Академический Документы
Профессиональный Документы
Культура Документы
14 0155
Загружено:
Mark Reinhardt0 оценок0% нашли этот документ полезным (0 голосов)
3 просмотров4 страницыsource: cdc.gov
Оригинальное название
14-0155
Авторское право
© © All Rights Reserved
Доступные форматы
PDF, TXT или читайте онлайн в Scribd
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документsource: cdc.gov
Авторское право:
© All Rights Reserved
Доступные форматы
Скачайте в формате PDF, TXT или читайте онлайн в Scribd
0 оценок0% нашли этот документ полезным (0 голосов)
3 просмотров4 страницы14 0155
Загружено:
Mark Reinhardtsource: cdc.gov
Авторское право:
© All Rights Reserved
Доступные форматы
Скачайте в формате PDF, TXT или читайте онлайн в Scribd
Вы находитесь на странице: 1из 4
Emerging Infectious Diseases www.cdc.gov/eid Vol. 20, No.
7, July 2014 1199
Severe Malaria
Not Responsive
to Artemisinin
Derivatives in Man
Returning from
Angola to Vietnam
Nguyen Van Hong, Alfred Amambua-Ngwa,
Nguyen Quang Tuan, Do Duy Cuong,
Nguyen Thi Huong Giang, Nguyen Van Dung,
Ta Thi Tinh, Nguyen Van Tien,
Bui Quang Phuc, Tran Thanh Duong,
Anna Rosanas-Urgell, Umberto DAlessandro,
Jean-Pierre Van Geertruyden, and Annette Erhart
Resistance to artemisinin derivatives, the most potent
antimalarial drugs currently used, has emerged in Southeast
Asia and threatens to spread to Africa. We report a case of
malaria in a man who returned to Vietnam after 3 years in
Angola that did not respond to intravenous artesunate and
clindamycin or an oral artemisinin-based combination.
A
rtemisinin derivatives are used in combination with
other drugs for treatment of Plasmodium falciparum
malaria. Nevertheless, P. falciparum resistance to artemisi-
nins has been recently detected in 4 countries (Cambodia,
Thailand, Myanmar, and Vietnam) in the Greater Mekong
subregion in Southeast Asia (1). Artemisinin resistance
could spread from these countries to other regions, includ-
ing sub-Saharan Africa, where the incidence of malaria is
highest, and where artemisinin resistance would have dev-
astating consequences. Increased and uncontrolled travel
between Asia and Africa might contribute to the spread of
artemisinin-resistant malaria parasites.
An estimated 40,000 Vietnamese workers travel annu-
ally to Angola (2), where P. falciparum malaria is the lead-
ing cause of illness and death (3,4). Over the past year, an
increasing number of severe malaria cases have been identi-
fed among Vietnamese migrants returning from Angola (5).
During Marchmid-April 2013, fve deaths from malaria
among Vietnamese workers in Angola were reported (68).
We report a case of malaria in a Vietnamese man who re-
turned from Angola and did not respond to intravenous arte-
sunate or oral artemisinin-based combination therapy.
The Study
In April 2013, a 58-year-old Vietnamese man was ad-
mitted to Bach Mai Hospital in Hanoi, Vietnam, because
of high fever, jaundice, and lack of consciousness. Eleven
days before hospitalization, he had returned from Saurimo
City in Angola, where he had been working in the con-
struction industry for the past 3 years, to his home village
in malaria-free Nam Dinh Province, 80 km from Hanoi.
Four days after returning from Angola, he reported fatigue,
fever with chills, and a cough. Two days later, he went to
the local district hospital where he was given a diagnosis
of bronchitis and received a third-generation cephalosporin
(cefxime) and antipyretics for 3 days. Ten days after his
arrival in Vietnam, the patient came to the emergency de-
partment of Bach Mai Hospital because of continuous high
fever (body temperature 39C40C), dyspnea, and urinary
incontinence. He was given fosfomycin for pyelonephritis.
Because his clinical condition worsened rapidly, the
patient was transferred the next day to the Infectious Dis-
eases Department in the same hospital because cerebral
malaria was diagnosed. At admission to the department,
the patient (weight 58 kg) was in a confused state and had
a Glasgow coma score of 13/15, generalized convulsions,
jaundice, and tachypnea (respiration rate 25 breaths/min),
a body temperature of 38.5C, a blood pressure of 130/80
mm Hg, and pulse rate of 121 beats/min. Clinical examina-
tion detected hepatomegaly and cracklings in both lungs.
