Академический Документы
Профессиональный Документы
Культура Документы
Trating Food Refusal in Adolescent With Asperger's Disorder
Загружено:
Andreea NicolaeОригинальное название
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Trating Food Refusal in Adolescent With Asperger's Disorder
Загружено:
Andreea NicolaeАвторское право:
Доступные форматы
Clinical
Case Studies
http://ccs.sagepub.com/
Treating Food and Liquid Refusal in an Adolescent With Asperger's Disorder
Michael P. Roth, Keith E. Williams and Candace M. Paul
Clinical Case Studies 2010 9: 260 originally published online 18 June 2010
DOI: 10.1177/1534650110373500
The online version of this article can be found at:
http://ccs.sagepub.com/content/9/4/260
Published by:
http://www.sagepublications.com
Additional services and information for Clinical Case Studies can be found at:
Email Alerts: http://ccs.sagepub.com/cgi/alerts
Subscriptions: http://ccs.sagepub.com/subscriptions
Reprints: http://www.sagepub.com/journalsReprints.nav
Permissions: http://www.sagepub.com/journalsPermissions.nav
Citations: http://ccs.sagepub.com/content/9/4/260.refs.html
>> Version of Record - Jul 12, 2010
Proof - Jun 18, 2010
What is This?
Downloaded from ccs.sagepub.com by Andreea Nicoleta Nicolae on October 12, 2011
Treating Food and Liquid
Refusal in an Adolescent
With Aspergers Disorder
Clinical Case Studies
9(4) 260272
The Author(s) 2010
Reprints and permission: http://www.
sagepub.com/journalsPermissions.nav
DOI: 10.1177/1534650110373500
http://ccs.sagepub.com
Michael P. Roth1, Keith E. Williams2,
and Candace M. Paul2
Abstract
Food refusal is a complicated condition that has both medical and social implications. In this study,
a 16-year-old boy with Aspergers disorder, dependent on gastrostromy tube feedings for
9 years, is treated with a behavioral intervention. The intervention consists of several components,
including stimulus fading for both solids and liquids, a token economy for solids, and an escape
prevention component for liquids. Before treatment, the participant consumes three different
foods and water. After treatment, the participant is consuming 78 foods and 13 beverages. At
the end of 14 days of treatment, all of the participants intakes are received orally, tube feedings
are eliminated, and the patient has gained more than 1 pound on oral feedings. The intervention
is generalized to both home and school settings, and maintenance of treatment gains is reported
by parents 3 months after the end of treatment.
Keywords
food refusal, autism spectrum disorder, token economy, stimulus fading
1 Theoretical and Research Basis
Food refusal has been described as a child failing to consume enough by mouth to maintain nutritional needs and having a height-to-weight ratio below the 5th percentile (Williams, Hendy, &
Knecht, 2008). It has been linked to medical conditions, for example, gastroesophogeal reflux
disease; cystic fibrosis (Field, Garland, & Williams, 2003; Linscheid, 2006; Piazza, Patel, Gulotta,
Sevin, & Layer, 2003); genetic disorders, for example, TreacherCollin syndrome, RusselSilver
syndrome (Ahearn, Castine, Nault, & Green, 2001; Coe et al., 1997); and psychological issues, for
example, choking phobia (Burklow & Linscheid, 2004).
Till date, only one study has examined the use of a token economy in the treatment of food
refusal. Kahng, Boscoe, and Byrne (2003) found that a token economy in conjunction with differential negative reinforcement of alternative behavior was more effective in increasing food
acceptance and reducing refusal behaviors than would a token economy with differential positive reinforcement of alternative behavior with or without physical guidance. Though this study
1
Pennsylvania State University, Harrisburg
Penn State Milton S. Hershey Medical Center
Corresponding Author:
Keith E. Williams, Feeding Program, 905 W. Governor Road, Hershey, PA 17033
E-mail: feedingprogram@hmc.psu.edu
Downloaded from ccs.sagepub.com by Andreea Nicoleta Nicolae on October 12, 2011
261
Roth et al.
demonstrated utility of a token economy as a component of treatment, the study had some
limitations. The study involved only pureed fruits and vegetables and included no foods of
higher texture or other additional food groups such as dairy, fats, grains, and meats. The food
was presented on a Nuk brush, and it was unclear whether there was a transition to other feeding
utensils. Furthermore, it was not reported whether the participant had advanced his feeding skills
at the time of follow-up. This study was, however, unique in that it did not involve the use of
escape prevention.
Although a range of interventions has been used to treat food refusal in children and adolescents, most interventions consist of several components, including some form of escape prevention in which the child is required to consume the food offered (Kerwin, 1999). One escape
prevention procedure, often termed exit criterion, involves having the child to eat a specified
amount of food, often initially a single bite, before being allowed to exit the session (Farrel,
Hagopian, & Kurtz, 2001; Paul, Williams, Riegel, & Gibbons, 2007). Another component that
has been included in interventions for food refusal is some form of stimulus fading, which has
typically involved the gradual increase in bite size or texture (Freeman & Piazza, 1998; Luiselli,
2000; Luiselli, & Gleason, 1987; Paul et al., 2007). Fading has also been used to increase volume of previously avoided drinks without eliciting negative behaviors (Babbitt, Shore, Smith,
Williams & Coe, 2001; Luiselli, Ricciardi, & Gilligan, 2005; Patel, Piazza, Kelley, Ochsner, &
Santana, 2001). This study examined use of a multicomponent intervention that included a
token economy and fading procedure for solid food and a fading procedure plus escape prevention for liquids.
Objectives
The goal of treatment was to eliminate need for gastrostomy tube feeds by increasing the volume
and variety of foods eaten to meet all of the participants nutritional needs. Liquid consumption
would also be increased both to increase caloric intake and to ensure adequate hydration.
