Академический Документы
Профессиональный Документы
Культура Документы
CC-Concept Map 2
Загружено:
MDCITYАвторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
CC-Concept Map 2
Загружено:
MDCITYАвторское право:
Доступные форматы
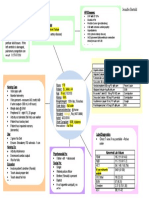
Admission date: 9/22
Admitting diagnosis: Unstable
Angina
Surgical procedure: CABG
Risk factors
Obesity, hyperlipidemia,
smoking, Family history of heart
disease, HTN, diabetes
Pertinent PMH/PSH:
Pathophysiology: CABG:
Coronary artery bypass grafting (CABG) may be the treatment of choice for people
with significant CAD who do not respond to medical treatment and who are not suitable candidates for PCI. It may also
be indicated as an emergent treatment for STEMI, in which case the surgery should be done within 4 to 6 hours of
symptom onset if possible. The procedure involves revascularization of the affected myocardium by placing a
saphenous vein graft between the aorta and the affected coronary artery distal to the site of occlusion, or by using the
internal mammary artery to revascularize the left anterior descending artery or its branches. One to five distal
anastomoses commonly are done. Emergent or urgent CABG, as a reperfusion strategy, is indicated in situations such
as failed PCI with persistent pain or hemodynamic instability, or for patients who are not candidates for PCI or
fibrinolytic therapy.
HTN, Hyperlipidemia, Diabetes
Mellitus, Fatty liver, Sleep apnea,
Unstable angina
Patient S/S
Last V/S, including O2 sat and
pain scale
HR-80, BP-146/73, RR-20, Spo292%, Temp-36.4, Pain 6/10
Current treatments (IV,
medications, catheters, tubes,
drains. O2, ostomies)
Sub-sternal chest pain
Unstable angina
Weakness, weight loss, and
anorexia, fatigue
SOB
Activity intolerance
Priority Assessments
Heart assessment
Nutrition: Cardiac
Oxygen saturation
Bilateral lung auscultation
Assessment of the nutrition
Mental Health: Stable
Incision site assessment
Other: Allergies:
Demerol, Prednisone, Tegretol,
Dilantin, IV Dye
K-36 low
CO2- 31 high
Recommended consults:
Cardiology consult 2 weeks
following discharge
PT/OT/Speech: PT, OT
Na-136 Low
Cl- 95 low
Right subclavian vein PICC linetriple lumen, Foley catheter, O2RA
MEDS: Amiodarone, Aspirin,
Atorvastatin, Docusate sodium,
Sennoside, Enoxaparin,
Furosemide, Glimperide- Amaryl.
Lab values with discussion of
expected/unexpected findings
RBC-4.02 Low
Diagnostic tests with discussion of
expected/unexpected findings
EKG
Hgb- 12.8 Low
Chest X ray
Hct- 36.4- low
Stress test
Glucose-155 high
Priority Nursing Diagnoses
1. Decreased cardiac output related to depressed cardiac function as
evidenced by
2. Acute pain related to traumatic surgery
3. Risk for infection related to open heart surgery as evidenced by
1. Decreased cardiac output related to depressed cardiac function as evidenced by
Interventions with rationale and citation
Expected Outcomes
(2)
1.Pateint will demonstrate adequate
cardiac output as evidenced by
blood pressure, pulse rate and
rhythm within normal parameters
for client within 24 hours
2. Patient will demonstrate lack of
chest discomfort or dyspnea as
evidenced by ability to tolerate
activity without shortness of breath
within 24 hours
Evaluation
Goal was partially met: Patient
was very realistic and
enthusiastic in helping health
care providers to achieve goal,
however due to lack of energy
OUTCOME #1:
1. Recognize primary characteristics of decreased cardiac output as fatigue, dyspnea, edema, orthopnea, paroxysmal nocturnal dyspnea, and increased central
venous pressure. Recognize secondary characteristics of decreased cardiac output as weight gain, hepatomegaly, jugular venous distention, palpitations, lung
crackles, oliguria, coughing, clammy skin, and skin color changes. EBN: A nursing study to validate characteristics of the nursing diagnosis decreased cardiac output in
a clinical environment identified and categorized related client characteristics that were present as primary or secondary (Martins, Alita, & Rabelo, 2010).
