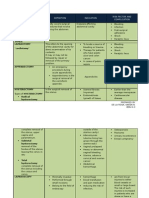
Академический Документы
Профессиональный Документы
Культура Документы
High Lateral Tension Abdominoplasty
Загружено:
Ahmad Arbi AninditoАвторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
High Lateral Tension Abdominoplasty
Загружено:
Ahmad Arbi AninditoАвторское право:
Доступные форматы
Section 12: Body contouring/bariatric massive weight loss
Go to
www.expertconsult.com
CHAPTER
to see updates to this chapter
See DVD
69
High lateral tension
abdominoplasty
Steven Teitelbaum
History
Physical evaluation
The history of the high lateral tension abdominoplasty (HLT)
begins not so much with the history of abdominoplasty but
with that of lower body lifting. This should come as no surprise, as Ted Lockwood, the creator of the HLT, considered it
a powerful lower body lifting procedure.
In 1993 Lockwood published his novel lower body lift
technique. Though this operation was designed to optimize
the contour in the buttock and thighs, it also produced a
greater improvement of the abdomen than did the abdominoplasty procedures of that day. He therefore eliminated the
posterior incision and the dissection down the thigh, thereby
creating a body lift procedure that could be done from the
supine position. The HLT was therefore a reduced version of
the lower body lift, eliminating the posterior incision, but
maintaining a pattern of excision anteriorly that offered
similar anterior improvement as achieved with a lower body
lift.
Two years after his lower body lift paper, Dr. Lockwood
published his landmark HLT paper. He ascribed four characteristics to the HLT. First, there would be no undermining
beyond what would either be excised or necessary to allow
exposure for rectus plication. Second, he advocated extensive
safe simultaneous liposuction in non-undermined areas.
Third, he advocated the use of permanent sutures to close the
superficial fascial system (SFS). Finally, the area on the incision with the greatest tension would be laterally rather than
centrally. This is the sine qua non of the HLT, yet it is the
most elusive to understand. Since the distribution of tension
along the incision is only felt by the surgeon intraoperatively,
it is difficult to simply demonstrate exactly what HLT means
in a drawing; in order to execute an HLT, one must understand its principles and apply them to each case.
The HLT is not just an abdominoplasty; it is a powerful
lower body lifting procedure, creating improvement not just
of the abdomen, but to the mons, inguinal region, proximal
thighs, and even the buttocks. Even posture can be improved
(Figs 69.1, 69.2).
Any abdominoplasty has the potential to correct three separate anatomical structures: skin, fat, and muscle. Each is evaluated separately in order to plan the operation and give the
patient expectations as to the final result.
Vertical skin laxity: The signatures of the high lateral
tension abdominoplasty is to place the highest tension on
the lateral portion of the incision, such that the central
third of the incision is nearly in apposition after closure
of each lateral third. This often means that the old umbilical site does not get excised, leaving a vertical scar from
its closure. While this usually heals well, and accepting the
presence of this scar may be considered part and parcel
with being a true HLT purist, this scar does not always
heal perfectly, and many patients and surgeons indeed do
want to avoid it. There are occasions preoperatively when
the surgeon cannot be certain as to whether the old site
will be able to be excised, without tension but if there is
any question, the patient should be warned that there are
three choices: proceeding with a classically marked HLT
and accepting that vertical scar if it is necessitated for
proper skin tension of excision intraoperatively, perhaps
locating the entire incision more superiorly in order to
increase the likelihood of getting out the old umbilical
site, or simply not doing an HLT, but resecting as much
tissue as necessary centrally in order to remove the site,
even if this means distorting or raising the height of the
mons.
Extent of skin laxity: Many patients today ask for a mini
tummy tuck, wanting the horizontal extent of the incision
to be as short as possible, perhaps even as narrow as their
C-section scar. It is rare to find women whose laxity is so
centrally located that such a short scar removes all of the
laxity that is troubling to the patient while creating a
smooth contour to the abdomen, and the patient should
always be evaluated sitting upright, as this demonstrates
the extent to which the laxity extends laterally. Patients
823
0075_ch69_9780702031687.indd 823
4/8/2009 3:49:29 PM
Section 12: Body contouring/bariatric massive weight loss
Aesthetic Plastic Surgery
Fig. 69.1 With the high angle of the lateral portion of the incision with the HLT, the thigh looks longer. Note the improvement of the quality of skin in the
thigh and inguinal region. The abdomen is smooth and tight, and thought he slit used to close the abdomen has widened with time.
can understand that if the laxity extends to the mid-axillary line that an incision the width of her previous Csection will fail to correct the lateral laxity. Even compared
to the standard abdominoplasty, the HLT does require a
wider incision. That is because the standard tummy tuck
is essentially an exercise in excising the umbilicus; the
width of the incision is determined according to one
parameter: how much is necessary to remove that vertical
excess without creating a dog-ear. But the HLT considers
that lateral excess the most important area for excision. By
pulling down and out laterally, a greater degree of flattening of the epigastrium occurs than pulling simply straight
inferiorly. This can easily be demonstrated to a patient by
creation of downward tension on the epigastrium by
pinching between the umbilicus and just above the mons,
and contrasting that with the greater improvement that
occurs to the epigastrium by simultaneously pinching
lateral, angled down and out, so that the epigastrium is
being pulled in two directions. The greatest laxity on the
trunk of the post-partum or weight loss patient is also
laterally, so this area needs the greatest amount of
excision.
Skin quality and texture: Just like with a mastopexy, after
skin is removed, the same skin that stretched once and
was damaged remains behind. The ultimate quality of the
result and appearance will be based upon the patients
own skin, for which we have little if any control. It is
important to asses the skin in order to give the patient
expectations as to what their particular outcome is likely
to be. Do stretch marks still exist superior to the likely line
of resection so that many will remain, or are they likely
to all be excised? Is the skin thin and/or sun-damaged,
likely to reloosen to a significant degree or have notable
lines or wrinkles? These issues must all be addressed with
the patient preoperatively in order to set their expectations, and patients should further realize that there is no
preoperative test that can predict how their particular skin
will hold up after surgery; the best a surgeon can do is
offer them an educated guess. The presence of pre-existing
abdominal scars must be assessed as they may have
affected blood supply in such a way so as to necessitate
modification of the HLT design, or to limit undermining
even more than usual. Occasionally the scar is adherent
to the underlying abdominal wall and consideration
needs to be given to whether the scar needs to be freed to
allow transfer of tightening forces beyond it, or whether
such a maneuver would compromise blood supply. There
are also sometimes transverse lines of adhesion, usually
824
0075_ch69_9780702031687.indd 824
4/8/2009 3:49:29 PM
Chapter 69 High lateral tension abdominoplasty
Fig. 69.2 Note the dramatic rejuvenation of the entire truncal unit, including the inguinal region and proximal thighs. Note also the more youthful pelvic tilt
as described by Lockwood.
between umbilicus and xyphoid between the midline and
the anterior axillary line that prevent transference of pull
from the abdominoplasty to the tissues cephalad to it. It
can take substantial undermining to free these up, and in
doing so the blood supply to the flap can be compromised. These issues need to be discussed with the patient
preoperatively.
Excess fat within flap: The HLT allows for safe suctioning
of the abdominoplasty flap. The flap should be evaluated
not just for the presence of significant subcutaneous fat,
but for the extent to which this fat is proportional to the
patients overall body habitus. Most important is noting
the thickness at the expected level of flap transection relative to where that tissue will be sewn inferiorly. It is frequently much thicker superiorly, and liposuction of the
flap should be considered to create a smooth transition. I
tend to suction abdominaplasty flaps only occasionally.
The patient population I predominantly see is thin. Moreover, though liposuction of the flap can be done safely, it
does seem to increase the likelihood of seroma formation
and prolong recovery.
