferior vena cava just below the diaphragm is another cordlike or bandlike structure, the vestige of the
embryonic continuation of the left umbilical vein, the ligamentum venosum. This, in intrauterine life, is the ductus venosus. Maternal blood passes from the
left umbilical vein to the liver, where some of the blood is shunted into the liver by the portal venous system, the remainder passing to the inferior vena
cava by way of the ductus venosus. The three ligaments falciform, round, and venosum divide the left lobe of the liver into two segments, the medial
and the lateral.
The visceral peritoneum continues over the inferior margin of the liver, passing from the diaphragmatic surface to the visceral surface of the right and left
lobes. On the right, parietal peritoneum leaves the visceral surface of the liver to cover the right adrenal gland and the upper part of the right kidney,
forming the hepatorenal ligament. It passes then to the left as the posterior (inferior) layer of the hepatic coronary ligament.
The peritoneum continues inferiorly from the vicinity of the right kidney, investing the first part of the duodenum and the hepatic flexure of colon and that
part of the inferior vena cava that forms the posterior border of the epiploic foramen of Winslow. This peritoneal covering continues to the left, forming
the floor of the lesser omental bursa.
At the right margin of the liver, the reflection of the coronary ligament from anterior to posterior forms a relatively sharply bordered right triangular
ligament (Fig. 10-8) which secures the right lobe to the diaphragm. This ligament forms the apex of the large posterosuperior bare area of the liver. At the
bare area, peritoneum reflects from the superior surface of the liver to the inferior surface of the diaphragm, leaving this portion of the upper surface of
the liver devoid of peritoneal covering, separated from the diaphragm only by areolar tissue. The base of the roughly triangular bare area is situated to the
left, at the groove for the inferior vena cava.
The fundus and inferior surface and sides of the gallbladder are covered with peritoneum that is continuous over the visceral surface of the right lobe of
the liver and the quadrate lobe to the porta hepatis, and the visceral surface of the lateral segment of the left lobe. At the sharp left margin of the liver,
the peritoneal attachment of the left lobe to the diaphragm forms the left triangular ligament (Fig. 10-8). From this region laterally, the peritoneum passes
freely around the lateral abdominal wall and over part of the posterior wall until it becomes continuous with the gastrophrenic and splenophrenic ligaments.
The caudal part of the splenophrenic ligament continues inferiorly over the left kidney as the splenorenal ligament and thence to the splenic flexure of the
colon, there forming the narrow phrenicocolic ligament.
From the left portion of the inferior margin of the diaphragmatic surface of the liver, the peritoneum passes cranially over its inferior visceral surface.
Reaching the anterior border of the porta hepatis and the left side of the fissure for the ligamentum venosum, peritoneum continues freely downward to
5/23/2014 Print: Chapter 10. Peritoneum, Omenta, and Internal Hernias
http://web.uni-plovdiv.bg/stu1104541018/docs/res/skandalakis' %20surgical%20anatomy%20-%202004/Chapter%2010_%20Peritoneum,%20Omenta,%20and% 12/62
Reaching the anterior border of the porta hepatis and the left side of the fissure for the ligamentum venosum, peritoneum continues freely downward to
the duodenum and the lesser curvature of the stomach, forming the anterior layer of the lesser omentum, the inferior extent of the primitive ventral
mesentery. Peritoneum continuous with the posterior layer of the coronary ligament covers the caudate lobe and its process and then passes inferiorly
from the posterior margin of the porta and the right side of the fissure for the ligamentum venosum, forming the posterior layer of the lesser omentum.
The left margin of the two-layered lesser omentum connects to the esophagus; the right free margin forms the anterior border of the epiploic foramen of
Winslow. The free border collectively ensheathes the hepatic arteries, extrahepatic biliary vessels, portal vein, lymph nodes and vessels, and the hepatic
plexus of nerves. Behind this ligament lies the epiploic foramen, the sole passageway between the greater peritoneal cavity and the lesser omental bursa.
The anterior and posterior laminae of the lesser omentum separate at the lesser curvature of the stomach, investing the left gastric vessels and nerves as
they approach the lesser curvature. This part of the lesser omentum is the hepatogastric ligament. After incorporating the stomach and the first part of
the duodenum, the anterior and posterior layers of gastric peritoneum leave the greater curvature of the stomach and duodenum as the anterior layer of
the greater omentum.
The double layer of peritoneum forming the anterior layer of the greater omentum descends across the transverse colon and passes inferiorly for a variable
distance to the lower end of this apronlike fold. The posterior layer of the greater omentum then ascends, passing superior to the transverse colon and
lying against the superior layer of the transverse mesocolon, with which it fuses to a variable degree, then attaches to the anterior aspect of the head
and body of the pancreas. The more inferior layer of peritoneum then descends, forming the superior layer of the peritoneum of the transverse colon; the
more superior layer becomes continuous with the peritoneal floor of the lesser omental bursa.
The surgeon uses this special anatomic relationship to secure a bloodless route to the lesser sac and the pancreas. The greater omentum is lifted up to
expose its posterior surface, a variable number of adhesions to the transverse colon are divided, and the plane between the posterior aspect of the fused
layers of the greater omentum lying anteriorly and the anterior layer of the peritoneum of the mesocolon is entered. Separation of these two layers leads
to the lesser sac. The greater omentum/stomach can be lifted cephalad over the costal margin for wide exposure of the pancreas.
That part of the greater omentum between the greater curvature of the stomach and the transverse mesocolon forms the gastrocolic ligament. The
ligament often includes both the anterior and posterior layers of the greater omentum, which have undergone fusion. It may consist primarily of the
anterior layer of the greater omentum if the omental bursa continues from behind the stomach at the greater curvature, intervening between the anterior
and posterior layers of the greater omentum as the inferior recess of the lesser omental bursa.
The anterior peritoneal layer of the transverse mesocolon continues inferiorly, passing about the transverse colon to ascend as the posterior peritoneal
layer. After reaching the head and body of the pancreas, this peritoneal layer continues inferiorly over the pancreas and the third and fourth parts of the
duodenum. To the right, peritoneum leaves the duodenum to reach the posterior abdominal wall. Near the midline, the peritoneum is carried away by the
superior mesenteric artery and vein and their branches as the radix or root of the mesentery, forming the right side of the mesentery of the small
intestine.
Continuing about the jejunum and ileum, peritoneum thereafter covers the left side of the mesentery of the small intestine. This peritoneum continues to
the left over the secondarily retroperitoneal descending colon to the lateral abdominal wall. Below and to the left, this peritoneal layer is elevated from the
posterior abdominal wall and pelvic sidewall as the anterior layer of the sigmoid mesocolon. Then, after investing the sigmoid colon, it ascends as the
posterior layer of the sigmoid mesocolon to reach the lateral wall of the pelvis and left iliac fossa. Inferiorly from the mesentery of the small intestine,
peritoneum covers the lower abdominal segments of the aorta, inferior vena cava, and their respective branches and tributaries.
The peritoneum continues downward into the pelvis. It covers the ventral surface and lateral aspects of the first part of the rectum, the ventral surface
alone of the second part of the rectum, and then forms the floor of the rectovesical pouch in the male, the rectouterine pouch of Douglas in the female.
Lateral to the rectum, the peritoneum forms right and left pararectal fossae, the depths of which vary, in keeping with the degree of rectal distension.
MALE PELVIS
In the male pelvis, the lateral boundaries of the pararectal fossae continue forward toward the urinary bladder as the sacrogenital folds. These folds are
formed by the peritoneal covering over relatively dense connective tissues, the ureter, and nerves and vessels passing ventrally from the sacrum and
pelvic sidewall toward the urogenital organs. The peritoneum of the rectovesical pouch ascends over the superior portions of the seminal vesicles, not
coming into contact with the prostate gland. It then sweeps upward over the base and superior surface of the urinary bladder to reach the anterior
abdominal wall.
Lateral to the urinary bladder, the pelvic peritoneum provides floors for the right and left paravesical fossae. Laterally in each pararectal fossa, the ductus
deferens raises a fold of peritoneum as it passes upward toward the pelvic brim and the deep inguinal ring. When the urinary bladder is empty, a variably
present, transverse vesical fold can be seen to pass medially from the pelvic sidewall. This fold extends between the paravesical fossae, crossing the
urinary bladder anterior to the fold over the ductus deferens.
Superior to the urinary bladder, the peritoneum upon the anterior abdominal wall is lifted by the underlying presence of the fibrous midline urachus or
remnant of the embryonic allantois. It extends upward from the apex of the bladder to the umbilicus, thus forming the median (middle) umbilical fold.
Lateral to this on both sides, and also directed toward the umbilicus, medial umbilical folds are formed as peritoneum crosses the obliterated segments of
the umbilical arteries. Further laterally, the inferior epigastric artery and vein and their coverings of peritoneum form less distinct lateral umbilical folds
which, though passing toward the rectus muscles, are not in reality directed to the umbilicus, but more laterally; therefore, they are probably named
inappropriately.
Between the median and medial umbilical folds are the supravesical fossae, the depths of which are dependent upon the degree of fullness of the urinary
bladder. Below these, the anterior surface of the bladder is in direct contact with the pubis and the lower extent of the anterior abdominal wall, separated
from them by the retropubic space of Retzius and its extension upward into the space of Bogros.
23
For some distance above the pubic crest, the
peritoneum is only loosely attached to the abdominal wall so that, as the bladder fills, it carries the peritoneum away from the wall.
Lateral to the medial umbilical ligament is the shallow, medial inguinal fossa. Just lateral to the lateral umbilical ligament is the lateral inguinal fossa. The
lateral inguinal fossa is the site of the deep, or internal inguinal ring, at which one may see more or less distinctly the convergence of the ductus deferens
and the testicular vessels. Below and medial to the beginning of the lateral umbilical ligament is a relatively indistinct and shallow femoral fossa, overlying
the abdominal surface of the femoral ring.
FEMALE PELVIS
5/23/2014 Print: Chapter 10. Peritoneum, Omenta, and Internal Hernias
http://web.uni-plovdiv.bg/stu1104541018/docs/res/skandalakis' %20surgical%20anatomy%20-%202004/Chapter%2010_%20Peritoneum,%20Omenta,%20and% 13/62
In the female pelvis the peritoneum of the rectouterine pouch or cul-de-sac (pouch of Douglas) ascends over the posterior fornix and apex of the vagina
to reach the uterine cervix. Laterally in the pararectal fossae and rectouterine pouch, uterosacral folds are prominent. These consist of peritoneum and
underlying connective tissue, smooth muscle, and elements of the pelvic nerve plexus which pass forward from the sacrum to the posterior fornix and
uterine cervix.
After covering the fundus and the ventral surface of the body of the uterus, peritoneum is reflected from the uterus at the region of the isthmus, the area
of junction of the body and cervix, toward the bladder. Between the uterus and the urinary bladder is the relatively shallow vesicouterine pouch. The more
anterior disposition of the peritoneum is similar to that of the male pelvis.
Peritoneum continues laterally from the uterine fundus and body. Anteroinferior and posterosuperior layers of peritoneum ensheathe the uterine tubes on
their anterior, superior, and posterior surfaces, being suspended from the tubes as the broad ligament.
The peritoneum immediately adjacent to the uterine tube is called the mesosalpinx. The peritoneum by which the ovary and proper ligament of the ovary
are suspended is the mesovarium. The ovary itself is not covered by the peritoneum; the peritoneum is continuous with the germinal layer of epithelium of
the ovary (a misnomer).
Laterally, peritoneum continues to the brim of the pelvis over the ovarian vessels and nerves as the infundibulopelvic ligament, suspensory ligament, or
suspensory ligament of the ovary. Anterolaterally on each side, the round ligament of the uterus raises a fold of peritoneum in the paravesical fossa as the
round ligament ascends toward the brim of the pelvis, in its course to the deep inguinal ring.
After its reflection upward from the urinary bladder to the anterior abdominal wall, the vertical disposition of the peritoneum terminates at the umbilical
area. With this termination, the greater peritoneal sac is formed.
Transverse (Horizontal) Disposition in the Abdominal Cavity
The disposition of the peritoneum is quite different in degree of complexity in the upper abdomen, lower abdomen, and pelvis.
The pathway of the peritoneum transversely at the level of the spleen is as follows (Fig. 10-9): From the linea alba anteriorly, the peritoneum can be
followed to the right laterally and posteriorly, where it sequentially covers the right kidney and right suprarenal gland, inferior vena cava, and aorta. The
peritoneum then passes ventral to the pancreas, duodenum, and left kidney, having formed the posterior wall of the omental bursa. Here it reflects
upward as the right side of the splenorenal and gastrosplenic ligaments to attain and cover the posterior wall of the stomach. The peritoneum then
courses to the right, enveloping the hepatic roots and forming the anterior wall of the omental bursa. Proceeding medially, peritoneum covers the anterior
gastric wall, leaving it as the left side of the gastrosplenic ligament. After forming the gastrosplenic ligament, the peritoneum covers the spleen. It forms
the left side of the splenorenal ligament, covers the left kidney and proceeds to the posterior lateral and anterior wall toward the linea alba.
Fig. 10-9.
Transverse section through spleen.
In the lower abdomen, the peritoneum is raised by a median fold and two bilateral lateral folds. The result is five folds or plica (also called ligaments) (Fig.
10-10): a median umbilical fold, two medial umbilical folds, and two lateral umbilical folds. These converge toward the umbilicus.
Fig. 10-10.
5/23/2014 Print: Chapter 10. Peritoneum, Omenta, and Internal Hernias
http://web.uni-plovdiv.bg/stu1104541018/docs/res/skandalakis' %20surgical%20anatomy%20-%202004/Chapter%2010_%20Peritoneum,%20Omenta,%20and% 14/62
Bladder and anterior abdominal wall (posterior view). Possible pathways of external supravesical hernias shown on left; internal supravesical hernias shown on
the right. A, Supravesical fossa with mouth of supravesical hernia. B, Medial fossa. C, Lateral fossa. D, Inguinal ligament. E, Umbilicus. F, Middle (median) umbilical
ligament (obliterated urachus). G, Lateral (medial) umbilical ligament (obliterated umbilical artery). H, Inferior (deep) epigastric artery. (Modified from Skandalakis
PN, Skandalakis LJ, Gray SW, Skandalakis JE. Supravesical hernia. In: Nyhus LM, Condon RE. Hernia (4th ed). Philadelphia: JB Lippincott, 1995; with permission.)
The median umbilical fold of peritoneum results from the peritoneal coverage of the underlying urachus, which extends from the apex of the bladder below
to the umbilicus above.
Somewhat laterally, leaving the pelvic brim medial to the position of the femoral fossa (under which lies the femoral ring) and adjacent to the lateral
aspect of the bladder, the left and right medial umbilical folds of peritoneum are elevated by the obliterated portions of the left and right umbilical arteries.
These also pass superiorly toward the umbilicus, invested by the vesicoumbilical fascia.
On each side, at the site of exit of the external iliac artery and vein from the abdomen, the inferior epigastric artery and vein pass upward and somewhat
medially to reach the rectus abdominis muscle. These vessels usually cause a slight ridge in the peritoneum, forming the lateral umbilical folds. These
course just medial to the dimple marking the position of the deep (internal) inguinal ring.
The two supravesical fossae, right and left (Fig. 10-10), are located between the median umbilical fold and the medial umbilical folds. The depths of these
fossae are related to the degree of fullness of the urinary bladder. The medial inguinal fossae are situated between the medial and lateral umbilical folds.
The lateral umbilical fossa is less distinct than the supravesical and medial inguinal fossa, and includes the deep inguinal ring, through which the embryonic
processus vaginalis and testis pass to enter the inguinal canal.
In the region of the inframesocolic compartment, peritoneum can be followed to the right laterally from the linea alba to the vicinity of the lateral border of
the quadratus lumborum muscle. Here the peritoneum is reflected forward over the right side of the ascending colon, lining the right paracolic gutter.
Passing across the ventral surface and the left side of the secondarily-retroperitoneal ascending colon, and investing the cecum and appendix, peritoneum
passes medially over the psoas muscle, the duodenum, and the inferior vena cava.
Passing ventrally from the posterior abdominal wall as the radix of the mesentery, peritoneum invests the superior mesenteric vessels, lymphatic elements
and nerves, ileum, and jejunum. The peritoneum then courses in a dorsal path toward the vertebral column. Thereafter the peritoneum can be followed to
the left as it passes across the aorta, the left psoas muscle, and the right side and ventral surface of the retroperitoneally-situated descending colon.
After covering the left side of the descending colon, it forms the floor of the left paracolic gutter and then lines the left side of the interior of the
5/23/2014 Print: Chapter 10. Peritoneum, Omenta, and Internal Hernias
http://web.uni-plovdiv.bg/stu1104541018/docs/res/skandalakis' %20surgical%20anatomy%20-%202004/Chapter%2010_%20Peritoneum,%20Omenta,%20and% 15/62
After covering the left side of the descending colon, it forms the floor of the left paracolic gutter and then lines the left side of the interior of the
abdominal wall to the linea alba.
MALE PELVIS
Within the true (lesser or minor) pelvis of males, peritoneum forms a mesentery for the sigmoid colon, which extends from the left sacroiliac joint diagonally
to the front of the sacrum. Peritoneum covers the right and left sides of the first part of the rectum, but only the ventral surface of the second part of
the rectum, before it reflects upward to the bladder. On either side of the rectum, peritoneum lines the pararectal fossae and is elevated laterally as the
sacrogenital folds. Passing forward from the pararectal fossa and across the rectovesical fossa toward the bladder, the ureter causes a slight elevation of
the peritoneum. The depths of the pararectal fossae are variable, depending upon the degree of distension of the organ.
Somewhat further forward, peritoneum lines the rectovesical pouch between the bladder and rectum. The peritoneum then sweeps upward over the
superior portions of the seminal vesicles and the fundus and superior surface of the bladder. The rectovesical pouch is shallow enough that the peritoneum
does not contact the prostate gland.
On each side of the bladder is a paravesical fossa, where a peritoneal fold limiting the posterior extent of the fossa overlies the course of the ductus
deferens as it passes toward the posterior aspect of the bladder to reach the prostate gland. Like the supravesical fossae, the depths of the paravesical
fossae are related to the degree of fullness of the bladder. When the bladder contains little or no urine, the transverse vesical fold may be seen crossing
its superior surface.
FEMALE PELVIS
The disposition of peritoneum in the posterior portion of the true pelvis in females is comparable to that in males, except that the uterosacral folds are
somewhat more prominent than the sacrogenital folds in the lateral aspects of the pararectal fossae. The uterosacral folds are formed by the coalescence
of the fascia of Waldeyer from the ventral surface of the sacrum and piriformis muscle fascia, together with underlying pelvic nerve elements which pass
lateral to the rectum toward the posterior fornix of the vagina and uterine cervix.
Between the rectum and the uterus, peritoneum lines the rectouterine pouch (cul de sac, or pouch, of Douglas), covering the posterior aspect of the
uterus and the posterior fornix of the vagina.
More anteriorly in the pelvis, the peritoneum is draped over the uterus and its appendages, forming the broad ligament. The superior part of the broad
ligament which is elevated by the uterine tubes is called mesosalpinx; the portion attached to the ovary and ovarian ligament is named mesovarium; that
which extends laterally from the ovary to the pelvic brim covers the ovarian vessels, lymphatics, and nerves and is referred to as the infundibulopelvic
ligament, or suspensory ligament of the ovary. Between this fold of peritoneum and the ureteric ridge provided by the peritoneum overlying the ureter is
the ovarian fossa. This fossa lies at the site of divergence of the internal iliac (hypogastric) and external iliac arteries.
The remainder of the broad ligament, covering most of the uterus and suspended like a blanket from one pelvic sidewall to the other is generally termed
the mesometrium. From the anterior aspect of each side of the body of the uterus, the round ligament elevates the peritoneum to a variable degree as it
passes forward and upward from the uterus to cross the pelvic brim in its passage to the deep inguinal ring.
Between the uterus and the urinary bladder, peritoneum lines the shallow vesicouterine pouch. The disposition of the peritoneum over the bladder in the
female is similar to that in the male, with lateral paravesical fossae which are limited posteriorly by the elevation of peritoneum over the round ligaments of
the uterus. A transverse vesical fold of peritoneum may, likewise, be seen in the female pelvis when the bladder is not distended. Laterally, beginning at
the pelvic sidewall in the paravesical fossae, the obliterated umbilical arteries pass medially and upward toward the umbilicus, passing close to the bladder
and raising the bilateral ridges of peritoneum, the medial umbilical folds, or ligaments.
