Академический Документы
Профессиональный Документы
Культура Документы
Long-Term Use Study
Загружено:
groberts1998Оригинальное название
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Long-Term Use Study
Загружено:
groberts1998Авторское право:
Доступные форматы
Pediatr Drugs 2003; 5 (12): 787-794
1174-5878/03/0012-0787/$30.00/0
LEADING ARTICLE
Adis Data Information BV 2003. All rights reserved.
Long-Term Use of Stimulants in Children with
Attention Deficit Hyperactivity Disorder
Safety, Efficacy, and Long-Term Outcome
Lily Hechtman and Brian Greenfield
Division of Child Psychiatry, McGill University, Montreal Childrens Hospital, Montreal, Quebec, Canada
Abstract
The purpose of this review is to summarize existing data on the long-term safety and efficacy of stimulant
treatment, and how long-term stimulant treatment of children with attention deficit hyperactivity disorder
(ADHD) affects their outcome. Existing controlled studies of children with ADHD treated and untreated with
stimulants, as well as long-term prospective follow-up studies, are reviewed. Children with ADHD treated with
stimulants for as long as 2 years continue to benefit from the treatment, with improvements observed in ADHD
symptoms, comorbid oppositional defiant disorder, and academic and social functioning, with no significant
problems of tolerance or adverse effects. Long-term, prospective follow-up studies into adulthood show that
stimulant treatment in childhood has slight benefits regarding social skills and self-esteem. Long-term adverse
effects from stimulant treatment in childhood regarding adult height or future substance abuse have not been
supported by existing studies.
Very few studies have been conducted that have examined the
effects of long-term use of stimulants (e.g. methylphenidate) on
outcome in children with attention deficit hyperactivity disorder
(ADHD). A recent meta-analysis of controlled trials, comparing
placebo and methylphenidate in children with ADHD under 18
years of age, was conducted by Schachter et al.[1] This study
identified 62 randomized trials, involving 2897 subjects, where
interventions lasted an average of 3 weeks, with no trials lasting
longer than 28 weeks. This meta-analysis limited itself to
double-blind, placebo-controlled trials, therefore did not include
some of the longer randomized trials that did not include placebo
controls.
This absence of studies of long-term stimulant treatment in
children with ADHD is particularly surprising, given the fact that
stimulants have been used to treat these children since the 1960s.
The National Institute of Mental Health consensus conference on
ADHD in 1998[2] clearly emphasized the need for long-term
studies of stimulant treatment of children with ADHD, citing
concerns that little is known about the long-term effects of
psychostimulants on the developing brain, cardiovascular functioning, and eventual growth. Questions regarding continuing
efficacy, tolerance, long-term adverse effects, and subsequent
substance abuse were also raised.
These concerns have recently become more pronounced with
reports of significant increases in the use of stimulants generally,[3,4] particularly for preschoolers.[5-7] Furthermore, stimulants
have been shown to be effective in adolescence[8] and adulthood;[9]
thus, the use of stimulants can now potentially become life-long,
starting in the preschool age group and continuing through the
elementary age group, adolescence, and adulthood. Little is known
about the impact of such extended long-term use. To date, there
have been few prospective controlled treatment studies in which
children with ADHD received more than 12 months of stimulant
treatment.
The goal of this review article is to summarize the existing data
on the long-term safety and efficacy of stimulant treatment, and to
discuss how long-term stimulant treatment of children with
ADHD affects outcome. Existing controlled, multimodal,[10-13] and
non-multimodal[14,15] studies of children with ADHD treated and
untreated with stimulants, as well as long-term prospective follow-up studies[16-30] are reviewed. Outcome in various domains, such
as ADHD symptoms, comorbidity, academic and social functioning, as well as self-esteem, are explored. Tolerance and adverse
788
Hechtman & Greenfield
effects, particularly with regard to height[31,32] and future substance
abuse,[29,30,33-37] are also discussed.
1. Treatment Studies
1.1 Multimodal Studies
The longest controlled stimulant treatment studies have occurred in the context of two different multimodal treatment studies, one lasting 2 years, and the other 14 months.
The first treatment study carried out by Hechtman and
Abikoff,[10,13] was a two-center study involving 103 children with
carefully diagnosed ADHD, aged 79 years, who were shown to
be responsive to methylphenidate. All children received welltitrated, carefully monitored methylphenidate for 24 months. Children were randomly assigned to either methylphenidate alone,
methylphenidate and multimodal treatment, which included parent
training and counseling, academic organizational skills and remediation, social skills training, and individual psychotherapy, or
methylphenidate and attentional control treatments, which controlled for the professional attention of the multimodal treatments.
Both the multimodal and attentional control treatments occurred
weekly in the first year, in the context of an after-school program
two afternoons per week. There were monthly boosters for each
intervention in the second year, with visits twice monthly. Weight,
height, blood pressure, pulse, and adverse effects were monitored
on a monthly basis and outcome was evaluated in academic,
social, emotional, self-esteem, and parenting domains, as well as
ADHD symptomatology. Parent, teacher, clinician ratings, and
direct observations in a structured academic classroom and during
gym were also used. Evaluations took place at 6, 12, 18, and 24
months. Results showed that all three groups improved significantly in most domains. An improvement was seen at 6 months,
and was maintained at 12, 18, and 24 months; thus, there was no
loss of efficacy during the less intensive booster phase of treatment. Surprisingly, there were no significant differences between
the three groups. The study suggests that for children with ADHD
who are not very comorbid (e.g. for severe learning disability and
conduct disorder [CD]), and who have well-functioning, motivated families, stimulant treatment may be sufficient and remains
effective without significant tolerance or adverse effects for 2
years.
The second study was a six-site study involving 576 children
with ADHD, aged 79.9 years. This 14-month, multisite, multimodal treatment study of children with ADHD (MTA),[11,12]
randomly assigned children to four treatment groups:
a medication strategy group that received careful titration and
monitoring of medication;
Adis Data Information BV 2003. All rights reserved.
a behavioral treatment group that received parent training and
counseling, consultation to the teacher to set up a daily report
card, an intensive 8-week summer treatment program, and a
classroom aide for half days, 5 days per week for 12 weeks;
a combined group that received both the medication and behavioral treatments;
a community treatment group that received treatment in the
community, the nature of which was documented in the study.