Excess fat in contiguous areas: When a patient seems to
have a large amount of fat in their abdominal flap, there
is usually an even greater amount of fat in the pubic area
or the posterior iliac crest area. Too much is made of
liposuctioning of abdominal fat within the flap. Oftentimes, there is not enough to remove to make a significant
difference in the appearance. Usually, the hips contain
substantially more fat in proportion to the abdomen. If
there is a lot to remove in the abdomen, there is usually
more in the hips or the thighs, and it is important to look
at those areas and consider treating them, lest the surgeon
create a disharmonious proportion. With the abdomen
flattened from an abdominoplasty, the width that results
from excess hip fat can be very apparent. In fact, by tightening the abdomen, the width of the hip area can appear
to increase following an abdominoplasty (Fig. 69.3). Narrowing the waist through suction of the posterior hip roll
can dramatically improve the appearance of the abdomen.
Similarly, excess fat in the mons area is often not noted
preoperatively. Either the abdomen may be protuberant
or there may be tissue overhanging the waist. After a
smooth and flatter abdomen, the mons can protrude in
clothing and be disconcerting. This can be treated with
liposuction at the time of abdominoplasty and this area
should be assessed for this preoperatively.
Rectus diastasis/hernia: The patient should be examined
standing, sitting, and laying back flat while raising her
825
0075_ch69_9780702031687.indd 825
4/8/2009 3:49:33 PM
Section 12: Body contouring/bariatric massive weight loss
Aesthetic Plastic Surgery
there to be relapse in any situation, this is certainly exacerbated in cases in which there is the greatest degree of
intra-abdominal fat. This is important because it might
weigh on your choice as to whether or not there is enough
of a benefit from plication to make it worth the additional
recovery. Also, it helps to warn patients about an increased
possibility of the repair loosening and restretching with
time.
Anatomy
Blood supply
Fig. 69.3 Even the slightest hip bulges such as this should be treated with
liposuction lest the waist appears more square following an HLT. Note also
that the scar is wide enough to be noticeable from the postoperative PA
view on the bottom.
shoulders up, as in doing a partial sit-up. This is a good
way to test for a rectus diastasis. From this position, one
can take the patients hands and show them the gap that
exists between their muscles. Some patients will comment
that they need to work out more. But they need to be
reassured that exercise will only increase the strength of
the muscles; only surgery can bring them back together. I
always discuss with patients that they have an option of
whether or not to plicate any diastasis. While the plication
can substantially improve the outcome, so too does it
lengthen the recovery and make it more uncomfortable.
The umbilicus is always assessed for the presence of a
fascial defect that may need to be repaired either separately or at the time of abdominoplasty. The patient
should also be examined in profile with her arms at her
sides and above her head, asking her to allow her abdominal musculature to relax. During plication, it is all too
tempting to tighten her as much as possible from pubis
to xyphoid; more important is to assess the patients laxity
and preplan where the abdomen needs to be tightened to
create the most attractive contour.
Intra-abdominal fat: Pressure from the internal organs
including intra-abdominal fat puts pressure on any repair
that is done of the rectus diastasis. While it is possible for
Plastic surgery is indeed the battle of beauty versus blood
supply whenever an undermined flap is involved, and few
such flaps involve the degree of undermining as does the
abdominoplasty flap. Fortunately, the rich blood supply combined with the limited undermining shown by Lockwood in
his description of the HLT usually results in the creation of
an excellent cosmetic result free from healing problems secondary to vascular insufficiency.
Prior to surgery, the abdominal wall is densely supplied by
vessels coursing inferiorly and medially from the superior
epigastric artery, the subcostal artery, and lumbar branches.
These anastamose with vessels ascending superiorly from the
deep and superficial epigastric vessels.
These anastomoses are obviously disrupted with the
abdominoplasty, leaving the flap to be supplied by the superior vessels that are coursing downward. The blood supply of
the inferior cut edge is not undermined and can be closed
under great tension with no issue of devascularization.
But the superior edge is dependent upon these vessels
coursing inferiorly. While the flap is robust, there is little if
any cosmetic advantage to any more undermining than necessary to complete the resection and expose the area needed for
plication; irregularities seen on the table will flatten out
postoperatively.
The skin/adipose layer
Most patients requesting an abdominoplasty have compromised skin as they are typically either post-partum, postmassive weight loss, or both. These make permanent changes
to the skin that will affect the final outcome. Notation should
be made of the extent, color, and severity of the striae. Redder
striae seem to be predictive of a redder final scar. Striae superior to the anticipated cut edge of the flap will obviously
remain following surgery.
It is not enough to just evaluate the skin of the abdomen.
The HLT is actually a body lifting procedure, and it can significantly tighten and rejuvenate the mons, inguinal region,
and proximal thigh. These areas should be assessed for laxity
and the potential for improvement.
It also must be appreciated that there is both horizontal
and vertical excess of the skin/subcutaneous fat layer. The
horizontal scar of an abdominoplasty obviously reduces the
vertical excess, but what about the horizontal excess? Usually
the body is wider at the height of the lower abdominoplasty
incision than it is at the upper abdominoplasty incision, so
826
0075_ch69_9780702031687.indd 826
4/8/2009 3:49:37 PM
Chapter 69 High lateral tension abdominoplasty
that when the edges are closed, the horizontal excess is apparently eliminated. But there is not a significant change in width
of the abdomen from the level of the xyphoid down to about
the level of the umbilicus; in fact, the body often narrows.
What this means is that the tissue that is transferred down
from the upper to the mid-abdomen during a tummy tuck
develops even greater horizontal laxity when a traditional
abdominoplasty is done, as the incision is relatively parallel
to the ground and the greatest pull is straight inferiorly. But
with the HLT, the lateral limbs of the final closure diverge
superiorly in an oblique direction, and they hold the greatest
amount of tension. This serves to excise that horizontal
redundancy in the epigastrium, thereby flattening it and significantly improving the abdominal contour.
The abdomen as well as these areas should be assessed for
laxity and the presence of fat, will determine how wide the
incision will need to be, and the direction of greatest laxity
will ultimately affect the angle of the lateral limbs of the HLT,
as tension will obviously be greatest perpendicular to those
angles. Lockwood has shown that the greatest redundancy is
usually laterally rather than centrally. While high central
tension distorts the mons, high lateral tension smooths out
the inguinal region and proximal thighs, and confers greater
smoothing effects to the epigastrium than does high central
tension.
Musculofascial layer
The abdominal wall itself is made of four major paired muscle
groups: the transversus abdominis, the external oblique,
internal oblique, and rectus abdominis muscles. Ideally, the
rectus sheath that envelopes the rectus muscles fuses in the
midline, forming a narrow and stout structure that maintains
just a few mm separation between the muscles. However with
pregnancy, and to a lesser extent weight loss, the linea can
attenuate and stretch, allowing the distance between the
muscles to separate. This is easiest to examine when the
patient does a sit-up. Whatever gap is noted during that
maneuver is amplified when the patient stands upright and
the pressure of the viscera is applied to the uncontracted
abdominal wall. A rectus diastasis is only a gap; it is not synonymous with a hernia. A true midline hernia is extremely
rare in the absence of a previous midline laparotomy incision.
Quite common, however, is an umbilical hernia. Every
abdominoplasty patient should be examined to assess for the
presence of one. Deep within the base of the umbilical stalk,
a fascial defect can be felt at the time of exam. This is important as it can worsen with time. Once noted, it should be
pointed out to the patient at the time of consultation, and if
ultimately she does not wish to undergo an abdominoplasty,
she should be advised to seek consultation with a general
surgeon for repair of the hernia.
Technical steps
See Fig. 69.4.
Photography should be done in a complete and consistent
manner. All patients should have photos of the entire aes-
thetic area from the shoulder to knee. Sometimes when the
view is too cropped, the effect of the result on the patients
overall physique is not as noticeable as when there is a wider
view. Images should be taken both AP and PA, both laterals,
and all four obliques. Photos should always be taken with
the patient sitting, particularly if the patient is thin and there
is not significant skin redundancy appreciated when standing
(Figs 69.569.7). Frankly, the abdomen always looks much
worse in a seated photo, but this is a position in which we
spend much of our lives, and the exaggeration of abdominal
redundancy noted in this position must be reckoned with.
