Академический Документы
Профессиональный Документы
Культура Документы
HP Jan05 Bleed
Загружено:
Syahanim IsmailОригинальное название
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
HP Jan05 Bleed
Загружено:
Syahanim IsmailАвторское право:
Доступные форматы
Review of Clinical Signs
Series Editor: Bernard M. Karnath, MD
Easy Bruising and Bleeding in the Adult
Patient: A Sign of Underlying Disease
Bernard M. Karnath, MD
chief complaint of easy bruising and bleeding
should alert the clinician to the possibility of a
serious underlying disease process. The evaluation includes a careful history and a complete physical examination. As many bleeding disorders are inherited, a detailed family history should also
be obtained. Laboratory investigations should be guided by the clinical impression.
In general, easy bruising is associated with platelet
disorders, whereas easy bleeding is associated with
coagulation disorders. There is significant overlap,
however, and platelet and coagulation disorders may
coexist. Platelet disorders as well as coagulation abnormalities must be considered in any patient with bruising or bleeding that is disproportionate to the offending trauma (Table 1).1 Common complaints associated
with platelet and coagulation disorders include epistaxis, gingival bleeding, menorrhagia, gastrointestinal
bleeding, ecchymosis, purpura, and petechia. Physical
abuse is always a consideration but must not be assumed.2 This article reviews the approach to evaluating
patients who present with easy bruising or bleeding.
Two illustrative cases are presented.
The definitions of petechia, purpura, and ecchymosis differ among sources, but the definitions used here
are as follows: Ecchymoses are large areas of bruising that
occur out of proportion to the offending trauma.
Petechiae are pinpoint (13 mm), nonraised, reddish
purple lesions that result from intradermal or submucous hemorrhage. Purpura are larger (> 3 mm) red to
purple nonblanching lesions that also result from
bleeding into the skin and mucous membranes.
Unlike bruising, petechiae and purpura do not result
from trauma.
APPROACH TO THE PATIENT WITH EASY BRUISING
Bruises are large areas of subcutaneous bleeding.
Bruising is considered abnormal if it is out of proportion to the offending trauma. Not all patients with easy
bruising have a serious underlying disorder, however.
www.turner-white.com
SIGNSEASY BRUISING AND BLEEDING
Easy bruising
Ecchymoses
Purpura
Petechiae
Easy bleeding
Epistaxis
Gastrointestinal/rectal bleeding
Gingival bleeding
Hemarthrosis
Hematuria
Menorrhagia
Prolonged bleeding during surgery/tooth extraction
Senile purpura, seen in elderly patients, is a benign
process caused by capillary fragility associated with
weakened connective tissue and is not a sign of a serious underlying disease. In addition, certain medications, such as aspirin, nonsteroidal anti-inflammatory
drugs (NSAIDs), corticosteroids, and anticoagulants
may be associated with purpura. Bruising restricted to
the lower limbs is usually normal. (This is not always
true, however, as illustrated in the case presented.)
Easy bruising over the trunk, neck, and face warrant
further hematologic evaluation.3 Although easy bruising is more commonly associated with thrombocytopenia, coexistence with coagulation disorders is common.
Clinical Evaluation
The history should focus on the onset of easy bruising as well as a family history of hematologic disorders.
A detailed history of medication use is critical. The
Dr. Karnath is an associate professor of internal medicine, University of
Texas Medical Branch at Galveston, Galveston, TX.
