Академический Документы
Профессиональный Документы
Культура Документы
Hemorrhoids During Pregnancy
Загружено:
Ann Michelle TarrobagoАвторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Hemorrhoids During Pregnancy
Загружено:
Ann Michelle TarrobagoАвторское право:
Доступные форматы
Hemorrhoids during Pregnancy
Pregnancy puts a woman at a higher risk for developing hemorrhoids. During
pregnancy, extra pressure is put on the internal and external hemorrhoidal
veins, which can result in symptoms ranging from a feeling of vague anal
discomfort to bright-red blood covering the stool. In some cases, hemorrhoids
can be prevented by getting regular exercise and consuming more fiber.
Treatment options include stool softeners, pain relievers, and warm baths.
Pregnancy and Hemorrhoids: An Overview
Among the many changes that happen to a woman's body during pregnancy, hemorrhoids is
one that most pregnant women could do without. However, hemorrhoids are a common
occurrence -- and even more so during the third trimester.
Understanding what hemorrhoids are and how to prevent them during pregnancy may help
many women avoid this complication. For women who do develop hemorrhoids,
understanding how to treat them may minimize the chances for continued problems.
The good news: For most women, hemorrhoids during pregnancy are just that. Once your
baby is delivered, hemorrhoids usually improve.
What Are Hemorrhoids?
The term hemorrhoids refer to a condition in which the veins around the anus or lower rectum
become swollen and inflamed. Several groups of veins surround the rectum and anus -- one
group is known as internal hemorrhoidal veins, and the others are known as external
hemorrhoidal veins.
There are two types of hemorrhoids: internal and external. As the name suggests, internal
hemorrhoids affect the internal hemorrhoidal veins; external hemorrhoids affect the internal
hemorrhoidal veins.
What Causes Hemorrhoids during Pregnancy?
During pregnancy, hemorrhoids are caused by an increase in pressure within either the
internal or external hemorrhoidal veins. There are several reasons why pressure may increase
during pregnancy. Some of these reasons include:
The fetus and uterus are growing, which puts more pressure on veins in the lower
pelvic area.
Hormonal changes cause the hemorrhoidal vessels to enlarge.
Severe pressure to the hemorrhoidal veins occurs during childbirth.
Frequent constipation during pregnancy. Constipation increases straining and pressure
during bowel movements.
What Are the Symptoms?
The symptoms of hemorrhoids during pregnancy are similar to those experienced by women
who are not pregnant. They are based on the type of hemorrhoid that develops.
Internal Hemorrhoids
The most common symptom of internal hemorrhoids is bright-red blood covering the stool,
on toilet paper, or in the toilet bowl.
Other symptoms may include feeling:
Vague anal discomfort
Fullness after a bowel movement.
Pain is not a common symptom.
External Hemorrhoids
Unlike internal hemorrhoids, which are usually not painful, external hemorrhoids can be quite
painful. Additional symptoms may include:
Bleeding
Anal itching.
Diagnosing and Treating Hemorrhoids during Pregnancy
It is important to tell your healthcare provider if you experience what you think are
hemorrhoids because other conditions can cause similar symptoms. Your healthcare provider
will be able to look for these conditions and recommend treatment based on what is found.
In most cases, treatment for hemorrhoids during pregnancy is focused on:
Relieving symptoms
Relieving pressure within the hemorrhoidal veins by increasing fiber and fluids
Modifying bowel habits.
Specific treatment options may include:
Ice packs (for external hemorrhoids) applied for 10 to 15 minutes three or four times a
day.
Warm baths four or five times a day for 20 to 30 minutes.
Increased fluids and fiber in the diet.
Stool softeners. These are often combined with prenatal vitamins, but you do not want
your system to become reliant on them.
Over-the-counter creams and ointments to help with itching or inflammation. Ask
your healthcare provider which brands are safe during pregnancy.
A compress soaked in witch hazel.
A pain reliever such as Tylenol.
In addition, your healthcare provider may suggest a bulk stool softener or a fiber supplement,
such as psyllium (Metamucil) or methylcellulose (Citrucel). It's best to avoid laxatives
during pregnancy.
It is also important to set aside a certain time each day to have an unhurried bowel movement
without vigorous wiping or rubbing. Patting, using a soft, moist pad (or even rinsing in the
shower), can be used as an alternative to wiping. Make sure to avoid straining during any
bowel movement or lingering on the toilet for long periods.
