Академический Документы
Профессиональный Документы
Культура Документы
Diarrhea (Pedia)
Загружено:
Eliza Paula BacudАвторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Diarrhea (Pedia)
Загружено:
Eliza Paula BacudАвторское право:
Доступные форматы
E
!
DIARRHEA
Grace L. Villa-Malayan MD, DPPS, DPAPP
OBJECTIVES
Definition of Diarrhea
Epidemiolgy
Mechanisms and Pathophysiology
Different causes of diarrhea
Diagnostics
Management
Prevention
GASTROENTERITIS
Denotes infections of the gastrointestinal tract
caused by bacterial, viral, or parasitic
pathogens
Most common manifestation is DIARRHEA
DIARRHEA
It is the an excessive loss of fluid and
electrolyte in the stool
It is a symptom of gastroenteritis with or
without vomiting, abdominal pain and fever
Acute diarrhea is a sudden onset of excessive
stools of >10 ml/kg/day in infants and
>200g/24 in older children which lasts for <14
days
Chronic or persistent diarrhea if the episode
lasts for >14 days
EPIDEMIOLOGY
Diarrheal disorders in childhood account for a
large portion (18%) of pediatric deaths
Estimated 1.5 Million deaths per year globally
WHO and UNICEF estimate that almost 2.5
Billion episodes of diarrhea occur in children
<5 years old
ETIOLOGY OF DIARRHEA
It is due infection through the fecal-oral route
or by ingestion of contaminated food or water
Associated with poverty, poor environmental
hygiene and development indices
Enteropathogens that are infectious in small
inoculums (shigella, enterohemorrhagic E. coli,
Campylobacter jejuni, noroviruses, rotavirus,
Giragia lamblia, Cryptosporidium parvum,
Entamoeba histolytica) ---- transmitted through
person-to-person contact
Cholera is a consequence of food or water
supply contamination
Food-borne outbreaks of bacterial diarrhea in
the US are commonly due to Salmonella, E.
coli, Clstridium botulinum, Clostridium
perfringens, and Staphylococcus aureus.
PATHOGENESIS OF INFECTIOUS DIARRHEA
Pathogenesis and severity of bacterial disease
depend on the presence of preformed toxins
(S.aureus, B.cereus), produce secretory
(cholera, E.coli, Salmonella, Shigella) or
cytotoxic (Shigella,S. aureus, V.
parahaemolyticus, C. difficile, EE. Coli, C.
jenuni) toxins or are invasive and on whether
they replicate in food.
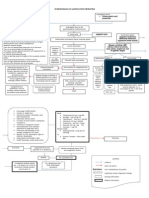
PATHOPHYSIOLOGY AND MECHANISM
The basis of diarrhea is disturbed intestinal
solute transport and water absorption
Water movement across intestinal membranes
is passive and both determined by both active
and passive fluxes of solutes like sodium.
Chloride and glucose
SECRETORY and DIARRHEA
Occurs when the intestinal epithelial cell solute
transport system in an active state of secretion
It is caused by secretagogue such as cholera
toxin
Toxin binds to epithelium of the bowel
Stimulates intracellular cAMP of cGMP
Increased secretion and electrolyte transport
E
#
PRIMARY
MECHANISM
DEFECT STOOL
EXAMINATION
EXAMPLES COMMENT
SECRETORY Decreased
absorption
Increased
secretion
Electrolyte
transport
Watery, normal
osmolality with ion
gap <100mOsm/kg
Cholera, toxigenic E.
