Академический Документы
Профессиональный Документы
Культура Документы
Introduction To ACT
Загружено:
Ran AlmogОригинальное название
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Introduction To ACT
Загружено:
Ran AlmogАвторское право:
Доступные форматы
CBPRA-00427; No of Pages 9: 4C
Available online at www.sciencedirect.com
Cognitive and Behavioral Practice xx (2012) xxx-xxx
www.elsevier.com/locate/cabp
SPECIAL SERIES
Acceptance and Commitment Therapy
Series Editor: Michael P. Twohig
Introduction: The Basics of Acceptance and Commitment Therapy
Michael P. Twohig, Utah State University
This is the introductory article to a special series in Cognitive and Behavioral Practice on Acceptance and Commitment Therapy
(ACT). Instead of each article herein reviewing the basics of ACT, this article contains that review. This article provides a description of
where ACT fits within the larger category of cognitive behavior therapy (CBT): CBT is an overarching term for a whole cluster of
therapies, and ACT is one of many forms of CBT. Functional contextualism and how it informs ACT is briefly reviewed. The behavior
analytic account of cognition that informs ACT, relational frame theory (RFT), and rule-governed behavior are covered. Psychological
flexibility and the 6 resulting psychological processes of change (acceptance, defusion, being present, self as context, values, and
committed action) are described. The empirical support for ACT and its related model are presented. Finally, characteristics of the ACT
model, including its therapeutic approach, desired outcomes, and processes of change, are reviewed.
special series on Acceptance and Commitment
Therapy (ACT) contains eight empirical papers on
the efficacy of ACT, its target processes, or how to administer it. Rather than having each author review the basic
concepts and terms used in ACT, this article will serve that
purpose. This article describes where ACT fits in the
larger field of CBT; the philosophical model on which
ACT is based, functional contextualism; the behavior
analytic account of cognition that informs ACT, relational
frame theory (RFT) and rule-governed behavior; the psychological construct that this model addresses, psychological flexibility; the empirical support for ACT and its
related model; and characteristics of the ACT model,
including its therapeutic approach, desired outcomes,
and processes of change.
HIS
ACT as a Type of CBT
There are many types of CBT, including traditional
cognitive therapy presented by Dr. Aaron Beck, exposure
with response prevention, dialectical behavior therapy,
schema therapy, and motivational interviewingto name
only a few. Because a large enough group of cognitive
Keywords: ACT; mindfulness; treatment; Acceptance and Commitment Therapy
behavioral therapies existed (by the early 2000s) that focused more heavily on processes such as acceptance, mindfulness, and second-order change, Hayes (2004) suggested
that a third wave of behavior therapy might be occurring
(with the first wave being behavior therapy and the second
wave being traditional cognitive therapy). This concept was
presented as the emergence of a new set or formulation of
dominant assumptions, methods, and goals, some implicit,
that help organize research, theory, and practice (p. 640).
The third wave was said to be not a rejection of the first
and second waves of behavioral and cognitive therapy
(p. 660) but rather a healing old wounds and divisions
between behavioral and cognitive perspectives (p. 660) that
encouraged the transformation of these earlier phases into
a new, broader, more interconnected form (p. 660). The
language of waves, however, led to a concern that previous
forms of CBT were being replaced and thus led to written
and verbal debates over whether there really is a third wave
and if it is anything new (Hofmann & Asmundsun, 2008).
This phase of concern seems to have passed, and ACT and
other new methods are now well positioned within larger
CBT as forms of contextual cognitive behavior therapy.
ACT is thus a form of CBT, with CBT being an umbrella
term for the larger number of therapies that fall under the
cognitive behavioral model.
Functional Contextualism
1077-7229/12/xxx-xxx$1.00/0
2012 Association for Behavioral and Cognitive Therapies.
Published by Elsevier Ltd. All rights reserved.
ACT comes from a philosophical framework called
functional contextualism (Hayes, Hayes, & Reese, 1988;
Please cite this article as: Twohig, Acceptance and Commitment Therapy, Cognitive and Behavioral Practice (2012), doi:10.1016/
j.cbpra.2012.04.003
Twohig
Hayes, Hayes, Reese, & Sarbin, 1993). This philosophical
approach shares many similarities with radical behaviorism, and in part for that reason ACT is considered a form
of clinical behavior analysis (Dougher & Hayes, 2000).
While philosophical assumptions are not usually at the
forefront of a therapeutic approach, in the case of ACT,
its philosophy of science guides most aspects of its research
and administration. Functional contextualism is not argued
to be chosen as ACT's philosophical stance because it is
inherently the best or right: it is simply stated, from the
beginning, as the chosen philosophic model and its
outcomes are judged against its goals. Its explication is
necessary because these assumptions emphasize the central
pragmatic concerns in developing and utilizing this
therapy.
