Академический Документы
Профессиональный Документы
Культура Документы
A Review of Adapalene in The Treatment of Acne Vulgaris
Загружено:
jparanotiОригинальное название
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
A Review of Adapalene in The Treatment of Acne Vulgaris
Загружено:
jparanotiАвторское право:
Доступные форматы
Journal of Adolescent Health 43 (2008) 421 424
Review article
A Review of Adapalene in the Treatment of Acne Vulgaris
Cynthia E. Irby, B.A.a, Brad A. Yentzer, M.D.a, and Steven R. Feldman, M.D., Ph.D.a,b,c,*
b
a
Department of Dermatology, Center for Dermatology Research, Wake Forest University School of Medicine; Winston-Salem, North Carolina
Department of Public Health Sciences, Center for Dermatology Research, Wake Forest University School of Medicine; Winston-Salem, North Carolina
c
Department of Pathology, Center for Dermatology Research, Wake Forest University School of Medicine; Winston-Salem, North Carolina
Manuscript received January 7, 2008; manuscript accepted June 9, 2008
Abstract
Topical retinoids help address the early lesions of acne vulgaris. Consensus guidelines advocate the
use of topical retinoids as the primary treatment for most forms of acne vulgaris. However, all
topical retinoid preparations may be irritating, and this may contribute to underutilization in clinical
practices. Topical adapalene fosters topical retinoid treatment of acne with less irritation. Adapalene
is a more stable molecule than tretinoin. Adapalene can be used without concern for photodeactivation. Because of its chemical stability, adapalene can be used in combination with benzoyl
peroxide products. The availability of a stable topical retinoid associated with little irritation may
facilitate meeting acne treatment consensus guidelines. 2008 Society for Adolescent Medicine.
All rights reserved.
Keywords:
Topical retinoids; Tretinoin; Comedolytic; Anti-inflammatory; Pediatricians
The pathophysiology of acne involves four key mechanisms of action: abnormal proliferation and differentiation of
keratinocytes, increased sebum production, hyperproliferation
of Propionibacterium acnes, and an inflammatory response
initiated by bacterial antigens and cytokines. Topical retinoids
target the abnormal proliferation and differentiation of keratinocytes and also have anti-inflammatory effects. In addition,
topical retinoids enhance penetration of other agents, such as
topical antibiotics, resulting in synergistic effects [13].
Retinoids used for acne therapy include tretinoin, tazarotene, adapalene, and isotretinoin (systemic). Topical retinoids are comedolytic and are successful at inhibiting the
formation of micro-comedones, the precursor to all acne
lesions. The first-generation retinoids (retinol, tretinoin, and
isotretinoin) are irritating, and may limit compliance. AdaPotential conflicts of interest: Dr. Feldman has received research,
speaking and/or consulting support from several manufacturers of topical
retinoids including Galderma, OrthoNeutrogena, and Stiefel. The Center
for Dermatology Research is supported by an educational grant from
Galderma Laboratories, L.P. Dr. Yentzer and Ms. Irby have no conflicts to
disclose.
*Address correspondence to: Steven R. Feldman, M.D., Ph.D., Department of Dermatology, Wake Forest University School of Medicine, Medical Center Boulevard, Winston-Salem, NC 27157-1071.
E-mail address: sfeldman@wfubmc.edu
palene is a third generation retinoid with minimal side
effects. Adapalene has become widely used because of its
comparable efficacy and favorable tolerability profile when
compared with other topical retinoids [2,3].
Adapalene for Treatment of Acne Vulgaris
Indications and use
Adapalene is available in two formulations: gel (.1%,
.3%) and cream (.1%). After washing with a gentle cleanser,
a thin layer should be applied once daily in the evening to
the entire face and any other affected area approved by the
physician [4]. Special care should be taken to avoid the
eyes, lips, mucous membranes, and other sensitive areas [4].
