Академический Документы
Профессиональный Документы
Культура Документы
D o Advphys 2
Загружено:
bananaboyjoy0 оценок0% нашли этот документ полезным (0 голосов)
27 просмотров3 страницыReduced elastins due to emphysema causing airway collapse. Reduced elasticity of the lung which increases lung volume. Patient has severe reduction of FEV1 as his observed value is below 40% of the predicted value. Unable to expire adequate amount of air in the first second when compared to the FVC.
Исходное описание:
Оригинальное название
d_o_advphys_2.docx
Авторское право
© © All Rights Reserved
Доступные форматы
DOCX, PDF, TXT или читайте онлайн в Scribd
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документReduced elastins due to emphysema causing airway collapse. Reduced elasticity of the lung which increases lung volume. Patient has severe reduction of FEV1 as his observed value is below 40% of the predicted value. Unable to expire adequate amount of air in the first second when compared to the FVC.
Авторское право:
© All Rights Reserved
Доступные форматы
Скачайте в формате DOCX, PDF, TXT или читайте онлайн в Scribd
0 оценок0% нашли этот документ полезным (0 голосов)
27 просмотров3 страницыD o Advphys 2
Загружено:
bananaboyjoyReduced elastins due to emphysema causing airway collapse. Reduced elasticity of the lung which increases lung volume. Patient has severe reduction of FEV1 as his observed value is below 40% of the predicted value. Unable to expire adequate amount of air in the first second when compared to the FVC.
Авторское право:
© All Rights Reserved
Доступные форматы
Скачайте в формате DOCX, PDF, TXT или читайте онлайн в Scribd
Вы находитесь на странице: 1из 3
1) Reduced elastins due to emphysema causing airway collapse which leads to air
trapping then to hyperinflation (Ferguson. 2006). Another reason could be due to
reduced elasticity of the lung which increases lung volume (Ferguson. 2006).
2) The patient has a very severe reduction of FEV1 as his observed value is below 40%
of the predicted value (White. 2014). This suggests that the patient has a severe
obstructive disease.
The patients has a 64% reduction of FVC, therefore he has a moderate reduction in
FVC (White. 2014). This suggests that the volume of the lungs is decreased possibly
due to a restrictive disease.
The patients FEV1/FVC % ratio is below predicted which suggests that he may have an
obstructive or mixed disease (obstructive and restrictive) (Pellegrino et al. 2005). He is
unable to expire adequate amount of air in the first second when compared to the FVC.
FEF25 is reduced and it represents the mid portion of the airways (small airways) and
this is consistent with an obstructive pattern.
3) The peak expiratory flow (PEF) is reduced due to airway obstruction (Llwellin et al.
2002). The area under curve B is significantly lower than curve A, indicating that the
volume of the lungs is decreased and this could be due to a restrictive disease. There is
also a dip in the curve which represents FEF 25%-75% which is seen in obstructive
diseases (Pellegrino et al. 2005).
4) The spirometry results show that the FEV1, FVC, FEV1/FVC and FEF 25%-75% are
all below the predicted values. The reduced FEV1/FVC indicated that the patient may
be suffering from an obstructive disease (Pellegrino et al. 2005). However, the FVC was
significantly lower than predicted value and the flow volume loop showed a TLC that
was lower than normal, which should not be the case with a solely obstructive disease.
The lower than predicted FVC and lower than normal TLC strongly suggested a mixed
disease (Pellegrino et al. 2005). Due to the patients long history of smoking he is likely
suffering from interstitial lung disease (ILD) (which is the restrictive component) and
Chronic Obstructive Pulmonary Disease (COPD) with characteristics of emphysema
(which is the obstructive component).
The wheezing of the patient is possibly due to the obstructive nature of emphysema.
The hyperinflation seen in the chest x-ray is possibly due to emphysema which is
causing elastin breakdown and reduces alveolar wall integrity. This causes the alveoli to
collapse in expiration causing gas trapping which increases residual volume. Inspiring
ontop of the increased residual volume causes the hyperinflation seen in the x-ray.
The low TLC value observed may possibly be due to pulmonary fibrosis associated with
ILD.
The decreased intensity of breath sounds are commonly seen in patients with
emphysema, this is because there is reduced ventilation due to alveolar destruction.
Relationship between lower than predicted PO
2
and CO
2
and patients shortness
of breath symptoms
The arterial blood gas results showed a lower than predicted PO
2
and higher than
predicted PCO
2
which indicated hypoxemia and hypercapnia respectively. The
hypoxemia and hypercapnia could possibly be related to emphysema. The reduction of
elastin in the alveolar walls in emphysema leads to airspace enlargement in the alveoli
which reduces alveolar capillary exchange area (Stoller & Juvelekian. 2012). These
structural changes lead to the decreased ability of the alveoli to exchange oxygen and
extract CO
2
from the capillaries which causes elevated arterial CO
2
leading to
hypercapnia and lowered arterial O
2
leading to hypoxemia (Stoller & Juvelekian. 2012).