coli; carcinoid, VIP,
neuroblastoma,
congenital chloride
diarrhea, Clostridium
difficile,
cryptosporidiosis
(AJDS)
Persists during
fasting; bile alt
malabsorption can
also increase
intestinal water
secretion; no stool
leukocytes
OSMOTIC Maldigestion
Transport
defects
Ingestion of
unabsorbable
substances
Watery, acidic, and
reducing substances:
increased osmolality
with ion gap >100
mOsm/kg
Lactase deficiency,
glucose galactose
malabsorption,
lactulose, laxative
abuse
Stops with
fasting:increased
breth hydrogen with
carbohydrate
malabsorption; no
stool leukocytes
INCREASED
MOBILITY
Decreased
transit time
Loose to normal
appearing stool,
stimulated by
gastrocolic reflex
Irritable bowel
syndrome,
thyrotoxicosis,
postvagotomy
dumping syndrome
Infection can also
contribute to
increased motility
DECREASED
MOBILITY
Defect in
neuromuscular
unit(s) stasis
(bacterial
overgrowth)
Loose to normal
appearing stool
Pseudo-obstruction,
blind loop
Possible bacterial
overgrowth
DECREASED
SURFACE
AREA
(OSMOTIC,
MOBILITY)
Decreased
functional
capacity
Watery
Short bowel
syndrome, celiac
disease, rotavirus
enteritis
Might require
elemental diet plus
parenteral
alimentation
MUCOSAL
INVASION
Inflammation,
decreased
colonic
Reabsorption,
increased
motility
Blood and increased
WBCs in stool
Salmonella, Shigella,
Infection; Amoebiasis;
Yersinia,
Campylobacter
Infections
Dysentery evident in
blood, mucus and
WBCs
Ion gap = Stool osmolality [[stool Na + stool K] x 2]
INFECTIOUS DIARRHEA
E. coli
Rotavirus
Salmonella
Shigella
Amoebiasis
E
$
COMPARISON OF THREE TYPES OF ENTERIC INFECTION
PARAMETER I II III
MECHANISM Noninflammatory
(enterotoxin or
adherence/superficial
invasion)
Inflammatory (invasion,
cytotoxin)
Penetrating
LOCATION Proximal small bowel Colon Distal small bowel
ILLNESS Watery diarrhea Dystentery Enteric fever
STOOL
EXAMINATION
No fecal leukocyte
Mild or no inc.
lactoferin
Fecal
polymorphonuclear
leukocytes
LActoferin
Fecal mononuclear
leukocyte
EXAMPLES Vibrio cholera
E. coli (ETEC,LT,ST)
C. perfringens
Bacillus cereus
Stphyloccoccus aureus
Also
+
:
Giardia lamblia
Rotavirus
Norwalk-like viruses
Cryptosporidium
parvum
E. coli (EPEC, EAEC)
Microsporidia
Cyclospora cayetanenis
Shigella
E. coli (EIEC, EHEC)
Salmonella enteridis
Vibrio
parahaemolyticus
Clostridium difficile
Campylobacter jejuni
Entamoeba histolytica
Salmonella typhi
Yersenia enterocolitica
?Campylobacter fetus
I. ESCHERICHIA COLI
Important causes of enteric infections
Member of the Enterobacteriaceae family
They are Facultative anaerobic, Gram negative bacilli
Most fecal E.coli do not cause diarrhea
E
%
ENTEROTOXIGENIC E.COLI (ETEC)
Causes 10-30% of dehydrating infantile
diarrhea in developing world
Causes 20-60% of travelers diarrhea
Responsible for 3-39% of overall diarrhea
episodes in the developing world
S/S
Explosive watery, nonmucoid, nonbloody
diarrhea, abdominal pain, nausea, vomiting
With or without fever
Self limiting
Usually resolves in 3-5 days but may last >1
week
PATHOGENESIS
Diarrhea is caused by the colonization of the
small intestine and elaboration of enterotoxins
Toxins: Heat-labile enterotoxin (LT) cAMP
Heat-stable enterotoxin (ST)-cGMP
Adherence is due to fimbrial colonization
factor antigens (CFs or CFAs)
ENTEROINVASIVE E.COLI (EIEC)
Watery diarrhea or dysentery syndrome ith
blood, mucus and leukocytes in stools
Fever, systemic toxicity, crampy abdominal
pain, tenesmus and urgency
Resembles bacillary dysentery
Most seen in outbreaks