Blood tests showed the following results: leukocyte count
13.3 10
9
cells/L, hemoglobin 15.3 g/L, platelet count 20.9
10
9
/L, blood urea nitrogen 19.8 mmol/L, serum creatinine
135 mmol/L, aspartate aminotransferase 125 IU/L, alanine
aminotransferase 45 IU/L, C-reactive protein 16 mg/L, pro-
calcitonin >120 ng/mL; total bilirubin 116 mol/L; direct
bilirubin 11.5 mol/L; and standard levels of electrolytes.
Parasite density/microliter of blood was calculated
after counting the total number of P. falciparum tropho-
zoites/200 leukocytes and assuming a leukocyte concentra-
tion of 8,000 cells/L. Microscopy identifed P. falciparum
trophozoites at a concentration of 378,470/L and some
schizonts. A chest radiograph showed bilateral pneumonia.
Analysis of cerebrospinal fuid and a computed tomograph-
ic scan of the brain showed standard results. Tests results
for HIV and hepatitis B surface antigen were negative.
The patient was given a diagnosis of P. falciparum
cerebral malaria and treated with intravenous (IV) arte-
sunate (batch no. 511004; Pharbaco, Hanoi, Vietnam) (60
mg every 12 h, loading dose 120 mg at admission) and IV
Author affliations: National Institute of Malariology, Parasitology
and Entomology, Hanoi, Vietnam (N. Van Hong, T.T. Tinh, B.Q.
Phuc, T.T. Duong); Institute of Tropical Medicine, Antwerp,
Belgium (N. Van Hong, A. Rosanas-Urgell, A. Erhart); and Univer-
sity of Antwerp, Antwerp (N. Van Hong, J.-P. Van Geertruyden);
Medical Research Unit, Fajara,. The Gambia (A. Amambua-Ngwa,
U. DAlessandro); and Bach Mai Hospital, Hanoi (N.Q. Tuan, D.D.
Cuong, N.T.H. Giang, N. Van Dung, N. Van Tien)
DOI: http://dx.doi.org/10.3201/eid2007.140155
1200 Emerging Infectious Diseases www.cdc.gov/eid Vol. 20, No. 7, July 2014
clindamycin (600 mg every 12 h). After 24 h of hospitaliza-
tion, the patient had a Glasgow coma score of 11, a body
temperature of 39.7C, and a parasite density of 329,411
parasites/L (Figure 1), a blood pressure of 70/40 mm Hg,
and a respiration rate of 30 breaths/min. An ultrasound ex-
amination showed hepatomegaly and bilateral pleural ef-
fusion. At day 2 of hospitalization, the patient was treated
with intubation and mechanical ventilation. At day 4, the
hemoglobin level had decreased to 9.3 g/dL and the patient
was given a blood transfusion. After 5 consecutive days of
treatment with IV artesunate and clindamycin, the patient
remained comatose and had continuous fever (39C) and
high parasite density (148,000 parasites/L).
At day 6 of hospitalization, artesunate and clindamy-
cin were discontinued, and oral treatment with dihydroar-
temisinin (40 mg/tablet)/piperaquine (320 mg/tablet) was
administered through a nasogastric tube for 3 days (4 tab-
lets/day the frst day, then 2 tablets/day). After 3 days of
treatment, the patient was still febrile (38.5C) and had
a Glasgow coma score of 12 and a parasite density of
113,409 parasites/L (Figure 1). Quinine (1,750 mg/day)
and doxycycline (200 mg/day) were then administered at
day 9 through a nasogastric tube (injectable quinine was
not available). Twelve hours after the frst dose of quinine,
parasite density was 55,558 parasites/L. It decreased to
9,668 parasites/L 72 h at day 11 after starting quinine
treatment, when fever eventually subsided. Two days later,
the patient regained consciousness, and at day 15 of hospi-
talization, blood slides were negative for parasites (Figure
1). The patient eventually recovered and was discharged 35
days after admission.
