Академический Документы
Профессиональный Документы
Культура Документы
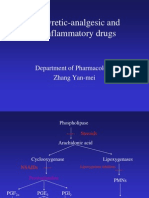
NSAID Mechanism COX Inhibition
Загружено:
Wissam DadiИсходное описание:
Оригинальное название
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
NSAID Mechanism COX Inhibition
Загружено:
Wissam DadiАвторское право:
Доступные форматы
a) Pharmacological class : NSAID Non selective inhibitors of the isoenzymes (COX-1 and COX-2)
b) Mechanism of Action : Ibuprofen is a non-selective inhibitor of cyclooxygenase, an
enzyme involved in prostaglandin synthesis via the arachidonic acid pathway. Its
pharmacological effects are believed to be due to inhibition cylooxygenase-2 (COX-2)
which decreases the synthesis of prostaglandins involved in mediating inflammation,
pain, fever and swelling. Antipyretic effects may be due to action on the hypothalamus,
resulting in an increased peripheral blood flow, vasodilation, and subsequent heat
dissipation. Inhibition of COX-1 is thought to cause some of the side effects of ibuprofen
including GI ulceration.
c) Pharmacologic effects :
It decreases the synthesis of prostaglandins involved in mediating inflammation, pain,
fever and swelling. Antipyretic effects may be due to action on the hypothalamus,
resulting in an increased peripheral blood flow, vasodilation, and subsequent heat
dissipation.
d) Therapeutic uses (indications) : For symptomatic treatment of rheumatoid arthritis,
juvenile rheumatoid arthritis and osteoarthritis. May be used to treat mild to moderate
pain and for the management of dysmenorrhea. May be used to reduce fever. Has been
used with some success for treating ankylosing spondylitis, gout and psoriatic arthritis.
May reduce pain, fever and inflammation of pericarditis. May be used IV with opiates to
relieve moderate to severe pain. Ibuprofen lysine may be used IV to treat patent ductus
arteriosus (PDA) in premature neonates.
e) Adverse Effects : Common adverse effects include: nausea, dyspepsia,
gastrointestinal ulceration/bleeding, raised liver enzymes, diarrhea, constipation,
epistaxis, headache, dizziness, rash, salt and fluid retention, and hypertension.
Infrequent adverse effects include: esophageal ulceration, heart failure, MI,
hyperkalemia, renal impairment CA, confusion, and bronchospasm. Ibuprofen can
exacerbate asthma, sometimes fatally. In skin ibuprofen has been associated with the
onset of bullous pemphigoid. it has been reported to be a photosensitizing agent and
extremely rare cause of the autoimmune disease Stevens-Johnson syndrome. It can
also cause erectile dysfunction or Miscarriage and Rhabdomyolysis, especially in people
with with high blood cholesterol, hyperlipidemia, high blood pressure, depression.
f) Contraindications : IBU tablets are contraindicated in patients with known
hypersensitivity to Ibuprofen. Should not be given to patients who have experienced
asthma, urticaria, or allergic-type reactions after taking aspirin or other NSAIDs. Severe,
rarely fatal, anaphylactic-like reactions to NSAIDs have been reported in such patients.
IBU tablets are contraindicated for the treatment of peri-operative pain in the setting of
coronary artery bypass graft (CABG) surgery.
g) Pharmacography : Cap 200mg, tab40/200/400/600/800mg, IV 100mg/ml
h) Prescription
Dg/ Rheumatoid arthritis
Rp/Ibuprofen 200mg
Nr. XLII
D.s. orally 3 tabs per day for 14days
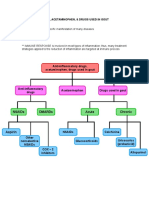
a) Pharmacological class : NSAID
b) Mechanism of Action : Acetaminophen is thought to act primarily in the CNS,
increasing the pain threshold by inhibiting both isoforms of cyclooxygenase, COX-1,
COX-2, and COX-3 enzymes involved in prostaglandin (PG) synthesis. Unlike NSAIDs,
acetaminophen does not inhibit cyclooxygenase in peripheral tissues and, thus, has no
peripheral anti-inflammatory affects. Studies suggest that acetaminophen selectively
blocks COX-3. Its exact mechanism of action is still poorly understood.
c) Pharmacologic effects : Acetaminophen inhibits prostaglandin synthesis in the CNS.
This explains its antipyretic properties from direct effects on the heat-regulating centers
of the hypothalamus resulting in peripheral vasodilation, sweating and hence heat
dissipation and analgesic properties. It has less effect on cyclooxygenase in peripheral
tissues, which accounts for its weak anti-inflammatory activity and does not affect
platelet function or increase blood clotting time.
d) Therapeutic uses (indications) : Acetaminophen is a suitable substitute for the
analgesic and antipyretic effects of aspirin for those patients with gastric complaints,
those in whom prolongation of bleeding time would be a disadvantage, or those who do
not require the anti-inflammatory action of aspirin. Acetaminophen is the
analgesic/antipyretic of choice for children with viral infections or chickenpox (recall that
aspirin increases the risk of Reye's syndrome and does not antagonize the uricosuric
agents probenecid or sulfinpyrazone and, therefore, may be used in patients with gout
who are taking these drugs.
e) Adverse Effects : Skin rash and minor allergic reactions occur infrequently. There may
be minor alterations in the leukocyte count, but these are generally transient. Renal
tubular necrosis and hypoglycemic coma are rare complications of prolonged, largedose therapy. With large doses of acetaminophen Hepatic necrosis, a very serious and
potentially life-threatening condition, can result. Renal tubular necrosis may also occur.
f) Contraindications : Liver Failure, Liver Problems, Serious Kidney Problems
g) Pharmacography :Tabs 500mg/1000mg, capsule, liquid suspension, suppository, IV,IM
h) Prescription
Dg/ fever
Rp/Paracetamol 500mg
Nr. XII
D.s. orally 1 tab every 6 hours for 3 days
a) Pharmacological class : NSAID
b) Mechanism of Action : IRREVERSIBLY inactivates cyclooxygenase, inhibiting
prostaglandin formation. This ability gives its anti-inflammatory, antipyretic and
analgesic effects.
The first two are due to the blockade of prostaglandin synthesis at the
thermoregulatory centers in the hypothalamus and at peripheral target sites.
The analgesic effect is due to the decrease of prostaglandin synthesis preventing
sintetization of pain receptors to both mechanical and chemical stimuli. It also
depress pain stimuli at subcortical sites (thalamus and hypothalamus).
c) Pharmacologic effects :
anti-inflammatory and antirheumatic action: modulates those aspects of
inflammation in which prostaglandins act as mediators
analgesic action: used mainly for the management of pain of low to
moderate intensity arising from musculoskeletal disorders
antipyretic action: lowers the body temperature of febrile patients by
increasing heat dissipation as a result of peripheral vasodilation and sweating.
Respiratory effects: increasing alveolar ventilation.
Gastric effects: increases acid secretion and decreases mucus formation.
Platelet effects: platelet aggregation (the first step in thrombus formation) is
reduced, producing an anticoagulant effect with a prolonged bleeding time.
Kidney effects: causing retention of sodium and water and may cause
edema and hyperkalemia.
d) Therapeutic uses (indications) :
Anti-inflammatory, antipyretic, and analgesic uses: used in the treatment
of gout, rheumatic fever, osteoarthritis, and Rheumatoid Arthritis. Commonly
treated conditions requiring analgesia include headache, arthralgia, and
myalgia.
External applications: used topically to treat corns, calluses, and warts.
