Академический Документы
Профессиональный Документы
Культура Документы
Temperamental Differences Between Bipolar Disorder, Borderline Personality Disorder, and Attention Deficit/hyperactivity Disorder: Some Implications For Their Diagnostic Validity.
Загружено:
eduardobar2000Оригинальное название
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Temperamental Differences Between Bipolar Disorder, Borderline Personality Disorder, and Attention Deficit/hyperactivity Disorder: Some Implications For Their Diagnostic Validity.
Загружено:
eduardobar2000Авторское право:
Доступные форматы
Journal of Affective Disorders ()
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
Q1
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
45
46
47
48
49
50
51
52
53
54
55
56
57
58
59
60
61
62
63
64
65
66
Contents lists available at ScienceDirect
Journal of Affective Disorders
journal homepage: www.elsevier.com/locate/jad
Brief report
Temperamental differences between bipolar disorder, borderline
personality disorder, and attention decit/hyperactivity disorder:
Some implications for their diagnostic validity
Dominique Eich n, Alex Gamma, Tina Malti, Marianne Vogt Wehrli, Michael Liebrenz,
Erich Seifritz, Jiri Modestin
Psychiatric University Hospital, Research Department, Lenggstrasse 31, 8032 Zurich, Switzerland
art ic l e i nf o
a b s t r a c t
Article history:
Received 25 October 2013
Received in revised form
20 May 2014
Accepted 21 May 2014
Background: The relationship between borderline personality disorder (BPD), bipolar disorder (BD), and
attention decit/hyperactivity disorder (ADHD) requires further elucidation.
Methods: Seventy-four adult psychiatric in- and out-patients, each of them having received one of these
diagnoses on clinical assessment, were interviewed and compared in terms of diagnostic overlap, age
and sex distribution, comorbid substance, anxiety and eating disorders, and affective temperament.
Results: Diagnostic overlap within the three disorders was 54%. Comorbidity patterns and gender ratio
did not differ. The disorders showed very similar levels of cyclothymia.
Limitations: Sample size was small and only a limited number of validators were tested.
Conclusions: The similar extent of cyclothymic temperament suggests mood lability as a common
denominator of BPD, BD, and ADHD.
& 2014 Published by Elsevier B.V.
Keywords:
Borderline
bipolar
ADHD
Diagnostic validity
Temperament
1. Introduction
2. Materials and methods
An important part of establishing diagnostic validity for a disorder
is to delineate it from similar diagnoses in nosological space (Robins
and Guze, 1970), i.e. to establish discriminant validity. This is possible
by comparing the candidate disorders by a number of external
validators such as family history, sex distribution, onset and course,
treatment response, and comorbidity.
Here we are concerned with the discrimination between a triplet
of disorders that are frequently diagnosed and show considerable
empirical overlap: borderline personality disorder (BPD), bipolar
disorder (BD) and attention decit/hyperactivity disorder (ADHD).
This overlap consists of several aspects: rst, these disorders are
frequently co-morbid (Ferrer et al., 2010; Kessler et al., 2006; Perugi
et al., 2013); second, they show a moderate overlap in diagnostic
criteria (Milberger et al., 1995); third, in clinical practice, it is
sometimes difcult to know which of the three disorders a patient's
symptoms belong to (Nilsson et al., 2010; Skirrow et al., 2012). We
report results from a patient study comparing these diagnoses in
terms of diagnostic overlap, sex distribution, comorbidity, and
affective temperaments.
2.1. Patients
n
Correspondence to: Psychiatric University Hospital Zurich, Division of ADHD
research, Lenggstrasse 31, 8032 Zurich, Switzerland. Tel.: 41 443842615
E-mail address: Dominique.Eich@puk.ch (D. Eich).
Consecutive referrals to the Psychiatric University Hospital
(PUK) whose principal clinical ICD-10 diagnoses at admission were
either BD, BPD, or ADHD were recruited for thorough diagnostic
re-evaluation. As the number of adult patients with ADHD referred
for a psychiatric hospitalization is limited, out-patients treated at
the consultation service for ADHD were additionally recruited. Of
104 subjects initially asked for participation, 25 declined. Of the
remaining 79 subjects, 5 did not meet the diagnostic criteria. The
nal sample consisted of 74 patients: 27 with BPD, 24 with BD (17
bipolar-I and 7 bipolar-II), and 23 with ADHD. Before participation
in the study, all subjects received written study information and
gave their written informed consent. The study was approved by
the local ethics committee.
2.2. Psychometric and diagnostic re-evaluation
The levels of ve temperaments (depressive, hyperthymic,
cyclothymic, anxious, and irritable) during the lifespan were
assessed using the TEMPS-A (Akiskal et al., 2002) self-rating scale.
The TEMPS-A asks for a patient's state during most of their life.
DSM-IV and ICD-10 criteria for ADHD, which are nearly identical,
are geared towards children. They are limited to symptoms of
http://dx.doi.org/10.1016/j.jad.2014.05.028
0165-0327/& 2014 Published by Elsevier B.V.