Species-specifc PCR (9) of a blood sample obtained on
day 3 of hospitalization confrmed the diagnosis of P. falci-
parum monoinfection. Further genotyping by using nested
PCR (merozoite surface proteins 1 and 2 repeat markers)
and capillary electrophoresis (10) of several flter paper
blood spots obtained during the 23 days of hospitalization
confrmed that the patient had a polyclonal P. falciparum in-
fection with 2 clones. These clones might have persisted
from admission through day 10 of hospitalization (Figure 2).
The quality of IV artesunate used was determined by
using high-performance liquid chromatography according
to USP34 NF29 specifcations at the National Institute of
Drug Quality Control (Hanoi, Vietnam) (http://nidqc.org.
vn/). The drug was found to be acceptable.
Conclusions
This clinical case of suspected artemisinin resistance
originating from sub-Saharan Africa is of concern be-
cause the patient had probably been infected in Angola
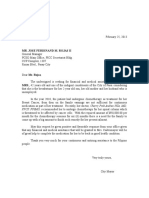
Figure 1. Evolution of Plasmodium
falciparum parasite density
(log scale) by day after start of
antimalaria treatments for man
with severe malaria who returned
from Angola to Vietnam in April
2013. Values are parasites/
microliter of blood. IV, intravenous.
DISPATCHES
Emerging Infectious Diseases www.cdc.gov/eid Vol. 20, No. 7, July 2014 1201
Severe Malaria Not Responsive to Artemisinin
and because the clinical presentation differed from de-
layed parasite clearance reported in Southeast Asia (1).
The patient had never had malaria and had worked con-
tinuously in Angola for the past 3 years before his return
(direct fight to Hanoi and then directly by car to his home
village) to a malaria-free area in Vietnam. Given the on-
set of symptoms only 4 days after his return, the patient
was most likely infected in Luanda Sul Province, Angola,
to which malaria is hyperendemic and where Vietnamese
workers have reportedly died of malaria (68).
Five days of treatment with intravenous artesunate and
clindamycin and a 3-day regimen of dihydroartemisinin/
piperaquine did not clear the infection because parasite
density remained high (>100,000 parasites/L) until the
eighth day of hospitalization. Parasite density showed a
logarithmic decrease only after treatment was changed to
quinine and doxycycline.
An external quality control of all blood slides was per-
formed by an expert microscopist at the National Institute
of Malariology, Parasitology and Entomology in Hanoi;
the parasite densities were confrmed. Therefore, this case
is suggestive of P. falciparum tolerance to artemisinin de-
rivatives. However, because no blood samples for pharma-
cokinetic or in vitro studies were obtained, drug resistance
could not be confrmed.
Identifcation of P. falciparum malaria parasites tolerant
to arteminins raises serious concerns that artemisin-resistant
strains have emerged or spread in Africa. This fnding would
be a major public health disaster and needs to be urgently
confrmed by larger treatment effcacy studies in Angola.
This study was supported by the Belgium Cooperation with-
in the Framework Agreement 3 Program.
Dr Van Hong is a physician, junior scientist, and doctoral
student at the National Institute of Malariology, Parasitology and
Entomology, Hanoi, Vietnam. Her research interests are genetic
diversity and population structure of P. vivax and antimalarial
drug resistance in P. falciparum and P. vivax.
References
1. World Health Organization. Joint assessment of the response to
artemisinin resistance in the greater Mekong sub-region. November
2011February 2012. Summary report [cited 2013 Dec 11]. http://
whothailand.healthrepository.org/bitstream/123456789/1484/3/
120418-Artemisinin-Resistance-in-GMS-SummaryReport.pdf
2. Dan Tri (offcial Journal of the Vietnamese government), 2013.
Vietnamese workers are tempted by high income in Angola.
Intellectuals Magazine. Interview with Prime Minister Le Thanh
Hoa, Deputy Minister of Labour, Invalid and Social Vietnam [cited
2013 Sep 22]. http://dantri.com.vn/xa-hoi/lao-dong-viet-bi-cam-do-
boi-muc-thu-nhap-cao-o-angola-733732.htm.
Figure 2. Clonal complexity of Plasmodium falciparum strain that caused severe malaria in man who returned from Angola to Vietnam
after treatment, as determined by merozoite surface protein 1 (MSP1) and MSP2 repeat length molecular typing. Allele sizes were
detected by capillary electrophoresis of amplifed MSP repeat regions and shown for each follow-up sample.