Cardiovascular applications: used to inhibit platelet aggregation. Low doses
are used prophylactically to:
o Reduce the risk of recurring transient ischemic attacks and stroke or
death.
o Reduce the risk of death in those having an acute myocardial infarction.
o Reduce the risk of recurrent nonfatal myocardial infarction and/or death
o Reduce the risk of myocardial infarction and sudden death in patients
with chronic stable angina pectoris.
e) Adverse effect :
Gastrointestinal: Epigastric distress, nausea, vomiting and microscopic GI
bleeding.
Blood: inhibition of platelet aggregation and a prolonged bleeding time
Respiratory: In toxic doses,it can cause respiratory depression and a
combination of uncompensated respiratory and metabolic acidosis.
Hypersensitivity: causing urticaria, bronchoconstriction, or angioedema.
Reye's syndrome: when given during viral infections, it has been associated
with an increased incidence of Reye's syndrome, which is an often fatal,
fulminating hepatitis with cerebral edema, especially encountered in children.
f) Contraindications :
Gastrointestinal: not to take with empty stomach.
Blood: Should not be taken for at least one week prior surgery.
Pregnancy and breast feeding.
g) Pharmacography : Oral or rectal administration. Aspirin exhibits analgesic activity
at low doses; only at higher doses do these drugs show anti-inflammatory activity.
For example, two 325-mg.
h) Prescription
Dg/ Muscular pain
Rp/ Acetylsalicylic acid/Aspirine
Nr. X
D.s. orally 1 tab every 12h for 5 days
a) Pharmacological class : NSAID
b) Mechanism of Action : selective noncompetitive reversible inhibitor of
cyclooxygenase-2 (COX-2) enzyme that synthetizes prostaglandin and thromboxane.
c) Pharmacologic effects :
anti-inflammatory and antirheumatic.
Analgesic action: for acute pain.
Gastric effects: increases acid gastric secretion and decreases mucus production.
Kidney effects: increases water and sodium retention.
d) Therapeutic uses (indications) :
Relief and management of rheumatoid arthritis and osteoarthritis
acute pain
primary dysmenorrhea
Familial adenomatous polyposis.
e) Adverse Effects :
37% increase in incidence of major vascular events: non-fatal myocardial infarction,
non-fatal stroke or death from a vascular cause.
81% increase in incidence of upper gastrointestinal complications: perforations,
obstructions or bleeds.
Hematologic events: anemia may occur.
Skin reactions.
f) Contraindications :
hypersensitivity.
Severe hepatic impairment.
History of asthma or urticaria.
Renal disease.
Late pregnancy and breast feeding
g) Pharmacography : 50, 100, 200, 400mg capsule
h) Prescription
Dg/ Osteoarthritis
Rp/ Celecoxib 200mg
Nr. XXX
D.s. 1 per 24h after meal for 1 month
a) Pharmacological class : NSAID
b) Mechanism of Action :
The inhibition of cyclooxygenase leads to the inhibition of prostaglandin synthesis. In
low dosages it shows selectivity for COX2.
c) Pharmacologic effects :
analgesic
antipyretic.
anti-inflammatory.
d) Therapeutic uses (indications) :
Indicated to relieve pain, tenderness, swelling, and stiffness associated with arthritis.
e) Adverse Effects :
chest pain, weakness, shortness of breath, slurred speech, problems with
vision or balance;
black, bloody, or tarry stools
coughing up blood or vomit that looks like coffee grounds;
swelling or rapid weight gain;
urinating less than usual or not at all;
nausea, upper stomach pain, itching, loss of appetite, dark urine, clay-colored
stools, jaundice (yellowing of the skin or eyes);
Severe skin reaction, fever, sore throat, swelling in your face or tongue,
burning in your eyes, skin pain, followed by a red or purple skin rash that
spreads (especially in the face or upper body) and causes blistering and
peeling.
f) contraindications :
Active ulcers.
Hepatic/renal insufficiency
Pregnancy and breast feeding.
Hypersensitivity
asthma
g) Pharmacography : Tablets: 7.5, 15 mg. Oral Suspension: 7.5 mg/ml
h) Prescription
Dg/ Arthritis
Rp/ Meloxicam 7,5mg
Nr. XX
D.s. 1 per 12h after meal for 10 days
a) Pharmacological class : Non absorbed antacid
b) Mechanism of Action : neutralize or buffer stomach acid with no direct effect on its
output, increasing pH and increases intra-esophageal pH and decrease pepsin activity
c) Phamacologic effects:
o antacid
o antiurolithic: reduction of phosphates in urine preventing urinary stones.
o Antihyperphosphatemic: reduce serum phosphate levels.
o Antihypocalcemic: increase the release of calcium from bone.
o Antidiarrheal: decrease fluidity of stools.
d) Therapeutic uses:
antiacid
antiurolithc
antihyperphosphatemic
antihypocalcemic.
Antidiarrheal
e) adverse effects:
Nausea
Diarrhoea
Constipation.
f) contraindications: Not to be taken with iron preparates or antibiotics
g) Parmacography: Tabs 400-800mg chewed, suspension
h) Prescription :
Dg/ GERD
Rp/ Maalox suspension
Nr. I
D.s. orally after meal 3 times per day for a
week
a) Pharmacological class : Mucosal protective agent
b) Mechanism of Action : It forms a protective coat. As an antidiarrheal, the exact
mechanism has not been determined. Bismuth subsalicylate may exert its antidiarrheal
action not only by stimulating absorption of fluid and electrolytes across the intestinal
wall (anti-secretory action) but also, when hydrolyzed to salicylic acid, by inhibiting
synthesis of a prostaglandin responsible for intestinal inflammation and hyper motility. In
addition, bismuth subsalicylate binds toxins produced by Escherichia coli. Both bismuth
subsalicylate and the intestinal reaction products, bismuth oxychloride and bismuth
hydroxide, are believed to have bactericidal action. As an antacid, bismuth has weak
antacid properties.
c) Pharmacologic effects: Bismuth subsalicylate displays anti-inflammatory action (due to
salicylic acid) and also acts as an antacid and mild antibiotic. It can also cause a black
tongue and black stools in some users of the drug, when it combines with trace amounts
of sulfur in their saliva and gastrointestinal tract. This discoloration is temporary and
harmless.
d) Therapeutic uses (indications) : Most important use is to treat H-pylori in a
combination with other drugs. Also used to treat nausea, heartburn, indigestion, upset
stomach, diarrhea, and other temporary discomforts of the stomach and gastrointestinal
tract.
e) Adverse Effects : It can cause a black tongue and black stools in some users of the
drug, when it combines with trace amounts of sulfur in saliva and the colon to form
bismuth sulfide. Bismuth sulfide is a highly insoluble black salt, and the discoloration
seen is temporary and harmless. Long-term use (greater than 6 weeks) may lead to
accumulation and toxicity. Also constipation and dry mouth are possible.
f) Contraindications: Children should not take medication with bismuth subsalicylate
while recovering from influenza or chicken pox, as epidemiologic evidence points to an
association between the use of salicylate-containing medications during certain viral
infections and the onset of Reye's syndrome. For the same reason, it is typically
recommended that nursing mothers not use medication containing bismuth subsalicylate
because small amounts of the medication are excreted in breast milk and pose a
theoretical risk of Reye's syndrome to nursing children.
g) Pharmacography : tabs, liquid, suppository, suspension
h) Prescription
Dg/ H-Pylori
Rp/ Bismuth Subsalicylate tabs
Nr. XXX
D.s. orally 3 tabs per day after food
a) Pharmacological class: H2 receptor antagonist.