The photos do not just force the surgeon to notice everything
relevant to the surgery and act as a basis for discussion with
the patient, but they serve a critical role of demonstrating for
the patient the rationale for the surgery down the road should
they question the width of the scar or the extent of improvement. Standardized photos can do much to allay patient
concern and anxiety. The recovery from the procedure is long
and there are often times in which a patient asks themselves
whether it was worth it; seeing the original picture can be very
helpful for them. If the scar ends up wide or thick, the photos
can remind the patient that the scar is less problematic than
their laxity.
Determining the position of the incision is the most critical
part of the operation. Always bear in mind two often conflicting forces: the surgeons determination of what scar will create
the best contour, and the patients wishes for the location of
the scar.
Oftentimes, the surgeon would like the lateral limbs of a
HLT scar to elevate more superiorly laterally than the patient
wants. I have never had a patient complain that I didnt create
a harmonious appearance to their abdomen, touted as an
advantage of the HLT by Lockwood. But I have had patients
complain that the lateral part of the scar was exposed above
low riding jeans or bikinis. Patients need to understand that
the upward angle of the scar allows for greater flattening of
the epigastrium and overall contour than a more horizontal
scar. While I believe that a significantly convex scar creates a
more pleasing contour, I have become increasingly willing to
make the scar more horizontal in order to satisfy patient
request. While I have seldom had a patient complain that I
could have created a more aesthetic trunkal unit a goal
of the HLT I have had complaints about the scar extending
above low riding jeans.
The patient wears a bikini bottom or underwear that is
typical of the style she likes to wear. Frequently, patients are
now wearing underwear that is relatively horizontal, preventing the scar from rising laterally as much as necessary to create
high tension that pulls obliquely from each lateral limb
against the epigastrium, thereby forcing the scar to be lower
and more horizontal than optimal for giving the patient the
best possible contour. There are two ways to deal with this.
First, one can advise the patient that a higher scar laterally
will give a better appearance to the abdomen, which is usually
the biggest concern to the patient. But it is also true that styles
change, and sooner or later swimsuits and underwear will
ride up higher again on the hips, meaning that a low scar
would be visible in even one-piece suits. However, a high scar
that is optimal for an HLT will always be covered by a one-
827
0075_ch69_9780702031687.indd 827
4/8/2009 3:49:40 PM
Section 12: Body contouring/bariatric massive weight loss
Aesthetic Plastic Surgery
Fig. 69.4 A, The outline of a typical pair of the patients panties is drawn. Then the proposed nal scar location is drawn (as shown here by the dotted blue
line). With the pen held at the level of that line, the skin is pushed cephalad with the expected amount of tension on the closure at that area to determine
where the initial incision must be made for the nal scar to end up at that dotted line. B, The patient is marked, measured, and checked multiple times for
symmetry. C, I have found it difcult to draw straight lines while holding a tape measure at against the body; use of 2-inch tape has facilitated the ability to
draw straight lines. D, Using the tape to checkerboard the stomach greatly facilitates drawing even lines of resection intraoperatively and makes nal closure
more precise. E, There should be about 7 cm of hairbairing skin on stretch above the anterior vulvar commissure. F, The PlasmaJet used to paint the entire raw
surface, reducing bleeding and sealing lymphatics, thereby reducing the time a drain is necessary and reducing the likelihood of seromas.
828
0075_ch69_9780702031687.indd 828
4/8/2009 3:49:40 PM
Chapter 69 High lateral tension abdominoplasty
Fig. 69.4, contd G, The Lockwood Dassumpco clamp is used to mark the extent of resection. It is critical to pull on the ap in the direction that it will be
closed and with the amount of tension that you wish to put on that part of the ap. There is less tension placed centrally, as high tension would distort the
mons. More tension is used laterally. After hash marks are made with the table exed at about 30 degrees, the patient is laid at, and the nal resection line is
made, using the checkerboard to assess symmetry. H, Final resection. Note not just the obviously greater resection laterally than centrally, but that in fact the
lateral resection is just a bit more than the central resection (see resection relative to original preoperative horizontal line from the preoperative markings). Also
note that even the upper line seems to drop inferiorly centrally, while the more lateral part of what was once a horizontal line rises up laterally. This is part of
the confusion of the HLT. While in fact there is more taken laterally than centrally, it is only a bit more, not a lot more. Most of what appears to be a greater
amount taken laterally is really due to the way the tissue is adherent to the deeper structures. I, The vertical lines are extremely helpful in arranging a speedy
and well-aligned closure. Note the umbilicus marking clamp; the deep side of the clamp is around the umbilical stalk, and the other side can be used to mark
exactly where that is transferred to the front. J, It is important for the closure to incorporate a sturdy bite of the cut edge of the SFS. The layer is always more
stout in the inferior cut edge than the superior edge. It tends to retract a signicant degree in the central third of the abdomen, and one needs to really.
K, Though usually less obvious than in the inferior edge, there is a prominent SFS in the superior ap. #1 Nurolon soaked in Betadine is used to make a tight
deep closure, taking all the tension off of the skin. L, Liposuction is performed at the end of the incision to reduce dog-ear and bulk in all but the thinnest of
patients. The extreme lateral tension requires that the incision be lengthened, but even with that, there still tends to be a thickening at the waist if the extra fat
829
is not removed.
0075_ch69_9780702031687.indd 829
4/8/2009 3:49:48 PM
Section 12: Body contouring/bariatric massive weight loss
Aesthetic Plastic Surgery
Fig. 69.4, contd M, The Insorb subcuticular stapler has reduced closing times and made the wound edges more evenly approximated. Because of the
double Adson forceps, it can help to smoothly redistribute mismatches in lengths of the two aps. Reducing operative time is an important part of reducing
DVT and PE risk, and the fact that scars are at least as good with this as with sutures argue strongly for its adoption. N, With the HLT, the greatest tension is
lateral. When it is closed, the incision above the pubic area almost comes together without a clamp in the area. This maximally rejuvenates the thighs as well
as the epigastrium, applying an oblique angle of tension to the epigastrium from each limb. The incision angles up more than a standard abdominoplasty in
the lateral area, and it also extends wider into the ank in order to not have a dog ear from the large lateral resection and tension that is thereby created.
O, Closure with a traditional abdominoplasty pulls most of the tension centrally. The only improvement to the epigastrium is that which occurs from the
straight downward tension, and there is no oblique lines of tension pulling on the thighs and epigastrium as there is with the HLT. P, This patient is lying
supine. The horizontal lines were drawn straight with a laser level, yet they are pulling up somewhat from the midline. Once the ap is released along the
lower incision, this happens to an even greater extent, thereby accentuating the perception of the extent of lateral tension. In reality, the resection is often only
a little bit more laterally than centrally with an HLT (blue line). But with a standard, the surgeon is usually focused on just getting out the old umbilical site,
and the length of the incision is that which is dictated to close it without skin redundancy (green line). Therefore, the standard usually does not have as wide
of an incision as does the HLT. Though the HLT resection drawn in blue here was able to be done on this patient, the HLT frequently results in non-excision of
the umbilicus. So long as there is sufcient lateral tension, there will not be laxity and redundancy in the epigastrium. One must be diligent about creating
adequate lateral tension, and be willing to extend the incision as far laterally as necessary to accomplish this.
830
0075_ch69_9780702031687.indd 830
4/8/2009 3:49:54 PM
Chapter 69 High lateral tension abdominoplasty
Fig. 69.5 Muscle wall laxity, skin redundancy, and fat excess should all be
assessed and documented.
Fig. 69.6 The same patient leaning slightly forward; it is not enough to
examine a patient standing. Standing is good for assessing adipose deposits,
but laying at and doing a sit-up is important for assessing the muscles, and
sitting down and bending forward is crucial for assessing skin laxity.