Vascular Supply of the Peritoneum
The blood supply to the abdominal parietal peritoneum is from the branches of the arteries of the abdominal wall. The blood supply of the pelvic parietal
peritoneum is from the blood vessels of the pelvic wall. Blood to the visceral peritoneum is from branches of the celiac trunk and from branches of the
superior and inferior mesenteric arteries, or the pelvic visceral blood vessels.
Lymphatics of the Peritoneum
The lymphatics of the parietal peritoneum join the lymphatics of the body wall, and all drain to parietal lymph nodes. However, the lymphatics of the
visceral peritoneum join the lymphatics of the related organs and are drained accordingly.
Allen and Weatherford
24
described the removal of particles of 10-20 microns from the peritoneal cavity through openings of the basement membrane with
the help of the peritoneal lymphatics. These peculiar lymphatics were found only in the peritoneum covering the abdominal surface of the diaphragm.
In 1863, Von Recklinghausen
25
was the first to describe the modified lymphatics which are able to remove particles from the peritoneal fluid during the
process of respiration. The relaxed diaphragm permits opening of the stomata of these lymphatic vessels, and the fluid enters the lymphatic circulation.
Higgins et al.
26
reported that contractions of the diaphragm pump the lymph and its contents (particulate matter and molecular substances) upward,
aided by one-way valves which are located within the lymphatics of the retrosternal area.
Innervation of the Peritoneum
The parietal peritoneum contains somatic afferent nerves. The peritoneum contains many sensory fibers for the sensation of pain; the anterior portion of
the parietal peritoneum is especially sensitive. The parietal peritoneum, therefore, is similar in sensitivity to the parietal pleura of the thorax.
In contrast, the visceral peritoneum has no somatic afferent nerves and is relatively insensitive to pain. Sensations which do occur are poorly perceived
and not clearly localized by the brain, as is characteristic of visceral afferent fibers carried by autonomic nerves to viscera in general. The principal
stimulus which can evoke pain from visceral peritoneum is tension upon or stretching of the tissue, or ischemia. A perforated viscus may, perhaps, produce
anterior abdominal wall rigidity, and an intraperitoneal fluid collection may produce painlike sensations of traction or tension on the mesentery in the
retroperitoneal space, but not localized pain. A similarity can be seen here also between visceral pleura and visceral peritoneum, in that the visceral pleura
which invests the lungs is relatively insensitive to pain.
Remember
The innervation of the parietal peritoneum, from above downward, is as follows.
5/23/2014 Print: Chapter 10. Peritoneum, Omenta, and Internal Hernias
http://web.uni-plovdiv.bg/stu1104541018/docs/res/skandalakis' %20surgical%20anatomy%20-%202004/Chapter%2010_%20Peritoneum,%20Omenta,%20and% 16/62
The peritoneum that covers the abdominal surface of the diaphragm is innervated at the periphery by the lower six pairs of intercostal nerves and the subcostal
nerves
Phrenic nerves convey sensory fibers from the peritoneum over the more centrally-disposed parts of the diaphragmatic peritoneum. Pathological process of the
centrally-located peritoneum over the diaphragm is referred as pain by the phrenic nerves to the distribution of spinal nerve levels C3, C4, and C5 over the
shoulder regions
The lower 6 intercostal and lumbar nerves innervate the parietal peritoneum of the abdominal cavity
The pelvic peritoneum is innervated by the obturator nerve
The innervation of the visceral peritoneum is uncertain, but sensory fibers for pain are carried by thoracic and lumbar splanchnic nerves.
Peritoneal Fossae and Recesses
Paraduodenal Fossae
The peri- or paraduodenal fossae (Fig. 10-6, Table 10-3) are "pockets" of the peritoneum on the posterior abdominal wall adjacent to the duodenal-jejunal
junction, particularly to the left of the junction. These fossae are enigmatic embryologically, anatomically, and clinically. They are inconstant: that is, any,
all, or none can be found in any one person. The boundaries of these fossae are complex; size, length, depth, and direction are all involved in naming the
actual anatomic entities related to them. Remember, the paraduodenal fossa may be intimately related with the inferior mesenteric vein.
Foramen of Winslow
The epiploic foramen of Winslow (Fig. 10-4) is an open, normal aperture. It has the following boundaries:
16
Superior: Caudate process of liver and inferior layer of coronary ligament (rare extension to left coronary ligament with hernia)
Anterior: Hepatoduodenal ligament and hepatic triad (portal vein, hepatic artery, common bile duct; cystic duct also present in free edge of lesser omentum)
Posterior: IVC
Inferior: First part of duodenum and transverse part of hepatic artery
Ileocecal Fossae
The superior and inferior ileocecal folds form the ileocecal fossae (Fig. 10-11). A third fossa, known as the retrocecal or subcecal fossa, may occasionally
appear.
Fig. 10-11.
5/23/2014 Print: Chapter 10. Peritoneum, Omenta, and Internal Hernias
http://web.uni-plovdiv.bg/stu1104541018/docs/res/skandalakis' %20surgical%20anatomy%20-%202004/Chapter%2010_%20Peritoneum,%20Omenta,%20and% 17/62
Hernia into the superior ileocecal fossa. A, Superior and inferior ileocecal folds forming fossae. B, The intestinal loop has been trapped by the right mesocolon
during the fusion with the peritoneum of the body wall. (Modified from Skandalakis LJ, Gadacz TR, Mansberger AR Jr, Mitchell WE Jr, Colborn GL, Skandalakis JE.
Modern Hernia Repair: The Embryological and Anatomical Basis of Surgery. New York: Parthenon, 1996; with permission.)
The superior ileocecal fossa has the following boundaries:
Anterior: Ileocecal fold and ileocecal artery
Posterior: Mesentery of terminal ileum and lateral right (ascending) colon
Medial: Below the terminal ileum
The inferior ileocecal fossa has the following boundaries:
Anterior: Ileocecal fold
Posterior: Mesoappendix
Inferior: Medial continuation of ileocecal fold
Superior: Terminal ileum and mesentery
The retrocecal or subcecal fossa, when present, has inconstant boundaries which depend on both its depth and its medial and lateral expansion. It is
found between the right colic gutter and the posterior surface of the cecum at the ileocecal gutter. It does not exist in the presence of a mobile cecum.
The senior author of this chapter (JES) has seen a herniation of the terminal ileum behind the cecum.
Intersigmoid Fossa
The intersigmoid fossa (Fig. 10-12A & B) is located in the pelvic mesocolon, which occupies the space from the pelvic wall to S3. The pelvic mesocolon
has the shape of the Greek letter LAMBDA ( ).
Fig. 10-12.
5/23/2014 Print: Chapter 10. Peritoneum, Omenta, and Internal Hernias
http://web.uni-plovdiv.bg/stu1104541018/docs/res/skandalakis' %20surgical%20anatomy%20-%202004/Chapter%2010_%20Peritoneum,%20Omenta,%20and% 18/62
A, Average measurements of sigmoid mesocolon. B, Relation of base of sigmoid mesocolon to left ureter. (Modified from Skandalakis JE, Gray SW, Rowe JS Jr.
Anatomical Complications in General Surgery. New York: McGraw-Hill, 1983; with permission; data in Fig. 10-12A from Vaez-Zadeh K, Dutz W. Ileosigmoid knotting.
Ann Surg 1970;172:1027.)
The attachment of the mesosigmoid to the body wall most commonly starts in the left iliac fossa, extending downward and to the right on a diagonal. The
attachment may also be sinuous, or shaped like a "C," "S," or inverted "U." Variations in length and breadth of this mesentery may occur by race and/or
diet.
The left ureter passes through the base of the sigmoid mesocolon in its course through the intersigmoid recess (Fig. 10-12B). The mouth of the fossa is
directed downward and to the left. The anatomic entities thus associated with the intersigmoid recess are the left ureter and the exterior iliac vessels.
Supravesical Fossae
The supravesical fossae (Fig. 10-10) are located between the median umbilical ligament (obliterated or non-obliterated urachus) and the medial umbilical
ligament (obliterated umbilical arteries). It partially overlies the area of the modern perception of the boundaries of the triangle of Hesselbach (Fig. 10-13).
Fig. 10-13.
5/23/2014 Print: Chapter 10. Peritoneum, Omenta, and Internal Hernias
http://web.uni-plovdiv.bg/stu1104541018/docs/res/skandalakis' %20surgical%20anatomy%20-%202004/Chapter%2010_%20Peritoneum,%20Omenta,%20and% 19/62
Part of the supravesical fossa lies within the Hesselbach triangle. The triangle as originally described is shown in the left of the diagram; and as accepted today
on the right. (Modified from Skandalakis PN, Skandalakis LJ, Gray SW, Skandalakis JE. Supravesical hernia. In: Nyhus LM, Condon RE. Hernia (4th ed).
Philadelphia: JB Lippincott, 1995; with permission.)
The floor of each supravesical fossa is formed in part by contributions of the endopelvic fascia, the transversalis fascia, and preperitoneal connective
tissue. In the presence of an empty bladder, the proximal part of the supravesical fossa is formed by the transversalis fascia. The vesical fascia and the
vesicoumbilical fascia, which continues upward to the umbilicus, is derived from preperitoneal connective tissue. This tissue continues into the pelvis
where it is continuous with the endopelvic fascia of the so-called lateral pillars of the bladder.
The upward continuation of the vesical fascia gradually becomes united with the transversalis fascia somewhere between the umbilicus and the
semicircular line of Douglas. Keynes
27
considered the transverse fold of the bladder the lower limit of the supravesical fossa; we concur. Although the
transverse fold of the bladder is more marked in certain individuals, to go beyond this more typical line would unnecessarily expand the concept of the
supravesical fossa.
Rare and Abnormal Peritoneal Folds
Occasionally adhesions, bands, and folds may be present in a virgin peritoneal cavity (one without previous surgery or inflammatory process). In most
cases their presence is quite benign. At times, they can be the cause of partial or complete intestinal obstruction.
The embryogenesis of these entities is enigmatic. Their location, size, length, width, etc., are not always constant. The following bands have been noted,
beginning from above and proceeeding downward.
At the right upper quadrant and the gallbladder area (on the right): In surgery and dissection, Skandalakis has viewed different anomalous or variable peritoneal
(lesser omental) folds from the gallbladder. In order of frequency, they are the cholecystoduodenal fold, the cholecystocolic fold, and the cholecystogastric fold
(Fig. 10-14).
On the left: A band which is unrelated to the ligament of Treitz or to the paraduodenal fossae may occasionally bridge the duodenojejunal junction to the
transverse mesocolon.
28
At the right lower quadrant: The membrane of Jackson is a thin sheet of peritoneum occasionally containing small blood vessels. It spreads from the right lateral
gutter to the right edge of the greater omentum, or occasionally, to the mesentery of the small bowel, partially covering the ascending colon, cecum and appendix.
It may be narrow or wide.
A thin band may run from the terminal ileum to the retroperitoneal space.
28
The so-called sustentaculum hepatis is a band that anchors the right wall of the ascending colon to the lateral abdominal wall at about the level of the iliac
crest.
28
At the left lower quadrant: At the proximal and distal ends of the sigmoid colon, a fibrous band brings the ends together.
28
There may be another band which fixes the proximal sigmoid colon to the posterior abdominal wall.
28
Fig. 10-14.
5/23/2014 Print: Chapter 10. Peritoneum, Omenta, and Internal Hernias
http://web.uni-plovdiv.bg/stu1104541018/docs/res/skandalakis' %20surgical%20anatomy%20-%202004/Chapter%2010_%20Peritoneum,%20Omenta,%20and% 20/62
Inconstant peritoneal folds of gallbladder to duodenum, colon, or stomach. (Modified from Skandalakis JE, Gray SW. Surgical anatomy of intestinal obstruction. In:
Fielding LP, Welch JP. Intestinal Obstruction. Edinburgh: Churchill Livingstone, 1987; with permission.)
Compartments of the Peritoneum
The peritoneal cavity can be divided into two major compartments by an imaginary cross-sectional plane that passes through the transverse mesocolon.
This division defines a supracolic and an infracolic compartment (see Fig. 10-7).
Within the supracolic compartment, the liver determines a right and left suprahepatic (subdiaphragmatic) space and a right and left infrahepatic space.
The infracolic compartment is divided by the mesentery of the small bowel into a right infracolic (supramesenteric) compartment, a left infracolic
(inframesenteric) compartment, and the pelvic cavity (compartment). In addition, there are right and left paracolic gutters, discussed later in this
chapter. The left gutter is infracolic only, being interrupted by the phrenicocolic ligament. The right gutter extends upward into the supracolic
compartment. There is no right phrenicocolic ligament.
The pelvic cavity is divided into right and left spaces by the sigmoid colon and the rectum. It is further subdivided in the female into anterior and posterior
spaces by the broad ligament, uterine tubes, and uterus.
Supracolic Compartment
MESOGASTRIA
Ventral Mesogastrium
From a technical standpoint, there is no question that the supracolic compartment is the most difficult surgical area of the peritoneal cavity. Our
description is based on the work of Livingston,
1
Ochsner and Graves,
29
Mitchell,
30
Autio,
31
Boyd,
32
Whalen,
33
Harley,
34
and Meyers.
35
Early in development there is a dorsal and a ventral mesentery. The ventral mesentery disappears, except for that of the foregut. Its persisting segment
extends from the umbilicus to the abdominal esophagus. The liver divides the ventral mesentery into the falciform ligament anteriorly and the lesser
omentum posteriorly. The falciform, coronary, and hepatogastric ligaments are derivatives of the primitive ventral mesogastrium. The greater omentum and
the gastrophrenic ligament are derivatives of the dorsal mesogastrium.
The falciform ligament begins at the umbilicus. It is attached to the abdominal wall and passes to the superior surface of the left lobe of the liver, where it
separates the lateral and medial segments of the left lobe.
The free edge of the falciform ligament contains the paraumbilical veins (of Sappey) and the cordlike round ligament (ligamentum teres) of the liver. This is
the remnant of the left umbilical vein. The right umbilical vein disappears early in development. The left umbilical vein carries placental blood to the fetus
and closes at birth. This vascular remnant is often patent for much of its length.
36
The intrahepatic portion of the left umbilical vein becomes the
ligamentum venosum, which connects the left branch of the portal vein with the left hepatic vein or the inferior vena cava. The falciform ligament is thus
the mesentery of the left umbilical vein.
The lesser omentum is divided into the hepatogastric ligament and the hepatoduodenal ligament (Fig. 10-15). The hepatogastric ligament extends from the
porta hepatis to the lesser curvature of the stomach and the abdominal esophagus. The ligament encloses the gastroesophageal junction on the right.
The two leaves rejoin on the left as the gastrosplenic ligament, a portion of the embryonic dorsal mesentery. The posterior leaf does not reach the
gastroesophageal junction, so there is a small bare area on the posterior wall of the stomach that lies on the left crus of the diaphragm. It is related to
the left adrenal gland and the left gastric artery and vein.
37
Fig. 10-15.
5/23/2014 Print: Chapter 10. Peritoneum, Omenta, and Internal Hernias
http://web.uni-plovdiv.bg/stu1104541018/docs/res/skandalakis' %20surgical%20anatomy%20-%202004/Chapter%2010_%20Peritoneum,%20Omenta,%20and% 21/62
Mesenteries of the stomach. (Modified from Skandalakis JE, Gray SW, Rowe JS Jr. Anatomical Complications in General Surgery. New York: McGraw-Hill, 1983; with
permission.)
The hepatogastric ligament contains the left gastric artery and vein and the hepatic division of the anterior vagal trunk. Occasionally, it may contain the
right gastric artery and vein and both vagal trunks. In about one-fourth of subjects, it contains the aberrant left hepatic artery, which arises from the left
gastric artery.
38
This aberrant left hepatic artery is liable to injury in the now rarely performed highly selective vagotomy operation or other procedures for
benign disease in the perigastric region, such as gastric devascularization for portal hypertension.
The hepatoduodenal ligament extends between the liver and the first portion of the duodenum, practically forming the right border of the hepatogastric
ligament. It contains the common bile duct, the hepatic artery, and the portal vein. In about one-fifth of patients, it contains an aberrant right hepatic
artery, usually arising from the superior mesenteric artery. This aberrant right hepatic artery invariably lies behind the portal vein as it passes upward
toward the liver, and therefore contrary to expectations is not usually in danger of injury during resection of the bile duct or hepatoduodenal ligament in
pancreaticobiliary operations. The prudent surgeon will, however, check for its presence once the posterior aspect of the portal vein has been exposed.
The hepatoduodenal ligament can be considered the mesentery of the portal triad. It is also the anterior boundary of the epiploic foramen of Winslow.
The coronary ligaments, as indicated previously, also are remnants of the embryonic ventral mesentery (Fig. 10-15). Their outer surface is peritoneum,
whereas their inner surface forms the boundary of the bare area. The right and left lateral extremities of the coronary ligaments are the triangular
ligaments. They are not located linearly: the right is more posterior and lateral; the left is more superior and medial. The coronary and triangular ligaments
are described in more detail in the chapter on the stomach.
Dorsal Mesogastrium
The primitive dorsal mesentery (Fig. 10-16A), unlike the ventral mesentery, persists in the adult. In the supracolic compartment, it forms the greater
omentum. Originally, the dorsal mesentery extended from the dorsal border of the stomach to the midline of the dorsal (posterior) body wall (Fig. 10-16A).
This simple relationship becomes altered by the counterclockwise rotation of the stomach through 90, and by the developing spleen.
Fig. 10-16.
5/23/2014 Print: Chapter 10. Peritoneum, Omenta, and Internal Hernias
http://web.uni-plovdiv.bg/stu1104541018/docs/res/skandalakis' %20surgical%20anatomy%20-%202004/Chapter%2010_%20Peritoneum,%20Omenta,%20and% 22/62
A, Primitive embryonic relations. B, Adult relations. Note location of ligaments. (Modified from Skandalakis JE, Gray SW, Rowe JS Jr. Anatomical Complications in
General Surgery. New York: McGraw-Hill, 1983; with permission.)
For all practical purposes, the embryonic dorsal mesogastrium is the adult greater omentum. It can be divided into three parts:
Upper: gastrophrenic ligament
Middle: gastrosplenic ligament
Lower: gastrocolic ligament
The gastrophrenic ligament extends from the proximal greater curvature of the stomach, the gastroesophageal junction, and the abdominal esophagus to
the diaphragm. The upper part is avascular; the lower part contains some short gastric vessels and lymph nodes.
The middle portion of the dorsal mesentery is interrupted by the spleen to form a posterior splenorenal ligament and a more anterior gastrosplenic ligament
(Fig. 10-16B, Fig. 10-17A). Together, these form the splenic pedicle (Fig. 10-17A & B).
Fig. 10-17.
5/23/2014 Print: Chapter 10. Peritoneum, Omenta, and Internal Hernias
http://web.uni-plovdiv.bg/stu1104541018/docs/res/skandalakis' %20surgical%20anatomy%20-%202004/Chapter%2010_%20Peritoneum,%20Omenta,%20and% 23/62
Splenic pedicle. A, Long pedicle with a presplenic fold. B, Short pedicle. (Modified from Skandalakis JE, Gray SW, Rowe JS Jr. Anatomical Complications in General
Surgery. New York: McGraw-Hill, 1983; with permission.)
The splenorenal ligament contains the splenic artery and vein and the tail of the pancreas. The gastrosplenic ligament contains the short gastric and left
gastroepiploic vessels. These relationships are described in more detail in the chapter on the spleen.
The gastrocolic ligament is the part of the dorsal mesogastrium between the greater curvature of the stomach and the transverse colon. At its earliest
appearance, the mesogastrium includes the duodenum and the pancreas; it attaches to the posterior body wall (Fig. 10-18A). By the fourth month of
gestation, the duodenum and the pancreas have become retroperitoneal (Fig. 10-18B and 10-19A-C). The future omentum has formed a sac, the omental
bursa, that extends in front of the transverse colon (Fig. 10-18B). Fusion of the anterior and posterior walls of the dependent portion of the omental
bursa obliterates most of the lower recess of the bursa, leaving only the superior portion of the cavity behind the stomach and in front of the colon (Fig.
10-18C).
Fig. 10-18.
Development of omentum and lesser sac. A, At two months. Duodenum and pancreas are contained in dorsal mesogastrium. Arrow indicates opening of epiploic
foramen into lesser sac. B, At four months. Duodenum and pancreas are retroperitoneal; greater omentum is elongating. C, Adult configuration. Cavity of greater
omentum is obliterated; posterior wall has fused with transverse colon (TC) and transverse mesocolon. L, liver; S, stomach; J, jejunum; P, pancreas; D,
duodenum. Dashed line indicates plane of fusion. (Modified from Skandalakis JE, Gray SW, Rowe JS Jr. Anatomical Complications in General Surgery. New York:
McGraw-Hill, 1983; with permission.)
Fig. 10-19.