b) Mechanism of action: competitively blocks the action of histamine on parietal cells in
the stomach decreasing their acid production. This is achieved by two ways:
a. Histamine released by enterocromoffin-like cells in the stomach is blocked from
binding on parietal cell H2 receptors.
b. Other substances that promote acid secretion (as gastrin, acetylcholine) have a
reduced effect on parietal cells when H2 receptors are blocked.
c) Pharmacologic effects: inhibit gastric acid secretion induced by histamine or gastrin.
d) Therapeutic uses:
a. Peptic ulcers.
b. Acute stress ulcers.
c. GERD.
d. Co-administered with NSAIDs to reduce risk of ulceration.
e. Preoperatively reduces risk of aspiration pneumonia.
e) adverse effects:
a. Reduction of vitamin B12 absorption.
b. Reduction of drugs absorption requiring acidic stomach.
c. Food or drug allergies.
d. Increase risk of pneumonia.
e. Increase risk of infectious diarrhea.
f. Fungal sepsis.
f) Contraindications:
a. Acute renal/cardiac failure.
b. Hypersensitivity.
g) Pharmacography:
a. Intravenous solution 1mg/ml or 25mg/ml
b. Tablet: 25, 75 150, 300mg.
c. Syrup: 15mg/ml
h) Prescription
Dg/ Peptic ulcer
Rp/Ranitidine tabl. 300mg
Nr.XXX
D.s. Orally, 1 tab every day for 30 days.
a) Pharmacological class: Proton pump inhibitor (antisecretory agent)
b) Mechanism of action: It binds the proton pump of the parietal cell supressing secretion
of hydrogen ions into the gastric lumen and thereby supressing secretion of gastric acid.
c) Pharmacologic effects: Inhibits both basal and stimulated gastric acid secretion.
d) Therapeutic uses:
Treating erosive esophagitis and active duodenal ulcer and eradicate H.pylori
together with antimicrobial regimens
Long-term treatment of pathologic hypersecretory conditions.
GERD
Reduce risk of bleeding from NSAIDs.
e) Adverse effects:
Increased concentrations of bacteria in stomach.
Low vitamin B12 (acid is required for its absorption).
Increased diarrhea.
f) Contraindications: When patient takes anticoagulant therapy
g) Pharmacography:
Capsule: 10, 20, 40 mg.
Tablets: 20mg, 40mg
b) Prescription : Combined for H. Pylori treatment
Dg/ Ulcer H. Pylori +
Rp1/Omeprazole, tab, 20 mg
Nr XXI
D.s1. Orally, 1tab/day/21days
Rp2/Amoxilcilin cap 500mg
Nr. XIV
D.s Orally 1 cap per 8 hours for 2 weeks
Rp3/Metronidazole tab 250mg
Nr. XIV
D.s Orally 1 tab per 8 hours for 2 weeks
a) Pharmacological class : Methylxanthines
b) Mechanism of Action :
It inhibits phosphodiesterase and results in increased intracellular cAMP which
may account for cardiac stimulation and smooth muscle relaxation
It inhibits the receptors of adenosine (modulators of adenylyl cyclase activity)
Adenosine is responsible for the isolated airway smooth muscle contraction and
histamine release from lung cells. Both these effects are antagonized by
theophylline
Anti-inflammatory action (type IV PDE) low-dose theophylline inhibits late
response to antigenic challenge
increases in CD4 and CD8 lymphocytes
c) Pharmacologic effects :
In Central Nervous System :
o increased alertness; reduced fatigue
o in more sensitive individuals: caffeine -- nervousness/insomnia
o very high methylxanthine doses: medullary stimulation, convulsions
o Primary side effect in patients requiring aminophylline (large doses) for
control of asthma: nervousness & tremor
In Cardiovascular :
o direct positive chronotropic
o direct enhanced myocardial contractility
Gastrointestinal Tract:
o enhanced secretion of gastric acid and digestive enzymes
o stimulates secretion (secretagogue)
Renal: weak diuretics, not therapeutically important (increased glomerular
filtration, reduced tubular sodium reabsorption)
Smooth Muscle: Major Effect in Bronchodilaton
d) Therapeutic uses (indications) :
Most effective xanthine bronchodilator
Relieves airway obstruction:
o in acute asthma and COPD
o reduces symptoms severity
e) Adverse Effects :
Particularly at higher doses, 10 mg/kg body weight/day or more, are significant
GI symptoms, nausea and vomiting are the early events
cardiac arrhythmias
seizures and even death
f) Contraindications : caution if seizure disorder, arrhythmias, pulmonary edema, cor
pulmonale, hepatic impairment, hypothyroidism, if sepsis or multi-organ failure
g) Pharmacography : tabs 100mg, 200mg, 300mg, 600mg
h) Prescription :
Dg/ COPD
Rp/ Theophylline 100mg
Nr. XXX
D.s. orally 1 tab/day after food for 30days
a) Pharmacological class : antihistaminic or Anti-asthmatic or anti-inflammatory agent
b) Mechanism of Action :
Alters function of delayed chloride channels (best demonstrated for nedocromil) and
inhibits cell activation
And has Chloride-mediated channel effects:
o inhibition of cough
o inhibition of early response to antigens from mast cells and inhibits degranulation
and release of histamine
- mast cells specific (cromolyn -minimal mediator released inhibition on
human basophils)
o inhibition of late response to antigens (eosinophils)
c) Pharmacologic effects :
o Blocks bronchoconstriction due to antigen inhalation
o Blocks aspirin-induced bronchoconstriction or bronchoconstriction induced by
environmental agents
o Reduces bronchodilators medication requirements and symptomatic severity in
patients with perennial asthma
o In chronic treatment appears to decrease the bronchial hyper-reactivity: airway
protection against inflammatory, chemical anaphylaxis mediators more effective in
reducing seasonal increases in bronchial reactivity (allergic asthma) but less
effective when compared with inhaled corticosteroids.
o Is also effective in reducing symptoms of allergic rhinitis & hay fever (allergic
condition )
d) Therapeutic uses (indications) : For the management of patients with bronchial
asthma (not acute). Also used in the treatment of Allergic rhinitis, Hayfever , vernal
keratoconjunctivitis, vernal conjunctivitis, and vernal keratitis.
e) Adverse Effects : Throat irritation, cough, mouth dryness, wheezing and chest
tightness
f) Contraindications : The drug is effective only for asthma prophylaxis, not treatment of
an acute asthma attack.
g) Pharmacography :
- Aerosol spray for inhalation: 800 mcg/spray
- Nasal solution: 40 mg/ml
- Ophthalmic solution: 4%
- Oral solution: 100 mg/5 ml
- Solution for nebulization: 10 mg/ml
h) Prescription
Dg/ Allergic Rhinitis
Rp/ Cromolyn Sodium nasal sol 40mg/ml
Nr. I
D.s. Nasally 1 time in each nostril 30 mins
before meal every 12h
a) Pharmacological class : Leukotriene receptor antagonist (LTRA)
b) Mechanism of Action : Montelukast selectively antagonizes leukotriene D4 (LTD4) at
the cysteinyl leukotriene receptor, CysLT1, in the human airway. It inhibits the actions of
LTD4at the CysLT1 receptor, preventing airway edema, smooth muscle contraction, and
enhanced secretion of thick, viscous mucus.
c) Pharmacologic effects : , Prevents airway edema, smooth muscle contraction, and
enhanced secretion of thick, viscous mucus.
d) Therapeutic uses (indications) : Used for a number of conditions including asthma
but not attacks, exercise induced bronchospasm, allergic rhinitis, and urticaria. It is
mainly used as a complementary therapy in adults in addition to inhaled corticosteroids,
if they alone do not bring the desired effect.