Fig. 69.7 There is always signicant scar with any abdominoplasty; document the patient in a position that most shows the deformity to be shown to them
later. Note that the vertical scar is still in somewhat of a slit; this will spread over the course of a year or more and become more round.
831
0075_ch69_9780702031687.indd 831
4/8/2009 3:49:57 PM
Section 12: Body contouring/bariatric massive weight loss
Aesthetic Plastic Surgery
piece and will be above it and visible only with a low onepiece. Ultimately, the patient must know what to expect with
the scar. The other option when the patient wants the scars
low is to make the scar lower above the mons, which allows
one more room to let the scar course more superiorly up to
the lateral ends of the incision. But one must be careful not
to remove too much hair-bearing skin in the pubic region;
generally it should be about 6.57 cm from the anterior labial
commissure to the top of the pubic hair on maximum stretch.
And the other problem with lowering the scar centrally is that
it makes it that much more likely that the old umbilical site
will not be able to be excised, and that a short vertical scar to
close it will remain in the infraumbilical/suprapubic region.
While most all facelifts can begin with a similar initial incision around the ear, varying only in final skin excision, the
initial abdominoplasty incision lacks the concrete anatomical
landmarks of the ear, and given various abdominal configurations and patient wishes, the initial incision must be customized to each patient.
The midline is marked from xyphoid to umbilicus to the
labial commissure. While it is embarrassing to mark this,
many women today have pubic hair that is trimmed unevenly,
so that drawing a line to the center of the pubic hair can result
in a crooked inset of the flap. I then draw a number of vertical
lines parallel to the first line from the midline going out laterally to where the incision is expected to end (Fig. 69.8). Additional horizontal lines are drawn to create a checkerboard on
the abdomen. This helps not just at this point while marking
the patient, but it makes for a much more rapid determination of final resection, reduces the likelihood of unevenness
of resection, and facilitates insetting the flap by lining up the
closure.
A line is then drawn where you would like the final scar
to be. The patient must inspect this and any compromises
discussed and made. This line is not where an incision will
be made! Because tension will vary along the length of the
incision, there are points at which this will be pulled up by
the final closure greater than at other areas. So with a pen
held horizontally at the level of the desired final scar, the
abdomen is pushed up superiorly with the expected tension
of the final closure at that point. This will yield a series of
dots below the incision. They are checked side by side for
evenness. I use a laser level to assure that both ends of the
incision are parallel to the floor (Fig. 69.9). Check to assure
that the incisions are also located at the same point relative
to the hipbone. If there are discrepancies between what is
even with the floor and what is even with the body, it needs
to be pointed out to the patient, discussed, and documented.
The final scar will never be symmetrical. Consents for abdominoplasty should require patients to initial the statement the
scar will not be symmetrical. Extend the lines for the incision
beyond what you think you will need, as this provides for
Fig. 69.8
Pre-incision view of the patient in Fig. 69.9.
Fig. 69.9 The laser level is used to establish
true vertical and horizontal lines. These are
assessed and compared to the patients own
anatomic landmarks. Few patients are symmetric,
and this allows for notation and documentation
that choices about how to deal with the
asymmetries were made with the patient.
832
0075_ch69_9780702031687.indd 832
4/8/2009 3:50:05 PM
Chapter 69 High lateral tension abdominoplasty
removal of any dog-ear with placement of the incision in the
proper location. Keep in mind that some of these patients will
at some stage decide to get the posterior part of a lower body
lift added, so end the incision at a point that would be within
a lower body lift scar. Mark the umbilicus at 12, 3, 6, and 9
so that it is easy to identify those areas and to inset the umbilicus later without concern for there being a twist. Areas for
liposuction are marked in the usual manner. Photographs are
taken of the marked patient and are printed and posted in
the operative room for intraoperative reference.
The patient is given a general anesthetic. A pillow is placed
behind the knees to increase venous flow and to take tension
off of the abdomen. The legs are slightly frog-legged to
further reduce tension on the lateral part of the incision. The
most critical perioperative decision revolves around DVT prophylaxis. Compression boots are used in all cases; consideration must be given to chemoprophylaxis. Guidelines of ASPS
should be referenced as recommendations are likely to change.
A single dose of perioperative antibiotics are given.
Incision is made and dissection continued with an electrocautery. Superficial epigastric vessels are identified and ligated.
Dissection proceeds up towards the umbilicus. A periumbilical incision is made and dissection is carried widely down
and around the umbilicus to its base. If the site is likely not
going to be excised, one may consider leaving less tissue
around the umbilicus as it can result in a depression deep to
the closure of the old umbilical site.
If it is obvious that the umbilical site will be removed, the
flap should be split to allow for easier dissection up towards
the xyphoid. Dissection should be no wider than necessary
to complete the plication.
Marcaine with epinephrine is injected along the rectus
sheath. Towel clamps are used to approximate the rectus
closure. Simple interrupted #1 Nurolon sutures soaked in
Betadine are used to place the first row. Figure-of-eight sutures
can also be used. Figure-of-eight sutures will shorten the vertical height of the rectus muscle by the cumulative effect of the
compression created between the upper and lower bites of
each of the sutures. While it is difficult to compare, it seems
that figure-of-eight sutures create more post-operative pain
and that it takes longer for patients to stand fully upright,
presumably due to the shortening that occurs from them.
Sutures should not be placed along exactly the same vertical
plane; though this looks neat, it creates a vertical line of weakness in which a small tear could progress to a longer tear. For
this reason, the suture bites are slightly staggered so that a
nidus of a fascial tear created by one bite does not progress
along the entire repair. If patients ever complain about their
abdominal contour, it is usually of an epigastric bulge, not a
hypogastric bulge. For this reason, start the plication at the
xiphoid and work inferiorly. If the plication begins inferiorly,
the tightened lower abdomen shifts abdominal contents and
results in less upper plication, and it is important to assure
good upper plication in order to avoid this bulge. Following
the interrupted sutures, a running 0 Prolene is placed starting
at the umbilicus and run all the way to the umbilicus; at the
xyphoid, it is perfunctorily run along one side of the umbilicus and once below it, the repair again continues. Tension
should not just be according to the most that can be created;
the goal is improving contour, so reference to the lateral preoperative views is helpful in planning the plication.
The flap is irrigated, debris is washed away, and hemostasis
is achieved. I have been using the PlasmaJet for improved
hemostasis and to seal lymphatics in an effort to reduce
seroma formation, and the preliminary results are
promising.
The patient is sat up only about 25 or 30 degrees; sitting
up more than that makes it too easy to over-resect centrally,
and it does not allow for significantly more lateral resection
which is where resection is emphasized. Start by determining
the amount of resection that can be done centrally. In the
traditional abdominoplasty, the surgeons mind is focused on
removing the old umbilical site. In the HLT, the surgeon is at
peace with leaving that site behind, but if it can be removed,
so much the better. Do not have the mons completely draped
off, as the amount of resection is determined by mons distortion. No more than a small of distortion should be accepted
and the extent to which the pubic hair is pulled cephalad is
also noted, as there must be an adequate distance left between
the umbilicus and the top of the pubic hair. Once this is
determined, the flap is split up to this point and tacked into
place. The Lockwood flap marker is then used to mark the
remaining flap, taking note that there should be greater
tension laterally than centrally. After it is marked, the central
clamp is released and the patient is laid flat again. The proposed excision is then carefully drawn assuring symmetry
(Figs 69.1069.12).
The excision is done with a knife in the skin and then a
cautery, pulling on the discarded part of the flap to assure that
the cut is done perpendicular to the cut edge. Lockwood
advocated back-cutting the flap in order to create a redundancy in the skin by the closure of the SFS; I have only had
devascularization of the skin edges on the occasions I have
done this, so it should be done with care and caution.