Please cite this article as: Eich, D., et al., Temperamental differences between bipolar disorder, borderline personality disorder, and
attention.... Journal of Affective Disorders (2014), http://dx.doi.org/10.1016/j.jad.2014.05.028i
D. Eich et al. / Journal of Affective Disorders ()
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
45
46
47
48
49
50
51
52
53
54
55
56
57
58
59
60
61
62
63
64
65
66
inattention, hyperactivity and impulsivity. Additional criteria
allowing for diagnosis of ADHD in adults have been established
by Wender (1995) in the so-called Utah-criteria. They include
additional subscales for affective lability, temperament, emotional
excitability, and disorganization, and are operationalized in the
clinician-administered WenderReimherr Interview (Ro
sler et al.,
2008), which was the diagnostic tool used in the present study.
In addition, the WURS-k (Retz-Junginger et al., 2003) and ADHS-SB
(Ro
sler et al., 2004) self-rating scales, which incorporate both
ICD-10 and DSM-IV criteria, were used for the retrospective
assessment in adulthood of childhood ADHD and the current
assessment of adult ADHD, respectively. BPD, BD and comorbid
substance use, anxiety, and eating disorders were assessed by the
respective sections of SCID-I/II (First et al., 1997, 2002). BD patients
were interviewed during a euthymic state. Both initial and
re-evaluated diagnoses were made by experienced clinicians.
2.3. Statistics
Between-group comparisons of frequencies were carried
out using 2-tests; comparisons on continuous data used Mann
Whitney and KruskalWallis tests. Temperaments were not only
compared among groups dened by their primary diagnoses, but
also among groups of pure cases without diagnostic overlap.
There were 12 pure bipolar, 12 pure borderline, and 10 pure ADHD
patients. Analyses were performed in SPSS 20 (IBM SPSS Statistics
for Windows, Version 20.0. Armonk, NY: IBM Corp.).
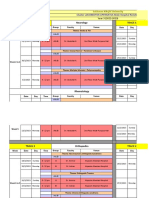
Table 2
Affective temperament.
Primary diagnosis
BPD
BD
ADHD
N
TEMPS-A
Depressive
Cyclothymic
Hyperthymic
Irritable
Anxious
27
Mean (SD)
12.2 (3.6)
13.0 (3.6)
8.5 (4.1)
10.5 (4.3)a
14.9 (4.5)
24
Mean (SD)
9.8 (3.6)
11.9 (4.7)
10.8 (4.8)
7.5 (5.1)
11.3 (5.9)b
23
Mean (SD)
10.9 (4.4)
12.7 (4.9)
10.2 (4.7)
10.0 (4.7)
15.2 (5.1)
.12
.72
.13
.017
.016
Pure diagnosis
BPD
BD
ADHD
N
TEMPS-A
Depressive
Cyclothymic
Hyperthymic
Irritable
Anxious
12
Mean (SD)
12.4 (3.7)c,d
10.7 (3.0)
6.6 (3.7)e
9.1 (3.0)f
14.2 (4.1)g
12
Mean (SD)
8.7 (2.8)
9.7 (4.9)
10.0 (4.7)
5.0 (3.6)
8.6 (5.4)h
10
Mean (SD)
7.7 (3.6)
9.6 (5.0)
10.9 (4.1)
7.9 (3.2)
12.3 (5.1)
.007
.66
.031
.035
.006
BPD Borderline personality disorder, BD Bipolar disorder, ADHD Attention
decit/hyperactivity disorder.
a
p o.02 vs. BD, MannWhitney U test.
p o .02 vs. ADHD, MannWhitney U test.
p o .02 vs. BD, MannWhitney U test.
d
p o .003 vs. ADHD, MannWhitney U test.
e
p o.007 vs. ADHD, MannWhitney U test.
f
p o .02 vs. BD, MannWhitney U test.
g
po .001 vs. BD, MannWhitney U test.
h
p o .05 vs. ADHD, MannWhitney U test.
b
c
3. Results
Sociodemographic data are shown in Table 1. Bipolar patients
were statistically signicantly older than borderline and ADHD
patients. No other differences were found.
For both groups dened by primary and by pure diagnoses,
irritable and anxious temperaments were the lowest in bipolar
patients. Hyperthymic temperament showed a trend towards lower
values in borderline patients in the primary groups, which became
signicant in the pure groups. Similarly, depressive temperament
showed a trend to be the highest in borderline patients in the
primary groups, which became signicant in the pure groups. Results
are summarized in Table 2.
The pattern of comorbidities among the three diagnoses BPD,
BD, and ADHD is shown in Table 3. All in all, 54% (40/74)
of patients were co-morbid with at least one other disorder
within the triplet of target diagnoses. No statistically signicant
differences in comorbidity with substance use, anxiety, or eating
disorders emerged.
4. Discussion
In a mixed sample of 74 in- and out-patients with primary
diagnoses of BPD, BD, and ADHD, there was considerable diagnostic overlap. At least half of the members of each disorder met
Table 1
Sociodemographic data.
Primary diagnosis
BPD
BD
ADHD
N (%)
Women
Age [mean (SD) years]
Living alone
Employed
27
20 (74)
32.8 (8.8)
20 (74)
13 (52)
24
16 (67)
41.8 (12.9)
17 (71)
11 (46)
23
15 (65)
31.3 (10.3)
17 (74)
15 (68)
.76
.01
.96
.35
Table 3
Comorbidity.