In fact, 66% of the community-treated groups received stimulant medication.
Results indicated that for ADHD symptoms, the medication
alone, and combined medication and behavioral treatment groups
showed significantly more improvement than the behavioral or
community-treated groups; however, the medication and combined groups were not significantly different from each other. The
behavioral and community-treated groups were also not significantly different from each other. For other domains, e.g. internalizing disorder, social, academic functioning, and self-esteem, the
combined group showed significantly more improvement than the
behavioral and community-treated groups, whereas the medication
group did not. The advantage of the combined treatment group
was also seen in composite outcome measures,[38,39] where combined treatment was generally best, followed by medication treatment then behavioral treatment and, finally, community treatment.
The relatively poor performance of the community treatment
group was surprising in light of the fact that 66% of this group
received stimulant medication; however, community stimulant
treatment was usually not well titrated, with no input from the
school. Dosages were significantly lower and less frequent than in
the MTA (20 mg/day versus 35 mg/day, twice daily versus three
times daily, 5 days per week versus 7 days per week). There was
also very infrequent monitoring, e.g. one visit every 36 months
versus monthly monitoring in the MTA. The study showed that
well-titrated, carefully monitored stimulant treatment is very effective for ADHD symptoms and the effect lasted with no tolerance or serious adverse effects for the 14 months of the study.
Adverse effects generally included decreased appetite, slight sleep
delay, and occasional rebound. The study also suggests that stimulant treatment in the community leaves much to be desired, with,
generally, little careful titration or monitoring.
1.2 Non-Multimodal Studies
Shorter, less comprehensive, and less well controlled treatment
studies have been conducted by Gillberg et al.[14] and Schachar et
al.[15] Gillberg et al.[14] conducted a 15-month prospective, randomized, double-blind, placebo-controlled discontinuation trial of
racemic amphetamines. Sixty-two children with ADHD were
Pediatr Drugs 2003; 5 (12)
Long-Term Use of Stimulants in Children with ADHD
openly titrated with racemic amphetamine over 3 months. Then, in
a randomized, double-blind protocol, 30 were assigned to placebo
and 32 continued on amphetamine for 12 months. Study endpoint
occurred when subjects had to be removed from the protocol and
given open treatment. Seventy-one percent of those assigned to
placebo, versus 29% of those assigned amphetamines (p < 0.05),
had to be removed from the protocol. Despite this significant
difference, favoring the efficacy of amphetamines, the study had a
number of limitations. There were no prior criteria for discontinuation. The study included children who were comorbid for pervasive developmental disorder. It is also unclear why 29% of those
subjects initially responsive to amphetamines and then randomized to placebo did not deteriorate during the ensuing 12 months.
Similarly, it is unclear why 29% of patients responsive to amphetamines who were randomized to stay on amphetamines needed to
be discontinued from this treatment; however, the study did show
that most of the patients with ADHD continued to benefit from
stimulants for 15 months.
Schachar et al.[15] conducted a 4-month randomized, doubleblind stimulant versus placebo study in 91 children with ADHD.
The study showed that stimulants given twice daily were effective
in school, but not at home after school; thus authors recommended
three times daily administration of short-acting stimulants and
other interventions to help the situation at home. Longer-acting
stimulants, e.g. Adderall XR1,[40] Concerta,[41] have been very
useful in providing 1012 hour coverage, thus decreasing behavioral problems after school and in the early evening. The study by
Schachar et al.[15] also indicated that efficacy of stimulants was
maintained for the 4-month period. Medication was effective for
ADHD symptoms as well as oppositional and defiant symptoms.
The studies described above lend support to the review conducted by Greenhill and coworkers[42] on the short- and long-term
safety and efficacy of stimulant treatment of children with ADHD.
Greenhill and colleagues[42] conclude that stimulant treatment
studies show robust, short-term efficacy and a good tolerability
profile. Longer-term studies[10-15] are few in number, but have
produced no conclusive evidence that careful therapeutic use of
these medications is harmful. The authors conclude that current
evidence indicates that stimulants show efficacy and safety in
studies up to 24 months.
2. Prospective Follow-Up Studies
There are a number of long-term prospective controlled followup studies. Generally, in these studies children are diagnosed and
treated with stimulants in childhood and followed prospectively
then re-evaluated periodically during adolescence and adulthood.
1
789
These studies have a number of significant limitations in evaluating long-term stimulant effects on outcome.
Children with ADHD who receive stimulants may in fact
constitute a more impaired population with more severe ADHD
symptoms and higher rates of serious comorbidity; thus, the longterm outcome of children with ADHD treated with stimulants who
have not been randomly assigned to stimulant treatment may be
negatively biased because, initially, the most impaired children
may have been medicated.
The length of the initial medication treatment can vary from
several weeks, a few months, to 35 years. Rarely are these
subjects on continuous stimulant medication for the entire followup period. Dosages the patients receive are also very variable, and
whether or not they are on optimal dose is often not determined or
is unclear. Compliance is rarely measured; thus, prospective follow-up studies basically look at adolescent and adult outcome in
children with ADHD who received some stimulant medication in
childhood. These children may have initially been a more disturbed group.
In an early study, Weiss and colleagues[16] compared three
groups of hyperactive children. The first group (n = 24) received
methylphenidate 2050 mg/day for 35 years; the second group (n
= 22) received chlorpromazine for 18 months to 5 years (mean
dose 75 mg/day); while the third group (n = 20) received no
medication treatment. The three groups were matched for age, IQ,
gender, and socioeconomic status. At adolescence, no significant
differences in emotional adjustment, delinquency, or academic
performance were seen in the three groups. It was surprising to see
that children who received stimulants for 35 years in childhood
did not have better long-term outcome than those who did not
receive this treatment. However, it should be pointed out that in
those subjects who were on stimulant medication, having a wellfunctioning family was significantly correlated with good outcome, as defined by academic achievement, absence of delinquency, and emotional adjustment; thus the interaction of medication
and other factors (e.g. family functioning) appears more important
in predicting outcome than medication itself. Similar findings
were reported by Conrad and Insel[43] and Loney et al.[17]
In her study of adolescent outcome, Loney and colleagues[17]
explored stimulant treatment as a predictor in 124 hyperactive
boys. Average duration of treatment in childhood was 29 months
and the average dose was 34 mg/day. In summary, response to
medication was a factor in only three of the many outcome
measures in adolescence. Subjects who responded well to medication in childhood had a less negative affect at follow-up, were
less involved in nonmedical drug use, and scored better on the
The use of tradenames is for product identification purposes only and does not imply endorsement.
