Академический Документы
Профессиональный Документы
Культура Документы
Who Aria
Загружено:
wilandayu0 оценок0% нашли этот документ полезным (0 голосов)
158 просмотров8 страницARIA oleh WHO
Оригинальное название
WHO ARIA
Авторское право
© © All Rights Reserved
Доступные форматы
PDF, TXT или читайте онлайн в Scribd
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документARIA oleh WHO
Авторское право:
© All Rights Reserved
Доступные форматы
Скачайте в формате PDF, TXT или читайте онлайн в Scribd
0 оценок0% нашли этот документ полезным (0 голосов)
158 просмотров8 страницWho Aria
Загружено:
wilandayuARIA oleh WHO
Авторское право:
© All Rights Reserved
Доступные форматы
Скачайте в формате PDF, TXT или читайте онлайн в Scribd
Вы находитесь на странице: 1из 8
BASED ON THE 2007 ARIA WORKSHOP REPORT AND THE IPAG HANDBOOK
In collaboration with WHO, GA
2
LEN, AllerGen, and Wonca
MANAGEMENT OF
ALLERGIC RHINITIS AND
ITS IMPACT ON ASTHMA
MANAGEMENT OF
ALLERGIC RHINITIS AND
ITS IMPACT ON ASTHMA
POCKET GUIDE
GLOBAL PRIMARY CARE EDUCATION
C
O
P
Y
R
I
G
H
T
E
D
M
A
T
E
R
I
A
L
,
D
O
N
O
T
A
L
T
E
R
O
R
R
E
P
R
O
D
U
C
E
.
THE PURPOSE OF THIS GUIDE
This document was prepared by the Wonca Expert Panel, including Bousquet J, Reid J, Van Weel C, Baena
Cagnani C, Demoly P, Denburg J, Fokkens WJ, Grouse L, Mullol K, Ohta K, Schermer T, Valovirta E, and
Zhong N. It was edited by Dmitry Nonikov. This material is based on the IPAG Handbook and the ARIA
Workshop Report, in collaboration with the World Health Organization, GA
2
LEN (Global Allergy and
Asthma European Network), AllerGen, International Primary Care Respiratory Group (IPCRG), European
Federation of Allergy and Airways Diseases Patients Associations (EFA), and the World Organization of
Family Doctors (Wonca).
Management that follows evidence-based practice guidelines yields better patient results. However, glob-
al evidence-based practice guidelines are often complicated and recommend the use of resources often
not available in the primary care setting worldwide. The joint Wonca/GARD expert panel offers support
to primary care physicians worldwide by distilling the existing evidence based recommendations into this
brief reference guide. The guide lists diagnostic and therapeutic measures that can be carried out world-
wide in the primary care environment and in this way provide the best possible care for patients with aller-
gic rhinitis. The material presented in sections 1-5 will assist you in diagnosing and treating allergic rhini-
tis.
PRIMARY CARE CHALLENGE
Allergic rhinitis is a growing primary care challenge since most patients consult primary care physicians.
General practitioners play a major role in the management of allergic rhinitis as they make the diagnosis,
start the treatment, give the relevant information, and monitor most of the patients. In some countries,
general practitioners perform skin prick tests. Studies in Holland and the UK found that common nasal aller-
gies can be diagnosed with a high certainty using simple diagnostic criteria. Nurses may also play an
important role in the identification of allergic diseases including allergic rhinitis in the primary care of devel-
oping countries and in schools. In addition, many patients with allergic rhinitis have concomitant asthma and
this must be checked.
ALLERGIC RHINITIS RECOMMENDATIONS
1- Allergic rhinitis is a major chronic respiratory disease due to its:
- Prevalence
- Impact on quality-of-life
- Impact on work/school performance and productivity
- Economic burden
- Links with asthma
2- In addition, allergic rhinitis is associated with co-morbidities such as conjunctivitis.
3- Allergic rhinitis should be considered as a risk factor for asthma along with other known risk factors.
4- A new subdivision of allergic rhinitis has been proposed:
- Intermittent (IAR)
- Persistent (PER)
5- The severity of allergic rhinitis has been classified as mild or moderate/severe depending on the
severity of symptoms and quality-of-life outcomes.
6- Depending on the subdivision and severity of allergic rhinitis, a stepwise therapeutic approach has been
proposed.
7- The treatment of allergic rhinitis combines:
- Pharmacotherapy
- Immunotherapy
- Education
8- Patients with persistent allergic rhinitis should be evaluated for asthma by means of a medical
history, chest examination, and, if possible and when necessary, the assessment of airflow
obstruction before and after bronchodilator.
9- Patients with asthma should be appropriately evaluated (history and physical examination) for
rhinitis.
10- Ideally, a combined strategy should be used to treat the upper and lower airway diseases to
optimize efficacy and safety.
1
C
O
P
Y
R
I
G
H
T
E
D
M
A
T
E
R
I
A
L
,
D
O
N
O
T
A
L
T
E
R
O
R
R
E
P
R
O
D
U
C
E
.
ALLERGIC RHINITIS QUESTIONNAIRE
1
Instructions: To evaluate the possibility of allergic rhinitis, start by asking the questions below to patients with nasal symptoms.