Primary diagnosis
BPD
BD
ADHD
N (%)
BPD
BD
ADHD
Botha
Total
27
6 (22)
7 (26)
2 (7)
15 (56)
24
6 (25)
4 (17)
2 (8)
12 (50)
23
7 (30)
8 (35)
2 (9)
13 (57)
Substance use
Anxiety disorders
Eating disorders
20 (74)
25 (93)
12 (44)
12 (50)
21 (87)
8 (33)
12 (52)
20( 87)
8 (35)
.15
.77
.67
BPD Borderline personality disorder, BD Bipolar disorder, ADHD Attention
decit/hyperactivity disorder.
a
Both comorbid diagnoses present: for BPD this means BD and ADHD were
also present; for BD it means that BPD and ADHD were also present; for ADHD it
means both BPD and BD were also present.
criteria for at least one of the other disorders. Consistent with this,
comorbidity rates for substance use, anxiety disorders and eating
disorder were very similar and not statistically signicantly
different among the groups. Levels of affective temperament were
partly similar among groups, with some notable differences: BPD
patients stood out by low levels of hyperthymia and by high
depressiveness, and BD patients stood out by low levels of anxious
and irritable-explosive temperament. These differences were all
statistically signicant in the pure groups. A cyclothymic temperament, however, was expressed on a similar and high level by BP,
BPD, and ADHD.
Due to the limited number of validators, this study could not
demonstrate with certainty that the three disorders are different,
let alone denitely the same. However, the ndings point to areas
of overlap and difference that should be investigated further in
larger studies.
Please cite this article as: Eich, D., et al., Temperamental differences between bipolar disorder, borderline personality disorder, and
attention.... Journal of Affective Disorders (2014), http://dx.doi.org/10.1016/j.jad.2014.05.028i
D. Eich et al. / Journal of Affective Disorders ()
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
45
46
47
48
49
50
51
52
53
54
55
56
57
58
59
60
61
62
63
64
65
66
The most striking commonality is the over 50% diagnostic overlap
between these disorders, accompanied by indistinguishable patterns
of comorbidity. While this nding matches frequent comments in the
literature on the difculty of differentiating among these disorders
(Akiskal et al., 1985a, 1985b, 1995; Akiskal, 1981; Nilsson et al., 2010;
Perugi and Akiskal, 2002; Skirrow et al., 2012), the overlap may seem
unusually strong. For example, Philipsen et al. (2008) found only 16%
comorbidity of BPD with ADHD. On the other hand, a more recent
study (Ferrer et al., 2010) reported a number as high as 38%.
Another commonality is the similar degree of cyclothymia in all
three diagnoses. Cyclothymia in the TEMPS-A is very broadly
dened as a chronic, but short-cycling instability of cognition
(sharp vs. dull), behavior (lively vs. sluggish), mood (euphoric vs.
dysphoric), energy (high vs. low), sociability (outgoing vs. withdrawn), self-condence (overcondent vs. unsure), and sleep (high
vs. low need). As such, this scale is likely to be sensitive to different
or overlapping manifestations of instability as encountered in BD,
BPD, and ADHD. High levels on the scale could therefore be
achieved without necessarily indicating a congruence of item
content among the disorders. This might make the scale rather
unspecic, unless the instability of mentation and behavior itself is
considered as a specic symptom. The concept of mood/emotional
lability might be a candidate for such a specic symptom that is
common to these disorders (MacKinnon and Pies, 2006; Perugi et
al., 2003; Skirrow and Asherson, 2012; Skirrow et al., 2009, but see
Benazzi (2008)), but plays itself out over somewhat different time
scales in ADHD, BPD, and BD. Mood lability, however, was not
examined in the present study.
Given the clinical knowledge that BPD and ADHD features are
chronic, interpretation of the temperament results for BD (e.g. lower
ratings for irritability and anxiousness) is difcult because lower
levels of these temperaments in BD could mean two things: BD
patients have a given temperament, but to a lesser extent than BPD
and ADHD; or, BD patients have a given temperament to the same
extent, but less often. Since the TEMPS-A asks for a patient's state
during most of their life, it is possible that bipolar respondents
form a temporal average of their temperament levels, resulting in a
lower value compared to the other, trait-like disorders.
This possibility may, for example, apply to the nding of a
tendency towards higher levels of depressiveness in BPD. BD
patients may episodically be as depressed as BPD patients, but
when evaluating most of their lives, they might rate their level of
depression lower than BPD patients. On the other hand, it is
possible that the intense dysphoria and chronic feelings of emptiness characteristic of BPD affect the depressive dimension of the
TEMPS-A more strongly than even the episodic depressiveness of
bipolar patients. They may also lead to a mitigating effect on
hyperthymia levels. This interpretation is consistent with previous
reports of weaker depressive temperament in BD compared to BPD
(Nilsson et al., 2010) and compared to patient controls (Kesebir et
al., 2005), as well as with a study in young adults showing a lack of
correlation of depressive temperament with either DSM- or broad
bipolar disorder, but a positive correlation with borderline symptoms (Walsh et al., 2012).
Irritable and anxious temperaments were stronger in the BPD
and ADHD groups compared to bipolar patients. This matches the
results found by Nilsson et al. (2010) for female BPD vs. BD
patients. While temporal averaging in BD patients could again be
an explanation, the strong association of irritability with borderline symptoms has been noted before (Walsh et al., 2012),
especially among patients with pronounced cyclothymia (Akiskal
et al., 1979). They display a tendency to overreact to aversive
stimuli with negative affect and to rapid shifts in mood with
erratic behaviors (Walsh et al., 2012).