Adis Data Information BV 2003. All rights reserved.
Pediatr Drugs 2003; 5 (12)
790
Wide Range Achievement Test[44] in reading and arithmetic.
Paternite and coworkers[18] followed this sample into young adulthood, 2123 years of age. Treatment with methylphenidate in
childhood had no effect on adult outcome in 63% of the sample;
however, such treatment had positive effects in adulthood for 34%
of subjects. Specifically, higher dosages of stimulant medication
were associated with fewer diagnoses of alcoholism or suicide
attempts, and better social functioning. Longer medication duration was associated with fewer schizotypic features, higher
Wechsler Adult Intelligence Scale[45] performance and full-scale
IQs, and better ratings in the Wide Range Achievement Test and
reading and arithmetic performance.
Most authors who have examined stimulant treatment in childhood as a predictor of hyperactive adolescent outcome have found
no effect as if the initial benefits of medication cited by many
studies do not somehow carry over into positive long-term outcome. Thus, Ackerman and colleagues[46] found that stimulant
drug treatment had no dramatic long-term results on academic
achievement in their three groups (hyperactive [n = 23], hypoactive [n = 14], and normoactive [n = 25]) of learning-disabled boys
at age 14 years. One could argue that the dual handicap of
hyperactivity and learning disability mitigated against the longterm positive effectiveness of the medication; however, Riddle and
Rapoport[47] also found no difference in academic achievement
between a subgroup of 20 hyperactive boys who had been randomly assigned to receive methylphenidate for 2 years in their total
group of 72 hyperactive boys, some of whom were taking imipramine.
Blouin and colleagues[19] compared two groups of hyperactive
adolescents. One group had received methylphenidate treatment in
childhood (1060 mg/day, mean 20 mg/day) for 1 month to 7 years
(mean 2 years [n = 23]), and the other did not (n = 22). The two
groups were matched for age, IQ, and academic achievement at
initial assessment. The authors stated that even when good and
poor responses were examined separately, no beneficial effect of
the drug on academic achievement, intellectual ability, or behavioral ratings was evident.
Charles and Stein[20] divided 62 hyperactive children into four
groups, depending on the length of time they had been on stimulant treatment (ranging from <6 months for group 1, to 4 years for
group 5). At 4-year follow-up, there were no group differences in
behavioral, social, or academic outcome measures, suggesting that
duration of stimulant intervention did not have a significant effect
on outcome.
The seeming ineffectiveness of childhood stimulant medication
in influencing adolescent outcome was further shown by Satterfield and coworkers.[21] In a prospective study, the authors
compared 110 adolescent hyperactive boys and 88 matched
Adis Data Information BV 2003. All rights reserved.
Hechtman & Greenfield
healthy controls on serious offenses, as obtained from official
arrest records. The hyperactive group had received stimulant treatment for approximately 2 years, as well as brief counseling;
however, this group had significantly more serious arrests and
institutionalization for delinquency than the matched healthy control group. The considerably more favorable outcome of Satterfield and colleagues[22] 3-year follow-up of hyperactive adolescents who received multimodal (medication plus any number of
other required interventions, e.g. psychotherapy, therapy for the
child and/or parents, family therapy, and educational therapy)
presents some suggestion as to why stimulant treatment has not
predicted more positive long-term outcome. It is clear that these
children have many academic, social, family, and personal problems. All of these difficulties require intervention, and relying on
medication alone to ameliorate all these areas now seems unrealistic. Satterfield et al.[22] showed that children who received longer
multimodal treatment had better outcome than children who discontinued treatment earlier; however, poorer family functioning
may have been a factor in the group that withdrew from treatment.
As mentioned before, Paternite and coworkers[18] also found that
longer medication treatment was associated with fewer
schizotypic features, better Minnesota Multiple Psychological
Inventory[48] scores, higher IQ scores, and better wide-range
achievement scores in reading and arithmetic. The findings of
Satterfield et al.[22] and Paternite et al.[18] are different from those
of Fischer et al.[49] and Lambert et al.,[50] who found that children
with ADHD who had longer treatment, had more negative outcome. In fact, these authors felt that the increased length of
treatment required may be a marker for greater severity of the
condition.
Many of the more recent prospective, longitudinal studies[23-26,51] have involved children with ADHD who received stimulant treatment in childhood; thus, they present an outcome picture
of a childhood medicated population.
In the studies by Gittelman et al.[23] and Mannuzza et al.,[24] 103
children with ADHD received an average of methylphenidate 45
mg/day for 6 months to 5 years during childhood. Together with a
matched control group (n = 100), they were reassessed at a mean
age of 18 and 26 years. Results showed that the ADHD group had
significantly poorer outcome with respect to continuing ADHD
symptoms, antisocial personality disorder, substance use disorder
(SUD), education completed, and work status when compared
with the matched control group.
Barkley et al.[25,30] and Fischer et al.[26] also conducted a controlled prospective follow-up of 147 children with ADHD who
received stimulant treatment in childhood. The dose and duration
of medication use is not clear. Patients with ADHD and matched
controls were followed up in adolescence (mean age 15 years) and
Pediatr Drugs 2003; 5 (12)
Long-Term Use of Stimulants in Children with ADHD
in young adulthood (mean age 21 years). The authors again found
that the ADHD group continued to have more ADHD symptoms
and other psychiatric disorders, poorer school and work histories,
higher rates of antisocial behaviors, and substance use.
These two studies[23-26] both showed that the ADHD group had
significantly worse adolescent and adult outcome than the
matched control group despite stimulant medication treatment in
childhood; however, the difference in outcome between the
ADHD group and the control group may have been even greater
had the ADHD group not received stimulant treatment in childhood. Thus, comparing the long-term outcome of patients with
ADHD who did and did not receive stimulant treatment in childhood is valuable.