This questionnaire contains the questions related to allergic rhinitis symptoms that have been identified in peer-reviewed literature
as having the greatest diagnostic value. It will not produce a definitive diagnosis, but may enable you to determine whether a
diagnosis of allergic rhinitis should be further investigated or is unlikely.
1. Do you have any of the following symptoms?
Symptoms on only one side of your nose Yes No
Yes No
Yes No
Yes No
Yes No
Yes No
Yes No
Yes No
Yes No
Yes No
Yes No
Thick, green or yellow discharge from your nose (see NOTE)
Postnasal drip (down the back of your throat) with thick mucus and/or runny nose (see NOTE)
Question Response Choices
Facial pain (see NOTE)
Recurrent nosebleeds
Loss of smell (see NOTE)
2. Do you have any of the following symptoms for at least one hour on most days (or on most days
during the season if your symptoms are seasonal)?
Watery runny nose
Sneezing, especially violent and in bouts
Nasal obstruction
Nasal itching
Conjunctivitis (red, itchy eyes)
Allergic Rhinitis Questionnaire
ALLERGIC RHINITIS DIAGNOSIS GUIDE
1
I16758&7,216: In patients of all ages with lower nasal symptoms only, whose responses to the Allergic Rhinitis Questionnaire sug-
gest that this diagnosis should be investigated, use this guide to help you evaluate the possibility of allergic rhinitis. All of the diag-
nostic investigations presented in this guide may not be available in all areas; in most cases, the combination of those diagnostic
investigations that are available and the individual health care professionals clinical judgement will lead to a robust clinical
diagnosis. This guide is intended to supplement, not replace, a complete physical examination and thorough medical history.
Physical examination
In persistent rhinitis:
anterior rhinoscopy using speculum and mirror gives
limited but often valuable information
nasal endoscopy (usually performed by specialist) may
be needed to exclude other causes of rhinitis, nasal
polyps, and anatomic abnormalities
Trial of therapy
Allergy skin testing or measurement of allergen-specific
IgE in serum (if symptoms are persistent and/or
moderate/severe, or if quality of life is affected)
Transverse crease of nose, allergic shiners, allergic salute.
Exclusion of other causes.
Improvement with antihistamines or intranasal
glucocorticosteroid.
Confirm presence of atopy.
Specific triggers identified.
D,$*1267,& "22/ F,1',1*6 7+$7 !833257 D,$*126,6
Nasal challenge tests (if occupational rhinitis suspected) Confirm sensitivity to specific triggers.
Allergic Rhinitis Diagnosis Guide
1- RECOGNIZE ALLERGIC RHINITIS
Evaluation:
The symptoms described in Question 1 are usually NOT found in allergic rhinitis. The presence of ANY ONE of them suggests
that alternative diagnoses should be investigated. Consider alternative diagnoses and/or referral to a specialist.
NOTE: Purulent discharge, postnasal drip, facial pain, and loss of smell are common symptoms of sinusitis. Because most
patients with sinusitis also have rhinitis (though not always allergic in origin), in this situation the clinician should also evaluate
the possibility of allergic rhinitis.
The presence of watery runny nose with ONE OR MORE of the other symptoms listed in Question 2 suggests allergic rhinitis,
and indicates that the patient should undergo further diagnostic assessment.
The presence of watery runny nose ALONE suggests that the patient MAY have allergic rhinitis. (Additionally, some patients
with allergic rhinitis have only nasal obstruction as a cardinal symptom.)
If the patient has sneezing, nasal itching, and/or conjunctivitis, but NOT watery runny nose, consider alternative diagnoses
and/or referral to a specialist.
In adults with late-onset rhinitis, consider and query occupational causes. Occupational rhinitis frequently precedes or
accompanies the development of occupational asthma. Patients in whom an occupational association is suspected should be
referred to a specialist for further objective testing and assessment.
2
1
International Primary Care Airways Group (IPAG) Handbook available at www.globalfamilydoctor.com.
C
O
P
Y
R
I
G
H
T
E
D
M
A
T
E
R
I
A
L
,
D
O
N
O
T
A
L
T
E
R
O
R
R
E
P
R
O
D
U
C
E
.
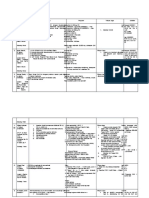
2- DIFFERENTIAL DIAGNOSIS OF ALLERGIC
RHINITIS
2
3- MAKE THE DIAGNOSIS OF ALLERGIC RHINITIS
2
Symptoms suggestive
of allergic rhinitis
Symptoms usually NOT associated
with allergic rhinitis
? 81,/$7(5$/ 6<037206
? 1$6$/ 2%6758&7,21 :,7+287 27+(5 6<037206
? 08&23858/(17 5+,1255+($
? 3267(5,25 5+,1255+($ (3267 1$6$/ '5,3)
?:,7+ 7+,&. 08&286
?$1'/25 12 $17(5,25 5+,1255+($
? 3$,1
? 5(&855(17 (3,67$;,6
? $1260,$
2 25 025( 2) 7+( )2//2:,1* 6<037206 )25
> 1 +5 21 0267 '$<6:
? :$7(5< $17(5,25 5+,1255+($
? 61((=,1*, (63(&,$//< 3$52;<60$/
? 1$6$/ 2%6758&7,21
? 1$6$/ 3585,7,6
> &21-81&7,9,7,6
C/$66,)< $1' $66(66 6(9(5,7<
(6(( 6(&7,21 4)
Symptoms suggestive of allergic rhinitis
A)/!-%*- -$%)*--$!a
S)!!5%)#
Na.a' *b./-0c/%*)
(a) +*..%b'4 */$!- )a.a' *- *c0'a- .4(+/*(.)