Preventing Pregnancy-Related Hemorrhoids
Preventing hemorrhoids may be easier said than done. However, there are some things that
you can do to decrease the chances of them occurring during pregnancy. Some suggestions
include:
Empty bowels as soon as possible after the urge occur.
Get daily exercise, such as walking. Exercise speeds up the intestines. Make sure to
talk to your healthcare provider about what exercises during pregnancy are safe.
Avoid sitting or standing for long periods.
Increase fiber and fluid in the diet. This helps reduce constipation and straining by
producing stools that are softer and easier to pass. Eating the right amount of fiber and
drinking six to eight glasses of fluid result in softer, bulkier stools. A softer stool
makes emptying the bowels easier and lessens the pressure on hemorrhoids caused by
straining. Eliminating straining also helps prevent hemorrhoids from protruding.
Good sources of fiber include:
o
o
o
o
Fruits
Vegetables, such as carrots and green vegetables
Whole grains
Bran.
Hemorrhoids during pregnancy
Reviewed by the BabyCenter Medical Advisory Board
last updated: March 2011
What are hemorrhoids?
Hemorrhoids are blood vessels in the rectal area that have become unusually swollen. They
typically range from the size of a pea to the size of a grape and can be inside the rectum or
protrude through the anus.
Hemorrhoids can be itchy and mildly uncomfortable or downright painful. Sometimes they
can even cause rectal bleeding, especially during a bowel movement.
Hemorrhoids are common during pregnancy, particularly in the third trimester. Some
women get them for the first time while they're pregnant. And if you've had them before
pregnancy, you're quite likely to have them again now. They may also develop while you're
pushing during the second stage of labor and are a common early postpartum complaint.
In most cases, hemorrhoids that developed during pregnancy will begin to resolve soon
after you give birth, especially if you're careful to avoid constipation.
Why are they more common during pregnancy?
Pregnancy makes you more prone to hemorrhoids, as well as to varicose veins in the legs
and sometimes even in the vulva, for a variety of reasons. Your growing uterus puts
pressure on the pelvic veins and the inferior vena cava, a large vein on the right side of the
body that receives blood from the lower limbs. This can slow the return of blood from the
lower half of your body, which increases the pressure on the veins below your uterus and
causes them to become more dilated or swollen.
Constipation, another common problem during pregnancy, can also cause or aggravate
hemorrhoids. That's because straining leads to hemorrhoids, and you tend to strain when
having a hard bowel movement.
In addition, an increase in the hormone progesterone during pregnancy causes the walls of
your veins to relax, allowing them to swell more easily. Progesterone also contributes to
constipation by slowing down your intestinal tract.
How can I avoid getting hemorrhoids?
You're more susceptible to hemorrhoids when pregnant, but they're not inevitable. Here are
some ways to ward them off or get rid of them if you do get them:
First and foremost, avoid constipation: Eat a high-fiber diet (plenty of whole grains,
beans, fruits, and vegetables), drink plenty of water (eight to ten glasses a day), and
get regular exercise, even if you only have time for a short, brisk walk. If you're
constipated, ask your practitioner about using a fiber supplement or stool softener.
Don't wait when you have the urge to have a bowel movement, try not to strain
when you're moving your bowels, and don't linger on the toilet, because it puts
pressure on the area.
Do Kegel exercises daily. Kegels increase circulation in the rectal area and
strengthen the muscles around the anus, decreasing the chance of hemorrhoids.
They also strengthen and tone the muscles around the vagina and urethra, which
can help your body recover after you give birth.
Avoid sitting or standing for long stretches of time. If your job involves sitting, get up
and move around for a few minutes every hour or so. At home, lie on your left side
when sleeping, reading, or watching TV to take the pressure off your rectal veins and
help increase blood return from the lower half of your body.
What else can I do to get relief?
Apply an ice pack (with a soft covering) to the affected area several times a day. Ice
may help decrease swelling and discomfort. Some women find cold compresses
saturated with witch hazel to be soothing.
Soak your bottom in warm water in a tub for 10 to 15 minutes a few times each day.
(If you don't have a tub, you can buy a sitz bath at the drugstore. It's a small plastic
basin that you fill with water and position over your toilet, allowing you to submerge
your rectal area simply by sitting down.)
Try alternating cold and warm treatments.
Gently but thoroughly clean the affected area after each bowel movement using
soft, unscented, white toilet tissue, which causes less irritation than colored, scented
varieties.
Moistening the tissue can help, too. Many women find using premoistened wipes
more comfortable than using toilet tissue. You can buy wipes medicated with witch
hazel that are made specifically for people with hemorrhoids.
