Академический Документы
Профессиональный Документы
Культура Документы
About PRP
Загружено:
AllanSalardaAdem0 оценок0% нашли этот документ полезным (0 голосов)
85 просмотров5 страницPlatelet-rich plasma (PRP) is a concentration of platelets from a patient's own blood that contains growth factors. It is prepared through centrifugation to separate and concentrate platelets suspended in plasma. PRP contains higher levels of growth factors like platelet-derived growth factor, transforming growth factor beta, and vascular endothelial growth factor that aid wound healing by attracting stem cells, limiting inflammation, promoting new blood vessel growth, and accelerating skin regrowth. Evidence shows PRP may help heal wounds like leg ulcers, burns, surgical wounds, as well as treat hair loss, wrinkles, and scars when injected into the skin or used topically.
Исходное описание:
Information
Авторское право
© © All Rights Reserved
Доступные форматы
DOC, PDF, TXT или читайте онлайн в Scribd
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документPlatelet-rich plasma (PRP) is a concentration of platelets from a patient's own blood that contains growth factors. It is prepared through centrifugation to separate and concentrate platelets suspended in plasma. PRP contains higher levels of growth factors like platelet-derived growth factor, transforming growth factor beta, and vascular endothelial growth factor that aid wound healing by attracting stem cells, limiting inflammation, promoting new blood vessel growth, and accelerating skin regrowth. Evidence shows PRP may help heal wounds like leg ulcers, burns, surgical wounds, as well as treat hair loss, wrinkles, and scars when injected into the skin or used topically.
Авторское право:
© All Rights Reserved
Доступные форматы
Скачайте в формате DOC, PDF, TXT или читайте онлайн в Scribd
0 оценок0% нашли этот документ полезным (0 голосов)
85 просмотров5 страницAbout PRP
Загружено:
AllanSalardaAdemPlatelet-rich plasma (PRP) is a concentration of platelets from a patient's own blood that contains growth factors. It is prepared through centrifugation to separate and concentrate platelets suspended in plasma. PRP contains higher levels of growth factors like platelet-derived growth factor, transforming growth factor beta, and vascular endothelial growth factor that aid wound healing by attracting stem cells, limiting inflammation, promoting new blood vessel growth, and accelerating skin regrowth. Evidence shows PRP may help heal wounds like leg ulcers, burns, surgical wounds, as well as treat hair loss, wrinkles, and scars when injected into the skin or used topically.
Авторское право:
© All Rights Reserved
Доступные форматы
Скачайте в формате DOC, PDF, TXT или читайте онлайн в Scribd
Вы находитесь на странице: 1из 5
Platelet-rich plasma dermatological applications
What is platelet-rich plasma?
Platelet rich plasma (PRP), also termed autologous platelet
gel, plasma rich in growth factors (PRGF), platelet
concentrate (PC), is essentially an increased concentration of
autologous platelets suspended in a small amount of plasma
after centrifugation.
Blood consists of approximately 93% red blood cells (RBC),
1% white blood cells (WBC) and 6% platelets, all suspended
in plasma. In platelet rich plasma, the RBC count is lowered
to 5, since they are less useful in the healing process, while
the platelet count is increased to 94%.
This leads to a plasma super rich in platelets, at a much
higher percentage than would be found in normal blood
concentrations i.e. 1,000,000 platelets/mL of plasma.
PRP is autologous, meaning that it comes from the patient's
own body.
How is PRP collected?
Blood is withdrawn from a patients arm by syringe.
The tubes containing withdrawn blood are placed in a
centrifuge and spun using a carefully determined
protocol.
The speed and duration of centrifugation is very important
to ensure the platelets are not damaged.
Centrifuging separates the red and white blood cells and
platelets and concentrates them at various levels in the
tubes.
Blood plasma that is rich in platelets is drawn off from the
appropriate level for therapeutic use.
An activating agent (e.g. calcium chloride) is added to
activate the platelets and release their content prior to
use.
Predictable and efficient compact systems to develop PRP
that are available commercially (e.g. RegenLab,
Switzerland) can be used in both office and hospital
settings.
Background information
Platelets are probably best known as components of the
blood clotting system. When injury disrupts a blood vessel
and causes bleeding, platelets are activated and help with
the formation of a clot that stems the flow of blood.
In addition, every platelet is also a biochemical storehouse of
regulatory, signalling and growth-factor molecules that
participate in recovery and healing of tissue in response to
injury.