e) Adverse Effects : Side effects include gastrointestinal disturbances, headaches,
hypersensitivity reactions, sleep disorders, and increased bleeding tendency, in addition
to other generic adverse reactions. Its use is associated with a higher incidence of
ChurgStrauss syndrome (whether or not this drug is 'unmasking' subclinical Churg
Strauss is as yet uncertain). Drowsiness is also a common side effect.
f) Contraindications : Shouldnt be administered if feeling restless, Depression, Abnormal
Dreams, Inflammation of Blood Vessels in the Skin, Hallucination, Involuntary Quivering,
Nervous, Increased Eosinophils in the Blood, Mood Changes, Anxious, suicidal
thoughts.
g) Pharmacography :
o For adults and adolescents 15 years of age and older: one 10-mg tablet.
o For pediatric patients 6 to 14 years of age: one 5-mg chewable tablet.
o For pediatric patients 2 to 5 years of age: one 4-mg chewable tablet or one
packet of 4-mg oral granules.
h) Prescription
Dg/Chronic Asthma
Rp/Montelukast 10mg
Nr. XXX
D.s. orally 1 tab every night
a) Pharmacological class : corticosteroids, specifically glucocorticoids
b) Mechanism of Action : Binds to the glucocorticoid receptor. Unbound corticosteroids
cross the membranes of cells such as mast cells and eosinophils, binding with high
affinity to glucocorticoid receptors (GR). The results include alteration of transcription
and protein synthesis, a decreased release of leukocytic acid hydrolases, reduction in
fibroblast proliferation, prevention of macrophage accumulation at inflamed sites,
reduction of collagen deposition, interference with leukocyte adhesion to the capillary
wall, reduction of capillary membrane permeability and subsequent edema, reduction of
complement components, inhibition of histamine and kinin release, and interference with
the formation of scar tissue. In the management of asthma, the glucocorticoid receptor
complexes down-regulates pro-inflammatory mediators such as interleukin 1, 3, and 5,
and up-regulates anti-inflammatory mediators such as IkappaB [inhibitory molecule for
nuclear factor kappaB1], interleukin-10, and interleukin-12. The anti-inflammatory
actions of corticosteroids are also thought to involve inhibition of cytosolic
phospholipase A2 (through activation of lipocortin-1 (annexin)) which controls the
biosynthesis of potent mediators of inflammation such as prostaglandins and
leukotrienes.
c) Pharmacologic effects : Fluticasone is an extremely potent vasoconstrictor and antiinflammatory agent. Its effectiveness in inhaled forms is due to its direct local effect.
d) Therapeutic uses (indications) : Fluticasone propionate, a medium-potency synthetic
corticosteroid, is used topically to relieve inflammatory and pruritic symptoms of
dermatoses and psoriasis, intranasally to manage symptoms of allergic and non-allergic
rhinitis, and orally for the maintenance treatment of asthma as prophylactic therapy and
for patients requiring oral corticosteroid therapy for asthma.
e) Adverse Effects : The topical drug has been associated with burning, stinging, skin
irritation, blisters, dryness, skin infection, infected eczema, viral warts, impetigo, atopic
dermatitis, pruritus, exacerbation of pruritus, exacerbation of eczema, erythema,
and folliculitis. There are also numerous side effects associated with the oral version of
this medication including headache, stuffy or runny nose, difficulty speaking, sore or
irritated throat and painful white patches in the mouth or throat. Candidiasis of mouth
and throat is reported as a "very common" side effect. Hoarseness is also common.
Hypocortisolism (suppressed cortisol) can be expected as a result of sudden withdrawal
from fluticasone propionate.
f) Contraindications : primary treatment of status asthmaticus or other acute episodes of
asthma or COPD where intensive measures are required.
Severe hypersensitivity to milk proteins
g) Pharmacography :
o Aerosol for inhalation
o Cream for Topical use
o Powder for Respiratory (inhalation)
o Spray for nasal use
h) Prescription
Dg/ Chronic Asthma
Rp/Fluticasone propionate discus
Nr. I
D.s. Inhalatory, 1 inhalation per 12h for 1
month.
a) Pharmacological class: Synthetic Prostaglandin E
Naturally occurring prostaglandin E2 is produced by mucosal cells of the stomach and
duodenum. It inhibits gastric acid secretion and increases mucous and bicarbonate,
mucosal blood flow and mucosal repair (cytoprotective effect) With inhibition of
Prostaglandin E, erosion and ulceration of the gastric mucosa may occur
b) Mechanism of action: Misoprostol seems to inhibit gastric acid secretion by a direct
action on the parietal cells through binding to the prostaglandin receptor. The activity of
this receptor is mediated by G proteins which normally activate adenylate cyclase. The
indirect inhibition of adenylate cyclase by Misoprostol may be dependent on guanosine5-triphosphate (GTP). The significant cytoprotective actions of misoprostol are related
to several mechanisms. These include:
Increased secretion of bicarbonate,
Considerable decrease in the volume and pepsin content of the gastric
secretions,
It prevents harmful agents from disrupting the tight junctions between the
epithelial cells which stops the subsequent back diffusion of H+ ions into the
gastric mucosa,
Increased thickness of mucus layer,
Enhanced mucosal blood flow as a result of direct vasodilatation,
Stabilization of tissue lysozymes/vascular endothelium,
Improvement of mucosal regeneration capacity.
Replacement of prostaglandins that have been depleted as a result of various
insults to the area.
Misoprostol has also been shown to increase the amplitude and frequency of uterine
contractions during pregnancy via selective binding to the EP-2/EP-3 prostanoid
receptors
c) .Pharmacologic effects: Stimulates increased secretion of the protective mucus that
lines the gastrointestinal tract and increases mucosal blood flow, thereby increasing
mucosal integrity.
d) Therapeutic uses: Indicated for patients at high risk for GI ulceration and bleeding and
in those who take NSAIDs. Misoprostol is also commonly used for labor induction in
missed miscarriage.
e) Adverse effects: Diarrhea, abdominal pain, fever, nausea, flatulence, headache,
dyspepsia, vomiting, and constipation.
f) Contraindications: Misoprostol should not be taken by pregnant women to reduce the
risk of NSAID induced gastric ulcers because it increases uterine tone and contractions
in pregnancy, which may cause partial or complete abortions, and because its use in
pregnancy has been associated with birth defects.
g) Pharmacography: tabs 50 mcg, 100mcg, 200mcg
h) Prescription :
Dg/Ulcer prophylaxis
Rp/ Misoprostol 100mcg
Nr.XXX
D.s.Orally, 1 tabl every 8h for 10 days
a) Pharmacological class: Nitrate
b) Mechanism of action: Nitroglycerin is converted to nitric oxide (NO), an active
intermediate compound which activates the enzyme guanylate cyclase. This stimulates
the synthesis of cyclic guanosine 3',5'-monophosphate (cGMP) which then activates a
series of protein kinase-dependent phosphorylations in the smooth muscle cells,
eventually resulting in the dephosphorylation of the myosin light chain of the smooth
muscle fiber. The subsequent release of calcium ions results in the relaxation of the
smooth muscle cells and vasodilation.
c) Pharmacologic effects: Nitrates decrease coronary vasoconstriction or spasm and
increase perfusion of the myocardium by relaxing coronary arteries. In addition, they
relax veins, decreasing preload and myocardial oxygen consumption.
d) Therapeutic uses: Nitroglycerin is used in the treatment of angina pectoris and
perioperative hypertension, to produce controlled hypotension during surgical
procedures, to treat hypertensive emergencies, and to treat congestive heart failure
associated with myocardial infarction.
e) Adverse effects: Tolerance, Flushing and can cause severe headaches, severe
hypotension, bradycardia and syncope.
f) Contraindications: It must not be used together with vasodilators that combat erectile
dysfunction, such as Viagra, Cialis, or Levitra. The combination of the two can lead to
severe hypotension, circulatory collapse and death.
g) Pharmacography:
Caps: 2.5mg, 6.5mg, 9mg
Injectable: 0.5-5mg/ml
Sublingual: 0.5mg
h) Prescription :
Dg/ Angina
Rp/ Nitroglycerin, tab 0,5 mg
Nr. V
Ds. Sublingually, 1 tab when necessary
a) Pharmacological class: Calcium Channel Blockers
b) Mechanism of action: The intracellular concentration of calcium plays an important role
in maintaining the tone of smooth muscle and in the contraction of the myocardium.