2. Monitor and report presence and degree of symptoms including dyspnea at rest or with reduced exercise capacity, orthopnea, paroxysmal nocturnal dyspnea,
nocturnal cough, distended abdomen, fatigue, or weakness. Monitor and report signs including jugular vein distention, S3 gallop, rales, positive hepatojugular reflux,
ascites, laterally displaced or pronounced PMI, heart murmurs, narrow pulse pressure, cool extremities, tachycardia with pulsus alternans, and irregular heartbeat.
EB: These are symptoms and signs consistent with heart failure (HF) and decreased cardiac output (Jessup et al, 2009). In a study of primary care clients,
breathlessness during exercise, limitations in physical activity, and orthopnea were the three most significant symptoms most often associated with HF (Devroey &
Van Casteren, 2011).
3. Monitor orthostatic blood pressures and daily weights. EB: These interventions assess for fluid volume status (Jessup et al, 2009). EB: The extent of volume
overload is key to deciding on appropriate treatment for HF (Lindenfeld et al, 2010).
4. Recognize that decreased cardiac output that can occur in a number of non-cardiac disorders such as septic shock and hypovolemia. Expect variation in orders for
differential diagnoses related to the etiology of decreased cardiac output, as orders will be distinct to address primary cause of altered cardiac output. EB: A
study of left ventricular function in patients with septic shock identified that 60% developed reversible left ventricular dysfunction that could successfully be
hemodynamically supported with IV vasoactive medications (Vieillard-Baron et al, 2008). Obtain a thorough history. EB: It is important to assess for behaviors
that might accelerate the progression of HF symptoms such as high sodium diet, excess fluid intake, or missed medication doses (Jessup et al, 2009).
5. Administer oxygen as needed per physicians order. Supplemental oxygen increases oxygen availability to the myocardium. EB: Clinical practice guidelines cite
that oxygen should be administered to relieve symptoms related to hypoxemia. Supplemental oxygen at night or for exercise is not recommended unless there is
concurrent pulmonary disease. Resting hypoxia or oxygen desaturation may indicate fluid overload or concurrent pulmonary disease (Jessup et al, 2009).
6. Monitor pulse oximetry regularly, using a forehead sensor if needed. CEB: In a study that compared oxygen saturation values of arterial blood gases to various
sensors, it was found that the forehead sensor was significantly better than the digit sensor for accuracy in clients with low cardiac output, while being easy to
use and not interfering with client care (Fernandez et al, 2007).
OUTCOME #2:
1.During acute events, ensure client remains on short-term bed rest or maintains activity level that does not compromise cardiac output. In severe HF,
restriction of activity reduces the workload of the heart (Fauci et al, 2008).
2.Provide a restful environment by minimizing controllable stressors and unnecessary disturbances. Schedule rest periods after meals and activities.
Rest helps lower arterial pressure and reduce the workload of the myocardium by diminishing the requirements for cardiac output (Fauci et al, 2008).
3.Apply graduated compression stockings or intermittent sequential pneumatic compression (ISPC) leg sleeves as ordered. Ensure proper fit by
measuring accurately. Remove stocking at least twice a day, then reapply. Assess the condition of the extremities frequently. Graduated compression
stockings may be contraindicated in clients with peripheral arterial disease (Kahn et al, 2012). EB: A study that assessed effects of ISPC on healthy
adults found that there were significant increases in cardiac output, stroke volume, and ejection fraction due to increased preload and decreased
afterload (Bickel et al, 2011); EBN: A study that assessed use of knee-length graduated compression stockings found they are as effective as thighlength graduated compression stockings. They are more comfortable for clients, are easier for staff and clients to use, pose less risk of injury to clients,
and are less expensive as recommended in this study (Hilleren-Listerud, 2009). EB: Graduated compression stockings, alone or used in conjunction
with other prevention modalities, help promote venous return and reduce the risk of deep vein thrombosis in hospitalized clients (Sachdeva et al, 2010).
4.Check blood pressure, pulse, and condition before administering cardiac medications such as angiotensin-converting enzyme (ACE) inhibitors,
angiotensin receptor blockers (ARBs), digoxin, and beta-blockers such as carvedilol. Notify physician if heart rate or blood pressure is low before
holding medications. It is important that the nurse evaluate how well the client is tolerating current medications before administering cardiac
medications; do not hold medications without physician input. The physician may decide to have medications administered even though the blood
pressure or pulse rate has lowered.