2 Case Presentation
Tyler (pseudonym) was a 16-year-old White boy diagnosed with Aspergers disorder. Tyler was
enrolled in a public school and participated in general education classes with his peers. He
attended a learning-support classroom to receive additional instruction for math, but otherwise
received no additional educational services. Tyler resided at home with his biological parents
and younger brother.
3 Presenting Complaints
Tyler was referred to the feeding program, due to lack of weight gain, poor growth, and food
refusal. Before treatment Tylers weight was 29.94 kilograms, and his height was 141centimeters, which was below the 3rd percentile in height and weight compared to boys of his age.
Furthermore, it was calculated that Tyler had the height of an average 10-year-old and the weight
of an average 9.5-year-old.
According to Tylers parents, Tylers began to refuse most foods at 5 years of age but was a
very selective eater at 4 years of age. They also reported that his diet became progressively more
selective until his intake was so limited that he became nutritionally compromised and required
tube feedings. His parents did not report medical conditions that could serve as a possible etiology to his initial food refusal, and a review of his medical records did not reveal possible biological factors. His parents did report that by the age of 16, Tyler had been dependent on gastrostomy
Downloaded from ccs.sagepub.com by Andreea Nicoleta Nicolae on October 12, 2011
262
Clinical Case Studies 9(4)
tube feeds for 9 years. Before treatment, his daily nutritional needs were met predominantly by
32 ounces of Nutren 2.0 formula delivered through gastrostomy tube. Tyler drank only water and
ate small amounts of a specific brand of three different foods. Though these three foodsbowtie
pasta, ham steak, and cerealwere of different textures, Tyler mentioned not liking how some
foods felt in his mouth. In addition to being selective by type and texture, he only used specific
utensils and dishes and only ate dinner. Tyler was given the diagnosis of food refusal as he did
not eat enough to sustain growth; however, he did not fit the more typical pattern of children with
food refusal. A recent review of food refusal examined 38 interventions studies and found that
212 of 218 participants described in these food refusal intervention studies had some form of
medical issue that could have served as an etiology to the food refusal (Williams, Field, &
Seiveling, 2010). In a sample of children referred to feeding programs, the most common feeding problem found among the children with autism spectrum disorders was food selectivity
(Field et al., 2003), but the severity of the feeding problems in these children was not as extreme
as exhibited by Tyler.
4 History
Tyler had a gastrostomy tube placed at 7 years of age, secondary to poor growth and malnutrition.
Other than his chronic refusal to eat, Tyler presented with no medical conditions (e.g., gastroesophageal reflux disease, oral-motor deficits, delayed gastric emptying, vomiting, etc.) that
would have interfered with his ability to eat or drink. Tyler had been diagnosed with Aspergers
disorder as a preschooler. Previous attempts to address his food refusal by community providers
and by two outpatient visits to a feeding program were not successful in improving his food and
beverage intake.
5 Assessment
Before treatment, Tylers parents completed a developmental, medical, and feeding history. The
parents also provided a list of all food and liquids eaten before treatment. In reviewing the history
with Tylers parents, they described behaviors such as refusal to speak on a telephone or demonstrating distress at the sound of a vacuum that rose to the level of specific phobias.
Baseline meals were conducted and data collected on the dependent measures are described
in Section 7.1. In these baseline meals, Tyler was presented with six foods and told he could eat
any of the foods presented but was not required to eat anything. During baseline meals, Tyler
was presented with both the three foods he ate before treatment as well as novel foods from all
food groups. During baseline, Tyler ate only foods he had previously eaten and avoided all novel
foods. After three baseline meals, during which Tyler ate only small amounts of previously eaten
foods, it was decided to implement treatment. As Tyler had only eaten the same foods for several
years, and the baseline meals confirmed this pattern of consumption, it was determined that
additional baseline meals were not necessary.
Potential reinforcers were determined by interviewing both Tyler and his parents. These reinforcers included access to his laptop, preferred videos, and computer games.
5.1 Interobserver Agreement
Interobserver agreement data were recorded to account for experimenter bias while providing
treatment to Tyler. Data were collected by having either an independent observer collecting data
through a one-way observation mirror or by observing videorecordings of meals. These data were
compared to the data collected by the therapist who conducted the meal session. Interobserver
Downloaded from ccs.sagepub.com by Andreea Nicoleta Nicolae on October 12, 2011
263
Roth et al.
agreement for bites consumed, negative vocalization, and gagging was calculated for 28% of the
meals conducted and was calculated to be 93.38%, 100%, and 100%, respectively. For the dependent variable liquid consumed, no agreement data were collected. Each beverage consumed was
weighed before and after treatment (using the same kitchen scale).
5.2 Treatment Integrity
Meals were videorecorded across the course of treatment. These videorecordings were rated
using a 14-item treatment integrity checklist developed by the experimenters to ensure consistent
implementation of treatment procedures. Each video was rated by an experimenter who was not
involved in implementation of the meal being rated. Overall treatment integrity was calculated
to be 99.6% of the 17 sessions recorded.