5/23/2014 Print: Chapter 10. Peritoneum, Omenta, and Internal Hernias
http://web.uni-plovdiv.bg/stu1104541018/docs/res/skandalakis' %20surgical%20anatomy%20-%202004/Chapter%2010_%20Peritoneum,%20Omenta,%20and% 24/62
Changing relations of duodenum, pancreas, and posterior body wall in developing embryo. A, Primitive ventral mesentery and dorsal and ventral pancreatic
primordia are present. B, Disappearance of ventral mesentery and fusion of pancreatic primordia. C, Final retroperitoneal position of duodenum and pancreas.
Compare with Figure 10-18C. (Modified from Skandalakis JE, Gray SW, Rowe JS, Skandalakis LJ. Anatomical complications of pancreatic surgery. Contemp Surg
15:17-40, 1979; with permission.)
The anterior wall of the sac in the adult remains free; the posterior layer fuses with the transverse colon and the mesocolon. Only with this fusion does it
become entitled to the name gastrocolic ligament. The size and extent of the omental bursa depends on the degree of fusion of the two walls of the sac
below, as well as on the fusion of the posterior wall of the sac with the transverse mesocolon. The right portion, which arises from the antrum of the
stomach, is frequently fused with the anterior surface of the head of the pancreas. The omentum should be freed from the pancreas from left to right.
39
Where two peritoneal layers of the posterior wall of the bursa fuse with two peritoneal layers of the transverse mesocolon, there are, at first, four
peritoneal layers. Only the two outer layers, above and below, are found in the adult mesocolon.
SPACES OF THE SUPRACOLIC COMPARTMENT
The several spaces formed by the peritoneum around the organs of the supracolic compartment are extremely important to radiologists and surgeons. We
are concerned here with those above and below the liver, the perihepatic spaces.
Suprahepatic (Subphrenic) Spaces
Parts of the superior surface of the liver and the inferior surface of the diaphragm are in direct contact with one another, and are thus barren of
peritoneal covering. This is the bare area. The margins of the bare area are the falciform, coronary, and triangular ligaments of the liver (see Fig. 10-8).
Except over this bare area, the serous surfaces of the liver and the diaphragm are in apposition, with a potential space between. This potential space may
become the site of intraperitoneal fluid collection and of suprahepatic (subphrenic) abscesses. The potential space is divided into right and left spaces by
the falciform ligament.
The right suprahepatic space (Fig. 10-20) lies between the diaphragm and the anterosuperior surface of the right lobe and the medial segment of the left
lobe of the liver. The medial boundary is the falciform ligament; the posterior boundary is composed of the right anterior coronary and right triangular
ligaments. The inferior boundary is the right lobe and the medial segment of the left lobe of the liver. The space opens into the general peritoneal cavity
anteriorly and inferiorly.
Fig. 10-20.
5/23/2014 Print: Chapter 10. Peritoneum, Omenta, and Internal Hernias
http://web.uni-plovdiv.bg/stu1104541018/docs/res/skandalakis' %20surgical%20anatomy%20-%202004/Chapter%2010_%20Peritoneum,%20Omenta,%20and% 25/62
Parasagittal section through right upper abdomen showing potential right suprahepatic and subhepatic spaces. Thick black line represents diaphragm. (Modified
from Skandalakis JE, Gray SW, Rowe JS Jr. Anatomical Complications in General Surgery. New York: McGraw-Hill, 1983; with permission.)
The corresponding suprahepatic space on the left (Fig. 10-21) is between the diaphragm and the superior surface of the lateral segment of the left lobe
of the liver and the fundus of the stomach. Medially, the left suprahepatic space is bounded by the falciform ligament and, posteriorly, by the left
coronary and triangular ligaments. Anteriorly and laterally, the space communicates with the infrahepatic space and the general peritoneal cavity.
Remember: on the left, the anterior and posterior leaves of the coronary ligament are in apposition.
Fig. 10-21.
Parasagittal section through left upper abdomen showing potential left suprahepatic and subhepatic spaces. (Modified from Skandalakis JE, Gray SW, Rowe JS Jr.
Anatomical Complications in General Surgery. New York: McGraw-Hill, 1983; with permission.)
Each of these spaces may be divided into anterior and posterior portions. The distinction is unimportant in the absence of disease. On the right (Fig. 10-
22), fluid may collect or an abscess may form between the liver and the diaphragm anteriorly, just beneath the sternum (right anterior suprahepatic
abscess), or it may form at the reflection of the anterior leaf of the coronary ligament (right posterior suprahepatic abscess) (Fig. 10-23). The single
space of the anatomist may thus be divided by pseudomembranes into two spaces.
Fig. 10-22.
5/23/2014 Print: Chapter 10. Peritoneum, Omenta, and Internal Hernias
http://web.uni-plovdiv.bg/stu1104541018/docs/res/skandalakis' %20surgical%20anatomy%20-%202004/Chapter%2010_%20Peritoneum,%20Omenta,%20and% 26/62
Relations of abscess in anterior portion of right suprahepatic space. (Modified from Skandalakis JE, Gray SW, Rowe JS Jr. Anatomical Complications in General
Surgery. New York: McGraw-Hill, 1983; with permission.)
Fig. 10-23.
Relations of abscess in posterior portion of right suprahepatic space. (Modified from Skandalakis JE, Gray SW, Rowe JS Jr. Anatomical Complications in General
Surgery. New York: McGraw-Hill, 1983; with permission.)
5/23/2014 Print: Chapter 10. Peritoneum, Omenta, and Internal Hernias
http://web.uni-plovdiv.bg/stu1104541018/docs/res/skandalakis' %20surgical%20anatomy%20-%202004/Chapter%2010_%20Peritoneum,%20Omenta,%20and% 27/62
Surgery. New York: McGraw-Hill, 1983; with permission.)
The left suprahepatic space (Figs. 10-24, 10-25) may be similarly compartmentalized by pseudomembranes between the liver and the diaphragm or the
abdominal wall. The left suprahepatic and left anterior infrahepatic spaces are not separated anatomically, but they may become separated pathologically
by pseudomembranes. Large accumulations of fluid may extend into the subhepatic space, where the stomach, spleen, and liver participate in walling off
the infection. The diaphragm is usually elevated over the abscess or fluid collection.
Fig. 10-24.
Relations of abscess in anterior portion of left suprahepatic space. (Modified from Skandalakis JE, Gray SW, Rowe JS Jr. Anatomical Complications in General
Surgery. New York: McGraw-Hill, 1983; with permission.)
Fig. 10-25.
5/23/2014 Print: Chapter 10. Peritoneum, Omenta, and Internal Hernias
http://web.uni-plovdiv.bg/stu1104541018/docs/res/skandalakis' %20surgical%20anatomy%20-%202004/Chapter%2010_%20Peritoneum,%20Omenta,%20and% 28/62
Relations of abscess in posterior portion of left suprahepatic space. (Modified from Skandalakis JE, Gray SW, Rowe JS Jr. Anatomical Complications in General
Surgery. New York: McGraw-Hill, 1983; with permission.)
Localization, extension, and size of the suprahepatic abscess or collection will determine the surgical approach. The surgeon and the radiologist must
cooperate to evaluate the anatomy that is altered by the formation of membranes and the pressure of the abscess.
Anteriorly, the approach from beneath the costal margin presents no anatomic complications. Posteriorly, the approach must be by an incision at the level
of the spinous process of the first lumbar vertebra to avoid entering the pleura. Remember the relationship of the pleura and the 12th rib at the vertebral
spine. Do not open the bed of the 12th rib.
Nowak et al.
40
advocated the dorsolateral approach to the left subphrenic area as well as to the omental bursa and the tail of the pancreas. This is a
particularly useful approach by a surgeon or radiologist for the drainage of a left-sided pancreatic abscess complicating acute pancreatitis. The approach
does not violate the peritoneal cavity and provides dependent drainage in the recumbent patient.
Infrahepatic Spaces
The right infrahepatic space (subhepatic space, hepatorenal space, pouch of Morison) (Fig. 10-26) is bounded superiorly and anteriorly by the right lobe
and the medial segment of the left lobe of the liver and the gallbladder, and superiorly and posteriorly by the posterior layer of the coronary and right
triangular ligament. Inferiorly, the space opens into the general peritoneal cavity and is partly bounded by the hepatic flexure of the colon and the
transverse mesocolon and, medially, by the hepatoduodenal ligament.
Fig. 10-26.
Relations of abscess in right infrahepatic space, right anteroinferior subhepatic space, and right posterosuperior subhepatic space. (Modified from Skandalakis JE,
Gray SW, Rowe JS Jr. Anatomical Complications in General Surgery. New York: McGraw-Hill, 1983; with permission.)
The right infrahepatic space communicates with the right suprahepatic space at the:
5/23/2014 Print: Chapter 10. Peritoneum, Omenta, and Internal Hernias
http://web.uni-plovdiv.bg/stu1104541018/docs/res/skandalakis' %20surgical%20anatomy%20-%202004/Chapter%2010_%20Peritoneum,%20Omenta,%20and% 29/62
The right infrahepatic space communicates with the right suprahepatic space at the:
Margin of the right lobe of the liver
Right triangular ligament
Quadrangular space of Mitchell
The quadrangular space of Mitchell is a small space bounded above by the quadrate lobe of the liver, below by the transverse colon, on the left by the
falciform ligament, and on the right by the gallbladder.
Remember
The coronary ligament suspends the liver not from above, but from the dorsum. The left triangular ligament suspends the left lobe not from the apex of
the diaphragm, but from the dorsal aspect of the diaphragm.
32
The left infrahepatic space may be divided into a small antegastric space and the larger lesser sac of the peritoneum (Fig. 10-27). The anterior space lies
between the left lobe of the liver above and the stomach below and behind. The boundaries superiorly and anteriorly are the left lobe of the liver and the
anterior abdominal wall; posteriorly, the stomach and the lesser omentum; and inferiorly, the middle third of the transverse colon. The term perigastric has
been used, but it is misleading, since this space is entirely anterior to the stomach. Hollinshead
41
felt that it is merely part of the left suprahepatic
(subphrenic) space in general.
Fig. 10-27.
Relations of abscess in left infrahepatic space and left anterior subhepatic space. (Modified from Skandalakis JE, Gray SW, Rowe JS Jr. Anatomical Complications in
General Surgery. New York: McGraw-Hill, 1983; with permission.)
The lesser sac of the peritoneum becomes, by the terminology used here, the left posterior infrahepatic space. This is a valid concept, but for practical
purposes, the lesser sac or the omental bursa are the preferred terms.
Extraperitoneal Spaces
There are two potential spaces in which extraperitoneal abscesses may occur. On the right, there is the bare area of the liver, which is outlined by the
falciform, coronary, and triangular ligaments (see Fig. 10-8). On the left, there is a poorly defined space that is bounded by the distal pancreas, the
descending (left) colon, the upper pole of the left kidney, the left adrenal gland, Gerota's perirenal fascia, and fat. For additional information about these
and other sites of retroperitoneal abscesses, we recommend the excellent study by Altemeier and Alexander.
42
INFRACOLIC COMPARTMENT
Paracolic Gutters
There are 2 paracolic gutters. They are located on the lateral and medial sides of the ascending and descending colon.
The right lateral paracolic gutter communicates freely with the right posterior subphrenic space. Therefore, pelvic fluid can reach the diaphragm and fluids
from the upper abdomen can drain into the pelvic cavity.
Because of the presence of the phrenicocolic ligament, the left lateral paracolic gutter does not communicate with the perisplenic areas and the left
subdiaphragmatic space.
Below the plane of the transverse mesocolon, the infracolic compartment is divided diagonally by the root of the mesentery of the small intestine. The
infracolic compartment is subdivided into a right infracolic (supramesenteric) compartment and a left infracolic (inframesenteric) compartment. Below these
areas is the pelvic cavity, and beside them are the paracolic gutters.
5/23/2014 Print: Chapter 10. Peritoneum, Omenta, and Internal Hernias
http://web.uni-plovdiv.bg/stu1104541018/docs/res/skandalakis' %20surgical%20anatomy%20-%202004/Chapter%2010_%20Peritoneum,%20Omenta,%20and% 30/62
The right infracolic space is bounded medially and inferiorly by the root of the mesentery, laterally by the ascending (right) colon, superiorly by the right
transverse mesocolon, and anteriorly by the greater omentum. The space is filled with loops of small intestine. It is in communication with the left
infracolic space anteriorly and the left pelvic space inferiorly.
The left infracolic space is bounded medially and superiorly by the root of the mesentery, laterally by the descending (left) colon, inferiorly and laterally by
the sigmoid colon, and anteriorly by the greater omentum. It communicates with the right infracolic space anteriorly and the right pelvic space inferiorly.
Drainage Patterns
The spread of fluid in the peritoneal cavity depends on all of the following:
Location of the source and the rate of fluid production
Pressure differences in the abdomen
Mesenteric partitions and peritoneal fossae
Position of the body in relation to gravity
Both infection and metastatic seeding of malignant cells will follow transcoelomic patterns determined by these factors.
Meyers
35
examined sites of metastatic seeding in several series of patients with primary cancer of the ovary, pancreas, stomach, or colon (Fig. 10-28).
The most frequently affected site was the pouch of Douglas (50%), the most dependent part of the peritoneum. The mesentery of the small intestine
(40%) and the sigmoid mesocolon (20%) both form barriers at which ascitic fluid may accumulate before spilling over into the pelvis. These barriers were
sites of metastatic seeding. In 20% of cases, seeding was to the right paracolic gutter.
Fig. 10-28.
5/23/2014 Print: Chapter 10. Peritoneum, Omenta, and Internal Hernias
http://web.uni-plovdiv.bg/stu1104541018/docs/res/skandalakis' %20surgical%20anatomy%20-%202004/Chapter%2010_%20Peritoneum,%20Omenta,%20and% 31/62
Posterior abdominal wall. Mesenteric attachments and chief sites of seeding of carcinoma of ovary, pancreas, stomach, and colon, in order of frequency: 1, Pouch
of Douglas; 2, Distal attachment of mesentery; 3, Attachment of sigmoid mesocolon; 4, Right paracolic gutter; BA, Bare area; C, Attachment of colon; D,
Attachment of duodenum; PC, phrenocolic ligament; S, Attachment of stomach; SB, Attachment of mesentery of small bowel. (Modified from Skandalakis JE, Gray
SW, Rowe JS Jr. Anatomical Complications in General Surgery. New York: McGraw-Hill, 1983; with permission; data from Meyers MA. Dynamic Radiology of the
Abdomen (4th ed). New York: Springer-Verlag, 1994.)
PELVIC CAVITY
The sigmoid colon and the rectum divide the pelvic cavity into right and left spaces. In the female, a further division into anterior and posterior spaces is
produced by the broad ligament, uterus, uterine tubes, and ovaries. The tunica vaginalis of the male scrotum is embryologically part of the pelvic cavity.
ABDOMINAL COMPARTMENT SYNDROME
By definition the abdominal compartment syndrome consists of bowel distention, edema, and intraperitoneal fluid collection such as exudates and blood.
Packs which are left intentionally for tamponade (or a pack accidentally left) also may produce the syndrome in severely injured patients.
Elevation of the abdominal pressure, reduced pulmonary compliance secondary to diaphragmatic compression, renal dysfunction, hepatic and intestinal
ischemia, and shock all produce the clinical entity of abdominal compartment syndrome. Mayberry et al.
43
advised prevention of the syndrome using
absorbable mesh prosthesis in severely injured patients undergoing celiotomy.
Organ and Porter
44
reported the following.
A major advance in recent years has been the application of the damage control approach to complex trauma and general surgery cases.
45
Damage
control is a paradigm shift in the surgical management of critically injured patients from repairing all injuries at the first operation to a staged
approach. It consists of 3 phases. The first phase is immediate exploratory laparotomy for the control of hemorrhage and gross contamination, with
rapid, simple closure of the abdomen. The second phase is continued resuscitation in the intensive care unit for correction of acidosis,
coagulopathy, and hypothermia. The final phase is definitive repair of all injuries after resuscitation has been completed.
Patients with extensive abdominal injuries, including those managed by the damage control approach, are at high risk for increased intra-abdominal
pressure and the abdominal compartment syndrome. This syndrome is defined as increased intra-abdominal pressure, increased airway pressures
with hypoxia and hypercarbia, and renal dysfunction (oliguria or anuria).
43,46
Ivatury et al.
46
described the profound abdominal and systemic
effects of intra-abdominal hypertension. The adverse hemodynamic and respiratory alterations associated with intra-abdominal hypertension act
synergistically with inadequate tissue perfusion, the cytokine cascade, and infections to produce organ dysfunction and death.
Abdominal compartment syndrome is, therefore, an increase in intraabdominal pressure secondary to trauma and other surgical or medical conditions.
Watson and Howdieshell
47
presented an excellent paper about the syndrome, the danger of which has only recently been recognized. They found
decompressive celiotomy to be the treatment of choice. Ertel and colleagues
48
recommended the continuous measurement of urinary bladder pressure in
at-risk patients as a less complex, noninvasive, cost-effective diagnostic tool for the early detection of elevated intra-abdominal pressure. They reported
that decompression laparotomy immediately restored impaired organ function.
SUMMARY
The intraperitoneal spaces are the:
Right suprahepatic (subphrenic) space (see Fig. 10-20); anterior and posterior sites of abscesses
Left suprahepatic (subphrenic) space (see Fig. 10-21); anterior and posterior sites of abscesses
Right infrahepatic (subhepatic) space (Fig. 10-26)
Left infrahepatic (subhepatic) space (Fig. 10-27); the antegastric recess and the lesser sac are potential sites of abscesses
The extraperitoneal spaces are the:
Bare area of the liver and the diaphragm
Left extraperitoneal space
The formation of adhesions and pseudomembranes may contribute to the formation of several collections of abscesses in various parts of each space.
All these spaces may be approached by an extraserous intercostal incision (right or left, anterior or posterior) at the level of the spinous process of the
first lumbar vertebra. A transpleural approach should not be used. Empyema and diaphragmatic injury have high mortality and morbidity.
SURGICAL ANATOMY OF THE OMENTA AND THE OMENTAL BURSA
Rutherford Morison
49
developed the concept of the omentum as an "abdominal policeman" of the peritoneal cavity. Both protection and brutality
characterize the omentum's role: protection in inflammatory processes; and the well-known "brutality" occurs in omental involvement in some forms of
cancer (ovarian, etc.).
There are two omenta, the greater and the lesser.
Greater Omentum
Surgically the greater omentum (see Figs. 10-3, 10-4, 10-5) can be divided into two parts:
The gastrocolic ligament connecting the greater curvature of the stomach and the transverse colon
5/23/2014 Print: Chapter 10. Peritoneum, Omenta, and Internal Hernias
http://web.uni-plovdiv.bg/stu1104541018/docs/res/skandalakis' %20surgical%20anatomy%20-%202004/Chapter%2010_%20Peritoneum,%20Omenta,%20and% 32/62
The fat apron or "greater omentum" which hangs from the transverse colon to the free peritoneal cavity
For all practical purposes, the greater omentum is the embryologic home of the spleen, pancreas, and all branches related to the splenic artery and vein.
By definition, the greater omentum hangs from the greater curvature of the stomach in the form of a thin-walled sac, which helps form the omental sac or
bursa (see Fig. 10-3). In the adult, the greater omentum extends downward to the transverse colon, fusing with it and the transverse mesocolon to a
varying degree. Continuing further down as a free fat apron, it covers loops of the small bowel and (occasionally) pelvic organs.
There is great variation in the length of the omentum. Anson et al.,
50
in a study of 125 cadavers, were not able to visualize the omentum in 19% of
cases. The omentum was a "mere fringe" in 2% of cases. It extended 14.0-19.5 cm below the xiphisternal joint in 8% of cases. The omentum extended
20-36 cm below the xiphosternal articulation in the remainder (71%).
In adulthood, the width of the greater omentum varies from individual to individual. In infancy, it is small and not well developed.
Liebermann-Meffert and White
4
discuss omental attachment to the duodenum and ascending colon, attachment from the pyloric area only, attachment to
the stomach, and attachment to the spleen. They also discuss the possibility of lack of attachment to the above organs. The abdominal surgeon
recognizes that the attachments of the greater omentum and its free edges are extremely variable. It is unusual to find the greater omentum "floating
free" in the peritoneal cavity; more often there are attachments which have to be lysed for its full mobilization. When upper abdominal surgeons operate
through a transverse or subcostal incision and wish to mobilize the greater omentum for an omentectomy or access to the lesser sac, they may find that
through such an incision these attachments are difficult to visualize and divide.
The gastrocolic ligament is composed of that part of the greater omentum that extends between the first part of the duodenum and great curvature of
the stomach to the transverse colon. The right and left gastroepiploic vessels are contained between the leaflets of the gastrocolic ligament.