Calcium enters muscle cells through special voltage-sensitive calcium channels. This
triggers release of calcium from the sarcoplasmic reticulum and mitochondria, which
further increases the cytosolic level of calcium. Calcium-channel antagonists block the
inward movement of calcium by binding to L-type calcium channels in the heart and in
smooth muscle of the coronary and peripheral vasculature.
c) Pharmacologic effects: Vascular smooth muscle relaxation and dilation mainly of
arterioles.
d) Therapeutic uses: Calcium-channel blockers have an intrinsic natriuretic effect and,
therefore, do not usually require the addition of a diuretic. These agents are useful in the
treatment of hypertensive patients who also have asthma, diabetes, angina, and/or
peripheral vascular disease ( Black hypertensives respond well to calcium-channel
blockers).
e) Adverse effects: Tachycardia, Flushing, Hypotension
f) Contraindications: Not to be administered in sick sinus syndrome, heart block (second
and third degree), lactation. Use cautiously with pregnancy, impaired hepatic function.
g) Pharmacography:
Tablets: 10mg, 5mg, 2.5mg
h) Prescription :
Dg/ Hypertension
Rp/ Felodipine 10 mg
Nr. XXX
DS: Orally, 1 tablet per day at breakfast,
for 1 month
a) Pharmacological class: calcium channel blocker - Benzothiazepines
b) Mechanism of action: Possibly by deforming the channel, inhibiting ion-control gating
mechanisms, and/or interfering with the release of calcium from the sarcoplasmic
reticulum, diltiazem, like verapamil, inhibits the influx of extracellular calcium across both
the myocardial and vascular smooth muscle cell membranes. The resultant inhibition of
the contractile processes of the myocardial smooth muscle cells leads to dilation of the
coronary and systemic arteries and improved oxygen delivery to the myocardial tissue.
c) Pharmacologic effects: Dilation of the coronary and systemic arteries and improved
oxygen delivery to the myocardial tissue.
d) Therapeutic uses: Used in the treatment of hypertension, angina pectoris, and some
types of arrhythmia, supraventricular tachycardia.
e) Adverse effects: hypotension, bradycardia, dizziness, and flushing.
f) Contraindications: In congestive heart failure, in SA node or AV conduction
disturbances, in low blood pressure patients with systolic blood pressures below 90 mm
Hg. It also may paradoxically increase ventricular rate in patients with Wolff-ParkinsonWhite syndrome because of accessory conduction pathways. Diltiazem is relatively
contraindicated in the presence of sick sinus syndrome, bradycardia, impaired left
ventricle function, peripheral artery occlusive disease, and chronic obstructive
pulmonary disease.
g) Pharmacography:
Caps: 120mg, 180mg, 240mg, 300mg
Tablets: 30mg, 60mg, 90mg, 120mg, 180mg, 240mg, 300mg
Injection IV
h) Prescription :
Dg/ Hypertension
Rp/ Diltiazem tab 90mg
Nr LX
Ds. Orally, 1 tab per 12h for 30 days
a) Pharmacological class: calcium channel blocker - Diphenylalkylamines
b) Mechanism of action: The intracellular concentration of calcium plays an important role
in maintaining the tone of smooth muscle and in the contraction of the myocardium.
Calcium enters muscle cells through special voltage-sensitive calcium channels. This
triggers release of calcium from the sarcoplasmic reticulum and mitochondria, which
further increases the cytosolic level of calcium. Calcium-channel antagonists block the
inward movement of calcium by binding to L-type calcium channels in the heart and in
smooth muscle of the coronary and peripheral vasculature. Since calcium channels are
especially concentrated in the sinoatrial and atrio-ventricular nodes, these agents can
be used to decrease impulse conduction through the AV node, thus protecting the
ventricles from atrial tachyarrhythmias. Calcium channels are also present in the smooth
muscle that lines blood vessels. By relaxing the tone of this smooth muscle, calciumchannel blockers dilate the blood vessels. This has led to their use in treating
hypertension and angina pectoris.
c) Pharmacologic effects: Verapamil is the least selective of any calcium-channel blocker
and has significant effects on both cardiac and vascular smooth muscle cells and
causes smooth muscle to relax, dilation mainly of arterioles.
d) Therapeutic uses: It is used to treat angina, supraventricular tachyarrhythmias, and
migraine headache. is also used intra-arterially to treat cerebral vasospasm.
e) Adverse effects: Some possible side effects of the drug are bradycardia, hypotension,
AV block, heart failure, headaches, facial flushing, dizziness, lightheadedness, swelling,
increased urination, fatigue, nausea, ecchymosis, galactorrhea, and constipation.
f) Contraindications: Verapamil should be avoided in patients with congestive heart
failure ,with atrioventricular block due to its negative inotropic (force of cardiac muscle
contraction) and dromotropic (velocity of conduction) effects and in vasospamic angina.
g) Pharmacography:
Tablets: 40mg 80mg 120mg
24h Capsules : 100mg 120mg 180mg 200mg - 240 mg 300mg 360mg
h) Prescription :
Dg/Hypertension
Rp/ Verapamil cap 120mg
Nr XXX
Ds. Orally, 1 tab per 24h
a) Pharmacological class: Selective 1 blocker
b) Mechanism of action: Drug, that preferentially blocks the beta-1 receptors, developed
to eliminate the unwanted bronchoconstrictor effect (beta-2 effect) of propranolol seen
among asthmatic patients. Cardioselective beta-blocker antagonizes beta-1 receptors,
at doses 50- to 100-fold less than those required to block beta-2 receptors, inhibiting
sympathetic stimulation. This cardioselectivity is thus most pronounced at low doses
and is lost at high doses.
c) Pharmacologic effects: Reduction in resting heart rate, cardiac output, systolic and
diastolic blood pressure, and reflex orthostatic hypotension.
d) Therapeutic uses: For the management of acute myocardial infarction, angina pectoris,
heart failure and mild to moderate hypertension. May be used to treat supraventricular
and tachyarrhythmias and as prophylaxis for migraine headaches.
e) Adverse effects: Dizziness, drowsiness, fatigue, diarrhea, unusual dreams, ataxia,
trouble sleeping, depression, and vision problems. It may also reduce blood flow to the
hands and feet, causing them to feel numb and cold. Due to the high penetration across
the blood brain barrier, lipophilic beta blockers such metoprolol are more likely than
other less lipophilic beta blockers to cause sleep disturbances such as insomnia and
vivid dreams and nightmares. Other possible effects are sexual dysfunction, erectile
dysfunction (impotence), hair loss, mental/mood changes, depression, dyspnea, cough,
dyslipidemia and polydipsia.