Fig. 69.10 Another example of the line for nal resection. The horizontal
lines drawn preoperatively are now elevated at closure. Though the planned
resection looks like it is going much higher laterally, if you look at the original
grid, it is obvious, that it is not even horizontal. So, although it is true that the
tension is higher laterally, the excision is often as much or even a little more
centrally.
833
0075_ch69_9780702031687.indd 833
4/8/2009 3:50:10 PM
Section 12: Body contouring/bariatric massive weight loss
Aesthetic Plastic Surgery
Fig. 69.11 After the nal resection, the extent to which the resection is
greater laterally is noted, in this case about 112 inches. But this varies with the
tension on the skin aps, and there are times that it is almost horizontal, yet
the tension is greater laterally than centrally.
Drains are placed as well as a pain pump, if desired. The
patient is sat back up, tacked shut, the umbilicus is matured,
and closure is done. Lockwood advocated a vertical slit with
no excision. If indeed the lateral arms of the abdominoplasty
are oblique, then their closure under tension will help to
open up the slit. One should be cautious about umbilicoplasty designs that might be prone to enlarge from the high
lateral tension.
The SFS is closed with simple buried 0 Nurolons dipped
in betadine. This should take all of the tension off of the
closure. Insorb absorbable subcuticular stables are used next.
They save significant time relative to individually placed
sutures, and reducing OR time is a goal one should strive
toward in order to reduce the likelihood of DVT and PE. It
also helps to even out thickness disparities between the two
flaps and it helps in evening out differences in length between
the two edges in that it uses a double Adson forceps which
are very helpful in cheating the longer side to line up evenly
with the shorter side. The final skin closure is done with 4-0
Monocryl followed by Steri-Strips.
Postoperative care
The Foley is removed at the conclusion of the operation to
assure that the patient walks the night of surgery. Since it is
hard to be sure that a patient will ambulate if in a recovery
center or a hospital, those patients are given compression
boots postoperatively. Chemoprophylaxis must be considered for DVT, and surgeons should refer to the most recent
recommendations of the ASPS. Pain pumps can be used, but
their efficacy has not been conclusively shown. One of the
most common reasons for flap loss is a tight dressing; any
dressing must be inspected the evening of surgery after the
patient has settled in the recovery facility and again several
times a day. Abdominal binders can be used, but it must be
emphasized to nursing staff that they are there only to hold
the dressing in place and to pin the drains to for the first few
days; only after that point can they start to be tightened. Most
Fig. 69.12 The blue lines on the patient were horizontal when drawn on
the patient standing. Following dissection, the lateral portion of the lines drift
superiorly and the central portion drifts inferiorly. Despite the high lateral
tension, note in this case that there is actually even a bit less removed
laterally than centrally. Observe also the pufness observed from the limited
undermining for the plication. This will smooth out in the initial weeks
postoperatively, and so there is no reason to reduce blood supply by
undermining enough to atten it out.
abdominal binders are too wide for most women, and as they
slide in bed, the top of the binder rubs under their breasts;
this is always uncomfortable, but it can be a significant
problem for a woman with an incision under her breasts from
concomitant mastopexy or reduction. As patients swell and
as their position changes in bed, what seemed like a loose
dressing can frequently tighten. The best way to prevent this
is to avoid large dressings, and if one is used, to cut the tape
in small pieces that are put at angles so as to avoid a horizontal constriction band. Depending upon where the patient
goes after surgery, sometimes IV fluids are continued to assure
hydration and blood flow to the flap. Compression boots are
used as long as a patient is in a hospital or recovery center.
Complications
Pulmonary embolism remains the most devastating complication of abdominoplasty. Risk seems to be increased by
performing other simultaneous procedures and is higher in
patients taking hormone supplements and with recent airline
travel. Compression boots should always be used and chemoprophylaxis always considered. It is unclear whether
muscle plication increases the risk, but so long as this is a
possibility, consideration should be given to forgoing plication in patients in whom there does not seem to be a significant advantage from performing the plication. Reducing
operating times, maintaining good hydration and early mobilization all help to reduce the risk. The office staff and the
patient must all be trained to be aware of the early signs of
DVT and PE.
Less serious problems are recurrent seroma formation.
Meticulous hemostasis appears to reduce the likelihood of
this occurrence, along with the use of the PlasmaJet. The
incidence appears to increase with concomitant liposuction.
834
0075_ch69_9780702031687.indd 834
4/8/2009 3:50:11 PM
Chapter 69 High lateral tension abdominoplasty
Pearls & pitfalls
Pearls
Pitfalls
Accept that removing the umbilical site is not a goal of the
procedure.
Realize that pulling inferolaterally from the epigastrium to
each groin most optimally rejuvenates the epigastrium and
avoids the distortion of the mons seen with a standard
abdominoplasty.
The HLT requires a longer scar than a traditional procedure
because of the amount of skin taken laterally, and it requires
that the lateral limbs be angled upwards so that they are
pulling at oblique angles towards the epigastrium. The
patient must be made aware of this and accept this.
Recognize that the nal scar is not where the initial incision
was made; it will oat superiorly based upon the tension
following nal resection.
The patient needs to know ahead of time how long the scar
will be; they also need to know that even with optimal SFS
repair that it may still widen. Many patients have a C-section
scar that they wish to compare it to; while occasionally it can
look that good, since the C-section scar heals in a condition
of skin laxity and the HLT in a condition of tension, the HLT
usually spreads more.
It sometimes seems very easy to pull just a bit more to
remove the umbilical site, but avoid the temptation to do so
if it distorts the mons or raises the pubic hair so high that the
umbilicus seems to close to the top of the pubic hair.
Sometimes the transition from the very high lateral tension
at the end of the incision to the unpulled skin behind it
results in a large dog-ear of sorts. With a traditional abdominoplasty, the greatest tension is in the center, so there is a
relatively long distance at which the tension gradually
diminishes. To reduce this, it is often necessary to lengthen
the incision and/or to perform aggressive liposuction to
defat this area.
PE, PE, PE. This cannot be overstated. Every patient should
be considered to be at risk. Keep abreast of the most current
recommendations. This is a very real and even inevitable
complication, but being diligent about avoiding it and
recognizing early signs and symptoms can reduce the
incidence and consequence.
Summary of steps
1.
2.
3.
4.
5.
6.
7.
Carry out photography.
The patient wears a bikini bottom or underwear that is
typical of the style she likes to wear.
The midline is marked from xyphoid to umbilicus to the
labial commissure. A number of vertical lines may be
drawn parallel to the rst line from the midline going out
laterally to where the incision is expected to end.
Additional horizontal lines are drawn to create a
checkerboard on the abdomen.
A line is then drawn where you would like the nal scar to
be.
The patient is given a general anesthetic.
Incision is made and dissection continued with an
electrocautery.
If it is obvious that the umbilical site will be removed, the
ap should be split to allow for easier dissection up
towards the xyphoid.
8.
9.
10.
11.
12.
Marcaine with epinephrine is injected along the rectus
sheath. Suturing is then done.
The ap is irrigated, debris is washed away, and
hemostasis is achieved.
The patient is sat up about 25 or 30 degrees. The amount
of resection that can be done centrally is determined. The
proposed excision is then carefully drawn assuring
symmetry.
The excision is done with a knife in the skin and then a
cautery, pulling on the discarded part of the ap to assure
that the cut is done perpendicular to the cut edge.
Drains are placed as well as a pain pump, if desired. The
SFS is closed with simple buried 0 Nurolons dipped in
betadine. The nal skin closure is done with 4-0 Monocryl
followed by Steri-Strips.
835
0075_ch69_9780702031687.indd 835
4/8/2009 3:50:14 PM
Section 12: Body contouring/bariatric massive weight loss
Aesthetic Plastic Surgery
Further reading
Lockwood TE. High-lateral-tension abdominoplasty with
superficial fascial system suspension. Plast Reconstr Surg
1995;96(3):603615.