EIEC causes colonic lesions with ulcerations,
hemorrhage, mucosal and submucosal edema
and infiltration by the polymorphonuclear
leukocytes
PATHOGENESIS
They invade the gut and produce dysentery like
illness
They enter into the cells --- intracellular
multiplication---- intracellular and intercellular
spread and host-cell death
Adheres thru invasion of the plasmid antigen
ENTEROPATHOGENIC E.COLI (EPEC)
The major cause of acute and persistent
diarrhea in children less than 2 years old in
developing countries
In developed countries, they cause occasional
outbreak in daycare centers and pediatric ward
S/S
Profuse watery, nonbloody diarrhea with
mucus, vomiting and low grade fever
Persistent diarrhea (>14 days) can lead to
malnutrition
PATHOGENESIS
EPEC causes blunting of villi, inflammatory
changes and sloughing superficial mucosa of
the duodenum and colon
Has characteristics attaching and effacing
(A/E) histopathologic lesion--- intimate
attachment of bacteria to the epithelial surface
and effacement of host cell microvilli
SHIGA TOXIN-PRODUCING E.COLI (STEC)
Five to 10% of children can have STEC
hemorrhagic colitis
Severe illness occurs most often among
children from 10 months to 10 years old
Transmitted from person to person as well as
by food and water
Poorly cooked hamburger is the most common
cause
S/S
Abdominal pain with diarrhea that is initially
watery but within a few days it can become
blood-streaked or grossly blood
PATHOGENESIS
STEC can affect the colon most severely
Organism adhere to intestinal cells
Strains affect humans by attaching-effacing
lesions
The attachment mechanism has genes (intimin,
tir, Esp A-D) very closely related to EPEC
Shiga toxin in the virulence factorC
ENTEROAGGRIVATIVE E.COLI (EAEC)
Associated with acute and persistent pediatric
diarrhea in developing countries, mostly in
children less than 2 years old.
S/S
Watery mucoid, secretory diarrhea with low-
grade fever and little or no vomiting
Watery diarrhea can persist for >14 days
Associated with growth retardation and
malnutrition in infants and developing
countries
PATHOGENESIS
It forms a characteristic biofilm on the
intestinal mucosa and induce shortening of the
E
&
villi, hemorrhagic necrosis and inflammatory
responses
PHASES OF PATHOGENESIS
1. Adherence to the intestinal mucosa by the way
of aggregative adherence fimbriae or related
adhesions
2. Enhanced production of mucus
3. Production of toxins
4. Inflammation that results in damage of the
mucosa and intestinal secretion
The intestinal inflammatory response
(increased fecal lactoferrin, interleukin-8 and
1Beta) may be related to growth impairment
and malnutrition
EAEC are recognized by adherence to Hep- 2
cells in an aggregative, stacked brick- like
pattern called aggregative adherence
DIFFUSELY ADHERENT E.COLI
? in doubt of its true pathogens
Both developed and developing countries have
associated the organisms with diarrhea
especially in children less than 2 years old
PATHOGENESIS
Two Putattive Adherence Factors:
1. Surface fimbriae responsible for the
diffuse adherence of phenotype in a
prototype strain
2. Outer membrane protein designated as
AIDA-I
DIAGNOSIS
Non-DNA dependent tests have been
developed for STEC
Serotype O157:H7 is suggested by isolation of
an E.coli that fails to ferment Sorbitol on
MacConkey Sorbitol medium
Other use tissue culture assays
Use of DNA probes for encoding various
virulence traits
EIEC there is positive fecal leukocyte
EIEC and STEC have elevated
polymorphonuclear leukocyte count with a left