Hospital Physician January 2005
35
Karnath : Easy Bruising and Bleeding : pp. 35 39
Table 1. Clues to the Diagnosis of Easy Bruising and Easy Bleeding
Finding
Easy bruising
Possible Cause
History
Bruising out of proportion to the offending trauma
Platelet disorder
Advanced age
Senile purpura
Family history of easy bruising
Qualitative platelet disorder
Medication use (eg, heparin, warfarin, aspirin, steroids, NSAIDs)
Platelet inhibition, coagulopathy
Physical examination
Easy bleeding
Multiple bruises, petechiae
Severe thrombocytopenia
Lymphadenopathy, splenomegaly
Hematologic malignancy
History
Prolonged bleeding from minimal trauma (eg, minor surgery, tooth
extractions)
Coagulation disorder and/or platelet disorder
Menorrhagia, spontaneous bleeding (eg, epistaxis, hemarthrosis,
hematuria, rectal bleeding)
Coagulation disorder and/or platelet disorder
Family history of easy bleeding
Hemophilia, qualitative platelet disorder
Medications (eg, heparin, warfarin, aspirin, steroids, NSAIDs)
Platelet inhibition, coagulopathy
Physical examination
Hemarthrosis
Hemophilia
Spider angiomata, scleral icterus, ascites, gynecomastia
Chronic liver disease
NSAID = nonsteroidal anti-inflammatory drug.
physical examination is essential in elucidating an
underlying cause. Take note of which areas are
bruised. Bruises on the lower extremities are not considered quite as abnormal as bruising elsewhere, but
petechiae, which are typically seen on the lower extremities, are a sign of severe thrombocytopenia. Evidence of hematologic malignancy should be sought,
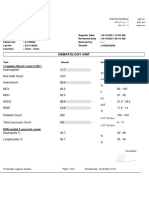
including lymphadenopathy and splenomegaly. Laboratory investigations should include a complete blood
count, platelet count, prothrombin time (PT), and partial thromboplastin time (PTT). Hematologic malignancy may be uncovered with a complete blood count
with peripheral smear.
mune disorders (including immune thrombocytopenic purpura).
Qualitative platelet disorders can be either congenital or acquired.4,5 Patients with qualitative platelet disorders have prolonged bleeding times despite a normal platelet count. A family history is important in
evaluating a patient with a qualitative platelet disorder.
Congenital disorders include Glanzmanns thrombasthenia and Bernard-Soulier syndrome, both of which
are rare autosomal recessive disorders. Acquired
platelet disorders can result from uremia and certain
drugs (eg, aspirin, NSAIDs). Uremia causes abnormal
platelet function by unknown mechanisms.
Platelet Disorders Associated with Easy Bruising
Platelet disorders can be divided into quantitative
and qualitative abnormalities.4,5 Quantitative disorders
are characterized by thrombocytopenia resulting from
sequestration, peripheral destruction, or decreased
production of platelets (Table 2).4,5 Bone marrow disorders causing thrombocytopenia include aplastic anemia, myelodysplasia, and hematologic malignancies.
Chronic alcoholism can also cause marrow suppression. Nonmarrow disorders causing thrombocytopenia
include disseminated intravascular coagulation, thrombotic thrombocytopenic purpura, hemolytic uremic
syndrome, liver failure, hypersplenisms, and autoim-
Illustrative Case
Case presentation. A 50-year-old woman presents
with a 3-week history of easy bruising and fatigue.
Physical examination is significant for an obese woman
with scattered areas of ecchymosis predominantly on
the lower extremities (Figure 1). Laboratory examination reveals a leukocyte count of 200 103/mm3 (normal, 4.810.8 103/mm3), hemoglobin concentration
of 9 g/dL (normal, 12.015.5 g/dL), and a platelet
count of 20 10 3 /mm 3 (normal, 150 450
103/mm3). A differential cell count shows 83% blasts.
Results of coagulation studies, including PT and activated PTT (aPTT), are normal.
36 Hospital Physician January 2005
www.turner-white.com
Karnath : Easy Bruising and Bleeding : pp. 35 39
Table 2. Causes of Thrombocytopenia
Decreased platelet production
Leukemia
Lymphoma
Aplastic anemia
Myelodysplasia
Chronic alcoholism
Vitamin B12 deficiency
Folic acid deficiency
Splenic sequestration
Cirrhosis with congestive splenomegaly
Myelofibrosis with splenomegaly
Figure 1. Area of ecchymosis (a large bruise).