P-%(a-4 ca-! S+!c%a'%./
P$a%a/*+ *-
M0'/%-a''!-#!) /!./
N!#a/%1!
R$%)%/%. %. 0)'%&!'4
/* b! a''!-#%c
A''!-#%c -$%)%/%.
N!#a/%1!
N*) a''!-#%c
-$%)%/%.
P*.%/%1!
+ c*--!'a/!
2%/$
.4(+/*(.
A''!-#%c -$%)%/%.
N!#a/%1!
I" ./-*)# .0##!./%*) *"
a''!-#4: +!-"*-( .!-0(
a''!-#!) .+!c%"%c I#E
P*.%/%1!
R$%)%/%. %. '%&!'4 /* b! a''!-#%c.
I" (*-! %)"*-(a/%*) )!!!
*- %((0)*/$!-a+4 /* b!
+-*+*.!
S&%) +-%c& /!./
P*.%/%1!
+ c*--!'a/!
2%/$
.4(+/*(.
t
t
t
t
t
t
t
t
t t
t
t
t
t
t
t
t
R!"!- /$!
+a/%!)/ /*
.+!c%a'%./
3
2
Allergic Rhinitis and its impact on Asthma (ARIA) 2007. Full text ARIA documents and resources: http://www.whiar.org.
C
O
P
Y
R
I
G
H
T
E
D
M
A
T
E
R
I
A
L
,
D
O
N
O
T
A
L
T
E
R
O
R
R
E
P
R
O
D
U
C
E
.
4- CLASSIFY ALLERGIC RHINITIS
2
Intermittent
symptoms
<4 days per week
or <4 consecutive weeks
Mild
all of the following
normal sleep
no impairment of daily activities, sport, leisure
no impairment of work and school
symptoms present but not troublesome
Moderate-Severe
one or more items
sleep disturbance
impairment of daily activities, sport, leisure
impairment of school or work
troublesome symptoms
Persistent
symptoms
>4 days/week
and >4 consecutive weeks
AIA 2007
I17(59(17,21 !A PA PE
$'8/76 &+,/'5(1 $'8/76 &+,/'5(1
O5$/ H1 A17,+,67$0,1( A A A A A
I175$1$6$/ H1 A17,+,67$0,1( A A A A A**
I175$1$6$/ C! A A A A A**
I175$1$6$/ &52021( A A A A
L"A6 A A (>6 <56) A A**
!8%&87$1(286 !I" A A A A A**
!8%/,1*8$/ / 1$6$/ !I" A A A B A**
A//(5*(1 $92,'$1&( D D A* B*
SAR - Seasonal Allergic Rhinitis
PAR - Perennial Allergic Rhinitis
PER - Persistent Allergic Rhinitis
CS - Corticosteroids
LTRAs - Anti-Leukotrienes
SIT - Specific Immunotherapy
*not effective in the general population
**extrapolated from studies in SAR/PAR
STRENGTH OF EVIDENCE FOR EFFICACY OF
RHINITIS TREATMENT
2
5- TREAT ALLERGIC RHINITIS
4
2
Allergic Rhinitis and its impact on Asthma (ARIA) 2007. Full text ARIA documents and resources: www.whiar.org.
"5($70(17 G2$/6
Goals for the treatment of rhinitis assume accurate diagnosis and assessment of severity as well as any link
with asthma in an individual patient. Goals include:
Unimpaired sleep
Ability to undertake normal daily activities, including work and school attendance, without limitation or
impairment, and the ability to participate fully in sport and leisure activities
No troublesome symptoms
No or minimal side-effects of rhinitis treatment
C
O
P
Y
R
I
G
H
T
E
D
M
A
T
E
R
I
A
L
,
D
O
N
O
T
A
L
T
E
R
O
R
R
E
P
R
O
D
U
C
E
.
DIAGNOSIS AND SEVERITY ASSESSMENT OF
ALLERGIC RHINITIS
2
02'(5$7(- 0,/'
6(9(5(
Not in preferred order
*-a' H1-a)/%$%./a(%)!
*- %)/-a)a.a'
H1-a)/%$%./a(%)!
a)/*- !c*)#!./a)/
*- %)/-a)a.a' CS*
*- LTRA**
(*- c-*(*)!)
%" "a%'0-!: ./!+-0+
%" %(+-*1!: c*)/%)0!
"*- 1 (*)/$
Diagnosis of allergic rhinitis
Intermittent
symptoms
0,/'
Not in preferred order
*-a' H1-a)/%$%./a(%)!
*- %)/-a)a.a'
H1-a)/%$%./a(%)!
a)/*- !c*)#!./a)/
*- LTRA**
02'(5$7(
6(9(5(
In preferred order
%)/-a)a.a' CS
H1-a)/%$%./a(%)! *- LTRA**
./!+-*2)
a) c*)/%)0!