shift
Fecal lactoferrin, IL8, IL-1 Beta are
inflammatory markers
Electrolytes are non specific
TREATMENT
The corner stone is still APPROPRIATE
FLUID AND ELECTROLYTE THERAPY as
specified by WHO
Oral rehydrating solutions are used to prevent
dehydration
Zinc supplementation
Antimicrobial therapy
PREVENTION
Proper hygiene
Prolonged breast-feeding
Proper food handling and disposal
ROTAVIRUS
Family : Reoviridae
Wheel-like, triple-shelled icosahedrons
containing 11 segments of double-stranded
RNA
Classified by serogroup A, B, C, D, F, G
Group A includes the common human
pathogens
PATHOGENESIS
Viruses can cause human diarrhea selectively
infect and destroy villus tip cells in the small
intestine
Biopsy showed villus blunting and round cell
infiltrate the lamina propia
Selective viral infection of intestinal villus tip
cells thus leads to:
a. Decreased absorption of salt and water
and an imbalance in the ratio of
intestinal fluid absorption to secretion
E
'
b. Diminished disaccharidase activity and
malabsorption of complex
carbohydrates particularly lactose
CLINICAL MANIFESTATION
Rotavirus infection incubation period is within
48 hrs (range 1-7 days) with mild to moderate
fever
Vomiting
Watery stools
Stool is without gross blood or WBC
Infection occurs among 4-36 months old
DIAGNOSIS
Based on clinical epidemiologic features
ELISA with >90% specificity
Latex agglutination tests
Electron microscopy
RNA PCR
LABORATORY
Isotonic dehydration with acidosis is the most
common finding in children with severe viral
enteritis
Stools are free of blood leukocyte
DIFFERENTIAL DIAGNOSIS
Other infectious causes of enteritis such as
bacteria and protozoa
Surgical cases such appendicitis, bowel
obstruction and intussusception
TREATMENT
Avoid and treating dehydration are the main
goals
Maintenance of the nutritional status
Lactobacillus species is helpful for mild cases
PROGNOSIS
Most fatalities occur in infants with poor
access to medical care and are attributed to
dehydration
Primary infection results in a predominantly
serotype-specific immune response
PREVENTION
Proper hygiene
Vaccination
SHIGELLA PATHOGENESIS
Superficial invasion of colonic mucosa through
M cells located over Peyer patches --- after
phagocytosisapoptosis of macrophages,
multiplication of bacteria, release of
transmigration of neutrophils into the lumen of
colon, neutrophil necrosis and degranulation
epithelial barrier and mucosal destruction
DIAGNOSIS
Asses degree of dehydration
History and PE
Clinically determine the etiology of diarrhea
E
(
Stool examination can give important data on
the etiology of diarrhea
TREATMENT
Oral rehydration therapy
Enteral feeding
Diet selection
Zinc supplementation
Probiotics?
Antibiotics?
HOME-MADE ORAL FLUID RECIPE
Preparing 1L of aral fluid using salt, sugar and water at
home. The ingredients to be mixed are:
1 tsp salt
8 leevl tsp sugar
1L (5 cupfuls) of clean drinkinf water or water
that has been boiled and then cooled.
Zinc supplementation for 10-14 days for less
than 0 months = 10 mg/day for more than 6
months = 20mg/day
Probiotics = restores good bacteria in the gut =
enhances host protective immunity such as
down-regulation of pro-inflammatory
cytokines and up-regulation of anti-
inflammatory cytokines
E
)
Dietary Recommendations
Antimicrobial agents for the treatment of specific
causes of diarrhea
PREVENTION
Report notifiable disease such as Botulinum,
E.coli, Salmonellosis, Shigellosis, Cholera,
Cryptosporidosis, and Cyclospora
