Академический Документы
Профессиональный Документы
Культура Документы
Figo Steroid
Загружено:
Dedy Chandra HariyonoАвторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Figo Steroid
Загружено:
Dedy Chandra HariyonoАвторское право:
Доступные форматы
Assessment and management of preterm
labour
Queensland Maternity and Neonatal Clinical Guideline: Assessment and management of preterm labour
Document title:
Assessment and management of preterm labour
Publication date:
September 2009
Document number:
MN09.6-V4-R14
Replaces document:
MN09.6-V3-R11
Author:
Audience:
Queensland Maternity and Neonatal Clinical Guidelines Program
Health professionals in Queensland public and private maternity services
Exclusions:
Management of premature rupture of membranes
Review date:
September 2014
Endorsed by:
Statewide Maternity and Neonatal Clinical Network
QH Patient Safety and Quality Executive Committee
Contact:
Queensland Maternity and Neonatal Clinical Guidelines Program
Email: MN-Guidelines@health.qld.gov.au
URL: www.health.qld.gov.au/qcg
Disclaimer
These guidelines have been prepared to promote and facilitate standardisation and consistency of
practice, using a multidisciplinary approach.
Information in this guideline is current at time of publication.
Queensland Health does not accept liability to any person for loss or damage incurred as a result of
reliance upon the material contained in this guideline.
Clinical material offered in this guideline does not replace or remove clinical judgement or the
professional care and duty necessary for each specific patient case.
Clinical care carried out in accordance with this guideline should be provided within the context of
locally available resources and expertise.
This Guideline does not address all elements of standard practice and assumes that individual
clinicians are responsible to:
Discuss care with consumers in an environment that is culturally appropriate and which
enables respectful confidential discussion. This includes the use of interpreter services
where necessary
Advise consumers of their choice and ensure informed consent is obtained.
Provide care within scope of practice, meet all legislative requirements and maintain
standards of professional conduct
Apply standard precautions and additional precautions as necessary, when delivering care
Document all care in accordance with mandatory and local requirements
This work is licensed under a Creative Commons Attribution Non-Commercial No Derivatives 2.5 Australia licence. To view a copy of this
licence, visit http://creativecommons.org/licenses/by-nc-nd/2.5/au/
State of Queensland (Queensland Health) 2010
In essence you are free to copy and communicate the work in its current form for non-commercial purposes, as long as you attribute the authors
and abide by the licence terms. You may not alter or adapt the work in any way.
For permissions beyond the scope of this licence contact: Intellectual Property Officer, Queensland Health, GPO Box 48, Brisbane Qld 4001,
email ip_officer@health.qld.gov.au , phone (07) 3234 1479. For further information contact Queensland Maternity and Neonatal Clinical
Guidelines Program, RBWH Post Office, Herston Qld 4029, email MN-Guidelines@health.qld.gov.au phone (07) 3131 6777.