Vascular Supply of the Greater Omentum
ARTERIES
The blood supply of the omentum is presented very well by Griffith.
51
For all practical purposes, the omentum is a transparent network with an excellent
blood supply from the gastroepiploic arteries (Fig. 10-29).
Fig. 10-29.
5/23/2014 Print: Chapter 10. Peritoneum, Omenta, and Internal Hernias
http://web.uni-plovdiv.bg/stu1104541018/docs/res/skandalakis' %20surgical%20anatomy%20-%202004/Chapter%2010_%20Peritoneum,%20Omenta,%20and% 33/62
Arterial supply of greater omentum. RGE, Right gastroepiploic; LGE, Left gastroepiploic; RE, Right epiploic; LE, Left epiploic; AB, Arc of Barkow; G, Gastric branches;
AE, Anterior epiploic branches; PE, Posterior epiploic branches; P, Pancreatic artery; VR, Vasa recta of midcolic artery.
The right and left gastroepiploic arteries anastomose and form the arc of Barkow through their branches (right and left epiploic) in the posterior omental
layer. The arc of Barkow is reinforced by anterior epiploic arches, which spring from the right and left gastroepiploic arteries and from posterior epiploic
branches from the pancreatic vessels.
Griffith
51
advised ligation of the anterior epiploic branches or ligation of the right gastroepiploic artery distal to the origin of the right epiploic artery. This
fosters omental viability since it preserves the arc of Barkow. It is an open question whether Griffith's approach is better than ligation of the gastric
branches that arise from the right and left gastroepiploic arteries to the greater curvature of the stomach. While the latter technique may be a tedious
task, it is the opinion of the authors of this chapter that it is a better choice and safer because most surgeons remember more of the anatomy of the
gastroepiploic vessels than of the epiploic vessels.
VEINS
The veins drain into the portal system.
Is the blood supply of the omentum ever insufficient? We do not know. Idiopathic infarction of the greater omentum has been reported by Skandalakis.
52
LYMPHATICS
According to Liebermann-Meffert and White,
4
there are two draining pathways for the lymphatics of the omentum (Fig. 10-30): one travels to the right
toward the subpyloric nodes; the other travels to the left toward the splenic nodes. Nylander and Tjernberg
53
and Sarrazin et al.
54
reported
communication between the lymphatics of the omentum and the stomach.
Fig. 10-30.
Lymphatic drainage. (Modified from Liebermann-Meffert D. Omentum in the adult. In: Liebermann-Meffert D, White H (eds). The Greater Omentum: Anatomy,
Physiology, Pathology, Surgery with a Historical Survey. New York: Springer-Verlag, 1983; with permission.)
Lesser Omentum
The lesser omentum (see Figs. 10-3, 10-5) is a double-layered entity suspended between the lesser curvature of the stomach and the proximal inch (2
cm) of the first part of the duodenum inferiorly and the porta hepatis and the fissure of the ligamentum venosum superiorly. The lesser omentum is divided
conventionally into two ligaments: the hepatogastric and the hepatoduodenal (see Fig. 10-15). Located within the lesser omentum are the hepatic triad,
branches of the anterior vagus nerve, some lymph nodes, and the right and left gastric arteries.
Omental Bursa or Lesser Sac
The omental bursa (lesser sac) is a potential space behind the stomach. It can be divided into a vestibule and into the bursa proper. The peritoneal
covering that can be traced from the spleen to the posterior abdominal wall covering the anterior surface of the pancreas is a part of the primitive dorsal
mesentery of the stomach.
5/23/2014 Print: Chapter 10. Peritoneum, Omenta, and Internal Hernias
http://web.uni-plovdiv.bg/stu1104541018/docs/res/skandalakis' %20surgical%20anatomy%20-%202004/Chapter%2010_%20Peritoneum,%20Omenta,%20and% 34/62
mesentery of the stomach.
The vestibule, beginning at the epiploic foramen, is formed by the pancreaticogastric fold, which contains the left gastric artery from the retroperitoneal
space to the lesser curvature of the stomach. It creates a bridge between the aorta, close to the esophageal hiatus of the diaphragm, and the
hepatogastric ligament. A finger-breadth below this fold is the pancreaticoduodenal fold, which contains the hepatic artery as it passes from the
retroperitoneal space to the hepatoduodenal ligament just below the pylorus and the first part of the duodenum. The opening of the vestibule into the
bursa proper has been called the second epiploic foramen.
The bursa proper, when considered in midsagittal section (see Fig. 10-18C), is bounded anteriorly by the lesser omentum, stomach, and gastrocolic
ligament, and posteriorly by the retroperitoneal space. The roof is formed by the caudate lobe of the liver, the coronary ligament on the right, and the
abdominal esophagus on the left. The floor is formed by the transverse colon and the mesocolon.
When considered in cross-section (Fig. 10-31), the bursa is bounded anteriorly by the hepatoduodenal ligament and the hepatic triad, the hepatogastric
ligament, the gastrosplenic ligament, and the stomach. Posteriorly, the bursa is bounded by the splenorenal ligament and the pancreas. On the right is the
epiploic foramen; on the left, in front, is the distal part of the gastrosplenic ligament; and behind is the distal part of the splenorenal ligament.
Fig. 10-31.
Omental bursa.
Other Mesenteries and Ligaments
Other mesenteries and ligaments of the peritoneal cavity and omentum will be described with their related organs.
PERIHEPATIC COLLECTIONS
Anatomic Sites of Abscesses and Fluid Collections
Abscesses and fluid collections may occupy any of the potential spaces. They are usually localized, i.e., walled off by pseudomembranes. Some of the
usual areas of abscesses and collections, discussed earlier in surgical anatomy, are summarized below.
Above the Liver (Suprahepatic, Subphrenic)
COLLECTIONS IN THE RIGHT ANTERIOR SUPRAHEPATIC SPACE
Fig. 10-22. The boundaries are:
Posterior: Liver
Anterior: Diaphragm and anterior abdominal wall
Posteroinferior: Pseudomembranes
Superior: Pseudomembranes
COLLECTIONS IN THE RIGHT POSTERIOR SUPRAHEPATIC SPACE
Fig. 10-23. The boundaries are:
Superior: Diaphragm
Anterior: Pseudomembranes and liver
Inferior: Superior coronary ligament
5/23/2014 Print: Chapter 10. Peritoneum, Omenta, and Internal Hernias
http://web.uni-plovdiv.bg/stu1104541018/docs/res/skandalakis' %20surgical%20anatomy%20-%202004/Chapter%2010_%20Peritoneum,%20Omenta,%20and% 35/62
COLLECTIONS IN THE LEFT ANTERIOR SUPRAHEPATIC SPACE
Fig. 10-24. The boundaries are:
Right medial: Falciform ligament
Superior: Left coronary ligament and triangular ligament
Left inferior: Infrahepatic space
Posterior: Lateral segment of left hepatic lobe and pseudomembranes
Anterior: Anterior abdominal wall
COLLECTIONS IN THE LEFT POSTERIOR SUPRAHEPATIC SPACE
Fig. 10-25. The boundaries are:
Superior: Diaphragm
Posterior: Left coronary ligament
Inferior: Liver
Anterior: Pseudomembranes
Left suprahepatic collections may be walled off by pseudomembranes that bridge the edge of the liver and the abdominal wall (Fig. 10-25). If the
collection is larger, the serosa of the stomach and spleen may participate in the sequestration. Pseudomembranes and mesenteric attachments may
subdivide the left suprahepatic space into small compartments or collections near the gastric fundus, spleen, or liver.
Below the Liver (Subhepatic)
COLLECTIONS IN THE RIGHT ANTEROINFERIOR SUBHEPATIC SPACE
Fig. 10-26. The boundaries are:
Superior: Liver
Inferior: Transverse colon and transverse mesocolon
Anterior and Posterior: Pseudomembranes
COLLECTIONS IN THE RIGHT POSTEROSUPERIOR SUBHEPATIC SPACE
Fig. 10-26. The boundaries are:
Superior: Liver
Posterior: Inferior coronary ligament
Inferior: Kidney and duodenum
Anterior: Pseudomembranes
COLLECTIONS IN THE LEFT ANTERIOR SUBHEPATIC SPACE
Fig. 10-27. An abscess or fluid collection will probably be limited by the left lateral segment of the liver, the lesser omentum, stomach, and transverse
colon. This limitation is not complete. The left segment of the liver is small, so there is free communication with the left suprahepatic space above. Below,
the space communicates with the general peritoneal cavity. A typical abscess in this area will be enveloped by adhesions or pseudomembranes between
the liver and the anterior abdominal wall and between the abdominal wall and the gastrocolic omentum.
Read an Editorial Comment
Whalen
33
described three additional common locations for abscesses and fluid collection:
Anterior to the stomach, bounded anteriorly by the liver and posteriorly by the anterior wall of the stomach
Lateral to the stomach, bounded anteriorly by the surface of the spleen and posteriorly by the splenic hilum
Posterior to the stomach, bounded anteriorly by the posterior wall of the stomach and the obliterated lesser sac and posteriorly by the retroperitoneal space of
the pancreas and the left kidney
ABSCESSES OR COLLECTIONS IN THE LESSER SAC (LEFT POSTERIOR INFRAHEPATIC SPACE)
Fig. 10-27. The lesser sac is the least common location for perihepatic abscess formation, but several sites are possible:
5/23/2014 Print: Chapter 10. Peritoneum, Omenta, and Internal Hernias
http://web.uni-plovdiv.bg/stu1104541018/docs/res/skandalakis' %20surgical%20anatomy%20-%202004/Chapter%2010_%20Peritoneum,%20Omenta,%20and% 36/62
Vestibule of the lesser sac
Upper recess, behind the lesser omentum and liver
Lower recess, behind the stomach and greater omentum
Splenic recess, bounded superiorly by the stomach and gastrosplenic ligaments, inferiorly by the pancreas and the splenorenal ligament, posteriorly by the
splenic pedicle, and anteriorly by the pseudomembranes
HISTOLOGY AND PHYSIOLOGY OF THE PERITONEUM AND OMENTA
Loose connective tissue and flat mesothelial cells compose the histologic pattern of the peritoneum. The loose connective tissue forms a layer that is
covered by flat mesothelial cells and resembles vascular endothelium. The peritoneum provides mobility for the intraperitoneal organs; it may permit partial
mobility to the retroperitoneal organs.
Both parietal and visceral parts of the peritoneum have the same histologic formation: a basement membrane covered by a single layer of mesothelial
cells. Loss of these cells produces nonphysiologic adhesions between the two parts. According to Bercovici et al.,
55
for all practical purposes, the parietal
and visceral parts are in contact, with no space intervening. The parietal layer is very loosely attached to the preperitoneal fat, but the visceral layer is
fixed firmly with the subserosa of the gastrointestinal tract.
The peritoneal cavity is a potential space containing approximately 50 ml of isotonic fluid, which contains approximately 300 mononuclear cells.
55
The
accumulation of several liters of fluid is possible in disease, but in healthy individuals the peritoneum contains minimal fluid. The fluid is composed of water,
proteins, electrolytes, and diverse cellular types, including mast cells, fibroblasts, lymphocytes, macrophages, and leucocytes. Peritoneal fluid provides
lubrication to facilitate movements of the viscera against one another and the body wall.
Golden and Shaw
56
demonstrated an increase in the volume of peritoneal fluid during inflammatory processes. The number of cells rises to approximately
3000, with a great number of neutrophils.
With an abnormal peritoneal collection of fluid, the phenomenon of absorption is limited in the lower abdomen. Absorption is more active in both subphrenic
spaces. This may be due to the existence of specialized subphrenic peritoneum with gaps or peritoneal stomata and slitlike orifices.
Francis D. Moore
57
wisely wrote:
Thus the peritoneum as the envelope of the gastrointestinal tract is at once a protector of the body from gastrointestinal contamination, a
reflector or barometer of the state of the gastrointestinal tract, and, when contamination is continuing or virulent, a large absorbing serous surface
which can rapidly develop a fatal infectious process.
We also mention the hippocratic face,
58
which is so characteristic prior to any death, but especially death from peritonitis:
. . .nose sharp, eyes hollow, temples sunken, ears cold and contracted with lobes turned outward, skin tense and parched, face discolored, eyelids
livid, mouth open, lips loose and blanched. . .
The peritoneum may within minutes clear bacteria by an unknown mechanism. Conversely, it may rapidly transport bacteria into the systemic circulation
via the diaphragm, perhaps producing bacteremia. Fig. 10-32A & B from Wittmann
59
summarizes the causes of infection in the peritoneum, and Fig. 10-33
presents bacterial counts in the gastrointestinal tract. To paraphrase Sinanan,
60
abscess formation is the final defense of this remarkable membrane if the
cellular, humoral, and clearance defense mechanisms are overwhelmed.
Fig. 10-32.
5/23/2014 Print: Chapter 10. Peritoneum, Omenta, and Internal Hernias
http://web.uni-plovdiv.bg/stu1104541018/docs/res/skandalakis' %20surgical%20anatomy%20-%202004/Chapter%2010_%20Peritoneum,%20Omenta,%20and% 37/62
A, Causes of peritonitis. B, Origins of peritonitis. (From Wittmann DH. Intra-abdominal Infections. New York: Marcel Dekker, 1991; with permission.)
Fig. 10-33.
5/23/2014 Print: Chapter 10. Peritoneum, Omenta, and Internal Hernias
http://web.uni-plovdiv.bg/stu1104541018/docs/res/skandalakis' %20surgical%20anatomy%20-%202004/Chapter%2010_%20Peritoneum,%20Omenta,%20and% 38/62
Bacterial count in gastrointestinal tract. (From Wittmann DH. Intra-abdominal Infections. New York: Marcel Dekker, 1991; with permission.)
The visceral peritoneum can stretch when the gastrointestinal tract is distended, and it can be peeled surgically when the urinary bladder is distended.
The parietal peritoneum, also, can withstand great stretching, as is illustrated by the degree to which the anterior abdominal wall can be expanded by a
tremendous increase of intraabdominal fluid.
Omenta and mesenteries have the same microscopic network as the peritoneum: connective tissue covered by mesothelial cells. The connective tissue is
the pathway of the blood vessels, lymphatics, and nerves.
It is not within the scope of this chapter to present in detail all the physiologic destinies of the omentum. Following the work of Williams
61
and other
authors, we name a few for the continuity of this chapter:
Repair of adhesions
Skin grafts
Revascularization
Implantation
Repair of defects
A note about the so-called "milky spots": these are dense aggregations of macrophages, lymphocytes, and monocytes.
INTERNAL ABDOMINAL HERNIAS
Paraduodenal Hernias
Right Paraduodenal Hernia
In right paraduodenal hernia (Fig. 10-34, Fig. 10-35A, sites 1, 3, 4, and 5), the sac lies behind the superior mesenteric artery or the ileocolic artery at the
base of the mesentery (mesentericoparietal fossa of Waldeyer) (Fig. 10-35B). The mouth of the sac opens to the left; the sac is directed to the right in
the retroperitoneal space behind the right or the transverse mesocolon.
Fig. 10-34.
5/23/2014 Print: Chapter 10. Peritoneum, Omenta, and Internal Hernias
http://web.uni-plovdiv.bg/stu1104541018/docs/res/skandalakis' %20surgical%20anatomy%20-%202004/Chapter%2010_%20Peritoneum,%20Omenta,%20and% 39/62
5/23/2014 Print: Chapter 10. Peritoneum, Omenta, and Internal Hernias
http://web.uni-plovdiv.bg/stu1104541018/docs/res/skandalakis' %20surgical%20anatomy%20-%202004/Chapter%2010_%20Peritoneum,%20Omenta,%20and% 40/62
Paraduodenal hernia. A, Right. B, Left. (Modified from Skandalakis LJ, Gadacz TR, Mansberger AR Jr, Mitchell WE Jr, Colborn GL, Skandalakis JE. Modern Hernia
Repair: The Embryological and Anatomical Basis of Surgery. New York: Parthenon, 1996; with permission.)
Fig. 10-35.
Paraduodenal hernias. A, Five most constant sites of paraduodenal hernias (jejunum has been turned to right): 1, 3, 4, 5 are right paraduodenal hernias; 2 is a
left paraduodenal hernia. B, Right paraduodenal hernia into (mesentericoparietal) fossa of Waldeyer (site 5 in A). (A, Modified from Sims WG, Skandalakis JE, Gray
SW. Right paraduodenal hernia into the fossa of Waldeyer. J Med Assoc Ga 60:105, 1971; with permission. B, Modified from Skandalakis JE, Gray SW, Akin JT Jr.
Surgical anatomy of hernial rings. Surg Clin North Am 54:1227, 1974; with permission.)
5/23/2014 Print: Chapter 10. Peritoneum, Omenta, and Internal Hernias
http://web.uni-plovdiv.bg/stu1104541018/docs/res/skandalakis' %20surgical%20anatomy%20-%202004/Chapter%2010_%20Peritoneum,%20Omenta,%20and% 41/62
The ring is formed superiorly by the duodenum, anteriorly by the superior mesenteric or ileocolic artery, and posteriorly by the vertebrae. Incision should
be made in the lower part of the ring to avoid vascular injury.
Left Paraduodenal Hernia
The mouth of a left paraduodenal hernia usually lies behind the inferior mesenteric vein and the left colic artery at the duodenojejunal flexure (Fig. 10-34B,
Fig. 10-35A, site 2). The mouth opens to the right; the sac is directed to the left in the retroperitoneal space behind the left mesocolon. The boundaries
of the sac are:
Superior: duodenojejunal flexure, pancreas, renal vessels
Anterior: inferior mesenteric vein, left colic artery
Lateral: aorta (on right), left kidney (on left)
A downward incision of the ring will avoid injury to the inferior mesenteric vein.
Finck et al.
62
used laparoscopy to diagnose and treat a congenital left paraduodenal hernia.
Transomental Hernia
The ring of the transomental hernia is formed of omentum (Fig. 10-36). A blood vessel usually forms one margin of the defect. Partial or total
omentectomy is the procedure of choice.
Fig. 10-36.
Transomental hernia through defect in greater omentum. (Modified from Skandalakis JE, Gray SW, Akin JT Jr. Surgical anatomy of hernial rings. Surg Clin North Am
54:1227, 1974; with permission.)
Transmesenteric Hernia
Transmesenteric hernias may occur through rents in the mesentery, the transverse mesocolon, or the sigmoid mesocolon (Fig. 10-37). A branch of the
superior or inferior mesenteric artery forms one or more of the edges of the defect. Most defects of the mesentery lie between the ileocolic trunk and the
last ileal branch of the superior mesenteric artery and vein. In the transverse mesocolon, most defects lie between the middle and left colic vessels.
63
Traumatic transmesenteric hernia may present with the clinical picture of strangulated ileus.
64
Fig. 10-37.
5/23/2014 Print: Chapter 10. Peritoneum, Omenta, and Internal Hernias
http://web.uni-plovdiv.bg/stu1104541018/docs/res/skandalakis' %20surgical%20anatomy%20-%202004/Chapter%2010_%20Peritoneum,%20Omenta,%20and% 42/62
Transmesenteric hernia. Ileal loop through defect in sigmoid mesocolon. (Modified from Skandalakis JE, Gray SW, Akin JT Jr. Surgical anatomy of hernial rings. Surg
Clin North Am 54:1227, 1974; with permission.)
Bircher and Stuart
65
have distinguished three types of herniation at the sigmoid mesocolon: intersigmoid at the intersigmoid fossa, transversosigmoid
through a defect in the mesocolon, and intrasigmoid in the left leaf only with the sac lying within the mesocolon.
Small mesenteric holes created during abdominal operations should be closed. If this is not practical, they should be widely opened to prevent
strangulation of intestinal loops. Injury to the blood supply of the intestine should be avoided.
Hernia Through the Epiploic Foramen of Winslow
The boundaries of the epiploic foramen (Fig. 10-38A) are:
Superior: caudate process of liver, inferior leaf of coronary ligament
Posterior: inferior vena cava
Inferior: first part of duodenum, hepatic artery
Anterior: hepatoduodenal ligament enclosing hepatic artery, portal vein, common bile duct
Fig. 10-38.
5/23/2014 Print: Chapter 10. Peritoneum, Omenta, and Internal Hernias
http://web.uni-plovdiv.bg/stu1104541018/docs/res/skandalakis' %20surgical%20anatomy%20-%202004/Chapter%2010_%20Peritoneum,%20Omenta,%20and% 43/62
Hernia through epiploic foramen of Winslow. A, Structures surrounding foramen of Winslow. B, Herniation into lesser sac. (Modified from Skandalakis JE, Gray SW,
Akin JT Jr. Surgical anatomy of hernial rings. Surg Clin North Am 54:1227, 1974; with permission.)
