Академический Документы
Профессиональный Документы
Культура Документы
Fishman Aug 06
Загружено:
verghese170 оценок0% нашли этот документ полезным (0 голосов)
42 просмотров5 страницhjghgjhjhkj
Авторское право
© © All Rights Reserved
Доступные форматы
PDF, TXT или читайте онлайн в Scribd
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документhjghgjhjhkj
Авторское право:
© All Rights Reserved
Доступные форматы
Скачайте в формате PDF, TXT или читайте онлайн в Scribd
0 оценок0% нашли этот документ полезным (0 голосов)
42 просмотров5 страницFishman Aug 06
Загружено:
verghese17hjghgjhjhkj
Авторское право:
© All Rights Reserved
Доступные форматы
Скачайте в формате PDF, TXT или читайте онлайн в Scribd
Вы находитесь на странице: 1из 5
262 Volume 33 Number 4, August 2006
The power of the family
in general practice:
Enhance your effectiveness when
caring for anorexia nervosa patients
Charles Fishman MD ARANZCP & Tana Fishman MS DO FRNZCGP
Charles Fishman is Clinical Director of
Youthlink Family Trust and Director of
New Zealand Eating Disorder Special-
ists. Dr Fishman has over 30 years of
experience in the treatment of eating
disorders. His knowledge and experi-
ence are reflected in numerous books
he has written, including the popular
Enduring change in eating disorders:
Interventions with long-term results.
Correspondence to: charles@nzeatingdisorderspecialists.co.nz
ABSTRACT
Anorexia nervosa (AN) is a severe condition and is influ-
enced by a variety of factors, most notably social envi-
ronment. Family therapy has been shown to be effective
in the treatment of AN, particularly in patients under the
age of 19 years. However, while general practitioners (GPs)
are often the first point of contact for patients, family
therapy is not often introduced during the initial assess-
ment. The aim of this paper is to introduce the key con-
cepts of family therapy to aid GPs during the assessment
and treatment planning, so that the benefits of family
therapy can be made fully available to patients with AN.
Key words
Eating disorder, family process
*
General practitioners are strategically placed on the
frontline of care delivery and have significant experi-
Tana Fishman is a Senior Lecturer at
the University of Aucklands Depart-
ment of General Practice and Primary
Health Care. In addition, she has worked
in general practice for 11 years.
There is a tendency for all living things to join up,
establish linkages, live inside each other,
return to earlier arrangements, get along whenever possible.
This is the way of the world.
Lewis Thomas, The Lives of the Cell (1974)
ence and skill in working with families across multiple
generations. This paper is designed to add to the
generalist perspective the power of the family and offer
techniques for detection, support and stabilisation of ano-
rexia nervosa, a complex eating disorder. A partnership
between physician, patient, and family may provide the
most effective and efficient form of medical care in gen-
eral.
1
This partnership is especially important in the treat-
ment of anorexia nervosa.
Anorexia nervosa (AN) is considered by the Royal
Australian and New Zealand College of Psychiatrists
(RANZCP) to be a severe, distressing and often chronic
mental illness.
2
AN is characterised by intense anxiety,
preoccupations with body weight and/or shape and ex-
treme control over eating and weight and has a mean
duration that can range from five years to a lifetime for
some patients.
2
Of concern for the general practitioner
(GP) is the high death rate and strong denial that is very
common among anorectic girls. Indeed, a recent review
Continuing Medical Education
263 Volume 33 Number 4, August 2006
indicated that anorectic girls have the
highest mortality per capita of any
psychiatric disease (up to 6% per dec-
ade of illness).
3
The importance of the involve-
ment of family members in the as-
sessment and treatment of AN is rec-
ognised by the RANZCP in the Treat-
ment guide for consumers and carers,
4
as well as the United Kingdoms Na-
tional Institute for Clinical Excel-
lence.
5
Furthermore, in the Practice
Guidelines for the Treatment of pa-
tients with eating disorders published
by the American Psychiatric Asso-
ciation, problems with family rela-
tionships are indicated as potential
contributing factors to the mainte-
nance of the disorder.
6
However, the
RANZCP suggests that there is no re-
search proving a link between fam-
ily dysfunction and the onset of AN.
Nonetheless, there is strong evidence
to support the use of family therapy
as a treatment modality in patients
under the age of 19 years.
7
Family systems concepts
These concepts are the foundation
and language that are used when
working with families. Family char-
acteristics and family structure, in-
cluding hierarchy,
boundaries, family
role selection, alli-
ances, and coali-
tions, are concepts
that are observed on
a daily basis on the
frontline. Height-
ened awareness of
the family processes
including enmeshment, disengage-
ment, triangulation, and family pat-
terns provide power as these proc-
esses are challenged.
