Академический Документы
Профессиональный Документы
Культура Документы
Basic Priciples of Heart Surgery
Загружено:
profarmah0 оценок0% нашли этот документ полезным (0 голосов)
634 просмотров6 страницBasic Priciples of Heart Surgery
Авторское право
© © All Rights Reserved
Доступные форматы
DOCX, PDF, TXT или читайте онлайн в Scribd
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документBasic Priciples of Heart Surgery
Авторское право:
© All Rights Reserved
Доступные форматы
Скачайте в формате DOCX, PDF, TXT или читайте онлайн в Scribd
0 оценок0% нашли этот документ полезным (0 голосов)
634 просмотров6 страницBasic Priciples of Heart Surgery
Загружено:
profarmahBasic Priciples of Heart Surgery
Авторское право:
© All Rights Reserved
Доступные форматы
Скачайте в формате DOCX, PDF, TXT или читайте онлайн в Scribd
Вы находитесь на странице: 1из 6
Basic principles of Open Heart Surgery
And Cardiopulmonary Bypass
Operative treatment of cardiac abnormalities is advancing rapidly, particularly
with the advent of new techniques for controlling the circulation and myocardial
preservation during surgery. The procedures can be, for practical purposes, placed
in one of 4 main categories:
A- Extra cardiac operations carried out on the main vessels outside the
heart as well as the pericardium. Examples include pericardiectomy for constrictive
pericarditis, ligation of patent ductus arteriosus, repair of aortic coarctation and
various palliative surgeries for congenital cyanotic heart diseases. Surgery is usually
performed without cardiopulmonary bypass and hence, avoids its inherent
complications. Also avoided is the prolonged mechanical ventilation as most of
those patients are extubated on table after surgery. After surgery, the ICU stay is
either short or the patient is directly admitted in an intermediate care facility.
B- Closed cardiac operations in which the surgeon tried to blindly repair
an intra cardiac pathology whether by finger or instrument placed inside the heart
through a purse string suture to avoid blood loss are no more than history. The last
procedure that was still carried out in some centers 10 years ago was closed mitral
valvotomy and is actually replaced by balloon valvotomy carried out by invasive
cardiologists. In fact, most of today cardiac surgery is performed by open heart
surgery techniques.
C- Classical Open heart surgery: In order to open the cardiac chambers
and perform a decent reliable and safe cardiac surgery, the heart must be empty
and motionless so as to see and be able to operate with precision. The heart should
be functionally disconnected form the circulation so as no blood is coming back
inside the heart from the vena cava and pulmonary veins, and no air is going out
form the opened-to-air heart to embolize other body organs. The question was the
following: If the heart has to be practically out of the circulation (i.e. arrested, not
receiving or pumping blood), we will be in need of a machine that can carry out
safely the cardiac function (receiving and pumping blood from and to the circulation);
and it was Charles Gibbons who invented the first safe cardiopulmonary by pass
(CPB) machine in conjunction with IBM engineers in 1954. Despite of hundreds of
renovations made on such machines, the basic idea was and remained simple
(figure 5):
1- Both right and left sides of the heart must be empty during surgery and
hence, systemic venous blood is drained by a cannula placed in the right atrium to
the CPB machine. The latter will then pump back the blood into the systemic
circulation through another cannula placed in the ascending aorta.
2- It is evident that the collected venous blood needs to be oxygenated
before being pumped back to the patients ascending aorta and systemic circulation
and hence, a synthetic bio membrane oxygenator has to be incorporated within the
CPB circuit to oxygenate the drained venous blood.
3- It is also evident that the patients blood can thrombose when collected
and pumped by a series of foreign synthetic materials and surfaces and hence, the
patient must be fully heparinized during CPB. After CPB, and in order to achieve
postoperative hemostasis, heparin is reversed by protamine sulfate on 1 to 1 basis.
4- In conclusion both the heart and lungs are functionally bypassed
during CPB and their main work which is: to receive and pump back blood i.e. to
maintain the systemic circulation (heart function) and to oxygenate this blood (lungs
function) is carried out by the CPB machine.
5- After establishing CPB as described, the heart can be arrested and
respiration can be stopped without fear of other organ damage. The question is now
the following: how would a heart being arrested and deprived from the circulation
survive the period of surgery? The absence of a perfect method to protect the heart
during this period explains the various measures adopted for myocardial
preservation. Classically, the ascending aorta is cross-clamped and a cold (4 C)
crystalloid hyperkalaemic solution is infused through the aortic root into the coronary
circulation. The solution arrests the heart during diastole and keep it arrested
(potassium), brings down to minimum its metabolic needs (coldness) and combats
acidosis induced by ischemia (different types of added buffer). The infusion is then
repeated every half an hour, until intracardiac procedures are terminated and
cardiac arrest is no more needed. Another common way of myocardial protection is
to infuse cold hyperkalaemic blood and not crystalloid into the coronary circulation.