Refer to online version, destroy printed copies after use
Page 2 of 14
Queensland Maternity and Neonatal Clinical Guideline: Assessment and management of preterm labour
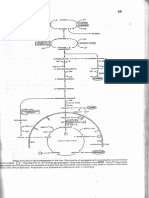
Flowchart: Assessment and management of preterm labour
Refer to online version, destroy printed copies after use
Page 3 of 14
Queensland Maternity and Neonatal Clinical Guideline: Assessment and management of preterm labour
Abbreviations
BP
cm
CTG
FBC
fFN
g
GBS
IM
IV
M/C/S
mg
min
mm
mmHg
MSU
PPROM
PROM
PTL
RSQ
stat
TVCL
VE
O
C
Blood pressure
Centimetres
Cardiotocograph
Full blood count
Fetal fibronectin
Grams
Group B streptococcus
Intramuscular
Intravenous
Microscopy / culture / sensitivity
Milligram
Minutes
Millimetres
Millimetres of mercury
Mid stream urine
Preterm premature rupture of membranes
Premature rupture of membranes
Preterm labour
Retrieval Services Queensland
Statim (immediately)
Transvaginal cervical length
Vaginal examination
Degrees Celsius
Refer to online version, destroy printed copies after use
Page 4 of 14
Queensland Maternity and Neonatal Clinical Guideline: Assessment and management of preterm labour
Table of Contents
Introduction.....................................................................................................................................6
1.1
Definition ................................................................................................................................6
1.2
Risk factors ............................................................................................................................6
2 Assessment ....................................................................................................................................6
2.1
Review history........................................................................................................................6
2.2
Assess for signs and symptoms of preterm labour ...............................................................6
2.3
Physical examination and initial Investigations......................................................................6
2.4
Fetal fibronectin testing..........................................................................................................7
2.5
Transvaginal ultrasound of cervical length ............................................................................7
2.5.1 Interpreting TVCL results...................................................................................................7
3 Management of preterm labour ......................................................................................................8
3.1
Negative fFN and no evidence of cervical change / TVCL > 20 mm.....................................8
3.2
Positive fFN and / or evidence of cervical change / TVCL < 20 mm .....................................8
4 Tocolysis.........................................................................................................................................8
4.1
Contraindications ...................................................................................................................8
4.2
Relative contraindications......................................................................................................8
4.3
Nifedipine ...............................................................................................................................9
4.3.1 Contraindications ...............................................................................................................9
4.3.2 Dosage and administration ................................................................................................9
5 Corticosteroids..............................................................................................................................10
5.1
Dosage and administration ..................................................................................................10
6 Antibiotics .....................................................................................................................................10
6.1
Dosage and administration ..................................................................................................10
7 Transfer ........................................................................................................................................10
References ..........................................................................................................................................11
Appendix A: Drug Table.......................................................................................................................13
Appendix B: Acknowledgements .........................................................................................................14
1
List of Tables
Table 1. Fetal fibronectin testing ........................................................................................................... 7
Table 2. Nifedipine dosage and administration ..................................................................................... 9
Table 3. Betamethasone dosage and administration .......................................................................... 10
Table 4. Antibiotics dosage and administration................................................................................... 10
Refer to online version, destroy printed copies after use
Page 5 of 14
Queensland Maternity and Neonatal Clinical Guideline: Assessment and management of preterm labour
Introduction
Fourteen percent of Australian perinatal deaths in 2005 were as a result of preterm delivery,1
however most women that present with symptoms of preterm labour will deliver at term with a small
minority delivering within seven days of onset of symptoms.2,3
1.1
Definition
Delivery occurring before 37 completed weeks gestation.
1.2
Risk factors
Previous preterm birth
Preterm premature rupture of membranes (PPROM)
Cervical incompetence
Cervical surgical procedures
Uterine anomalies
Multiple gestation
Polyhydramnios
Placental abruption
Vaginal bleeding
Smoking
Illicit drug use
Assessment
The aim of assessment is to determine the risk of delivery within the next seven days and to assess
fetal and maternal wellbeing.
2.1
Review history
Medical
Surgical
Obstetric
2.2
Assess for signs and symptoms of preterm labour
2.3
Lower abdominal cramping
Pelvic pressure
Lower back pain
Vaginal spotting or show
Regular uterine activity
Cervical effacement / dilatation
Physical examination and initial Investigations
Vital signs
Mid-stream urinalysis and consider microscopy/culture/sensitivity
Maternal abdominal examination
Fetal heart rate +/- cardiotocograph (CTG)
Sterile speculum examination
Exclude premature rupture of membranes (PROM)
Obtain fFN test if not contraindicated [refer section 2.4]
High vaginal swab with M/C/S
Low vaginal/anorectal swab for Group B streptococcus
Assess cervical dilatation by sterile digital vaginal examination unless contraindicated by
o Ruptured membranes
o Suspected placenta praevia
Refer to online version, destroy printed copies after use
Page 6 of 14
Queensland Maternity and Neonatal Clinical Guideline: Assessment and management of preterm labour
2.4
Fetal fibronectin testing
Fetal fibronectin (fFN) is a screening test used to assess the risk of preterm delivery within the next
seven days. Point of care fFN testing should be utilised in the assessment of preterm labour.
