Академический Документы
Профессиональный Документы
Культура Документы
Adult Outpatient Assessment
Загружено:
Khaskheli NusratАвторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Adult Outpatient Assessment
Загружено:
Khaskheli NusratАвторское право:
Доступные форматы
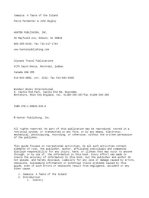
LOWELL GENERAL HOSPITAL
ADULT OUTPATIENT INITIAL ASSESSMENT
(ACU,PRESCREENING)
Date
Time
Name/Label
Family Spokesperson/Relationship and
phone#:___________________________________________________________________
ID Band in Place
Preferred Language: English Other________________________ Interpreter Offered: Name ____________________________ Declined Interpreter Services
Information Obtained: Patient
Significant Other
Family Extended Care Facility
Advanced Directive Health Care Proxy: On File Information Given Name of proxy ______________________________________________ PCP_________________________
CHIEF COMPLAINT / REASON FOR ADMISSION / PLANNED PROCEDURE:
VITAL SIGNS
RR
PAIN LEVEL
Current: _____ / 10
Max _____ / 10
Pain related to chief complaint? Yes / No; Acute / Chronic
BP
Patients Pain Goal ___________
Unconscious Patient Assess & document behaviors & physiologic changes consistent with pain.
02SAT
Weight (kg)
Height
Onset ________________________________________________________________
Location______________________________________________________________
Duration______________________________________________________________
Characteristics_________________________________________________________
Aggravating___________________________________________________________
Relieved______________________________________________________________
Treatment_____________________________________________________________
PROBLEMS: YES NO
ALLERGIES
ALLERGIES / INTOLERANCES (Include medication, food, environment, latex, contrast media)
No Known Allergies
Reaction Codes: (1) Anaphylactic reactions (2) Breathing problems (3) ENT swelling (4) Mental changes (5) GI disturbances (6) Skin reactions
Severity Codes: (M) Mild (MO) Moderate (S) Severe
Allergy/Intolerance
Reaction & Severity Codes
Allergy/Intolerance
Reaction & Severity Codes
Shellfish
Iodine
IV Contrast
Latex
No Known Allergies
PAST MEDICAL HISTORY
Cardiac / Vascular
No history
Hypertension
MI/Angina
Metabolic/Endocrine
No history
Diabetes
Cardiac disease
Heart Failure
Pacemaker
Defibrillator
Psychiatric Illness
No history
Depression Anxiety
Cardiac surgery
Valve replacement
VAD
Other
Musculoskeletal
No history
Joint replacement
Arthritis
Other
Respiratory
No history
COPD
Tuberculosis
Pneumonia
Asthma
Sleep apnea
Other
Cancer
No history
Yes If yes, describe:
No history
Yes If yes, describe:
PVD
GI/GU/GYN
No history
Hepatitis
GYN problems
Kidney Stones
GI Bleed
Pancreatitis
GU problems
Surgery
Kidney Disease
GERD
Other
Prostate
Anesthesia Problems
Neurologic
No history
Dementia
Migraines
Comments:
Seizures
Other
Vision/Hearing Problems
EENT
CVA
Cataracts
Other
Other
History of falls
LMP_______________
Alcohol Intake __________________ Substance Abuse __________________________________________
Would you want to speak with someone about this? Yes No
CURRENT MEDICATIONS / HERBS / VITAMINS
Medication
Thyroid disease
Dose
Smoking PPD ______
( List Prescription, Over-the-counter Drugs, Vitamin/Mineral Supplements, Herbs, Home Remedies)
Frequency
Time of last dose
Medication
Dose
Taking no medications
Frequency
Time of last dose
Comments & focused physical assessment: __________________________________________________________________________________________________
______________________________________________________________________________________________________________________________________
______________________________________________________________________________________________________________________________________
______________________________________________________________________________________________________________________________________
Signature:
Z:nadmin/Assessment Forms/Adult Assessment Outpatient ACU Prescreening 04/16/04 , 06/28/04, 101904 ; 10/11/05 MR# 2002-015
Page 1 of 2
NAME:
MEDICAL RECORD #:
PROBLEMS: YES NO
FUNCTIONAL SCREEN
PT Orthopedic Surgery
OT ________________________________________________
PT Crutches/Walker
Speech ____________________________________________
PHYSICAL THERAPY REFERRAL
Date / Time Notified ___________
OT / PT / SPEECH THERAPY REFERRAL
Date / Time Notified ___________
PT Other
NUTRITIONAL ASSESSMENT
NPO Since _______________________
PROBLEMS: YES NO
NUTRITION REFERRAL
Date / Time Notified: _________
N Initial enteral feeding placement
MENTAL STATUS
Alert
Disoriented
Unconscious
Developmentally Delayed
Oriented
Confused
Combative
Other
Does the patient demonstrate present behaviors and or have a past medical history that puts him/her at risk for
Harming self and/or others? Yes No If yes, ask the patient to describe techniques, methods and/or tools that
have helped to de-escalate behaviors. __________________________________________________________________
PROBLEMS: YES NO
LEARNING ASSESSMENT
1. Readiness to Learn
2. How Do You Learn
3. Barriers to Learning
(explain all checked)
4. Learning Needs
PROBLEMS: YES NO
High
Reading
Communication Deficit
Language
Memory deficit
Patient
Disease
Medications
Diet
Other
Check in
function
Medium
Listening
Literacy
Hearing/Visual
Family
Poor
Demonstration
Psychosocial/Anxiety
Other None
Patient
Treatment
Pain Management
Equipment
Surgery
Family
ABUSE ASSESSMENT
PROBLEMS: YES NO
S
OCIAL
WORKER REFERRAL
1. Do you feel safe at home? Yes SW No
If No, Why Not? ___________________________
2. Have you been hurt physically, verbally, emotionally, sexually, or financially exploited by someone within the past year? Date / Time Notified:_____________
SW Yes No Please explain. _____________________________________
3. Would you like to discuss this with a member of our staff? SW Yes No
Domestic Violence Notice Given Yes
VALUE ASSESSMENT
Is there any conflict between your religious/cultural beliefs that are in conflict with your medical treatment? Yes No
Religion:
PROBLEMS: YES NO
PRELIMINARY DISCHARGE PLANNING
Return home with responsible adult
Name: ______________________________________
CM Home services anticipated
PROBLEMS: YES NO
LIVING
SITUATION
SUPPORT
SYSTEMS
CM Transportation arrangements for discharge
CM Return to previous facility
Alone
CM
Assisted Living
CM
Elder Services/VNA
SW
Homeless
CASE MANAGEMENT REFERRAL
With Family/Friends
CM
Nursing Home
CM
Group home
CM
History of falls
Date Time Notified:______________
DeferredPatient Condition
Completed:
Date / Time / Initial:______________
PROBLEMS: YES NO
CM > 80Yrs living alone
Spouse/Significant Other
Other
Escort Home:
Friends
Involved family
Uninvolved family
SW None
Other
ADDITIONAL NOTES: __________________________________________________________________________________________________________________
Neighbors
____________________________________________________________________________________________________
____________________________________________________________________________________________________
____________________________________________________________________________________________________
____________________________________________________________________________________________________
____________________________________________________________________________________________________
____________________________________________________________________________________________________
_____________________________________________________________________________________________PreScreen
Date:
Time:
ing RN:
Z: nadmin/Assessment Forms/Adult Assessment Outpatient ACU,Prescreening 04/16/04 , 06/28/04, 101904
MR# 2002-015
Page 2 of 2
Вам также может понравиться
- The Yellow House: A Memoir (2019 National Book Award Winner)От EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Рейтинг: 4 из 5 звезд4/5 (98)