/-!a/(!)/
"*- 1 (*)/$
Persistent
symptoms
%)c-!a.! -$%)*--$!a
%)/-a)a.a' CS a %+-a/-*+%0(
*.! %/c$/.)!!5! b'*c&a#!
a H1 a)/%$%./a(%)! a
!c*)#!./a)/
*- *-a' CS
(.$*-/-/!-()
.0-#%ca' -!"!--a'
I) &21-81&7,9,7,6 a:
*-a' H1-a)/%$%./a(%)!
*- %)/-a*c0'a- H1-a)/%$%./a(%)!
*- %)/-a*c0'a- c-*(*)!
(*- .a'%)!)
C216,'(5 63(&,),& ,008127+(5$3<
-!1%!2 /$! +a/%!)/
a"/!- 2-4 2&.
%(+-*1!
"a%'0-!
"a%'0-!
-!1%!2 %a#)*.%.
-!1%!2 c*(+'%a)c!
,0!-4 %)"!c/%*).
*- */$!- ca0.!.
%) +!-.%./!)/ -$%)%/%.
-!1%!2 /$! +a/%!)/
a"/!- 2-4 2!!&.
A''!-#!) a) %--%/a)/ a1*%a)c! (a4 b! a++-*+-%a/!
Check for asthma
especially in
patients with
moderate-severe
and/or persistent
rhinitis
*T*/a' *.! *" /*+%ca' CS .$*0' b! c*).%!-! %"
%)$a'! ./!-*%. a-! 0.! "*- c*)c*(%/a)/ a./$(a
**I) +a-/%c0'a-, %) +a/%!)/. 2%/$ a./$(a
PEDIA"IC A!PEC"!
Allergic rhinitis is part of the "allergic march" during childhood but intermittent allergic rhinitis is unusual before two years
of age. Allergic rhinitis is most prevalent during school age years. In preschool children, the diagnosis of AR is difficult.
In school children and adolescents, the principles of treatment are the same as for adults, but doses may be adapted,
and special care should be taken to avoid the side effects of treatments typical in this age group.
5
2
Allergic Rhinitis and its impact on Asthma (ARIA) 2007. Full text ARIA documents and resources: www.whiar.org.
C
O
P
Y
R
I
G
H
T
E
D
M
A
T
E
R
I
A
L
,
D
O
N
O
T
A
L
T
E
R
O
R
R
E
P
R
O
D
U
C
E
.
GLOSSARY OF RHINITIS MEDICATIONS
1
O5$/ H
1
$17,+,67$0,1(6
H
1
-%/2&.(56
N$0( $1'
A/62 .12:1 $6
G(1(5,& 1$0( M(&+$1,60 2)
$&7,21
!,'( ())(&76 C200(176
21' *(1(5$7,21
Cetirizine
Ebastine
Fexofenadine
Loratadine
Mizolastine
Acrivastine
Azelastine
Mequitazine
N(: 352'8&76
Desloratadine
Levocetirizine
Rupatadine
- blockage of H
1
receptor
- some anti-allergic
activity
- new generation
drugs can be used
once daily
- no development of
tachyphylaxis
21' *(1(5$7,21
- no sedation for
most drugs
- no anti-cholinergic
effect
- no cardiotoxicity
- acrivastine has
sedative effects
- oral azelastine
may induce
sedation and a
bitter taste
- First-line therapy except in
Moderate/ Severe
Persistent Allergic Rhinitis
- 2nd generation oral H
1
-
blockers are preferred for
their favorable efficacy/
safety ratio and pharma-
cokinetics; first generation
molecules are no longer
recommended because of
their unfavorable safety/
efficacy ratio
- Rapidly effective (less than 1hr)
on nasal and ocular symptoms
- Moderately effective on
nasal congestion
* Cardiotoxic drugs
(astemizole, terfenadine)
are no longer marketed in
most countries
L2&$/ H
1
$17,+,67$0,1(6
(,175$1$6$/,
,175$2&8/$5)
Azelastine
Levocabastine
Olopatadine
- blockage of H
1
receptor
- some anti-allergic
activity for azelastine
- Minor local side
effects
- Azelastine: bitter taste
in some patients
Rapidly effective
(less than 30 min)
on nasal or ocular
symptoms
I175$1$6$/
*/8&2&257,&2-
67(52,'6
Beclomethasone
dipropionate
Budesonide
Ciclesonide
Flunisolide
Fluticasone
propionate
Fluticasone furoate
Mometasone furoate
Triamcinolone
acetonide
- potently reduce
nasal inflammation
- reduce nasal
hyperreactivity
- Minor local side
effects
- Wide margin for
systemic side
effects
- Growth concerns
with BDP only
- In young children
consider the
combination of
intranasal and
inhaled drugs
- The most effective
pharmacologic
treatment of allergic
rhinitis; first-line
treatment for
Moderate/ Severe
Persistent Allergic
Rhinitis
- Effective on nasal
congestion
- Effective on smell
- Effect observed after
6-12 hrs but maximal
effect after a few days
- Patients should be
advised on the proper
method of administering
intranasal glucocortico-
steroids, including the
importance of directing
the spray laterally rather
than medially (toward
the septum) in the nose
6- ASSESS POSSIBILITY OF ASTHMA
2
The patient does not know if he
(she) is asthmatic
Patient with a diagnosis of asthma
#6( A67+0$ D,$*126,6 $1' A67+0$ C21752/
Q8(67,211$,5(6 21 AIA :(%6,7( (:::.:+,$5.25*)
4 6,03/( 48(67,216:
? +$9( <28 +$' $1 $77$&. 25 5(&855(17 $77$&.6 2) :+((=,1*?