DISPATCHES
1202 Emerging Infectious Diseases www.cdc.gov/eid Vol. 20, No. 7, July 2014
3. Demographic and Health Surveys. Angola malaria indicators,
survey 2011 [cited 2013 Nov 26]. http://www.measuredhs.com/
what-we-do/survey/survey-display-395.cfm
4. US Agency for International Development. Presidents Malaria
Initiative. (PMI), Country Profle, Angola, April 2013 [cited 2014
Mar 28]. http://www.pmi.gov/countries/profles/angola_profle.pdf
5. Health and Life. Vietnam Ministry of Health. Imported malaria warn-
ing, 2013 [cited 2013 Dec 1]. http://suckhoedoisong.vn/y-te/canh-
bao-sot-ret-ngoai-nhap-khang-thuoc-2013081409111 9352.htm
6. Institute of Malariology, Parasitology and Entomology, Quy Nhon,
Vietnam, 2013. What can be seen from Vietnam workers who died
of malaria in Angola? [cited 2013 Apr 18]. http://www.impe-qn.org.
vn/impe-qn/vn/portal/InfoDetail.jsp?area=58&cat=944&ID=6382
7. Dan Tri (offcial journal of the Vietnamese government). A Viet-
namese worker died of complicated malaria in Angola, 2013 [cited
2013 Aug 14]. http://dantri.com.vn/xa-hoi/them-mot-lao-dong-viet-
tu-vong-vi-sot-ret-ac-tinh-o-angola-742723.htm
8. One more Vietnamese male worker died of malaria in Angola.
Education Magazine, 2013 [cited 2013 Nov 30]. http://giaoduc.net.
vn/Xa-hoi/Phat-hien-them-mot-nam-lao-dong-chet-vi-sot-ret-tai-
Angola/299241.gd
9. Rubio JM, Post RJ, van Leeuwen WM, Henry MC, Lindergard G,
Hommel M. Alternative polymerase chain reaction method to identify
Plasmodium species in human blood samples: the semi-nested multiplex
malaria PCR (SnM-PCR). Trans R Soc Trop Med Hyg. 2002;96(Suppl
1):S199204. http://dx.doi.org/10.1016/S0035-9203(02)90077-5
10. Liljander A, Wiklund L, Falk N, Kweku M, Martensson A,
Felger I, et al. Optimization and validation of multi-coloured cap-
illary electrophoresis for genotying of Plasmodium falciparum
merozoite surface proteins (msp1 and 2). Malar J. 2009;8:78. http://
dx.doi.org/10.1186/147528758-78.
Address for correspondence: Annette Erhart, Institute of Tropical Medicine,
Nationalestraat155, Antwerp 2000, Belgium; email: aerhart@mrc.gm
Sign up for Twitter and fnd the latest
information about emerging infectious diseases
from the EID journal.
@CDC_EIDjournal
Вам также может понравиться
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeОт EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeРейтинг: 4 из 5 звезд4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreОт EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreРейтинг: 4 из 5 звезд4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItОт EverandNever Split the Difference: Negotiating As If Your Life Depended On ItРейтинг: 4.5 из 5 звезд4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceОт EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceРейтинг: 4 из 5 звезд4/5 (895)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersОт EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersРейтинг: 4.5 из 5 звезд4.5/5 (344)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureОт EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureРейтинг: 4.5 из 5 звезд4.5/5 (474)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)От EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Рейтинг: 4.5 из 5 звезд4.5/5 (121)