As retinoids may increase photosensitivity, patients should
be instructed to minimize sun exposure and to apply a
noncomedogenic sunscreen every morning. The safety and
efficacy in children 12 years of age have not been determined [5]. Adapalene is pregnancy category C and should
be used with caution in pregnant women.
Description and clinical pharmacology
Adapalenes chemical structure is more stable to light
and oxidation compared with tretinoin. In an in vitro
1054-139X/08/$ see front matter 2008 Society for Adolescent Medicine. All rights reserved.
doi:10.1016/j.jadohealth.2008.06.005
422
C.E. Irby et al. / Journal of Adolescent Health 43 (2008) 421 424
study of adapalene and tretinoin, 95% of tretinoin was
degraded within 24 hours in the presence of sunlight and
benzoyl peroxide, whereas adapalene had essentially no
degradation under these conditions, even at 72 hours
[3,6]. Unlike generic tretinoin gel, adapalene is formulated in an aqueous gel, which may account for some of
the improved tolerability. However, adapalene is also
better tolerated than other formulations of tretinoin
(cream and microsphere gel) [7].
A proposed mechanism for adapalenes greater tolerability is its selective binding affinity. Unlike tretinoin, adapalene does not bind to the cytosolic retinoic acid binding
proteins but instead selectively binds to the nuclear retinoic
acid receptor (RAR) subtypes and [3,8]. This selective
binding affinity may play a role in adapalenes greater
inhibition of keratinocyte differentiation than tretinoin,
which was demonstrated in a study using keratinocyte transglutaminase expression as a marker [3]. This inhibition of
keratinocyte differentiation and proliferation is responsible
for adapalenes comedolytic effect. In an in vivo study,
adapalenes ability to reduce comedone formation was demonstrated by a 50 60% reduction in comedone counts compared with vehicle [9].
Another important factor in acne pathogenesis is the
inflammation that occurs after microcomedone formation.
Adapalene inhibits the inflammatory response to microcomedone formation and bacterial antigens [1,2]. Adapalenes anti-inflammatory effects result from inhibition of
neutrophil chemotaxis and the lipoxygenase pathyway, both
of which are associated with cutaneous inflammatory reactions [2,8]. Adapalene is more effective at inhibiting neutrophil lipoxygenase than is tretinoin [2,8]. Adapalene also
has other unique anti-inflammatory mechanisms that may
contribute to its efficacy [8].
Clinical Studies of Adapalene
Clinical efficacy
Adapalene is an effective acne treatment. A multicenter,
randomized, investigator-blinded study with 297 enrolled
patients compared the efficacy of adapalene .1% solution to
that of tretinoin .025% gel in a once-daily dosage regimen
for 12 weeks. Both agents provided significant mean improvements in inflammatory lesions (47% and 50%, respectively), and noninflammatory lesions (57% and 54%) [10].
In another multicenter, randomized, investigator-blinded
study, 105 patients with mild to moderate acne vulgaris
were treated with adapalene .1% gel versus tretinoin .025%
gel for 3 months. Adapalene gel was found to be more
efficacious than tretinoin gel after 1 week of treatment, with
respect to a decrease in inflammatory lesions (32% and
17%, respectively, p .001) and total lesion counts (28%
and 22%, p .042); however there was no statistically
significant difference at week 12 [11].
Another 12-week study compared adapalene .1% gel to
tretinoin .1% microsphere. At week 4, a greater reduction in
non-inflammatory lesions was observed for the tretinoin
.1% microsphere; however the tretinoin group also had a
greater incidence of skin irritation. Both products had similar efficacies (33% vs. 35% mean total lesion reduction) by
week 12 [12].
A new formulation of adapalene in a .3% gel is now
available and is even more effective than its .1% predecessor. Compared with adapalene .1% gel, adapalene .3% gel
showed greater median percent reduction in total lesion
(56% vs. 48%; p .020) and inflammatory lesion counts
(63% vs. 58%; p .015) [13]. Both concentration performed significantly better than gel vehicle (p .001).