Nonmarrow disorders
Idiopathic thrombocytopenic purpura
HIV infection
Drugs (heparin, quinidine, quinine, sulfa-containing)
Disseminated intravascular coagulation (cancer, sepsis)
Thrombotic thrombocytopenic purpura
Hemolytic-uremic syndrome
Paroxysmal nocturnal hemoglobinuria
Discussion. In this case, a middle-aged woman presents with nonspecific complaints of easy bruising and
fatigue. She reports that the largest bruise, which is on
her left thigh, is the result of insignificant contact with
a waste can. The resulting bruise is out of proportion
to the force of contact. Although the patient has severe
thrombocytopenia, petechiae are not present. Results
of coagulation studies are normal, but the complete
blood count reveals a markedly elevated leukocyte
count, anemia, and severe thrombocytopenia. The
peripheral smear shows a predominance of blasts.
Acute leukemia, specifically acute myelogenous leukemia, was subsequently diagnosed.
Acute myelogenous leukemia accounts for 80% of
acute leukemias in adults and acute lymphocytic
leukemia accounts for the remaining 20%.6 Acute lymphocytic leukemia is primarily a childhood leukemia.
The median age of patients with acute myelogenous
leukemia is about 50 years.6 Approximately one third
of patients present with easy bruising or easy bleeding.
The leukocyte count is elevated and blasts are seen on
the peripheral blood smear. Moderate anemia is present
and the platelet count is often less than 20 103/mm3.
APPROACH TO THE PATIENT WITH EASY BLEEDING
A bleeding disorder should be considered in a
patient with easy bleeding, recurrent epistaxis, menorrhagia, hemarthrosis, prolonged bleeding during oper-
www.turner-white.com
ations and tooth extractions, hematuria, or rectal
bleeding. Although any of these conditions can occur
alone, spontaneous bleeding from multiple sites (eg,
epistaxis, hematuria, rectal bleeding) further raises the
suspicion of a bleeding disorder. A bleeding disorder
should be especially considered in a patient with any of
the aforementioned conditions together with a family
history of a bleeding disorder. In general, easy bleeding is associated with coagulation disorders, although
coexistence with platelet disorders can occur. Qualitative platelet disorders are more likely to cause easy
bleeding than quantitative disorders unless severe.
The history should focus on the onset of easy bleeding as well as a family history of hematologic disorders.
A long history of easy bleeding is an indication of an
inherited disorder, whereas acute onset of easy bleeding is indicative of an acquired disorder. A detailed history of medication use is essential. Anticoagulants such
as warfarin and heparin can prolong the PT and PTT.
Aspirin and NSAIDs can prolong the bleeding time by
inhibiting platelet aggregation. Take note of the sites
of bleeding. Spontaneous bleeding from multiple sites
is a red flag for underlying coagulopathy.
The physical examination is useful in finding clues
to an underlying cause. Lymphadenopathy and splenomegaly are signs of possible hematologic malignancy.
Chronic liver disease can lead to easy bleeding due to
depletion of vitamin Kdependent clotting factors.
Signs of chronic liver disease include scleral icterus,
spider angiomata, gynecomastia, palmar erythema,
and digital clubbing. Laboratory investigation of patients with easy bleeding should include a complete
blood count, platelet count, PT, aPTT, bleeding time,
and liver function tests.