f) Contraindications: Metoprolol is contraindicated in patients with bradycardia < 45
beats/min, second and third degree heart block, significant first degree heart block (P-R
interval 0.24 sec) and systolic blood pressure < 100 mmHg; or moderate-to-severe
cardiac failure.
g) Pharmacography:
IV vials : 1mg/ml
Tablets: 25mg 50mg 100mg 200mg
h) Prescription :
Dg/Hypertension
Rp/Metoprolol, tabl 50mg
Nr.XXX
D.s. Orally, 1 tabl/day for 30 days
a) Pharmacological class: Selective 1 blocker
b) Mechanism of action: Bisoprolol selectively blocks catecholamine stimulation of 1adrenergic receptors in the heart and vascular smooth muscle.This results in a reduction
of heart rate, cardiac output, systolic and diastolic blood pressure, and possibly reflex
orthostatic hypotension. At higher doses (e.g. 20 mg and greater) bisoprolol may
competitively block 2-adrenergic receptors in bronchial and vascular smooth muscle
causing bronchospasm and vasodilation. . In addition, 1-selective blockers prevent the
release of renin, a hormone produced by the kidneys that cause constriction of blood
vessels.
c) Pharmacologic effects: Activation of 1-receptors (located mainly in the heart) by
epinephrine increases heart rate and the blood pressure causing the heart to consume
more oxygen. 1-adrenergic blocking agents such as bisopolol lower the heart rate and
blood pressure and may be used to reduce workload on the heart and hence oxygen
demands. They are routinely prescribed in patients with ischemic heart disease.
d) Therapeutic uses: Used to treat cardiovascular diseases such as hypertension,
coronary heart disease, arrhythmias, ischemic heart diseases and treatment of
myocardial infarction after the acute event. Patients with compensated congestive heart
failure may be treated with bisoprolol as a comedication (usually together with an ACE
inhibitor, a diuretic and a digitalis-glycosid, if indicated). In patients with congestive heart
failure, it reduces the need for and the consumption of oxygen of the heart muscle. It is
very important to start with low doses, as bisoprolol reduces also the muscular power of
the heart, which is an undesired effect in congestive heart failure.
e) Adverse effects: Fatigue, hypotension, low blood sugar, bronchospasms and
bradycardia. Bronchospasms and low blood sugar because at high doses drug can be
an antagonist for 2 adrenergic receptors located in lung and in liver. Bronchspasm due
to blockage in lungs of 2 receptor and low blood sugar because of decreased
stimulation of glycogenolysis and gluconeogenesis in the liver via 2 receptor.
f) Contraindications: Beta-blockers can precipitate asthma and this effect can be
dangerous. They should be avoided in patients with a history of asthma or
bronchospasm.
g) Pharmacography:
Tablets combined with diuretics : Bisoprolol-Hydrochlorothiazide 2.5 or 5 or 10-6.25 mg
Tablets: 5mg 10mg
h) Prescription :
Dg/Hypertension
Rp/Bisoprolol-Hydrochlorothiazide, tab 5-6.25 mg
Nr.XXX
D.s. Orally, 1 tabl/day for 30 days
a) Pharmacological class: Angiotensin-converting enzyme (ACE)
b) Mechanism of action: Captopril, one of the few ACE inhibitors that is not a prodrug,
competes with ATI (Angiotensin) for binding to ACE and inhibits and enzymatic
proteolysis of ATI to ATII. Decreasing ATII levels in the body decreases blood pressure
by inhibiting the pressor effects of ATII. Captopril also causes an increase in plasma
renin activity likely due to a loss of feedback inhibition mediated by ATII on the release
of renin and/or stimulation of reflex mechanisms via baroreceptors. Captoprils affinity for
ACE is approximately 30,000 times greater than that of ATI.
c) Pharmacologic effects: Captopril, an ACE inhibitor, antagonizes the effect of the
RAAS. ACE inhibitors inhibit the rapid conversion of ATI to ATII and antagonize RAASinduced increases in blood pressure. ACE (also known as kininase II) is also involved in
the enzymatic deactivation of bradykinin, a vasodilator. Inhibiting the deactivation of
bradykinin increases bradykinin levels and may sustain its effects by causing increased
vasodilation and decreased blood pressure.{ PHYSIOLOGY : The RAAS is a homeostatic
mechanism for regulating hemodynamics, water and electrolyte balance. During sympathetic
stimulation or when renal blood pressure or blood flow is reduced, renin is released from the
granular cells of the juxtaglomerular apparatus in the kidneys. In the blood stream, renin cleaves
circulating angiotensinogen to ATI, which is subsequently cleaved to ATII by ACE. ATII increases
blood pressure using a number of mechanisms. First, it stimulates the secretion of aldosterone
from the adrenal cortex. Aldosterone travels to the distal convoluted tubule (DCT) and collecting
tubule of nephrons where it increases sodium and water reabsorption by increasing the number
of sodium channels and sodium-potassium ATPases on cell membranes. Second, ATII
stimulates the secretion of vasopressin (also known as antidiuretic hormone or ADH) from the
posterior pituitary gland. ADH stimulates further water reabsorption from the kidneys via
insertion of aquaporin-2 channels on the apical surface of cells of the DCT and collecting
tubules. Third, ATII increases blood pressure through direct arterial vasoconstriction. Stimulation
of the Type 1 ATII receptor on vascular smooth muscle cells leads to a cascade of events
resulting in myocyte contraction and vasoconstriction. In addition to these major effects, ATII
induces the thirst response via stimulation of hypothalamic neurons.}
d) Therapeutic uses: For the treatment of essential or renovascular hypertension (usually
administered with other drugs, particularly thiazide diuretics). May be used to treat
congestive heart failure in combination with other drugs (e.g. cardiac glycosides,
diuretics, -adrenergic blockers). May improve survival in patients with left ventricular
dysfunction following myocardial infarction. May be used to treat nephropathy, including
diabetic nephropathy.
e) Adverse effects: These include postural hypotension, renal insufficiency, hyperkalemia,
angioedema, and a persistent dry cough. The potential for symptomatic hypotension
with ACE inhibitor therapy requires careful monitoring.
f) Contraindications: ACE inhibitors should not be used in pregnant women, because
they are fetotoxic. Anaphylactoid reaction is plausible.
g) Pharmacography:
Tablets: 12.5mg 25mg 50mg 100mg
h) Prescription :
Dg/Hypertension
Rp/Captopril, tab 50 mg
Nr.XXX
D.s. Orally, 1 tabl/day for 30 days
a) Pharmacological class: Angiotensin II-receptor blocker (ARB)
b) Mechanism of action: Valsartan is an ARB that selectively inhibits the binding of
angiotensin II to AT I, which is found in many tissues such as vascular smooth muscle
and the adrenal glands. This effectively inhibits the ATI-mediated vasoconstrictive and
aldosterone-secreting effects of angiotensin II and results in a decrease in vascular
resistance and blood pressure. Valsartan is selective for AT and has virtually no affinity
for ATII. Inhibition of aldosterone secretion may inhibit sodium and water reabsorption in
the kidneys while decreasing potassium excretion.
c)
Pharmacologic effects: All the ARBs are approved for treatment of hypertension based
on their clinical efficacy in lowering blood pressure and reducing the morbidity and
mortality associated with hypertension. Their use in HF is as a substitute for ACE
inhibitors in those patients with severe cough or angioedema.
d) Therapeutic uses: May be used as a first line agent to treat uncomplicated
hypertension, isolated systolic hypertension and left ventricular hypertrophy. May be
used as a first line agent to delay progression of diabetic nephropathy. Losartan may be
also used as a second line agent in the treatment of congestive heart failure, systolic
dysfunction, myocardial infarction and coronary artery disease in those intolerant of ACE
inhibitors.
e) Adverse effects: Headache and dizziness and sometimes fatigue.
f) Contraindications: ACE inhibitors should not be used in pregnant women, because
they are fetotoxic.
g) Pharmacography:
Caps: 40 mg, 80 mg, or 160 mg
Tablets: 40 mg , 80 mg, 160 mg, or 320 mg. Usual dosage from 40320 mg daily.