The cystic duct is present in the free edge of the lesser omentum. Intestinal loops are present in about two-thirds of such hernias (Fig. 10-38B); cecum
and right colon are present in one-third. The transverse colon is occasionally present.
66
Nagayoshi and Nakashima
67
presented a case in which a
retrogastric colon presented topographicoanatomically like a hernia of the foramen of Winslow or a left paraduodenal hernia.
Because there are many structures in the vicinity of the neck of the sac that are subject to injury, the neck must not be incised. The hepatogastric
omentum may be incised for decompression of the proximal loop of the incarcerated intestine.
Read an Editorial Comment
Internal Supravesical Hernia
There is considerable confusion in the classification of internal supravesical hernias. The location of the internal supravesical hernia, as well as the
pathway of the hernial sac is presented in Figures 10-39, 10-40, 10-41, 10-42, 10-43, and 10-44. By definition, they all start in the supravesical fossa,
but their subsequent course varies. The terms prevesical, paravesical, and retrovesical have been used by Keynes,
27
Adler,
68
and others. Burton
69
used
the terms prevesical, supravesical, and paravesical. He excluded the retrovesical hernias. These terms are readily understood, but they are awkward in
combination with the collective term supravesical. We have proposed the following classification of internal supravesical hernias based on whether their
course is in front of, beside, or behind the bladder:
Anterior supravesical hernia
Retropubic supravesical hernia
Invaginating supravesical hernia
Right or left lateral supravesical hernia
Posterior supravesical hernia
Fig. 10-39.
5/23/2014 Print: Chapter 10. Peritoneum, Omenta, and Internal Hernias
http://web.uni-plovdiv.bg/stu1104541018/docs/res/skandalakis' %20surgical%20anatomy%20-%202004/Chapter%2010_%20Peritoneum,%20Omenta,%20and% 44/62
Supravesical hernias. (Modified from Gray SW, Skandalakis JE, McClusky DA. Atlas of Surgical Anatomy for General Surgeons. Baltimore: Williams & Wilkins, 1985;
with permission.)
Fig. 10-40.
Highly diagrammatic section of the body at the level of the acetabulum showing some of the landmarks of the spaces around the bladder. (Inset) 1, location of
sac in anterior internal supravesical hernia. 2, location of sac in lateral internal supravesical hernia. 3, location of sac in posterior internal supravesical hernia.
(Modified from Skandalakis PN, Skandalakis LJ, Gray SW, Skandalakis JE. Supravesical hernia. In: Nyhus LM, Condon RE, eds. Hernia, 4th Ed. Philadelphia: JB
Lippincott, 1995; with permission.)
Fig. 10-41.
5/23/2014 Print: Chapter 10. Peritoneum, Omenta, and Internal Hernias
http://web.uni-plovdiv.bg/stu1104541018/docs/res/skandalakis' %20surgical%20anatomy%20-%202004/Chapter%2010_%20Peritoneum,%20Omenta,%20and% 45/62
Comparison of anterior and posterior internal supravesical hernias. Most are of the anterior type. The posterior hernia is illustrated in a patient who previously
had undergone a hysterectomy. (Modified from Skandalakis JE, Gray WS, Burns WB, Sangmalee U, Sorg JL. Internal and external supravesical hernia. Am Surg
42:142-146, 1976; with permission.)
Fig. 10-42.
5/23/2014 Print: Chapter 10. Peritoneum, Omenta, and Internal Hernias
http://web.uni-plovdiv.bg/stu1104541018/docs/res/skandalakis' %20surgical%20anatomy%20-%202004/Chapter%2010_%20Peritoneum,%20Omenta,%20and% 46/62
Invaginating type of anterior internal supravesical hernia. (Modified from Skandalakis PN, Skandalakis LJ, Gray SW, Skandalakis JE. Supravesical hernia. In: Nyhus
LM, Condon RE, eds. Hernia, 4th Ed. Philadelphia: JB Lippincott, 1995; with permission.)
Fig. 10-43.
Three possible pathways of posterior internal supravesical hernias in men. 1, path of true retrovesical hernia. 2, path of retrovesical hernia. 3, path of hernia
through rectovesical pouch. (Modified from Skandalakis PN, Skandalakis LJ, Gray SW, Skandalakis JE. Supravesical hernia. In: Nyhus LM, Condon RE, eds. Hernia,
4th Ed. Philadelphia: JB Lippincott, 1995; with permission.)
Fig. 10-44.
5/23/2014 Print: Chapter 10. Peritoneum, Omenta, and Internal Hernias
http://web.uni-plovdiv.bg/stu1104541018/docs/res/skandalakis' %20surgical%20anatomy%20-%202004/Chapter%2010_%20Peritoneum,%20Omenta,%20and% 47/62
Two possible pathways of posterior internal supravesical hernias in women. 1, path of true rectovesical hernia. 2, path of hernia through the vesicovaginal pouch.
(Modified from Skandalakis PN, Skandalakis LJ, Gray SW, Skandalakis JE. Supravesical hernia. In: Nyhus LM, Condon RE, eds. Hernia, 4th Ed. Philadelphia: JB
Lippincott, 1995; with permission.)
The invaginating and posterior supravesical hernias are extremely rare.
The anterior retropubic and the lateral hernias pass into the retropubic space of Retzius behind the pubis and in front of the bladder. The invaginating
type pushes the anterior bladder wall in, rather than descending behind the pubis. This type has been called intravesical, but this term is misleading,
because the hernia does not enter the bladder.
The posterior hernias pass into the retrovesical space between the bladder and the rectum in men, or between the bladder and the uterus in women.
They form a definite, but small group of supravesical hernias.
In practice, only well-developed anterior and lateral hernias, accurately described by the surgeon, can be classified. A hernia can be reduced and the sac
ligated without examination of the pathway the sac has taken. In many cases, the sac is small and the hernia has not descended completely. Anterior
retropubic and lateral supravesical hernias are especially difficult to differentiate in the early stages of their development. Attempts at precise
classification of many cases in the literature are futile.
Knowledge of the surgical anatomy of the supravesical fossa and the spaces around the bladder is essential to a clear understanding of these hernias.
Paracecal Hernias
Estrada
71
described the following six fossae related to the cecum:
Superior ileocecal fossa
Inferior ileocecal fossa
Paracolic fossa
Retrocecal or retrocolic fossa
Hartmann's fossa
Iliaco-subfascialis
We will describe only the first three. The most important boundary of the superior ileocecal fossa is the presence of the ileocolic or ileocecal fold (see Fig.
10-11), which is formed by a semilunar elevation of the ileocolic mesentery containing the anterior branch of the ileocolic artery and which is located
anteriorly. The hernial sac travels under the right mesocolon or under the descending colon.
5/23/2014 Print: Chapter 10. Peritoneum, Omenta, and Internal Hernias
http://web.uni-plovdiv.bg/stu1104541018/docs/res/skandalakis' %20surgical%20anatomy%20-%202004/Chapter%2010_%20Peritoneum,%20Omenta,%20and% 48/62
anteriorly. The hernial sac travels under the right mesocolon or under the descending colon.
The inferior ileocecal fossa has an anterior prominent ileoappendicular fold which occasionally contains the ileoappendicular artery. The hernial sac may be
found under the cecum.
The paracolic fossa is located at the right gutter due to nonfusion of the lateral and posterior wall of the ascending colon. The sac travels under the
proximal ascending colon. We have seen one case where a loop of terminal ileum was found within the fossa.
Superior and inferior ileocecal hernias (see Fig. 10-11), which are rare, are formed by the same developmental process as are paraduodenal hernias. Their
repair is similar: reduction of the herniated loop and either closure or enlargement of the ring to prevent recurrence. Avoid the right ileocolic and right colic
arteries when incising the ring. Aspiration of the proximal loop should be considered.
Hernia Through the Broad Ligament
This triangular mesentery of the uterus, tubes, and ovaries is extended from each lateral uterine side to the lateral pelvic wall. Medially, the broad
ligament envelops the uterus. The upper free part is related to the tubes (mesosalpinx) and ovaries (mesovarium), and the lower fixed part is attached to
the levator ani muscle through a special formation, the cardinal ligament. The broad ligament has thin vascular areas (defects) through which a viscus
may pass (Fig. 10-45). A bowel loop can be inserted and incarcerated from either side of this ligament. Like other mesenteric defects, the cause of this
rare hernia is unknown.
Fig. 10-45.
Repair of hernia through the broad ligament. (Modified from Skandalakis LJ, Gadacz TR, Mansberger AR Jr, Mitchell WE Jr, Colborn GL, Skandalakis JE. Modern
Hernia Repair: The Embryological and Anatomical Basis of Surgery. New York: Parthenon, 1996; with permission.)
Repair is by incising the ring carefully in an avascular area. Then the loop should be reduced and the defect closed, or the ligament should be removed.
Hernia Through the Falciform Ligament
5/23/2014 Print: Chapter 10. Peritoneum, Omenta, and Internal Hernias
http://web.uni-plovdiv.bg/stu1104541018/docs/res/skandalakis' %20surgical%20anatomy%20-%202004/Chapter%2010_%20Peritoneum,%20Omenta,%20and% 49/62
The falciform ligament begins at the umbilicus and passes obliquely to the superior surface of the left lobe of the liver, where it forms an excellent
landmark that separates the lateral and medial segments of the left lobe. The free edge of the falciform ligament contains the cordlike round ligament
(ligamentum teres) of the liver. This is the remnant of the left umbilical vein. The right umbilical vein disappears early in development; the left vein carries
placental blood to the fetus and closes at birth. This vascular remnant is often patent for much of its length.
36
Its intrahepatic portion becomes the
ligamentum venosum, which connects the left branch of the portal vein with the left hepatic vein. The falciform ligament is thus the mesentery of the
umbilical vein.
A possible defect in the mesentery of the falciform ligament may produce a herniation (Fig. 10-46). Reduction of the hernia is by proximal and distal
ligation, then incision of the falciform and round ligaments.
Fig. 10-46.
Repair of hernia through the falciform ligament. (Modified from Skandalakis LJ, Gadacz TR, Mansberger AR Jr, Mitchell WE Jr, Colborn GL, Skandalakis JE. Modern
Hernia Repair: The Embryological and Anatomical Basis of Surgery. New York: Parthenon, 1996; with permission.)
Retroanastomotic Hernias
Retroanastomotic hernias are, of course, iatrogenic hernias that may occur postoperatively.
72
Hernia after Retrocolic Gastrojejunostomy
The boundaries of the ring (Fig. 10-47A) are:
Anterior: gastrojejunostomy, efferent or afferent intestinal loop
Posterior: parietal peritoneum
Superior: transverse mesocolon, posterior wall of gastric remnant
Inferior: suspensory ligament of Treitz, duodenojejunal fold
Fig. 10-47.
5/23/2014 Print: Chapter 10. Peritoneum, Omenta, and Internal Hernias
http://web.uni-plovdiv.bg/stu1104541018/docs/res/skandalakis' %20surgical%20anatomy%20-%202004/Chapter%2010_%20Peritoneum,%20Omenta,%20and% 50/62
5/23/2014 Print: Chapter 10. Peritoneum, Omenta, and Internal Hernias
http://web.uni-plovdiv.bg/stu1104541018/docs/res/skandalakis' %20surgical%20anatomy%20-%202004/Chapter%2010_%20Peritoneum,%20Omenta,%20and% 51/62
Repair of retroanastomotic hernia. A, Gastrojejunostomy has been constructed behind the transverse colon (retrocolic). B, Gastrojejunostomy has been
constructed in front of the transverse colon (antecolic). (Modified from Skandalakis LJ, Gadacz TR, Mansberger AR Jr, Mitchell WE Jr, Colborn GL, Skandalakis JE.
Modern Hernia Repair: The Embryological and Anatomical Basis of Surgery. New York: Parthenon, 1996; with permission).
The ring should not be incised. Reduction of the hernia may be accomplished by enterostomy. This should be followed by closure of the ring.
Hernia after Antecolic Gastrojejunostomy
Where the afferent intestinal loop attaches to the greater curvature of the stomach, the hernial ring is formed as follows (Fig. 10-45B):
Anterior: gastrojejunostomy, afferent jejunal loop
Posterior: omentum, mesocolon
Superior: transverse colon, mesocolon
Inferior: muscle of Treitz, duodenojejunal peritoneal fold
No incision should be made, and the ring should be closed after reduction of the herniated loop.
SURGERY OF THE PERITONEUM AND OMENTA
Abdominal Paracentesis
The site for paracentesis can be determined after a sonogram or a CAT scan. The usual sites (Fig. 10-48) are in each of the four quadrants, the right or
left flank, or in the midline below the umbilicus.
Fig. 10-48.
5/23/2014 Print: Chapter 10. Peritoneum, Omenta, and Internal Hernias
http://web.uni-plovdiv.bg/stu1104541018/docs/res/skandalakis' %20surgical%20anatomy%20-%202004/Chapter%2010_%20Peritoneum,%20Omenta,%20and% 52/62
Sites of paracentesis. A, B, C, D, "Four quadrant" paracentesis. E, F, Flank paracentesis. G, Infraumbilical paracentesis. (Modified from Skandalakis JE, Gray SW,
Akin JT Jr. Surgical anatomy of hernial rings. Surg Clin North Am 54:1227, 1974; with permission.)
Paracentesis must be performed under absolutely sterile conditions to avoid peritonitis. Some surgeons give antibiotics for this purpose. During
paracentesis, the needle can puncture the intestine. This is not usually dangerous, because the needle hole will automatically seal itself.
Peritoneal lavage is optional and perhaps should be carried out as an additional procedure. Moore et al.
73
reported that the rate of complications and
accuracy of diagnosis of closed peritoneal lavage was similar for patients with and without previous abdominal surgery.
The results of paracentesis require careful evaluation. A negative tap gives no information. Unclotted blood signals intraperitoneal bleeding. Clotting blood
suggests aspiration from a blood vessel in the abdomen or the abdominal wall; this is not uncommon in obese patients.
Currently, ultrasonography-guided paracentesis is the procedure of choice for the detection and evaluation of intraperitoneal collections secondary to
trauma, inflammatory process, etc. Rodriguez et al.,
74
Ross et al.,
75
and Goletti et al.
76
reported excellent results with this procedure. Multiple-view
sonography is used to identify free intraperitoneal fluid associated with hepatic and splenic injury.
77
Ross and colleagues
75
advocated sonographically-
guided paracentesis as an effective procedure for short-term relief of malignant ascites. Jennings et al.
78
recommended paracentesis through the umbilical
ring in ectopic pregnancy.
Several contraindications may be present. Avoid paracentesis:
With abdominal distention
In an abdomen with multiple scars
Of cystic abdominal masses
In the upper midline, because the falciform ligament may be punctured.
Collection of intraperitoneal fluid secondary to intraperitoneal spread of intra-abdominal cancer is termed malignant ascites if neoplastic cells are identified.
Malignant ascites is treated by extensive surgical debulking (cytoreductive surgery) followed by local or systemic chemotherapy, hyperthermia,
phototherapy, etc.
We quote from Marincola and Schwartzentruber
79
:
[M]alignant ascites represents in most instances a debilitating symptom of end-stage cancer. Purely palliative measures on one extreme and
aggressive therapeutic interventions on the other represent the wide range of treatment options. Reported survival of patients treated with
curative intent, in general, is better than that of patients receiving palliative procedures, but clearly reflects differences in patient selection
(differences in stage, histology, extent of disease, and so forth). No randomized studies have been performed to evaluate the treatment of
malignant ascites. Several questions remain unanswered, such as the value of a peritoneovenous shunt insertion compared with medical
management or intermittent drainage; the role of external versus internal drains; and the effectiveness of locoregional curative efforts. Scant
information is available regarding the effectiveness of intracavitary versus systemic therapy.
Culdocentesis
In culdocentesis, the needle is inserted at the posterior fornix into the cul-de-sac (rectovaginal pouch of Douglas). Culdocentesis should not be performed
in women who have undergone vaginal or abdominal hysterectomy or low anterior rectosigmoid resection. It should not be attempted if there is distention
of the intestines. Other contraindications are the same as those for abdominal paracentesis.
Falfoul et al.
80
and Tariq and Korejo
81
discussed the use of culdocentesis for diagnosis of ectopic pregnancy in "third-world" medical settings. Glezerman
5/23/2014 Print: Chapter 10. Peritoneum, Omenta, and Internal Hernias
http://web.uni-plovdiv.bg/stu1104541018/docs/res/skandalakis' %20surgical%20anatomy%20-%202004/Chapter%2010_%20Peritoneum,%20Omenta,%20and% 53/62
and colleagues
82
found an unacceptably high rate of false negatives. The interested student will find excellent information in Vande Krol and Abbott's
83
1992 article, "The Current Role of Culdocentesis."
Exploration of the Abdomen
To determine the limits of known disease and to discover unknown or suspected disease, it may be necessary to explore the patient's abdomen. Not every
patient with an abdominal complaint can be or should be completely explored. The incision may be too small (as for appendicitis), there may be extensive
adhesions, the patient may be too ill, or the surgeon may encounter peritoneal pus or fluid collections that contraindicate further exploration until the
affected areas have been drained or otherwise rendered sterile. Common sense will dictate when to explore and when not to explore.
The diagnosis and treatment of peritonitis, a well-known indication for surgery, is controversial. Chen et al.
84
found ultrasonography a more sensitive
technique than clinical judgment in diagnosing peritonitis, especially when the clinical cause was unclear.
Seiler et al.
85
advocated a conservative surgical treatment for diffuse peritonitis which included early intervention, source control, and extensive
intraoperative lavage to reduce the reoperation rate.
Bosscha and colleagues
86
gave measured support for open management of peritonitis:
Despite open management of the abdomen and planned re-operation, mortality of severe bacterial peritonitis still continues to be too high, and both
short and long-term morbidity are appreciable. The value of open management of the abdomen and planned re-operations rests only on the clinical
observation that other conventional surgical treatments of severe bacterial peritonitis often fail.
The surgeon's approach to exploration of the abdomen is an individual matter. All that is necessary is some system for evaluating normal and pathologic
anatomy. Once the surgeon has established a satisfactory pattern of exploration, it should be followed rigidly.
One rule should always be observed: the organ with the primary lesion for which the abdomen has been opened should be left to the end, so that the
surgeon's interest in it will not detract from the attention given to the other organs.
Bassett
87
wrote an excellent small book on exploration of the abdomen and the maneuvers necessary to carry it out. He suggested three sequences that
may be used: regional, systemic, and circular. The following sequence is drawn from Bassett's regional route:
1. Inspect the abdomen. Note any obvious pathology that (a) may need immediate treatment (i.e., a ruptured spleen) or (b) may contraindicate
further exploration (i.e., a perforated colonic diverticular abscess).
2. If the clinical status of the patient warrants further exploration, examine the transverse colon. Pull the colon downward. Examine the supracolic
region from right to left. Include the:
right kidney and adrenal gland
epiploic foramen of Winslow and common bile duct
gallbladder
right lobe of liver
first and second portions of duodenum
pancreas
left lobe segments of liver
pylorus and lesser curvature of stomach
fundus of stomach and abdominal esophagus
greater curvature of stomach
spleen
left adrenal area
Pull the transverse colon upward. Examine the infracolic region from right to left. Include the:
cecum and appendix
right colon and hepatic flexure
right retroperitoneal space and lower pole of right kidney
third and fourth portions of duodenum and superior mesenteric artery
small intestine and mesentery
tail of pancreas
left kidney
aorta and left retroperitoneal space
left colon and splenic flexure
5/23/2014 Print: Chapter 10. Peritoneum, Omenta, and Internal Hernias
http://web.uni-plovdiv.bg/stu1104541018/docs/res/skandalakis' %20surgical%20anatomy%20-%202004/Chapter%2010_%20Peritoneum,%20Omenta,%20and% 54/62
sigmoid colon
3. Examine the pelvic cavity. Include the:
sigmoid colon
rectum and uterosacral ligaments
uterus, tubes, and ovaries
pelvic wall
inguinal and femoral regions
iliac vessels
4. Do not forget to examine the greater omentum. Torsion of the omentum will be obvious.
88
Idiopathic infarction, especially at the right lower end,
is obvious.
52
If this or any other system is used habitually, it will become automatic. As Bassett
87
said: "The goal is to achieve gentleness, accuracy, thoroughness,
and speed."
Multiple organ dysfunction syndrome (MODS) calls into question the value of relaparotomy for persisting abdominal sepsis. Koperna and Schulz
89
assert
that "...aggressive surgical treatment has reached its limit in patients whose source of infection could not be controlled at the initial operation. To improve
overall survival the decision to perform a relaparotomy on demand after an initially successful eradication of the source of infection must be made within
48 hr, at least before MODS emerges."