Coagulation Disorders Associated with Easy Bleeding
Coagulation disorders can be either inherited or
Hospital Physician January 2005
37
Karnath : Easy Bruising and Bleeding : pp. 35 39
Table 3. Causes of Coagulation Disorders
Intrinsic pathway
Prekallikrein
Extrinsic pathway
High-molecular-weight
(Tissue factor pathway)
kininogen (HMWK)
Factor XII
Tissue factor (factor III)
Factor XI
Factor VII
Factor IX
Factor VIII
Common pathway
Factor X
Factor V
Factor II (prothrombin)
Fibrinogen
Factor XIII
Causes of prolonged prothrombin time
Liver disease
Vitamin K deficiency
Warfarin
Factor VII deficiency
Causes of prolonged partial thromboplastin time
Factor deficiencies:
Factor XII
Factor XI
Factor VIII (hemophilia A)
Factor IX (hemophilia B)
Figure 2. A simplified version of the coagulation pathway
showing the involved clotting factors.
von Willebrands disease
Heparin administration
Lupus anticoagulant
Acquired factor inhibitors
acquired. Inherited disorders are likely to manifest in
childhood whereas acquired disorders present later. In
evaluating a patient for coagulation disorders, a careful
history should include inquiries about excessive bleeding during previous procedures such as tooth extractions. Hereditary disorders of coagulation can be elicited through a detailed family history.
Laboratory evaluation of the coagulation pathways
incorporates 4 tests: PT, aPTT, thrombin time, and fibrinogen assays. The aPTT and PT are the most commonly performed tests of hemostasis. An understanding of the coagulation cascade is important (Figure 2).
The extrinsic, or tissue factor, pathway is the mechanism by which coagulation is initiated in response to
tissue trauma. In this pathway, released tissue factor
activates factor VII.5,8 The intrinsic pathway is activated
when blood comes in contact with an injured vessel
wall, activating factor XII.5,8 Both pathways proceed to
a common pathway that leads to the formation of a
clot by cross-linking of fibrin.
Causes of Prolonged PT
The PT evaluates the extrinsic pathway of coagulation (factors II, V, VII, X, and fibrinogen). Causes of
prolonged PT include liver disease, vitamin K deficiency, warfarin, and factor VII deficiency (Table 3).
The PT has a normal range of 11 to 15 seconds. The
clotting factors are synthesized in the liver; patients
with liver failure, therefore, whether acute or chronic,
are likely to develop coagulopathy evidenced by a
prolonged PT disproportionate to the aPTT. Patients
on prolonged antibiotic therapy are also prone to
developing coagulopathy secondary to deficiency of
the vitamin Kdependent factors (factors II, VII, IX,
38 Hospital Physician January 2005
and X). The PT is used to monitor patients on warfarin therapy.
Causes of Prolonged aPTT
The aPTT evaluates the intrinsic coagulation pathway. The test is most sensitive for factors VIII, IX, XI,
and XII. The most common cause of prolonged aPTT
is incorrect collection of blood through an indwelling
catheter that has been flushed with heparin. The aPTT
has a normal range of 22 to 38 seconds. The aPTT test
is preferred to the original PTT test.
Hemophilia A (factor VIII deficiency) is the most
common hereditary disorder of blood coagulation. The
next most common disorders are hemophilia B (factor
IX deficiency) and von Willebrands disease. Both
hemophilia A and hemophilia B are X-linked recessive
disorders only males are clinically affected and
females may be carriers. von Willebrands disease is an
autosomal dominant disorder. Acquired factor inhibitors (autoantibodies) can also develop.9 The most
common acquired inhibitor is that against factor VIII.
Illustrative Case
Case presentation. A 70-year-old man presents with
a 2-week history of hematuria, melena, and easy bruising and bleeding from minor trauma. His past medical
history is otherwise unremarkable. Physical examination is remarkable for a thin elderly man with scattered areas of ecchymosis. Rectal examination reveals
guaiac-positive stool. Laboratory examination reveals a
leukocyte count of 8.0 103/mm3, hemoglobin of
www.turner-white.com
Karnath : Easy Bruising and Bleeding : pp. 35 39
8 g/dL, platelet count of 170 10 3/mm 3, PT of
11 seconds (normal, 1115 seconds), and an aPTT of
84 seconds (normal, 2238 seconds). Laboratory results from 1 year ago (including coagulation studies)
are normal.