Currently, there are no head-to-head efficacy comparisons
of adapalene .3% gel to tretinoin gel, cream, or microsphere.
The value of adapalene for maintenance therapy was
established in a multicenter, randomized, investigatorblinded study with a total of 253 subjects. The subjects were
successfully treated (at least 50% improvement from baseline) in a previous 12-week study, and were randomized to
receive adapalene .1% gel or gel vehicle once daily for 16
weeks. Adapalene maintenance therapy resulted in higher
rates of maintaining at least 50% improvement (75% vs.
54%; p .001) and significantly lower lesion counts compared with gel vehicle [14].
Because of the chemical stability of adapalene, it is well
suited for use in combination with other topicals such as
benzoyl peroxide or antibiotics. The effectiveness of adapalene in combination therapy for the treatment of mild to
severe acne vulgaris was determined in several studies. In a
multicenter, randomized, investigator-blinded study with a
total of 249 subjects, the efficacy and tolerability of the
combination of adapalene .1% gel and topical clindamycin
.1% lotion was compared with topical clindamycin .1%
lotion and gel vehicle for the treatment of mild to moderate
acne. The subjects applied adapalene or vehicle gel once
daily in the evening, and topical clindamycin twice daily for
12 weeks. The combination of adapalene and topical clindamycin was more effective than topical clindamycin alone
in reducing the total lesions (46.7% vs. 25.5%, p .001),
inflammatory lesions (55.0% vs. 44.2%, p .004), and
non-inflammatory lesions (42.5% vs. 16.3%, p .001)
[15]. In another multicenter, randomized, investigatorblinded study, 467 patients with severe acne were randomized to receive either the combination of adapalene .1% gel
and oral doxycycline or gel vehicle and oral doxycycline for
a duration of 12 weeks. Compared with oral doxycyline
alone, the combination of adapelene and oral doxycycline
resulted in a larger reduction in median percent change of
total lesions (61% vs. 45%, p .001), inflammatory lesions
(65% vs. 59%, p .02), and non-inflammatory lesions
(60% vs. 41%, p .001) [16].
C.E. Irby et al. / Journal of Adolescent Health 43 (2008) 421 424
Safety and tolerability
In two controlled, randomized, investigator-blinded, intraindividual comparison studies, the tolerance of adapalene
.1% gel was compared with six different tretinoin formulations (tretinoin .025%, .05%, and .1% cream; tretinoin .01%
and .025% gel; and tretinoin .1% gel microsphere) and
control (petrolatum). In these studies, adapalene, tretinoin
formulations, and petrolatum were applied to the back daily
followed by occlusion 5 days per week for 3 weeks to
evaluate the cumulative irritation potential. The evaluation
of irritancy was based on an eight-point scale accounting for
dryness, erythema, papular or papulovesicular responses,
edema, and erosions or crusting. Adapalene was significantly better tolerated than all formulations of tretinoin
(including tretinoin microsphere), and was not statistically
different from the control, petrolatum gel (no p value reported) [7].
In one multicenter, randomized, investigator-blinded
study, 105 patients with mild to moderate acne vulgaris
were treated with adapalene .1% gel versus tretinoin .025%
gel for 3 months to compare the onset of action, tolerability,
and impact on quality of life. Adapalene was significantly
better tolerated (p .05) than tretinoin when evaluated on
a four-point scale for dryness, erythema, immediate and
persistent burning, and pruritus. Using the DLQI, there was
a statistically significant improvement in quality of life for
both treatment groups (p .05). At weeks 1 and 12, there
were improvements in quality of life in favor of adapalene
for items related to problems with close contacts, skin
symptoms, and social interactions [11].
The effectiveness and safety of adapalene gel .1% when
used with other acne treatments was evaluated in a prospective, open-label, multicenter, observational, phase 4 study.