Clinical case review
A 16-year-old girl who had lost 9kg
over three months was referred by
her GP. She had a body mass index
(BMI) of 17. She was restricting food,
compulsively exercising and had
amenorrhea. Medical investigations
were unremarkable. A family assess-
ment was conducted with mother, fa-
ther and two younger siblings; fa-
ther worked professionally and
mother was at home. The adolescent
was leaving for university and the
launching of children, a stage of the
family life cycle, was reviewed.
Boundaries, subgroups, and hierar-
chies were observed along with shift-
ing alliances and coalitions. The fam-
ily, together with the therapeutic team
including the GP, worked to amelio-
rate her AN through support and re-
structuring her context to ensure a
successful launch was effective. At
discharge, her BMI was 20. The con-
tinued care was provided by her GP
and University Health Centre. (The
Family Therapy Model is based on
general systems theory and focuses
on contemporary forces influencing
and maintaining the symptoms.)
Prevalence
The Christchurch Psychiatric Epide-
miology Study (CPES) found only
three women per thousand in the gen-
eral population suffer from AN.
9
From our clinical and research ex-
perience, this finding is consistent
with both the general New Zealand
population and the worldwide pat-
terns of prevalence. With such a low
rate, the CPES study
found it difficult to
address risk factors
for the development
of AN. As sometimes
happens in general
practice, the atten-
tion and resources
that are required are
vastly out of propor-
tion to the prevalence. However, the
severity of AN is compounded by as-
sociated medical problems including
osteoporosis, amenorrhoea, hypogly-
caemia, and multi-organ failure.
10
Risk factors
Identifying risk factors has proved
to be an illusive exercise for many
reasons including the failure of pre-
vious studies to use appropriate
methodology and the fact that al-
though disordered eating can be dem-
onstrated, only a small proportion of
women develop a full anorexic syn-
drome. However, being female and
being young are two of the most
clearly identified risk factors.
11
Ad-
ditionally, being Westernised and
upper-middle class has been asserted
to be a risk factor. Richard Gordon
interviewed South Korean psychia-
trist Kim Joon Ki; prior to 1991, Kim
had seen only one patient with an
eating disorder (ED) however by
1997, he had seen over 200. As
Gordon points out, these changes
were concurrent with the forces of
industrialisation, consumerism and
democratisation that produced a
rapid cultural transition.
12
Even in
economically deprived countries like
India, EDs are starting to manifest.
This phenomenon is again co-occur-
ring with the rapid commercial and
industrial development and the emer-
gence of high technology.
Anne Becker, a psychiatrist and
anthropologist, visited Fiji on two
occasions separated by eight years. On
her first visit in the early 1990s, the
overweight Fijian women were accept-
ing of their size. Upon her return, there
Early clues and behaviours of
anorexia nervosa
4
Family history of anorexia.
Occupational groups e.g. ballet danc-
ers, gymnasts, jockeys and models.
Physical clues: loss of periods or fail-
ure to begin menstruating, weight loss
without evidence of any other illness.
Psychological clues: obsessive con-
cern about body weight, shape and
dieting, unrealistic perception about
being fat, extreme fear of getting fat
or gaining weight or of eating.
Behavioural clues: cutting out foods
once enjoyed, excessive exercise, vom-
iting and using laxatives, and avoid-
ing sharing meal times with others.
Body weight of 15% lower than ex-
pected, or BMI < 17.5.
As sometimes happens
in general practice, the
attention and resources
that are required are
vastly out of proportion
to the prevalence
Continuing Medical Education
264 Volume 33 Number 4, August 2006
were large numbers of women, espe-
cially teenagers, who were unhappy
with their body size and were actively
dieting. Again, the change to Fijian
culture was attributed to the introduc-
tion of the television.
12
A key aspect of Western culture
that is regarded to be an ED risk fac-
tor is the cultural value that thinness
is beautiful. Media
exposure has been
difficult to study
measuring expo-
sure is quite ap-
proximate. How-
ever, there is a per-
ception that women
(including young
girls) are bom-
barded by TV,
magazines, and
movies carrying
the ubiquitous message that the ideal
body image is thin. In spite of this
avalanche of body image pressure on
women, the disease remains rare.
Evidence-based treatments
Christopher Fairburn recently ques-
tioned whether evidence-based treat-
ment of AN was possible.
13
Fairburn
indicated that there was a range of
treatment options and treatment set-
tings, within which are a variety of
interventions: pharmacological, psy-
chological or both (often more than
one treatment is employed within any
one setting). There is limited research
on the treatment of AN and much of
it is inconclusive. The reasons for this
lack of research are many but the ma-
jor one is that AN is uncommon. Nev-
ertheless, we have included some
common treatment outcomes.
Medications
A search of randomised-control tri-
als (RCT) for medication research
found studies that were limited by
small sample sizes and research de-
sign. Most studies add medication to
comprehensive hospital-based treat-
ment programmes making it difficult
to determine unique effectiveness.