Discussion. In this case, an elderly man presents
with episodes of spontaneous bleeding and easy bruising. His laboratory results from 1 year ago are normal,
thereby providing evidence that his coagulopathy is
newly acquired. A family history for bleeding disorders
is negative. The patient has an isolated elevation of the
aPTT. An acquired inhibitor was suspected.
Spontaneous inhibitors are autoantibodies to coagulation factors.8 The most common factor involved is factor VIII. Factor VIII inhibition prolongs the aPTT but
not the PT. A simple test that checks for the presence of
an inhibitor (an inhibitor screen) can be performed by
incubating mixtures of patient plasma and normal plasma. Failure of the normal plasma to correct the prolonged aPTT indicates the presence of an inhibitor.
CONCLUSION
Although easy bruising and easy bleeding are often
normal, they can be ominous signs of a serious underlying disease process. Platelet disorders and coagulation disorders must be considered. A detailed family
history is important because many bleeding disorders
are inherited. Laboratory examination must include a
complete blood count and coagulation studies, including PT and aPTT.
HP
REFERENCES
1. Sham RL, Francis CW. Evaluation of mild bleeding disorders and easy bruising. Blood Rev 1994;8:98104.
2. Male I, Kenney I, Appleyard C, Evans N. Neoplasia masquerading as physical abuse. In: Child abuse review:
Journal of the British Association for the Study and
Prevention of Child Abuse and Neglect. England: John
Wiley; 2000:1427.
3. Vora A, Makris M. Personal practice: an approach to
investigation of easy bruising. Arch Dis Child 2001;
84:48891.
4. Goebel RA. Thrombocytopenia. Emerg Med Clin North
Am 1993;11:44564.
5. Angelos MG, Hamilton GC. Coagulation studies: prothrombin time, partial thromboplastin time, bleeding
time. Emerg Med Clin North Am 1986;4:95113.
6. Devine SM, Larson RA. Acute leukemia in adults: recent
developments in diagnosis and treatment. CA Cancer J
Clin 1994;44:32652.
7. Triplett DA. Coagulation and bleeding disorders: review
and update. Clin Chem 2000;46(8 Pt 2):12609.
8. Dahlback B. Blood coagulation. Lancet 2000;355:
162732.
9. Green D. Spontaneous inhibitors to coagulation factors.
Clin Lab Haematol 2000;22 Suppl 1:2132.
Copyright 2005 by Turner White Communications Inc., Wayne, PA. All rights reserved.
www.turner-white.com
Hospital Physician January 2005
39
Вам также может понравиться
- ThrombocytopeniaДокумент9 страницThrombocytopenia8pvz96ktd9Оценок пока нет
- Bleeding Disorder (Paediatrics)Документ95 страницBleeding Disorder (Paediatrics)Nurul Afiqah Mohd YusoffОценок пока нет
- 5hematologic DiseaseДокумент40 страниц5hematologic DiseaseAli SherОценок пока нет
- 1 s2.0 S0899588513000701 Main PDFДокумент8 страниц1 s2.0 S0899588513000701 Main PDFRicki HanОценок пока нет
- Anasarca - StatPearls - NCBI BookshelfДокумент5 страницAnasarca - StatPearls - NCBI Bookshelfemail lombaОценок пока нет
- Peripheral Arterial Disease: AbnetДокумент142 страницыPeripheral Arterial Disease: AbnetAbnet WondimuОценок пока нет