Tablets combined with diuretics: (valsartan/HCTZ mg) 80 or 160 or 320/12.5 mg and
160 or 320/25 mg.
h) Prescription :
Dg/Hypertension
Rp/Valsartanl, tab 160 mg
Nr.XXX
D.s. Orally, 1 tab/day for 30 days
Вам также может понравиться
- Antpyretic-Analgesic and Antinlammatory DrugsДокумент38 страницAntpyretic-Analgesic and Antinlammatory DrugskasondaОценок пока нет
- Antipyretic-Analgesic and Antiinflammatory Drugs: Department of Pharmacology Zhang Yan-MeiДокумент39 страницAntipyretic-Analgesic and Antiinflammatory Drugs: Department of Pharmacology Zhang Yan-MeiIshu SethiОценок пока нет
- Anti Inflamatory Drugs AINSДокумент39 страницAnti Inflamatory Drugs AINSEl FaroukОценок пока нет
- Antipyretic-Analgesic and Antiinflammatory DrugsДокумент46 страницAntipyretic-Analgesic and Antiinflammatory DrugsAYU SUKARNI PUTRIОценок пока нет
- NSAIDSДокумент38 страницNSAIDSShahmir KhanОценок пока нет
- Analgesics: Non-Steroidal Anti-Inflammatory Drugs andДокумент8 страницAnalgesics: Non-Steroidal Anti-Inflammatory Drugs andWilliam C ChishaОценок пока нет
- NSAID Mechanism and UsesДокумент11 страницNSAID Mechanism and UsesSuranjan GhoshОценок пока нет
- Anti Pyretic 2013Документ15 страницAnti Pyretic 2013Faizah Al GhamdiОценок пока нет
- NSAIDs: Mechanisms, Effects and UsesДокумент43 страницыNSAIDs: Mechanisms, Effects and UsesRitu ShewaniОценок пока нет
- Kharkov National Medical University Department of Pharmacology Lecture on Anti-inflammatory DrugsДокумент82 страницыKharkov National Medical University Department of Pharmacology Lecture on Anti-inflammatory DrugsHerry HendrayadiОценок пока нет
- 3 Analgesic Anitpyretic InfamДокумент10 страниц3 Analgesic Anitpyretic InfamAnonymous dRAu54Оценок пока нет
- Guide to NSAIDs (Non-Steroidal Anti-Inflammatory DrugsДокумент40 страницGuide to NSAIDs (Non-Steroidal Anti-Inflammatory DrugsHarini Bala100% (1)
- Cefradime, Paracetamol, KetorolacДокумент10 страницCefradime, Paracetamol, KetorolacMae_Sheryn_Lip_1795Оценок пока нет
- PAIN ControllersДокумент39 страницPAIN ControllersAyro Business CenterОценок пока нет
- Week 9 - Course Task - Case Analysis Renal DisordersДокумент4 страницыWeek 9 - Course Task - Case Analysis Renal DisordersJohnmarkLorenzanaRoveroОценок пока нет
- Anti-Inflammatory Drugs Class Notes 2023Документ82 страницыAnti-Inflammatory Drugs Class Notes 2023Jacob MasikaОценок пока нет
- Treatment of Acute GoutДокумент38 страницTreatment of Acute GoutAnoop PkОценок пока нет
- Bp1 Sgd1: TopicsДокумент7 страницBp1 Sgd1: TopicsAlan Joseph BaldovinoОценок пока нет
- NSAIDsДокумент12 страницNSAIDsjelly100% (1)
- Drug Study Effects and UsesДокумент11 страницDrug Study Effects and UsesVincent QuitorianoОценок пока нет
- Drug 25Документ17 страницDrug 25carol_gigliotti24100% (1)
- Penyakit Tersering Di PuskesmasДокумент5 страницPenyakit Tersering Di PuskesmasRama Al MaduriОценок пока нет
- pharamcology unit 10 answersДокумент13 страницpharamcology unit 10 answersLovren YoungОценок пока нет
- Relieve Angina & Congestive Heart FailureДокумент6 страницRelieve Angina & Congestive Heart FailureBij Hilario100% (1)
- Nursing Drug CardsДокумент32 страницыNursing Drug CardsJenna Rasmussen100% (3)
- NSAIDsДокумент34 страницыNSAIDsAliImadAlKhasaki75% (4)
- Anti Inflammatory DrugsДокумент82 страницыAnti Inflammatory DrugsShardendu MishraОценок пока нет
- Respiratory Tract PharmacologyДокумент68 страницRespiratory Tract PharmacologyRohaan SharmaОценок пока нет
- Prostaglandins and NSAIDs in InflammationДокумент21 страницаProstaglandins and NSAIDs in InflammationAmr SalemОценок пока нет
- NSADs: Non-Steroidal Anti-Inflammatory DrugsДокумент26 страницNSADs: Non-Steroidal Anti-Inflammatory DrugsSai Kishore K100% (1)
- B-Selective: I Group: Nonsteroidal Anti-Inflammatory Drugs (Nonsteroidal Ntiinflammatory)Документ6 страницB-Selective: I Group: Nonsteroidal Anti-Inflammatory Drugs (Nonsteroidal Ntiinflammatory)Moataz TrabehОценок пока нет
- Clinical Toxicology: Dep. of Biopharmaceutics and Clinical PharmacyДокумент32 страницыClinical Toxicology: Dep. of Biopharmaceutics and Clinical Pharmacymalak amerОценок пока нет
- Drug StudyДокумент19 страницDrug StudyCalimlim KimОценок пока нет
- NSAIDS 3, 4 SummaryДокумент29 страницNSAIDS 3, 4 SummaryAhmed ExaminationОценок пока нет
- Nsaids Nonsteroidal Anti-Inflammatory Drugs: Maher Khdour Msc. Phd. Clinical PharmacyДокумент65 страницNsaids Nonsteroidal Anti-Inflammatory Drugs: Maher Khdour Msc. Phd. Clinical PharmacyYousef JafarОценок пока нет
- GOUT PresentationДокумент24 страницыGOUT Presentationtasneemsofi100% (1)
- Analgesics: DR Mohammed Malik AfrozДокумент37 страницAnalgesics: DR Mohammed Malik AfrozMohee DawabshehОценок пока нет
- Lec9 د ذو الفقارДокумент4 страницыLec9 د ذو الفقارMohammed JaberОценок пока нет
- Drug StudyДокумент8 страницDrug StudyMike Faustino SolangonОценок пока нет
- Drug Study Gentamicin Sulfate and SalbutamolДокумент7 страницDrug Study Gentamicin Sulfate and SalbutamolEduardОценок пока нет
- Drug and NCPДокумент15 страницDrug and NCPgeelawlietОценок пока нет
- Drug Study CompilationДокумент9 страницDrug Study CompilationRene John FranciscoОценок пока нет
- NSAIDs: Non-steroidal Anti-inflammatory DrugsДокумент45 страницNSAIDs: Non-steroidal Anti-inflammatory DrugsArvi KhanОценок пока нет
- Nonsteroidal Antiinflammatory Drugs and Antipyretic - AnalgesicsДокумент28 страницNonsteroidal Antiinflammatory Drugs and Antipyretic - AnalgesicsJasveen SawhneyОценок пока нет
- Pharmacology of Adrenocorticoids and Adrenocorticotropic AntagonistsДокумент32 страницыPharmacology of Adrenocorticoids and Adrenocorticotropic AntagonistsJoyce VillanuevaОценок пока нет