Adverse events and tolerability of adapalene gel .1% were
evaluated in 1864 subjects. Subjects nave to acne treatment
(n 1396) received initial combination therapy with adapalene gel, whereas subjects already on nonretinoid therapy
(n 468) added adapalene to their existing regimen. The
overall rates of moderate to severe cutaneous irritation at
423
week 12 measured on a four-point scale of erythema, peeling/scaling, dryness, and stinging/burning were low, ranging between 1.5% and 3.2% [17].
Discussion
The development of topical retinoids has proved to be
essential in the management of acne. As such, our review of
adapalene is important from a therapeutic perspective because topical retinoids are underutilized in practice [16].
The most compelling predictor of the use or nonuse of
topical retinoids was physician specialty, with nondermatologists significantly less likely to use topical retinoids than
dermatologists (39.4% vs. 23%) [18]. More recent data
suggest that there is an even broader disparity in use of
topical retinoids between dermatologists and pediatricians.
(46.4% vs. 15.2%) [19].
Physicians may be reluctant to prescribe topical retinoids
because of the irritating side effects of the earlier retinoids,
resulting in poor adherence to treatments and complaints
about the treatment regimen. Acne treatment regimens may
also be complicated by the need to use some retinoids at
different times than benzoyl peroxide or sun exposure. Adapalene, however, can be used in conjunction with benzoyl
peroxide and sun exposure, with less risk of irritation.
In 2003, an international committee of physicians and
researchers developed the most recent set of guidelines for
acne management [20]. These largely evidence-based recommendations advocate targeting as many processes in the
pathogenesis of acne vulgaris as possible. The consensus
guidelines state that a topical retinoid should be used as the
primary treatment for mild to moderate acne (including
inflammatory acne), secondary to its anti-inflammatory
properties and its inhibition of the formation of the microcomedone, the precursor to all acne lesions. Therefore topical retinoids target two key mechanisms in the pathogenesis of acne. To target three pathogenic factors, it is
recommended that antimicrobial agents be in used in combination with topical retinoids when inflammatory lesions
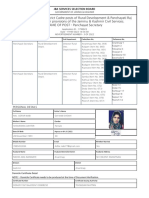
Table 1
Acne treatment algorithm
Treatment
Mild
Moderate
Severe
Comedonal
Papular/pustular
Papular/pustular
First-line
Topical retinoid
Topical retinoid BPO
Oral antibiotic topical retinoid BPO
Second-line
Salicylic acid
Topical retinoid salicylic
acid or BPO/AB
Oral antibiotic topical
retinoid BPO/ABa
Maintenance
Topical retinoid BPO or BPO/AB
BPO benzoyl peroxide; AB topical antibiotic.
Adapted from Gollnick et al. [20].
a
For female patients, hormonal therapy (oral contraceptives) may be added.
b
For refractory cases only.
Nodular
Nodular
a
Oral antibiotic topical
retinoid BPO/ABa
or Oral isotretinoinb
Oral antibiotic topical
retinoid BPO/ABa
Oral isotretinoina
424
C.E. Irby et al. / Journal of Adolescent Health 43 (2008) 421 424
are present. Oral antibiotics are the drug of choice for
moderate to severe acne, but should be used in combination
with topical retinoids, and should be discontinued as soon as
possible (within 8 12 weeks) to prevent development of
bacterial resistance. Finally, topical retinoids are critical for
maintenance therapy because of their effect on the microcomedone (Table 1) [20].
Several topical retinoid preparations are available that
can be used in monotherapy and combination regimens that
meet acne treatment consensus guidelines. From an economic view, the two leading topical retinoids, adapalene gel
and tretinoin microsphere, are comparable in price (150
per 45 g) [21]. Similar to the microsphere formulation of
tretinoin, the chemical stability of adapalene facilitates its
use in combination regimens with topical benzoyl peroxide
products. Although adapalene has similar, and often slightly
better, efficacy than other topical retinoids, it is the lack of
side effects that places adapalene clinically above the rest.