? '2 <28 +$9( $ 728%/(620( &28*+, (63(&,$//< $7 1,*+7?
? '2 <28 &28*+ 25 :+((=( $)7(5 (;(5&,6(?
? '2(6 <285 &+(67 )((/ 7,*+7?
If YES to any of these questions
<285 3$7,(17 0$< %( $67+0$7,&
N((' )25 $67+0$ (9$/8$7,21
6
1
International Primary Care Airways Group (IPAG) Handbook available at www.globalfamilydoctor.com.
2
Allergic Rhinitis and its impact on Asthma (ARIA) 2007. Full text ARIA documents and resources: www.whiar.org.
C
O
P
Y
R
I
G
H
T
E
D
M
A
T
E
R
I
A
L
,
D
O
N
O
T
A
L
T
E
R
O
R
R
E
P
R
O
D
U
C
E
.
O5$/
'(&21*(67$176
Ephedrine
Phenylephrine
Phenyl-
propanolamine
Pseudoephedrine
Oral H1-
antihistamine-
decongestant
combination
- sympathomimetic
drug
- relieve symptoms
of nasal
congestion
- Hypertension
- Palpitations
- Restlessness
- Agitation
- Tremor
- Insomnia
- Headache
- Dry mucous
membranes
- Urinary retention
- Exacerbation of
glaucoma or
thyrotoxicosis
Use oral decongestants
with caution in patients
with heart disease
O5$/ H1-
$17,+,67$0,1(
'(&21*(67$17
&20%,1$7,21
products may be more
effective than either
product alone but side
effects are combined
I175$1$6$/
'(&21*(67$176
Oxymethazoline
Others
- sympathomimetic
drugs
- relieve symptoms
of nasal
congestion
- Same side effects as
oral decongestants but
less intense
- Rhinitis
medicamentosa
is a rebound pheno-
menon occurring with
prolonged use
(over 10 days)
Act more rapidly and
more effectively than
oral decongestants
Limit duration of
treatment to less than
10 days to avoid
rhinitis medicamentosa
I175$1$6$/
$17,-
&+2/,1(5*,&6
Ipratropium
- anticholinergics block
almost
exclusively
rhinorrhea
- Minor local side
effects
- Almost no systemic
anticholinergic activity
Effective in allergic
and nonallergic
patients with
rhinorrhea
C<6L"
$17$*21,676
A17,/(8.275,(1(6
Montelukast
Pranlukast
Zafirlukast
- Block CysLT
receptor
- Excellent tolerance
Effective on rhinitis and
asthma
Effective on all symptoms
of rhinitis and on
ocular symptoms
()(5(1&(6: 1) International Primary Care Airways Group (IPAG) Handbook available at www.globalfamilydoctor.com.
2) Allergic Rhinitis and its impact on Asthma (ARIA) 2007. Full text ARIA documents and resources: www.whiar.org.
GINA materials have been used with permission from the Global Initiative for Asthma (www.ginasthma.org). Material from the IPAG
Handbook has been used with permission from the International Primary Care Airways Group.
L2&$/ &52021(6
(,175$1$6$/,
,175$2&8/$5)
Cromoglycate
Nedocromil
Naaga
- mechanism of
action poorly
known
- Minor local side
effects
Intraocular cromones
are very effective
Intranasal cromones
are less effective
and their effect is
short lasting
Overall excellent
safety
O5$/ / IM
*/8&2&257,&2-
67(52,'6
Dexamethasone
Hydrocortisone
Methylpredisolone
Prednisolone
Prednisone
Triamcinolone
Betamethasone
Deflazacort
- Potently reduce
nasal inflammation
- Reduce nasal
hyperreactivity
- Systemic side
effects common in
particular for IM
drugs
- Depot injections
may cause local
tissue atrophy
When possible,
intranasal glucocortico-
steroids should replace
oral or IM drugs
However, a short
course of oral gluco-
corticosteroids may be
needed if moderate/
severe symptoms
The printing of this ARIA Pocket Guide has been
supported by an educational grant from:
The ARIA Initiative has been supported
by educational grants from:
ALk Ab!''6
G'a3*S(%/$k'%)!
G-0+* U-%ac$
M!a P$a-(a
MSD
N*1a-/%.
N4c*(!
P$a%a
Sa)*"% A1!)/%.
Sc$!-%)#-P'*0#$
S/a''!-#!)!.
ARIA source documents are at www.whiar.org
MCR Inc.
Copies of this document are available at www.us-health-network.com
C
O
P
Y
R
I
G
H
T
E
D
M
A
T
E
R
I
A
L
,
D
O
N
O
T
A
L
T
E
R
O
R
R
E
P
R
O
D
U
C
E
.