One of the earliest prospective (5, 10, and 15 year) controlled
follow-up studies was conducted by Weiss et al.[27,28] and involved
104 children with ADHD who were not medicated because stimulants were not generally used in Canada at that time. The long-term
outcome of this untreated group was worse than their matched
control group in academic, work, social, and emotional areas.
Subsequently, Hechtman and colleagues[29] compared the outcome of this untreated group with the 20 young adults (mean age
22 years) with ADHD who received 3 years of sustained stimulant
medication (methylphenidate 2050 mg/day) between 6 and 12
years of age and a matched control group. Results indicated that in
many areas (e.g. school, work, and personality disorders) patients
with ADHD treated with stimulants functioned significantly worse
than matched controls, but similar to the untreated patients with
ADHD. In some areas (e.g. fewer car accidents, more positive
view of their childhood, lesser delinquency, better social skills and
self-esteem), patients with ADHD treated with stimulants did
better than their untreated counterparts. Drug and alcohol abuse
was generally not significantly different in the three groups; thus,
stimulant treatment in childhood may not eliminate future educational, work, or life difficulties, but may result in less social
ostracism and improved feelings toward themselves and others.
3. Adverse Effects of Long-Term Stimulant Use
In evaluating the outcome of long-term stimulant treatment,
one must evaluate possible benefits with regard to symptoms and
functioning, but also explore any adverse effects of such treatment.
3.1 Effects on Growth
Safer and colleagues[52] showed that stimulants potentially suppressed height and weight gains of children treated with these
medications. Safer and Allen[53] found that this was a dose-related
phenomenon, not seen in methylphenidate dosages under 20 mg/
Adis Data Information BV 2003. All rights reserved.
791
day, and more pronounced with dextroamphetamine, which occurred predominantly in the first year of treatment. Furthermore,
the initial suppression is followed by a rebound in growth or
habituation to this effect,[54,55] and there is no effect on overall
adult height or weight.[31,32] Effects on growth are thought to be
secondary to appetite suppression, but no systematic study has
clearly demonstrated this. One study found a direct effect on blood
levels of growth hormone.[56]
Even though growth suppression is believed to be minor and
relatively transient, with no lasting impact on adult growth, there
have been no studies of children who have been continuously
treated with stimulants from childhood through adolescence to
adulthood. Such studies are clearly needed. Complicating the
picture still further, Spencer et al.[57] suggested that children with
ADHD are somewhat smaller than their healthy peers prior to
puberty and catch up with their peers in adolescence. This growth
delay is thought to be associated with the disorder and not stimulant treatment.
Generally, it is recommended that clinicians monitor the height
and weight of children being treated with stimulant medication
and introduce drug holidays during the summer or school vacations, so as to increase the probability of growth rebound.
3.2 Substance Abuse
There has been a long-standing concern that stimulant treatment during childhood may increase the risk of future substance
abuse. This concern pertains to abuse of both stimulants and other
drugs. Dexedrine, methylphenidate, and Adderall are accepted as
potential drugs of abuse and have been classified as schedule II
drugs by the US Drug Enforcement Administration. This classification is based on a large body of data from periods where these
drugs were used and abused recreationally, animal studies, and
adult addict case reports. Concern regarding abuse potential is
increasing as there has been a 5-fold increase in the production and
use of methylphenidate between 1986 and 1996.[58] In addition,
many adolescents with ADHD are being treated with stimulants;
therefore, there may be a greater risk of stimulants being abused,
diverted, or serving as a gateway drug to other illicit drugs.
However, several factors suggest that the concern may be unwarranted. Stimulants differ in their ability to produce euphoria. A
Positive Emission Tomography study has shown that oral methylphenidate demonstrates markedly slower absorption, occupancy of
dopamine transporter, and clearance, than does intravenous cocaine.[59] Similarly, oral methylphenidate does not induce euphoria.[59] In addition, there is little evidence that ADHD per se or that
stimulant treatment of children with ADHD increases the risk of
later substance abuse.[17,33,60-62] Most often it is the combination of
Pediatr Drugs 2003; 5 (12)
792
Hechtman & Greenfield
continued severe ADHD symptoms and comorbid CD which
increases the risk of substance abuse in this population.[25,26,49,60,63,64]
There have been several recent reviews which have addressed
the question of whether stimulant treatment in children with
ADHD increases the risk of future substance use and abuse.[35,65,66]
Studies fall roughly into three groups:
studies that show stimulant treatment in childhood is protective,
i.e. decreases the risk of future substance use and abuse;[33-35]
studies which show that stimulant treatment in childhood does
not increase or decrease the risk of future substance use and
abuse;[28-30]
studies which show that stimulant treatment in childhood increases the risk of future substance use and abuse.[37]
3.2.1 Decreased Risk
Biederman and colleagues[33] carried out a 4-year prospective
study of 56 medicated children with ADHD (type of medication
was not specified), 19 non-medicated children with ADHD, and
137 non-ADHD comparison children. At follow-up (mean age
1719 years), prevalence of SUD was significantly greater among
non-medicated (75%) versus medicated (25%), and comparison
(18%) children. These results seem to suggest a significant protective effect of medication in the development of SUD; however, the
three groups had significant baseline differences for age, social
class, and rate of CD (27% in the medicated group, 47% in the
non-medicated group, 4% in the non-ADHD group). Furthermore,
the rates of SUD pretreatment also differed significantly (0% in
the medicated group, 37% in the non-medicated group, and 13% in
the non-ADHD group). The authors tried to control these important differences statistically in their data analysis.
Another study, which suggested a protective value of medication treatment, was carried out by Loney and coworkers.[34]
They followed 219 children with ADHD into adulthood. Of these,
182 received stimulant treatment in childhood, while 37 did not
due to different physician preferences. At follow-up, all subjects
who had been treated had discontinued stimulant treatment for at
least 4 years. The authors found no relationship between stimulant
treatment in childhood and extent of drug use in adulthood for
most drugs. An actual protective effect of stimulant treatment was
seen, i.e. the medicated group had less involvement with tobacco,
stimulants, inhalants (glue), or opiates by follow-up. Boys who
had been medicated were also less likely to be diagnosed with
alcoholism in adulthood. This was a more randomized study in
that there was random assignment to faculty physicians with very
different treatment preferences; however, the choice of whom to
medicate may still have been based on clinical considerations.