6 Case Conceptualization
The participants age and high level of functioning makes him dissimilar to not only to previous
patients treated for food refusal in this feeding program (who tend to be younger and have more
significant delays in development) but also to participants in other published food refusal intervention studies (Williams, Field, & Seiveling, 2010). A significant consideration in the development of this intervention were the characteristics of the participant. His parents described him as
being anxious, which led us to focus more on the use of establishing operations and antecedent
manipulations rather than the escape extinction procedures used in past research (Williams &
Seiverling, 2010). Although escape extinction has been shown to be a highly effective component in the treatment of food refusal, like all extinction procedures, it can be accompanied with
negative side-effects such as crying or tantrums. One of the unique aspects to this intervention
was the way in which the daily schedule of meals was presented. Though the daily schedule of
meals is often not mentioned in articles describing the treatment of food refusal, some descriptions of interventions describe participants receiving between three (Linscheid, 2006) and five
(Patel, Piazza, Layer, Coleman, & Swartzwelder, 2005) meals or sessions per day. In this treatment, a meal was presented, the participant completed the meal, exchanged his tokens for time
in his arcade, and then when the time earned in the arcade had elapsed, another meal was
presented. Thus, the participant controlled the number of meals that occurred per day through his
response effort in meals. The greater number of bites and drinks consumed at a meal would not
only result in more minutes spent in his arcade but would also limit the number of meals presented per day. The participant learned this relationship quickly and would verbalize during
meals that he would eat more to get a long break.
Even though this intervention consisted of several components including appetite manipulation, stimulus fading for both solids and liquids, token economy for solids, and escape prevention
for liquids, it was not clear which of the components were necessary in producing the positive
outcome. Appetite manipulation, in this case the elimination of tube feeds, has been suggested as
being the most important component in the treatment of food refusal (Linscheid, 2006) and
was probably important in this intervention. Before elimination of the tube feeds, the participant
was not able to consume enough calories to meet caloric goals, but after elimination of the tube
feeds his intake increased rapidly and dramatically. Before treatment, the participant refused to
taste novel foods to the point of crying and gagging for his parents. The stimulus fading for both
the solids and liquids possibly reduced the response effort to the point that the participant was
able to successfully consume bites and drinks without collateral behaviors. Numerous times
across the course of treatment, the participant verbalized that he liked a particular food or that the
food tasted good to foods that his parents reported he had previously refused without tasting. The
Downloaded from ccs.sagepub.com by Andreea Nicoleta Nicolae on October 12, 2011
264
Clinical Case Studies 9(4)
stimulus fading may have made it possible for the participant to taste novel foods and thus
develop preferences for them. It has been suggested that positive reinforcement alone cannot
increase acceptance of food in children with food refusal but may decrease negative vocalizations and inappropriate behavior in some children (Piazza, 2008).
Although our participant verbalized his liking for the preferred activities in his arcade, it
was not clear whether access to these items was responsible for his eating behavior. Though his
solid and liquid consumption dramatically increased during treatment when compared to baseline, functional control was not demonstrated. We did demonstrate that the treatment package
increased intake when compared to baseline. Though we had planned a usewithdraw design,
removing the token economy, to examine the effectiveness of the treatment, this plan was not
successful. On the fifth day of treatment, meal without the token economy was conducted. At this
meal, the participants intake was equivalent to previous treatment meals. When the participant
was informed that he would not be earning tokens, he stated he liked his arcade, but just really
needed a break, perhaps indicating that the tokens were not as important in increasing feeding
behavior as was the backup reinforcer of earning time for a break. Although the participants
performance in this probe meal was equivalent with meals conducted with the token economy, it
was decided to continue the token economy until his intake goals were met and then eliminate
the token economy for generalization training. For the last 3 days of treatment, the participant
was offered meals without the token economy in a variety of settings in preparation for discharge. This intervention could also be conceptualized as being based on negative reinforcement,
with the participant being able to avoid frequent meals by expending a greater response effort
during meals and taking a greater number of bites and drinks.
Although the solid food portion of this intervention could be conceptualized as being based
on positive reinforcement as tokens were earned for consumption, it is likely that negative reinforcement, in terms of avoiding more frequent meals by expending a greater response effort and
eating more, is a significant factor in the success of the intervention. There was no escape prevention component for solid foods; however, it was included for liquids to ensure a minimal level
of liquid consumption because the participant had been dependent on tube feeds for 9 years and
it was unclear whether he would drink enough to maintain hydration. There were only 11 meals
during the entire course of treatment when the participant had to sit in the therapy room beyond
the 15-minute meal duration to complete his liquids. The escape prevention contingency never
came into effect after the eighth day of treatment. Given the participants success with the food,
it is possible that the escape prevention component was not necessary.
7 Course of Treatment and Assessment of Progress
Treatment sessions were conducted in a therapy room equipped with two tables, three chairs, an
observation window, and a camcorder. Tokens consisted of three stacks of laminated cards in the
shape of a lions paw, each of a different color. Also, an electronic kitchen scale was used to
measure liquid consumption before and after every meal.
7.1 Dependent Measures
Data were collected on four variables. The participants solid intake was measured by bites
consumed, operationally defined as the number of bites the participant placed in his mouth and
swallowed. Liquid consumed was measured in ounces by subtracting the postweights of the
beverages offered from their preweights. Water and other beverages (e.g., milk, juice) were
measured separately. Number of solid foods was used as a measure of diet variety and determined
by counting each food eaten by the participant, but only if two tablespoons of that food was
Downloaded from ccs.sagepub.com by Andreea Nicoleta Nicolae on October 12, 2011
265
Roth et al.
consumed. Number of liquids was also used as a measure of diet variety and was determined by
counting each beverage consumed if at least two ounces were consumed of that beverage. In
addition, data were collected on two aberrant behaviorsnegative vocalization and gagging.
Negative vocalization was defined as any instance where the participant screamed, yelled, cried,
or said no, and/or made negative statements in reference to the presented food. Gagging was
defined as any instance where the participant made gagging sounds or indicated gagging through
neck extensions, tongue protrusions, or changes in skin color.
7.2 Experimental Procedure
Before treatment, all procedures were explained to both the participant and his parents. In
addition, a list of preferred items and activities was provided by the participant.