Table 1. Fetal fibronectin testing
Indications4
Contraindications
Relative
Contraindications
Procedure
Positive Result
Negative Result
2.5
Symptomatic preterm labour between 24 and 36 weeks gestation and
Intact membranes and
Cervical dilatation less than 3 cm
Ruptured membranes
Visual evidence of moderate or gross bleeding
Cervical cerclage insitu
After the use of lubricants or disinfectants
Within 24 hours of coitus
Within 24 hours of vaginal examination
Performed during sterile speculum examination prior to any examination
or manipulation of the cervix or vagina
Use only sterile water as a lubricant
Obtain the sample for testing from the posterior fornix of the vagina
As per test kit instructions
Consider transvaginal ultrasound of cervical length if available (see 2.5)
Admit for tocolysis and steroids
Consider transfer to appropriate level facility
False positive result may occur as a result of recent4,5
o Coitus
o Digital vaginal examination
o Transvaginal ultrasound
Low risk of delivery within seven days
False negative result may occur due to4,5
o Use of lubricant with speculum examination
o Intravaginal disinfectants.
Transvaginal ultrasound of cervical length
Transvaginal ultrasound of cervical length (TVCL) is an additional screening test that can aid in
assessing the risk of preterm delivery. TVCL must be performed by a credentialed clinician. Lack of
local capability to perform this test is not a reason for transfer.
2.5.1 Interpreting TVCL results
A cervical length less than 15 mm is associated with an increased risk of spontaneous preterm birth.3
Due to the distances required for transfer from Queensland regional centres, a TVCL cut-off of 20
mm is appropriate.
Refer to online version, destroy printed copies after use
Page 7 of 14
Queensland Maternity and Neonatal Clinical Guideline: Assessment and management of preterm labour
Management of preterm labour
Tocolysis and steroids are the main strategies to manage preterm labour [see section 4, 5]. Transfer
may also be necessary, dependent on the acuity level of the facility and nursery requirements.
Management options will depend on the services available at each facility, such as:
screening test availability
equipment (eg CTG) availability
acuity level of the nursery
If necessary, contact an obstetrician for further advice.
3.1
Negative fFN and no evidence of cervical change / TVCL > 20 mm
There is a low risk of delivery within the next 7 days therefore:
if contractions are infrequent / irregular
o offer discharge home with follow-up as an outpatient within 7 days
if contractions are regular and painful:
o admit for observation
o offer analgesia
o reassess in 2 hours
if contractions are persistent and painful
o consider steroids
o tocolysis and
o transfer if necessary
3.2
Positive fFN and / or evidence of cervical change / TVCL < 20 mm
There is an increased risk of delivery within the next 7 days therefore:
admit and offer analgesia
administer steroids and commence tocolysis (if no contraindications)
continuous fetal monitoring with CTG
transfer if necessary
Tocolysis
The aim of tocolysis is to suppress uterine contractions and delay preterm delivery6,7 to:
allow in-utero transfer to an appropriate level facility
allow for the administration of corticosteroids
4.1
Contraindications
4.2
Gestation > 34 weeks
Labour is too advanced
In utero fetal death
Lethal fetal anomalies
Suspected fetal compromise
Placental abruption
Suspected intra-uterine infection
Maternal hypotension: BP < 90 mmHg systolic
Relative contraindications
Cautiously give tocolysis if:
pre-eclampsia
placenta praevia (if not bleeding)
Refer to online version, destroy printed copies after use
Page 8 of 14
Queensland Maternity and Neonatal Clinical Guideline: Assessment and management of preterm labour
4.3
Nifedipine
Nifedipine is the tocolytic of choice. Nifedipine is a calcium channel blocker that relaxes smooth
muscle.8 It is an effective tocolytic with fewer side effects than other tocolytics available.6
4.3.1 Contraindications
If there are contraindications to Nifedipine, liaise with an Obstetrician to determine alternate