Adis Data Information BV 2003. All rights reserved.
Huss and Lehmkuhl[35] conducted a retrospective study in 215
patients with ADHD. They also found that methylphenidate treatment in childhood significantly reduced the risk of SUD in adulthood. This group is currently conducting a prospective study with
225 children to be followed at 5-year intervals for 15 years.
Preliminary analysis also suggests that early treatment with
methylphenidate reduces the risk of SUD.
3.2.2 No Impact on Risk
A study by Burke et al.[36] evaluated 177 clinically-referred
children with ADHD annually for 9 years until the age of 15 years.
Although the adolescents with ADHD had more tobacco, marijuana, alcohol, and other illicit drug use compared with matched
controls, this association became nonsignificant when CD was
statistically controlled. Similarly, stimulant medication use in
childhood was initially associated with tobacco use by adolescence; however, this association disappeared when childhood and
adolescent CD was controlled for. We thus see the importance of
controlling for CD, which appears to have a much greater impact
on later SUD than ADHD or stimulant treatment.
In a recent study, Barkley et al.[30] prospectively followed 147
clinically-referred children with ADHD for 13 years into adulthood (mean age 21 years, range 1925 years). Children treated
with stimulants had no greater frequency of drug use in adolescence or young adulthood. Furthermore, duration of stimulant
treatment was not significantly associated with frequency of any
form of drug use in young adulthood.
Stimulant treatment in high school appeared to only be associated with increased use of cocaine in adulthood; however, this
increased use was primarily mediated by severity of CD in childhood, adolescence, and young adulthood, and not stimulant treatment. This study also supports the notion that stimulant treatment
in childhood and adolescence does not increase the risk of future
substance use and abuse.
The long-term, prospective follow-up study of young adults by
Hechtman et al.,[29] described earlier, involved the comparison of
untreated hyperactive individuals (n = 68), treated hyperactive
individuals (n = 20), and matched controls (n = 20) at a mean age
of 22 years. Drug and alcohol abuse was generally not significantly different in the three groups. This study also showed that
stimulant treatment in childhood had no impact on adult substance
abuse.
3.2.3 Increased Risk
There is only one study (conducted by Lambert and Hartsough[37]) which suggests that stimulant treatment in childhood
increased the risk of substance abuse in adulthood. It involved a
prospective 10-year follow-up to adulthood of 93 children with
Pediatr Drugs 2003; 5 (12)
Long-Term Use of Stimulants in Children with ADHD
ADHD who received stimulant medication and 81 who did not
receive stimulant medication in childhood.
The authors subdivided the group into those subjects who were
never treated with stimulants, those who were treated for 1 year,
and those who were treated for >1 year. Stimulant treatment for 1
year was associated with more cigarette smoking and cocaine
SUD; however, this study did not control for CD or severity of
ADHD symptoms in the medication treated and untreated hyperactive groups, which may in fact have been responsible for the
increase in substance use reported.
In summary, most studies have shown that stimulant treatment
in childhood of patients with ADHD does not increase the risk of
substance abuse in adulthood. At times, this increased use and
abuse of substances seen in this population is usually related to the
combination of continuing severe ADHD and comorbid CD. Furthermore, there are some emerging studies which suggest that
stimulant treatment in childhood may have a protective function
with regard to future substance abuse.
4. Conclusions
There are very few controlled long-term stimulant treatment
studies. The longest available controlled studies involve approximately 2 years of treatment. These studies[10,11,14] show that stimulants are effective in improving ADHD symptoms, comorbid
oppositional defiant disorder, as well as academic and social
functioning. During this 2-year treatment period, tolerance was not
a problem and adverse effects were minimal.
Long-term prospective follow-up studies[24,26,28-30,34] indicate
that stimulant treatment in childhood still results in patients with
ADHD functioning worse in academic, work, social, and emotional domains when compared with matched healthy controls; however, a comparison of patients with ADHD treated with stimulants
versus untreated patients with ADHD suggests similarities between the two groups with regard to academic and work functioning, although the treated group appeared to have fewer car accidents, better social skills, and self-esteem.
Concerns about long-term adverse effects of stimulant treatment with regard to growth and future substance abuse have not
been supported by most existing studies.[28-30,34] In fact, some
studies[33-35] suggest that stimulant treatment in childhood may be
protective against future substance abuse.
Acknowledgements
The author receives research support from the National Institute of Mental
Health, Purdue Pharma, Jensen Ortho, and Shire Pharmaceuticals.
Adis Data Information BV 2003. All rights reserved.
793
References
1. Schachter HM, Pham B, King J, et al. How efficacious and safe is short-acting
methylphenidate for the treatment of attention deficit disorder in children and
adolescents: a meta-analysis. CMAJ 2001; 165 (11): 1475-88
2. NIH Consensus Development Program-110. Diagnosis and treatment of attention
deficit hyperactivity disorder. Consensus development conference statement.
Bethesda (MD): National Institutes of Health, 1998
3. Safer DJ, Zito JM, Fine EM. Increased methylphenidate usage for attention deficit
disorder in the 1990s. Pediatrics 1996; 98: 1084-8
4. Safer DJ, Malever M. Stimulant treatment in Maryland public schools. Pediatrics
2000; 106: 533-9
5. Zito JM, Safer DJ, dos Reis S, et al. Trends in the prescribing of psychotropic
medication to preschoolers. JAMA 2000; 283: 1025-30
6. Rappley MD, Mullan PB, Alvarez AJ, et al. Diagnosis of attention deficit disorder
and the use of psychotropic medication in very young children. Arch Pediatr
Adolesc Med 1999; 153: 1039-45
7. Connor DF. Preschool attention deficit hyperactivity disorder: a review of prevalence, diagnosis, neurobiology, and stimulant treatment. J Dev Behav Pediatr
2002; 23 (1 Suppl.): S1-9
8. Weiss M, Jain U, Garland J. Clinical suggestions for management of stimulant
treatment in adolescents. Can J Psychiatry 2000; 45: 717-23
9. Spencer T, Biederman J, Wilens T, et al. Pharmacotherapy of attention deficit
disorder across the life cycle. J Am Acad Child Adolesc Psychiatry 1996; 35:
409-32
10. Hechtman L, Abikoff H. Methylphenidate and multimodal treatment in attention
deficit hyperactive disorder. In: Jensen PS, Hibbs ED, editors. Psychosocial
treatment research with children and adolescents. Washington, DC: APA Press,
1996: 341-69
11. MTA Cooperative Group, Jensen P, Arnold LE, et al. A 14-month randomized
clinical trial of treatment strategies for attention deficit hyperactivity disorder
(ADHD). Arch Gen Psychiatry 1999; 56: 1073-86
12. MTA Cooperative Group, Hinshaw S, Swanson J, et al. Moderators and mediators
of treatment response for children with ADHD: the MTA Study. Arch Gen
Psychiatry 1999; 56: 1088-96
13. Hechtman L, Abikoff H. Multimodal treatment plus stimulants vs stimulant treatment in ADHD children: results from a two-year comparative treatment study.