- Incident Near Miss ReportingДокумент38 страницIncident Near Miss ReportingKhaskheli Nusrat100% (3)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeОт EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeРейтинг: 4 из 5 звезд4/5 (5795)
- Taking Care of Your Wound After Skin SurgeryДокумент1 страницаTaking Care of Your Wound After Skin SurgeryKhaskheli NusratОценок пока нет
- NICE Chest Pain (EDocFind - Com)Документ2 страницыNICE Chest Pain (EDocFind - Com)Khaskheli NusratОценок пока нет
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureОт EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureРейтинг: 4.5 из 5 звезд4.5/5 (474)
- Patient Education: Recommended Curriculum Guidelines For Family Medicine ResidentsДокумент8 страницPatient Education: Recommended Curriculum Guidelines For Family Medicine ResidentsKhaskheli NusratОценок пока нет
- Graduate Nurses in The Intensive Care Unit: An Orientation ModelДокумент10 страницGraduate Nurses in The Intensive Care Unit: An Orientation ModelKhaskheli Nusrat100% (1)
- The Dynamic Turkish Healthcare Industry: Commerce, Cooperation & ConsumersДокумент26 страницThe Dynamic Turkish Healthcare Industry: Commerce, Cooperation & ConsumersKhaskheli NusratОценок пока нет
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryОт EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryРейтинг: 3.5 из 5 звезд3.5/5 (231)
- Taking Your Blood Pressure at Home: Establish A ScheduleДокумент1 страницаTaking Your Blood Pressure at Home: Establish A ScheduleKhaskheli NusratОценок пока нет
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceОт EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceРейтинг: 4 из 5 звезд4/5 (895)
- SM 091027143835 Phpapp02Документ91 страницаSM 091027143835 Phpapp02Khaskheli NusratОценок пока нет
- Never Split the Difference: Negotiating As If Your Life Depended On ItОт EverandNever Split the Difference: Negotiating As If Your Life Depended On ItРейтинг: 4.5 из 5 звезд4.5/5 (838)
- Chapter 6 Strategy Analysis and Choice 1296011800 Phpapp02Документ76 страницChapter 6 Strategy Analysis and Choice 1296011800 Phpapp02Khaskheli NusratОценок пока нет
- The Little Book of Hygge: Danish Secrets to Happy LivingОт EverandThe Little Book of Hygge: Danish Secrets to Happy LivingРейтинг: 3.5 из 5 звезд3.5/5 (400)
- Health ProductivityДокумент47 страницHealth ProductivityKhaskheli NusratОценок пока нет
- Six Sigma Project - Operators AttritionДокумент25 страницSix Sigma Project - Operators AttritionHuman Resources Revinfotech100% (3)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersОт EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersРейтинг: 4.5 из 5 звезд4.5/5 (345)
- CHCA Auditor ListДокумент7 страницCHCA Auditor ListKhaskheli NusratОценок пока нет
- Adm Ptconsent English OnlineДокумент1 страницаAdm Ptconsent English OnlineKhaskheli NusratОценок пока нет
- The Unwinding: An Inner History of the New AmericaОт EverandThe Unwinding: An Inner History of the New AmericaРейтинг: 4 из 5 звезд4/5 (45)
- CPHQ Review Course Nov 28-29 2012Документ195 страницCPHQ Review Course Nov 28-29 2012Khaskheli Nusrat100% (2)
- Team of Rivals: The Political Genius of Abraham LincolnОт EverandTeam of Rivals: The Political Genius of Abraham LincolnРейтинг: 4.5 из 5 звезд4.5/5 (234)
- Brochure CPHQ Dubai 2012Документ2 страницыBrochure CPHQ Dubai 2012Khaskheli NusratОценок пока нет
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyОт EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyРейтинг: 3.5 из 5 звезд3.5/5 (2259)
- Infection Control Checklist Nursing DepartmentДокумент5 страницInfection Control Checklist Nursing DepartmentKhaskheli NusratОценок пока нет
- Admission Nursing AssessmentДокумент20 страницAdmission Nursing AssessmentKhaskheli NusratОценок пока нет
- Microbiological ControlДокумент46 страницMicrobiological ControlMat100% (1)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaОт EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaРейтинг: 4.5 из 5 звезд4.5/5 (266)
- NCM 67 Lecture SyllabusДокумент22 страницыNCM 67 Lecture SyllabusRichard Allan SolivenОценок пока нет