As an autologous preparation, PRP is safer to use than
allogenic or homologous preparations and is free from
concerns over transmissible diseases such as HIV, hepatitis,
West Nile fever, and Creutzfeldt-Jakob disease.
PRP requires no special considerations regarding antibody
formation, effectively preventing the risk of graft vs. host
disease and leading to better acceptance by patients.
Role of platelet rich plasma in wound healing
PRP effects soft tissue healing via growth factors released
after platelet degranulation. These growth factors initiate
and enhance physiological processes that contribute to
tissue recovery and healing after injury.
Growth-factor molecules associated with platelets include:
Platelet-derived growth factor (PDGF)
Transforming growth-factor-beta TGF-b)
Vascular endothelial growth factor (VEGF)
Epidermal growth factor (EGF)
Fibroblast growth factor-2 (FGF-2)
Insulin-like growth factor (IGF)
These growth factors aid healing by:
attracting undifferentiated stem cells into the newly formed
matrix and triggering cell division
suppressing cytokine release and limiting inflammation
attracting macrophages to improve tissue healing and
regeneration
promoting new capillary growth (new blood vessel
formation), and accelerating epithelialisation.
Indications for use of PRP
There is accumulating evidence that PRP can help in the
following skin conditions:
Venous and arterial leg ulcers
Diabetic foot ulcers
Pressure ulcers (bedsores)
Skin graft donor sites
First and second degree thermal burns
Superficial injuries, cuts, abrasions and surgical wounds
Hair loss disorders PRP has been shown to reinvigorate
dormant hair follicles and stimulate new hair growth
Facial rejuvenation PRP injections can treat wrinkles,
photodamage and discoloration in conjunction together
with other treatment modalities
Post-traumatic scars PRP combined with centrifuged fat
tissue and fractional laser resurfacing improve cosmetic
appearance of scars.
Safety, complications and contraindications for PRP
PRP is immunologically neutral and poses no danger of
allergy, hypersensitivity or foreign-body reactions.
Sterile technique must be used at every stage of PRP
preparation and application. Sterile technique is especially
important if a patient has an underlying medical condition
that predisposes to infection.
PRP may be injected intralesionally or perilesionally or mixed
with autologous thrombin at a 9:1 ratio, forming a platelet
gel and used topically.
When administered by intradermal injection, a brief period of
inflammation at wound sites may be experienced. Nerve
trauma is another potential complication.
The following medical conditions are a contraindication for
use of PRP:
Critical thrombocytopaenia (low platelet count)
Hypofibrinogenaemia
Haemodynamic instability (collapse)
Sepsis (infection)
Acute and chronic infections
Chronic liver disease
Anti-coagulation therapy (warfarin, dabigatran, heparin)
What is the evidence to support PRP use in wound
healing?
Available data are largely based on case series. These
studies have demonstrated:
healing of post-traumatic and vascular wounds, diabetic
and chronic ulcers with a combination of PRP and
autologous fat supported by a 3-dimensional matrix of
hyaluronic acid
cosmetic improvement of scars with fat grafts mixed with
PRP, followed by skin resurfacing with nonablative laser
healing of open and chronic wounds of the heel and ankle
with a combination of PRP and hyaluronic acid
healing of dehiscent infected sternal wounds with local
application of PRP.
Case studies conducted in a number of countries have also
shown that for patients who may have moderate wrinkling
due to exposure to sunlight and/or simply due to age can
benefit from PRP treatment.
Results show that when PRP is applied by superficial or
deep dermal injection, skin texture, tone and firmness
can improve within 3 weeks with ongoing
improvements over the next few months.
Areas commonly treated using the PRP for rejuvenation
include cheeks, around the eyes, jawline, back of
hands, neck, knees, elbows, upper arms and postpregnancy stretch marks.
Related information
References:
Cervelli V, De Angelis B, Lucarini L, Spallone D, et al. Tissue
regeneration in loss of substance on the lower limbs
through use of platelet-rich plasma, stem cells from
adipose tissue, and hyaluronic acid Adv Skin Wound
Care. 2010 Jun; 23(6):262-72.
Cervelli V, Nicoli F, Spallone D, et al. Treatment of
traumatic scars using fat grafts mixed with platelet-rich
plasma, and resurfacing of skin with the 1540 nm
nonablative laser. Clin Exp Dermatol. 2012 Jan;
37(1):55-61.
Cervelli V, Lucarini L, Spallone D, et al. Use of platelet rich
plasma and hyaluronic acid on exposed tendons of the
foot and ankle.. J Wound Care. 2010 May; 19(5):188190.