- The Emperor of All Maladies: A Biography of CancerОт EverandThe Emperor of All Maladies: A Biography of CancerРейтинг: 4.5 из 5 звезд4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingОт EverandThe Little Book of Hygge: Danish Secrets to Happy LivingРейтинг: 3.5 из 5 звезд3.5/5 (399)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyОт EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyРейтинг: 3.5 из 5 звезд3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)От EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Рейтинг: 4 из 5 звезд4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaОт EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaРейтинг: 4.5 из 5 звезд4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryОт EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryРейтинг: 3.5 из 5 звезд3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnОт EverandTeam of Rivals: The Political Genius of Abraham LincolnРейтинг: 4.5 из 5 звезд4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaОт EverandThe Unwinding: An Inner History of the New AmericaРейтинг: 4 из 5 звезд4/5 (45)
- Implementing Guidelines On The Organisation of Health Clubs (DOH AO 2016-014)Документ13 страницImplementing Guidelines On The Organisation of Health Clubs (DOH AO 2016-014)IanBuluag75% (8)
- Roleplay Discharge PlanningДокумент3 страницыRoleplay Discharge PlanningAnonymous KQKONmD9H100% (1)
- Patrol LP Scenario03 July2021Документ25 страницPatrol LP Scenario03 July2021Mark ReinhardtОценок пока нет
- WW Idaho Power Co. - Natural Gas Plant Cooling Water Draft PermitДокумент27 страницWW Idaho Power Co. - Natural Gas Plant Cooling Water Draft PermitMark ReinhardtОценок пока нет
- H0001Документ2 страницыH0001Mark ReinhardtОценок пока нет
- Sustainability of Idaho's Direct Care Workforce (Idaho Office of Performance Evaluations)Документ80 страницSustainability of Idaho's Direct Care Workforce (Idaho Office of Performance Evaluations)Mark ReinhardtОценок пока нет
- 20221230final Order No 35651Документ5 страниц20221230final Order No 35651Mark ReinhardtОценок пока нет
- MMCP CY2023 Idaho Blue Cross Medicaid ContractДокумент185 страницMMCP CY2023 Idaho Blue Cross Medicaid ContractMark ReinhardtОценок пока нет
- Patrol LP Scenario04 July2021Документ24 страницыPatrol LP Scenario04 July2021Mark ReinhardtОценок пока нет
- 20200206press Release IPC E 18 15Документ1 страница20200206press Release IPC E 18 15Mark ReinhardtОценок пока нет
- The First Rules of Los Angeles Police DepartmentДокумент1 страницаThe First Rules of Los Angeles Police DepartmentMark ReinhardtОценок пока нет
- A Bill: 117 Congress 1 SДокумент22 страницыA Bill: 117 Congress 1 SMark ReinhardtОценок пока нет
- Transitioning Coal Plants To Nuclear PowerДокумент43 страницыTransitioning Coal Plants To Nuclear PowerMark ReinhardtОценок пока нет
- Affidavit Writing Made EasyДокумент6 страницAffidavit Writing Made EasyMark ReinhardtОценок пока нет
- Crime Scene Manual Rev3Документ153 страницыCrime Scene Manual Rev3Mark ReinhardtОценок пока нет
- Bills 113s987rsДокумент44 страницыBills 113s987rsMark ReinhardtОценок пока нет
- NIYSTXДокумент19 страницNIYSTXMark ReinhardtОценок пока нет
- A Bill: 116 Congress 2 SДокумент15 страницA Bill: 116 Congress 2 SMark ReinhardtОценок пока нет
- HJR003Документ1 страницаHJR003Mark ReinhardtОценок пока нет
- City of Boise Housing Bonus Ordinance and Zoning Code Rewrite MemoДокумент11 страницCity of Boise Housing Bonus Ordinance and Zoning Code Rewrite MemoMark ReinhardtОценок пока нет
- NIYSWAДокумент17 страницNIYSWAMark ReinhardtОценок пока нет
- Idaho H0098 2021 SessionДокумент4 страницыIdaho H0098 2021 SessionMark ReinhardtОценок пока нет
- NIYSVAДокумент15 страницNIYSVAMark ReinhardtОценок пока нет
- NIYSTNДокумент5 страницNIYSTNMark ReinhardtОценок пока нет
- NIYSUTДокумент4 страницыNIYSUTMark ReinhardtОценок пока нет
- NIYSVTДокумент4 страницыNIYSVTMark ReinhardtОценок пока нет
- NIYSSCДокумент11 страницNIYSSCMark ReinhardtОценок пока нет
- NIYSPRДокумент7 страницNIYSPRMark ReinhardtОценок пока нет
- NIYSSDДокумент4 страницыNIYSSDMark ReinhardtОценок пока нет
- NIYSWIДокумент8 страницNIYSWIMark ReinhardtОценок пока нет
- NIYSRIДокумент9 страницNIYSRIMark ReinhardtОценок пока нет