7.2.1 Solid Food Procedure. All gastrostomy tube feeds were eliminated on Treatment Day
1. The participant was allowed to eat and drink whatever he desired overnight as long as it was
not one of his three preferred foods. On the first day of treatment the participants preferred items
(e.g., laptop computer, DVD player, game consoles) were placed in an empty room in the clinic.
The participant was informed that this room was his arcade and that he could earn time in the
room by taking bites of food. Before the initial meal of each day, the participant and a staff member reviewed a list of ranked foods from a list of 78 different food items (e.g., vegetables, fruits,
meats, starches, fats, and dairy). Foods were ranked either as a Category 1 foodviewed by the
participant as an easy food to eat; a Category 2 foodviewed by the participant as being of
medium difficulty to eat; or a Category 3 foodviewed by the participant as being a very difficult food to eat. For every meal, the participant and the staff member selected six foods from the
food list. The participant was asked to choose two Category 1 foods, two Category 2 foods, and
two Category 3 foods. A meal consisting of these six foods was presented. The participant was
informed that he would earn 1 minute in his arcade per bite of a Category 1 food, 2 minutes
per bite of a category 2 food, and 3 minutes per bite of a category 3 food. Thus, the more difficult
the food was rated, the greater the amount of time he could earn in his arcade. There was no
escape prevention component included for solid foods. Each meal lasted only 15 minutes, and
the end of the meal was marked by the ringing of a timer. The participant was allowed to continue
to eat after the timer rang, but was not required to do so. The participant could only earn tokens
during his 15-minute meals. The length of the participants break between meals was determined
by the number of minutes earned through the token economy.
If the participant consumed a particular food item for three consecutive sessions, the bite size
for that food was increased. All bites started at the size of a grain of rice and progressed to pea
size, then half teaspoon, and finally a full teaspoon. At the end of every day of treatment, the
participant was asked to choose six new foods from his rated categories that he had not chosen
in the sessions conducted that day. This was done to ensure a variety of foods were presented to
the participant across treatment. The participant was permitted to replace a food he had selected
for the day if he consumed at least 15 bites of that food before requesting change. In addition,
once a category had been exhausted, a new food was chosen from another category. For example,
if all foods had been tried from Category 1 and thereby exhausted, or the participant did not rate
any of the foods as being a Category 1 food (easy to eat), then two foods from Category 2, and
four foods from Category 3 were chosen. The participant was permitted to choose foods that he
had previously selected for meals as long as the foods were not offered on the previous day.
7.2.2 Liquid Procedure. During each 15-minute session the participant was presented with
four drinksone from each of the three categories and an 8-ounce cup of water. The participant
was not required to finish all of the water as it was a preferred drink of the participants and was
consumed regularly. He was allowed to consume the beverages throughout the 15-minute meal.
Downloaded from ccs.sagepub.com by Andreea Nicoleta Nicolae on October 12, 2011
266
Clinical Case Studies 9(4)
In meals where the participant did not consume the beverages within the 15-minute period, a
timer was set to record the time that had elapsed between the end of the session and the consumption of the drinks. The participant was required to finish the three rated beverages before
leaving the room and exchanging his tokens. This was the only escape prevention contingency
used in the intervention.
There was also a stimulus-fading criterion for the liquids. If the participant completed any
rated beverage within the 15-minute time limit, the quantity of this particular beverage was
increased by 0.25 ounce. If the participant did not finish a particular drink before the timer rang,
it remained at the same quantity for the next session. Once the drinks were consumed (either
before or after the timer rang), the participant was permitted to exchange the tokens for access to
the arcade. Once the participant was in the arcade, the timer was set to the number of tokens
exchanged (1 bite/1 drink = 1, 2, or 3 minutes of arcade time depending on the rating of food and
drink consumed). On each treatment day, the participant picked three beverages from his rated
liquid list that were not used during the previous treatment day. As it was expected that there
would not be an even distribution of beverages among the three categories, multiple drinks were
sometimes used from the same category. For example, two drinks from Category 2, one drink
from Category 3, and no drink from Category 1. Again, having the child choose different beverages on subsequent days was done to increase exposure to a wider range of drinks.
7.2.3 Liquid Procedure Modified. As gastrostomy tube feeds were eliminated on the first
day of treatment and the participant was not receiving the nutritional supplement administered
through a gastrostomy tube, it was decided to increase milk consumption as a means of increasing the participants daily caloric intake. This was accomplished by modifying the liquid procedure on the third day of treatment. Milk was also systematically increased using the same
criterion as the other beverages. Milk was included for all meals and as milk was increased the
amount of water was decreased by the same amount. Consistent with the other beverages,
changes in volume of milk were not made, unless the milk was completely consumed before the
timer sounded. By the eighth day of treatment, Tyler was drinking a range of beverages in addition to milk and water. It was decided at this point to reduce the number of beverages offered to 3,
one drink from his rated liquid list, milk and water.
7.3 Generalization Training
During the last 3 treatment days, meals were conducted as they would be in the participants
home and school settings. For each meal, the participant was given one main dish or entre
(e.g., Salisbury steak, turkey sandwich, cheeseburger, peanut butter and jelly sandwich, French
toast sticks), and three or four side dishes (e.g., cooked vegetables, salad, fresh fruit, cookies,
chips). During each session for each of these 3 days, no food items were presented consecutively. Data were collected on each bite consumed during each generalization meal. Throughout
the generalization training, no tokens were distributed and no foods were ranked. However, the
participant did receive breaks contingent on the number of bites consumed. It was determined
that if the participant consumed less than 25 bites he would receive a 20-minute break, but if he
consumed 25 bites or more then he received at least a 45-minute break. During these breaks, he
was not permitted to watch preferred videos, play electronic games, or use his laptop. He was
allowed to take walks, look at books, or magazines and converse with parents or staff.