Exclusive breast-feeding
Improved complementary feeding practices
Rotavirus immunization
Improved water and sanitary facilities and
promotion of personal and domestic hygiene
Improved case management of diarrhea
___END___
Вам также может понравиться
- ACUTE GASTROENTERITIS GUIDEДокумент54 страницыACUTE GASTROENTERITIS GUIDEVincent LaranjoОценок пока нет
- Junior Intern Review - Oral Revalida 2016Документ170 страницJunior Intern Review - Oral Revalida 2016Cyrus ZalameaОценок пока нет
- Clerks REVALIDA Review 2017Документ51 страницаClerks REVALIDA Review 2017Mara Medina - BorleoОценок пока нет
- CPG On Acute GastroenteritisДокумент24 страницыCPG On Acute GastroenteritisAbegail Fermanejo-Generao100% (1)
- Upper Gastrointestinal Bleeding (Ugib) : First Shift: August 13, 2018Документ10 страницUpper Gastrointestinal Bleeding (Ugib) : First Shift: August 13, 2018Angelo Dela Cruz VillaromanОценок пока нет
- Pedia ReviewerДокумент27 страницPedia ReviewerEvangeline GoОценок пока нет
- Final Oral Revalida Internal Medicine Compilation 1Документ45 страницFinal Oral Revalida Internal Medicine Compilation 1Joel SaluОценок пока нет
- Diarrhea: Cause Signs and Symptoms Pathophysiolog Y Prognosis StatisticsДокумент13 страницDiarrhea: Cause Signs and Symptoms Pathophysiolog Y Prognosis StatisticsRogie SaludoОценок пока нет
- Pedia Lecture 1-b Preventive Healthcare in Pediatrics TransДокумент10 страницPedia Lecture 1-b Preventive Healthcare in Pediatrics TransRemelou Garchitorena AlfelorОценок пока нет
- The Hydrocephalus Foundation of The Philippines, Inc.: Save A Life, I PledgeДокумент4 страницыThe Hydrocephalus Foundation of The Philippines, Inc.: Save A Life, I PledgejomitraОценок пока нет
- Oral Revalida 2019Документ28 страницOral Revalida 2019April Cabarlo100% (6)
- Bleeding Peptic Ulcer Disease Case StudyДокумент17 страницBleeding Peptic Ulcer Disease Case StudyChino Dela Cruz100% (2)
- PCAP Report ClerkshipДокумент54 страницыPCAP Report ClerkshipMichelleAquinoSuzukiОценок пока нет
- Hemophilia Nursing CareДокумент10 страницHemophilia Nursing CareEla 15Оценок пока нет
- Notes For Pedia HandoutДокумент2 страницыNotes For Pedia HandoutAiszel Angeli Pepito Ligo100% (2)
- Cirrhosis Complications and TreatmentsДокумент8 страницCirrhosis Complications and TreatmentsAlka Sangwan100% (2)
- Derma EAMC ReviewerДокумент25 страницDerma EAMC ReviewerJanna Janoras ŰОценок пока нет
- Surgery Ple ReviewerДокумент5 страницSurgery Ple ReviewerReinhard Ivan MansibangОценок пока нет
- Rectal Cancer Diagnosis and TreatmentДокумент15 страницRectal Cancer Diagnosis and TreatmentTarquin TomadaОценок пока нет
- 1 LiverДокумент10 страниц1 LiverAlbino Fulgencio Santos III100% (1)
- Tips For Ust Med FreshmenДокумент3 страницыTips For Ust Med FreshmenFred EvidorОценок пока нет
- Vii. Pathophysiology A. AlgorithmДокумент2 страницыVii. Pathophysiology A. AlgorithmJonna Mae TurquezaОценок пока нет
- TOPNOTCH Microbiology-Supertable-by-Dr - Cocoy-Calderon-Jaffar-Pineda-Troy-Soberano-UPDATED-NOVEMBER-2017 PDFДокумент34 страницыTOPNOTCH Microbiology-Supertable-by-Dr - Cocoy-Calderon-Jaffar-Pineda-Troy-Soberano-UPDATED-NOVEMBER-2017 PDFWaiwit KritayakiranaОценок пока нет
- Medicine OB History and PE TemplateДокумент9 страницMedicine OB History and PE TemplateJanella SuerteОценок пока нет
- Tuberculosis in Infancy and ChildhoodДокумент8 страницTuberculosis in Infancy and ChildhoodsamioОценок пока нет
- AGE Pedia CaseДокумент83 страницыAGE Pedia CaseLadybelle GototosОценок пока нет