Lockwood TE. The role of excisional lifting in body contour
surgery. Clin Plast Surg 1996;23(4):695712.
Matarasso A. Abdominolipoplasty: A system of classification and
treatment for combined abdominoplasty and suction-assisted
lipectomy. Aesthet Plast Surg 1991;15(2):111121.
Lockwood TE. Is the standard abdominoplasty obsolete? In:
JurkiewiczMJ, Culbertson JH, eds. Operative techniques in
plastic and reconstructive surgery: Abdominoplasty.
Philadelphia, PA: WB Saunders, 1996, pp. 7781.
Matarasso A. Liposuction as an adjunct to a full abdominoplasty
revisited. Plast Reconstr Surg 2000;106(5):11971202.
Lockwood TE. Lower body lift with superficial fascial system
suspension. Plast Reconstr Surg 1993;92(6):11121122.
Matarasso A. Liposuction as an adjunct to a full abdominoplasty.
Plast Reconstr Surg 1995;95(5):829836.
Lockwood TE. Lower-body lift. Aesthet Surg J 2001;
21(4):355370.
Shestak KC. Marriage abdominoplasty expands the miniabdominoplasty concept. Plast Reconstr Surg
1999;103(3):10201031.
Lockwood TE. Maximizing aesthetics in lateral-tension
abdominoplasty and body lifts. Clin Plast Surg
2004;31(4):523537.
Teitelbaum S. Demystifying high-lateral-tension abdominoplasty.
Aesthet Surg J 2006;26(3):325329.
Lockwood TE. Superficial fascial system (SFS) of the trunk and
extremities: a new concept. Plast Reconstr Surg
1991;87(6):10091018.
836
0075_ch69_9780702031687.indd 836
4/8/2009 3:50:14 PM
Вам также может понравиться
- Plastic & Hand Surgery in Clinical Practice: Classifications and DefinitionsОт EverandPlastic & Hand Surgery in Clinical Practice: Classifications and DefinitionsОценок пока нет
- Simple MastectomyДокумент3 страницыSimple MastectomyCindy DayocОценок пока нет
- Traditional AbdominoplastyДокумент23 страницыTraditional AbdominoplastyNguyen DuongОценок пока нет
- Structural Fat GraftingДокумент19 страницStructural Fat GraftingGautam KalraОценок пока нет
- Compartment Syndrome: Sebelas Maret UniversityДокумент8 страницCompartment Syndrome: Sebelas Maret Universitykhrisna satyaksaОценок пока нет
- Inflammatory Bowel Disease: DefinitionДокумент4 страницыInflammatory Bowel Disease: Definitionkarl abiaadОценок пока нет
- Surgery Sheet SchemeДокумент51 страницаSurgery Sheet SchemeReem E.MОценок пока нет
- Fat Emboli in LiposuctionДокумент34 страницыFat Emboli in LiposuctionRicky Herdianto100% (1)
- Supracondylar FractureДокумент53 страницыSupracondylar Fracturedesire kbpОценок пока нет
- Carcinoma of The Breast - Bailey & LoveДокумент5 страницCarcinoma of The Breast - Bailey & LoveKeyshia Yazid100% (1)
- Stoma Examination OSCE GuideДокумент5 страницStoma Examination OSCE GuideEssa AfridiОценок пока нет
- Gynecomastia Surgery - Power Assisted LiposuctionДокумент4 страницыGynecomastia Surgery - Power Assisted LiposuctionAlfredo Callanta,M.D.Оценок пока нет
- Urethral InjuryДокумент56 страницUrethral InjuryParty NoriОценок пока нет
- ComponentsДокумент5 страницComponentsprakashmathewОценок пока нет
- Blunt Trauma AbdomenДокумент41 страницаBlunt Trauma AbdomenSanthanu SukumaranОценок пока нет
- SurgeryДокумент12 страницSurgeryManusheeОценок пока нет
- Surgery CaseДокумент43 страницыSurgery CaseAvni GuptaОценок пока нет
- Amputation in Lower LimbsДокумент35 страницAmputation in Lower LimbsSamОценок пока нет
- Staplesinsurgery 170529191209Документ30 страницStaplesinsurgery 170529191209Elena CaterevОценок пока нет
- Vascular Diseases (1 of 3)Документ4 страницыVascular Diseases (1 of 3)Doctor GeneralОценок пока нет
- Introduction To Trauma: LSU Medical Student Clerkship, New Orleans, LAДокумент31 страницаIntroduction To Trauma: LSU Medical Student Clerkship, New Orleans, LAnandangОценок пока нет
- Dr. Rani - Surgical Management of Pressure SoreДокумент19 страницDr. Rani - Surgical Management of Pressure SoreOtto NaftariОценок пока нет
- Esophageal Motility Disorders FinalДокумент48 страницEsophageal Motility Disorders FinalAshish SatyalОценок пока нет
- 4-Conservative Treatment FX, CastingДокумент53 страницы4-Conservative Treatment FX, CastingMuhammad TaqwaОценок пока нет
- History:: Breast History and ExaminationДокумент4 страницыHistory:: Breast History and ExaminationkylieverОценок пока нет
- Latissimus Dorsi FlapДокумент17 страницLatissimus Dorsi Flapokida192Оценок пока нет
- SC - Fracture ZMHДокумент51 страницаSC - Fracture ZMHMis StromОценок пока нет
- Neck Examination PDFДокумент2 страницыNeck Examination PDFNizam Mischievous'Lovely Schremo BoyysОценок пока нет
- Oncoplastic and Reconstructive BreastДокумент14 страницOncoplastic and Reconstructive BreastYefry Onil Santana Marte100% (1)
- SAGES Gallbladder CBDДокумент54 страницыSAGES Gallbladder CBDSAGESWeb100% (1)
- Neligan Mandible FractureДокумент17 страницNeligan Mandible FractureRibka TheodoraОценок пока нет
- ElectrosurgeryДокумент22 страницыElectrosurgeryRavish BangreОценок пока нет
- Incisional HerniaДокумент13 страницIncisional HerniaMaya Dewi permatasariОценок пока нет
- Barium StudyДокумент34 страницыBarium StudyJahanavi JaluОценок пока нет
- SurgeryДокумент13 страницSurgerykarendelarosa06100% (2)
- Traumatic Amputations: Lisa K. Cannada MDДокумент111 страницTraumatic Amputations: Lisa K. Cannada MDaatir javaidОценок пока нет
- DR TahirДокумент61 страницаDR TahirRohail GulОценок пока нет
- StomasДокумент4 страницыStomasSaravanan Sridharan100% (1)
- Anorectal Surgery PDFДокумент33 страницыAnorectal Surgery PDFLuminitaDumitriuОценок пока нет
- Surgical Anatomy-Anal Canal: Dr. Belal MansoorДокумент79 страницSurgical Anatomy-Anal Canal: Dr. Belal MansoorYogi drОценок пока нет
- Anal ProblemsДокумент35 страницAnal ProblemsSandip VaghelaОценок пока нет
- Surgical Management of ObesityДокумент13 страницSurgical Management of Obesityمحمد حميدانОценок пока нет
- Of The Multiply Injured PatientДокумент29 страницOf The Multiply Injured PatientAjay DherwaniОценок пока нет
- ROJA RANI Abstract For PosterДокумент4 страницыROJA RANI Abstract For Postersaikrishnamedico100% (1)
- Hernia Examination SchemeДокумент4 страницыHernia Examination Schemeatribecalledquest20Оценок пока нет
- Burn WoundДокумент68 страницBurn WoundjrefkyОценок пока нет
- What Is A Gastrectomy?Документ4 страницыWhat Is A Gastrectomy?Priyanka JangraОценок пока нет