Furthermore, the gas trapping associated with emphysema causes CO
2
retention and
can lead to hypercapnia. Airflow obstruction indicated by the patients severely low
FEV1 also makes expiration very difficult which can also lead to hypercapnia and
shortness of breath symptoms. The patient felt out of breath on minimal exertion. This is
likely because the metabolic demand for O
2
and CO
2
extraction on exertion cannot be
met effectively because there are less functional alveoli and less surface area for gas
exchange.
The progressive shortness of breath over the last 3 years is possibly due to the
progressive narrowing of the patients airways. Studies have shown that in patients with
COPD, terminal bronchiole narrowing precedes the emphysemic destruction of the
alveoli (McDonough et al. 2011). This suggests that the patients alveolar ventilation
may have become progressively worse over time due to the increasing severity of
obstruction in his terminal bronchioles. This interpretation is consistent with the patients
increasing intensity of shortness of breath in the last 3 years.
References
-Ferguson, G.T. 2006, "Why does the lung hyperinflate?", Proceedings of the American
Thoracic Society, vol. 3, no. 2, pp. 176-179.
- White, A 2014, '3014BPS Advanced Physiology Week 10 Lecture: Introduction to
Respiratory Function Testing', Retrieved from Griffith University, School of Natural
Sciences, Learning@Griffith web site: https://bblearn.griffith.edu.au/bbcswebdav/pid-
1120011-dt-content-rid-
3173540_1/courses/3014BPS_3145_NA/Lecture%205%20respiratory%20full%20colour
%20slides.pdf
- Pellegrino, R., Viegi, G., Brusasco, V., Crapo, R.O., Burgos, F., Casaburi, R., Coates,
A., van der Grinten,C P M., Gustafsson, P., Hankinson, J., Jensen, R., Johnson, D.C.,
MacIntyre, N., McKay, R., Miller, M.R., Navajas, D., Pedersen, O.F., Wanger, J.,
Sahlgrenska akademin, Institutionen fr kvinnors och barns hlsa, Sahlgrenska
Academy, University of Gothenburg, Institute for the Health of Women and Children &
Gteborgs universitet 2005, "Interpretative strategies for lung function tests", The
European respiratory journal, vol. 26, no. 5, pp. 948-968.
- Llewellin, P., Sawyer, G., Lewis, S., Cheng, S., Weatherall, M., Fitzharris, P. &
Beasley, R. 2002, "The relationship between FEV1 and PEF in the assessment of the
severity of airways obstruction", Respirology (Carlton, Vic.), vol. 7, no. 4, pp. 333-337.
-Stoller, JK., Juvelekian, G. 2012, Chronic Obstructive Pulmonary Disease, viewed 16
October 2014,
<http://www.clevelandclinicmeded.com/medicalpubs/diseasemanagement/pulmonary/ch
ronic-obstructive-pulmonary-disease/#bib13>
-McDonough, J.E., Yuan, R., Suzuki, M., Seyednejad, N., Elliott, W.M., Sanchez, P.G.,
Wright, A.C., Gefter, W.B., Litzky, L., Coxson, H.O., Par, P.D., Sin, D.D., Pierce, R.A.,
Woods, J.C., McWilliams, A.M., Mayo, J.R., Lam, S.C., Cooper, J.D. & Hogg, J.C. 2011,
"Small-Airway Obstruction and Emphysema in Chronic Obstructive Pulmonary
Disease", The New England journal of medicine, vol. 365, no. 17, pp. 1567-1575.