Ask your healthcare practitioner to recommend a safe topical anesthetic or
medicated suppository. There are many hemorrhoid-relief products on the market,
but consult your practitioner before trying one on your own. Most of these products
should be used for no more than a week. Continued use can cause even more
inflammation.
When should I call my practitioner?
If your own preventive and relief efforts don't help or if you have severe pain or notice
bleeding consult your doctor or midwife. (Any rectal bleeding should be checked by your
practitioner.)
For most women, hemorrhoids will get better after delivery with the help of these selftreatment measures. In some cases, you may need to see a specialist for treatment to help
shrink your hemorrhoids. Rarely, minor surgery is required to correct the problem.
Objective 1: Demonstrates individual professionalism through personal behaviors and appearance.
I demonstrated individual professionalism through maintaining client confidentiality by promoting one to one
dialogue within a physical space where no other person can noticeably hear/interrupt without asking
permission to do so. The clients chart was accessed within a room/area where there the information written
there cannot be gleaned by others not directly involved in the care of the client. My initiative for learning was
supported via collaboration with other members of the daycare centers interdisciplinary team of nurse aids,
registered nurses, physical therapist, social workers, and recreational therapist. Additional collaboration was
also done via telephone conversations with clients significant other such that continuity of care can be
maintained. Guidance from clinical professor/instructor was solicited as needed; also in depth discussion of
plan of care was addressed in clinical conferences. Punctuality and appropriate attire in attendance for clinical
rotation is paramount here as it sets the tone for the day and convey a sense of respect for those you work
with.
Objective 2: Employ analytical reasoning and critical thinking skills when providing care to individuals and
families in the community setting.
To accomplish this objective, the concept of individualizing a client based teaching plan that would be a
realistic accomplishment for the client along with their significant others via repetition of measurable goal
based interventions. This objective could only have been attained following careful inventory of all
assessment data obtained from clients chart, care team members, client significant others, and the client
themselves.. A complete physical assessment could not be done due to the casual nature of a community
based setting and medications were not administered here as well. Evaluations of the expected outcomes
from the teaching plan ultimately validated and verify the appropriateness of my interventions in achieving the
goals set forth.
Objective 3: Effectively communicate with diverse groups and disciplines using a variety of strategies regarding
the health needs of individuals and families in the community setting.
Effective communication was maintained via casual dialogues with clients. The dialogues with clients were
structured from broad to narrow such that most of the clients concerns could be captured and addressed
within my scope of practice. Appropriate referrals were made as needed via the social workers and registered
nurse in charge. Being particularly astute to non-verbal cues shown by the clients, an opportunity for
clarification/ validation of clients thoughts/feelings was utilized. Since most of the client population in this
clinical setting comprises those of varying stages of dementia, repetition and appropriate verbal tone/ques
was noted to be highly effective here. Also, emotional support to the informal caregivers for these clients was
done in a timely manner via telephone.
Objective 4: Establish environment conductive to learning and use a plan for learners based on evidence-based
practice.
Every interaction with a client starts with establishing an environment conductive for learning. For example,
being that our dominant client population was made up of those with varying stages of dementia, music has
been shown to tap into their sense of expression and thereby also allowing them to participate in group
activities. This structured routine allowed for them to focus on the dance leader in the front of the room and
provides a workable platform to build upon the activities of the day arts and crafts, prayers, developmentally
appropriate games, and short lectures (15-20 mins) on health issues ( done by each member of our clinical
group). To enhance learning with these clients, teaching props were used to bring teaching to a concrete level.
The lively question and answer session following these weekly lectures were proof that our clients were more
than engaged on a superficial level.
Objective 5: Utilize informational technology when managing individual and families in the community.
This objective was not applicable as computerized documentation was not done at this clinical site.
Objective 6: Demonstrate a commitment to professional development.
Commitment to professional development is important to every aspect of the nursing profession. Particularly
to that of the community health nurse, the need to commit to lifelong learning is of great importance as the
effect of their interventions reaches not only one person, but rather a community of citizens. With this in
mind, planning care by way of a teaching plan, as I did, requires a focus on evidence based practice as it
impacts current statistics on many health related issues.. Evaluating learning outcomes not only assisted with
assessing the impact of teaching strategies, it also reflected on me the effect I have as an educator within the
community Also, as an independent practitioner in the community, a comprehensive understanding of ones
self via self-evaluation and the health issues facing the community helps to give direction about how to
address the challenges faced by a community health nurse. One such challenge is allocating resources for
community that would help to ameliorate health disparities.