7.4 Outcomes
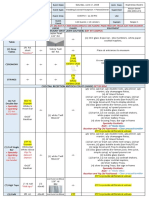
There was a substantial increase in bites consumed across the course of treatment as shown in
Figure 1. As demonstrated in Figure 1, the participant consumed 10 bites in the first treatment
Downloaded from ccs.sagepub.com by Andreea Nicoleta Nicolae on October 12, 2011
267
Roth et al.
Number of bites consumed
60
Baseline
Treatment
Generalization
50
40
30
20
10
0
1
7 10 13 16 19 22 25 28 31 34 37 40 43 46 49 52 55 58 61 64 67 70 73 76 79 82 85 88 91
Meal
Figure 1. Number of bites consumed per meal
Note: The data depict three baseline meals (solid diamond) followed by the treatment package (solid square). A single
probe meal without token economy (open triangle) was conducted with a return to the treatment package. The final
phase depicts generalization without the token economy (open triangle). The graph only shows number of bites and
does not display the increase in bite size that occurred across treatment.
meal and 45 bites on the last treatment meal. As described in the solid food procedure, bite size
for each food was increased as Tyler met criterion for that food; thus, the bite size of each food
started at the size of a grain of rice, then progressed to pea size, half teaspoon, and finally full
teaspoon size. Although not depicted in the graphs, the bite size of foods was increased as each
particular food met criterion. Thus, not only did the number of bites increase across the course of
treatment but the size of the individual bites also increased. Across treatment, the number of
meals per day decreased as the number of bites increased. These changes are shown in Figure 2.
Liquid consumed was measured in terms of ounces consumed, with water and milk displayed
as separate data paths in Figure 3. On the third day of treatment, milk was introduced, and
3.25 ounces were consumed for the day. On the last treatment day, a total of 31 ounces of milk
were consumed. In only 11 of the 93 meals did the participant take longer than the allotted
15 minutes to consume the liquids for a particular meal. All of these 11 meals were in the initial
8 days of treatment.
Again, before treatment, the participant consumed only three foods; at the end of treatment,
the number of solid foods that the participant consumed totaled 78 foods. At the 1-month followup, the participants parents reported he had added an additional 27 new foods to his diet. Before
treatment, the participant drank only water. At the end of treatment, the number of liquids consumed was a total of 13 different drinks and at the 1-month follow-up visit the participant had
added 2 more drinks to his diet. Tyler drank only water before treatment; he drank milk and a
variety of other beverages, mostly juices, by the end of treatment. When analyzing data from the
two aberrant behaviors recorded, negative vocalization and gagging, it was found that on the first
treatment day the participant had engaged in a total eight occurrences of these two behaviors,
and, after the first day of treatment, the participant never exceeded two instances of negative
vocalizing or gagging when combined per day as shown in Figure 4.
Before treatment, the participant was largely dependent on tube feeds, receiving 2000 calories
per day through tube feeds. All tube feeds were eliminated, and the participant remained off all
Downloaded from ccs.sagepub.com by Andreea Nicoleta Nicolae on October 12, 2011
268
Clinical Case Studies 9(4)
Generalization
Treatment
45
40
35
30
25
20
15
Average number of bites
consumed
Meals
10
5
0
10
11
Meals conducted
Average number of bites consumed
BL
50
1
12
13
14
Treatment Day
Figure 2. Average number of bites consumed per treatment day
8
7
BL
Water
Milk
Meals
Treatment
Generalization
8
7
6
10
11
12
13
14
Meals conducted
Average volume consumed (ounces)
Note: This graph depicts the increase in bites per meal across both the treatment and generalization (solid
squares) phases. Stimulus fading was used across the course of the treatment phase, where the size of the bites
was systematically increased. The number of bites increased further across the generalization phase. The graph
only shows average number of bites consumed per day and does not display the average increase in bite size that
occurred across each day.
Treatment day
Figure 3. Average volume of liquids consumed per treatment day
Note: On each day of treatment, the researchers added the total number of ounces consumed for both milk and
water and divided it by the number of sessions conducted each day. The z-axis measures the number of meals
conducted, the abscissa measures what treatment day the data were recorded, and the ordinate measures the
average volume of liquid consumed. The solid black squares represent average water consumption per meal per
treatment day, whereas the solid black circle markers represent average milk consumption per meal per treatment
day. The figure demonstrates that as milk was increased water was decreased, through the specified fading protocol.
Before treatment, the participant only drank water.
Downloaded from ccs.sagepub.com by Andreea Nicoleta Nicolae on October 12, 2011
269
Roth et al.
9
Negative vocalizations
Number of Occurrences
Gagging
Total of abherrant behaviors
6
5
4
3
2
1
0
1
10
11
12
13
14
Treatment day
Figure 4. Aberrant behaviors
Note: The table depicts the data collected for both negative vocalization (open square) and gagging (open diamond)
during each treatment day. As demonstrated, when combining the occurrences of each behavior (open circle), the
behaviors never appeared more than twice after the initial day of treatment.
tube feeds at the 1-month follow-up. Across the 3-week course of treatment, the participant
gained 1 pound and 4 ounces.
7.5 Social Validation of Treatment Protocol
A total of 5 weeks after the conclusion of the study, the participants parents were sent a satisfaction questionnaire. They were asked 13 questions pertaining to their satisfaction of the program
and using a 5-point Likert-type scale, they reported the highest level of satisfaction for every
question. The parents also reported that family meals were more enjoyable and that family stress
was reduced. The parents also provided additional comments describing their childs success
stating that now their child never hesitates to taste a novel food, began bringing a lunch to school,
and even eats leftover food from other family members plates.
8 Complicating Factors
There were no complicating factors in the clients history of significant importance that was not
already discussed in the client history section. Tyler was compliant for a majority of treatment
and displayed low rates of inappropriate behavior as demonstrated in Figure 4.