Laparoscopic Peritoneal Exploration
The senior author of this chapter remembers the so-called diagnostic laparotomy as an approach to the secrets of the Pandora's box, the peritoneal
cavity. He wonders how many times a peritoneal mesothelioma was disseminated, which can, of course, happen also during laparoscopic procedures.
Currently laparoscopy is used as a diagnostic procedure for peritoneal exploration. Muensterer et al.
90
reported that laparoscopy with biopsy of peritoneal
nodules is a valuable method by which a histologic diagnosis is established. They warned, though, that port sites must be excised to prevent dissemination
of intraabdominal malignancy. Laparoscopic peritoneal exploration continues to evolve and to be very helpful by avoiding laparotomy. Estrada Saiz et al.
91
stated that laparoscopy is also useful in diagnosing primary peritoneal mesothelioma as a cause of ascites.
Ditmars and Bongard
92
concluded that the use of diagnostic laparoscopy is very valuable for triage of penetrating trauma; it helps the surgeon decide
whether to explore or use conservative treatment. A similar conclusion was expressed by Fernando et al.
93
The role of laparoscopy in trauma is evolving, according to Poole et al.,
94
and further research into its diagnostic role and therapeutic applications is
clearly needed.
Maffei Faccioli et al.
95
stated that laparoscopy and peritoneal wash represent useful tools in the staging of patients with carcinoma of the pancreas.
Diagnosis of endometriosis is possible with laparoscopy. However, Nezhat et al.
96
cautioned that this procedure should be augmented with techniques
utilizing careful palpation and visualization.
A study by al Quorain et al.
97
found that laparoscopy saves unnecessary laparotomies, particularly in cases of tuberculous peritonitis, chronic liver
disease, and hepatocellular carcinoma.
Faranda et al.
98
advocated laparoscopic treatment of generalized peritonitis due to perforated sigmoid diverticula for its lower morbidity, shorter hospital
stay, and avoidance of colostomy.
For early and prompt diagnosis and treatment of tuberculous ascites, Ahmad and Ahmed
99
advise the following diagnostic modalities:
1. Mini laparoscopy
2. Sampling of the ascitic fluid for adenosine deaminase activity and polymerase chain reaction
3. Early antituberculin treatment if such a diagnosis is suspected.
Observations
Most of the surgical applications of the peritoneum and its derivatives will be described with the organs involved. However, repetition in the study of
anatomy is a common and unavoidable phenomenon (and also helpful!).
In 1932 Livingston
1
very wisely promulgated the following thoughts. Unfortunately, they have been forgotten in an era when embryology and anatomy
play a small role in the curriculum of medical students and the training of residents:
Obviously a surgeon possessing clear insight into the modus operandi through which final arrangements in the abdomen are produced is in a position
to know how he may safely proceed while operating (in mobilizing portions of bowel; in avoiding important vessels; in relieving intestinal obstruction;
in reducing internal hernias; in segregating segments of intestine or creating short-circuits in the alimentary canal); he is qualified to recognize
congenital arrests in development when such are encountered. He can differentiate bands and peritoneal folds which represent normal variations,
5/23/2014 Print: Chapter 10. Peritoneum, Omenta, and Internal Hernias
http://web.uni-plovdiv.bg/stu1104541018/docs/res/skandalakis' %20surgical%20anatomy%20-%202004/Chapter%2010_%20Peritoneum,%20Omenta,%20and% 55/62
congenital arrests in development when such are encountered. He can differentiate bands and peritoneal folds which represent normal variations,
from those which are abnormal formations; and he can judge with reasonable accuracy when intra-abdominal conditions are, and when they are
not, consistent with good functional activity. And the diagnostician is aided no less than the operator by a thorough understanding of
developmental details.
Adhesions
All adhesions (congenital, postoperative, secondary to radiation) should be treated with care. If they are transparent, they should be incised carefully to
protect the serosa of the viscus. If they are thick, they should be cut between two clamps, with both parts ligated.
Special attention should be paid to adhesions secondary to radiation enteritis. Morgenstern et al.
100
advised lysis only when absolutely necessary since
minute openings into the intestine can be produced, leading to perforation or fistulae. Performing a bypass or a resection is a wise decision.
Shiraishi et al.
101
advised surgical resection of the part of the intestine involved with radiation enterocolitis; this reduces bleeding and improves survival.
Fossae
The several fossae may be the sites of partial or complete intestinal obstruction secondary to internal herniation. Their anatomy is peculiar. The surgeon
should remember anatomic entities which are closely related to these fossae, such as the left ureter at the intersigmoid fossa, the inferior mesenteric vein
at the paraduodenal fossae, the hepatic triad at the foramen of Winslow, the right and left epiploic vessels, the right ileocolic and right colic arteries, and
the superior mesenteric artery at the mesentericoparietal fossa of Waldeyer.
Folds
The peritoneal folds suspend the various intraperitoneal entities; at the same time, they convey blood vessels, lymphatics, and nerves to the related
organs. The surgeon should be familiar with these folds, which are NOT adhesions.
Because of anatomic arrangements, pelvic fluid may reach the right diaphragm (Fitz-Hugh and Curtis syndrome, gonococcal perihepatitis), presenting the
peculiar clinical picture of acute cholecystitis.
Remember
There is no such thing as a right phrenicocolic ligament.
Omentum
The omentum may protect sutured anastomotic intestinal lines. It may occasionally close perforations of the gastrointestinal tract. At times, it may be
fixed with other organs to idiopathic adhesions or to adhesions secondary to well known processes.
To general surgeons, the greater omentum is very useful for wrapping anastomoses, covering perforated duodenal ulcers, and filling large cavities
secondary to evacuation of hepatic or splenic cysts.
Kuroyama et al.
102
advised early single-stage omental transposition to treat sternomediastinitis. Ovnat et al.
103
used omentopexy to treat recurring
lymphoceles following renal transplantation.
After low anterior resection with total mesorectal excision, Averbach et al.
104
advised pelvic omentoplasty.
In 1906, Rutherford Morison
49
described angiogenesis in the greater omentum with the formation of new blood vessels. Situations in which omental
angiogenesis may occur are shown in a table by Williams
61
(Table 10-5).
Table 10-5. Omental Angiogenesis
Intraabdominal adhesions
Surgical anastomoses
Biological free grafts (skin, bone, urothelium)
Microporous prostheses (trachea)
Occlusive arterial disease (extremities, CNS)
Transperitoneal tumor metastasis
Source: Williams R. Angiogenesis and the greater omentum. In: Goldsmith HS. Omentum: Proceedings of the First International Conference on the Omentum Held in
Research Triangle Park, North Carolina, October 28-31, 1988. New York: Springer-Verlag, 1990, pp 45-62.
Laparoscopic treatment of idiopathic segmental infarction of the greater omentum was presented by Goti et al.
105
Segmental infarction may be caused by torsion of the omentum.
106
A case of omental torsion has been reported in pregnancy.
107
Al-Husaini et al.
108
advised, "A high index of suspicion for primary omental torsion is important when a small right lower abdominal incision, which has been made for acute
appendicitis, reveals a normal appendix especially in the presence of free intraperitoneal serosanguinous fluid."
The student with an interest in the omentum should read the excellent books of Liebermann-Meffert and White
4
and Goldsmith.
109
Peritoneal Closure
It is well known that the peritoneum has the capability to heal very rapidly, restoring large defects within hours or days. Differentiated stem cells located
within the subperitoneal tissues may be responsible for rapid peritoneal healing. Participation of mesothelial cells in transperitoneal migration and ingrowth
may also play a role.
Adhesions are formed by a delay in peritoneal healing.
5/23/2014 Print: Chapter 10. Peritoneum, Omenta, and Internal Hernias
http://web.uni-plovdiv.bg/stu1104541018/docs/res/skandalakis' %20surgical%20anatomy%20-%202004/Chapter%2010_%20Peritoneum,%20Omenta,%20and% 56/62
Mazier et al.
110
reported no significant difference in outcome between the primary closure of the pelvic peritoneum and the lack of peritoneal closure.
Thome Saint Paul and coworkers
111
asserted that fewer postoperative complications (lymphoceles, fever, etc) developed with visceral
nonperitonealization. Spernol et al.
112
strongly advocated that the pelvic peritoneum be left open. A similar recommendation was made by Nagele and
coworkers.
113
Than et al.
114
suggested a similar course following abdominal hysterectomy, in particular, Wertheim-Meigs operations. However, Dimpfl and
colleagues
115
reported that their own results with 343 women did not give sufficient proof that nonperitoneal closure significantly reduces the incidence of
symptomatic lymphocysts.
When treating rectal carcinoma, Chen et al.
116
performed pelvic peritoneal reconstitution to prevent postoperative radiation enteritis. They used the
posterior rectus sheath and the peritoneum to partition the abdominal cavity at the umbilical and sacral promontory levels.
Read an Editorial Comment
Each surgeon should decide how to manage the pelvic floor. The choice of open or closed method should be based on the procedure with which the
surgeon is most comfortable. With peritoneal contamination, the open method is essential. Neither the open method nor the closed method is a "myth": in
the absence of contraindications, both reflect sound surgical judgment.
ANATOMIC COMPLICATIONS INVOLVING THE PERITONEUM AND OMENTA
The complications of procedures within the peritoneal cavity are shown in Table 10-6. These are complications of procedures on the gastrointestinal tract
and the three unpaired organs: the liver, spleen, and pancreas. The specific complications of surgery of each of these organs have been discussed in
separate chapters.
Table 10-6. Summary of Anatomic Complications of Some Peritoneal Procedures
Procedure Vascular Injury Nerve Injury Organ Injury Inadequate
Procedure
Procedures within the
peritoneum
Numerous injuries possible None Discussed with specific organs Peritonitis
Hemoperitoneum
Exploration of the
abdomen
Hemorrhage from cutting adhesions None Viscera or solid organs Incision too small
Failure to recognize
pathology
Paracentesis and
culdocentesis
Hematoma from epigastric, omental,
mesenteric or pelvic vessels
9th to 12th
spinal nerves
Puncture of intestines, gallbladder, urinary bladder,
liver, spleen or ovarian cyst
None
Source: Skandalakis JE, Gray SW, Rowe JS Jr. Anatomical Complications in General Surgery. New York: McGraw-Hill, 1983; with permission.
The single unifying complication of all these procedures is peritonitis, the inflammation of the peritoneal cavity. A good (but not ideal) set of classifications
of peritonitis was reported by Wittmann
59
(Tables 10-7, 10-8). Inflammation may be sterile from the leakage of bile, pancreatic juice, or blood into the
cavity, or it may be septic from contamination of the peritoneum by aerobic or anaerobic bacteria.
Table 10-7. Classification According to Etiology
I. Primary peritonitis C. Posttraumatic peritonitis
A. Spontaneous peritonitis in children 1. Peritonitis after blunt abdominal trauma
B. Spontaneous peritonitis in adults 2. Peritonitis after penetrating abdominal trauma
C. Peritonitis in patients with CAPD 3. Other forms
D. Tuberculous peritonitis III. Tertiary peritonitis
E. Other forms A. Peritonitis without pathogens
II. Secondary peritonitis B. Peritonitis with fungi
A. Acute perforation peritonitis (acute suppurative peritonitis) C. Peritonitis with low-grade pathogenic bacteria
1. GI tract perforation IV. Intra-abdominal abscess
2. Bowel wall necrosis (intestinal ischemia) A. Associated with primary peritonitis
3. Pelviperitonitis B. Associated with secondary peritonitis
4. Other forms C. Associated with tertiary peritonitis
B. Postoperative peritonitis
1. Leak of an anastomosis
2. Leak of a suture line
3. Stump insufficiency
4. Other iatrogenic leaks
Source: Wittmann DH. Intra-abdominal Infections. New York: Marcel Dekker, 1991.
Table 10-8. Classification According to the Spread of Infection
1. Diffuse peritonitis
2. Localized peritonitis
Intra-abdominal abscess
5/23/2014 Print: Chapter 10. Peritoneum, Omenta, and Internal Hernias
http://web.uni-plovdiv.bg/stu1104541018/docs/res/skandalakis' %20surgical%20anatomy%20-%202004/Chapter%2010_%20Peritoneum,%20Omenta,%20and% 57/62
Intra-abdominal abscess
Interloop abscess
Douglas abscess
Subphrenic abscess
Retrocolic abscess
Pancreas abscess
Other abscesses
Source: Wittmann DH. Intra-abdominal Infections. New York: Marcel Dekker, 1991.
Peritonitis is a possible sequel to any intraabdominal procedure clean, contaminated, or already infected. According to Wittmann,
59
perforation peritonitis
is the most common form of acute intraabdominal infection. Peritonitis is also a major complication of peritoneal dialysis.
The following are necessary for prevention of peritonitis secondary to peritoneal dialysis:
117
Sterile connections under sterile conditions without deviation from appropriate procedural protocols
Careful patient training
Antibiotic prophylaxis
Cautious assessment of high-risk patients (patients with skin disease, patients who are blind and lack assistance, patients with severe intraabdominal
adhesions)
Adoption of new catheter technology
Adoption of new dialysis solutions/buffering agents
We will not enter the controversy that surrounds prevention of peritonitis by irrigation and drainage as prophylactic measures. A prospective study of over
23,000 surgical wounds in Calgary, Canada, by Cruse and Foord
118
is well worth reading for its analysis of the factors affecting the incidence of
postoperative infection.
Two studies indicate that drainage is unnecessary in uncomplicated cholecystectomy.
119,120
Hunt
121
compared the mortality of patients with residual
peritoneal contamination treated by (1) no peritoneal irrigation, (2) intraoperative irrigation only, and (3) intraoperative and postoperative irrigation. He
found no significant difference in the mortality among the three groups. There were only 44 patients in this study; a larger series might have different
results.
One factor that increases mortality regardless of type of treatment is the patient's age. Mortality doubles, or more than doubles, with age.
118,121,122
Good anastomosis is paramount. A hematoma welcomes infection. Should injury or perforation of a viscus occur, isolate the area at once and correct the
situation.
Finally, all procedures demand a knowledge of anatomy. Peritonitis with toxemia and sepsis can be avoided by understanding the triad of strategy,
technique, and anatomy (Table 10-9).
Table 10-9. the Prevention of Peritonitis
Strategy
Prior to surgery Antibiotics, hyperalimentation, cleansing enemas, respiratory toilet
At operation Irrigations, antibiotics, closed suction drainage, delayed skin closure
After surgery Antibiotics, hyperalimentation, respiratory toilet
Technique Good surgery without "breaks"
Surgical anatomy Understanding of the normal and pathological anatomy of the area
Source: Skandalakis JE, Gray SW, Rowe JS Jr. Anatomical Complications in General Surgery. New York: McGraw-Hill, 1983; with permission.
Recurrent or persistent intraperitoneal infections can occur in spite of good treatment of primary or secondary peritonitis. According to Nathens et al.
123
tertiary peritonitis may develop in 74% of patients, and the most common organisms are Enterococcus, Candida, Staphylococcus epidermidis, and
Enterobacter. The same authors stated that tertiary peritonitis is a syndrome that appears to be more a reflection than a cause of adverse outcome.
Complications of Paracentesis and Culdocentesis
Vascular Injury
Bleeding can result from injury to the superior or inferior epigastric vessels of the abdominal wall or from intraabdominal vessels of the omentum,
mesentery, or pelvic region. The result will be a hematoma within the peritoneal cavity or in the abdominal wall, or more grave problems.
Nerve Injury
There may be slight discomfort from injury to branches of the 9th to 12th spinal nerves.
Organ Injury
Puncture of the small or large intestine, gallbladder, or urinary bladder is always possible; the bladder should be emptied to minimize the chance of
puncture. Intestinal punctures seal quickly. The possibility of sepsis and peritonitis is remote, but the danger is always there.
5/23/2014 Print: Chapter 10. Peritoneum, Omenta, and Internal Hernias
http://web.uni-plovdiv.bg/stu1104541018/docs/res/skandalakis' %20surgical%20anatomy%20-%202004/Chapter%2010_%20Peritoneum,%20Omenta,%20and% 58/62
puncture. Intestinal punctures seal quickly. The possibility of sepsis and peritonitis is remote, but the danger is always there.
Injury to the liver during paracentesis is similar to that by liver biopsy. Both bleeding from the spleen and rupture are possible. An ovarian cyst may be
injured. Bleeding or even carcinomatosis may result from a ruptured malignant cyst.
Roberts and Athey
124
presented six occurrences of air in the myometrium, complicating culdocentesis. In 3,656 transvaginal ultrasonographically-guided
retrievals of oocytes, Dicker et al.
125
reported 14 cases with severe, life-threatening abdominal complications.
Complications of Exploration of the Abdomen
Exploration of the abdomen is not without complications of its own. The failure to find or to recognize pathology that later becomes manifest must be
considered an inadequate procedure. The cutting of folds and bands mistakenly thought to be bloodless can result in hemorrhage. Traction on the spleen
occasionally leads to rupture.
One should be aware that the lower pole of the spleen is often joined to the gastrocolic ligament by an accessory ligament referred to by Morgenstern
126
as the "criminal fold." The spleen can be torn by traction upon this ligament.
Complications of Omentoplasty
The use of the omentum in surgery may produce various anatomic complications. Van Garderen et al.
127
presented several complications of pedicled
omentoplasty. These included, among others, necrosis of the omental flap and infarction. Boiskin et al.
128
reported herniation of the transverse colon
following omentoplasty. Massard and colleagues
129
reported two cases of diaphragmatic hernia after omentoplasty for thoracic wall excision. John and
Buchmann
130
used omental flaps for perineal wound healing after rectal excision; in one case, the omentum became partially necrotic.
In the treatment of carcinoma of the rectum, Lechner and Cesnik
131
advised using the omentum to form an artificial diaphragm between the abdominal
cavity and the true pelvis (abdominopelvic omentopexy). By keeping the intestinal loops out of the low pelvis, radiation enteritis may be avoided.
REFERENCES
1. Livingston EM. A Clinical Study of the Abdominal Cavity & Peritoneum. New York: Hoeber, 1932.
2. Swaen A. Recherches sur le dveloppement du foie, du tube digestif, du pritoine et du msentre. J Anat (Paris) 1897;33:32-88, 222-258, 523-585.
3. Broman I. Warum wird die Entwicklung der bursa omentalis in Lehrbchern fort wchrend unrichtig beschrieben? Anat Anz 1938;86:195-204.
4. Liebermann-Meffert D, White H. Development and appearance. In: Liebermann-Meffert D, White H (eds). The Greater Omentum: Anatomy, Physiology,
Pathology, Surgery with a Historical Survey. New York: Springer-Verlag, 1983.
5. Krutsiak VN, Voitiv II. Spatial organization of the lesser peritoneal sac during the early stages of human ontogeny. Arkh Anat Gistol Embriol 1984;87:46-
54. [PubMed: 6525052]
6. Kiuchi M, Kawachi Y, Kimura Y. Sudden infant death due to asplenia syndrome. Am J Forensic Med Pathol 1988;9:102-104. [PubMed: 3381787]
7. Skandalakis JE. [Idiopathic hemorrhagic infarction of the greater omentum]. Surg Rev (Greece) 1954;15:2-7.
8. Spurney RF, McCormack KM. Immature omental teratoma. Arch Pathol Lab Med 1987;3:762-764.
9. Boehner JF. Solid ovarian teratoma with neurological metastases to periaortic lymph nodes and omentum. South Med J 1987;5:649-652.
10. Liebermann-Meffert D, Gloor F. Pathological conditions, specific investigations, and therapy: tissue deposits. In: Liebermann-Meffert D, White H (eds).
The Greater Omentum: Anatomy, Physiology, Pathology, Surgery with a Historical Survey. New York: Springer-Verlag, 1983.
11. Haider R. Congenital pericardio-peritoneal communication with herniation of omentum into the pericardium: a rare cause of cardiomegaly. Br Heart J
1973;35:981-984. [PubMed: 4270239]
12. Hodach RJ. Studies of malformation syndromes in man. XXXVI: the Pfeiffer syndrome, association with kleeblattschadel and multiple visceral anomalies.
Z Kinderheilkd 1975;119:87-103.
13. Zwiren GT, Andrews HG, Ahmann P. Jejunal atresia with agenesis of the dorsal mesentery ("apple-peel small bowel"). J Pediatr Surg 1972;4:414.