tocolysis.9
Contraindications include8:
previous adverse reaction to calcium channel blockers
maternal cardiac disease
hypotension
hepatic dysfunction
concurrent use with salbutamol or other beta-sympathomimetics
concurrent use of nitrates or antihypertensive medication
4.3.2
Dosage and administration
Table 2. Nifedipine dosage and administration
Nifedipine
Route
Dose
Maintenance Dose
Comments
Side Effects
Observations6,10
Oral
20 mg stat
If contractions persist after 30 minutes: Repeat 20 mg
If contractions persist after a further 30 minutes: Repeat 20 mg
If blood pressure is stable, 20 mg every 6 hours for 48 hours. Further
maintenance therapy is ineffective6
Maximum dose is 160 mg/day8
Do not use sustained release formulation
Use cautiously with magnesium sulphate8
Hypotension
Headache
Facial flushing
Cardiac failure
Tachycardia, palpitations
Nausea
Dizziness
Cardiotocograph monitoring until contractions cease
Pulse rate, respiratory rate and blood pressure monitoring
o every thirty minutes for first hour, then
o second hourly for 24 hours, then
o four hourly
Measure and record temperature every four hours
Refer to online version, destroy printed copies after use
Page 9 of 14
Queensland Maternity and Neonatal Clinical Guideline: Assessment and management of preterm labour
Corticosteroids
Administration of corticosteroids can reduce fetal mortality and morbidity.11 Antenatal corticosteroid
therapy should be initiated in women between 24 and 34 weeks gestation.12
5.1
Dosage and administration
Table 3. Betamethasone dosage and administration
Betamethasone
Route
Dose
Comments
IM
11.4 mg
Repeat 24 hours after initial dose12-14
Where delivery is not imminent, routine prophylactic administration of
steroids is not recommended15,16
If delivery is imminent and it is more than 10 days since the initial dose,
subsequent steroid dose may be administered. Careful clinical
assessment is required, including fFN testing
Antibiotics
Prophylactic antibiotics for GBS are not recommended in threatened preterm labour.17
Prophylactic antibiotics for GBS should be administered in established preterm labour.18
6.1
Dosage and administration
Table 4. Antibiotics dosage and administration
Penicillin
Route
Dose
Comments
IV
1.2 g stat then 600 mg every 4-6 hours19
If there is penicillin hypersensitivity give
o Lincomycin 600 mg IV every 8 hours (on the QH List of
Approved Medications) or
o Clindamycin 900 mg IV every 8 hours19 (not on the QH List of
Approved Medications)
Erythromycin should be avoided17
If GBS screening tests are negative - cease antibiotics
Transfer
Neonatal outcome is improved with appropriate in-utero transfer
If transfer is indicated the relevant obstetric medical coordinator should be contacted via
Retrieval Services Queensland (RSQ) on 1300 799 127
If after discussion with the obstetric coordinator it is thought there may be a risk of
delivery during transfer, in-utero transfer should not be attempted
Refer to online version, destroy printed copies after use
Page 10 of 14
Queensland Maternity and Neonatal Clinical Guideline: Assessment and management of preterm labour
References
1. Australian Bureau of Statistics. Causes of death. [online]. 2005 [cited 2009 March 3]; 2009.
Available from:
http://www.ausstats.abs.gov.au/ausstats/subscriber.nsf/0/3FFF8096D9500CA9CA25729D001C0B05
/$File/33030_2005.pdf.
2. Giles W, Bisits A, Knox M, Madsen G, Smith R. The effect of fetal fibronectin testing on
admissions to a tertiary maternal-fetal unit and cost savings. Am J Obstet Gynecol. 2000; 182(2):43942.
3. Tsoi E, Akmal S, Geerts L, Jeffery B, Nicolaides K. Sonographic measurement of cervical length
and fetal fibronectin testing in threatened preterm labour. Ultrasound Obstet Gynecol. 2006; 27:36872.
4. The Royal Australian and New Zealand College of Obstetricians and Gynaecologists. Use of
cervical fetal fibronectin as a screening test for preterm birth. College Statement C-Obs 26. 2008
[cited 2009 March 3]. Available from: www.ranzcog.edu.au/publications/statements/C-obs26.pdf.