9 Managed Care Considerations
Tylers treatment was rapid and produced long-term success. In a previous study, the cost of tube
feeding was reported for several patients. The lowest of the costs reported was US$16, 320 per
year for the cost of the tube feeding supplies and formula (Williams, Riegel, Gibbons, & Field,
2007). Tylers treatment was paid by state medical assistance who was charged less than US$500/
day as a result of a contractual arrangement between the medical facility and the medical
Downloaded from ccs.sagepub.com by Andreea Nicoleta Nicolae on October 12, 2011
270
Clinical Case Studies 9(4)
assistance program and the state. We estimate the cost of treatment to the state medical assistance
program was lower than the cost of tube feeding for a period of 1 year. Tyler had received tube
feedings for 9 years; if intensive treatment had been provided earlier with this same level of success, the cost savings would have been substantial.
10 Follow-Up
Follow-up visits were scheduled 2 and 4 weeks after treatment in the clinic. During these visits,
Tyler and his parents met with the licensed psychologist and graduate intern feeding therapist to
discuss ongoing progress, to record stature to weight proportions and answer any questions that
Tyler and his parents may have had, and to construct a timeline for the complete removal of
Tylers gastrostomy tube. It was decided at these follow-up meetings that the gastrostomy tube
would be removed in the spring due to the predicted active flu season. In addition, follow-up was
also conducted over the phone once a week for 2 months. During the placed phone calls, Tylers
variety of foods and liquids consumed as well as any weight or height gains that were made since
the previous visit or phone call were discussed.
As discussed earlier, Tyler continued to add new foods and beverages to his diet after discharge. He eats meals without the token economy and is gaining weight at faster rate than when
he was dependent on tube feedings.
11 Treatment Implications of the Case
It is with little argument that gastrostomy tubes and other tube feeding methods (e.g., nasogastric
intubation) can be considered life saving. However, the effect of gastrostomy tube placement on
an individuals quality of life has been reported as being both physically and socially intrusive
and producing adverse psychological consequences (Jordan, Philpin, Warring, Cheung, &
Williams, 2006). The current study demonstrated a successful intervention for the treatment of
food refusal that was brief in duration (14 days), easy to implement, and generalized to both the
home and school settings. This type of intervention, in which the number of meals and the duration of reinforcement is dependent on the participants amount of response effort, may be well
suited for older children or adolescents who could understand the contingencies and for whom
more intrusive escape prevention techniques are less socially acceptable.
12 Recommendations to Clinicians and Students
To further develop the literature in this area, it is recommended that future clinicians and students
attempt a scientific design that underlines the effectiveness of each component of this treatment
package. Though it is believed that the combination of appetite manipulation, stimulus fading,
and reinforcement made the treatment successful, the contribution of each component was not
assessed.
This study also had the participant evaluate the difficulty of each novel food and rate each
food on the basis of the perceived difficulty in eating that food. Although this was not difficult
for staff, it was not clear whether this was necessary. It is also recommended that future studies
examine other possible alternatives to having a participant earn break time without having to
rank foods according to a level of perceived difficulty.
Declaration of Conflicting Interests
The authors declared that they had no conflicts of interests with respect to their authorship or the publication of this article.
Downloaded from ccs.sagepub.com by Andreea Nicoleta Nicolae on October 12, 2011
271
Roth et al.
Funding
The authors received no financial support for the research and/or authorship of this article.
References
Ahearn, W. H., Castine, T., Nault, K., & Green, G. (2001). An assessment of food acceptance in children
with autism or pervasive developmental disorder-not otherwise specified. Journal of Autism and Developmental Disorders, 31, 505-511.
Babbitt, R. L., Shore, B. A., Smith, M., Williams, K. E., & Coe, D. A. (2001). Stimulus fading in the treatment of adipsia. Behavioral Interventions, 16, 1-11.
Burklow, K. A., & Linscheid, T. (2004). Rapid inpatient behavioral treatment for choking phobia in
children. Childrens Health Care, 33, 93-107.
Coe, D. A., Babbitt. R. L., Williams, K. E., Hajimihalis, C., Snyder, A. M., Ballard, C., . . . Efron, L. A.
(1997). Use of extinction and reinforcement to increase food consumption and reduce expulsion. Journal of Applied Behavior Analysis, 30, 581-583.
Farrel, D. A., Hagopian, L. P., & Kurtz, P. F. (2001). A hospital- and home-based behavior intervention
for a child with chronic food refusal and gastrostomy tube dependence. Journal of developmental and
Physical Disabilities, 13, 407-418.
Field, D., Garland, M., & Williams, K. (2003). Correlates of specific childhood feeding problems. Journal
of Paediatric and Child Health, 39, 299 -304.
Freeman, K. A., & Piazza, C. C. (1998). Combining stimulus fading, reinforcement, and extinction to treat
food refusal. Journal of Applied Behavior Analysis, 31, 691-694.
Jordan, S., Philpin, S., Warring, J., Cheung, W. Y., & Williams, J. (2006). Percutaneous endoscopic gastrostomies: The burden of treatment from a patient perspective. Journal of Advanced Nursing, 56, 270-281.
Kahng, S., Boscoe, J. H., & Byrne, S. (2003). The use of escape contingency and a token economy to
increase food acceptance. Journal of Applied Behavior Analysis, 36, 349-353.
Kerwin, M. E. (1999). Empirically supported treatments in pediatric psychology: Severe feeding problems.
Journal of Pediatric Psychology, 24, 193-214.
Linscheid, T. R. (2006). Behavioral treatments for pediatric feeding disorders. Behavior Modification, 30,
6-23.