Вам также может понравиться
- Aria PoketДокумент8 страницAria PoketNaifmxОценок пока нет
- Management of Allergic Rhinitis and Its Impact On Asthma Pocket GuideДокумент0 страницManagement of Allergic Rhinitis and Its Impact On Asthma Pocket GuideDanil Anugrah JayaОценок пока нет
- Cleveland Clinic Journal of Medicine 2012 SCHROER 285 93Документ9 страницCleveland Clinic Journal of Medicine 2012 SCHROER 285 93reioctabianoОценок пока нет
- Management of Allergic and Non-Allergic Rhinitis: A Primary Care Summary of The BSACI GuidelineДокумент11 страницManagement of Allergic and Non-Allergic Rhinitis: A Primary Care Summary of The BSACI GuidelinePriscila Ratna SupraptoОценок пока нет
- Diagnosing Rhinitis: Allergic vs. Nonallergic: David M. Quillen, M.D., and David B. Feller, M.DДокумент8 страницDiagnosing Rhinitis: Allergic vs. Nonallergic: David M. Quillen, M.D., and David B. Feller, M.DLia Mbag LiaОценок пока нет
- Cleveland Clinic Journal of Medicine 2012 SCHROER 285 93Документ9 страницCleveland Clinic Journal of Medicine 2012 SCHROER 285 93Joelyn Fatima BurnardОценок пока нет
- Aria Pharm PGДокумент14 страницAria Pharm PGBlack3Fox56Оценок пока нет
- Allergic Rhinitis in Children: Jomary Torres Mercado Medico Interno Manati Medical CenterДокумент38 страницAllergic Rhinitis in Children: Jomary Torres Mercado Medico Interno Manati Medical CenterJomary Torres MercadoОценок пока нет
- Allergic 2Документ5 страницAllergic 2EiynaMaulydhaОценок пока нет
- Evidence-Basedpractice: Sublingual Immunotherapy For Allergic RhinitisДокумент10 страницEvidence-Basedpractice: Sublingual Immunotherapy For Allergic RhinitisPeter SalimОценок пока нет
- CPG On Allergic Rhinitis 2Документ8 страницCPG On Allergic Rhinitis 2mkct111Оценок пока нет
- Dissertation Allergic RhinitisДокумент8 страницDissertation Allergic RhinitisWritingPaperServicesReno100% (1)
- Guia - 4209 Guia Rinitis AlergicaДокумент16 страницGuia - 4209 Guia Rinitis AlergicaJesus Manuel Armenta VelderrainОценок пока нет
- Allergic Rhinitis - StatPearls - NCBI BookshelfДокумент9 страницAllergic Rhinitis - StatPearls - NCBI BookshelfIndra kusuma mardiaОценок пока нет
- Allergic Rhinitis:: The Most Prevalent of Type I Allergic DisДокумент35 страницAllergic Rhinitis:: The Most Prevalent of Type I Allergic DisRini Oyien WulandariОценок пока нет
- Allergic Rhinitis: University of Michigan Guidelines For Health System Clinical CareДокумент12 страницAllergic Rhinitis: University of Michigan Guidelines For Health System Clinical Carerko_akibОценок пока нет
- Essential Update: New Recommendations For Treating Allergic Rhinitis ReleasedДокумент3 страницыEssential Update: New Recommendations For Treating Allergic Rhinitis ReleasedHerty FeliciaОценок пока нет
- Allergic Rhinitis in Children: Dr. Yousf AhmedДокумент45 страницAllergic Rhinitis in Children: Dr. Yousf AhmedYousfОценок пока нет
- AriaДокумент57 страницAriamushroom bestОценок пока нет
- Allergic Rhinitis in Children: DDR - Yousf AhmedДокумент45 страницAllergic Rhinitis in Children: DDR - Yousf AhmedYousfОценок пока нет
- Respiratory System Upper Respiratory DiseasesДокумент32 страницыRespiratory System Upper Respiratory DiseasesPrince Rener Velasco Pera100% (1)
- Management of Allergic and Non-Allergic Rhinitis: A Primary Care Summary of The BSACI GuidelineДокумент6 страницManagement of Allergic and Non-Allergic Rhinitis: A Primary Care Summary of The BSACI GuidelineGinanjar Tenri SultanОценок пока нет
- Aria - in - The - Pharmacy 2002Документ15 страницAria - in - The - Pharmacy 2002emmanuellagrace06Оценок пока нет
- ABCDE Approach To Emergency ManagementДокумент20 страницABCDE Approach To Emergency Managementluq9fifОценок пока нет
- Nih Public Access: N Engl J Med. Author Manuscript Available in PMC 2015 JULY 29Документ34 страницыNih Public Access: N Engl J Med. Author Manuscript Available in PMC 2015 JULY 29Haha RowlingОценок пока нет
- Rinitis Alergi Only DR - SPH 2Документ34 страницыRinitis Alergi Only DR - SPH 2ezradamanikОценок пока нет
- Rhinitis and Sinusitis: Office Management: Juan C. Guarderas, MDДокумент5 страницRhinitis and Sinusitis: Office Management: Juan C. Guarderas, MDyudha dodolОценок пока нет