Several classes of pharmacologic
agents have been studied in patients
with acute AN without finding clear
benefits to eating, weight, body shape
concerns and associated psychopa-
thology.
14
Traditional antipsychotic medica-
tions are not considered in routine
care due to their significant side ef-
fects and limited evidence of their
clinical benefit. However, atypical
antipsychotic
medications may
have a role in the
treatment; an RCT
is the necessary
next step.
14
Fluoxetine may
be helpful in pre-
venting relapse in
weight-restored AN
patients.
15
However,
fluoxetine offered
no benefit when
compared with placebo to AN inpa-
tients undergoing weight restoration.
14
It is unclear why the medication
trials conducted to date have been
so universally discouraging. There is
criticism that the studies consistently
appear to be driven by only two gen-
eral hypotheses appetite stimula-
tion and alleviation of symptoms such
as anxiety and depression.
14
Psychological therapies
Of the few RCT for AN, most have fo-
cused on adolescent patients and sug-
gest that family therapy is an effec-
tive treatment for these patients.
16
The
benefits of family therapy with adult
patients, however, have been less clear.
In addition, attempts to demonstrate
effectiveness of Cognitive Behavioural
Therapy (CBT) in AN have yielded
only equivocal results.
17
Psychosomatic Family Model
In the early 1970s, three girls in their
early teens with severe uncontrolla-
ble juvenile onset diabetes (Type I)
were admitted to the Childrens Hos-
pital of Philadelphia in diabetic ke-
toacidosis. Salvador Minuchin and
his group from the Philadelphia Child
Guidance Clinic were investigating
psychosomatic illness and made a
startling observation: the girls dia-
betes spiralled out of control in only
one context the home. The
Minuchin team hypothesised that
some family interactional pattern may
be contributing to these exacer-
bations. They tested a model they
called the Psychosomatic Family.
This family is characterised by: ri-
gidity, triangulation, diffusion of
conflict, and over protectiveness.
They proposed that it was dysfunc-
tional patterns observable in the
therapy room that contributed to the
patients illness or symptoms.
To determine how these family
patterns affected diabetes, Minuchin
studied the physiologic responses of
diabetic children to a stressful family
interview.
18
Summarising the pioneer
work of the Family Stress Interview,
the researchers measured the free fatty
acids of the family members to deter-
mine where and when the acids arose
relative to the interactional patterns
within the family. If one assumes that
free fatty acids correlate with stress,
the interviews demonstrated the rela-
tionship between symptomatology and
the family interactional patterns. Par-
ents free fatty acids drop as their con-
flict is detoured or diffused through
the chronically ill child. The childs
free fatty acids rise steeply a huge
cost to the child in terms of exacer-
bation of symptoms. And to the ex-
tent the parents focus moves from
their conflict to their child, their stress
has been decreased, thus stabilising
the family system.
Following on from their work
with uncontrolled diabetes, the Psy-
chosomatic Family Model provided
the framework for anorexia patients.
In the original psychosomatic
project, follow-ups were conducted
with 53 anorectic adolescents (mean
age of 14) over two to seven years.
GP role in initial assessment
4
Full physical check up
Provide diagnosis
Organise other health professionals
including a referral to a psychiatrist
There is criticism that
studies consistently
appear to be driven by
only two general
hypotheses appetite
stimulation and alleviation
of symptoms such as
anxiety and depression
Continuing Medical Education
265 Volume 33 Number 4, August 2006
The findings indicated that 86% were
asymptomatic with good psychoso-
cial functioning. A study by Martin
19
conducted with anorectic adolescents
in Toronto and followed-up at five
years used a similar treatment ap-
proach and found the same degree
of success in outcome.
The Maudsley Family-based
Treatment Model
In the mid 1980s Christopher Dare and
colleagues at the Maudsley Hospital
of London developed a model with a
focus on many of the tenets and as-
sumptions as the Minuchin Model.
20
Parents work together and form a cru-
cial role in the treatment of their ano-
rexic child. The results favoured fam-
ily-based treatment (FBT) known as
the Maudsley method.
16
Benefits of family interventions
(literature review by McDaniel et al.
1
)
Minuchin successfully treated psy-
chosomatic families using Struc-
tural Family Therapy to disengage
the diabetic children and establish
more appropriate boundaries. In
15 cases, the pattern of recurring
ketoacidosis ceased and insulin
doses were reduced.
Two RCTs of family therapy in se-
vere childhood
asthma reported
improved health
outcomes. The
children who re-
ceived family
therapy had re-
duced symptoms,
medication use,
and school ab-
sences. Their
lung function improved as well.
One of the most successfully docu-
mented family interventions is
family psychoeducation. This in-
tervention provides information,
support, and problem-solving
skills to help families cope with a
chronic illness. It has been shown
to improve the outcomes in child-
hood diabetes, asthma, recurrent
abdominal pain and developmen-
tal disabilities.