Regarding high levels of anxious temperament in BPD and ADHD,
indirect support comes from ndings of high harm avoidance in
borderline (Barnow et al., 2006) and ADHD patients (Anckarster
et al., 2006; Mller et al., 2010; Salgado et al., 2009), since harm
avoidance refers to a general propensity for being pessimistic and
anxious. In both adult BPD (Ferrer et al., 2010; Philipsen et al., 2008)
and ADHD (Nigg et al., 2002; Skirrow and Asherson, 2012), high
comorbidity rates with anxiety symptoms and disorders have been
reported. However, the effect of having both disorders is not clear
yet. While in BPD women specic phobias and panic disorder were
related to comorbid ADHD (Philipsen et al., 2008); Ferrer et al. (2010)
reported less comorbidity with anxiety disorders in male and female
BPD patients with concomitant ADHD than those without ADHD
(Ferrer et al., 2010).
It is possible that the weaker anxious temperament in our BD
patients is due to their being mostly of the BP-I type. In BP-II
disorder, comorbid anxiety and panic disorders seem to be the rule
(Perugi et al., 2006; Perugi and Akiskal, 2002) and anxious
temperament is more frequent than in BP-I disorder (Fletcher
et al., 2012), in which it has been found not to differ from patientand relative-controls (Kesebir et al., 2005).
This study has signicant limitations. The sample size was
small. Only a limited number of diagnostic validators were used,
while many classical validators such as family history, age of onset,
course, treatment, consequences and outcomes were not available.
Participants were self-selected and may not be representative of
patients with these disorders in general. There is a possibility that
spurious diagnostic overlap could have been generated by inaccurate clinical assessment. We believe this to be unlikely since
our patients have been diagnosed twice (initial and re-evaluated
diagnosis) according to standardized criteria, and due attention
was paid to the fundamental differences of these disorders, such as
the episodic vs. chronic nature of BD and BPD/ADHD, respectively.
However, when comparing episodic with chronic disorders as in
the present study, psychometric ndings are ambiguous between
two alternative interpretations, one of which assumes temporal
averaging of rating levels over episodes, while the other assumes
that rating levels of one or several maximally severe episodes are
reported. Disambiguating between these possibilities requires
further studies addressed to this particular aspect of psychometric
evaluation.
In conclusion, weaker anxious and irritable temperament in BD
and stronger depressive and weaker hyperthymic temperament in
BPD separated the three diagnoses BPD, BD, and ADHD. These
temperamental differences were accentuated in the pure groups,
which might suggest the presence of distinct core disorders; thus
adding discriminant validity to the diagnostic separation of the
three disorders. This issue should be further investigated in more
highly powered studies. However, in the primary groups there was
considerable diagnostic overlap, indistinguishable comorbidity
rates for substance use, anxiety and eating disorders, and very
similar levels of cyclothymia, which may point to mood lability as
a common denominator of these disorders (Perugi et al., 2012).
Clinicians should be aware of the frequent co-occurrence of these
conditions and, when one of them is present, routinely check for
the presence of the other two.
Role of funding source
This study required no sponsoring or external funding, with the exception of
ML, who was nancially supported by the Prof. Dr. Max Clotta foundation, Zurich,
Switzerland, and the Uniscientia foundation, Vaduz, Principality of Liechtenstein.
These foundations played no role in any part of this study, viz. neither in the study
design, in the collection, analysis and interpretation of data, in the writing of the
report, and in the decision to submit the article for publication.
Conict of interest
DE, AG, TM, MVW, ML, ES, and JM declare that they have no conicts of interest.
Please cite this article as: Eich, D., et al., Temperamental differences between bipolar disorder, borderline personality disorder, and
attention.... Journal of Affective Disorders (2014), http://dx.doi.org/10.1016/j.jad.2014.05.028i
D. Eich et al. / Journal of Affective Disorders ()
1
Acknowledgments
Michael Liebrenz was nancially supported by the Prof. Dr. Max Clotta
2 Q2
foundation, Zurich, Switzerland, and the Uniscientia foundation, Vaduz, Principality
3
of Liechtenstein.
4
5
References
6
7
Akiskal, H.S., Brieger, P., Mundt, C., Angst, J., Marneros, A., 2002. Temperament und
8
affektive Sto
rungen. Der Nervenarzt 73, 262271.
9
Akiskal, H.S., Chen, S.E., Davis, G.C., Puzantian, V.R., Kasper, J., Bolinger, J.M., 1985a.
Borderline: an adjective in search of a noun. J. Clin. Psychiatr..
10 Q3
Akiskal, H.S., Khani, M.K., Scott-Strauss, A., 1979. Cyclothymic temperamental
11
disorders. Psychiatr. Clin. N. Am. 2, 527557.
12
Akiskal, H.S., Yerevanian, B.I., Davis, G.C., King, D., Lemmi, H., 1985b. The nosologic
status of borderline personalityclinical and polysomnographic study. Am. J.
13
Psychiatr. 142, 192198.
14
Akiskal, H.S.H., 1981. Subaffective disorders: dysthymic, cyclothymic and bipolar II
15
disorders in the borderline realm. Psychiatr. Clin. N. Am. 4, 2546.
Akiskal, H.S.H., Maser, J.D.J., Zeller, P.J.P., Endicott, J.J., Coryell, W.W., Keller, M.M.,
16
Warshaw, M.M., Clayton, P.P., Goodwin, F.F., 1995. Switching from unipolar to
17
bipolar II. An 11-year prospective study of clinical and temperamental pre18
dictors in 559 patients. Arch. Gen. Psychiatr. 52, 114123.