Objective 7: Incorporate professional nursing standards and accountability into practice.
I incorporated nursing standards and accountability into practice by first starting out with the ethical code of
beneficence. The nursing process was used in developing a teaching plan which was examined for research
based content quality. This content quality was further scrutinized via collaboration from my colleagues within
my clinical group and clinical instructor. In evaluating learning outcomes for my client, I was able to evaluate
my own professional practice and in turn, assess my adherence to standards of professional performance.
Objective 8: Collaborate with clients, significant support persons and members of the health care team.
Collaboration with health care team, clients, and significant support persons helped me to attain the goals of
my interventions. In so doing, the quality of care for my client was significantly improved. In one instance for
example, a client I was working with at my clinical site, was absent for a few days. While speaking to him in the
dining room after his breakfast, I noticed that his shirt was wet from the beverage he was drinking. This was an
interesting observation for me as I have never seen him in this condition before. Upon further inquiry, I
learned of his sudden visual compromise. This posed an immediate safety threat for him, one the health care
team knew nothing of. I followed up with a phone call to his spouse (significant support person) in the
presence of the nurse in charge to verify whether she was aware of this finding and if he was being followed
up by his primary care physician. His care plan was immediately modified such that his safety can be
maintained while his condition is being managed.
Objective 9: Recognize the impact of economic, political, social, and demographic forces that affect the
delivery of health care services.
This objective was partially met in that even though the impact of the economic, political, social, and
demographic forces were fulminant in the reality of this great recession, the focus on quality of care has been
blurred by gaps in maintaining continuity of care. This was highly evident with the apparent safety risk the
client mentioned earlier was exposed to. So the only avenue of advocating for this client was to engage his
significant support person to keep the adult health daycare center up to date with changes in his health. As far
as reaching out to outside resources, I was unable to as this clinical site has its own internal resources its
people.
In conclusion, my view of nursing as a profession prior to this course was that of hospital nursing. This course
helped me to realize the impact that nurses can have on a community in terms of making policies that combat
health disparities in any community. All they have to do is to know where and how to access resources for
their client the community. Also this course reaffirmed the responsibility nurses have in committing
themselves as a lifelong learner. Their role as educator regardless of setting drives this need. Now I can
imagine new possibilities as a registered nursing professional that I could apply my clinical background as a
hospital nurse to. Professionally, I have grown to the point where I have no problem bothering a doctor
irrespective of time of day just to advocate for a patient. Similarly, I just need to be comfortable with tapping
resources to go beyond the fences of the hospital.
Вам также может понравиться
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryОт EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryРейтинг: 3.5 из 5 звезд3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)От EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Рейтинг: 4.5 из 5 звезд4.5/5 (119)
- Never Split the Difference: Negotiating As If Your Life Depended On ItОт EverandNever Split the Difference: Negotiating As If Your Life Depended On ItРейтинг: 4.5 из 5 звезд4.5/5 (838)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaОт EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaРейтинг: 4.5 из 5 звезд4.5/5 (265)