5. Anderson HF. Use of fetal fibronectin in women at risk for preterm delivery. Clin Obstet Gynecol.
2000; 43(4):746-58.
6. King J, Flenady V, Papatsonis D, Dekker G, Carbonne B. Calcium channel blockers for inhibiting
preterm labour. Cochrane Database Syst Rev. 2003; Issue1.Art, No.: CD002255.
DOI10.1002/14651858.CD002255.
7. Department of Health New South Wales. Tocolytic agents - protocols for administration for
threatened preterm labour. Circular No 2002/49. 2002.
8. Australian Medicines Handbook. Nifedipine [online]2009 [cited 2009 May 25]. Available from:
https://www-amh-netau.cknservices.dotsec.com/online/view.php?page=chapter17/monographnifedipine02.html#nifedipine-02.
9. The Royal Australian and New Zealand College of Obstetricians and Gynaecologists. The use of
nifedipine in obstetrics. College Statement C-Obs 15. 2008.
10. King JF, Flenady V, Papatsonis D, Dekker G, Carbonne B. Calcium channel blockers for
inhibiting preterm labour; a systematic review of the evidence and a protocol for administration of
nifedipine. Aust N Z J Obstet Gynaecol. 2003; 43(3):192-8.
11. Roberts D, Dalziel S. Antenatal corticosteroids for accelerating fetal lung maturation for women
at risk of preterm birth. Cochrane Database Syst Rev. 2006; Issue 3. Art. No.: CD004454. DOI:
10.1002/14651858.CD004454.pub2.
12. Royal College of Obstetricians and Gynaecologists. Antenatal corticosteroids to prevent RDS.
Guideline No.7 [online]. 2004 [cited 2009 March 25]. Available from: http://www.rcog.org.uk/files/rcogcorp/uploaded-files/GT7AntenatalCorticosteroids2004.pdf.
13. Australian Medicines Handbook. Betamethasone [online]2009 [cited 2009 May 25]. Available
from: https://www-amh-netau.cknservices.dotsec.com/online/view.php?page=chapter14/monographbetamethasone.html#betam
ethasone.
14. Antenatal corticosteroids revisited: repeat courses. National Institute of Health Consensus
Statement [online]. 2000 [cited 2009, June 25]; 17(2):1-10. Available from:
http://consensus.nih.gov/2000/2000AntenatalCorticosteroidsRevisted112html.htm.
15. Murphy K, Hannah M, Willan A, Hewson S, Ohlsson A, Kelly E. Multiple courses of antenatal
corticosteroids for preterm birth. Lancet. 2008; 372:2143-51.
Refer to online version, destroy printed copies after use
Page 11 of 14
Queensland Maternity and Neonatal Clinical Guideline: Assessment and management of preterm labour
16. Newnham JP, Jobe AH. Should we be prescribing repeated courses of antenatal
corticosteroids? Semin Fetal Neonatal Med. 2009; 14(3):157-63.
17. Kenyon SL. Broad spectrum antibiotics for spontaneous preterm labour: the ORACLE II trial.
Lancet. 2001; 357:1319-27.
18. Flenady V, Jenkins-Manning, S. Prevention of neonatal early onset Group B streptococcal
disease (EOGBSD). Queensland Clinical Practice Guidelines Working Party 2007.
19. Australasian Society for Infectious Diseases. Management of perinatal infections. [online]. 2002
[cited 2009 May 25]. Available from:
http://www.asid.net.au/downloads/Management%20of%20Perinatal%20Infections%20ASID%202002
%20rev%202007.pdf.