19
Anckarster, H., Stahlberg, O., Larson, T., Hakansson, C., Jutblad, S.-B., Niklasson, L.,
Nydn, A., Wentz, E., Westergren, S., Cloninger, C., Gillberg, C., Rastam, M.,
20
2006. The impact of ADHD and autism spectrum disorders on temperament,
21
character, and personality development. Am. J. Psychiatr. 163, 12391244.
22
Barnow, S., Herpertz, S.C., Spitzer, C., Stopsack, M., Preuss, U.W., Grabe, H.J., Kessler,
C., Freyberger, H.J., 2006. Temperament and character in patients with border23
line personality disorder taking gender and comorbidity into account. PsychoQ4
24
pathology 40, 369378.
25
Benazzi, F., 2008. A relationship between bipolar II disorder and borderline personality disorder? Prog. Neuropsychopharmacol. Biol. Psychiatr. 32, 10221029.
26
Ferrer, M., Andin, O., Matal, J., Valero, S., Navarro, J.A., Ramos-Quiroga, J.A.,
27
Torrubia, R., Casas, M., 2010. Comorbid attention-decit/hyperactivity disorder
28
in borderline patients denes an impulsive subtype of borderline personality
disorder. J. Personal. Disord. 24, 812822.
29
First, M.B., Gibbon, M., Williams, J.B.W., Spitzer, R.L., Benjamin, L.S., 1997. Structured
30
Clinical Interview for DSM-IV Axis II Personality Disorders (SCID-II). American
31
Psychiatric Press, Inc., Washington, D.C..
First, M.B., Spitzer, R.L., Gibbon, M., Williams, J.B.W., 2002. Structured Clinical
32
Interview for DSM-IV-TR Axis I Disorders, Research Version, Non-Patient
33
Edition (SCID-I/NP). Biometrics Research, New York State Psychiatric Institute,
34
New York.
35
Fletcher, K., Parker, G., Barrett, M., Synnott, H., McCraw, S., 2012. Temperament and
personality in bipolar II disorder. J. Affect. Disord. 136, 304309.
36
Kesebir, S., Vahip, S., Akdeniz, F., Ync, Z., Alkan, M., Akiskal, H., 2005. Affective
37
temperaments as measured by TEMPS-A in patients with bipolar I disorder and
38
their rst-degree relatives: a controlled study. J. Affect. Disord. 85, 127133.
Kessler, R.C.R., Adler, L.L., Barkley, R.R., Biederman, J., Conners, C.K.C., Demler, O.O.,
39
Faraone, S.V., Greenhill, L.L.L., Howes, M.J.M., Secnik, K.K., Spencer, T.T., Ustun, T.B.T.,
40
Walters, E.E.E., Zaslavsky, A.M.A., 2006. The prevalence and correlates of adult
41
ADHD in the United States: results from the National Comorbidity Survey
Replication. Am. J. Psychiatr. 163, 716723.
42
MacKinnon, D.F., Pies, R., 2006. Affective instability as rapid cycling: theoretical and
43
clinical implications for borderline personality and bipolar spectrum disorders.
44
Bipolar Disord. 8, 114.
Milberger, S., Biederman, J., Faraone, S.V., Murphy, J., Tsuang, M.T., 1995. Attention45
decit hyperactivity disorder and comorbid disordersissues of overlapping
46
symptoms. Am. J. Psychiatr. 152, 17931799.
47
48
Mller, D.J.D., Chiesa, A.A., Mandelli, L.L., De Luca, V.V., De Ronchi, D.D., Jain, U.U.,
Serretti, A.A., Kennedy, J.L.J., 2010. Correlation of a set of gene variants, life
events and personality features on adult ADHD severity. J. Psychiatr. Res. Q5
44598604
Nigg, J.T., John, O.P., Blaskey, L.G., Huang-Pollock, C.L., Willcutt, E.G., Hinshaw, S.P.,
Pennington, B., 2002. Big ve dimensions and ADHD symptoms: links between
personality traits and clinical symptoms. J. Personal. Soc. Psychol. 83, 451469.
Nilsson, A.K.K., Jrgensen, C.R., Straarup, K.N., Licht, R.W., 2010. Severity of affective
temperament and maladaptive self-schemas differentiate borderline patients,
bipolar patients, and controls. Compr. Psychiatr. 51, 486491.
Perugi, G., Angst, J., Azorin, J.-M., Bowden, C., Vieta, E., Young, A.H., The BRIDGE
Study Group, 2013. The bipolar-borderline personality disorders connection in
Q6
major depressive patients. Acta Psychiatr. Scand.128376383
Perugi, G., Toni, C., Maremmani, I., Tusini, G., Ramacciotti, S., Madia, A., Fornaro, M.,
Akiskal, H.S., 2012. The inuence of affective temperaments and psychopathological traits on the denition of bipolar disorder subtypes: a study on bipolar I
Italian national sample. J. Affect. Disord. 136, e41e49.
Perugi, G., Toni, C., Passino, M.C.S., Akiskal, K.K., Kaprinis, S., Akiskal, H.S., 2006.