- Homework Help, Research Papers, Online TutoringДокумент78 страницHomework Help, Research Papers, Online TutoringWilliam Soneja CalapiniОценок пока нет
- Endocrine Disorders and Exam QuestionsДокумент6 страницEndocrine Disorders and Exam QuestionsMartina GarciaОценок пока нет
- Gastric Outlet Obstruction PathophysiologyДокумент2 страницыGastric Outlet Obstruction PathophysiologyTania Noviza100% (1)
- Surgery Revalida Review PDFДокумент11 страницSurgery Revalida Review PDFMara Medina - BorleoОценок пока нет
- January 11 January 25 February 6 February 22: Date SubjectsДокумент3 страницыJanuary 11 January 25 February 6 February 22: Date SubjectsShams JailaniОценок пока нет
- Stroke (Bisaya and English)Документ4 страницыStroke (Bisaya and English)AnaОценок пока нет
- Pathology Polycystic Kidney DiseaseДокумент4 страницыPathology Polycystic Kidney DiseaseOnyedika EgbujoОценок пока нет
- Ulcerative ColitisДокумент18 страницUlcerative ColitisHoussein EL HajjОценок пока нет
- MalariaДокумент5 страницMalariaMiguel Cuevas Dolot100% (1)
- 2017 Wise 3RD Year With KeyДокумент24 страницы2017 Wise 3RD Year With KeyAnne Lorraine BringasОценок пока нет
- Chronic Suppurative Otitis Media in AdultsДокумент10 страницChronic Suppurative Otitis Media in AdultsRstadam TagalogОценок пока нет
- Essential Newborn Care StepsДокумент40 страницEssential Newborn Care StepsNehemiah FranciscoОценок пока нет
- The Pathophysiology of Peptic UlcerДокумент15 страницThe Pathophysiology of Peptic UlcerKike Meneses100% (1)
- Peptic Ulcer DiseaseДокумент119 страницPeptic Ulcer DiseaseJoy LacunaОценок пока нет
- Obstetrics Midterms Rationale 2nd Sem 2018 2019Документ21 страницаObstetrics Midterms Rationale 2nd Sem 2018 2019Gene Paulo UyОценок пока нет
- Case Study ON Hodgkin LymphomaДокумент8 страницCase Study ON Hodgkin LymphomaMeena KoushalОценок пока нет
- Course in The Wards FormatДокумент2 страницыCourse in The Wards FormatJade MonrealОценок пока нет
- Pharmacology Table - GonzalesДокумент14 страницPharmacology Table - GonzalesMark Angelo PonferradoОценок пока нет
- Ang Kwento Ni RosarioДокумент4 страницыAng Kwento Ni RosarioSheinna BarcelonaОценок пока нет
- Pathophysiology Diabetic Foot UlcerДокумент7 страницPathophysiology Diabetic Foot UlcerAnnisa ClaraОценок пока нет
- Pathophysiology AHS HTN EДокумент1 страницаPathophysiology AHS HTN Erod navalesОценок пока нет
- Surgery I #3 - Fluid and ElectrolytesДокумент9 страницSurgery I #3 - Fluid and ElectrolytesCarl Earvin L. Favorito100% (1)
- Gram Positive: NotesДокумент37 страницGram Positive: Notesgabb bbОценок пока нет
- Clinical Therapeutics Oral Revalida Review Notes: CASE 1: Dr. Abraham Daniel C. CruzДокумент31 страницаClinical Therapeutics Oral Revalida Review Notes: CASE 1: Dr. Abraham Daniel C. CruzNoreenОценок пока нет
- O High Fat, High Carbohydrate o Caffeinated and Carbonated o 73 Years Old o MaleДокумент4 страницыO High Fat, High Carbohydrate o Caffeinated and Carbonated o 73 Years Old o MaleJoherОценок пока нет
- Prevent Food & Waterborne DiseasesДокумент3 страницыPrevent Food & Waterborne DiseasesRolena Johnette B. PiñeroОценок пока нет
- Schistosomiasis Case StudyДокумент5 страницSchistosomiasis Case Studyapi-318749549Оценок пока нет
- MINDANAO STATE UNIVERSITY GRAND ROUNDS PROTOCOLДокумент14 страницMINDANAO STATE UNIVERSITY GRAND ROUNDS PROTOCOLArjay Amba0% (1)
- CyclosporineДокумент3 страницыCyclosporineraki9999Оценок пока нет
- Diarrea Crónica UPTODATEДокумент6 страницDiarrea Crónica UPTODATEConsuelo RiveraОценок пока нет