Besides the above mentioned protective effects, the presence of blood add
nourishment to the myocardium during the arrest and is of course the best known
buffer to fight arrest induced acidosis. Nevertheless, Besides the use of one of the
many types of cardioplegia, other procedures that are concomitantly carried out to
improve myocardial preservation are: shortening the procedure and hence,
myocardial ischemic time, lowering the temperature of CPB itself (around 28 C) and
covering the heart itself with ice cold saline which further drops the myocardial
temperature and hence, minimizing its metabolic demands.
6- After terminating the intra cardiac procedure (heart valve replacement
or repair, coronary artery bypass grafting, repair of congenital anomaly, etc) all the
carried out processes are simply reversed: the cardiac chamber is closed and
carefully de-aired so that no air embolism occurs when the ascending aorta is de-
clamped and the heart is reconnected to the circulation. Ice cold saline is removed
and CPB blood is re-warmed to normal temperature. The patient is gradually
weaned off CPB by allowing the heart to gradually receive and pump more blood
until it regains its full action. After resuming normal ventilation and ensuring that the
heart can alone ensure full hemodynamic stability, cannulae are removed, heparin is
reversed by protamine sulfate, hemostasis is carried out and the wound is closed
before discharging the classically anesthetized and ventilated patient to the ICU.
Figure 5: The figure shows the basic cardiopulmonary bypass
circuit. Blood is collected from the right atrium via the venous
cannula (on the left). By gravity blood is then collected in a venous
reservoir placed at a lower level than the operating table. The
electric roller pump receives the blood from the reservoir to
actively push it inside the membrane oxygenator. The pump
controls the rate by which the oxygenated blood is then pushed
back to the systemic circulation via the cannula placed inside the
ascending aorta and hence, controls the cardiac output during
bypass. As shown, the system is further supplied by a heat
exchanger to control the blood, and hence, the body temperature
and a filter to catch any formed debris or air bubbles.
D-Minimal invasive cardiac surgery:
Cardiac surgery is a rapidly progressing branch for being essentially based on
the fast evolving modern technology. The field of progress is vast and ranges from
robotic surgery and genetic remodeling of pigs hearts to prevent their rejection once
transplanted in man to automated anastomosis equipments that replaced the
surgeons talent in creating a hand made anastomosis. The aim is to permit a safer
surgery with a short hospital stay and a better short as well as long term prognosis.
In this setting, minimal invasive cardiac surgery includes a variety of procedures
which aim to decrease the inherent morbidity of open heart surgery. Their use is
both patient and surgeon dependent and the gained benefit must be always
weighted with the possible drawbacks. The most famous examples are the following:
1- Minimal invasive approach: classically open heart surgery is performed
through median sternotomy which provides an excellent exposure and almost
permits all known open heart procedures. However, the scar of median sternotomy
is always visible, sometimes ugly and depressing especially for young adults.
Although less painful than a thoracotomy, yet delayed healing is associated with
severe pains that can last for months. Healing problems are met with in obese and
diabetic patients as well as in those cases where both mammary arteries (a major
blood source for the sternum) are used for coronary artery bypass grafting.
Moreover and whenever infection settles in, the mediastinum can be involved with a
resulting -sometimes fatal- mediastinitis. A limited left thoracotomy (5 cm length) can
be used for bypassing a stenosed left anterior descending coronary artery (major
and most important coronary artery) by an internal mammary artery that is harvested
endoscopically. The anastomosis can be carried out endoscopically too, which can
limit incisions to 3 short hardly visible ones. Equally, many open heart procedures
(mitral valve replacement, closure of atrial septal defect, etc) can be carried out
through a limited practically invisible sub-mammary right thoracotomy. Although
minimal invasive approaches have the advantages of giving a better and rapidly
healing scar, yet they have the disadvantages of needing more experienced
surgeons for the small field they supply, of being insufficient in cases of emergency
and of not allowing performing all types of surgeries.
2- Coronary artery bypass grafting with or without the use of CPB.