References
[1] Webster GF. The pathophysiology of acne. Cutis 2005;76(2 Suppl):
4 7.
[2] Shalita A. The integral role of topical and oral retinoids in the early
treatment of acne. J Eur Acad Dermatol Venereol 2001;15(Suppl
3):439.
[3] Czernielewski J, Michel S, Bouclier M, et al. Adapalene biochemistry
and the evolution of a new topical retinoid for treatment of acne. J Eur
Acad Dermatol Venereol 2001;15(Suppl 3):512.
[4] Galderma Laboratories L.P. Differin (adapalene gel) Gel, 0.3%
Product Insert. Available at: http://www.differin.com/AboutDifferin/
ProductInsert_Gel03.aspx. Accessed October 14, 2007.
[5] Akhavan A, Bershad S. Topical acne drugs: Review of clinical
properties, systemic exposure, and safety. Am J Clin Dermatol 2003;
4:47392.
[6] Martin B, Meunier C, Montels D, Watts O. Chemical stability of
adapalene and tretinoin when combined with benzoyl peroxide in
presence and in absence of visible light and ultraviolet radiation. Br J
Dermatol 1998;139(Suppl 52):8 11.
[7] Galvin SA, Gilbert R, Baker M, et al. Comparative tolerance of
adapalene 0.1% gel and six different tretinoin formulations. Br J
Dermatol 1998;139(Suppl 52):34 40.
[8] Shroot B, Michel S. Pharmacology and chemistry of adapalene. J Am
Acad Dermatol 1997;36(6 Pt 2):S96 103.
[9] Bouclier M, Chatelus A, Ferracin J, et al. Quantification of epidermal
histological changes induced by topical retinoids and CD271 in the
rhino mouse model using a standardized image analysis technique.
Skin Pharmacol 1991;4:6573.
[10] Ellis CN, Millikan LE, Smith EB, et al. Comparison of adapalene
0.1% solution and tretinoin 0.025% gel in the topical treatment of
acne vulgaris. Br J Dermatol 1998;139(Suppl 52):417.
[11] Grosshans E, Marks R, Mascaro JM, et al. Evaluation of clinical
efficacy and safety of adapalene 0.1% gel versus tretinoin 0.025% gel
in the treatment of acne vulgaris, with particular reference to the onset
of action and impact on quality of life. Br J Dermatol 1998;139(Suppl
52):26 33.
[12] Nyirady J, Grossman RM, Nighland M, et al. A comparative trial of
two retinoids commonly used in the treatment of acne vulgaris. J
Dermatol Treat 2001;12:149 57.
[13] Thiboutot D, Pariser DM, Egan N, et al. Adapalene gel 0.3% for the
treatment of acne vulgaris: A multicenter, randomized, double-blind,
controlled, phase III trial. J Am Acad Dermatol 2006;54:24250.
[14] Thiboutot DM, Shalita AR, Yamauchi PS, et al. Adapalene gel, 0.1%,
as maintenance therapy for acne vulgaris: A randomized, controlled,
investigator-blind follow-up of a recent combination study. Arch
Dermatol 2006;142:597 602.
[15] Wolf JE Jr, Kaplan D, Kraus SJ, et al. Efficacy and tolerability of
combined topical treatment of acne vulgaris with adapalene and
clindamycin: A multicenter, randomized, investigator-blinded study.
J Am Acad Dermatol 2003;49(3 Suppl):S2117.
[16] Thiboutot DM, Shalita AR, Yamauchi PS, et al. Combination therapy
with adapalene gel 0.1% and doxycycline for severe acne vulgaris: A
multicenter, investigator-blind, randomized, controlled study. Skinmed
2005;4:138 46.
[17] Wolf JE Jr. Safety and tolerability in the MORE trial. Cutis 2006;78(1
Suppl):19 25.