14. Weitzman JJ, Vanderhoof RS. Jejunal atresia with agenesis of the dorsal mesentery with "Christmas tree" deformity of the small intestine. Am J Surg
1966;111:443. [PubMed: 5907010]
15. Zerella JZ, Martin LW. Jejunal atresia with absent mesentery and a helical ileum. Surgery 1976;80:550. [PubMed: 824753]
16. Skandalakis LJ, Gadacz TR, Mansberger AR Jr, Mitchell WE Jr, Colborn GL, Skandalakis JE. Modern Hernia Repair: The Embryological and Anatomical
Basis of Surgery. Pearl River NY: Parthenon, 1996.
17. Moynihan BGA. Retro-peritoneal hernia. London: Balliere, 1889.
18. Skandalakis JE, Gray SW, Harlaftis M, Collier HS. Herniation into the fossa of Waldeyer: three cases of right paraduodenal hernia with emphasis on
surgical anatomy. In: Pontidas EJ (ed). In Honour of Thomas Doxiadis. Athens, Greece: Hospital Evangelismis, 1976.
5/23/2014 Print: Chapter 10. Peritoneum, Omenta, and Internal Hernias
http://web.uni-plovdiv.bg/stu1104541018/docs/res/skandalakis' %20surgical%20anatomy%20-%202004/Chapter%2010_%20Peritoneum,%20Omenta,%20and% 59/62
19. Sims WG, Skandalakis JE, Gray SW. Right paraduodenal hernia into the fossa of Waldeyer. J Med Assoc GA 1971;60:105-108.
20. Gray SW, Skandalakis JE. Paraduodenal hernia. Contemp Surg 1978;12:26-39.
21. Sawyer KC. Acute intestinal obstruction. Rocky Mount Med J 1953;50:639-645. [PubMed: 13075876]
22. Laslie M, Durden C, Allen L. Concealed umbilical hernia: Papez's concept of so-called paraduodenal hernia. Anat Rec 1966;155: 145-150. [PubMed:
4960420]
23. Colborn GL, Skandalakis JE. Anatomical commentaries on the space of Bogros. Postgrad Gen Surg 6(1):21-22, 1995.
24. Allen L, Weatherford T. Role of fenestrated basement membrane in lymphatic absorption from the peritoneal cavity. Am J Physiol 1959;197:551.
[PubMed: 13792765]
25. von Recklinghausen FT. Lymphatics and absorption. Arch Pathol Anat Physiol 1863;26:172.
26. Higgins GM, Beaver MG, Lemon WS. Phrenic neurectomy and peritoneal absorption. Am J Anat 1930;45:137.
27. Keynes WM. Supravesical hernia. In: Nyhus LM, Harkins HN (eds). Hernia. Philadelphia: Lippincott, 1964.
28. Williams PL (ed). Gray's Anatomy (38th ed). New York: Churchill Livingstone, 1995.
29. Ochsner A, Graves AM. Subphrenic abscess: an analysis of 3,372 collected and personal cases. Ann Surg 1933;98:961.
30. Mitchell GAG. The spread of acute intraperitoneal effusions. Br J Surg 1940;28:291.
31. Autio V. The spread of intraperitoneal infection. Acta Chir Scand 1964;5:321.
32. Boyd DP. The subphrenic spaces and the emperor's new robes. N Engl J Med 1966;275:911. [PubMed: 5331126]
33. Whalen JP. Radiology of the Abdomen: Anatomic Basis. Philadelphia: Lea & Febiger, 1976.
34. Harley HRS. Subphrenic abscess. In: Maingot R (ed). Abdominal Operations (7th ed). New York: Appleton-Century-Crofts, 1980.
35. Meyers MA. Dynamic Radiology of the Abdomen (4th ed). New York: Springer-Verlag, 1994.
36. Silva YJ. In vivo use of human umbilical vessels and the ductus venosus Arantii. Surg Gynecol Obstet 1979;148:595. [PubMed: 432777]
37. Michels NA. Blood Supply and Anatomy of the Upper Abdominal Organs. Philadelphia: JB Lippincott, 1955.
38. Gray SW, Rowe JS Jr, Skandalakis JE. Surgical anatomy of the gastroesophageal junction. Am Surg 1979;45:575. [PubMed: 507565]
39. Alday ES, Goldsmith HD. Surgical technique for omental lengthening based on arterial anatomy. Surg Gynecol Obstet 1972;135:103. [PubMed:
5032625]
40. Nowak W, Wolfram T, Leonhardt M. [Dorsolateral approach to the left subphrenic area, to the bursa omentalis and to the cauda pancreatitis]. Chirurg
1993;64:495-498. [PubMed: 8359062]
41. Hollinshead WH. Anatomy for Surgeons. New York: Hoeber, 1956.
42. Altemeier WA, Alexander JW. Retroperitoneal abscess. Arch Surg 83:512-524, 1961. [PubMed: 13860719]
43. Mayberry JC, Mullins RJ, Crass RA, Trunkey DD. Prevention of abdominal compartment syndrome by absorbable mesh prosthesis closure. Arch Surg
1997;132:957-962. [PubMed: 9301607]
44. Organ CH, Porter JM. General surgery. JAMA 280(6):495-496, 1998.
45. Rotondo MF, Zonies DH. The damage control sequence and underlying logic. Surg Clin North Am, 77:761-777, 1997. [PubMed: 9291979]
46. Ivatury RR, Diebel L, Porter JM, Simon RJ. Intraabdominal hypertension and the abdominal compartment syndrome. Surg Clin North Am 77:783-800,
1997. [PubMed: 9291981]
47. Watson RA, Howdieshell TR. Abdominal compartment syndrome. South Med J 91(4):326-332, 1998.
48. Ertel W, Oberholzer A, Platz A, Stocker R, Trentz O. Incidence and clinical pattern of the abdominal compartment syndrome after "damage-control"
laparotomy in 311 patients with severe abdominal and/or pelvic trauma. Crit Care Med 2000;28:1747-1753. [PubMed: 10890613]
49. Morison R. Remarks on some functions of the omentum. Br Med J 1:76-78, 1906.
50. Anson BJ, Lyman RY, Lander HH. The abdominal viscera in situ: a study of 125 consecutive cadavers. Anat Rec 1936;67:17.
51. Griffith CA. Anatomy of the stomach and duodenum. In: Wastell C, Nyhus LM, Donahue PE. Surgery of the Esophagus, Stomach, and Small Intestine
(5th ed). Boston: Little, Brown, 1995, p. 388-417.
5/23/2014 Print: Chapter 10. Peritoneum, Omenta, and Internal Hernias
http://web.uni-plovdiv.bg/stu1104541018/docs/res/skandalakis' %20surgical%20anatomy%20-%202004/Chapter%2010_%20Peritoneum,%20Omenta,%20and% 60/62
(5th ed). Boston: Little, Brown, 1995, p. 388-417.
52. Skandalakis JE. [Spontaneous idiopathic hemorrhagic infarction of the greater omentum]. Surg Rev (Greece) 1954;18:1-7.
53. Nylander G, Tjernberg B. The lymphatics of the greater omentum. Lymphology 1967;2:3-7.
54. Sarrazin R, Pissas A, Dyon JF, Bouchet Y. [Lymphatic drainage of the stomach]. Anat Clin 1979;2:95-110.
55. Bercovici B. Antimicrobial activity of human peritoneal fluid. Surg Gynecol Obstet 1972;141:885.
56. Golden GT, Shaw A. Primary peritonitis. Surg Gynecol Obstet 1972;135:513. [PubMed: 4562119]
57. Moore FD. The gastrointestinal tract and the acute abdomen. In: Warren R. Surgery. Philadelphia: WB Saunders, 1963, p. 748.
58. Clagett M. Greek Science in Antiquity. New York: Barnes & Noble, 1994, p. 40.
59. Wittmann DH. Intra-abdominal Infections. New York: Marcel Dekker, 1991.
60. Sinanan MA, Acute abdomen and appendix. In: Greenfield LJ. Surgery: Scientific Principles and Practice. Philadelphia: JB Lippincott, 1993, p. 1120-
1141.
61. Williams R. Angiogenesis and the greater omentum. In: Goldsmith HS. Omentum: Proceedings of the First International Conference on the Omentum
Held in Research Triangle Park, North Carolina, October 28-31, 1988. New York: Springer-Verlag, 1990, p. 45-62.
62. Finck CM, Barker S, Simon H, Marx W. A novel diagnosis of left paraduodenal hernia through laparoscopy. Surg Endosc (Online) 2000;14:87. [PubMed:
10854514]
63. Janin Y, Stone AM, Wise L. Mesenteric hernia. Surg Gynecol Obstet 150:747, 1980. [PubMed: 6988996]
64. Kuga T, Taniguchi S, Inoue T, Zempo N, Esato K. The occurrence of a strangulated ileus due to a traumatic transmesenteric hernia: report of a case.
Surg Today 2000;30:548-550. [PubMed: 10883470]
65. Bircher MD, Stuart AE. Internal herniation involving the sigmoid mesocolon. Dis Colon Rectum 24:404, 1981. [PubMed: 7261828]
66. Erskine JM. Hernia through the foramen of Winslow. Surg Gynecol Obstet 125:1093, 1967. [PubMed: 4864553]
67. Nagayoshi K, Nakanishi K. [Retrogastric colon mimicking foramen of Winslow hernia or left paraduodenal hernia: report of a case]. Nippon Acta Radiol
2000;60:445-447. [PubMed: 10965751]
68. Adler GG. Die Hernia supravesicalis. Bruns' Beitr Klin Chir 218:225, 1970. [PubMed: 5493516]
69. Burton CC. Hernias of the supravesical, inguinal, and lateral pelvis fossae: their diagnosis, classification, and relationship. Int Abstr Surg 91:1, 1950.
[PubMed: 15436198]
70. Skandalakis JE, Gray SW, Burns WB, Sangmalee U, Sorg JL. Internal and external supravesical hernia. Am Surg 42:142, 1976. [PubMed: 1247255]
71. Estrada RL. Internal Intra-Abdominal Hernias. Austin: RG Landes, 1994, pp. 138-48.
72. Markowitz AM. Retroanastomotic hernia. In: Nyhus LM, Harkins HN (eds). Hernia. Philadelphia: Lippincott, 1964.
73. Moore GP, Alden AW, Rodman GH. Is closed diagnostic peritoneal lavage contraindicated in patients with previous abdominal surgery? Acad Emerg Med
1997;4:287-290. [PubMed: 9107327]
74. Rodriguez MH, Smith J, Clark SL, Phelan JP. Ultrasound-guided paracentesis in the diagnosis of postpartum hemoperitoneum: a report of three cases. J
Reprod Med 1987;32:456-458. [PubMed: 3302252]
75. Ross GJ, Kessler HB, Clair MR, Gatenby RA, Hartz WH, Ross LV. Sonographically guided paracentesis for palliation of symptomatic malignant ascites. AJR
Am J Roentgenol 1989;153:1309-1311. [PubMed: 2479242]
76. Goletti O, Ghiselli G, Lippolis PV, Chiarugi M, Braccini G, Macaluso C, Cavina E. The role of ultrasonography in blunt abdominal trauma: results in 250
consecutive cases. J Trauma 1994;36:178-181. [PubMed: 8114131]
77. Ma OJ, Kefer MP. Ultrasound detection of free intraperitoneal fluid associated with hepatic and splenic injuries. South Med J 2001;94:54-57. [PubMed:
11213943]
78. Jennings OG, Howarth GR, Bhana M, Snyman LC, Hellstrom L, Bruintjies J. Infraumbilical-ring capillary abdominocentesis in late presentation ectopic
pregnancy: a prospective study. Int J Gynecol Obstet 1992;38:201-206. [PubMed: 1360422]
79. Marincola FM, Schwartzentruber DJ. Malignant ascites. In: DeVita VT Jr, Hellman S, Rosenberg SA (eds). Cancer: Principles and Practice of Oncology
(6th ed). Philadelphia: Lippincott Williams & Wilkins, 200l, pp. 2745-2752.
80. Falfoul A, Makni MY, Bellasfar M, Tnani M, Kaabar N, Kharouf M. [The role of culdocentesis in the diagnosis of ectopic pregnancy: prospective study of
478 cases]. J Gynecol Obstet Biol Reprod (Paris) 1991;20:917-922. [PubMed: 1838756]
5/23/2014 Print: Chapter 10. Peritoneum, Omenta, and Internal Hernias
http://web.uni-plovdiv.bg/stu1104541018/docs/res/skandalakis' %20surgical%20anatomy%20-%202004/Chapter%2010_%20Peritoneum,%20Omenta,%20and% 61/62
478 cases]. J Gynecol Obstet Biol Reprod (Paris) 1991;20:917-922. [PubMed: 1838756]
81. Tariq TA, Korejo R. Culdocentesis in diagnosis of disturbed ectopic pregnancy still a useful procedure in developing countries. JPMA J Pak Med Assn
1992;42:5-6. [PubMed: 1545483]
82. Glezerman M, Press F, Carpman M. Culdocentesis is an obsolete diagnostic tool in suspected ectopic pregnancy. Arch Gynecol Obstet 1992;252:5-9.
[PubMed: 1417089]
83. Vande Krol L, Abbott JT. The current role of culdocentesis. Am J Emerg Med 1992;10:354-358.
84. Chen SC, Lin Fy, Hsieh YS, Chen WJ. Accuracy of ultrasonography in the diagnosis of peritonitis compared with the clinical impression of the surgeon.
Arch Surg 2000;135:170-173. [PubMed: 10668876]
85. Seiler CA, Brugger L, Forssmann U, Baer HU, Buchler MW. Conservative surgical treatment of diffuse peritonitis. Surgery 2000;127:178-184. [PubMed:
10686983]
86. Bosscha K, Hulstaert PF, Visser MR, van Vroonhoven TJ, van der Werken C. Open management of the abdomen and planned reoperations in severe
bacterial peritonitis. Eur J Surg 2000;166: 44-49. [PubMed: 10688216]
87. Bassett JW. Exploration of the Abdomen. Springfield IL: Charles Thomas, 1967.
88. Singhabhandhu B, Ritz C, Gray SW, Bohman MD, Skandalakis JE. Lesions of the omentum. J Med Assoc Ga 1971;61:9-13.
89. Koperna T, Schulz F. Relaparotomy in peritonitis: prognosis and treatment of patients with persisting intraabdominal infection. World J Surg
2000;24:32-37. [PubMed: 10594200]
90. Muensterer OJ, Averbach AM, Jacquet P, Otero SE, Sugarbaker PH. Malignant peritoneal mesothelioma. Case-report demonstrating pitfalls of diagnostic
laparoscopy. Int Surg 82(3):240-243, 1997.
91. Estrada Saiz RV, Loscos Valerio JM, Garcia-Paredes J, del Pozo Camaron A, Estrada Perez V. [The role of laparoscopy in the diagnosis of primary
peritoneal mesothelioma]. [Review] [Spanish]. Rev Esp Enferm Dig 87(5):403-406, 1995.
92. Ditmars ML, Bongard F. Laparoscopy for triage of penetrating trauma: the decision to explore. J Laparoendosc Surg 6(5):285-291, 1996.
93. Fernando HC, Alle KM, Chen J, Davis I, Klein SR. Triage by laparoscopy in patients with penetrating abdominal trauma. Br J Surg 81(3):384-385, 1994.
94. Poole GV, Thomae KR, Hauser CJ. Laparoscopy in trauma. [Review] Surg Clin North Am 76(3):547-556, 1996.
95. Maffei Faccioli A, Meduri F, Caldironi MW, Diana F, Losacco L, Merenda R, Zuin A, Zangrandi F, Gerunda GE. [The role of laparoscopy and peritoneal
cytology in the preoperative staging of pancreatic carcinoma]. [Italian] Chir Ital 46(2):26-29, 1994.
96. Nezhat F, Allan CJ, Nezhat C, Martin DC. Nonvisualized endometriosis at laparoscopy. Int J Fertil 36(6):340-343, 1991.
97. al Quorain AA, Satti MB, al Gindan YM, al Ghassab GA, al Freihi HM. Tuberculous peritonitis: the value of laparoscopy. Hepato-Gastroenterology 38
Suppl 1:37-40, 1991.
98. Faranda C, Barrat C, Catheline JM, Champault GG. Two-stage laparoscopic management of generalized peritonitis due to perforated sigmoid diverticula:
eighteen cases. Surg Laparoscop Endosc Percutaneous Tech 2000;10:135-138. [PubMed: 10872974]
99. Ahmad M, Ahmed A. Tuberculous peritonitis: Fatality associated with delayed diagnosis. South Med J 1999;92:406-8. [PubMed: 10219360]
100. Morgenstern L, Thompson R, Friedman NB. The modern enigma of radiation enteropathy: sequelae and solutions. Am J Surg 1977;134:166. [PubMed:
879409]
101. Shiraishi M, Hiroyasu S, Ishimine T, Shimabuku M, Kusano T, Higashi M, Muto Y. Radiation enterocolitis: overview of the past 15 years. World J Surg
22:491-493, 1998. [PubMed: 9564294]
102. Kuroyama N, Sakai A, Hattori T, Hanayama N, Oosawa M. [Early omental transposition for postoperative sterno-mediastinitis]. [Japanese] Rinsho
Kyobu Geka 1994;14:417-419. [PubMed: 9423120]
103. Ovnat A, Pontin AR, Manas D, Swanepoel CR, Cassidy MJ, Kahn D. Omentopexy for the difficult perigraft lympocele after renal transplantation. S Afr J
Surg 1995;33:159-161. [PubMed: 8677466]
104. Averbach AM, Steves MA, Ettinghausen SE, Sugarbaker PH. Pelvic omentoplasty after low anterior resection with total mesorectal excision. Contemp
Surg 52(6):379-384, 1998.
105. Goti F, Hollman R, Stieger R, Lange J. Idiopathic segmental infarction of the greater omentum successfully treated by laparoscopy: report of case.
Surg Today 2000;30:451-453. [PubMed: 10819485]
106. Stella DL, Schelleman TG. Segmental infarction of the omentum secondary to torsion: ultrasound and computed tomography diagnosis. Australasian
Radiol 2000;44:212-215. [PubMed: 10849989]
107. Stachowicz N, Czekierdowski A. [Omental torsion in pregnant woman]. Wiadomosci Lekarskie 2000;53:109-111. [PubMed: 10806931]
5/23/2014 Print: Chapter 10. Peritoneum, Omenta, and Internal Hernias
http://web.uni-plovdiv.bg/stu1104541018/docs/res/skandalakis' %20surgical%20anatomy%20-%202004/Chapter%2010_%20Peritoneum,%20Omenta,%20and% 62/62
108. Al-Husaini H, Onime A, Oluwole SF. Primary torsion of the greater omentum. J Nat Med Assn 2000;92:306-308. [PubMed: 10918767]
109. Goldsmith HS. Omentum: Proceedings of the First International Conference on the Omentum Held in Research Triangle Park, North Carolina, October
28-31, 1988. New York: Springer-Verlag, 1990.
110. Mazier WP, Surrell JA, Senagore AJ. The bottom end: handling of the perineal wound after abdominoperineal resection. Am Surg 1991;57:454-458.
[PubMed: 2058853]
111. Thome Saint Paul M, Bremond A, Rochet Y. [Absence of peritonealization after pelvic cancer surgery: results in 157 cases]. J Gynecol Obstet Biol
Reprod (Paris) 1991;20:957-960.
112. Spernol R, Hecher K, Gorzer H, Szalay S. [Complications of radical operation of uterine cancer. Closure of the peritoneal defects--yes or no?].
Geburtshilfe Frauenheilkunde 1992;52:210-213.
113. Nagele F, Kurz C, Husselein. [Abdominal hysterectomy without internal peritonealization: primary vaginal closure with stapler or open and drained
vagina]. Geburtshilfe Frauenheilkd 1994;54: 228-232. [PubMed: 8013858]
114. Than GN, Arany AA, Schunk E, Vizer M, Krommer KF. Closure or non-closure of visceral peritoneums after abdominal hysterectomies and Wertheim-
Meigs radical abdominal hysterectomies. Acta Chir Hung 1994;34:79-86. [PubMed: 7604632]
115. Dimpfl T, Stumpfe M, Maassen V, Genz T. [Lymphocele and complications after pelvic/para-aortic lymph node excision in relation to closure of the
peritoneum]. Geburtshilfe Frauenheilkunde 1994;54:233-236. [PubMed: 8013859]
116. Chen JS, Chang Chien CR, Wang JY, Fan HA. Pelvic peritoneal reconstruction to prevent radiation enteritis in rectal carcinoma. Dis Colon Rectum
1992;35:897-901. [PubMed: 1387358]
117. Keane WF, Vas SI. Peritonitis. In: Gokal R, Nolph KD (eds). The Textbook of Peritoneal Dialysis. Boston: Kluwer, 1994, pp. 473-502.