Вам также может понравиться
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)От EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Рейтинг: 4.5 из 5 звезд4.5/5 (119)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaОт EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaРейтинг: 4.5 из 5 звезд4.5/5 (265)
- The Little Book of Hygge: Danish Secrets to Happy LivingОт EverandThe Little Book of Hygge: Danish Secrets to Happy LivingРейтинг: 3.5 из 5 звезд3.5/5 (399)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryОт EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryРейтинг: 3.5 из 5 звезд3.5/5 (231)
- Never Split the Difference: Negotiating As If Your Life Depended On ItОт EverandNever Split the Difference: Negotiating As If Your Life Depended On ItРейтинг: 4.5 из 5 звезд4.5/5 (838)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeОт EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeРейтинг: 4 из 5 звезд4/5 (5794)
- Team of Rivals: The Political Genius of Abraham LincolnОт EverandTeam of Rivals: The Political Genius of Abraham LincolnРейтинг: 4.5 из 5 звезд4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyОт EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyРейтинг: 3.5 из 5 звезд3.5/5 (2219)
- The Emperor of All Maladies: A Biography of CancerОт EverandThe Emperor of All Maladies: A Biography of CancerРейтинг: 4.5 из 5 звезд4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreОт EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreРейтинг: 4 из 5 звезд4/5 (1090)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersОт EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersРейтинг: 4.5 из 5 звезд4.5/5 (344)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceОт EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceРейтинг: 4 из 5 звезд4/5 (894)
- Abdomen - FRCEM SuccessДокумент275 страницAbdomen - FRCEM SuccessAbin ThomasОценок пока нет
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureОт EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureРейтинг: 4.5 из 5 звезд4.5/5 (474)
- The Unwinding: An Inner History of the New AmericaОт EverandThe Unwinding: An Inner History of the New AmericaРейтинг: 4 из 5 звезд4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)От EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Рейтинг: 4 из 5 звезд4/5 (98)
- Monster of The Week Tome of Mysteries PlaybooksДокумент10 страницMonster of The Week Tome of Mysteries PlaybooksHyperLanceite XОценок пока нет
- Ancient MesopotamiaДокумент69 страницAncient MesopotamiaAlma CayapОценок пока нет
- Antonovsky (1979)Документ280 страницAntonovsky (1979)M.Fakhrul Kurnia100% (1)
- Reiki BrochureДокумент2 страницыReiki BrochureShikha AgarwalОценок пока нет
- Survey Report on Status of Chemical and Microbiological Laboratories in NepalДокумент38 страницSurvey Report on Status of Chemical and Microbiological Laboratories in NepalGautam0% (1)
- Revolutionizing Energy Harvesting Harnessing Ambient Solar Energy For Enhanced Electric Power GenerationДокумент14 страницRevolutionizing Energy Harvesting Harnessing Ambient Solar Energy For Enhanced Electric Power GenerationKIU PUBLICATION AND EXTENSIONОценок пока нет
- Telco XPOL MIMO Industrial Class Solid Dish AntennaДокумент4 страницыTelco XPOL MIMO Industrial Class Solid Dish AntennaOmar PerezОценок пока нет
- Chap 2 Debussy - LifejacketsДокумент7 страницChap 2 Debussy - LifejacketsMc LiviuОценок пока нет
- VA TearDownДокумент5 страницVA TearDownfaj_larcfave5149Оценок пока нет
- 07 Raction KineticsДокумент43 страницы07 Raction KineticsestefanoveiraОценок пока нет
- Feline DermatologyДокумент55 страницFeline DermatologySilviuОценок пока нет
- VivsayamДокумент87 страницVivsayamvalarumsakthi100% (2)
- Draft Initial Study - San Joaquin Apartments and Precinct Improvements ProjectДокумент190 страницDraft Initial Study - San Joaquin Apartments and Precinct Improvements Projectapi-249457935Оценок пока нет
- TutorialДокумент324 страницыTutorialLuisAguilarОценок пока нет
- Evolutionary PsychologyДокумент10 страницEvolutionary PsychologyShreya MadheswaranОценок пока нет
- Cost Analysis and Financial Projections for Gerbera Cultivation ProjectДокумент26 страницCost Analysis and Financial Projections for Gerbera Cultivation ProjectshroffhardikОценок пока нет
- De Thi HSG Tinh Binh PhuocДокумент9 страницDe Thi HSG Tinh Binh PhuocDat Do TienОценок пока нет
- Naukri LalitaSharma (3y 4m)Документ2 страницыNaukri LalitaSharma (3y 4m)rashika asraniОценок пока нет
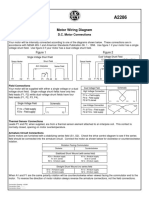
- Motor Wiring Diagram: D.C. Motor ConnectionsДокумент1 страницаMotor Wiring Diagram: D.C. Motor Connectionsczds6594Оценок пока нет
- Organizing Small Items with Glass Bottle OrganizersДокумент70 страницOrganizing Small Items with Glass Bottle OrganizersDy SaiОценок пока нет
- The Art of Now: Six Steps To Living in The MomentДокумент5 страницThe Art of Now: Six Steps To Living in The MomentGiovanni AlloccaОценок пока нет
- Innovative Food Science and Emerging TechnologiesДокумент6 страницInnovative Food Science and Emerging TechnologiesAnyelo MurilloОценок пока нет
- Private Schools Provide Better EducationДокумент2 страницыPrivate Schools Provide Better EducationcitraОценок пока нет
- Idioms & Phrases Till CGL T1 2016Документ25 страницIdioms & Phrases Till CGL T1 2016mannar.mani.2000100% (1)
- ASA 2018 Catalog WebДокумент48 страницASA 2018 Catalog WebglmedinaОценок пока нет
- Design of Fixed Column Base JointsДокумент23 страницыDesign of Fixed Column Base JointsLanfranco CorniaОценок пока нет
- Cyclograph User ManualДокумент15 страницCyclograph User ManualPeter BateОценок пока нет
- ML AiДокумент2 страницыML AiSUYASH SHARTHIОценок пока нет
- STS Chapter 1 ReviewerДокумент4 страницыSTS Chapter 1 ReviewerEunice AdagioОценок пока нет