Although arresting the heart is mandatory for all intra-cardiac procedures, yet
coronary artery bypass grafting (CABG) does not involve opening the heart itself, as
coronary arteries just run on the heart surface and hence, some surgeons prefer to
carry CABG on beating heart with or without CPB. The procedure is tempting as the
heart is not arrested and hence the arrest-induced myocardial ischemia is avoided
however the perfection of coronary anastomosis while the heart is beating can
always be questionable. Avoiding CPB offers the advantages of avoiding its hazards
which includes: postoperative bleeding due to coagulation defects, CNS
complications due to cerebral edema and air embolism etc In absence of CPB,
there is no machine to support the circulation during surgery and the heart remains
the sole generator of body perfusion. As surgery on the beating heart necessitates
cardiac manipulations that can induce serious arrhythmias and hemodynamic
instability, a not less than perfect anesthetic techniques are required.
Вам также может понравиться
- Cardiac SurgeryДокумент27 страницCardiac SurgeryReeti Singh100% (1)
- A Simple Guide to Hypovolemia, Diagnosis, Treatment and Related ConditionsОт EverandA Simple Guide to Hypovolemia, Diagnosis, Treatment and Related ConditionsОценок пока нет
- DefibrillationДокумент25 страницDefibrillationAnisha Bagaria100% (2)
- Chest Tube InsertionДокумент3 страницыChest Tube InsertionprofarmahОценок пока нет
- Advanced Cardiac ProcedureДокумент9 страницAdvanced Cardiac ProcedureSachin DwivediОценок пока нет
- Cardiac MonitoringДокумент5 страницCardiac MonitoringAmit Kl100% (1)
- Arterial LineДокумент2 страницыArterial LineRaghav Goyal100% (1)
- A Simple Guide to Circulatory Shock, Diagnosis, Treatment and Related ConditionsОт EverandA Simple Guide to Circulatory Shock, Diagnosis, Treatment and Related ConditionsОценок пока нет
- Arterial Line Arterial LineДокумент13 страницArterial Line Arterial LineLinamaria Lozano100% (1)
- CCUДокумент82 страницыCCUSarah100% (1)
- CARDIOVERSION Vs DEFIBRILLATIONДокумент7 страницCARDIOVERSION Vs DEFIBRILLATIONjames garciaОценок пока нет
- Chest TraumaДокумент79 страницChest TraumaAnusha VergheseОценок пока нет
- Crash Cart Medication and ManagementДокумент20 страницCrash Cart Medication and ManagementSilpa Kuruvilla100% (2)
- Disorders of AortaДокумент25 страницDisorders of Aortavani reddyОценок пока нет
- Management Acute StrokeДокумент108 страницManagement Acute StrokeratuhamimОценок пока нет
- Cardiac Surgeries: and ManagementДокумент64 страницыCardiac Surgeries: and ManagementSimon Josan0% (1)
- Defibrillation and Cardioversion PDFДокумент12 страницDefibrillation and Cardioversion PDFmadeОценок пока нет
- PneumothoraxДокумент52 страницыPneumothoraxtrisna satrianaОценок пока нет
- Heart-Lung MachineДокумент4 страницыHeart-Lung Machinearsalanbook100% (2)
- Cardiac Enzyme StudiesДокумент4 страницыCardiac Enzyme StudiesDara VinsonОценок пока нет
- Defibrillation TypedДокумент8 страницDefibrillation TypedValarmathiОценок пока нет
- EmpyemaДокумент107 страницEmpyemaNITHA KОценок пока нет
- Pulse OximeterДокумент13 страницPulse Oximeteramanuel waleluОценок пока нет
- BLS (Basic Life Support)Документ10 страницBLS (Basic Life Support)harpreetОценок пока нет
- OrganisationДокумент46 страницOrganisationShreyas Walvekar100% (1)
- Medical Surgical Nursing Suretech College of NursingДокумент18 страницMedical Surgical Nursing Suretech College of NursingSanket TelangОценок пока нет
- Report of Departmental Study On Ot Complex: ObjectivesДокумент52 страницыReport of Departmental Study On Ot Complex: Objectivesvvvvtusebt100% (1)
- Percutaneous Transluminal Coronary AngioplastyДокумент22 страницыPercutaneous Transluminal Coronary AngioplastyArya Gaunker100% (1)