- NIYSPAДокумент8 страницNIYSPAMark ReinhardtОценок пока нет
- Medical TechnologistДокумент2 страницыMedical Technologistapi-307429612Оценок пока нет
- Lecture 2 - Lower Extremity Venous Ulceration - DR Caitriona Canning PDFДокумент40 страницLecture 2 - Lower Extremity Venous Ulceration - DR Caitriona Canning PDFAlexander EnnesОценок пока нет
- Down SyndromeДокумент20 страницDown SyndromeJessa DiñoОценок пока нет
- Guidelines For The Management of Common Mental DisordersДокумент95 страницGuidelines For The Management of Common Mental DisordersAruna HarikrishnanОценок пока нет
- Hypothyroidism Pregnancy BrochureДокумент2 страницыHypothyroidism Pregnancy BrochureNungky KusumaОценок пока нет
- Telemedicine Seminar HMTI v1.5Документ25 страницTelemedicine Seminar HMTI v1.5PriaTongОценок пока нет
- Er DR Ward ScriptДокумент3 страницыEr DR Ward ScriptChristine Mae MacatangayОценок пока нет
- Project CharterДокумент9 страницProject CharterTatianaObregon100% (1)
- Time - Special Edition - The Future of Medicine, 2023Документ100 страницTime - Special Edition - The Future of Medicine, 2023carlos samboniОценок пока нет
- Segundo - Medical Words - Compound NounsДокумент0 страницSegundo - Medical Words - Compound NounsCarlos Billot AyalaОценок пока нет
- Approach by Health Professionals To The Side Effects of Antihypertensive Therapy: Strategies For Improvement of AdherenceДокумент10 страницApproach by Health Professionals To The Side Effects of Antihypertensive Therapy: Strategies For Improvement of AdherenceSabrina JonesОценок пока нет
- Patient's RightsДокумент7 страницPatient's RightsLorraine RiegoОценок пока нет
- Ki Penyakit RJ WilayahДокумент216 страницKi Penyakit RJ WilayahPhapa Yadien ManggenggulaОценок пока нет
- Risks Factors DFU 1Документ10 страницRisks Factors DFU 1Benny JuntakОценок пока нет
- Sample CollectionДокумент41 страницаSample Collectionsoumen100% (1)
- Journal Club On N Corona VirusДокумент20 страницJournal Club On N Corona VirusNandha KumarОценок пока нет
- Case Study On: Lyceum of The Philippines UniversityДокумент4 страницыCase Study On: Lyceum of The Philippines UniversityarturogarcesjrОценок пока нет
- Mr. Jose Ferdinand M. Rojas Ii: FPCP, FPSMO, Recommended Her To Undergo Chemotherapy For Her Spinal Column WhichДокумент3 страницыMr. Jose Ferdinand M. Rojas Ii: FPCP, FPSMO, Recommended Her To Undergo Chemotherapy For Her Spinal Column Whichglenn padernalОценок пока нет
- Veterinary DiagnosisДокумент2 страницыVeterinary Diagnosissuscripciones.meОценок пока нет
- Patient Specific QA in RT When/How/Analysis: ESMPE European School For Medical Physics ExpertsДокумент3 страницыPatient Specific QA in RT When/How/Analysis: ESMPE European School For Medical Physics ExpertsHidajeta ĐedovićОценок пока нет
- Kaur, Diabetic Autonomic Neuropathy Pathogenesis and Treatment, 2014Документ8 страницKaur, Diabetic Autonomic Neuropathy Pathogenesis and Treatment, 2014elbueno21Оценок пока нет
- Corpus Callosum Lipomas in Children: Original InvestigationДокумент4 страницыCorpus Callosum Lipomas in Children: Original InvestigationHILA GINAОценок пока нет
- Drug Study - AlleyahДокумент10 страницDrug Study - AlleyahLorenzo, Alleyah Jaira D.Оценок пока нет
- Leva FlukeДокумент5 страницLeva FlukeراجيرحمةربهОценок пока нет
- Varicose Veins Diagnosis and TreatmentДокумент7 страницVaricose Veins Diagnosis and Treatmenthossein kasiriОценок пока нет
- Contoh Soal Epilepsy and SeizureДокумент4 страницыContoh Soal Epilepsy and SeizurejumasriОценок пока нет
- NCM 116 - RLE Activity#1 - VALDEZ PDFДокумент6 страницNCM 116 - RLE Activity#1 - VALDEZ PDFDexel Lorren ValdezОценок пока нет
- Diabetes Thesis PDFДокумент4 страницыDiabetes Thesis PDFcynthiawilsonarlington100% (1)