[18] Balkrishnan R, Fleischer AB Jr, Paruthi S, Feldman SR. Physicians
underutilize topical retinoids in the management of acne vulgaris:
Analysis of U.S. National Practice Data. J Dermatol Treat 2003;14:
172 6.
[19] Yentzer BA, Irby CE, Fleischer AB, Feldman SR. Differences in acne
treatment prescribing patterns of pediatricians and dermatologists: An
analysis of nationally representative data. Pediatr Dermatol 2008. In
press.
[20] Gollnick H, Cunliffe W, Berson D, et al. Management of acne: A
report from a Global Alliance to Improve Outcomes in Acne. J Am
Acad Dermatol 2003;49(1 Suppl Part 2):S137.
[21] Drugstore.com. Available at: http://www.drugstore.com. Accessed
May 8, 2008.
Вам также может понравиться
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeОт EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeРейтинг: 4 из 5 звезд4/5 (5794)
- Dan Kärreman and Mats AlvessonДокумент31 страницаDan Kärreman and Mats AlvessonjparanotiОценок пока нет
- OpposedДокумент10 страницOpposedjparanotiОценок пока нет
- The Lone Ranger and Tonto Fistfight in HeavenДокумент6 страницThe Lone Ranger and Tonto Fistfight in HeavenjparanotiОценок пока нет
- Imposition of Sanctions MeasuresДокумент5 страницImposition of Sanctions MeasuresjparanotiОценок пока нет
- Leadership Theories and PracticeДокумент44 страницыLeadership Theories and PracticeDeepak KanojiaОценок пока нет
- RebuttalДокумент7 страницRebuttaljparanotiОценок пока нет
- Graphic Novels Fall 2012 SyllabusДокумент10 страницGraphic Novels Fall 2012 SyllabusjparanotiОценок пока нет
- Jeffrey D. Ford 2010Документ13 страницJeffrey D. Ford 2010jparanotiОценок пока нет
- Dan Kärreman and Mats AlvessonДокумент31 страницаDan Kärreman and Mats AlvessonjparanotiОценок пока нет
- Chicago Style Citations: First Reference To A SourceДокумент11 страницChicago Style Citations: First Reference To A SourcejparanotiОценок пока нет
- Jeffrey D. Ford 2005Документ17 страницJeffrey D. Ford 2005jparanotiОценок пока нет
- Sherman S ReviewДокумент4 страницыSherman S ReviewjparanotiОценок пока нет
- Resistance To Change and Ways of Reducing Resistance in EducationalДокумент8 страницResistance To Change and Ways of Reducing Resistance in EducationaljparanotiОценок пока нет
- Spss 17Документ35 страницSpss 17jparanotiОценок пока нет
- Lodine-Chaffey Jennifer ThesisДокумент125 страницLodine-Chaffey Jennifer ThesisjparanotiОценок пока нет
- Graphic Novels Fall 2012 SyllabusДокумент10 страницGraphic Novels Fall 2012 SyllabusjparanotiОценок пока нет
- Study GuideДокумент25 страницStudy GuidejparanotiОценок пока нет
- HamletДокумент35 страницHamletjparanoti100% (2)
- Annotated Bibliography: Academic Tip SheetДокумент2 страницыAnnotated Bibliography: Academic Tip SheetjparanotiОценок пока нет
- Annotated Bibliography: Academic Tip SheetДокумент2 страницыAnnotated Bibliography: Academic Tip SheetjparanotiОценок пока нет
- Critical Analysis of Journal ArticleДокумент3 страницыCritical Analysis of Journal ArticlejparanotiОценок пока нет
- An Introduction To Researching Writing An Essay 2012-06Документ19 страницAn Introduction To Researching Writing An Essay 2012-06jparanotiОценок пока нет
- Freck EltonДокумент21 страницаFreck EltonjparanotiОценок пока нет
- Managing Risk EpidДокумент226 страницManaging Risk EpidjparanotiОценок пока нет
- Binder 1Документ2 страницыBinder 1jparanotiОценок пока нет