Two types of family interventions
are effective in the treatment of
hypertension. Couples-communi-
cation training, in which one of
the couple has hypertension. In one
large study, providing family sup-
port to assist with compliance with
blood pressure medication re-
sulted in improved compliance,
reduced blood pressure and a 50%
reduction in mortality.
For more on the benefits of family
interventions and the complete lit-
erature review, see McDaniel et al.
1
Practical strategies for the
general practitioner
Many of the tenets of the Psychoso-
matic Family Model serve to instruct
the GP to assess and intervene with
families of AN patients. The impor-
tant contributions of researchers who
work at the interface between medi-
cine and family interventions can pro-
vide, in our opinion, practical strat-
egies for the GP. Their work, based
on grounded observations of family
interactions, extrapolates to the gen-
eral practice frontline in the follow-
ing ways:
The family partnership to diagno-
sis and treatment should be en-
gaged early. Family patterns are
very likely to be ob-
served in your con-
sultation room if
members of the so-
cial context are in-
cluded. The family
serves as the doctors
eyes and ears and
provides support and
safety nets for the
anorexia sufferer.
Beware of triangulation. When
conflict starts to arise, a third per-
son is recruited into a two-per-
son system in order to diffuse the
conflict and the stress in the sys-
tem. The GP is most often in the
best position to determine con-
textual trouble-signs such as tri-
angulation. When a child becomes
symptomatic, look for triangula-
tion. It tends to be a consistent
characteristic of the Psychoso-
matic Family that is seen not only
with AN but also with other psy-
chosomatic problems.
Conflict avoidance. The family
should be encouraged to support
the sufferer to address, and not
avoid, the conflicts in their life,
to be proactive and assertive in
their relationships.
Conclusion
Family Therapy is a discrete skill set
that requires considerable training
and is effective in the treatment of
AN. As indicated by the RANZCP, the
GP is often the first point of contact
and although he or she is not ex-
pected to conduct family therapy, the
points noted above aim to help en-
hance understanding and improve as-
sessment and treatment. In addition,
the GP may organise other health pro-
fessionals to be involved in the treat-
ment plan,
4
as treatment of AN is best
served by multidisciplinary teams
who can address the medical and psy-
chiatric complexities of this disease.
Nonetheless, the GP remains central
to the medical care and is the key
clinician for oversight prior to and
after psychological interventions. The
family is the true partner and em-
powers the team.
Competing interests
None declared
Key Points
Encourage family partnership
Beware triangulation
Beware conflict avoidance
Many of the tenets of
the Psychosomatic
Family Model serve to
instruct the GP to assess
and intervene with
families of AN patients
WARNING
The Food and Drug Administration (FDA)
in 2004 concluded that children and
adolescents taking antidepressants had
elevated risks for suicidal thoughts or
attempts.
8
Continuing Medical Education
266 Volume 33 Number 4, August 2006
References
1. McDaniel S, Campbell T, Hepworth J, Lorenz A. Family-ori-
ented primary care. 2nd ed. New York: Springer Science and
Business Media; 2005.
2. Beumont P, Hay P, Beumont D, Birmingham L, Derham H, Jor-
dan A, et al. Australian and New Zealand clinical practice guide-
lines for the treatment of anorexia nervosa. A N Z J Psychiatry
2004; 38(9):659-70.
3. Vitiello B, Lederhendler I. Research on eating disorders: Current
status and future prospects. Biol Psychiatry 2000; 47(9):777-86.
4. Royal Australian and New Zealand College of Psychiatrists. Ano-
rexia nervosa: Treatment guide for consumers and carers. New
South Wales: Royal Australian and New Zealand College of Psy-
chiatrists; 2003.
5. National Institute for Health and Clinical Excellence. National
guideline Complete summary. Available at: URL:http://
www.guideline.gov/summary/pdf.aspx?doc_id=5066&stat=
1&string=. Accessed May 20, 2006.
6. Yager J, Andersen A, Devlin M, Egger H, Herzog D, Mitchell J,
et al. Practice guideline for the treatment of patients with eating
disorders. 2nd ed. Washington, DC: American Psychiatric Asso-
ciation; 2000.
7. Dare C, Eisler I, Russell G, Treasure J, Dodge L. Psychological
therapies for adults with anorexia nervosa: Randomised controlled
trial of out-patient treatments. Brit J Psychiatry 2001; 178:216-21.
8. Dubovsky S. Do antidepressants increase suicidality in younger
patients? Journal Watch Psychiatry 2006; 12(5):44-51.
9. Wells JE, Bushnell J A, Hornblow AR. Christchurch epidemiology
study part 1: Methodology and lifetime prevalence for specific
psychiatric disorders. A N Z J Psychiatry 1989; 23(3):315-26.