There are many elements of functional contextualism
that are worth familiarizing oneself with if interested in
ACT, but for the sake of brevity, two main concepts will
be reviewed: the chosen unit of analysis and its truth
criterion. The whole event is studied from the functional
contextual model. Elements of the larger event are generally not studied in isolation because doing so may
disregard important contextual features to any action.
This issue is that formally similar actions may have very
different functions depending on context. Knowing the
function of an action is important to successfully intervene
on that behavior. This is similar to the way reinforcers and
punishers are definedfunctionally, not topographically.
The same thing applies to all inner experiences (thoughts,
feelings, bodily sensations): none are inherently problematic or positive; it all has to do with how they function for the
person.
The truth criterion of contextualism is effective action;
functional contextualism refines that general criterion
to a more specific goalprediction and influence with
precision, scope, and depth (Hayes et al., 1993). All truth
criterions provide a metric against which success can be
measured, and merely allows principles, theories, and
methods to be judged against predefined goals. This
applies to therapy outcomes as well as the larger scientific
endeavor. If functional contextual science does not result
in effective clinical interventions and progressive ways of
doing scientific work, then it fails. If meaningful clinical
outcomes are seen and its related science is progressing in
a useful manner, then it is succeeding. This differs from
other models, such as mechanistic or developmental
models, that might be more interested in constructing
models of the parts, relations, and forces that make up the
world, or predicting and observing the pattern of growth.
Functional contextualism also highlights the need for the
science to be progressive by demanding that the work
cohere with other scientific levels and domains (that is
what is meant by depth), while maintaining a suitable
level of precision and utility within the field of psychology.
Clinically, functional contextualism leads to certain
theoretical viewpoints that are central to ACT. First,
because of the emphasis on influence, ACT takes on a
behavioral viewpoint of inner experiences. Inner experiences are seen as responses to environmental events rather
than independent causes of action. From a behavioral
perspective, an event may evoke or elicit a particular inner
experience, and that inner experience may influence one's
actions, but the cause is back in the environment. This is
partially why inner experiences are addressed with acceptance and mindfulness strategies rather than more direct
strategies such as cognitive challenging. ACT attempts to
take the cognitions out of the way so that the individual
can better interact with the actual contingencies. Additionally, the goal of successful working is not restricted to
diagnosable disorders; this ties into the great number of
ACT studies that address issues of social importance that
are not diagnosable disordersfor example, increasing
the use of evidence-based practices (Varra, Hayes, Roget, &
Fisher, 2008), infertility stress (Peterson & Eifert, 2011),
and marital distress (Peterson, Eifert, Feingold, & Davidson,
2009), to name a few.
Behavior Analytic Account of Cognition: RFT
Consistent with the functional contextual philosophy
of science, an account of cognition that is clinically useful
is needed to guide the larger base of work that informs
ACT. Two lines of research from behavior analysis inform
ACT: RFT (Hayes, Barnes-Holmes, & Roche, 2001) and
rule-governed behavior (Hayes, 1989), both of which have
a considerable research base; therefore, only a cursory
review can occur here.
RFT
Cognitive humans do not simply respond to the formal
properties of the stimuli that we interact with like other
nonverbal animals do. A dog trained to respond to a
stimulus will respond similarly to ones that share formal
properties with it (stimulus generalization). Humans with
cognitive abilities have a way of effectively responding to
stimuli (external and internal) based on properties that
go beyond direct experience or stimulus generalization;
we can respond to stimuli based on a learned ability to
relate stimuli mutually and in combination and to alter
their functional properties on that basis (Hayes et al.,
2001). Relational framing of this kind is argued to be
learned, operant behavior, meaning we learn through
multiple exemplars and shaping when and how to
relationally respond to stimuli. There are many tested
forms of relational responding including, same, different,
better, time, and cause.
The type of relational framing that will occur is guided
by contextual cues, one set guiding relations themselves
and another guiding the functions of the stimuli that are
Please cite this article as: Twohig, Acceptance and Commitment Therapy, Cognitive and Behavioral Practice (2012), doi:10.1016/
j.cbpra.2012.04.003
Introduction: Basics of ACT
altered by a relational network. Laboratory research has
shown that the type of relation and the derived function
are governed by these different contextual features.