5.Observe for and report chest pain or discomfort; note location, radiation, severity, quality, duration, associated manifestations such as nausea,
indigestion, and diaphoresis; also note precipitating and relieving factors. Chest pain/discomfort may indicate an inadequate blood supply to the heart,
which can further compromise cardiac output. EB: Clients with decreased cardiac output may present with myocardial ischemia. Those with myocardial
ischemia may present with decreased cardiac output and HF (Jessup et al, 2009; Lindenfeld et al, 2010).
Closely monitor fluid intake, including intravenous lines. Maintain fluid restriction if ordered. In clients with decreased cardiac output, poorly functioning
ventricles may not tolerate increased fluid volumes.
2. Acute pain related to traumatic surgery
Expected Outcomes (2)
Evaluation
Interventions with rationale and citation
References:
Nursing Process Concept Map
Article Summary
Faculty comment on Clinical Care Map
Article Reference & Summary Faculty Comments:
Faculty comment on Nursing Process Map
Вам также может понравиться
- Concept Map HypertensionДокумент1 страницаConcept Map Hypertensiongeorge pearson0% (1)
- Colorectal Concept Map Group 2Документ2 страницыColorectal Concept Map Group 2Maria CristinaОценок пока нет
- Concept Map On Renal FailureДокумент1 страницаConcept Map On Renal FailureJessilda Damian VeranoОценок пока нет
- Pathology of Thyroid DiseasesДокумент5 страницPathology of Thyroid DiseasesNur Kamalia KamalОценок пока нет
- Reason For Needing Health Care: Key Problem / ND: Noncompliance Key Problem / NDДокумент6 страницReason For Needing Health Care: Key Problem / ND: Noncompliance Key Problem / NDnursing concept mapsОценок пока нет
- Management of The Difficult-To-Wean Adult Patient in The Intensive Care Unit - UpToDateДокумент19 страницManagement of The Difficult-To-Wean Adult Patient in The Intensive Care Unit - UpToDateJulio AceroОценок пока нет
- CC Concept MapДокумент11 страницCC Concept Mapapi-546355187Оценок пока нет
- Concept MapДокумент2 страницыConcept MapCrystal Leigh Malunes Dagting83% (6)
- Concept Map of CellulitisДокумент8 страницConcept Map of CellulitisReese Anne100% (1)
- Shock Comparison ChartДокумент2 страницыShock Comparison Chartlinnaete88% (8)
- Heart Failure COncept MapДокумент2 страницыHeart Failure COncept MapJrBong SemaneroОценок пока нет
- Knee Examination - OSCE SkillsДокумент3 страницыKnee Examination - OSCE Skillsfranksmith51Оценок пока нет
- CardiomyopathyДокумент1 страницаCardiomyopathyTrisha VergaraОценок пока нет
- Concept MapДокумент6 страницConcept Mapmenickel3100% (1)
- Nursing Concept MapДокумент2 страницыNursing Concept MapMary Mann100% (1)
- Concept Map 3 MM (Abdominal Pain)Документ2 страницыConcept Map 3 MM (Abdominal Pain)Matt McKinleyОценок пока нет
- Peripheral Vascular Disease NursingДокумент13 страницPeripheral Vascular Disease NursingCatlyn Chatpman100% (1)
- Concept Map Due 04Документ9 страницConcept Map Due 04api-545711468Оценок пока нет
- Congestive Heart Failure and Pulmonary Edema Concept MapДокумент1 страницаCongestive Heart Failure and Pulmonary Edema Concept MapAndrew Godwin100% (5)
- NUR129 Endocrine Concept Mapping InstructorДокумент8 страницNUR129 Endocrine Concept Mapping InstructorAmber EssmanОценок пока нет
- NUR 200 Tanner's Model - Noticing Through Reflecting-Updated 2020Документ4 страницыNUR 200 Tanner's Model - Noticing Through Reflecting-Updated 2020Oliver NamyaloОценок пока нет