Luiselli, J. K. (2000). Cueing, demand fading, and positive reinforcement to establish self-feeding and oral
consumption in a child with chronic food refusal. Behavior Modification, 24, 348-358.
Luiselli, J. K., & Gleason, D. J. (1987). Combining sensory reinforcement and texture fading procedures
to overcome chronic food refusal. Journal of Behavioral Therapy and Experimental Psychiatry, 18,
149-155.
Luiselli, J. K., Ricciardi, J. N., & Gilligan, K. (2005). Liquid fading to establish milk consumption by a
child with autism. Behavioral Interventions, 20, 155-163.
Patel, M.R., Piazza, C.C., Kelly, M.L., Ochsner, C.A., & Santana,C.M. (2001) Using a fading procedure
to increase fluid consumption in a child with feeding problems. Journal of Applied Behavior Analysis,
34, 357 -360.
Patel, M. R., Piazza, C. C., Layer, S. A., Coleman, R., & Swartzwelder, D. M. (2005). A systematic evaluation of food texture to decrease packing and increase oral intake in children with pediatric feed disorder.
Journal of Applied Behavior Analysis, 38, 89-100.
Paul, C., Williams, K. E., Riegel, K., & Gibbons, B. (2007). Combining repeated taste exposure and escape
prevention: An intervention for the treatment of extreme food selectivity. Appetite, 49, 708-711.
Piazza, C. C. (2008). Feeding disorders and behavior: What have we learned? Developmental Disabilities
Research Reviews, 14, 174-181.
Piazza C. C., Patel M. R., Gulotta, C. S., Sevin, B. M., & Layer, S. A. (2003). On the relative contributions
of positive reinforcement and escape extinction in treatment of food refusal. Journal of Applied Behavior
Analysis, 36, 309-324.
Downloaded from ccs.sagepub.com by Andreea Nicoleta Nicolae on October 12, 2011
272
Clinical Case Studies 9(4)
Williams, K. E., Hendy, H., & Knecht, S. (2008). Parent feeding practices and child variables associated
with childhood feeding problems. Journal of Developmental and Physical Disabilities, 20, 231-242.
Williams, K.E., Seiverling, L., & Field, D.G. (2010). Food refusal: A review of the literature. Research in
Developmental Disabilities, 31, 625-633.
Williams, K. E., Riegel, K., Gibbons, B., & Field, D. G. (2007) Intensive behavioral treatment for severe
feeding problems: A cost-effective alternative to tube feeding. Journal of Physical and Developmental
Disabilities, 19, 227-235.
Bios
Michael Roth, M.A., recently graduated with his Masters in Applied Behavior Analysis from the Penn
State University, Harrisburg Campus. His clinical interests include working with children with autism spectrum disorders.
Keith Williams, Ph.D., is the Director of the Feeding Program at the Penn State Hershey Medical Center.
His research interests include the study of ingestive behaviors in children with chronic health problems.
Candace Paul, M.A., is a Feeding Therapist II in the Feeding Program at the Penn State Hershey Medical
Center. Her research interests include working with children with food selectivity and choking phobias.
Downloaded from ccs.sagepub.com by Andreea Nicoleta Nicolae on October 12, 2011
Вам также может понравиться
- The Yellow House: A Memoir (2019 National Book Award Winner)От EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Рейтинг: 4 из 5 звезд4/5 (98)
- Behavioral Activation in Breast Cancer PatientsДокумент14 страницBehavioral Activation in Breast Cancer PatientsAndreea NicolaeОценок пока нет
- An Investigation of Health Anxiety in FamiliesДокумент12 страницAn Investigation of Health Anxiety in FamiliesAndreea NicolaeОценок пока нет
- Don't Kick Me OutДокумент14 страницDon't Kick Me OutAndreea NicolaeОценок пока нет
- Internet-Related Psychopathology Clinical Phenotypes and PerspectivesДокумент138 страницInternet-Related Psychopathology Clinical Phenotypes and PerspectivesAndreea NicolaeОценок пока нет
- Behavioral Activation As An Intervention For Coexistent Depressive and Anxiety SymptomsДокумент13 страницBehavioral Activation As An Intervention For Coexistent Depressive and Anxiety SymptomsAndreea NicolaeОценок пока нет
- Treating Depression in Prison Nursing HomeДокумент21 страницаTreating Depression in Prison Nursing HomeAndreea NicolaeОценок пока нет
- The Five Therapeutic RelationshipsДокумент16 страницThe Five Therapeutic RelationshipsAndreea Nicolae100% (2)
- The Use of Homework Success For A Child With Attention-Deficit/ Hyperactivity Disorder, Predominantly Inattentive TypeДокумент14 страницThe Use of Homework Success For A Child With Attention-Deficit/ Hyperactivity Disorder, Predominantly Inattentive TypeAndreea NicolaeОценок пока нет
- Behavioral Therapy For Anxiety DisordersДокумент18 страницBehavioral Therapy For Anxiety DisordersAndreea NicolaeОценок пока нет
- Occupational Stress Fractors That Contribute To Its Occurrence and Effective ManagementДокумент158 страницOccupational Stress Fractors That Contribute To Its Occurrence and Effective ManagementAnonymous 0zM5ZzZXCОценок пока нет
- A Time-Series Study of The Treatment of Panic DisorderДокумент21 страницаA Time-Series Study of The Treatment of Panic Disordermetramor8745Оценок пока нет
- Clinical Case Studies.Документ14 страницClinical Case Studies.Andreea NicolaeОценок пока нет