10. Russell JD, Beumont PJV. Risk and prevention in eating disor-
ders. In: Raphael B, Burrows G, editors. Handbook of Studies on
Preventive Psychiatry. Amsterdam: Elsevier; 1995.
11. Bushnell J. Eating disorders. In: Ellis PM, Collings SCD, editors.
Public health report number 3: Mental health in New Zealand
from a public health perspective. Wellington: Public Health
Group-Ministry of Health; 1997.
12. Gordon RA. Eating disorders: Anatomy of a social epidemic.
2nd ed. Oxford: Blackwell Publishers; 2000.
13. Fairburn CG. Evidence-based treatment of anorexia nervosa. Int
J Eat Disord 2005; 37(S1):S26-S30.
14. Attia E, Schroeder L. Pharmacologic treatment of anorexia nervosa:
Where do we go from here? Int J Eat Disord 2005; 37(S1):S60-S63.
15. Kaye WH, Nagata T, Weltzin TE, Hsu LKG, Sokol MS, McConaha
C, et al. Double-blind placebo-controlled administration of
fluoxetine in restricting- and restricting-purging-type anorexia
nervosa. Biol Psychiatry 2001; 49(7):644-52.
16. Russell GFM, Szmukler GI, Dare C, Eisler I. An evaluation of
family therapy in anorexia nervosa and bulimia nervosa. Arch
Gen Psychiatry 1987; 44:104756.
17. Channon S, De Silva WP, Helmsley D, Perkins RE. A controlled
trial of cognitive-behavioural and behavioural treatment of ano-
rexia nervosa. Behav Res Ther 1989; 27:529-35.
18. Minuchin S. Families & Family Therapy. London: Tavistock
Publications; 1974.
19. Martin FE. The treatment and outcome of anorexia nervosa in
adolescence: Prospective study and five year follow-up. J
Psychiatr Res 1985; 19:509-14.
20. Dare C, Eisler I, Colahan M, Crowther C, Senior R, Asen E. The
listening heart and the chi square: Clinical and empirical percep-
tions in the family therapy of anorexia nervosa. Journal of Fam-
ily Therapy. Special Issue: Eating disorders 1995; 17(1):31-57.
Continuing Medical Education
Вам также может понравиться
- Summary of The Obesity Code: Unlocking the Secrets of Weight Loss (Why Intermittent Fasting Is the Key to Controlling Your Weight) | A Guide To Dr. Jason Fung's BookОт EverandSummary of The Obesity Code: Unlocking the Secrets of Weight Loss (Why Intermittent Fasting Is the Key to Controlling Your Weight) | A Guide To Dr. Jason Fung's BookОценок пока нет
- 222Документ7 страниц222Erl DrizОценок пока нет
- Eating Disorders: Anorexia Nervosa, Bulimia Nervosa, and Binge EatingДокумент14 страницEating Disorders: Anorexia Nervosa, Bulimia Nervosa, and Binge EatingmahaОценок пока нет
- Dissociation, Abuse and The Eating Disorders: Evidence From An Australian PopulationДокумент8 страницDissociation, Abuse and The Eating Disorders: Evidence From An Australian PopulationCoordinacionPsicologiaVizcayaGuaymasОценок пока нет
- Research Paper Over Eating DisordersДокумент6 страницResearch Paper Over Eating Disordersafeartslf100% (1)
- TreasureДокумент21 страницаTreasureAndrea EspinosaОценок пока нет
- Sample Research Paper On Eating DisordersДокумент8 страницSample Research Paper On Eating Disorderst1tos1z0t1d2100% (1)
- Jrsocmed00123 0041Документ5 страницJrsocmed00123 0041Estefania AraqueОценок пока нет
- Research Paper Thesis On Eating DisordersДокумент6 страницResearch Paper Thesis On Eating Disordersp0zikiwyfyb2100% (1)
- Research Paper On Anorexia NervosaДокумент6 страницResearch Paper On Anorexia Nervosasacjvhbkf100% (1)
- ReconceptuALIZING AnДокумент8 страницReconceptuALIZING AnloloasbОценок пока нет
- Anorexia Nervosa Patient Centered CareДокумент4 страницыAnorexia Nervosa Patient Centered Careapi-315748471100% (1)
- Strong Thesis Statement On Anorexia Nervosa and Bulimia and The MediaДокумент4 страницыStrong Thesis Statement On Anorexia Nervosa and Bulimia and The Mediabk4pfxb7100% (1)
- Literature Review Anorexia NervosaДокумент4 страницыLiterature Review Anorexia Nervosac5p6e5z1100% (1)