- Echocardiogram MayoДокумент4 страницыEchocardiogram MayoMarta KitaОценок пока нет
- English Recovery RoomДокумент5 страницEnglish Recovery RoomRahima PutriОценок пока нет
- Cardio Vascular Assessment: Manali H Solanki F.Y.M.Sc - Nursing J G College of NursingДокумент46 страницCardio Vascular Assessment: Manali H Solanki F.Y.M.Sc - Nursing J G College of NursingmeghanaОценок пока нет
- Care of Chest Tube Drainage & Nursing Manangement SHДокумент82 страницыCare of Chest Tube Drainage & Nursing Manangement SHJoanna RemollinoОценок пока нет
- INOTROPESДокумент28 страницINOTROPESsinghal297% (30)
- Oropharyngeal Airway InsertionДокумент6 страницOropharyngeal Airway InsertionydtrgnОценок пока нет
- Intercostal DrainageДокумент39 страницIntercostal DrainagePutri AdiratnaОценок пока нет
- Peripheral Arterial DseДокумент2 страницыPeripheral Arterial Dsemiss RNОценок пока нет
- Pain Assessment & ManagementДокумент36 страницPain Assessment & ManagementremeroseОценок пока нет
- Extubation Criteria PDFДокумент3 страницыExtubation Criteria PDFDediSutanto100% (1)
- Admission and EmergencyДокумент12 страницAdmission and EmergencyRashid AyubiОценок пока нет
- Arterial LinesДокумент13 страницArterial LinesberhanubedassaОценок пока нет
- DefibrillatorДокумент8 страницDefibrillatorJisha JanardhanОценок пока нет
- Introduction Definition: Types of PacemakersДокумент8 страницIntroduction Definition: Types of PacemakersPrasann RoyОценок пока нет
- Fumigation in Operation TheatresДокумент22 страницыFumigation in Operation TheatresUtkarsh RaiОценок пока нет
- Electroencephalography: Preparation of Patients and Assisting With EEGДокумент15 страницElectroencephalography: Preparation of Patients and Assisting With EEGPaul MОценок пока нет
- Neuromuscular Blocking AgentsnewДокумент22 страницыNeuromuscular Blocking Agentsnewvinay0717100% (1)
- Respiratory Failure (1) .Документ36 страницRespiratory Failure (1) .Ibrahim HemdanОценок пока нет
- Assisting Central Venous Catheter (CVC) Insertion (Procedure1)Документ7 страницAssisting Central Venous Catheter (CVC) Insertion (Procedure1)BsBs A7medОценок пока нет
- Heart Muscle Shortness of Breath Tired Swelling of The Legs Heart Failure Irregular Heart Beat Fainting Sudden Cardiac DeathДокумент6 страницHeart Muscle Shortness of Breath Tired Swelling of The Legs Heart Failure Irregular Heart Beat Fainting Sudden Cardiac DeathSachin DwivediОценок пока нет
- Icu & Critical Care Unit Management Time Material PersonnelДокумент62 страницыIcu & Critical Care Unit Management Time Material PersonnelsheslyОценок пока нет
- Inotropes in Critical Care UnitДокумент48 страницInotropes in Critical Care UnitKelvin Christopher Ker100% (1)
- Chest Tube and Water-Seal DrainageДокумент25 страницChest Tube and Water-Seal DrainageGhadaОценок пока нет
- Cardiovascular Examination:: General InspectionДокумент6 страницCardiovascular Examination:: General InspectionPhysician AssociateОценок пока нет
- Cardiac Monitor, ECG and CauterizationДокумент28 страницCardiac Monitor, ECG and CauterizationGlaiza Mae Olivar-ArguillesОценок пока нет
- Pulmonary Function Tests ScribdДокумент34 страницыPulmonary Function Tests ScribdNamita JadhaoОценок пока нет
- 0347burst AbdomenДокумент24 страницы0347burst AbdomenSathishKumar100% (1)
- Seminar On CV Thoracic SurgeriesДокумент81 страницаSeminar On CV Thoracic SurgeriesMegha lakraОценок пока нет
- Pre and Post Operative Care For Patient After Cardiac SurgeryДокумент20 страницPre and Post Operative Care For Patient After Cardiac SurgeryGayathri RОценок пока нет
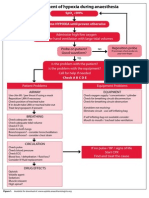
- Management of Hypoxia During AnaesthesiaДокумент5 страницManagement of Hypoxia During AnaesthesiaNurhafizahImfista100% (1)