- Master Degree in Plastic Surgery ThesisДокумент117 страницMaster Degree in Plastic Surgery ThesisMohamed Ahmed El-RoubyОценок пока нет
- Open Inguinal Hernia RepairДокумент6 страницOpen Inguinal Hernia RepairKris TejereroОценок пока нет
- Clinical Practice Guidelines 2012Документ50 страницClinical Practice Guidelines 2012Immanuel Van Donn Batubara100% (1)
- Plastic Surgery: Acharya Institute of Allied Health Sciences By: Ishika Basak BHA, 2 YrДокумент14 страницPlastic Surgery: Acharya Institute of Allied Health Sciences By: Ishika Basak BHA, 2 Yrlokitoka zigОценок пока нет
- Carcinoma Penis Management: Dr. Lilamani Rajthala MS Resident Moderator: Dr. Samir ShresthaДокумент63 страницыCarcinoma Penis Management: Dr. Lilamani Rajthala MS Resident Moderator: Dr. Samir ShresthaBibek GhimireОценок пока нет
- Postcholecystectomy SyndromeДокумент27 страницPostcholecystectomy SyndromeMonica TurnerОценок пока нет
- Oncoplastic Breast SurgeryДокумент20 страницOncoplastic Breast SurgeryGeorge Yacoup100% (1)
- Dr. Robert Tirtowijoyo (Paediatric Condition) Inggris UMJ Maret 2008 EditedДокумент73 страницыDr. Robert Tirtowijoyo (Paediatric Condition) Inggris UMJ Maret 2008 EditedMuhamad Agung SupriyantoОценок пока нет
- Ulcer, Cyst, Tumoures, Sinus, FistullaДокумент40 страницUlcer, Cyst, Tumoures, Sinus, Fistulladrhiwaomer100% (2)
- CME Trunk, Abdomen, and Pressure Sore ReconstructionДокумент15 страницCME Trunk, Abdomen, and Pressure Sore ReconstructionVeronica TomaselloОценок пока нет
- Management of Acute Appendicitis in Adults - UpToDateДокумент28 страницManagement of Acute Appendicitis in Adults - UpToDateaulia rachman100% (1)
- Fracture FemurДокумент21 страницаFracture FemurDanus RamadanusОценок пока нет
- VVVДокумент9 страницVVVAhmad Arbi AninditoОценок пока нет
- APДокумент12 страницAPAhmad Arbi AninditoОценок пока нет
- AHДокумент11 страницAHAhmad Arbi AninditoОценок пока нет
- ALДокумент16 страницALAhmad Arbi AninditoОценок пока нет
- AFДокумент4 страницыAFAhmad Arbi AninditoОценок пока нет
- ANДокумент12 страницANAhmad Arbi AninditoОценок пока нет
- FFFДокумент8 страницFFFAhmad Arbi AninditoОценок пока нет
- RRRДокумент8 страницRRRAhmad Arbi AninditoОценок пока нет
- UuuДокумент10 страницUuuAhmad Arbi AninditoОценок пока нет
- JJJДокумент10 страницJJJAhmad Arbi AninditoОценок пока нет
- LLLДокумент6 страницLLLAhmad Arbi AninditoОценок пока нет
- Hum. Reprod.-2013-Romosan-1569-79Документ11 страницHum. Reprod.-2013-Romosan-1569-79Ahmad Arbi AninditoОценок пока нет
- TTTДокумент8 страницTTTAhmad Arbi AninditoОценок пока нет
- GGGДокумент8 страницGGGAhmad Arbi AninditoОценок пока нет
- J Gastrointest SurgДокумент12 страницJ Gastrointest SurgAhmad Arbi AninditoОценок пока нет
- AДокумент12 страницAAhmad Arbi AninditoОценок пока нет
- EeeДокумент8 страницEeeAhmad Arbi AninditoОценок пока нет
- ACCPioДокумент8 страницACCPioAhmad Arbi AninditoОценок пока нет
- ACCPioДокумент12 страницACCPioAhmad Arbi AninditoОценок пока нет
- Clinical Science Session: Oleh Ahmad Arbi Anindito 1018011036Документ1 страницаClinical Science Session: Oleh Ahmad Arbi Anindito 1018011036Ahmad Arbi AninditoОценок пока нет
- Figo PPH 2012Документ12 страницFigo PPH 2012Ahmad Arbi AninditoОценок пока нет
- Prevention and Management of Primary Postpartum Haemorrhage-Clinical Practice Guideline FinalДокумент27 страницPrevention and Management of Primary Postpartum Haemorrhage-Clinical Practice Guideline FinalLeonardo RikatsyaОценок пока нет
- CDC - Pelvic Inflammatory Disease - 2010 STD Treatment GuidelinesДокумент7 страницCDC - Pelvic Inflammatory Disease - 2010 STD Treatment GuidelinesAhmad Arbi AninditoОценок пока нет
- Improving Aesthetics in Lateral Tension AbdominoplastyДокумент8 страницImproving Aesthetics in Lateral Tension AbdominoplastyAhmad Arbi AninditoОценок пока нет
- Mini AbdominoplastyДокумент4 страницыMini AbdominoplastyAhmad Arbi AninditoОценок пока нет
- PDFДокумент6 страницPDFAhmad Arbi AninditoОценок пока нет
- Antidiabetic Potential of Medicinal Plants PDFДокумент6 страницAntidiabetic Potential of Medicinal Plants PDFBog G DanОценок пока нет
- Journal Pone 0057218 PDFДокумент13 страницJournal Pone 0057218 PDFAhmad Arbi AninditoОценок пока нет
- Music TherapyДокумент7 страницMusic Therapyzakir2012Оценок пока нет
- Corrected Ortho QsДокумент48 страницCorrected Ortho QsMuhamad Danial Kholili Al-JaloriОценок пока нет
- BibliopocДокумент4 страницыBibliopocKarlo ReyesОценок пока нет
- Acute Glomerulonephritis (AGN) : Paediatric Department CMEДокумент25 страницAcute Glomerulonephritis (AGN) : Paediatric Department CMENurul Syazwani Ramli67% (3)
- 18Th June 2019 Plab 1 Mock Test Plab ResourcesДокумент30 страниц18Th June 2019 Plab 1 Mock Test Plab Resourceskhashayar HajjafariОценок пока нет
- Interpretation of MriДокумент12 страницInterpretation of Mrijimitkapadia100% (1)
- H&P - Sample - Partial ExamДокумент6 страницH&P - Sample - Partial Exam808kailuaОценок пока нет
- The Morrison Technique: A Free-Hand Method For Capturing Photomicrographs Using A SmartphoneДокумент3 страницыThe Morrison Technique: A Free-Hand Method For Capturing Photomicrographs Using A SmartphoneGamal DawoodОценок пока нет
- The African Roots of La Santa Muerte PDFДокумент33 страницыThe African Roots of La Santa Muerte PDFAli Sarwari-Qadri67% (3)
- Strengths Based NursingДокумент22 страницыStrengths Based NursingTHOHAROH0% (1)
- LT 2 Members: Raazia Jalil, Ali Amjad & Ali Raza: Project 2 Doctors InterviewДокумент3 страницыLT 2 Members: Raazia Jalil, Ali Amjad & Ali Raza: Project 2 Doctors InterviewfatimaОценок пока нет
- Prenatal RhogamДокумент3 страницыPrenatal Rhogamgshastri7Оценок пока нет
- 1998-08 HP JournalДокумент90 страниц1998-08 HP JournalElizabeth WilliamsОценок пока нет
- Branches of ZoologyДокумент3 страницыBranches of ZoologyVivek Morya100% (1)
- Mental Status ExamДокумент10 страницMental Status ExamSrini VoruОценок пока нет
- Hunter2019 PDFДокумент15 страницHunter2019 PDFCarlos Andrés BernalОценок пока нет
- Effects of AntidepressantsДокумент204 страницыEffects of AntidepressantsAMCArroyoОценок пока нет
- Emergency Psychiatry Other Than Suicide: Dr. Pooja Singh, MD Assistant ProfessorДокумент45 страницEmergency Psychiatry Other Than Suicide: Dr. Pooja Singh, MD Assistant Professorpooja singhОценок пока нет