- Who Aria 2008 YrДокумент94 страницыWho Aria 2008 YrFairuz NazilahОценок пока нет
- Otolaryngology - Head and Neck Surgery-2015 - Rhinitis AllergicДокумент43 страницыOtolaryngology - Head and Neck Surgery-2015 - Rhinitis AllergicAlpascaFirdausОценок пока нет
- BSACI Guidelines Non Allergic RhinitisДокумент24 страницыBSACI Guidelines Non Allergic RhinitisEdgardo GarciaОценок пока нет
- Emergency Treatment of Anaphylaxis in Adults: Concise GuidanceДокумент5 страницEmergency Treatment of Anaphylaxis in Adults: Concise Guidanceikhsan07Оценок пока нет
- Update Who Aria 2008, SuprihatiДокумент27 страницUpdate Who Aria 2008, SuprihatiivensОценок пока нет
- Nasal Smear Eosinophilia For The Diagnosis of Allergic Rhinitis and Eosinophilic Non Allergic RhinitisДокумент7 страницNasal Smear Eosinophilia For The Diagnosis of Allergic Rhinitis and Eosinophilic Non Allergic RhinitisAJITH KUMARОценок пока нет
- AnafilaktikДокумент60 страницAnafilaktikHusnia NabilahОценок пока нет
- GINA Pocket2013 May15Документ0 страницGINA Pocket2013 May15David BarzalloОценок пока нет
- Adults With Suspected Epiglottitis - Supraglottitis Guidelines For The Management ofДокумент2 страницыAdults With Suspected Epiglottitis - Supraglottitis Guidelines For The Management ofAlexandros MegasОценок пока нет
- Allergic Rhinitis - University of MichiganДокумент12 страницAllergic Rhinitis - University of MichiganarsyiadlinaОценок пока нет
- Diagnosing Allergic Rhinitis - Is There A Need?Документ3 страницыDiagnosing Allergic Rhinitis - Is There A Need?Alfa Suryani ArdliОценок пока нет
- Diagnostic Tools in Ocular AllergyДокумент14 страницDiagnostic Tools in Ocular AllergySara AlvesОценок пока нет
- RhinitisДокумент7 страницRhinitisShen ParilОценок пока нет
- Allergen-Specifi C Nasal Provocation Testing: Review by The Rhinoconjunctivitis Committee of The Spanish Society of Allergy and Clinical ImmunologyДокумент12 страницAllergen-Specifi C Nasal Provocation Testing: Review by The Rhinoconjunctivitis Committee of The Spanish Society of Allergy and Clinical ImmunologyRian Permana PОценок пока нет
- WC500022748 2 PDFДокумент0 страницWC500022748 2 PDFMostofa RubalОценок пока нет
- Febrile NeutropeniaДокумент11 страницFebrile Neutropeniamadimadi11Оценок пока нет
- Nassal Provocation Test - 6Документ5 страницNassal Provocation Test - 6Lengkung BajaОценок пока нет
- Anaphylaxis: Educational Programs Are NeededДокумент2 страницыAnaphylaxis: Educational Programs Are NeededNadin RussuОценок пока нет
- Diagnostics of AllergiesДокумент20 страницDiagnostics of AllergiesPaola ViñéОценок пока нет
- Anaphylaxis ArticuloДокумент12 страницAnaphylaxis ArticuloFrancelia Quiñonez RuvalcabaОценок пока нет
- 102v57n2a13096838pdf001 2Документ7 страниц102v57n2a13096838pdf001 2Fatkhul Ali ImronОценок пока нет
- Apa 1 115Документ8 страницApa 1 115Beizar YudhistiraОценок пока нет
- Allergic Rhinitis 2011Документ9 страницAllergic Rhinitis 2011SheinGervacioErnacioОценок пока нет
- Allergic Rhinitis and Its Impact On AsthmaДокумент188 страницAllergic Rhinitis and Its Impact On AsthmaSergioОценок пока нет
- Alterations With Infectious, Inflammatory, and Immunologic ResponseДокумент130 страницAlterations With Infectious, Inflammatory, and Immunologic ResponseAmerainahDimangadapОценок пока нет
- Vasomotor RhinitisДокумент6 страницVasomotor RhinitisdewawsОценок пока нет
- GA LEN/EAACI Pocket Guide For Allergen-Specific Immunotherapy For Allergic Rhinitis and AsthmaДокумент6 страницGA LEN/EAACI Pocket Guide For Allergen-Specific Immunotherapy For Allergic Rhinitis and AsthmaYohana VeronicaОценок пока нет
- Fast Facts: Respiratory Allergies: Understand aeroallergens, improve treatment responseОт EverandFast Facts: Respiratory Allergies: Understand aeroallergens, improve treatment responseОценок пока нет
- Diagnosis and Treatment of Chronic CoughОт EverandDiagnosis and Treatment of Chronic CoughSang Heon ChoОценок пока нет
- Complementary and Alternative Medical Lab Testing Part 2: RespiratoryОт EverandComplementary and Alternative Medical Lab Testing Part 2: RespiratoryОценок пока нет
- Bronchoscopic Drainage of A Malignant Lung Abscess: ASE EportДокумент4 страницыBronchoscopic Drainage of A Malignant Lung Abscess: ASE EportAlfani FajarОценок пока нет