- The Emperor of All Maladies: A Biography of CancerОт EverandThe Emperor of All Maladies: A Biography of CancerРейтинг: 4.5 из 5 звезд4.5/5 (271)
- Zinc OxideДокумент4 страницыZinc OxideyundayundaaОценок пока нет
- 2013 Quintiles Annual Report - Final PDFДокумент147 страниц2013 Quintiles Annual Report - Final PDFLate ArtistОценок пока нет
- 3 - 1 Blood Glucose-Lowering MedicinesДокумент41 страница3 - 1 Blood Glucose-Lowering MedicinesEva PrimanandaОценок пока нет
- FDA Notion of Opportunity For Hearing Re Penicillin, 1977Документ22 страницыFDA Notion of Opportunity For Hearing Re Penicillin, 1977marynmckОценок пока нет
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreОт EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreРейтинг: 4 из 5 звезд4/5 (1090)
- Selectividad Abuseofantibiotics - June2001Документ3 страницыSelectividad Abuseofantibiotics - June2001Penny RivasОценок пока нет
- Nurs 218 - AssignmentДокумент6 страницNurs 218 - Assignmentapi-354434651Оценок пока нет
- Wasynczuk CV May 2018Документ6 страницWasynczuk CV May 2018api-403363741Оценок пока нет
- ILO 001 Medicine Chest - Rev. 1Документ13 страницILO 001 Medicine Chest - Rev. 1RihardsОценок пока нет
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)От EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Рейтинг: 4.5 из 5 звезд4.5/5 (121)
- MaritimeFloatingStaff ClaimForHospitalisationTreatmentДокумент3 страницыMaritimeFloatingStaff ClaimForHospitalisationTreatmentSidhartha MishraОценок пока нет
- NP1 Nursing Board Exam December 2007Документ17 страницNP1 Nursing Board Exam December 2007Michelle Luba OlsenОценок пока нет
- 2004 Schuhly Major Herbs of Ayurveda E M Williamson Ed Churchill Livingstone New York 2002 361pp Price 49 95 ISBN 0 443 07203 5 HCДокумент2 страницы2004 Schuhly Major Herbs of Ayurveda E M Williamson Ed Churchill Livingstone New York 2002 361pp Price 49 95 ISBN 0 443 07203 5 HCnermal93Оценок пока нет
- Nurse's Role and Responsibilities in Administration of MedicationДокумент88 страницNurse's Role and Responsibilities in Administration of MedicationSonia Singh88% (34)
- Pharmaceutical Care DocumentationДокумент19 страницPharmaceutical Care Documentationapi-217086427Оценок пока нет
- Case Study - SPSДокумент5 страницCase Study - SPSShubham ParmarОценок пока нет
- DeontologyДокумент4 страницыDeontologyDavid JoacОценок пока нет
- The Accidental AddictsДокумент6 страницThe Accidental AddictsnorthandsouthnzОценок пока нет
- Technology Transfer Challenges in Pharmaceutical IndustryДокумент32 страницыTechnology Transfer Challenges in Pharmaceutical Industrygino100% (2)
- The Source: Reducing The Risk of Errors Associated With Concentrated Electrolyte SolutionsДокумент12 страницThe Source: Reducing The Risk of Errors Associated With Concentrated Electrolyte SolutionsStephen LeonelОценок пока нет
- Medication ErrorsДокумент2 страницыMedication Errors88AKKОценок пока нет
- Mpharm HandbookДокумент130 страницMpharm HandbookanilОценок пока нет
- CD-3 Counterfeit Detection Device - FC0413Документ2 страницыCD-3 Counterfeit Detection Device - FC0413Josh A. KrycerickОценок пока нет
- Excerpt From The Disease Delusion by Dr. Jeffrey S. BlandДокумент12 страницExcerpt From The Disease Delusion by Dr. Jeffrey S. BlandRachel Jackson100% (2)
- CFR 2013 Title21 Vol4Документ248 страницCFR 2013 Title21 Vol4maunab_patraОценок пока нет
- Kangen Water PresentasionДокумент50 страницKangen Water PresentasionKang SyaifulОценок пока нет
- The Bridge, March 19, 2015Документ28 страницThe Bridge, March 19, 2015The BridgeОценок пока нет
- Using The Pharmaceutical Literature (2006)Документ303 страницыUsing The Pharmaceutical Literature (2006)muopioidreceptorОценок пока нет
- Quantitative Techniques - III: Merck & Company: Evaluating A Drug Licensing OppurtunityДокумент5 страницQuantitative Techniques - III: Merck & Company: Evaluating A Drug Licensing OppurtunityKrishna MoorthyОценок пока нет
- The Wonders of Honey - Healing For HumankindДокумент4 страницыThe Wonders of Honey - Healing For HumankindmbazalОценок пока нет