Refer to online version, destroy printed copies after use
Page 12 of 14
Queensland Maternity and Neonatal Clinical Guideline: Assessment and management of preterm labour
Appendix A: Drug Table
Drug Name
Tocolysis
Nifedipine
Dose
Route
Comments
20 mg stat
Repeat 20 mg (if still contracting at
30 minutes)
Final 20 mg (if still contracting after
further 30 minutes)
Maintenance 20 mg every 6 hours
for 48 hours
oral
Do not use sustained
release
CTG whilst
administering
Monitor vital signs
Maximum dose of 160
mg/day
11.4 mg stat, then
Repeat 11.4 mg 24 hours after
initial dose
IM
Repeat doses after
initial course not
recommended
Corticosteroids
Betamethasone
Antibiotics
IV
1.2 g stat, then
Group B streptococcus
prophylaxis
600 mg every 4 6 hours
If the patient has Penicillin hypersensitivity give either Lincomycin or Clindamycin
IV
600 mg every 8 hours
On the QH List of
Lincomycin
Approved Medications
IV
Clindamycin
900 mg every 8 hours
Not on the QH List of
Approved Medications
Penicillin
Refer to online version, destroy printed copies after use
Page 13 of 14
Queensland Maternity and Neonatal Clinical Guideline: Assessment and management of preterm labour
Appendix B: Acknowledgements
The Maternity and Neonatal Clinical Guidelines Program gratefully acknowledge the contribution of
Queensland clinicians and other stakeholders who participated throughout the guideline development
process particularly:
Working Party Clinical Lead
Dr Liana Tanda, Obstetrician, Caboolture Hospital
Working Party Members
Ms Karen Baker, Midwife, Mackay Base Hospital
Dr Kathleen Braniff, Obstetrician, Mackay Base Hospital
Ms Penelope Dale, Midwife, Royal Brisbane and Womens Hospital
Professor Ian Jones, Obstetrician, Royal Brisbane and Womens Hospital
Dr Christopher King, Obstetrician, Mt Isa Hospital
Ms Mary Hindmarsh, Midwife, Weipa
Professor Michael Humphrey, Obstetrician, Office of Rural and Remote Health
Associate Professor Rebecca Kimble, Obstetrician, Royal Brisbane and Womens Hospital
Dr David Moore, Obstetric Registrar, Gold Coast Hospital
Ms Vivienne Rybarczyk, Midwife, Rockhampton Base
Dr Renukar Sekar, Obstetrician, Royal Brisbane and Womens Hospital
Ms Mary Tredinnick, Pharmacist, Royal Brisbane and Womens Hospital
Program Team
Associate Professor Rebecca Kimble, Director, Queensland Maternity and Neonatal Clinical
Guidelines Program
Ms Joan Kennedy, Principal Program Officer, Queensland Maternity and Neonatal Clinical Guidelines
Program
Mr Stephen Aitchison, Program Officer, Queensland Maternity and Neonatal Clinical Guidelines
Program
Ms Jacinta Lee, Program Officer, Queensland Maternity and Neonatal Clinical Guidelines Program
Mrs Catherine van den Berg, Program Officer, Queensland Maternity and Neonatal Clinical
Guidelines Program
Steering Committee Queensland Maternity and Neonatal Clinical Guidelines Program
Refer to online version, destroy printed copies after use
Page 14 of 14
Вам также может понравиться
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeОт EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeРейтинг: 4 из 5 звезд4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreОт EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreРейтинг: 4 из 5 звезд4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItОт EverandNever Split the Difference: Negotiating As If Your Life Depended On ItРейтинг: 4.5 из 5 звезд4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceОт EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceРейтинг: 4 из 5 звезд4/5 (894)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureОт EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureРейтинг: 4.5 из 5 звезд4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersОт EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersРейтинг: 4.5 из 5 звезд4.5/5 (344)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)От EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Рейтинг: 4.5 из 5 звезд4.5/5 (119)