Akhundov K, Pietramaggiori G, Waselle L, et al.
Development of a cost-effective method for plateletrich plasma (PRP) preparation for topical wound
healing. Ann Burns Fire Disasters. 2012 Dec 31;
25(4):207-13.
Park KY, Kim IS, Yeo IK, et al. Treatment of refractory
venous stasis ulcers with autologous platelet-rich
plasma and light-emitting diodes: a pilot study. J
Dermatolog Treat. 2013 Jun 27. [Epub ahead of print]
Salcido RS. Autologous platelet-rich plasma in chronic
wounds. Adv Skin Wound Care. 2013 Jun; 26(6):248.
Shan GQ, Zhang YN, Ma J, et al. Evaluation of the effects of
homologous platelet gel on healing lower extremity
wounds in patients with diabetes. Int J. Low Extrem
Wounds. 2013 Mar; 12(1):22-9.
On DermNet NZ:
Role of growth factors in skin creams
Leg ulcers
Hair loss
Wound healing course
Other websites:
Books about skin diseases:
See the DermNet NZ bookstore
Вам также может понравиться
- A Simple Guide to Extensor Tendonitis, Diagnosis, Treatment and Related ConditionsОт EverandA Simple Guide to Extensor Tendonitis, Diagnosis, Treatment and Related ConditionsОценок пока нет
- Trochanteric Bursitis, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsОт EverandTrochanteric Bursitis, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsОценок пока нет
- TropocellsДокумент6 страницTropocellsIsrael Exporter100% (1)
- Treatment of Tendinopathy What Works, What Does Not, and What Is On The Horizon PDFДокумент16 страницTreatment of Tendinopathy What Works, What Does Not, and What Is On The Horizon PDFFranciscoJavierRoblesОценок пока нет
- Gluteal Tendinopathy A Review of Mechanisms, Assessmentand ManagementДокумент13 страницGluteal Tendinopathy A Review of Mechanisms, Assessmentand ManagementDaniela Villablanca100% (1)
- Iliopsoas Syndrome - The Hidden Root of PainДокумент13 страницIliopsoas Syndrome - The Hidden Root of Painpeter1234u0% (1)
- Transversus Abdominis Plane (Tap) BlockДокумент6 страницTransversus Abdominis Plane (Tap) BlockSuresh KumarОценок пока нет
- AAPMR - What Makes The Practice of Physiatry MultidisciplinaryДокумент3 страницыAAPMR - What Makes The Practice of Physiatry MultidisciplinaryJared CoganОценок пока нет
- Marfan Syndrome With Atypical PresentationДокумент4 страницыMarfan Syndrome With Atypical PresentationaiОценок пока нет
- Differential Release of Mast Cell Mediators and The Pathogenesis of InflammationДокумент14 страницDifferential Release of Mast Cell Mediators and The Pathogenesis of InflammationklaumrdОценок пока нет
- Tendinopathy vs. TendinitisДокумент4 страницыTendinopathy vs. TendinitismatnpeteОценок пока нет
- Achilles TendonДокумент30 страницAchilles TendonMeldianaОценок пока нет
- @ankle BreakerДокумент2 страницы@ankle BreakerEGОценок пока нет
- Dr. Arnadi Fraktur & DislokasiДокумент77 страницDr. Arnadi Fraktur & DislokasiPuji Yunisyah RahayuОценок пока нет
- Diabetic Foot InfectionsДокумент52 страницыDiabetic Foot Infectionsshivakumar52Оценок пока нет
- Platelet-Rich Plasma in Osteoarthritis Treatment: Review of Current EvidenceДокумент18 страницPlatelet-Rich Plasma in Osteoarthritis Treatment: Review of Current EvidenceIrham KhairiОценок пока нет
- Kay SPJ: Cleft Hand, in Green DP (Ed) : Green's Operative Hand Surgery. Philadelphia, Pa, Churchill Livingston, 1999, PP 402-414Документ75 страницKay SPJ: Cleft Hand, in Green DP (Ed) : Green's Operative Hand Surgery. Philadelphia, Pa, Churchill Livingston, 1999, PP 402-414Héctor Pando SánchezОценок пока нет