- Thesis Statement For Research Paper On Eating DisordersДокумент8 страницThesis Statement For Research Paper On Eating Disordersdanaybaronpembrokepines100% (2)
- Am J Psychiatry 2013 May 170-5 - 6 EnigmaticДокумент8 страницAm J Psychiatry 2013 May 170-5 - 6 EnigmaticKarla MenaresОценок пока нет
- Anorexia Literature ReviewДокумент5 страницAnorexia Literature Reviewdafobrrif100% (1)
- Research Methods in Social SciencesДокумент9 страницResearch Methods in Social SciencesNesrin MemedОценок пока нет
- Authors: Joellen Watson Hawkins: A B B B CДокумент4 страницыAuthors: Joellen Watson Hawkins: A B B B Cविजय सिंह धानकОценок пока нет
- Gangguan Makan Pada ObesitasДокумент13 страницGangguan Makan Pada ObesitasDiaa NagitaaОценок пока нет
- Nihms 962269Документ12 страницNihms 962269api-582051116Оценок пока нет
- Midwifery Dissertation Eating DisordersДокумент5 страницMidwifery Dissertation Eating DisordersPaperWritingHelpOnlineUK100% (1)
- Recent Research AnДокумент9 страницRecent Research AnloloasbОценок пока нет
- Research Paper Bulimia NervosaДокумент4 страницыResearch Paper Bulimia Nervosaefjk5y50100% (1)
- Binge Eating Disorder ANNAДокумент12 страницBinge Eating Disorder ANNAloloasbОценок пока нет
- Anorexia Research Paper ExampleДокумент4 страницыAnorexia Research Paper Examplevvgnzdbkf100% (3)
- Research Paper Eating DisordersДокумент7 страницResearch Paper Eating DisordersjppawmrhfОценок пока нет
- Anorexia Nervosa Handbook ChapterДокумент17 страницAnorexia Nervosa Handbook ChapterOchaОценок пока нет
- Scientific Article June 2012Документ12 страницScientific Article June 2012ahgirl93Оценок пока нет
- Anorexia Nervosa Research PaperДокумент8 страницAnorexia Nervosa Research Paperb0pitekezab2Оценок пока нет
- Writing A Research Paper On Eating DisordersДокумент7 страницWriting A Research Paper On Eating Disordersafnkyarofeepzh100% (1)
- Anorexia NervosaДокумент9 страницAnorexia NervosaDouglas SantosОценок пока нет
- SchizophreniaДокумент10 страницSchizophreniadickaОценок пока нет
- Bulimia Nervosa in Adolescents - Prevalence and Treatment ChallengesДокумент6 страницBulimia Nervosa in Adolescents - Prevalence and Treatment ChallengesCamila CesteroОценок пока нет
- Research Clinical 1 1Документ18 страницResearch Clinical 1 1api-459656816Оценок пока нет
- Anorexia Paper ThesisДокумент6 страницAnorexia Paper ThesisBestPaperWritersKansasCity100% (2)
- Research Paper Eating Disorders Thesis StatementДокумент5 страницResearch Paper Eating Disorders Thesis Statementgtkyxjiig100% (1)
- Nutrition and Childhood ObesityДокумент8 страницNutrition and Childhood ObesityErick MuthengiОценок пока нет
- Bulimia Nervosa Research PaperДокумент8 страницBulimia Nervosa Research Paperfznn7hzd100% (1)
- Eating ProblemsДокумент4 страницыEating ProblemsximerodriguezcОценок пока нет
- Rakel: Textbook of Family Medicine, 7th Ed.Документ4 страницыRakel: Textbook of Family Medicine, 7th Ed.Nicolás Rojas MontenegroОценок пока нет
- Eating ProblemsДокумент4 страницыEating ProblemsNicolás Rojas MontenegroОценок пока нет
- Running Head: ABNORMAL PSYCHOLOGY 1Документ6 страницRunning Head: ABNORMAL PSYCHOLOGY 1Brittany JacksonОценок пока нет
- Bulimia Research Paper OutlineДокумент6 страницBulimia Research Paper Outlinefyt18efeОценок пока нет
- Running Head: Treatment Options For Anorexia Nervosa 1Документ7 страницRunning Head: Treatment Options For Anorexia Nervosa 1Khawar AzizОценок пока нет
- 논문원문Документ7 страниц논문원문Donghee LeeОценок пока нет
- Argumentative Research Paper On Eating DisordersДокумент8 страницArgumentative Research Paper On Eating Disordersh01xzacm100% (1)
- Nejm AnorexiaДокумент9 страницNejm AnorexiaRodrigo EstebanОценок пока нет
- 10 1002@eat 23236Документ12 страниц10 1002@eat 23236LucíaОценок пока нет
- Anorexia Nervosa Thesis StatementДокумент6 страницAnorexia Nervosa Thesis StatementPaperWritingServicesOnlineCanada100% (1)