Annual Meeting of the American Academy of Child and Adolescent Psychiatry; 1995 Oct 18-26; New Orleans (LA)
14. Gillberg C, Melander H, von Knorring A, et al. Long-term central stimulant
treatment of children with attention-deficit hyperactivity disorder: a randomized double-blind placebo-controlled trial. Arch Gen Psychiatry 1997; 54:
857-64
15. Schachar RJ, Tannock R, Cunningham C, et al. Behavioral, situational, and
temporal effects of treatment of ADHD with methylphenidate. J Am Acad
Child Adolesc Psychiatry 1997; 36: 754-63
16. Weiss G, Kruger E, Danielson U, et al. Effects of long-term treatment of
hyperactive children with methylphenidate. CMAJ 1975; 112: 159-65
17. Loney J, Kramer J, Milich R. The hyperkinetic child grows up: predictors of
symptoms, delinquency, and achievement at follow-up. In: Gadow KD, Loney
J, editors. Psychosocial aspects of drug treatment for hyperactivity. Boulder
(CO): Westview Press, 1981: 381-415
18. Paternite CE, Loney J, Salisbury H, et al. Childhood inattention-overactivity,
aggression, and stimulant medication history as predictors of young adult
outcomes. J Child Adolesc Psychopharmacol 1999; 9 (3): 169-84
19. Blouin AGA, Bornstein R, Trites R. Teen-age alcohol use among hyperactive
children: a 5-year follow-up study. J Pediatr Psychol 1978; 3: 188-94
20. Charles L, Stein R. A four-year follow-up study of the effects of methylphenidate
on the behavior and academic achievement of hyperactive children. J Abnorm
Child Psychol 1981; 9: 495-505
21. Satterfield J, Hoppe CM, Schell AM. A prospective study of delinquency in 110
adolescent boys with attention deficit disorder and 88 normal adolescent boys.
Am J Psychiatry 1982; 139: 797-8
22. Satterfield JH, Satterfield BT, Cantwell DP. Three-year multimodal treatment
study of 100 hyperactive boys. J Pediatr 1981; 98: 650-5
23. Gittelman R, Mannuzza S, Shenker R, et al. Hyperactive boys almost grown-up.
Arch Gen Psychiatry 1985; 42: 937-47
Pediatr Drugs 2003; 5 (12)
794
Hechtman & Greenfield
24. Mannuzza S, Klein RG, Bessler A, et al. Adult outcome in hyperactive boys. Arch
Gen Psychiatry 1993; 50: 565-76
47. Riddle KD, Rapoport JL. A 2-year follow-up of 72 hyperactive boys. J Nerv Ment
Dis 1976; 162: 126-34
25. Barkley RA, Fischer M, Edelbrock CS, et al. The adolescent outcome of hyperactive children diagnosed by research criteria: an 8-year prospective follow-up
study. J Am Acad Child Adolesc Psychiatry 1990; 29: 546-57
48. Hathaway SR, McKinley JC. Minnesota multiphasic personality inventory-2:
manual for administration and scoring. Minneapolis (MN): University of Minnesota Press, 1989
26. Fischer M, Barkley RA, Smallish L, et al. Young adult follow-up of hyperactive
children: self-report psychiatric disorders comorbidity and the role of childhood
conduct problems and teen CD. J Abnorm Child Psychol 2002; 30 (5): 463-75
49. Fischer M, Barkley RA, Fletcher KE, et al. The adolescent outcome of hyperactive
children: predictors of psychiatric, academic, social, and emotional adjustment.
J Am Acad Child Adolesc Psychiatry 1993; 32 (2): 324-32
27. Weiss G, Minde K, Werry J, et al. A five-year follow-up of 91 hyperactive school
children. Arch Gen Psychiatry 1971; 24: 409-14
50. Lambert N, Hartsaugh C, Sassone D. Persistence of hyperactivity symptoms from
childhood to adolescence. Am J Orthopsychiatry 1987; 57: 22-31
28. Weiss G, Hechtman L. Hyperactive children grown up. New York: Guilford Press,
1993
51. Biederman J, Faraone S, Milberger S, et al. A prospective 4-year follow-up study
of attention-deficit hyperactivity and related disorders. Arch Gen Psychiatry
1996; 53 (5): 437-46
29. Hechtman L, Weiss G, Perlman T, et al. Young adult outcome of hyperactive
children who received long-term stimulant treatment. J Am Acad Child Adolesc
Psychiatry 1984; 23 (3): 261-9
30. Barkley RA, Fischer M, Smallish L, et al. Does stimulant treatment of ADHD
contribute to substance use and abuse: a 13-year prospective study. Pediatrics
2003; 3 (1): 97-109
31. Zeiner P. Body growth and cardiovascular function after extended (1.75 years)
with methylphenidate in boys with attention-deficit hyperactivity disorder. J
Child Adolesc Psychopharmacol 1995; 5: 129-38
32. Klein R, Mannuzza S. Hyperactive boys almost grown up (III): methylphenidate
effects on ultimate height. Arch Gen Psychiatry 1988; 45: 1131-4
33. Biederman J, Wilens T, Mick E, et al. Pharmacotherapy of attention-deficit/
hyperactivity disorder reduces risk for substance use disorder. Pediatrics 1999;
104: E20
34. Loney J, Kramer J, Salisbury H. Medicated versus unmedicated ADHD children:
adult involvement with legal and illegal drugs. In: Jensen P, Cooper JR, editors.