Bulimia nervosa in atypical depression: the mediating role of cyclothymic
temperament. J. Affect. Disord. 929197
Perugi, G., Toni, C., Travierso, M.C., Akiskal, H.S., 2003. The role of cyclothymia in
atypical depression: toward a data-based reconceptualization of the
borderline-bipolar II connection. J. Affect. Disord. 73, 8798.
Perugi, G.G., Akiskal, H.S., 2002. The soft bipolar spectrum redened: focus on the
cyclothymic, anxious-sensitive, impulse-dyscontrol, and binge-eating connection in bipolar II and related conditions. Psychiatr. Clin. N. Am. 25, 713737.
Philipsen, A., Limberger, M.F., Lieb, K., Feige, B., Kleindienst, N., Ebner-Priemer, U.,
Barth, J., Schmahl, C., Bohus, M., 2008. Attention-decit hyperactivity disorder
as a potentially aggravating factor in borderline personality disorder. Br. J.
Psychiatr. 192, 118123.
Retz-Junginger, P., Retz, W., Blocher, D., Stieglitz, R.-D., Georg, T., Supprian, T.,
Wender, P.H., Ro
sler, M., 2003. Reliability and validity of the German short
version of the WenderUtah rating scale for the retrospective assessment of
attention decit/hyperactivity disorder. Nervenarzt 74, 987993.
Robins, E., Guze, S.B., 1970. Establishment of diagnostic validity in psychiatric
illness: its application to schizophrenia. Am. J. Psychiatr. 126, 983987.
Ro
sler, M., Retz, W., Retz-Junginger, P., Thome, J., Supprian, T., Nissen, T., Stieglitz,
R.-D., Blocher, D., Hengesch, G., Trott, G.E., 2004. Tools for the diagnosis of
attention-decit/hyperactivity disorder in adults. Self-rating behaviour questionnaire and diagnostic checklist. Nervenarzt 75, 888895.
Ro
sler, M., Retz-Junginger, P., Retz, W., Stieglitz, R.-D., 2008. HASEHomburgerADHS-Skalen fr Erwachsene. Hogrefe, Go
ttingen.
Salgado, C.A.I., Bau, C.H.D., Grevet, E.H., Fischer, A.G., Victor, M.M., Kalil, K.L.S.,
Sousa, N.O., Garcia, C.R., Belmonte-de-Abreu, P., 2009. Inattention and hyperactivity dimensions of ADHD are associated with different personality proles.
Psychopathology 42, 108112.
Skirrow, C., Asherson, P., 2012. Emotional lability, comorbidity and impairment in Q7
adults with attention-decit hyperactivity disorder. J. Affect. Disord., 18.
Skirrow, C., Hosang, G.M., Farmer, A.E., Asherson, P., 2012. An update on the
debated association between ADHD and bipolar disorder across the lifespan. J.
Affect. Disord. 141, 143159.
Skirrow, C., McLoughlin, G., Kuntsi, J., Asherson, P., 2009. Behavioral, neurocognitive
and treatment overlap between attention-decit/hyperactivity disorder and
mood instability. Expert Rev. Neurother. 9, 489503.
Walsh, M.A., Royal, A.M., Barrantes-Vidal, N., Kwapil, T.R., 2012. The association of
affective temperaments with impairment and psychopathology in a young
adult sample. J. Affect. Disord. 141, 373381.
Wender, P.H., 1995. Attention-decit hyperactivity disorder in adults. University
Press, Oxford.
Please cite this article as: Eich, D., et al., Temperamental differences between bipolar disorder, borderline personality disorder, and
attention.... Journal of Affective Disorders (2014), http://dx.doi.org/10.1016/j.jad.2014.05.028i
Вам также может понравиться
- Bruch 1958 PDFДокумент6 страницBruch 1958 PDFeduardobar2000Оценок пока нет
- Borderline - An Adjective in Search of A NoumДокумент8 страницBorderline - An Adjective in Search of A Noumeduardobar2000Оценок пока нет
- Moskowitz.2004 Catatonia - Evolutionary PDFДокумент19 страницMoskowitz.2004 Catatonia - Evolutionary PDFeduardobar2000Оценок пока нет
- Obesity, The Jews and Psychoanalisis (Sander L. Gilman, 2006)Документ13 страницObesity, The Jews and Psychoanalisis (Sander L. Gilman, 2006)eduardobar2000Оценок пока нет
- Effect of Combined Naltrexone and Bupropion Therapy On The Brain's Reactivity To Food CuesДокумент7 страницEffect of Combined Naltrexone and Bupropion Therapy On The Brain's Reactivity To Food Cueseduardobar2000Оценок пока нет
- Developmental Obesity and SchizophreniaДокумент6 страницDevelopmental Obesity and Schizophreniaeduardobar2000100% (1)
- Moving Towards Causality in Attention-Deficit Hyperactivity Disorder: Overview of Neural and Genetic MechanismsДокумент13 страницMoving Towards Causality in Attention-Deficit Hyperactivity Disorder: Overview of Neural and Genetic Mechanismseduardobar2000100% (1)
- Aspectos Psicologicos de La ObesidadДокумент14 страницAspectos Psicologicos de La ObesidadNicolás CanalesОценок пока нет
- Child Murder by Parents and Evolutionary PsychologyДокумент15 страницChild Murder by Parents and Evolutionary Psychologyeduardobar2000Оценок пока нет
- Aspectos Psicologicos de La ObesidadДокумент14 страницAspectos Psicologicos de La ObesidadNicolás CanalesОценок пока нет
- Schizophrenia and Suicide: Systematic Review of Risk FactorsДокумент13 страницSchizophrenia and Suicide: Systematic Review of Risk Factorseduardobar2000Оценок пока нет