- DrugsДокумент2 страницыDrugsgailannreyesОценок пока нет
- DrugsДокумент2 страницыDrugsgailannreyesОценок пока нет
- Kuliah Gouty ArthritisДокумент56 страницKuliah Gouty Arthritischrysandre100% (1)
- E Kart DrugsДокумент3 страницыE Kart DrugsNichole CastleОценок пока нет
- Drug StudyДокумент11 страницDrug StudyKaloy KamaoОценок пока нет
- Drug StudiesДокумент16 страницDrug Studiesvitcloud23100% (2)
- Celecoxib uses, dosage, side effectsДокумент4 страницыCelecoxib uses, dosage, side effectsAbigail LonoganОценок пока нет
- Drug Study OrthoДокумент6 страницDrug Study OrthoKrisia CastucianoОценок пока нет
- Pharm Chapter's Focus Review 2Документ16 страницPharm Chapter's Focus Review 2Briana SmetОценок пока нет
- Drug Study No.1 Brand Name: Paracetamol Generic Name: Tempra Classification: Anti-Infectives Dosage: 100mg, 1ml Drops q4hrДокумент7 страницDrug Study No.1 Brand Name: Paracetamol Generic Name: Tempra Classification: Anti-Infectives Dosage: 100mg, 1ml Drops q4hrMary EnsomoОценок пока нет
- Individual NSAIDs Mechanisms and UsesДокумент4 страницыIndividual NSAIDs Mechanisms and UsesJsnanbjrihОценок пока нет
- Bronchial Asthma 2.0Документ15 страницBronchial Asthma 2.0Bisweswar OjhaОценок пока нет
- NSAIDs, DMARDs, Analgesics & Gout DrugsДокумент114 страницNSAIDs, DMARDs, Analgesics & Gout DrugsMani Jee100% (1)
- Solu-Cortef (Hydrocortisone)Документ3 страницыSolu-Cortef (Hydrocortisone)E100% (2)
- Medical Pharmacology Ovidius 2014 1st TestДокумент19 страницMedical Pharmacology Ovidius 2014 1st TestWissam DadiОценок пока нет
- Immunology 1Документ10 страницImmunology 1Elena DalcaranОценок пока нет
- Genetics Labs 1Документ28 страницGenetics Labs 1Wissam DadiОценок пока нет
- Basic Surgical InstrumentsДокумент37 страницBasic Surgical Instrumentsapi-2658787991% (33)
- Datasheet PLASBLAK PE4637pdfДокумент2 страницыDatasheet PLASBLAK PE4637pdfGodesPow. Jose L. Godes: Entrenamiento con potenciaОценок пока нет
- Enzyme Assay Units: Amylase Units Lactase UnitsДокумент4 страницыEnzyme Assay Units: Amylase Units Lactase UnitsDaniel RincónОценок пока нет
- Hardness Desalination1Документ18 страницHardness Desalination1Swati U NaikОценок пока нет
- Rubber Property-Abrasion Resistance (Rotary Drum Abrader) : Standard Test Method ForДокумент9 страницRubber Property-Abrasion Resistance (Rotary Drum Abrader) : Standard Test Method Formohammed karasnehОценок пока нет
- Dungs ATEX en 161 Solenoid ValvesДокумент12 страницDungs ATEX en 161 Solenoid Valvesstefan-romocki-4927Оценок пока нет
- Group II Cation AnalysisДокумент4 страницыGroup II Cation AnalysisClare CaspeОценок пока нет
- Objectives Identify The Two Main Classes of Vitamins. List Seven Minerals Your Body Needs inДокумент28 страницObjectives Identify The Two Main Classes of Vitamins. List Seven Minerals Your Body Needs inyosysilalahiОценок пока нет
- Heat Transfer Study GuideДокумент6 страницHeat Transfer Study GuideCarlosCD17100% (1)
- Experiment 5Документ30 страницExperiment 5Mags CabelinОценок пока нет
- Thermal Conductivity Meter: Guarded Heat Flow Test MethodДокумент2 страницыThermal Conductivity Meter: Guarded Heat Flow Test Methodrajesh_rbpОценок пока нет
- Laboratory Manual Machine Shop 1 PDFДокумент59 страницLaboratory Manual Machine Shop 1 PDFVinz Bryan AlmacenОценок пока нет
- Lecture 1 Pendahuluan BiokatalisДокумент18 страницLecture 1 Pendahuluan BiokatalisSabar SitioОценок пока нет
- AAMA Vs Qualicoat 2018Документ12 страницAAMA Vs Qualicoat 2018viet nguyen cao0% (1)
- CentrifugationДокумент12 страницCentrifugationVytheeshwaran Vedagiri100% (16)
- Salt HydrolysisДокумент3 страницыSalt Hydrolysisna_napanda100% (1)
- Indirect RestorationsДокумент32 страницыIndirect RestorationsNaji Z. Arandi100% (1)
- Review of Literature on Aloe Vera and Hand SanitizersДокумент4 страницыReview of Literature on Aloe Vera and Hand SanitizersRamОценок пока нет
- Membrane Technology: Reverse Osmosis Ultrafiltration MicrofiltrationДокумент66 страницMembrane Technology: Reverse Osmosis Ultrafiltration MicrofiltrationShivani MunishwarОценок пока нет
- Final PG Sby 0024Документ3 страницыFinal PG Sby 0024Afwa Wildan RomadhonОценок пока нет
- Multirae Lite: Wireless Portable Multi-Gas MonitorДокумент2 страницыMultirae Lite: Wireless Portable Multi-Gas MonitorAnticristh6666Оценок пока нет
- Karbohidrat: Dyke Gita Wirasisya, S.Farm., M.SC., Apt Program Studi Farmasi, Fakultas Kedokteran, Universitas MataramДокумент37 страницKarbohidrat: Dyke Gita Wirasisya, S.Farm., M.SC., Apt Program Studi Farmasi, Fakultas Kedokteran, Universitas Matarambrahmani ptrОценок пока нет
- Acid BassДокумент41 страницаAcid BassRobert Edwards100% (1)
- 1 s2.0 S1319610311002407 MainДокумент14 страниц1 s2.0 S1319610311002407 Mainspanu oanaОценок пока нет
- Experiment 4 (Hydrates)Документ3 страницыExperiment 4 (Hydrates)Zaharahni Md SehatОценок пока нет
- Saudi Aramco Test Report: Internal Tank Bottom Testing 30-Oct-17 CP-SATR-X-3205Документ8 страницSaudi Aramco Test Report: Internal Tank Bottom Testing 30-Oct-17 CP-SATR-X-3205Tayyab AchakzaiОценок пока нет
- (Unit 1&2) PDFДокумент41 страница(Unit 1&2) PDFJaiPrakashОценок пока нет
- Evaluation of Steam Jet EjectorsДокумент11 страницEvaluation of Steam Jet EjectorsRajeh Somrani100% (3)
- Alimentos Funcionais em UanДокумент12 страницAlimentos Funcionais em UanEduardo MartinsОценок пока нет
- Who Took Jerell'S Ipod? - An Organic: Compound MysteryДокумент8 страницWho Took Jerell'S Ipod? - An Organic: Compound Mysteryakm1187Оценок пока нет
- 2010 Proportional CatalogДокумент16 страниц2010 Proportional CatalogjondesousaОценок пока нет