- BUERGER's Inavasc IV Bandung 8 Nov 2013Документ37 страницBUERGER's Inavasc IV Bandung 8 Nov 2013Deviruchi GamingОценок пока нет
- Simple Purpura (Easy Bruising Syndrome)Документ4 страницыSimple Purpura (Easy Bruising Syndrome)Rebecca WongОценок пока нет
- Essential ThrombocytosisДокумент12 страницEssential ThrombocytosisGd Padmawijaya100% (1)
- ThrombocytopeniaДокумент4 страницыThrombocytopeniaValerrie NgenoОценок пока нет
- Anemi Aplastik Dan MielodisplasiaДокумент34 страницыAnemi Aplastik Dan MielodisplasiaRoby KieranОценок пока нет
- roDAKS Chapter 37Документ3 страницыroDAKS Chapter 37John DavidОценок пока нет
- Data Interpretation For Medical StudentДокумент18 страницData Interpretation For Medical StudentWee K WeiОценок пока нет
- What Is ThrombocytosisДокумент3 страницыWhat Is ThrombocytosisFred C. MirandaОценок пока нет
- Upper Gastrointestinal Bleeding.Документ13 страницUpper Gastrointestinal Bleeding.Gieselle Scott100% (1)
- Haemolytic Anaemia and Sickle Cell DiseaseДокумент26 страницHaemolytic Anaemia and Sickle Cell DiseaseGideon HaburaОценок пока нет
- Hemorrhage Lec 1Документ30 страницHemorrhage Lec 1balachris64Оценок пока нет
- Aortoiliac Occlusive DiseaseДокумент37 страницAortoiliac Occlusive Diseasewolff_512Оценок пока нет
- Hemorrhagic Shock Clinical Presentation: HistoryДокумент12 страницHemorrhagic Shock Clinical Presentation: HistoryVictor Hugo SchneiderОценок пока нет
- Why Does My Patient Have Thrombocytopenia PDFДокумент22 страницыWhy Does My Patient Have Thrombocytopenia PDFElena Villarreal100% (1)
- HemorrhageДокумент8 страницHemorrhageammarmashalyОценок пока нет
- Blue Toe SyndromeДокумент20 страницBlue Toe SyndromeDaeng MakelloОценок пока нет
- 5.the Kidney - 5Документ19 страниц5.the Kidney - 5madhuОценок пока нет
- Arterial Stenosis or OcclusionДокумент83 страницыArterial Stenosis or OcclusionMuhammad Umer Farooq NadeemОценок пока нет
- Essential Thrombocytemia: Rahmawati Minhajat A. Fachruddin BenyaminДокумент12 страницEssential Thrombocytemia: Rahmawati Minhajat A. Fachruddin BenyaminHajrahPalembanganОценок пока нет
- Osler-Weber-Rendu Disease - StatPearls - NCBI BookshelfДокумент4 страницыOsler-Weber-Rendu Disease - StatPearls - NCBI BookshelfanaОценок пока нет
- Kuliah Platelets DisordersДокумент22 страницыKuliah Platelets DisordersDesi AdiyatiОценок пока нет
- 3 Renal Vascular Disease 3Документ46 страниц3 Renal Vascular Disease 3Coy NuñezОценок пока нет
- Anemia Hip Pain Sickle Cell DiseaseДокумент9 страницAnemia Hip Pain Sickle Cell DiseasePerplexed CeleryОценок пока нет
- The Spleen: Schwartz's Principles of Surgery 11th EdДокумент54 страницыThe Spleen: Schwartz's Principles of Surgery 11th EdaddelinsОценок пока нет
- Aplastic AnemiaДокумент29 страницAplastic AnemiaAshish SoniОценок пока нет
- Deep Vein ThrombosisДокумент43 страницыDeep Vein Thrombosisoctaviana_simbolonОценок пока нет
- Hematologic Disorders: JeffreyДокумент582 страницыHematologic Disorders: JeffreyPalak GuptaОценок пока нет
- The Spleen: Schwartz's Principles of Surgery 11th EdДокумент54 страницыThe Spleen: Schwartz's Principles of Surgery 11th EdMuhammad Fhandeka IsrarОценок пока нет