- The Association of Restrained Eating With Weight Change Over Time in A Community-Based Sample of TwinsДокумент13 страницThe Association of Restrained Eating With Weight Change Over Time in A Community-Based Sample of Twinseduardobar2000Оценок пока нет
- The Relationship Between Dissociation and Voices: A Systematic Literature Review and Meta-AnalysisДокумент52 страницыThe Relationship Between Dissociation and Voices: A Systematic Literature Review and Meta-Analysiseduardobar2000100% (1)
- BMJ f185 Full PDFДокумент13 страницBMJ f185 Full PDFeduardobar2000Оценок пока нет
- Kretschmer. Heredity and Constitution.Документ4 страницыKretschmer. Heredity and Constitution.eduardobar2000Оценок пока нет
- "Scared Stiff": Catatonia As An Evolutionary-Based Fear ResponseДокумент19 страниц"Scared Stiff": Catatonia As An Evolutionary-Based Fear Responseeduardobar2000Оценок пока нет
- Homology, Homoplasy, Novelty, and BehaviorДокумент9 страницHomology, Homoplasy, Novelty, and Behavioreduardobar2000Оценок пока нет
- (CANMAT) GuideliCanadian Network For Mood and Anxiety Treatmentsnes For The Management of Patients WithbipolarДокумент65 страниц(CANMAT) GuideliCanadian Network For Mood and Anxiety Treatmentsnes For The Management of Patients WithbipolarDahij1014Оценок пока нет
- Towards A Bottom-Up Perspective On Animal and Human CognitionДокумент8 страницTowards A Bottom-Up Perspective On Animal and Human Cognitioneduardobar2000Оценок пока нет
- Systems Genetics of Obesity in An F2 Pig Model by Genome-Wide Association, Genetic Network, and Pathway AnalysesДокумент15 страницSystems Genetics of Obesity in An F2 Pig Model by Genome-Wide Association, Genetic Network, and Pathway Analyseseduardobar2000Оценок пока нет
- Animal Models of Obsessive-Compulsive Disorder: Exploring Pharmacology and Neural SubstratesДокумент17 страницAnimal Models of Obsessive-Compulsive Disorder: Exploring Pharmacology and Neural Substrateseduardobar2000Оценок пока нет
- Changes in Body Composition Over 8 Years in A Randomized Trial of A Lifestyle Intervention: The Look AHEAD StudyДокумент8 страницChanges in Body Composition Over 8 Years in A Randomized Trial of A Lifestyle Intervention: The Look AHEAD Studyeduardobar2000Оценок пока нет
- Constraints and Flexibility in Mammalian Social Behaviour: Introduction and SynthesisДокумент10 страницConstraints and Flexibility in Mammalian Social Behaviour: Introduction and Synthesiseduardobar2000Оценок пока нет
- Psychobiological Traits in The Risk Profile For Overeating and Weight GainДокумент5 страницPsychobiological Traits in The Risk Profile For Overeating and Weight Gaineduardobar2000Оценок пока нет
- The Hunger Genes: Pathways to Obesity and Individual SusceptibilityДокумент14 страницThe Hunger Genes: Pathways to Obesity and Individual Susceptibilityeduardobar2000Оценок пока нет
- The Nocturnal Bottleneck and The Evolution of Activity Patterns in MammalsДокумент11 страницThe Nocturnal Bottleneck and The Evolution of Activity Patterns in Mammalseduardobar2000Оценок пока нет
- The Thrifty Psychiatric PhenotypeДокумент3 страницыThe Thrifty Psychiatric Phenotypeeduardobar2000Оценок пока нет
- Neural Control of Energy Balance: Translating Circuits To TherapiesДокумент13 страницNeural Control of Energy Balance: Translating Circuits To Therapieseduardobar2000Оценок пока нет
- Nutrition: Applied Nutritional InvestigationДокумент6 страницNutrition: Applied Nutritional Investigationeduardobar2000Оценок пока нет
- Obese-Type Gut Microbiota Induce Neurobehavioral Changes in The Absence of ObesityДокумент9 страницObese-Type Gut Microbiota Induce Neurobehavioral Changes in The Absence of Obesityeduardobar2000Оценок пока нет
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceОт EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceРейтинг: 4 из 5 звезд4/5 (894)
- The Yellow House: A Memoir (2019 National Book Award Winner)От EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Рейтинг: 4 из 5 звезд4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingОт EverandThe Little Book of Hygge: Danish Secrets to Happy LivingРейтинг: 3.5 из 5 звезд3.5/5 (399)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeОт EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeРейтинг: 4 из 5 звезд4/5 (5794)
- Never Split the Difference: Negotiating As If Your Life Depended On ItОт EverandNever Split the Difference: Negotiating As If Your Life Depended On ItРейтинг: 4.5 из 5 звезд4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureОт EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureРейтинг: 4.5 из 5 звезд4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryОт EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryРейтинг: 3.5 из 5 звезд3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerОт EverandThe Emperor of All Maladies: A Biography of CancerРейтинг: 4.5 из 5 звезд4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreОт EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreРейтинг: 4 из 5 звезд4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyОт EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyРейтинг: 3.5 из 5 звезд3.5/5 (2219)