- The Emperor of All Maladies: A Biography of CancerОт EverandThe Emperor of All Maladies: A Biography of CancerРейтинг: 4.5 из 5 звезд4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingОт EverandThe Little Book of Hygge: Danish Secrets to Happy LivingРейтинг: 3.5 из 5 звезд3.5/5 (399)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyОт EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyРейтинг: 3.5 из 5 звезд3.5/5 (2219)
- The Yellow House: A Memoir (2019 National Book Award Winner)От EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Рейтинг: 4 из 5 звезд4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaОт EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaРейтинг: 4.5 из 5 звезд4.5/5 (265)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryОт EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryРейтинг: 3.5 из 5 звезд3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnОт EverandTeam of Rivals: The Political Genius of Abraham LincolnРейтинг: 4.5 из 5 звезд4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaОт EverandThe Unwinding: An Inner History of the New AmericaРейтинг: 4 из 5 звезд4/5 (45)
- Stockard Tests UE & LE TДокумент4 страницыStockard Tests UE & LE TLinh HoangОценок пока нет
- Virtual Pig Dissection Worksheet 06-07 2Документ6 страницVirtual Pig Dissection Worksheet 06-07 2api-255054890Оценок пока нет
- St. Victoria Hospital Nursing Service Ward DeptДокумент50 страницSt. Victoria Hospital Nursing Service Ward DeptPat MagpaliОценок пока нет
- Lovenox (Enoxaparin)Документ1 страницаLovenox (Enoxaparin)E100% (1)
- (2017) OGUNYEMI, Boluwaji MILLER-MONTHROPE, Yvette. The State of Ethnic Dermatology in CanadaДокумент3 страницы(2017) OGUNYEMI, Boluwaji MILLER-MONTHROPE, Yvette. The State of Ethnic Dermatology in CanadaCassandra VérasОценок пока нет
- Mercy Obstetric Triage OTDA A Standardised Approach To Care CHA SlidesДокумент28 страницMercy Obstetric Triage OTDA A Standardised Approach To Care CHA Slidessaepulloh bin amingОценок пока нет
- Practical Medical Oncology Textbook (Antonio Russo, Marc Peeters, Lorena Incorvaia Etc.)Документ1 104 страницыPractical Medical Oncology Textbook (Antonio Russo, Marc Peeters, Lorena Incorvaia Etc.)Paolo FassinaОценок пока нет
- Data Thermal Printer CSДокумент24 страницыData Thermal Printer CSDedy Chandra HariyonoОценок пока нет
- KlikBCA Individual Save PageДокумент1 страницаKlikBCA Individual Save PageDedy Chandra HariyonoОценок пока нет
- ManagementДокумент1 страницаManagementDedy Chandra HariyonoОценок пока нет
- Promoting Products: Brand of Product Product Category Company ShapeДокумент2 страницыPromoting Products: Brand of Product Product Category Company ShapeDedy Chandra HariyonoОценок пока нет
- Manufacturing and ServicesДокумент1 страницаManufacturing and ServicesDedy Chandra HariyonoОценок пока нет
- CV (Yessy)Документ1 страницаCV (Yessy)Dedy Chandra HariyonoОценок пока нет
- CV (Yessy)Документ1 страницаCV (Yessy)Dedy Chandra HariyonoОценок пока нет
- Manufacturing and ServicesДокумент1 страницаManufacturing and ServicesDedy Chandra HariyonoОценок пока нет
- Manufacturing and ServicesДокумент1 страницаManufacturing and ServicesDedy Chandra HariyonoОценок пока нет
- Promoting Products: Brand of Product Product Category Company ShapeДокумент2 страницыPromoting Products: Brand of Product Product Category Company ShapeDedy Chandra HariyonoОценок пока нет