- Paneer Do DaДокумент7 страницPaneer Do Darockingtwo07Оценок пока нет
- History of SensorДокумент37 страницHistory of SensornsdewОценок пока нет
- Leukemia EssayДокумент4 страницыLeukemia EssaydanarajОценок пока нет
- Ineffective Health MaintenanceДокумент6 страницIneffective Health MaintenanceRYAN SAPLADОценок пока нет
- TST Straight Volumed Modular Stem ENGДокумент16 страницTST Straight Volumed Modular Stem ENGNorel Nicolae BalutaОценок пока нет
- Hazardous Chemical Products in Home.Документ17 страницHazardous Chemical Products in Home.taratarabuzuОценок пока нет
- Ceohns Disease ECCO Guideline SumarizedДокумент19 страницCeohns Disease ECCO Guideline Sumarizednishad nilangaОценок пока нет
- L10 ToleranceДокумент19 страницL10 Tolerancesara garciaОценок пока нет
- Tennis Elbow' or Lateral Epicondylitis: Information For YouДокумент4 страницыTennis Elbow' or Lateral Epicondylitis: Information For YouvivinОценок пока нет
- Cervical Cancer - PreventionДокумент10 страницCervical Cancer - PreventionRae Monteroso LabradorОценок пока нет
- Ethical Dilemmas in The Practice of NursingДокумент15 страницEthical Dilemmas in The Practice of Nursingestudiant9Оценок пока нет
- MRCPass Notes For MRCP 1 - HEMATOLOGYДокумент9 страницMRCPass Notes For MRCP 1 - HEMATOLOGYsabdali100% (1)
- Strong Is the New Beautiful: Embrace Your Natural Beauty, Eat Clean, and Harness Your PowerОт EverandStrong Is the New Beautiful: Embrace Your Natural Beauty, Eat Clean, and Harness Your PowerРейтинг: 4 из 5 звезд4/5 (5)
- Chair Yoga: Sit, Stretch, and Strengthen Your Way to a Happier, Healthier YouОт EverandChair Yoga: Sit, Stretch, and Strengthen Your Way to a Happier, Healthier YouРейтинг: 3.5 из 5 звезд3.5/5 (5)
- Functional Training and Beyond: Building the Ultimate Superfunctional Body and MindОт EverandFunctional Training and Beyond: Building the Ultimate Superfunctional Body and MindРейтинг: 4.5 из 5 звезд4.5/5 (1)
- Power of 10: The Once-A-Week Slow Motion Fitness RevolutionОт EverandPower of 10: The Once-A-Week Slow Motion Fitness RevolutionРейтинг: 3.5 из 5 звезд3.5/5 (11)
- Peak: The New Science of Athletic Performance That is Revolutionizing SportsОт EverandPeak: The New Science of Athletic Performance That is Revolutionizing SportsРейтинг: 5 из 5 звезд5/5 (96)
- Aging Backwards: Reverse the Aging Process and Look 10 Years Younger in 30 Minutes a DayОт EverandAging Backwards: Reverse the Aging Process and Look 10 Years Younger in 30 Minutes a DayОценок пока нет
- Whole Body Barefoot: Transitioning Well to Minimal FootwearОт EverandWhole Body Barefoot: Transitioning Well to Minimal FootwearРейтинг: 4 из 5 звезд4/5 (16)
- Muscle for Life: Get Lean, Strong, and Healthy at Any Age!От EverandMuscle for Life: Get Lean, Strong, and Healthy at Any Age!Рейтинг: 4.5 из 5 звезд4.5/5 (22)
- Boundless: Upgrade Your Brain, Optimize Your Body & Defy AgingОт EverandBoundless: Upgrade Your Brain, Optimize Your Body & Defy AgingРейтинг: 4.5 из 5 звезд4.5/5 (66)
- Yamas & Niyamas: Exploring Yoga's Ethical PracticeОт EverandYamas & Niyamas: Exploring Yoga's Ethical PracticeРейтинг: 4.5 из 5 звезд4.5/5 (111)
- Mind Your Body: 4 Weeks to a Leaner, Healthier LifeОт EverandMind Your Body: 4 Weeks to a Leaner, Healthier LifeРейтинг: 4.5 из 5 звезд4.5/5 (5)
- The Yogi Code: Seven Universal Laws of Infinite SuccessОт EverandThe Yogi Code: Seven Universal Laws of Infinite SuccessРейтинг: 4.5 из 5 звезд4.5/5 (104)
- Buteyko Breathing Course Manual: For use with the Advanced Buteyko CourseОт EverandButeyko Breathing Course Manual: For use with the Advanced Buteyko CourseРейтинг: 5 из 5 звезд5/5 (1)
- Easy Strength: How to Get a Lot Stronger Than Your Competition-And Dominate in Your SportОт EverandEasy Strength: How to Get a Lot Stronger Than Your Competition-And Dominate in Your SportРейтинг: 4.5 из 5 звезд4.5/5 (17)
- 80/20 Running: Run Stronger and Race Faster by Training SlowerОт Everand80/20 Running: Run Stronger and Race Faster by Training SlowerРейтинг: 4.5 из 5 звезд4.5/5 (97)
- Music For Healing: With Nature Sounds For Natural Healing Powers: Sounds Of Nature, Deep Sleep Music, Meditation, Relaxation, Healing MusicОт EverandMusic For Healing: With Nature Sounds For Natural Healing Powers: Sounds Of Nature, Deep Sleep Music, Meditation, Relaxation, Healing MusicРейтинг: 5 из 5 звезд5/5 (1)
- Wall Pilates: Quick-and-Simple to Lose Weight and Stay Healthy. A 30-Day Journey with + 100 ExercisesОт EverandWall Pilates: Quick-and-Simple to Lose Weight and Stay Healthy. A 30-Day Journey with + 100 ExercisesОценок пока нет
- The Yoga Sutras of Patanjali: The Final Guide for the Study and Practice of Patanjali's Yoga SutrasОт EverandThe Yoga Sutras of Patanjali: The Final Guide for the Study and Practice of Patanjali's Yoga SutrasОценок пока нет
- Weight Lifting Is a Waste of Time: So Is Cardio, and There’s a Better Way to Have the Body You WantОт EverandWeight Lifting Is a Waste of Time: So Is Cardio, and There’s a Better Way to Have the Body You WantРейтинг: 4.5 из 5 звезд4.5/5 (38)
- If You Like Exercise … Chances Are You’Re Doing It Wrong: Proper Strength Training for Maximum ResultsОт EverandIf You Like Exercise … Chances Are You’Re Doing It Wrong: Proper Strength Training for Maximum ResultsРейтинг: 4.5 из 5 звезд4.5/5 (7)
- Endure: Mind, Body, and the Curiously Elastic Limits of Human PerformanceОт EverandEndure: Mind, Body, and the Curiously Elastic Limits of Human PerformanceРейтинг: 4.5 из 5 звезд4.5/5 (237)
- Structural Integration and Energy Medicine: A Handbook of Advanced BodyworkОт EverandStructural Integration and Energy Medicine: A Handbook of Advanced BodyworkРейтинг: 4 из 5 звезд4/5 (1)
- Not a Diet Book: Take Control. Gain Confidence. Change Your Life.От EverandNot a Diet Book: Take Control. Gain Confidence. Change Your Life.Рейтинг: 4.5 из 5 звезд4.5/5 (124)
- Fascial Training: With Easy Exercises To More Mobility And Less Pain (10 Minutes Fascia Workout For Home)От EverandFascial Training: With Easy Exercises To More Mobility And Less Pain (10 Minutes Fascia Workout For Home)Рейтинг: 5 из 5 звезд5/5 (3)
- The Yamas & Niyamas: Exploring Yoga's Ethical PracticeОт EverandThe Yamas & Niyamas: Exploring Yoga's Ethical PracticeРейтинг: 4.5 из 5 звезд4.5/5 (19)