- Iaedp Research Summaries 3 FinalДокумент6 страницIaedp Research Summaries 3 Finalapi-250253869Оценок пока нет
- Bulimia Research Paper TopicsДокумент7 страницBulimia Research Paper Topicsfvfpvgph100% (1)
- Update On Binge EatingДокумент12 страницUpdate On Binge EatingloloasbОценок пока нет
- Research Paper On Eating Disorders Thesis StatementДокумент5 страницResearch Paper On Eating Disorders Thesis StatementafnknohvbbcpbsОценок пока нет
- Thesis Statement For Eating Disorder Research PaperДокумент5 страницThesis Statement For Eating Disorder Research PaperFaith Brown100% (1)
- Term Paper Eating DisordersДокумент7 страницTerm Paper Eating Disordersea442225100% (1)
- Incidence, Prevalence and Mortality of Anorexia Nervosa and Bulimia NervosaДокумент10 страницIncidence, Prevalence and Mortality of Anorexia Nervosa and Bulimia NervosaElisabet BautistaОценок пока нет
- Eating Disorders CPGДокумент62 страницыEating Disorders CPGLuis Pablo HsОценок пока нет
- Thesis Anorexia NervosaДокумент7 страницThesis Anorexia Nervosaafjrtdoda100% (1)
- UCOL Nursing Textbook List 2015dsfefeefefeДокумент5 страницUCOL Nursing Textbook List 2015dsfefeefefeverghese17Оценок пока нет
- Updated Service Pamphlet 24 (2) .10.06Документ9 страницUpdated Service Pamphlet 24 (2) .10.06verghese17Оценок пока нет
- Abdominal Assessment 1Документ12 страницAbdominal Assessment 1verghese17Оценок пока нет
- Early Psychosis DeclarationДокумент6 страницEarly Psychosis Declarationverghese17Оценок пока нет
- NMPSS 2007 - Bennett Et AlДокумент10 страницNMPSS 2007 - Bennett Et Alverghese17Оценок пока нет
- Guide To Mental Health ActДокумент87 страницGuide To Mental Health Actverghese17Оценок пока нет
- الانوركسيا و العلاج الاسريДокумент5 страницالانوركسيا و العلاج الاسريPsych NotesОценок пока нет
- BN Booklist - S2 2014 - Year 2Документ1 страницаBN Booklist - S2 2014 - Year 2verghese17Оценок пока нет
- Wpa 040142Документ5 страницWpa 040142verghese17Оценок пока нет
- Bowers Anderson 2007 CBT Eating DisordersДокумент13 страницBowers Anderson 2007 CBT Eating Disordersverghese17Оценок пока нет
- Mond 2010klkoojljljlДокумент20 страницMond 2010klkoojljljlverghese17Оценок пока нет
- 01 0071 0128757 00 - Statement - 2014 08 14 PDFДокумент1 страница01 0071 0128757 00 - Statement - 2014 08 14 PDFverghese17Оценок пока нет
- Psychotherapeutic Treatment For Anorexia Nervosa: Modernist, Structural Treatment Approaches, and A Post-Structuralist PerspectiveДокумент45 страницPsychotherapeutic Treatment For Anorexia Nervosa: Modernist, Structural Treatment Approaches, and A Post-Structuralist Perspectiveverghese17Оценок пока нет
- HC Sample A Pa PaperДокумент9 страницHC Sample A Pa Paperverghese17Оценок пока нет
- Volk PrizepaperДокумент12 страницVolk Prizepaperverghese17Оценок пока нет
- MOH Submission On Eating Disorder Services 140607 Final VersionДокумент18 страницMOH Submission On Eating Disorder Services 140607 Final Versionverghese17Оценок пока нет
- Revised BSC NДокумент218 страницRevised BSC Nverghese17Оценок пока нет
- 7 Gestational DiabetesДокумент2 страницы7 Gestational Diabetesverghese17Оценок пока нет
- Pre Test Annotated Answer KeyfhfghhhДокумент4 страницыPre Test Annotated Answer Keyfhfghhhverghese17Оценок пока нет
- Rajiv Gandhi University of Health Sciences, Karnataka: 4 T' Block, Jayanagar, Bangalore - 560 041Документ4 страницыRajiv Gandhi University of Health Sciences, Karnataka: 4 T' Block, Jayanagar, Bangalore - 560 041verghese17Оценок пока нет
- Fitness To PractiseДокумент5 страницFitness To Practiseverghese17Оценок пока нет
- Brief Cognitive-Behavioral Therapy For Weight Loss in Midlife Women: A Controlled Study With Follow-UpДокумент9 страницBrief Cognitive-Behavioral Therapy For Weight Loss in Midlife Women: A Controlled Study With Follow-Upverghese17Оценок пока нет
- WedeghjgtjhykjДокумент1 страницаWedeghjgtjhykjverghese17Оценок пока нет