- Current Status of Arterial Grafts For Coronary Artery Bypass GraftingДокумент4 страницыCurrent Status of Arterial Grafts For Coronary Artery Bypass GraftingprofarmahОценок пока нет
- Emergent Treatment of Aortic Rupture in Acute Type B DissectionДокумент7 страницEmergent Treatment of Aortic Rupture in Acute Type B DissectionprofarmahОценок пока нет
- Discordant Atrioventricular Connections 1Документ1 страницаDiscordant Atrioventricular Connections 1profarmahОценок пока нет
- Congenital Heart Surgery: The Appropriate Diagnosis Is Achieved byДокумент9 страницCongenital Heart Surgery: The Appropriate Diagnosis Is Achieved byprofarmahОценок пока нет
- Common Post Operative Complication and ManagementДокумент7 страницCommon Post Operative Complication and ManagementprofarmahОценок пока нет
- CPRДокумент10 страницCPRprofarmahОценок пока нет
- Chest Wall and Sternal Resection and ReconstructionДокумент5 страницChest Wall and Sternal Resection and ReconstructionprofarmahОценок пока нет
- CABGДокумент3 страницыCABGprofarmahОценок пока нет
- Aortic Arch Replacement With Frozen Elephant TrunkДокумент6 страницAortic Arch Replacement With Frozen Elephant TrunkprofarmahОценок пока нет
- Central Aortic Cannulation For Minimally Invasive Mitral Valve Surgery Through Right MinithoracotomyДокумент2 страницыCentral Aortic Cannulation For Minimally Invasive Mitral Valve Surgery Through Right MinithoracotomyprofarmahОценок пока нет
- Cardiac Post Opt OrdersДокумент1 страницаCardiac Post Opt OrdersprofarmahОценок пока нет
- Cardiac AnasthesiaДокумент3 страницыCardiac AnasthesiaprofarmahОценок пока нет
- Cardiac Surgery MCQДокумент43 страницыCardiac Surgery MCQprofarmah100% (7)
- Central Aortic Cannulation For Minimally Invasive Mitral Valve Surgery Through Right MinithoracotomyДокумент2 страницыCentral Aortic Cannulation For Minimally Invasive Mitral Valve Surgery Through Right MinithoracotomyprofarmahОценок пока нет
- Contraindications: Indications For SurgeryДокумент5 страницContraindications: Indications For SurgeryprofarmahОценок пока нет
- BYPASSДокумент2 страницыBYPASSprofarmahОценок пока нет
- Cabg 2Документ4 страницыCabg 2profarmahОценок пока нет
- Aorta Replacement and Repair Thoracic Aortic DissectionДокумент3 страницыAorta Replacement and Repair Thoracic Aortic DissectionprofarmahОценок пока нет
- Brom Aoroplasty For Supravalvar Aortic StenosisДокумент6 страницBrom Aoroplasty For Supravalvar Aortic StenosisprofarmahОценок пока нет
- BronchgramДокумент1 страницаBronchgramprofarmah100% (1)
- Aortic Dissection and Aneurysm 2Документ13 страницAortic Dissection and Aneurysm 2profarmahОценок пока нет
- Aortic Valve RepiarДокумент6 страницAortic Valve RepiarprofarmahОценок пока нет
- Left Hyper Lucency Left Hemithorax Larger Air in Pleural Cavity (No Vascular Markings) Atelectatic Lung (Upper Arrow) Bleb (Lower Arrow)Документ1 страницаLeft Hyper Lucency Left Hemithorax Larger Air in Pleural Cavity (No Vascular Markings) Atelectatic Lung (Upper Arrow) Bleb (Lower Arrow)profarmahОценок пока нет
- Calcified Nodes Calcified Nodules in Lungs: HistoplasmosisДокумент1 страницаCalcified Nodes Calcified Nodules in Lungs: HistoplasmosisprofarmahОценок пока нет
- Pleural EffusionДокумент10 страницPleural EffusionprofarmahОценок пока нет
- Multiple Bilateral Basal Air Fluid Levels See Close Up View BelowДокумент1 страницаMultiple Bilateral Basal Air Fluid Levels See Close Up View BelowprofarmahОценок пока нет
- EmpyemaДокумент1 страницаEmpyemaprofarmahОценок пока нет
- Inhomogeneous Cardiac Density Left Hilum Pulled Down Non-Visualization of Left Diaphragm Triangular Retrocardiac Atelectatic LLLДокумент1 страницаInhomogeneous Cardiac Density Left Hilum Pulled Down Non-Visualization of Left Diaphragm Triangular Retrocardiac Atelectatic LLLprofarmahОценок пока нет