- Team of Rivals: The Political Genius of Abraham LincolnОт EverandTeam of Rivals: The Political Genius of Abraham LincolnРейтинг: 4.5 из 5 звезд4.5/5 (234)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersОт EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersРейтинг: 4.5 из 5 звезд4.5/5 (344)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaОт EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaРейтинг: 4.5 из 5 звезд4.5/5 (265)
- The Unwinding: An Inner History of the New AmericaОт EverandThe Unwinding: An Inner History of the New AmericaРейтинг: 4 из 5 звезд4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)От EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Рейтинг: 4.5 из 5 звезд4.5/5 (119)
- Nervous System and Endocrine SystemДокумент90 страницNervous System and Endocrine SystemCeres LucenteОценок пока нет
- Neuro Motor Readiness Pl2011Документ94 страницыNeuro Motor Readiness Pl2011mohitnet1327100% (3)
- Kessler 2005Документ11 страницKessler 2005mccg1478Оценок пока нет
- Psychedelic IntegrationДокумент91 страницаPsychedelic IntegrationWhomever me100% (3)
- Axonal degeneration: causes, effects and regenerationДокумент1 страницаAxonal degeneration: causes, effects and regenerationYogi drОценок пока нет
- Pinocchio SyndromeДокумент1 страницаPinocchio SyndromeTakeshi ClairОценок пока нет
- Five Senses Lesson PlanДокумент6 страницFive Senses Lesson PlanJolie rose CapanОценок пока нет
- Ana Phisio Lab Report.Документ4 страницыAna Phisio Lab Report.Diana Amor100% (1)
- What Is The Nervous SystemДокумент3 страницыWhat Is The Nervous SystemSittie Asleah SandiganОценок пока нет
- Principles of Hearing Aid AudiologyДокумент9 страницPrinciples of Hearing Aid AudiologyANURAG PANDEYОценок пока нет
- SMK MAMBAU SCIENCE CURRICULUM SPECIFICATIONSДокумент26 страницSMK MAMBAU SCIENCE CURRICULUM SPECIFICATIONSNurul AzniОценок пока нет
- Perceptual Pleasure and The Brain by Irving Biederman & Edward VesselДокумент8 страницPerceptual Pleasure and The Brain by Irving Biederman & Edward VesselAmiraОценок пока нет
- Otvori Glave PDFДокумент1 страницаOtvori Glave PDFAnnieОценок пока нет
- Brainstem Bravo AnnotatedДокумент13 страницBrainstem Bravo AnnotatedMia CadizОценок пока нет
- Febrile SeizureДокумент6 страницFebrile SeizurepipimseptianaОценок пока нет
- The Rare and The Unexpected Miller Fisher SyndromeДокумент4 страницыThe Rare and The Unexpected Miller Fisher SyndromedoctorebrahimОценок пока нет
- Trace Decay Theory of ForgettingДокумент3 страницыTrace Decay Theory of ForgettingJecel Biagan100% (2)
- Perception Chapter 2Документ37 страницPerception Chapter 2Hajra ArifОценок пока нет
- Abnormal Psychology 7th Edition by Susan Nolen Hoeksema-Test BankДокумент60 страницAbnormal Psychology 7th Edition by Susan Nolen Hoeksema-Test BankakasagillОценок пока нет
- Neurologic NCLEX Practice Test Part 1Документ10 страницNeurologic NCLEX Practice Test Part 1mpasague100% (2)
- Lesions of Upper Motor Neurons and Lower Motor NeuronsДокумент9 страницLesions of Upper Motor Neurons and Lower Motor NeuronsAdhitya Rama Jr.Оценок пока нет
- Responses in Animals-OCR Biology A2Документ17 страницResponses in Animals-OCR Biology A2Alan TaylorОценок пока нет
- ILAE classification of seizures and epilepsyДокумент13 страницILAE classification of seizures and epilepsyKrissia SalvadorОценок пока нет
- Understanding Kundalini Energy and its Role in Spiritual EvolutionДокумент190 страницUnderstanding Kundalini Energy and its Role in Spiritual Evolutionnityanandroy100% (1)
- Sulaiman AlRajhi University Neurology & Orthopedics Hospital Rotation ScheduleДокумент10 страницSulaiman AlRajhi University Neurology & Orthopedics Hospital Rotation ScheduleAbdullah MelhimОценок пока нет
- Neuroplasticity: Presented By: Advincula, Arnina Fortus, Jacyrone Pitpit, MarcusДокумент17 страницNeuroplasticity: Presented By: Advincula, Arnina Fortus, Jacyrone Pitpit, MarcusCLAIRE DENISSE DEVISОценок пока нет
- Surgical Treatment of Traumatic Bifrontal Contusion When and HowДокумент37 страницSurgical Treatment of Traumatic Bifrontal Contusion When and HowNGUYỄN HOÀNG LINHОценок пока нет
- Brain Booster WorkbookДокумент10 страницBrain Booster WorkbookPete Singh50% (2)
- Brain Parts and Functions Chart KeyДокумент2 страницыBrain Parts and Functions Chart Keybhihi jkgug;u75% (4)
- WBBSE Class IX English SyllabusДокумент47 страницWBBSE Class IX English SyllabusSoumadip MukherjeeОценок пока нет