- Outpatientassessmentand Managementofthediabeticfoot: John A. DipretaДокумент21 страницаOutpatientassessmentand Managementofthediabeticfoot: John A. DipretaAnonymous kdBDppigEОценок пока нет
- Chapter 4 and 4a Introduction To Medicine and DermatologyДокумент16 страницChapter 4 and 4a Introduction To Medicine and DermatologypodmmgfОценок пока нет
- Cavus Foot: Monica Paschoal Nogueira,, Fernando Farcetta,, Alexandre ZucconДокумент12 страницCavus Foot: Monica Paschoal Nogueira,, Fernando Farcetta,, Alexandre ZucconCesar AlvaradoОценок пока нет
- Forensic Gait Analysis: A Primer For CourtsДокумент36 страницForensic Gait Analysis: A Primer For Courtsfaye wongОценок пока нет
- CCRST Footanklepostop HandoutsДокумент75 страницCCRST Footanklepostop HandoutsExternalОценок пока нет
- Clinicas de Endocrino. Pie Diabetico - Dic 2013Документ15 страницClinicas de Endocrino. Pie Diabetico - Dic 2013Betzabeth RodriguezОценок пока нет
- Musculoskeletal Disease Associated With Diabetes MellitusДокумент290 страницMusculoskeletal Disease Associated With Diabetes Mellituscharanmann9165Оценок пока нет
- Necessary Elements of A Dermatologic History and Physical Evaluation PDFДокумент9 страницNecessary Elements of A Dermatologic History and Physical Evaluation PDFkyle31Оценок пока нет
- Mechanisms of LaborДокумент18 страницMechanisms of LaborleslyjoyОценок пока нет
- Thoracic Outlet Syndrome - Shoulder & Elbow - OrthobulletsДокумент13 страницThoracic Outlet Syndrome - Shoulder & Elbow - OrthobulletsSylvia GraceОценок пока нет
- Krozer ManualДокумент148 страницKrozer Manualpoddata100% (3)
- Evaluation and Management of Hip Pain An Algorithmic Approach PDFДокумент2 страницыEvaluation and Management of Hip Pain An Algorithmic Approach PDFEulaОценок пока нет
- Pelvis: Stable Pelvic FracturesДокумент4 страницыPelvis: Stable Pelvic FracturesEloise PateñoОценок пока нет
- Minireview: Intestinal Pathophysiology in AutismДокумент11 страницMinireview: Intestinal Pathophysiology in Autism__aguОценок пока нет
- Benign Joint HypermobilityДокумент4 страницыBenign Joint HypermobilityFranklin MartinezОценок пока нет
- Health QuestionaireДокумент4 страницыHealth Questionaireapi-269450405Оценок пока нет
- Osteochondritis Dissecans: Vivek PandeyДокумент25 страницOsteochondritis Dissecans: Vivek PandeyRabin DasОценок пока нет
- Gait & Posture Volume Issue 2018 - Gluteal Tendinopathy and Hip Osteoarthritis - Different PatholДокумент23 страницыGait & Posture Volume Issue 2018 - Gluteal Tendinopathy and Hip Osteoarthritis - Different PatholGiancarlo Gardella MartínezОценок пока нет
- Staged Approach For Rehabilitation ClassificationДокумент10 страницStaged Approach For Rehabilitation ClassificationCambriaChicoОценок пока нет
- Pes CavusДокумент4 страницыPes CavusPurohit_RОценок пока нет
- Lower Extremity DisordersДокумент25 страницLower Extremity DisordersJameson87Оценок пока нет
- Central Sensitisation Another Label or Useful DiagnosisДокумент4 страницыCentral Sensitisation Another Label or Useful DiagnosisMohamed ElMeligieОценок пока нет
- Hip StrengtheningДокумент1 страницаHip Strengtheningapi-282526794Оценок пока нет
- Cinahl Rotator Cuff InjuriesДокумент11 страницCinahl Rotator Cuff InjurieslizardbeeОценок пока нет
- Pes Planus - Synopsis of CausationДокумент14 страницPes Planus - Synopsis of CausationSari HestiyariniОценок пока нет
- CTEV-Hanum Maftukha AДокумент30 страницCTEV-Hanum Maftukha ADevi Fitri AryaniОценок пока нет
- The Neglected ClubfootДокумент3 страницыThe Neglected ClubfootAngelica Mercado SirotОценок пока нет
- Ctev NewДокумент48 страницCtev NewDhinie NovianiОценок пока нет