- The Little Book of Hygge: Danish Secrets to Happy LivingОт EverandThe Little Book of Hygge: Danish Secrets to Happy LivingРейтинг: 3.5 из 5 звезд3.5/5 (399)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyОт EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyРейтинг: 3.5 из 5 звезд3.5/5 (2219)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeОт EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeРейтинг: 4 из 5 звезд4/5 (5794)
- Team of Rivals: The Political Genius of Abraham LincolnОт EverandTeam of Rivals: The Political Genius of Abraham LincolnРейтинг: 4.5 из 5 звезд4.5/5 (234)
- The Emperor of All Maladies: A Biography of CancerОт EverandThe Emperor of All Maladies: A Biography of CancerРейтинг: 4.5 из 5 звезд4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreОт EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreРейтинг: 4 из 5 звезд4/5 (1090)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersОт EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersРейтинг: 4.5 из 5 звезд4.5/5 (344)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceОт EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceРейтинг: 4 из 5 звезд4/5 (894)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureОт EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureРейтинг: 4.5 из 5 звезд4.5/5 (474)
- Conflict Management ReportДокумент7 страницConflict Management ReportAnn Michelle Tarrobago100% (1)
- The Unwinding: An Inner History of the New AmericaОт EverandThe Unwinding: An Inner History of the New AmericaРейтинг: 4 из 5 звезд4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)От EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Рейтинг: 4 из 5 звезд4/5 (98)
- Anti-Drug Campaign SpeechДокумент2 страницыAnti-Drug Campaign SpeechGracel Gonzaga Eviota91% (11)
- Schema Focused TherapyДокумент34 страницыSchema Focused TherapyKen Murray100% (6)
- Morality and Ethics - BasicsДокумент23 страницыMorality and Ethics - BasicsAnn Michelle Tarrobago50% (2)
- Sorry Wrong Number by Lucille FletcherДокумент25 страницSorry Wrong Number by Lucille FletcherAnn Michelle Tarrobago100% (6)
- Emergency NursingДокумент19 страницEmergency Nursingshenric16Оценок пока нет
- Introduction To HospitalsДокумент15 страницIntroduction To Hospitalskapgarg50% (2)
- Orthopedic NursingДокумент202 страницыOrthopedic NursingRigo76801100% (3)
- NCLEX Test CVA, Neuro 24Документ19 страницNCLEX Test CVA, Neuro 24Ann Michelle TarrobagoОценок пока нет
- Motivation TheoriesДокумент18 страницMotivation TheoriesMM Ayehsa Allian Schück100% (1)
- DECS Form 178ORIGINALДокумент1 страницаDECS Form 178ORIGINALJhon FurioОценок пока нет
- Role of Clinician in AssessmentДокумент9 страницRole of Clinician in AssessmentTamara Platenkamp100% (1)
- PNI Psychosocial Factors that Impact Immune SystemДокумент23 страницыPNI Psychosocial Factors that Impact Immune SystemAnn Michelle TarrobagoОценок пока нет
- CANCER NSG QuestionsДокумент43 страницыCANCER NSG QuestionsAnn Michelle Tarrobago83% (6)
- Nutrition in The Critically Ill PatientДокумент13 страницNutrition in The Critically Ill PatientnainazahraОценок пока нет
- Maternal and Child Nursing QuestionsДокумент87 страницMaternal and Child Nursing QuestionsAnn Michelle Tarrobago50% (2)
- Pathophysiology (Risk Factors & Symptoms)Документ20 страницPathophysiology (Risk Factors & Symptoms)Ann Michelle TarrobagoОценок пока нет
- ExpoДокумент5 страницExpoAnn Michelle TarrobagoОценок пока нет
- Planning ProcessДокумент10 страницPlanning ProcessAnn Michelle TarrobagoОценок пока нет
- PediatricsДокумент21 страницаPediatricsAnn Michelle TarrobagoОценок пока нет
- Pathophysiology (Risk Factors & Symptoms)Документ20 страницPathophysiology (Risk Factors & Symptoms)Ann Michelle TarrobagoОценок пока нет
- Assessing male infertility and significance of sperm motilityДокумент94 страницыAssessing male infertility and significance of sperm motilityAnn Michelle Tarrobago100% (1)
- Introduction To OrthopaedicsДокумент53 страницыIntroduction To OrthopaedicsAnn Michelle TarrobagoОценок пока нет
- Elements of PoetryДокумент14 страницElements of PoetryAnn Michelle TarrobagoОценок пока нет
- Orthopedic Lecture 06Документ131 страницаOrthopedic Lecture 06Ann Michelle TarrobagoОценок пока нет
- Neuro PlasticityДокумент20 страницNeuro PlasticityAnn Michelle TarrobagoОценок пока нет
- Well-balanced diet and routine tests orderedДокумент8 страницWell-balanced diet and routine tests orderedAnn Michelle TarrobagoОценок пока нет