- Visual Storytelling The Digital Video Documentary - Original PDFДокумент44 страницыVisual Storytelling The Digital Video Documentary - Original PDFjparanoti100% (1)
- Reflective Writing Guide - Brodie PDFДокумент20 страницReflective Writing Guide - Brodie PDFjparanotiОценок пока нет
- Balanced Scorecard PDFДокумент14 страницBalanced Scorecard PDFjparanotiОценок пока нет
- Fiduciary Duty Without Equity Fiduciary Duties of Directors Under The Revised Company Law of The PRC PDFДокумент30 страницFiduciary Duty Without Equity Fiduciary Duties of Directors Under The Revised Company Law of The PRC PDFjparanotiОценок пока нет
- The Yellow House: A Memoir (2019 National Book Award Winner)От EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Рейтинг: 4 из 5 звезд4/5 (98)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceОт EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceРейтинг: 4 из 5 звезд4/5 (895)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersОт EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersРейтинг: 4.5 из 5 звезд4.5/5 (344)
- The Little Book of Hygge: Danish Secrets to Happy LivingОт EverandThe Little Book of Hygge: Danish Secrets to Happy LivingРейтинг: 3.5 из 5 звезд3.5/5 (399)
- The Emperor of All Maladies: A Biography of CancerОт EverandThe Emperor of All Maladies: A Biography of CancerРейтинг: 4.5 из 5 звезд4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaОт EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaРейтинг: 4.5 из 5 звезд4.5/5 (266)
- Never Split the Difference: Negotiating As If Your Life Depended On ItОт EverandNever Split the Difference: Negotiating As If Your Life Depended On ItРейтинг: 4.5 из 5 звезд4.5/5 (838)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryОт EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryРейтинг: 3.5 из 5 звезд3.5/5 (231)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureОт EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureРейтинг: 4.5 из 5 звезд4.5/5 (474)
- Team of Rivals: The Political Genius of Abraham LincolnОт EverandTeam of Rivals: The Political Genius of Abraham LincolnРейтинг: 4.5 из 5 звезд4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyОт EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyРейтинг: 3.5 из 5 звезд3.5/5 (2259)
- The Unwinding: An Inner History of the New AmericaОт EverandThe Unwinding: An Inner History of the New AmericaРейтинг: 4 из 5 звезд4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreОт EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreРейтинг: 4 из 5 звезд4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)От EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Рейтинг: 4.5 из 5 звезд4.5/5 (120)
- Midterm Exam (Regulatory Framework and Legal Issues in Business Law) 2021 - Prof. Gerald SuarezДокумент4 страницыMidterm Exam (Regulatory Framework and Legal Issues in Business Law) 2021 - Prof. Gerald SuarezAlexandrea Bella Guillermo67% (3)
- Short Tutorial On Recurrence RelationsДокумент13 страницShort Tutorial On Recurrence RelationsAbdulfattah HusseinОценок пока нет
- Machine DesignДокумент34 страницыMachine DesignMohammed Yunus33% (3)
- Nicolopoulou-Stamati - Reproductive Health and The EnvironmentДокумент409 страницNicolopoulou-Stamati - Reproductive Health and The EnvironmentGiorgos PapasakelarisОценок пока нет
- Effect of Boron Content On Hot Ductility and Hot Cracking TIG 316L SSДокумент10 страницEffect of Boron Content On Hot Ductility and Hot Cracking TIG 316L SSafnene1Оценок пока нет