- Mirror TherapyДокумент4 страницыMirror TherapyIOSRjournalОценок пока нет
- Intravenous TherapyДокумент48 страницIntravenous TherapyFrancr ToledanoОценок пока нет
- EE3BA3 2013 OutlineДокумент4 страницыEE3BA3 2013 OutlineadiazОценок пока нет
- New Perspectives On Neurogenic Thoracic Outlet SyndromeДокумент10 страницNew Perspectives On Neurogenic Thoracic Outlet SyndromeMourning_WoodОценок пока нет
- Osteoarthritis of The KneeДокумент8 страницOsteoarthritis of The Kneeas3syamut649250% (2)
- Clemens Attinger 10 Angiosomes and Wound Care in The Diabetic FootДокумент26 страницClemens Attinger 10 Angiosomes and Wound Care in The Diabetic FootDorin DvornicОценок пока нет
- EMR Documentation TemplatesДокумент25 страницEMR Documentation TemplatesFlint Ray100% (1)
- Ultrasound Guided Lower Limb Blocks Tony AllenДокумент39 страницUltrasound Guided Lower Limb Blocks Tony Allenrepre64Оценок пока нет
- SI Provocative TestsДокумент7 страницSI Provocative TestsGumDrop100% (1)
- Oh My Painful FOOT!!!: Plantar FasciitisДокумент20 страницOh My Painful FOOT!!!: Plantar FasciitisAsogaa MeteranОценок пока нет
- Lumbar Radiculopathy Medback Castillo Mendez EDITEDДокумент12 страницLumbar Radiculopathy Medback Castillo Mendez EDITEDSteve ColbertОценок пока нет
- Motor Imagery and MirrorTherapyДокумент5 страницMotor Imagery and MirrorTherapyLorenaMariaОценок пока нет
- Charcot Neuropathy TBH PresentationДокумент15 страницCharcot Neuropathy TBH PresentationHuguette Marie NseleОценок пока нет
- Notes For PTA NPTEFFДокумент19 страницNotes For PTA NPTEFFFarhana Rashena100% (1)
- Phylogenic Diagrams of Helminths and ArthropodsДокумент2 страницыPhylogenic Diagrams of Helminths and ArthropodsAllanSalardaAdemОценок пока нет
- LDM2 Practicum Portfolio With AnnotationДокумент19 страницLDM2 Practicum Portfolio With AnnotationAllanSalardaAdemОценок пока нет
- 7 Pasidungog Search: Annex AДокумент4 страницы7 Pasidungog Search: Annex AAllanSalardaAdem100% (1)
- Summary of MovsДокумент8 страницSummary of MovsAllanSalardaAdemОценок пока нет
- Practical Research 1 RubricsДокумент1 страницаPractical Research 1 RubricsAllanSalardaAdem100% (4)
- Tool CommunicationДокумент6 страницTool CommunicationAllanSalardaAdemОценок пока нет
- June 2018Документ7 страницJune 2018AllanSalardaAdemОценок пока нет
- Disaster Readiness and Risk ReductionДокумент295 страницDisaster Readiness and Risk ReductionAllanSalardaAdem89% (38)
- IntonationДокумент26 страницIntonationAllanSalardaAdemОценок пока нет
- Basic AmericanismДокумент19 страницBasic AmericanismAllanSalardaAdemОценок пока нет
- Authentic AssessmentДокумент29 страницAuthentic AssessmentAllanSalardaAdemОценок пока нет
- American ConsonantsДокумент22 страницыAmerican ConsonantsAllanSalardaAdemОценок пока нет
- PsoriasisДокумент1 страницаPsoriasisAllanSalardaAdemОценок пока нет
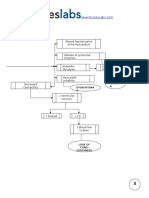
- PRP PathwayДокумент2 страницыPRP PathwayAllanSalardaAdemОценок пока нет
- Faq PRP CebuДокумент2 страницыFaq PRP CebuAllanSalardaAdemОценок пока нет
- NCP TetanusДокумент6 страницNCP Tetanusjoanna50% (6)
- Health Certificate PDFДокумент2 страницыHealth Certificate PDFPedro KunstОценок пока нет
- Myocardial Infarction Pathophysiology Schematic DiagramДокумент3 страницыMyocardial Infarction Pathophysiology Schematic Diagramnursing concept mapsОценок пока нет
- Link L8 U2 Unit TestAДокумент2 страницыLink L8 U2 Unit TestAKatarzyna Szkodzińska100% (1)
- Initial Antimicrobial Management of Sepsis: Review Open AccessДокумент11 страницInitial Antimicrobial Management of Sepsis: Review Open AccessblanquishemОценок пока нет