- READING TESTS: MULTIPLE CHOICE QUESTIONSДокумент3 страницыREADING TESTS: MULTIPLE CHOICE QUESTIONSverghese17Оценок пока нет
- READING TESTS: MULTIPLE CHOICE QUESTIONSДокумент3 страницыREADING TESTS: MULTIPLE CHOICE QUESTIONSverghese17Оценок пока нет
- AuthorsДокумент8 страницAuthorsHector MartinezОценок пока нет
- 2 Case StudyДокумент8 страниц2 Case Studysehrish khawerОценок пока нет
- Exercise C: Cocurrent and Countercurrent FlowДокумент6 страницExercise C: Cocurrent and Countercurrent FlowJuniorОценок пока нет
- 10CV54 Unit 05 PDFДокумент21 страница10CV54 Unit 05 PDFvinodh159Оценок пока нет
- Networks Lab Assignment 1Документ2 страницыNetworks Lab Assignment 1006honey006Оценок пока нет
- KCL Thesis PrintingДокумент4 страницыKCL Thesis PrintingMelinda Watson100% (2)
- Ace3 1122.03 GB PDFДокумент16 страницAce3 1122.03 GB PDFArpit VermaОценок пока нет
- Earth and Beyond PDFДокумент5 страницEarth and Beyond PDFNithyananda Prabhu100% (1)
- Gamma World Character SheetДокумент1 страницаGamma World Character SheetDr8chОценок пока нет
- Optimum Work Methods in The Nursery Potting ProcessДокумент107 страницOptimum Work Methods in The Nursery Potting ProcessFöldi Béla100% (1)
- Lte Numbering and AddressingДокумент3 страницыLte Numbering and AddressingRoderick OchiОценок пока нет
- Löwenstein Medical: Intensive Care VentilationДокумент16 страницLöwenstein Medical: Intensive Care VentilationAlina Pedraza100% (1)
- Classification of Methods of MeasurementsДокумент60 страницClassification of Methods of MeasurementsVenkat Krishna100% (2)
- Ohta, Honey Ren R. - Activity 7.2 (Reflection Agriculture and Religion)Документ5 страницOhta, Honey Ren R. - Activity 7.2 (Reflection Agriculture and Religion)honey ohtaОценок пока нет
- Efficient Power Supply for Inductive LoadsДокумент7 страницEfficient Power Supply for Inductive LoadsMary AndersonОценок пока нет
- Pic Attack1Документ13 страницPic Attack1celiaescaОценок пока нет
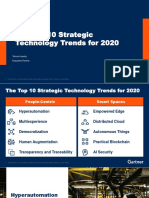
- The Top 10 Strategic Technology Trends For 2020: Tomas Huseby Executive PartnerДокумент31 страницаThe Top 10 Strategic Technology Trends For 2020: Tomas Huseby Executive PartnerCarlos Stuars Echeandia CastilloОценок пока нет
- C++ Programmierung (Benjamin Buch, Wikibooks - Org)Документ257 страницC++ Programmierung (Benjamin Buch, Wikibooks - Org)stefano rossiОценок пока нет
- Developmen of Chick EmbryoДокумент20 страницDevelopmen of Chick Embryoabd6486733Оценок пока нет
- Clinical Indications, Treatment and Current PracticeДокумент14 страницClinical Indications, Treatment and Current PracticefadmayulianiОценок пока нет
- 8086 Microprocessor: J Srinivasa Rao Govt Polytechnic Kothagudem KhammamДокумент129 страниц8086 Microprocessor: J Srinivasa Rao Govt Polytechnic Kothagudem KhammamAnonymous J32rzNf6OОценок пока нет
- Costos estándar clase viernesДокумент9 страницCostos estándar clase viernesSergio Yamil Cuevas CruzОценок пока нет
- Lay Out New PL Press QltyДокумент68 страницLay Out New PL Press QltyDadan Hendra KurniawanОценок пока нет
- Galley cleaning hazards and controlsДокумент9 страницGalley cleaning hazards and controlsRosalie RosalesОценок пока нет
- Case Presentation - Bipolar Affective Disorder 2Документ73 страницыCase Presentation - Bipolar Affective Disorder 2Hemant's galaxy All is hereОценок пока нет
- Twitch V CruzzControl CreatineOverdoseДокумент19 страницTwitch V CruzzControl CreatineOverdoseAndy ChalkОценок пока нет
- Type of PoemДокумент10 страницType of PoemYovita SpookieОценок пока нет
- Newton Raphson Method MCQДокумент15 страницNewton Raphson Method MCQmd junaidОценок пока нет
- BE 510 Business Economics 1 Problem Set 5 SolutionsДокумент5 страницBE 510 Business Economics 1 Problem Set 5 SolutionsCreative Work21stОценок пока нет
- Chapter 04Документ3 страницыChapter 04gebreОценок пока нет
- Parenteral NutritionДокумент78 страницParenteral NutritionImen YunieОценок пока нет