Diagnosis and treatment of attention deficit hyperactivity disorder. Kingston
(NJ): Civic Research Institute, 2002
35. Huss M, Lehmkuhl U. Methylphenidate and substance abuse: a review of pharmacology, animal, and clinical studies. J Atten Disord 2002; 6: S65-71
36. Burke JD, Loeber R, Lahey BB. Which aspects of ADHD are associated with
tobacco use in early adolescence? J Child Psychol Psychiatry 2001; 42: 493-502
37. Lambert NM, Hartsough CS. Prospective study of tobacco smoking and substance
dependencies among samples of ADHD and non-ADHD participants. J Learn
Disabil 1998; 31: 533-44
38. Conners K, Epstein J, March J, et al. Multimodal treatment of ADHD in the MTA:
an alternative outcome analysis. J Am Acad Child Adolesc Psychiatry 2001; 40
(2): 159-67
39. Swanson J, Kraemer H, Hinshaw S, et al. Clinical relevance of the primary
findings of the MTA: success rates based on severity of ADHD and ODD
symptoms at the end of treatment. J Am Acad Child Adolesc Psychiatry 2001;
40 (2): 167-79
40. Biederman J, Lopez F, Boellner S, et al. A randomized, double-blind, placebocontrolled, parallel-group study of SLI381 in children with attention deficit/
hyperactivity disorder. Pediatrics 2002; 110 (2): 1-9
41. Wolraich ML, Greenhill L, Pelham W, et al. Randomized, controlled trial of oros
methylphenidate once a day in children with attention-deficit/hyperactivity
disorder. Pediatrics 2001; 108 (4): 883-92
52. Safer D, Allen R, Barr E. Depression of growth in hyperactive children on
stimulant drugs. N Engl J Med 1972; 287: 217-20
53. Safer DJ, Allen RP. Factors influencing the suppressant effects of two stimulant
drugs on the growth of hyperactive children. Pediatrics 1973; 51: 660-7
54. Safer DJ, Allen RP, Barr E. Growth rebound after termination of stimulant drugs.
Pediatrics 1975; 86: 113-6
55. Mattes JA, Gittelman R. Growth of hyperactive children on maintenance regimen
of methylphenidate. Arch Gen Psychiatry 1983; 40: 317-21
56. Reeve E, Garfinkel B. Neuroendocrine and growth regulations: the role of sympathomimetic medication. In: Greenhill LL, Osmon BB, editors. Ritalin: theory
and patient management. New York: Mary Ann Liebert, 1991: 289-300
57. Spencer TJ, Biederman J, Harding M, et al. Growth deficits in ADHD children
revisited: evidence for disorder-associated growth delays? J Am Acad Child
Adolesc Psychiatry 1996; 35: 1460-9
58. Goldman L, Genel M, Bezman R, et al. Diagnosis and treatment of attentiondeficit/hyperactivity disorder. JAMA 1998; 279: 1100-7
59. Volkow N, Wang G, Fowler J, et al. Dopamine transporter occupancies in the
human brain induced by therapeutic doses of oral methylphenidate. Am J
Psychiatry 1998; 155: 1325-31
60. Biederman J, Wilens T, Mick E, et al. Is ADHD a risk factor for psychoactive
substance use disorders: findings from a four-year prospective follow-up study.
J Am Acad Child Adolesc Psychiatry 1997; 36 (1): 21-9
61. Hechtman L. Adolescent outcome of hyperactive children treated with stimulants
in childhood: a review. Psychopharmacol Bull 1985; 21: 178-91
62. Kramer J, Loney J, Whaley-Klahn M. The role of prescribed medication in
hyperactive youths substance use. In: Scientific Proceedings of the American
Psychological Association. Los Angeles (CA): American Psychological Association, 1981
63. Barkley RA, Fischer M, Edelbrock CS, et al. The adolescent outcome of hyperactive children diagnosed by research criteria (III): mother-child interactions,
family conflicts and maternal psychopathology. J Child Psychol Psychiatry
1991; 32 (2): 233-55
64. Milberger S, Biederman J, Faraone SV, et al. ADHD is associated with early
initiation of cigarette smoking in children and adolescents. J Am Acad Child
Adolesc Psychiatry 1997; 36 (1): 37-44
42. Greenhill LL, Halperin JM, Abikoff H. Stimulant medications. J Am Acad Child
Adolesc Psychiatry 1999; 38 (5): 503-12
65. Wilens TE, Faraone SV, Biederman J, et al. Does stimulant therapy of attentiondeficit/hyperactivity disorder beget later substance abuse: a meta-analytic review of the literature. Pediatrics 2003; 111: 179-85
43. Conrad WG, Insel J. Anticipating the response to amphetamine therapy in the
treatment of hyperkinetic children. Pediatrics 1967; 40: 96-8
66. Barkley RA. Does stimulant treatment medication therapy for ADHD in children
predispose to later drug use? ADHD Report 2003; 11 (1): 2-7
44. Wilkinson GS. The wide range achievement test-revised: administration manual.
Wilmington (DE): Wide Range, Inc., 1993
45. Wechsler D. Wechsler adult intelligence scale-III. San Antonio (TX): The Psychological Corporation, 1997
46. Ackerman PT, Dykman RA, Peters JE. Teenage status of hyperactive and nonhyperactive learning disabled boys. Am J Orthopsychiatry 1977; 47: 577-96
Adis Data Information BV 2003. All rights reserved.
Correspondence and offprints: Professor Lily Hechtman, Division of Child
Psychiatry, McGill University, Montreal Childrens Hospital, 4018 St Catherine Street West, Montreal, PQ H3Z-1P2, Canada.