- JKSSB Panchayat Secretary Adfar NabiДокумент3 страницыJKSSB Panchayat Secretary Adfar NabiSHEIKHXUNIОценок пока нет
- Noceda vs. Court of Appeals (Property Case)Документ3 страницыNoceda vs. Court of Appeals (Property Case)jokuanОценок пока нет
- Analysis of Effectiveness of Heat Exchanger Shell and Tube Type One Shell Two Tube Pass As Cooling OilДокумент6 страницAnalysis of Effectiveness of Heat Exchanger Shell and Tube Type One Shell Two Tube Pass As Cooling OilHendrik V SihombingОценок пока нет
- DR LukeДокумент126 страницDR Lukegabryelbarretto7Оценок пока нет
- Reading #2: Participatory Action ResearchДокумент45 страницReading #2: Participatory Action Researchapi-3723169100% (2)
- Hapter 2: Theoretical FrameworkДокумент18 страницHapter 2: Theoretical FrameworkMohamed HamzaОценок пока нет
- COMPOSITION Analysis of A Jazz StandardДокумент9 страницCOMPOSITION Analysis of A Jazz StandardAndresОценок пока нет
- An Objective of Dress Code PolicyДокумент4 страницыAn Objective of Dress Code PolicySiddhraj Singh KushwahaОценок пока нет
- CR Injector Repair Kits 2016Документ32 страницыCR Injector Repair Kits 2016Euro Diesel100% (2)
- Chap 4 Debts Under Hindu LawДокумент26 страницChap 4 Debts Under Hindu LawKishoore BaskaranОценок пока нет
- PG 19 - 20 GROUP 5Документ2 страницыPG 19 - 20 GROUP 5Kevin Luis Pacheco ZarateОценок пока нет
- Synthesis - Mind Rubrics: Moderator Dr.P.Satyaveni M.D.Homoeo Dept of RepertoryДокумент79 страницSynthesis - Mind Rubrics: Moderator Dr.P.Satyaveni M.D.Homoeo Dept of RepertorySharika BachuОценок пока нет
- Cns Spectrums: The Clinical Challenges of Akathisia CME Review ArticleДокумент16 страницCns Spectrums: The Clinical Challenges of Akathisia CME Review Articledzakiyah nurul israОценок пока нет
- Nursing Informatics: Sanil VargheseДокумент55 страницNursing Informatics: Sanil VarghesePalwasha KhanОценок пока нет
- Persuasive SpeechДокумент2 страницыPersuasive SpeechAngel Zachary RayyanОценок пока нет
- Analysis of The SPM QuestionsДокумент5 страницAnalysis of The SPM QuestionsHaslina ZakariaОценок пока нет
- Stability Result 15275 MT - Initial StowageДокумент1 страницаStability Result 15275 MT - Initial StowageLife with Our planetОценок пока нет
- Quality of Life After Functional Endoscopic Sinus Surgery in Patients With Chronic RhinosinusitisДокумент15 страницQuality of Life After Functional Endoscopic Sinus Surgery in Patients With Chronic RhinosinusitisNarendraОценок пока нет
- Castigliano's 2nd TheoremДокумент29 страницCastigliano's 2nd TheoremMiddle East100% (4)
- M40 Mix DesignДокумент2 страницыM40 Mix DesignHajarath Prasad Abburu100% (1)
- Erotic Massage MasteryДокумент61 страницаErotic Massage MasteryChristian Omar Marroquin75% (4)
- Scholarly Article: Ritam Mukherjee: Post-Tagore Bengali Poetry: Image of God' and SecularismДокумент6 страницScholarly Article: Ritam Mukherjee: Post-Tagore Bengali Poetry: Image of God' and SecularismbankansОценок пока нет
- Accounting Volume 1 Canadian 8th Edition Horngren Solutions ManualДокумент25 страницAccounting Volume 1 Canadian 8th Edition Horngren Solutions ManualElizabethBautistadazi100% (43)
- E-Gift Shopper - Proposal - TemplateДокумент67 страницE-Gift Shopper - Proposal - TemplatetatsuОценок пока нет
- Men Orr HagiaДокумент8 страницMen Orr HagiaAtika Bashirati IlmanОценок пока нет