118. Cruse PJE, Foord R. A five-year prospective study of 23,649 surgical wounds. Arch Surg 1973;107:206. [PubMed: 4719566]
119. Farha GF, Chang FC, Matthews EH. Drainage in elective cholecystectomy. Am J Surg 1981;142:678. [PubMed: 7316031]
120. Johnson G, Gilsdorf R. Routine versus selective drainage of the gallbladder bed after cholecystectomy. Am J Surg 1981;142;651.
121. Hunt JL. Generalized peritonitis: to irrigate or not to irrigate the abdominal cavity. Arch Surg 1982;117:209. [PubMed: 7055434]
122. Dawson JL. A study of some factors affecting the mortality rate in diffuse peritonitis. Gut 1963;4:368.
123. Nathens AB, Rotstein OD, Marshall JC. Tertiary peritonitis: clinical features of a complex nosocomial infection. World J Surg 22:158-163, 1998.
[PubMed: 9451931]
124. Roberts CE, Athey PA. Sonographic demonstration of air in the myometrium: a complication of culdocentesis. J Ultrasound Med 1992;11:7-9.
125. Dicker D, Ashkenazi J, Feldberg D, Levy T, Deckel A, Ben-Rafael Z. Severe abdominal complications after transvaginal ultrasonographically guided
retrieval of oocytes for in vitro fertilization and embryo transfer [see comments]. Fertil Steril 1993;59:1313-1315. [PubMed: 8495784]
126. Morgenstern L. Anatomy and embryology of the spleen. In: Hiatt JR, Phillips EH, Morgenstern L (eds). Surgical Diseases of the Spleen. Berlin:
Springer, 1997, p. 20.
127. van Garderen JA, Wiggers T, van Geel AN. Complications of the pedicled omentoplasty. Neth J Surg 1991;43:171-174.
128. Boiskin I, Karna A, Demos TC, Blakeman B. Herniation of the transverse colon: an unusual complication of pedicled omentoplasty. Can Assoc Radiol J.
1995;46:223-225. [PubMed: 7538887]
129. Massard G, Wilk A, Dumond P, Rodier-Bruant C, Wihlm JM. [Diaphragmatic hernia complicating omentoplasty after thoracic wall excision: reflection
apropos of 2 cases]. Ann Chir Plast Esthet 1992;37:329-332. [PubMed: 1296511]
130. John H, Buchmann P. Improved perineal wound healing with the omental pedicle graft after rectal excision. Int J Colorectal Dis 1991;6:193-196.
[PubMed: 1770285]
131. Lechner P, Cesnik H. Abdominopelvic omentopexy: preparatory procedure for radiotherapy in rectal cancer. Dis Colon Rectum 1992;35:1157-1160.
[PubMed: 1473418]
Copyright 2006 The McGraw-Hill Companies. All rights reserved.
Privacy Notice. Any use is subject to the Terms of Use and Notice. Additional Credits and Copyright Information.
Вам также может понравиться
- Chapter 23 Kidneys and UretersДокумент71 страницаChapter 23 Kidneys and UretersMACON824Оценок пока нет
- Peritoneal Cavity PowerpointДокумент34 страницыPeritoneal Cavity Powerpointjojolilimomo100% (4)
- Abdomen and Pelvis 2nd Year Topical Past Papers 2005-22Документ10 страницAbdomen and Pelvis 2nd Year Topical Past Papers 2005-22Maliha sajid100% (1)
- Maniobras QuirurgicasДокумент6 страницManiobras Quirurgicasyesmaster15100% (3)
- Sample Case Study BurnДокумент27 страницSample Case Study BurnRj Cordero75% (4)
- Science Grade 4 Q2Документ291 страницаScience Grade 4 Q2Shie Pante80% (5)
- Interceptive OrthodonticsДокумент38 страницInterceptive OrthodonticsFinhas100% (5)
- Hemomancy: The Arcane Arts of BloodДокумент12 страницHemomancy: The Arcane Arts of BloodMathieu Bst-georges100% (1)
- High Yield Step 1 FactsДокумент3 страницыHigh Yield Step 1 Factsadmitone01Оценок пока нет
- Chapter 14 EsophagusДокумент48 страницChapter 14 EsophagusSMEY204Оценок пока нет
- Chapter 24 Urinary BladderДокумент42 страницыChapter 24 Urinary BladderMACON824Оценок пока нет
- PneumoperitoneumДокумент31 страницаPneumoperitoneumRaif RizqullahОценок пока нет
- Pneumo PeritoneumДокумент31 страницаPneumo PeritoneumRaif RizqullahОценок пока нет
- Chapter 18 Large Intestine and AnorectumДокумент159 страницChapter 18 Large Intestine and AnorectumSMEY204Оценок пока нет
- Chapter 22 SpleenДокумент69 страницChapter 22 SpleenMACON824100% (1)
- HerniaДокумент31 страницаHerniaDimas GunawanОценок пока нет
- International Journal of Surgery Case ReportsДокумент3 страницыInternational Journal of Surgery Case Reportshussein_faourОценок пока нет
- Course Code: Ran 1206 Course Title: Radiography Anatomy IiДокумент9 страницCourse Code: Ran 1206 Course Title: Radiography Anatomy IisamuelОценок пока нет
- Study On Clinical Profile, Management & Outcome of Gastrointestinal Duplication in ChildrenДокумент35 страницStudy On Clinical Profile, Management & Outcome of Gastrointestinal Duplication in ChildrenIJAR JOURNALОценок пока нет
- Us Gastro y Pared AbdДокумент64 страницыUs Gastro y Pared AbdLibelulaCoutureОценок пока нет
- Cystogram With Dumbbell Shaped Urinary Bladder in A Sliding Inguinal HerniaДокумент12 страницCystogram With Dumbbell Shaped Urinary Bladder in A Sliding Inguinal Hernia6281326189433Оценок пока нет
- Samir PDF Oral Exam ReviewДокумент42 страницыSamir PDF Oral Exam ReviewThomas Johnson100% (1)
- Anatomie Colon RectДокумент11 страницAnatomie Colon RectLarisa StanОценок пока нет
- A Tour ofДокумент10 страницA Tour ofChaimae OuafikОценок пока нет
- Intrapleural Ruptured Hydatid Cyst of Liver Presented As Eosinophilic Pleural Effusion: Case ReportДокумент7 страницIntrapleural Ruptured Hydatid Cyst of Liver Presented As Eosinophilic Pleural Effusion: Case ReportIJAR JOURNALОценок пока нет
- Abdomen CAP Questions and AnswersДокумент6 страницAbdomen CAP Questions and AnswersRathnaОценок пока нет
- Case Report: Identification of The Transverse Mesocolon and Root of Small Bowel Mesentery A New Sign of PneumoperitoneumДокумент3 страницыCase Report: Identification of The Transverse Mesocolon and Root of Small Bowel Mesentery A New Sign of PneumoperitoneumKrsna DharmasyaОценок пока нет
- Esophagealcancer:A Historicalperspective: Guy D. EslickДокумент15 страницEsophagealcancer:A Historicalperspective: Guy D. EslickNatalindah Jokiem Woecandra T. D.Оценок пока нет
- Cystogram With Dumbbell Shaped Urinary Bladder in A Sliding Inguinal HerniaДокумент3 страницыCystogram With Dumbbell Shaped Urinary Bladder in A Sliding Inguinal HerniaSuhesh Kumar NОценок пока нет
- Peritoneal SpaceДокумент54 страницыPeritoneal Spacehsah radiologyОценок пока нет
- Hernia Refarat Khansa 2Документ31 страницаHernia Refarat Khansa 2Khansa Hanifah Mutia100% (1)
- Acute Appendicitis: Anatomy, Pathophysiology, and Clinical PresentationДокумент26 страницAcute Appendicitis: Anatomy, Pathophysiology, and Clinical PresentationSimonGonzalezAponteОценок пока нет
- Primary Omental Torsion: A Case ReportДокумент3 страницыPrimary Omental Torsion: A Case Reportprabowoaji12Оценок пока нет
- Anatomy of LiverДокумент11 страницAnatomy of LiverSyed NusrathОценок пока нет
- Nosocomial Urinary Tract Infection Related Retro-Peritoneal Abscess With Internal Colonic FistulaДокумент5 страницNosocomial Urinary Tract Infection Related Retro-Peritoneal Abscess With Internal Colonic FistulaYuko Dwi ApriantoОценок пока нет
- Hartmann ProcedureДокумент87 страницHartmann Procedureariansahmargaluta0% (1)
- Case Report: Unusual Presentations in Inguinal Hernia: Four Cases With Review of LiteratureДокумент7 страницCase Report: Unusual Presentations in Inguinal Hernia: Four Cases With Review of LiteratureHolly JonesОценок пока нет
- Tuberculosis of The Chest Wall With Massive Tuberculous Pleural EffusionДокумент3 страницыTuberculosis of The Chest Wall With Massive Tuberculous Pleural EffusionwulanОценок пока нет
- Congenital Abdominal Wall Defects: An IntroductionДокумент38 страницCongenital Abdominal Wall Defects: An IntroductionAhmad Abu KushОценок пока нет
- Pneumothorax, Pneumomediastinum, Pneumoperitoneum, Pneumoretroperitoneum, and Subcutaneous Emphysema After ERCPДокумент4 страницыPneumothorax, Pneumomediastinum, Pneumoperitoneum, Pneumoretroperitoneum, and Subcutaneous Emphysema After ERCPSuryani MalikОценок пока нет
- Anesthetic Considerations For Abdominal TraumaДокумент14 страницAnesthetic Considerations For Abdominal TraumaTrinh TrầnОценок пока нет
- Unit13 Anatomy MCQsДокумент50 страницUnit13 Anatomy MCQsAsadullah Yousafzai100% (2)
- Pancreas AnularДокумент4 страницыPancreas AnularmariaОценок пока нет
- 10.3906 Sag 1210 97 131912Документ6 страниц10.3906 Sag 1210 97 131912Oktavia firnandaОценок пока нет
- PeritonioДокумент5 страницPeritonioSandro PinhoОценок пока нет
- Ovarian Vein Syndrome: A Case ReportДокумент3 страницыOvarian Vein Syndrome: A Case ReportIJAR JOURNALОценок пока нет
- Urinary DiversionДокумент44 страницыUrinary Diversionminnalesri100% (1)
- Necropsy - Killer Whale NamiДокумент5 страницNecropsy - Killer Whale NamiThe Orca Project Corp100% (1)
- Appendico-Ileal Fistula in An Acute Ileus Patient: Bir Akut İleus Olgusunda Apendiko-İleal FistülДокумент2 страницыAppendico-Ileal Fistula in An Acute Ileus Patient: Bir Akut İleus Olgusunda Apendiko-İleal Fistülyacine tarikОценок пока нет
- Enterogenous Cysts of - Ileum: Pinniger, D.M., M.R.C.P. Lecturer in Pathology, St. Thomas's Hospital SchoolДокумент6 страницEnterogenous Cysts of - Ileum: Pinniger, D.M., M.R.C.P. Lecturer in Pathology, St. Thomas's Hospital SchoolAnsharah KhanОценок пока нет
- Anal CanalДокумент129 страницAnal CanalPalanki GopalОценок пока нет
- Hirschsprung Disease ExplainedДокумент14 страницHirschsprung Disease Explainedyuyu tuptupОценок пока нет
- Apendicitis Aguda1Документ4 страницыApendicitis Aguda1Montserrat CandiaОценок пока нет
- Chapter 53 - Exocrine Pancreas: Michael L. Steer M.DДокумент70 страницChapter 53 - Exocrine Pancreas: Michael L. Steer M.DpablenqueОценок пока нет
- Dr. Dhanti - CSL Membaca Foto PolosДокумент74 страницыDr. Dhanti - CSL Membaca Foto Polosm zainul fikriОценок пока нет
- Management of Incidental Bochdalek Hernia in An Asymptomatic Adult: A Case ReportДокумент4 страницыManagement of Incidental Bochdalek Hernia in An Asymptomatic Adult: A Case ReportBhushan D ThombareОценок пока нет
- 1 s2.0 S0039610905704084 MainДокумент25 страниц1 s2.0 S0039610905704084 Mainjuan pablo mesa mejiaОценок пока нет
- An Unusual Cause of "Appendicular Pain" in A Young Girl: Mesenteric Cystic LymphangiomaДокумент3 страницыAn Unusual Cause of "Appendicular Pain" in A Young Girl: Mesenteric Cystic LymphangiomaSherif Abou BakrОценок пока нет
- Indirect Inguinal Hernia Masquerading As A Spigelian HerniaДокумент3 страницыIndirect Inguinal Hernia Masquerading As A Spigelian HerniaMuhammad Benny SetiyadiОценок пока нет
- Jurnal DanielДокумент33 страницыJurnal DanielDaniel DerianОценок пока нет
- Recurrenthematocolpos Due To Isolatedatresia of The Lowerthird of The Vagina: A Case RepportДокумент7 страницRecurrenthematocolpos Due To Isolatedatresia of The Lowerthird of The Vagina: A Case RepportIJAR JOURNALОценок пока нет
- Treatise on the Anatomy and Physiology of the Mucous Membranes: With Illustrative Pathological ObservationsОт EverandTreatise on the Anatomy and Physiology of the Mucous Membranes: With Illustrative Pathological ObservationsОценок пока нет
- Atlas of Equine UltrasonographyОт EverandAtlas of Equine UltrasonographyJessica A. KiddОценок пока нет
- The Ileoanal Pouch: A Practical Guide for Surgery, Management and TroubleshootingОт EverandThe Ileoanal Pouch: A Practical Guide for Surgery, Management and TroubleshootingJanindra WarusavitarneОценок пока нет
- Amcsecondary Amenorrhea Gynecology WorkbookДокумент2 страницыAmcsecondary Amenorrhea Gynecology WorkbookSMEY204Оценок пока нет
- Blood On Ice in The Artic Is Not A Sign of DeathДокумент1 страницаBlood On Ice in The Artic Is Not A Sign of DeathSMEY204Оценок пока нет
- Clinical Effectiveness and Safety of Vildagliptin in With Type 2 DiabetesДокумент8 страницClinical Effectiveness and Safety of Vildagliptin in With Type 2 DiabetesSMEY204Оценок пока нет
- Vildagliptin Effectiveness and Safety in T2DM Patients in Real-World SettingsДокумент5 страницVildagliptin Effectiveness and Safety in T2DM Patients in Real-World SettingsSMEY204Оценок пока нет
- 1 Anatomy & Physiology of Eye For Ophthalmic NursesДокумент124 страницы1 Anatomy & Physiology of Eye For Ophthalmic NursesSMEY204100% (1)
- Sentence Analogies 1Документ1 страницаSentence Analogies 1Deea EaОценок пока нет
- Vildagliptin Effectiveness and Safety in T2DM Patients in Real-World SettingsДокумент5 страницVildagliptin Effectiveness and Safety in T2DM Patients in Real-World SettingsSMEY204Оценок пока нет
- Vildagliptin Effectiveness and Safety in T2DM Patients in Real-World SettingsДокумент5 страницVildagliptin Effectiveness and Safety in T2DM Patients in Real-World SettingsSMEY204Оценок пока нет
- Presentation SlidesДокумент8 страницPresentation SlidesSMEY204Оценок пока нет
- The Polar BearДокумент2 страницыThe Polar BearSMEY204Оценок пока нет
- Notes On Joints of The BodyДокумент19 страницNotes On Joints of The BodySMEY204Оценок пока нет
- PP Ulcere de La CorneeДокумент31 страницаPP Ulcere de La CorneeSMEY204Оценок пока нет
- Clinical Effectiveness and Safety of Vildagliptin in With Type 2 DiabetesДокумент8 страницClinical Effectiveness and Safety of Vildagliptin in With Type 2 DiabetesSMEY204Оценок пока нет
- Joints Sample Pop QuizДокумент2 страницыJoints Sample Pop QuizSMEY204Оценок пока нет
- Joints Picture ofДокумент1 страницаJoints Picture ofSMEY204Оценок пока нет
- Joints Old Test SampleДокумент5 страницJoints Old Test SampleSMEY204Оценок пока нет
- Chapter 22 SpleenДокумент69 страницChapter 22 SpleenMACON824100% (1)
- Brulure Oculaire: By: DR To Chhun SengДокумент22 страницыBrulure Oculaire: By: DR To Chhun SengSMEY204Оценок пока нет
- Chapter 18 Large Intestine and AnorectumДокумент159 страницChapter 18 Large Intestine and AnorectumSMEY204Оценок пока нет
- Anatomy PDFДокумент4 страницыAnatomy PDFSMEY204Оценок пока нет
- Brulure Oculaire: By: DR To Chhun SengДокумент22 страницыBrulure Oculaire: By: DR To Chhun SengSMEY204Оценок пока нет
- Chapter 13 PharynxДокумент40 страницChapter 13 PharynxSMEY204Оценок пока нет
- Chapter 10 Peritoneium, Omenta, and InternalДокумент62 страницыChapter 10 Peritoneium, Omenta, and InternalSMEY204Оценок пока нет
- Chapter 3 Breast PDFДокумент35 страницChapter 3 Breast PDFSMEY204Оценок пока нет
- Chapter 2 Thoracic Wall and Pleurae PDFДокумент40 страницChapter 2 Thoracic Wall and Pleurae PDFSMEY204Оценок пока нет
- Chapter 1 NeckДокумент125 страницChapter 1 NeckMACON824Оценок пока нет
- Jamorama Chord BookДокумент76 страницJamorama Chord BookJamie Chan JieminОценок пока нет
- Causas de Pancitopenia Canina y FelinaДокумент12 страницCausas de Pancitopenia Canina y FelinaMarisol AsakuraОценок пока нет
- 10 3 2 Ijmr PDFДокумент4 страницы10 3 2 Ijmr PDFSindhu ShreeОценок пока нет
- MS Parent Bulletin (Week of May 22 To 26)Документ11 страницMS Parent Bulletin (Week of May 22 To 26)International School ManilaОценок пока нет
- Immune System - Answer KeyДокумент3 страницыImmune System - Answer Keyapi-250022577Оценок пока нет
- A Case Study Of: Status EpilepticusДокумент18 страницA Case Study Of: Status EpilepticusalexaОценок пока нет
- ANIMAL CALICIVIRUSESДокумент11 страницANIMAL CALICIVIRUSESlmreginioОценок пока нет
- The Use The Occlusogram in Planning Orthodontic TreatnaentДокумент13 страницThe Use The Occlusogram in Planning Orthodontic TreatnaentAna Molina Coral100% (1)
- Respiratory SystemДокумент2 страницыRespiratory SystemEmilia AmmariОценок пока нет
- Development of Dentition and Occlusion - Dr. Nabil Al-ZubairДокумент124 страницыDevelopment of Dentition and Occlusion - Dr. Nabil Al-ZubairNabil Al-Zubair75% (4)
- PDHPE Yearly NotesДокумент11 страницPDHPE Yearly NotesAnjaliОценок пока нет
- The Scientific AmericanДокумент46 страницThe Scientific AmericanShifa LeghariОценок пока нет
- Burch & Wartofsky Criteria For Thyroid StormДокумент2 страницыBurch & Wartofsky Criteria For Thyroid StormrulisakaroziОценок пока нет
- Microbiological Examination of Dairy ProductsДокумент6 страницMicrobiological Examination of Dairy ProductsLaksilu Viduraga PeirisОценок пока нет
- Khartoum University - Faculty of Dentistry Enterance Examinations McqsДокумент24 страницыKhartoum University - Faculty of Dentistry Enterance Examinations McqsHazim Rhman AliОценок пока нет
- Eye Movement Control and the Role of the Superior ColliculiДокумент10 страницEye Movement Control and the Role of the Superior ColliculiDavis KallanОценок пока нет
- Ana Histology PDFДокумент79 страницAna Histology PDFNagesh NОценок пока нет
- Measuring Vital SignsДокумент7 страницMeasuring Vital SignsPrischeilla InkiriwangОценок пока нет
- Diagnosis of viral infectionsДокумент3 страницыDiagnosis of viral infectionsRandy Butternubs100% (2)
- Omphalocele and GastroschisisДокумент12 страницOmphalocele and Gastroschisisluisisea100% (1)
- A N SДокумент2 страницыA N Samr ahmedОценок пока нет
- Protokol Kelahiran Pada Domba Dan KambingДокумент6 страницProtokol Kelahiran Pada Domba Dan KambingtrykartikadewiОценок пока нет
- GerdДокумент34 страницыGerdmrbrutusОценок пока нет
- Cleft LectДокумент76 страницCleft LectDiandra Puspa WidyasariОценок пока нет
- Anatomy Previous Question PaperДокумент2 страницыAnatomy Previous Question Paperpk1969Оценок пока нет
- Thesis Statement On Pro Animal TestingДокумент7 страницThesis Statement On Pro Animal Testingdianaolivanewyork100% (2)