E-mail: lhechtman@hotmail.com
Pediatr Drugs 2003; 5 (12)
Вам также может понравиться
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeОт EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeРейтинг: 4 из 5 звезд4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingОт EverandThe Little Book of Hygge: Danish Secrets to Happy LivingРейтинг: 3.5 из 5 звезд3.5/5 (399)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryОт EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryРейтинг: 3.5 из 5 звезд3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceОт EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceРейтинг: 4 из 5 звезд4/5 (894)
- The Yellow House: A Memoir (2019 National Book Award Winner)От EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Рейтинг: 4 из 5 звезд4/5 (98)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureОт EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureРейтинг: 4.5 из 5 звезд4.5/5 (474)
- Never Split the Difference: Negotiating As If Your Life Depended On ItОт EverandNever Split the Difference: Negotiating As If Your Life Depended On ItРейтинг: 4.5 из 5 звезд4.5/5 (838)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaОт EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaРейтинг: 4.5 из 5 звезд4.5/5 (265)
- The Emperor of All Maladies: A Biography of CancerОт EverandThe Emperor of All Maladies: A Biography of CancerРейтинг: 4.5 из 5 звезд4.5/5 (271)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersОт EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersРейтинг: 4.5 из 5 звезд4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnОт EverandTeam of Rivals: The Political Genius of Abraham LincolnРейтинг: 4.5 из 5 звезд4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaОт EverandThe Unwinding: An Inner History of the New AmericaРейтинг: 4 из 5 звезд4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyОт EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyРейтинг: 3.5 из 5 звезд3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreОт EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreРейтинг: 4 из 5 звезд4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)От EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Рейтинг: 4.5 из 5 звезд4.5/5 (119)
- Cases in Surgical Critical CareДокумент36 страницCases in Surgical Critical CareHasan ShanawaniОценок пока нет
- Vaccination ScheduleДокумент1 страницаVaccination ScheduleAmanda KamienОценок пока нет
- Chapter 38 - Pediatric and Geriatric HematologyДокумент3 страницыChapter 38 - Pediatric and Geriatric HematologyNathaniel Sim100% (2)
- Rheumatological History Taking OSCE GuideДокумент11 страницRheumatological History Taking OSCE GuideChen BrionesОценок пока нет
- Designed To Enhance From The Inside Out: Apd TherapyДокумент7 страницDesigned To Enhance From The Inside Out: Apd TherapyNumael Alfonso Serrato AlvaradoОценок пока нет
- Cutaneous MelanomaДокумент226 страницCutaneous MelanomaGriskalia ChristineОценок пока нет
- Aesthetic Dermal Filler Injections For Facial Rejuvenation (PDFDrive)Документ60 страницAesthetic Dermal Filler Injections For Facial Rejuvenation (PDFDrive)Drhisham AttiaОценок пока нет
- Sample Birthing PlanДокумент2 страницыSample Birthing PlanChuohОценок пока нет
- Najib Khalife - Advances in TPET and Its Immunomodulatory Effect in NMDДокумент6 страницNajib Khalife - Advances in TPET and Its Immunomodulatory Effect in NMDMarina ShinkoОценок пока нет
- Ibuprofen - Pharmacology, Therapeutics and Side Effects. 2012Документ260 страницIbuprofen - Pharmacology, Therapeutics and Side Effects. 2012VuqarОценок пока нет
- Causes of Psychiatric Illness - JAMA - 2019Документ7 страницCauses of Psychiatric Illness - JAMA - 2019ran almogОценок пока нет
- Bitemporal HemianopiaДокумент7 страницBitemporal HemianopiasriОценок пока нет
- Qip ProjectДокумент13 страницQip Projectapi-534216481Оценок пока нет
- NCP Impaired Skin IntegrityДокумент3 страницыNCP Impaired Skin IntegrityMiar QuestОценок пока нет
- Penicillin Allergy DelabelingДокумент31 страницаPenicillin Allergy Delabelingapi-506607906Оценок пока нет
- Germ Cell Tumors (2003)Документ385 страницGerm Cell Tumors (2003)LeopoldОценок пока нет
- Apollo Hospitals: Porters Generic FrameworkДокумент6 страницApollo Hospitals: Porters Generic FrameworkVaibhav AroraОценок пока нет
- Changes in Central Corneal Thickness in Healthy Pregnant Women-A Clinical StudyДокумент3 страницыChanges in Central Corneal Thickness in Healthy Pregnant Women-A Clinical StudyIJAR JOURNALОценок пока нет
- Signs of Latent TetanyДокумент3 страницыSigns of Latent TetanyJohn GettyОценок пока нет
- Associate Professor:Ivan Bonet. Obstetric and Gynecology Associate Professor:Ivan Bonet. Obstetric and GynecologyДокумент31 страницаAssociate Professor:Ivan Bonet. Obstetric and Gynecology Associate Professor:Ivan Bonet. Obstetric and Gynecologyivan0% (1)
- Cns 765 Final Case StudyДокумент10 страницCns 765 Final Case Studyapi-581708536Оценок пока нет
- How To Protect Yourself and OthersДокумент2 страницыHow To Protect Yourself and OtherslistmyclinicОценок пока нет
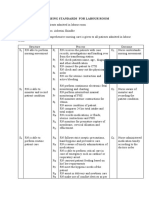
- Nursing Standards for Labour RoomДокумент3 страницыNursing Standards for Labour RoomRenita ChrisОценок пока нет
- Electrical Burn PathophysiologyДокумент1 страницаElectrical Burn PathophysiologydanicaОценок пока нет
- Challenges Providing Palliative Care Cancer Patients PalestineДокумент35 страницChallenges Providing Palliative Care Cancer Patients PalestineHammoda Abu-odah100% (1)
- AssociationBetweenBRAFV600EMutationand MortalityДокумент9 страницAssociationBetweenBRAFV600EMutationand MortalityMade RusmanaОценок пока нет
- Guide To Genetic CounselingДокумент24 страницыGuide To Genetic Counselingmady_elenutza0% (1)
- Patient Care Assistant ResumeДокумент8 страницPatient Care Assistant Resumeafazakemb100% (2)
- Geriatric Medicine Certification Examination Blueprint - ABIMДокумент7 страницGeriatric Medicine Certification Examination Blueprint - ABIMabimorgОценок пока нет
- Cap MRДокумент4 страницыCap MRKit BarcelonaОценок пока нет