- PneumoniaДокумент7 страницPneumoniaprofarmahОценок пока нет
- Evaluation of UNHCR's Leadership of The Global Protection Cluster and Field Protection Clusters, 2017Документ101 страницаEvaluation of UNHCR's Leadership of The Global Protection Cluster and Field Protection Clusters, 2017andyfeatherstoneОценок пока нет
- Ansari Ibnarabdoctrine 1999Документ45 страницAnsari Ibnarabdoctrine 1999JYOTI PALОценок пока нет
- Num PyДокумент46 страницNum Pyytmusik4Оценок пока нет
- Quantitative Option Strategies: Marco Avellaneda G63.2936.001 Spring Semester 2009Документ29 страницQuantitative Option Strategies: Marco Avellaneda G63.2936.001 Spring Semester 2009Adi MОценок пока нет
- Thesis Report On: Bombax InsigneДокумент163 страницыThesis Report On: Bombax InsigneShazedul Islam SajidОценок пока нет
- Celex 02003L0109-20110520 en TXTДокумент22 страницыCelex 02003L0109-20110520 en TXTertanОценок пока нет
- 21st Century Managerial and Leadership SkillsДокумент19 страниц21st Century Managerial and Leadership SkillsRichardRaqueno80% (5)
- Lesson Guides in Grade 1Документ99 страницLesson Guides in Grade 1Mary Ann FigueroaОценок пока нет
- Sagittarius The HeroДокумент2 страницыSagittarius The HeroСтеди Транслейшънс0% (1)
- Azeem English Magazine Vol. 22 Issue 01Документ68 страницAzeem English Magazine Vol. 22 Issue 01Raheel Asghar100% (1)
- Brand Management Bacardi SamveditaДокумент32 страницыBrand Management Bacardi SamveditaSamvedita IndrajeetОценок пока нет
- Do Large Language Models Need Sensory Grounding For Meaning and Understanding?Документ38 страницDo Large Language Models Need Sensory Grounding For Meaning and Understanding?Zakhar KoganОценок пока нет
- Ed 2 Module 8 1Документ5 страницEd 2 Module 8 1Jimeniah Ignacio RoyoОценок пока нет
- Kerala University PHD Course Work Exam SyllabusДокумент4 страницыKerala University PHD Course Work Exam Syllabuslozuzimobow3100% (2)
- Social Defence Vision 2020: Dr. Hira Singh Former Director National Institute of Social DefenceДокумент19 страницSocial Defence Vision 2020: Dr. Hira Singh Former Director National Institute of Social DefencePASION Jovelyn M.Оценок пока нет
- BM AssignmentДокумент7 страницBM AssignmentAntony LawrenceОценок пока нет
- National Social Protection Strategy GhanaДокумент95 страницNational Social Protection Strategy GhanaSisiraPinnawalaОценок пока нет
- Supply Chain Assignment Retail SupermarketДокумент20 страницSupply Chain Assignment Retail SupermarketBNthangeniОценок пока нет
- Ir21 Geomt 2022-01-28Документ23 страницыIr21 Geomt 2022-01-28Master MasterОценок пока нет
- IEM Notes Unit-2Документ2 страницыIEM Notes Unit-2Ashish YadavОценок пока нет
- In Defense of Imam BarbahariДокумент12 страницIn Defense of Imam Barbahariiliaswa33Оценок пока нет
- The Best WayДокумент58 страницThe Best Wayshiela manalaysayОценок пока нет
- HM3 ChaosHallsДокумент36 страницHM3 ChaosHallsBrady Mcghee100% (2)
- Tony Robbins ResultДокумент11 страницTony Robbins ResultSalee BuiserОценок пока нет
- Upholding Malay Language Strengthening Command English LanguageДокумент12 страницUpholding Malay Language Strengthening Command English LanguagemucheliaОценок пока нет
- USA v. William Gazafi Plea Letter To Judge TitusДокумент13 страницUSA v. William Gazafi Plea Letter To Judge TitusSouthern Maryland OnlineОценок пока нет
- 4 5 and 6 - Approaches To HR MeasurementДокумент14 страниц4 5 and 6 - Approaches To HR MeasurementRahul RaoОценок пока нет
- Journal of The Neurological Sciences: SciencedirectДокумент12 страницJournal of The Neurological Sciences: SciencedirectBotez MartaОценок пока нет
- Katehi Grievance LetterДокумент12 страницKatehi Grievance LetterSacramento BeeОценок пока нет
- Factors Influencing The PerceptionДокумент1 страницаFactors Influencing The PerceptionTinesh Kumar100% (1)