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeОт EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeРейтинг: 4 из 5 звезд4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingОт EverandThe Little Book of Hygge: Danish Secrets to Happy LivingРейтинг: 3.5 из 5 звезд3.5/5 (400)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureОт EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureРейтинг: 4.5 из 5 звезд4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryОт EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryРейтинг: 3.5 из 5 звезд3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceОт EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceРейтинг: 4 из 5 звезд4/5 (895)
- Team of Rivals: The Political Genius of Abraham LincolnОт EverandTeam of Rivals: The Political Genius of Abraham LincolnРейтинг: 4.5 из 5 звезд4.5/5 (234)
- Never Split the Difference: Negotiating As If Your Life Depended On ItОт EverandNever Split the Difference: Negotiating As If Your Life Depended On ItРейтинг: 4.5 из 5 звезд4.5/5 (838)
- The Emperor of All Maladies: A Biography of CancerОт EverandThe Emperor of All Maladies: A Biography of CancerРейтинг: 4.5 из 5 звезд4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaОт EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaРейтинг: 4.5 из 5 звезд4.5/5 (266)
- The Unwinding: An Inner History of the New AmericaОт EverandThe Unwinding: An Inner History of the New AmericaРейтинг: 4 из 5 звезд4/5 (45)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersОт EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersРейтинг: 4.5 из 5 звезд4.5/5 (345)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyОт EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyРейтинг: 3.5 из 5 звезд3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreОт EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreРейтинг: 4 из 5 звезд4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)От EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Рейтинг: 4.5 из 5 звезд4.5/5 (121)
- Member Rewards Catalogue 2020/21 EditionДокумент22 страницыMember Rewards Catalogue 2020/21 EditionNORMALA ABDUL RANIОценок пока нет
- Determining Textual EvidenceДокумент4 страницыDetermining Textual EvidenceKaren R. Royo100% (4)
- The Most Wanted Rice Cooker - Google SearchДокумент15 страницThe Most Wanted Rice Cooker - Google SearchDoni RandanuОценок пока нет
- Times Leader 09-19-2012Документ40 страницTimes Leader 09-19-2012The Times LeaderОценок пока нет
- Science 4 - q1 - Module 4of6 - Changes That Mareials Undergowhen Mixed With Other Materials - v2Документ20 страницScience 4 - q1 - Module 4of6 - Changes That Mareials Undergowhen Mixed With Other Materials - v2Mary Ann BernalesОценок пока нет
- FFD ProgramДокумент4 страницыFFD ProgramMarkYamaОценок пока нет
- A Christmas Crossword PuzzleДокумент3 страницыA Christmas Crossword Puzzlemakbuddy50% (2)
- Market Survey ReportДокумент6 страницMarket Survey ReportxulphikarОценок пока нет
- 18 - Student Guide VolksgartenДокумент3 страницы18 - Student Guide Volksgartenanon_383527604Оценок пока нет
- Trends and Status of Public Service Delivery in UgandaДокумент151 страницаTrends and Status of Public Service Delivery in UgandaOnziki Adelia MosesОценок пока нет
- Activity EnglishДокумент2 страницыActivity EnglishJennefer Arzaga OlaОценок пока нет
- Menu Punjabi TadkaДокумент4 страницыMenu Punjabi TadkaSheikh Muhammed TadeebОценок пока нет
- Captains Packet - Lemon&Lime Aysa & Briggs 06-15-23Документ68 страницCaptains Packet - Lemon&Lime Aysa & Briggs 06-15-23OSCAR LUIS JUSTINIANO ARIASОценок пока нет
- VadilalДокумент84 страницыVadilalMIltaniyoОценок пока нет
- Getting Laid in NYCДокумент19 страницGetting Laid in NYCAlberto Ronin Gonzalez100% (2)
- Case-Study OB (Individual Work)Документ4 страницыCase-Study OB (Individual Work)Dilana ChalayaОценок пока нет
- The Scholarship - Isabella MarconДокумент40 страницThe Scholarship - Isabella Marconapi-595140229Оценок пока нет
- Teaching Plan For DiabetesДокумент4 страницыTeaching Plan For DiabetesanrefОценок пока нет
- Mayr Franz. Zulu ProverbsДокумент10 страницMayr Franz. Zulu ProverbsAzarias VilanculosОценок пока нет
- The Food Song - Kids + Children Learn English SongsДокумент2 страницыThe Food Song - Kids + Children Learn English SongsWilliam JimenezОценок пока нет
- I G Economics SampleДокумент12 страницI G Economics SampleNietharshan Eapen100% (1)
- Text For No. 1 - 4: A. Choose One Correct Answer Out of The Four Options Given!Документ7 страницText For No. 1 - 4: A. Choose One Correct Answer Out of The Four Options Given!Lisa Aprilia AprisaОценок пока нет
- The Puerto Rican StoryДокумент11 страницThe Puerto Rican StoryellenquiltОценок пока нет
- Young's MMPL Pricelist 2022Документ6 страницYoung's MMPL Pricelist 2022Newstar EaОценок пока нет
- Text 1 You Will Read A Passage About Competitive Eating. Answer The Questions Based On What You Have ReadДокумент4 страницыText 1 You Will Read A Passage About Competitive Eating. Answer The Questions Based On What You Have ReadCaroline Cezario Meme75% (4)
- Nandini NehraДокумент102 страницыNandini NehraShivraj CyberОценок пока нет
- Qse Adv TG 09 Exam Answer KeyДокумент4 страницыQse Adv TG 09 Exam Answer KeyCristian GutierrezОценок пока нет
- Kasān Haida Full PhrasebookДокумент10 страницKasān Haida Full Phrasebooklanguage warrior100% (1)
- Year 4 - Familiarisation Pack-2022-Answers-14 July 2023Документ17 страницYear 4 - Familiarisation Pack-2022-Answers-14 July 2023s.amnafaisalОценок пока нет
- Workbook Answer Key: Unit 9Документ1 страницаWorkbook Answer Key: Unit 9Управление ПерсоналомОценок пока нет