- KlikBCA Individual Save Page - JPGGДокумент1 страницаKlikBCA Individual Save Page - JPGGDedy Chandra HariyonoОценок пока нет
- CV (Yessy)Документ1 страницаCV (Yessy)Dedy Chandra HariyonoОценок пока нет
- Pericarditis and Pericardial EffusionДокумент31 страницаPericarditis and Pericardial EffusionDedy Chandra HariyonoОценок пока нет
- CardiomyopathyДокумент23 страницыCardiomyopathyDedy Chandra HariyonoОценок пока нет
- 1015Документ7 страниц1015Bang DeОценок пока нет
- TorrentДокумент1 страницаTorrentDedy Chandra HariyonoОценок пока нет
- Glukoneogenesis (Dr. Hairrudin)Документ1 страницаGlukoneogenesis (Dr. Hairrudin)devezzfilОценок пока нет
- TorrentДокумент1 страницаTorrentDedy Chandra HariyonoОценок пока нет
- Makanan PengawetДокумент6 страницMakanan PengawetDedy Chandra HariyonoОценок пока нет
- Herbalife 1 - Slimming at All Costs: HerbalifeÒ-induced Liver InjuryДокумент3 страницыHerbalife 1 - Slimming at All Costs: HerbalifeÒ-induced Liver InjuryMohammed AyubОценок пока нет
- Insya AllahДокумент1 страницаInsya AllahDedy Chandra HariyonoОценок пока нет
- (José Almeida) Atlas of Endovascular Venous SurgeДокумент516 страниц(José Almeida) Atlas of Endovascular Venous SurgeTa TaОценок пока нет
- Placenta Previa (New) - 1Документ32 страницыPlacenta Previa (New) - 1Ibrahim ZainabОценок пока нет
- Ethicon Suture & Needles wall chart (2 pages)Документ2 страницыEthicon Suture & Needles wall chart (2 pages)andy liОценок пока нет
- Guide to Head and Neck DiseasesДокумент47 страницGuide to Head and Neck DiseasesDonna LabaniegoОценок пока нет
- A Practical Guide to HPIДокумент11 страницA Practical Guide to HPIMichael NyaongoОценок пока нет
- Eyelid Trauma and Orbital FracturesДокумент16 страницEyelid Trauma and Orbital FracturesFachroni Agim RahmanОценок пока нет
- Officinalis) : Lavender (LavandulaДокумент3 страницыOfficinalis) : Lavender (LavandulaMacsim RoxanaОценок пока нет
- Lower Extremity Venous Duplex USДокумент6 страницLower Extremity Venous Duplex USjmg_mdОценок пока нет
- Labor and Birth Process 3 Stage & 4 Stage: RD THДокумент23 страницыLabor and Birth Process 3 Stage & 4 Stage: RD THبشائر حمادةОценок пока нет
- Anesthesia Professional Coding For McKesson Anesthesia Care™Документ2 страницыAnesthesia Professional Coding For McKesson Anesthesia Care™McKesson Surgical SolutionsОценок пока нет
- Report On The Hospital VisitДокумент4 страницыReport On The Hospital VisitSolanki PrakashОценок пока нет
- Lath AДокумент118 страницLath AManish PandeyОценок пока нет
- Tugas Dr. Domingos Da SilvaДокумент6 страницTugas Dr. Domingos Da Silvadenilay richardoОценок пока нет
- A Study On "Contract Labour"Документ67 страницA Study On "Contract Labour"Phani BabuОценок пока нет
- Population Welfare Program and ServicesДокумент57 страницPopulation Welfare Program and Servicesadeel_khan_48Оценок пока нет
- Eswl 1Документ33 страницыEswl 1G Vignesh GvsОценок пока нет
- Nelson MCQ PDFДокумент595 страницNelson MCQ PDFPavan Kumar100% (5)
- Artificial Limb Research in BangladeshДокумент5 страницArtificial Limb Research in BangladeshMd IslamОценок пока нет
- Nursing Bullets Fundamentals GuideДокумент89 страницNursing Bullets Fundamentals GuideJek NevadoОценок пока нет
- ICRA Form v08.07Документ5 страницICRA Form v08.07Indra Juang Putra HarefaОценок пока нет
- Ceramic Restorations: Bonded Porcelain Veneers - Part 1: PerspectiveДокумент5 страницCeramic Restorations: Bonded Porcelain Veneers - Part 1: PerspectiveVinisha Vipin SharmaОценок пока нет
- Biodata: PARGANAS, KOLKATA-700102, West BengalДокумент3 страницыBiodata: PARGANAS, KOLKATA-700102, West BengalTina lovelyОценок пока нет
- Treatment and Management AppendicitisДокумент3 страницыTreatment and Management Appendicitisruthjoy23upgirlОценок пока нет