- FNCP - Inadequate Exercise & Breeding Site For MosquitoesДокумент2 страницыFNCP - Inadequate Exercise & Breeding Site For MosquitoesGwyneth Fisher100% (1)
- The Impact of Lifestyle Interventions On Type 2 Diabetes Management, A Comprehensive AnalysisДокумент2 страницыThe Impact of Lifestyle Interventions On Type 2 Diabetes Management, A Comprehensive AnalysisJohn nyoikeОценок пока нет
- EAU 2022 - Prostate CancerДокумент229 страницEAU 2022 - Prostate Cancerpablo penguinОценок пока нет
- Clotting Cascade Cheat SheetДокумент1 страницаClotting Cascade Cheat Sheetiomega61Оценок пока нет
- Discover Health PompleteДокумент2 страницыDiscover Health PompletenawabОценок пока нет
- Shutter Island Presentation For ArtifactДокумент8 страницShutter Island Presentation For Artifactapi-478108843Оценок пока нет
- Wim Hof Basic Technique 2017PDFДокумент3 страницыWim Hof Basic Technique 2017PDFKaveh EbadiОценок пока нет
- Promotion 2013-2014 With AnswerДокумент36 страницPromotion 2013-2014 With AnswerAloah122346Оценок пока нет
- SAR PPT 1-Program - 07Документ36 страницSAR PPT 1-Program - 07ni60Оценок пока нет
- Postpartum Haemorrhage Dr. G. Al-ShaikhДокумент51 страницаPostpartum Haemorrhage Dr. G. Al-ShaikhRaphzid InurfaceОценок пока нет
- Notes by Dr. Khurram PDFДокумент22 страницыNotes by Dr. Khurram PDFAdnan AsgharОценок пока нет
- Clinical Neurology and Neurosurgery: Erica Braun, Francesca M. Gualano, Prabha Siddarth, Eric SegalДокумент4 страницыClinical Neurology and Neurosurgery: Erica Braun, Francesca M. Gualano, Prabha Siddarth, Eric SegalNicolas LondoñoОценок пока нет
- Respiratory Distress Syndrome (Hyaline Membrane Disease)Документ98 страницRespiratory Distress Syndrome (Hyaline Membrane Disease)Miraf MesfinОценок пока нет
- Doon Institute of Medical Science2 (Exam Paper)Документ3 страницыDoon Institute of Medical Science2 (Exam Paper)Shaila PanchalОценок пока нет
- DR Stuart Crisp DR Per Grinsted: Written byДокумент8 страницDR Stuart Crisp DR Per Grinsted: Written byRizky MarethaОценок пока нет
- Astigmidwife Vlogs Online Tutorial: All Rights Are Reserved. No Part of This Publication May Be ReproducedДокумент12 страницAstigmidwife Vlogs Online Tutorial: All Rights Are Reserved. No Part of This Publication May Be ReproducedLynden BulanОценок пока нет
- Renal and Perinephric AbscessДокумент11 страницRenal and Perinephric AbscessYusak DpОценок пока нет
- Late Pregnancy Bleeding (LPB) : Antepartum Hemorrhage (Aph) Dr. A. MutungiДокумент3 страницыLate Pregnancy Bleeding (LPB) : Antepartum Hemorrhage (Aph) Dr. A. Mutungikhadzx100% (2)
- Paracetamol - DSДокумент3 страницыParacetamol - DSEnoch LabianoОценок пока нет
- The Child With Endocrine DysfunctionДокумент5 страницThe Child With Endocrine Dysfunctionhenny1620Оценок пока нет
- Gambaran Klinis Dan Patologis Pada Ayam Yang Terserang Flu Burung Sangat Patogenik (HPAI) Di Beberapa Peternakan Di Jawa Timur Dan Jawa BaratДокумент9 страницGambaran Klinis Dan Patologis Pada Ayam Yang Terserang Flu Burung Sangat Patogenik (HPAI) Di Beberapa Peternakan Di Jawa Timur Dan Jawa BaratILHAM BAGUS DARMA .NОценок пока нет
- MH Guideline For Web v2Документ1 страницаMH Guideline For Web v2FilbertaОценок пока нет
- MeningomyeloceleДокумент34 страницыMeningomyelocelerajan kumarОценок пока нет
- Oceanic Question Bank Year 4Документ358 страницOceanic Question Bank Year 4maryОценок пока нет
- PRECIO PromalabДокумент6 страницPRECIO PromalabJenny QuingaОценок пока нет