- Dahlia 1Документ7 страницDahlia 1Alfani FajarОценок пока нет
- Hypertension in Pregnancy - Malang 23-9-201Документ34 страницыHypertension in Pregnancy - Malang 23-9-201Alfani FajarОценок пока нет
- Kdigo-Gn-Guideline GN PDFДокумент143 страницыKdigo-Gn-Guideline GN PDFFerry JuniansyahОценок пока нет
- BronchiolitisДокумент22 страницыBronchiolitisAlfani FajarОценок пока нет
- Exchange TransfusionДокумент9 страницExchange TransfusiondewpraОценок пока нет
- 10 Commandments of ConsultationДокумент4 страницы10 Commandments of ConsultationZlatan KurjakovicОценок пока нет
- 4 Life TestimoniesДокумент87 страниц4 Life TestimoniesBhavin VoraОценок пока нет
- UrosepsisДокумент22 страницыUrosepsisWita Ferani KartikaОценок пока нет
- Ataxia 10Документ19 страницAtaxia 10Cristina GhizdavetОценок пока нет
- Deyo 1992Документ6 страницDeyo 1992Wwwanand111Оценок пока нет
- Albendazole - Drug Information PDFДокумент7 страницAlbendazole - Drug Information PDFjjjkkОценок пока нет
- Heart Disease Power PointДокумент13 страницHeart Disease Power PointMuhamad AzwanОценок пока нет
- Assessment of ADHD and ComorbidityДокумент3 страницыAssessment of ADHD and ComorbidityFelipe CafureОценок пока нет
- Lambdoid Sutures: at The Coronal SutureДокумент14 страницLambdoid Sutures: at The Coronal SutureSyed Irfan ArifОценок пока нет
- Modified Ashworth ScaleДокумент3 страницыModified Ashworth ScaleSundarajan ManiОценок пока нет
- Why Women May Be Better Equipped To Fight COVIDДокумент46 страницWhy Women May Be Better Equipped To Fight COVIDjudith retanaОценок пока нет
- Science Grade 7 Second QuarterДокумент12 страницScience Grade 7 Second QuarterAnneKARYLE67% (3)
- Clinic Accomplishment ReportДокумент9 страницClinic Accomplishment ReportJen Apinado100% (6)
- Facial TicsДокумент2 страницыFacial TicsNdhe PoetryОценок пока нет
- Foundations in Microbiology: TalaroДокумент76 страницFoundations in Microbiology: Talaromertx013Оценок пока нет
- Muscular Dystrophy and Its Ayurvedic PerspectivesДокумент149 страницMuscular Dystrophy and Its Ayurvedic PerspectivesMuktha ShenoyОценок пока нет
- EDiR Notebook (For European Diploma in Radiology)Документ250 страницEDiR Notebook (For European Diploma in Radiology)Parthiban Bala100% (4)
- The Control and Prevention of MRSA in Hospitals and in The CommunityДокумент41 страницаThe Control and Prevention of MRSA in Hospitals and in The CommunityDimas RfОценок пока нет
- Breast Sarcoidosis An Extremely Rare Case of Idiopathic Granulomatous MastitisДокумент3 страницыBreast Sarcoidosis An Extremely Rare Case of Idiopathic Granulomatous MastitisInternational Journal of Innovative Science and Research TechnologyОценок пока нет
- MCQ Tyba Abnormal Psychology 2020Документ16 страницMCQ Tyba Abnormal Psychology 2020phanishashidharОценок пока нет
- Yoga & Lifestyle: Topics of Unit: 3Документ14 страницYoga & Lifestyle: Topics of Unit: 3UNKNOWN KNOWLEDGEОценок пока нет
- Naomi Williams FindingsДокумент58 страницNaomi Williams Findingsscott.faulkner.taylorОценок пока нет
- Nausea and Vomitting-FonДокумент52 страницыNausea and Vomitting-FonZephas HillsОценок пока нет
- Nhis Drug Price List Final (2013 Ed)Документ32 страницыNhis Drug Price List Final (2013 Ed)holuwadamilare935Оценок пока нет
- Complete Protein Antigens and Low - Molecular-Weight Substances - Complete Protein Antigens, Such As AnimalДокумент1 страницаComplete Protein Antigens and Low - Molecular-Weight Substances - Complete Protein Antigens, Such As AnimalApple BananaОценок пока нет
- Immunofluorescence Techniques: Ian D. Odell and Deborah CookДокумент4 страницыImmunofluorescence Techniques: Ian D. Odell and Deborah CookbalamurugantОценок пока нет
- Pathogenesis of Non-Hodgkin's Lymphoma: Ournal of Linical NcologyДокумент9 страницPathogenesis of Non-Hodgkin's Lymphoma: Ournal of Linical NcologyZullymar CabreraОценок пока нет
- CBAHI StandardsДокумент264 страницыCBAHI StandardsAnjo Cinco83% (30)
- Fact Sheet Central Retinal Vein OcclusionДокумент2 страницыFact Sheet Central Retinal Vein OcclusionAini Nur Syafa'ahОценок пока нет
- Brilliance iCT Technical BackgrounderДокумент2 страницыBrilliance iCT Technical Backgroundermedgadget100% (4)