- Careplan Concept MapДокумент1 страницаCareplan Concept MapAmanda Simpson100% (3)
- Concept MapДокумент5 страницConcept Mapmild_tea100% (1)
- DVT Concept Map-1Документ1 страницаDVT Concept Map-1Kuroudo IkutaОценок пока нет
- Concept Map of DMДокумент2 страницыConcept Map of DMLeslie Marie Rendon100% (9)
- Hypertension PathoДокумент2 страницыHypertension Pathojake90210100% (1)
- Sepsis Is The Consequence of A Dysregulated Inflammatory Response To An Infectious InsultДокумент11 страницSepsis Is The Consequence of A Dysregulated Inflammatory Response To An Infectious InsultShrests SinhaОценок пока нет
- Concept Map COPDДокумент2 страницыConcept Map COPDJilian McGugan88% (40)
- Hypertension Concept MapДокумент1 страницаHypertension Concept Mapgfhbgfhgf71% (7)
- Small Animal Clinical NutritionДокумент57 страницSmall Animal Clinical NutritionJairo Pereira100% (1)
- Hypothyroidism Concept MapДокумент5 страницHypothyroidism Concept Mapnursing concept maps0% (1)
- COPD Concept MapДокумент2 страницыCOPD Concept MapJilian McGugan100% (9)
- Pneumonia Concept MapДокумент11 страницPneumonia Concept Mapiz11100% (3)
- QSEN Simulation Template Post CABG PatientДокумент8 страницQSEN Simulation Template Post CABG PatientMissK2216Оценок пока нет
- SepsisДокумент19 страницSepsisapi-308355800Оценок пока нет
- Concept Map PEДокумент3 страницыConcept Map PERobert MariasiОценок пока нет
- Fluids Concept MappingДокумент1 страницаFluids Concept Mappingmariagarcia415100% (1)
- Unit Plan B.Sc. (Nursing) I Year Nutrition (Proteins)Документ5 страницUnit Plan B.Sc. (Nursing) I Year Nutrition (Proteins)Abhilasha Solomon100% (1)
- Coronary Artery Bypass Graph Concept MapДокумент5 страницCoronary Artery Bypass Graph Concept Mapnursing concept maps100% (1)
- CHF Cardiomegaly Volume OverloadДокумент1 страницаCHF Cardiomegaly Volume Overloadnursing concept mapsОценок пока нет
- Concept Map 2Документ1 страницаConcept Map 2lanrevoiceОценок пока нет
- Sepsis, Septic Shock, MODSДокумент19 страницSepsis, Septic Shock, MODSPaul Zantua80% (5)
- Cardiovascular Disease Concept MapДокумент5 страницCardiovascular Disease Concept MapRye Anch100% (1)
- COPD Care PLAN PDFДокумент2 страницыCOPD Care PLAN PDFVanessaMUeller100% (1)
- Enzyme CatalysisДокумент65 страницEnzyme Catalysissushant100% (1)
- Chronic Bronchitis and EmphesemaДокумент2 страницыChronic Bronchitis and Emphesemanursing concept maps100% (2)
- NursingCareAfterKidneyTransplantCaseReport PDFДокумент7 страницNursingCareAfterKidneyTransplantCaseReport PDFJohn Louie SolitarioОценок пока нет
- Acute PainДокумент1 страницаAcute Painnursing concept mapsОценок пока нет
- Concept Map 1Документ2 страницыConcept Map 1yfortilus100% (1)
- Concept Map Pleural EffusionДокумент1 страницаConcept Map Pleural Effusionapi-341263362Оценок пока нет
- Concept Map 360Документ6 страницConcept Map 360api-273469220Оценок пока нет
- Pa Tho Physiology of Congestive Heart FailureДокумент3 страницыPa Tho Physiology of Congestive Heart FailureErin MarieОценок пока нет
- Clinical Concept MapДокумент5 страницClinical Concept MapMj FernandezОценок пока нет
- CHF Concept MapДокумент1 страницаCHF Concept MapChristy Wegner Cooper100% (4)
- Nursing Plan of Care Concept Map - Immobility - Hip FractureДокумент2 страницыNursing Plan of Care Concept Map - Immobility - Hip Fracturedarhuynh67% (6)
- Concept Map Acute PainДокумент1 страницаConcept Map Acute PaincryblrОценок пока нет