- Manejo Melena 2004Документ6 страницManejo Melena 2004Wilmer JimenezОценок пока нет
- Ischemic Limb Gangrene With PulsesДокумент14 страницIschemic Limb Gangrene With PulsesJustin Ryan TanОценок пока нет
- Acute Gastrointestinal Bleeding Upper GI BleedingДокумент18 страницAcute Gastrointestinal Bleeding Upper GI BleedingAldwin AyuyangОценок пока нет
- ThrombocytopeniaДокумент9 страницThrombocytopeniaamjad_muslehОценок пока нет
- Peripheral Arterial OcclusionДокумент50 страницPeripheral Arterial Occlusionshefalika mandremОценок пока нет
- Tromboembolismo FelinoДокумент18 страницTromboembolismo FelinoFelipeОценок пока нет
- Diagnostic Approach To The Patient With CirrhosisДокумент17 страницDiagnostic Approach To The Patient With CirrhosisXimenaEspinaОценок пока нет
- Hemostasis - Hematology BlockДокумент40 страницHemostasis - Hematology BlockamandaОценок пока нет
- Aplastic AnemiaДокумент9 страницAplastic AnemiaGaluh Dyah PrameswariОценок пока нет
- Jurnal: Lila Esi Mustika, Amkg NIK: PK2013050Документ11 страницJurnal: Lila Esi Mustika, Amkg NIK: PK2013050lilaОценок пока нет
- Introduction To Vascular SurgeryДокумент13 страницIntroduction To Vascular Surgeryapi-3858544100% (1)
- Disorder of PlateletsДокумент27 страницDisorder of PlateletsRoby KieranОценок пока нет
- ENDOCRINE HYPERTENSION. A Number of Hormonal Secretions May Produce Secondary HyДокумент5 страницENDOCRINE HYPERTENSION. A Number of Hormonal Secretions May Produce Secondary HyIsak ShatikaОценок пока нет
- Massive Bleeding/Major Hemorrhage: DefinitionДокумент6 страницMassive Bleeding/Major Hemorrhage: DefinitionGerome Isaiah RabangОценок пока нет
- Arterial InsufficiencyДокумент48 страницArterial InsufficiencySyAmil MeNzaОценок пока нет
- Aplastic Anemia - An Overview: DR Aniruddh Shrivastava Guided By: DR S.H. Talib SIRДокумент42 страницыAplastic Anemia - An Overview: DR Aniruddh Shrivastava Guided By: DR S.H. Talib SIRdoctoranswerit_84161Оценок пока нет
- PVDДокумент7 страницPVDmiss RNОценок пока нет
- Venous Thromboembolic DiseaseДокумент27 страницVenous Thromboembolic DiseaseAndra BauerОценок пока нет
- Lo Minggu 2Документ16 страницLo Minggu 2inaseptОценок пока нет
- 10.21.09 Jenkins TTPДокумент16 страниц10.21.09 Jenkins TTPOdiliaDeaNovenaОценок пока нет
- Chapter 146excessive Bleeding and BruisingДокумент7 страницChapter 146excessive Bleeding and BruisinghgpОценок пока нет
- Penatalaksanaan CAPДокумент31 страницаPenatalaksanaan CAPridhoОценок пока нет
- Asepsis and Infection ControlДокумент24 страницыAsepsis and Infection Controlabdisalaan hassanОценок пока нет
- Insuficienta Renala Acuta, Leziunea Acuta RenalaДокумент40 страницInsuficienta Renala Acuta, Leziunea Acuta RenalaLeoveanu MirelОценок пока нет
- Makalah Leigh Disease by Boys KДокумент6 страницMakalah Leigh Disease by Boys KAzizul HakimОценок пока нет
- 1-29-20 Diabetes Protocol Draft With Pandya and Alvarez EditsДокумент12 страниц1-29-20 Diabetes Protocol Draft With Pandya and Alvarez Editsapi-552486649Оценок пока нет
- ShouldiceДокумент16 страницShouldiceAbdullah AhmedОценок пока нет