- I Can Teach and Guide But Not Control Your LifeДокумент1 страницаI Can Teach and Guide But Not Control Your LifeAnn Michelle TarrobagoОценок пока нет
- Leadership StyleДокумент3 страницыLeadership StyleAnn Michelle TarrobagoОценок пока нет
- Gastroenteritis Bronchopneumonia Ear InfectionДокумент34 страницыGastroenteritis Bronchopneumonia Ear InfectionAnn Michelle TarrobagoОценок пока нет
- Goldsman ScoreДокумент1 страницаGoldsman ScoreAnn Michelle TarrobagoОценок пока нет
- NCLEX Review About Immune System Disorders 24Документ12 страницNCLEX Review About Immune System Disorders 24Ann Michelle Tarrobago67% (3)
- NarrativeДокумент1 страницаNarrativeAnn Michelle TarrobagoОценок пока нет
- 2015 Calendar Mini MonthДокумент12 страниц2015 Calendar Mini MonthCherilyn SaagundoОценок пока нет
- June 2015 CalendarДокумент1 страницаJune 2015 CalendarAnn Michelle TarrobagoОценок пока нет
- Indian Calendar With HolidaysДокумент12 страницIndian Calendar With HolidayssmiledepakОценок пока нет
- Definition of DXДокумент2 страницыDefinition of DXAnn Michelle TarrobagoОценок пока нет
- Ethical Issues at The End of LifeДокумент24 страницыEthical Issues at The End of Lifeorderstuff36160100% (1)
- Treatment of Child Victims of Abuse and NeglectДокумент18 страницTreatment of Child Victims of Abuse and NeglectSri Harsha KothapalliОценок пока нет
- Thalassemia: BY: Deddy Ramadhan G2A016098Документ11 страницThalassemia: BY: Deddy Ramadhan G2A016098deddy ramadhanОценок пока нет
- NSK 2013 A00-000-001 enДокумент26 страницNSK 2013 A00-000-001 enThato Merapelo PuleОценок пока нет
- Parkland Formula For Burns Calculated DecisionsДокумент2 страницыParkland Formula For Burns Calculated DecisionsJulia Ines ObregonОценок пока нет
- Medicinal Plants of Sheringal Valley, Dir Upper, KPK, Pakistan PDFДокумент3 страницыMedicinal Plants of Sheringal Valley, Dir Upper, KPK, Pakistan PDFFaiz Ul HaqОценок пока нет
- Catalogue: ProductДокумент24 страницыCatalogue: ProductRavi KrishnanОценок пока нет
- AminoglycosidesДокумент6 страницAminoglycosidesLlosa JuneОценок пока нет
- S - "Sakit Ahong Tinahian" As Verbalized byДокумент6 страницS - "Sakit Ahong Tinahian" As Verbalized bylandilinoОценок пока нет
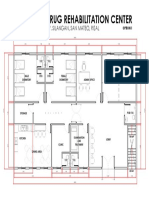
- Proposed Drug Rehabilitation Center: Monterey Sudb., Brgy. Silangan, San Mateo, RizalДокумент1 страницаProposed Drug Rehabilitation Center: Monterey Sudb., Brgy. Silangan, San Mateo, RizalJonathan MazonОценок пока нет
- Fracture of Radius, Ulna, and HumerusДокумент20 страницFracture of Radius, Ulna, and HumerusAmanda Nur Shinta PertiwiОценок пока нет
- Essential medicines certificateДокумент2 страницыEssential medicines certificateAnji KaringuОценок пока нет
- Cognitive Behavioral Model of Clinical Perfectionism Shafran Cooper Fairburn 2002 En-UsДокумент1 страницаCognitive Behavioral Model of Clinical Perfectionism Shafran Cooper Fairburn 2002 En-UsPavlov PicassoОценок пока нет
- Sensory Deprivation and Loss-4Документ32 страницыSensory Deprivation and Loss-4Scott Daniel Phillips100% (1)
- Joella Pregnancy Support GroupДокумент2 страницыJoella Pregnancy Support GroupElle ctrica100% (2)
- Applying Client-Centred Guidelines to Pediatric OTДокумент7 страницApplying Client-Centred Guidelines to Pediatric OTRaphael AguiarОценок пока нет
- Omeprazole, Potassium Chloride, Citicoline, GlimepirideДокумент5 страницOmeprazole, Potassium Chloride, Citicoline, GlimepirideJenivic Empig PuedanОценок пока нет
- Indira GandhiДокумент8 страницIndira GandhiDanisОценок пока нет
- Pharmacology of Interferons: Mechanisms, Indications, and Treatment of Hepatitis CДокумент30 страницPharmacology of Interferons: Mechanisms, Indications, and Treatment of Hepatitis CRam NareshОценок пока нет
- Sustained Release Dosage FormsДокумент9 страницSustained Release Dosage FormsJasdeep KaurОценок пока нет
- The Differences Between Coaching Mentoring Therapy and Counselling PDFДокумент5 страницThe Differences Between Coaching Mentoring Therapy and Counselling PDFghinaОценок пока нет
- COPD, Asthma, and Lung Disease Nursing Assessment QuestionsДокумент8 страницCOPD, Asthma, and Lung Disease Nursing Assessment QuestionsMichael Boado100% (3)
- 3 ConstipationДокумент18 страниц3 Constipationكسلان اكتب اسميОценок пока нет