- Care Plan For Excess Fluid Volume ExampleДокумент3 страницыCare Plan For Excess Fluid Volume ExampleVette Angelikka Dela CruzОценок пока нет
- Concept Map HypertensionДокумент1 страницаConcept Map Hypertensionninapot100% (1)
- Nursing Management Concept MapДокумент1 страницаNursing Management Concept MapXy-Za Roy Marie100% (1)
- Nursing Care Plan 2Документ30 страницNursing Care Plan 2Shayla HudsonОценок пока нет
- ConceptMap AMLДокумент1 страницаConceptMap AMLnursing concept mapsОценок пока нет
- Peripheral Arterial Occlusive DiseaseДокумент4 страницыPeripheral Arterial Occlusive Diseasekrisfred14100% (1)
- Case Analysis: Medical Surgical NursingДокумент7 страницCase Analysis: Medical Surgical NursingMaria ThereseОценок пока нет
- Ac HF2 PDFДокумент6 страницAc HF2 PDFKocsis IldikoОценок пока нет
- Interpretation of Cardiac Enzymes:: Test: SGOTДокумент4 страницыInterpretation of Cardiac Enzymes:: Test: SGOTMohammed AbdouОценок пока нет
- Tajuk-Tajuk Penting Kertas 2 & 3 Biologi SPMДокумент67 страницTajuk-Tajuk Penting Kertas 2 & 3 Biologi SPMCaryn YeapОценок пока нет
- Mcqs On Excretory SystemДокумент3 страницыMcqs On Excretory SystemIshfaq LoneОценок пока нет
- Recent Advances in HypertensionДокумент6 страницRecent Advances in Hypertensionrudi saputraОценок пока нет
- Ventriculo UnicoДокумент19 страницVentriculo UnicoDavid MartínezОценок пока нет
- Head and Neck Block HandbookДокумент50 страницHead and Neck Block HandbookGrace Poon OnionОценок пока нет
- 6 MonocytopoiesisДокумент8 страниц6 MonocytopoiesisVannisa Dwi NovianaОценок пока нет
- Nursing TheoriesДокумент15 страницNursing TheoriesPatrick Rivera Oca100% (1)
- Neurological Complications in Lumbar Spine SurgeryДокумент9 страницNeurological Complications in Lumbar Spine SurgeryMimi SyakilaОценок пока нет
- YJBMT1198 - Proof PART 1-1Документ17 страницYJBMT1198 - Proof PART 1-1Wanniely KussОценок пока нет
- Cells TestДокумент3 страницыCells TestSabita SinghОценок пока нет
- Dopamine Receptor Subtypes, Physiology and Pharmacology - New Ligands and Concepts in SchizophreniaДокумент17 страницDopamine Receptor Subtypes, Physiology and Pharmacology - New Ligands and Concepts in SchizophreniaolivukovicОценок пока нет
- Ethanol Injection Method Liposomes PDFДокумент2 страницыEthanol Injection Method Liposomes PDFElizabeth100% (1)
- Object and Space PerceptionДокумент10 страницObject and Space PerceptionadriricaldeОценок пока нет
- 29 Lab Tech. (MLT)Документ17 страниц29 Lab Tech. (MLT)Anjali JoshiОценок пока нет
- Jotwani (2016) PDFДокумент9 страницJotwani (2016) PDFJanine NogueraОценок пока нет
- Physiotherapy SyllabusДокумент50 страницPhysiotherapy SyllabusAdonis GaleosОценок пока нет
- Gen Bio - Immune SystemДокумент28 страницGen Bio - Immune SystemAvegel VillaciteОценок пока нет
- Barotac Nuevo National Comprehensive High SchoolДокумент2 страницыBarotac Nuevo National Comprehensive High SchoolVon AlexisОценок пока нет
- Chapter 039Документ40 страницChapter 039Chandra MuraliОценок пока нет
- Threshold and RecruitmentДокумент16 страницThreshold and RecruitmentShamaine Anne SalvadorОценок пока нет
- ThreePointer's Guide To Histology Steeple Chase For 022 ClassДокумент54 страницыThreePointer's Guide To Histology Steeple Chase For 022 ClassNnaemeka Neboh100% (1)
- ElectroДокумент10 страницElectroJohn John BenitezОценок пока нет
- HematologyДокумент38 страницHematologyNicole Ann RoseteОценок пока нет
- Jurnal 11Документ14 страницJurnal 11Zulvi RiriОценок пока нет