- PERSISTENT DIARRHEA IN NEONATES AND INFANTS UNDER 6 MONTHSДокумент6 страницPERSISTENT DIARRHEA IN NEONATES AND INFANTS UNDER 6 MONTHSConsuelo RiveraОценок пока нет
- Gastroenteritis Causes, Symptoms, and TreatmentДокумент20 страницGastroenteritis Causes, Symptoms, and TreatmentSuresh ThanneruОценок пока нет
- Intestinal Pathogens: Department of Clinical Microbiology Medical Faculty Universitas BrawijayaДокумент56 страницIntestinal Pathogens: Department of Clinical Microbiology Medical Faculty Universitas BrawijayaPipitОценок пока нет
- Diarrhea Mechanisms and ManagementДокумент54 страницыDiarrhea Mechanisms and ManagementMwanja Moses100% (1)
- Brain Stimulation Methods PsychiatryДокумент49 страницBrain Stimulation Methods PsychiatryEliza Paula BacudОценок пока нет
- Surgical Pathology Diseases of The Thyroid and ParathyroidДокумент13 страницSurgical Pathology Diseases of The Thyroid and ParathyroidEliza Paula BacudОценок пока нет
- Surgical Pathology Thyroid GlandДокумент24 страницыSurgical Pathology Thyroid GlandEliza Paula BacudОценок пока нет
- Viral Infections of The Nervous SystemДокумент11 страницViral Infections of The Nervous SystemEliza Paula BacudОценок пока нет
- Esophagus and Stomach Surgical Pathology 2015Документ18 страницEsophagus and Stomach Surgical Pathology 2015Eliza Paula BacudОценок пока нет
- Microbiology - Fundamentals of CHEMOTHERAPHYДокумент21 страницаMicrobiology - Fundamentals of CHEMOTHERAPHYEliza Paula BacudОценок пока нет
- ENT-Lec 4 Diseases of The Salivary Glands and HypopharynxДокумент11 страницENT-Lec 4 Diseases of The Salivary Glands and HypopharynxEliza Paula BacudОценок пока нет
- Formulary Clinical PharmacologyДокумент30 страницFormulary Clinical PharmacologyEliza Paula BacudОценок пока нет
- Microbiology - Fundamentals of Immunology InfectionДокумент19 страницMicrobiology - Fundamentals of Immunology InfectionEliza Paula BacudОценок пока нет
- Serum Markers For The Diagnosis of Myocardial InfarctionДокумент4 страницыSerum Markers For The Diagnosis of Myocardial InfarctionEliza Paula BacudОценок пока нет
- Neurology: Degenerative Diseases of The Nervous System-Dementing DisordersДокумент8 страницNeurology: Degenerative Diseases of The Nervous System-Dementing DisordersEliza Paula BacudОценок пока нет
- Neurology: Degenerative Diseases of The Nervous System 2 - Movement DisordersДокумент13 страницNeurology: Degenerative Diseases of The Nervous System 2 - Movement DisordersEliza Paula BacudОценок пока нет
- Maxillofacial Injuries ManagementДокумент7 страницMaxillofacial Injuries ManagementEliza Paula BacudОценок пока нет
- Neurology: Multiple Sclerosis and Allied Demyelinative DiseasesДокумент10 страницNeurology: Multiple Sclerosis and Allied Demyelinative DiseasesEliza Paula BacudОценок пока нет
- Approach To A The Child With A Fever and RashДокумент7 страницApproach To A The Child With A Fever and RashlaureeateОценок пока нет
- Nutritional Pathology: Vitamins, Minerals and Their FunctionsДокумент4 страницыNutritional Pathology: Vitamins, Minerals and Their FunctionsEliza Paula Bacud100% (3)
- 2nd SHIFTING EXAM Schedule and CoverageДокумент2 страницы2nd SHIFTING EXAM Schedule and CoverageEliza Paula BacudОценок пока нет
- A Qualitative Phenomenological Exploration of Teachers Experience With Nutrition EducationДокумент14 страницA Qualitative Phenomenological Exploration of Teachers Experience With Nutrition EducationDelfin ValdezОценок пока нет