- Homeopathic ImmunizationДокумент53 страницыHomeopathic Immunizationalex100% (2)
- Case Study UrtiДокумент9 страницCase Study UrtiRonica GonzagaОценок пока нет
- Karya - KTI - Poltekkes Kemenkes SurakartaДокумент11 страницKarya - KTI - Poltekkes Kemenkes Surakartasheenazz •Оценок пока нет
- Review Material Exam TypeДокумент9 страницReview Material Exam TypeFelimon BugtongОценок пока нет
- Congenital Anomalies and Variations of The Bile and Pancreatic Ducts - Magnetic Resonance Cholangiopancreatography Findings, Epidemiology and Clinical SignificanceДокумент19 страницCongenital Anomalies and Variations of The Bile and Pancreatic Ducts - Magnetic Resonance Cholangiopancreatography Findings, Epidemiology and Clinical SignificanceRoberto HernandezОценок пока нет
- D Dimer Test in VTEДокумент35 страницD Dimer Test in VTEscribmedОценок пока нет
- Letting Go by Atul GawandeДокумент18 страницLetting Go by Atul Gawandetakoyakilovers100% (2)
- Renal NursinglДокумент36 страницRenal NursinglgireeshsachinОценок пока нет
- Microbiology: Pathogenic Gram-Positive Cocci (Streptococcus)Документ26 страницMicrobiology: Pathogenic Gram-Positive Cocci (Streptococcus)Shuler0071Оценок пока нет
- Perineal Techniques During The Second Stage of Labour For Reducing Perineal Trauma (Review)Документ118 страницPerineal Techniques During The Second Stage of Labour For Reducing Perineal Trauma (Review)Ppds ObgynОценок пока нет
- Thrombocytopenia: Decreased Production Increased Destruction Sequestration PseudothrombocytopeniaДокумент43 страницыThrombocytopenia: Decreased Production Increased Destruction Sequestration PseudothrombocytopeniaDea Tasha MeicitaОценок пока нет
- Temporal Bone Radiology ReadyДокумент136 страницTemporal Bone Radiology Readyadel madanyОценок пока нет
- What Is-Thrombocythemia and ThrombocytosisДокумент4 страницыWhat Is-Thrombocythemia and ThrombocytosisFred C. MirandaОценок пока нет
- Difference Between Serum and PlasmaДокумент2 страницыDifference Between Serum and PlasmaCynthia Adeline SОценок пока нет
- Spiggle & Theis BrochureДокумент8 страницSpiggle & Theis BrochureHaag-Streit UK (HS-UK)Оценок пока нет
- ANC ModuleДокумент103 страницыANC ModulePreeti ChouhanОценок пока нет
- Hematology Unit: Complete Blood Count (CBC)Документ2 страницыHematology Unit: Complete Blood Count (CBC)Rasha ElbannaОценок пока нет
- MCQs in para (With Answers)Документ20 страницMCQs in para (With Answers)janiceli020785% (26)
- BreechДокумент2 страницыBreechBrel KirbyОценок пока нет
- NCP Ko BabyДокумент3 страницыNCP Ko BabyDaniel ApostolОценок пока нет
- Intramedullary Spinal Cord Tumors: Part II - Management Options and OutcomesДокумент10 страницIntramedullary Spinal Cord Tumors: Part II - Management Options and OutcomeszixzaxoffОценок пока нет
- Groove Pancreatitis - Cause of Recurrent PancreatitisДокумент7 страницGroove Pancreatitis - Cause of Recurrent PancreatitisroxxanaОценок пока нет
- Preterm Neonate VS AssessmentДокумент10 страницPreterm Neonate VS AssessmentggggangОценок пока нет
- Blocked Goat Urolithiasis HandoutДокумент22 страницыBlocked Goat Urolithiasis Handoutapi-262327869100% (1)