- Event Service AgreementДокумент5 страницEvent Service AgreementPNC ChoraleОценок пока нет
- Chapter I - The Research Problem: Introduction/Background of The StudyДокумент4 страницыChapter I - The Research Problem: Introduction/Background of The StudyCha LinsengОценок пока нет
- Selected Answer:: 2 Out of 2 PointsДокумент15 страницSelected Answer:: 2 Out of 2 PointsAkansha dwivediОценок пока нет
- SWOT Analysis AuchanДокумент2 страницыSWOT Analysis AuchanDaniela DogaruОценок пока нет
- Doble M4000 User GuideДокумент204 страницыDoble M4000 User GuidePablo Toro Lopez100% (1)
- Commissioning Requirements Section 01810Документ28 страницCommissioning Requirements Section 01810tivesterОценок пока нет
- Child Development: Resilience & Risk, A Course SyllabusДокумент17 страницChild Development: Resilience & Risk, A Course SyllabusJane GilgunОценок пока нет
- Esea Elementary and Secondary Education Act Outline CampionДокумент9 страницEsea Elementary and Secondary Education Act Outline Campionapi-340155293Оценок пока нет
- APA Style Guide For StudentsДокумент18 страницAPA Style Guide For StudentsTeacher Jorge Omar NievesОценок пока нет
- Advanced GeomorphologyДокумент30 страницAdvanced GeomorphologyCarlos Letras100% (3)
- Eyebrow Tattoos Bản EnglishhДокумент3 страницыEyebrow Tattoos Bản EnglishhThùy Dương nèОценок пока нет
- PEPSICOДокумент35 страницPEPSICOAnkit PandeyОценок пока нет
- ODI AmE L1 ExtraGrammarWkshtДокумент30 страницODI AmE L1 ExtraGrammarWkshtJuan Carlos FlorezОценок пока нет
- Ficha Tecnica Sonometro Artisan SL2100PSДокумент1 страницаFicha Tecnica Sonometro Artisan SL2100PSJackson Steward Ríos SastoqueОценок пока нет
- LPT22Документ3 страницыLPT22Leonardo Vinicio Olarte CarrilloОценок пока нет
- Vote of Thanx For Grandparents Day at SchoolДокумент1 страницаVote of Thanx For Grandparents Day at SchoolkoolsurdieОценок пока нет
- TV Commercials Depicting MothersДокумент2 страницыTV Commercials Depicting MothersClarence TumabiaoОценок пока нет
- Jim106 Chapter 1 Practice ExercisesДокумент3 страницыJim106 Chapter 1 Practice ExercisesHor KaiОценок пока нет
- Worksheet - 2 (Gas Laws, Density, Molar Mass)Документ4 страницыWorksheet - 2 (Gas Laws, Density, Molar Mass)Jose Ruben SortoОценок пока нет
- I-WEB - Com.vn Manual 498031910Документ94 страницыI-WEB - Com.vn Manual 498031910IBJSC.comОценок пока нет
- Disjointed.S01E03.720p.webrip.x264 STRiFE (Ettv) .SRTДокумент32 страницыDisjointed.S01E03.720p.webrip.x264 STRiFE (Ettv) .SRTArthur CarvalhoОценок пока нет
- CHAPTER 6 Maintenance Management: Introduction, Importance, Types & ReliabilityДокумент29 страницCHAPTER 6 Maintenance Management: Introduction, Importance, Types & Reliabilitynur aidaОценок пока нет
- LakesДокумент14 страницLakesmanwartejam8Оценок пока нет
- Top 10 Credit Rating Agencies in WorldДокумент3 страницыTop 10 Credit Rating Agencies in Worldvmktpt100% (4)
- The Bondage of Sin Edward WelchДокумент8 страницThe Bondage of Sin Edward Welchandrés_torres_58Оценок пока нет
- Fever With Rash in Table Form.Документ4 страницыFever With Rash in Table Form.Azizan HannyОценок пока нет
- Role of NGOs in RehabilitationДокумент9 страницRole of NGOs in RehabilitationShamim HossainОценок пока нет
- PE and Health 3 Week 2 FINALДокумент8 страницPE and Health 3 Week 2 FINALFritzie SulitanaОценок пока нет
- Dum Aloo Recipe - How To Make Punjabi Dum Aloo, Restaurant StyleДокумент14 страницDum Aloo Recipe - How To Make Punjabi Dum Aloo, Restaurant Styleabhishek.mishrajiОценок пока нет