Written more colloquially, what a stimuli is and its suggested response are under the control of different features of
the environment. This has meaningful clinical implications in that therapy can either address the relational or
functional context that external stimuli or inner experiences occur in. ACT by and large focuses on the
functional context because research has shown that
once relational contexts are trained they cannot be
untrained (Wilson & Hayes, 1996), but that the functional
context under which stimuli occur can be altered while
leaving what a stimuli is in place (Hooper, Saunders, &
McHugh, 2010). Thus, if a client is having the thought, I
am a terrible person, instead of addressing the accuracy
of that thought, ACT would work with the person to
experience that thought in a way that does not negatively
affect his actions while possibly allowing the content of the
thought to stay the same.
gencies suggest is most effective. New rules will be created,
but additional methods are used so that the client stays
open to the likelihood that these contingencies too may
change. This illustrates the focus in ACT on behavior
change as well as flexibility with cognitions.
This is an overarching theme in a functional contextual account of language and cognitionour verbal and
cognitive abilities are very useful, but they can also have
a dangerous side. Thus, the corresponding therapeutic
approaches will focus on finding ways to utilize our verbal
abilities, while at the same time learning when to step
back from them and not follow them when they are not
useful. Events outside us and our thoughts, feelings, and
emotions will push us into actions that are not in our best
interest, and basic research suggests there are instances
when these events can be altered and instances when they
cannot be changed. The key is to determine this difference and make useful choices in these situations.
Rule-Governed Behavior
One of the implications of relational framing is that we
can create cognitive networks that represent the way
environmental contingencies function. Unfortunately,
these cognitively specified contingencies may not reflect
the environment contingencies actually in place and thus
can lead to dysfunctional behavior patterns. In general,
the ability to develop cognitive contingencies is useful
because it allows us to create effective behavior plans
without direct experience, but can also be at the root
of many forms of psychopathology. A simple example is
someone with obsessive-compulsive disorder developing
a rule that a ritualized shower is necessary to rid oneself
of germs and that any interruption of the ritual results
in recontamination. The core of this rule, showering is
good, is useful: but the verbally constructed rule (that
the ritual must be followed) does not accurately represent
the way the world works. The result of this verbal rule is
that the person follows it rather than following the actual
contingency that would indicate something other than
the verbal rule.
The most notable finding from rule governance
research is that cognitive rules make us less sensitive to
environmental contingencies (Hayes, 1989). Again, cognitive rules may be useful in some contexts and
problematic in others; the client needs to be aware of
learned or derived rules, and show the flexibility to follow
them in some situations and not follow them in others.
Oftentimes, it is problematic to either follow inaccurate
rules or follow useful rules too rigidly. Therefore, in ACT,
many direct and subtle steps are taken to help the client
contact actual environmental contingencies so that they
may shape behavior to what the environmental contin-
Because language is viewed as a pragmatic tool, ACT
theorists have attempted to construct a functional
contextual model of psychopathology and psychotherapy
that uses a series of psychological constructs that are more
easily disseminated and understood than the basic terms
of behavioral principles and RFT. The mid-level terms in
these clinical models are themselves analyzed using basic
terms and experimentation, thus there is a conscious effort
to keep traffic flowing on the bridge between applied and
basic sciences. Basic work in behavior analysis on learning
and on cognition, applied research on these psychological
constructs and their utility, and efficacy and effectiveness
studies on the resulting clinical intervention all work
together to inform this line of work. The treatment model
is designed to be clinically accessible, however, so that
practitioners need not understand RFT and similar
concepts to begin to use ACT.
The Resulting Clinical Model: Development of
Psychological Flexibility
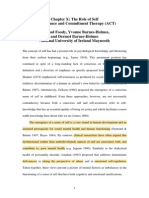
Psychological Flexibility
The core functional concept from this model is psychological flexibility, which is the ability to fully contact the present
moment and the inner experiences that are occurring,
without needless defense, and, depending upon the context,
persisting or changing in the pursuit of goals or personal
values (Hayes, Luoma, Bond, Masuda, & Lillis, 2006). It is
the opposite of psychological inflexibility (see Figure 1), which
is argued to be a core process in psychopathology (Hayes
et al., 2006). In order to address psychological flexibility, this
model targets six easily understood psychological processes
of change.
ACT
ACT directly aims to increase psychological flexibility,
and it does this through the following six psychological
Please cite this article as: Twohig, Acceptance and Commitment Therapy, Cognitive and Behavioral Practice (2012), doi:10.1016/
j.cbpra.2012.04.003
Twohig
I flexibly pay attention to
what is occurring in the
present moment
high
ATTENTION TO
PRESENT SCALE
I willingly
accept my
thoughts and
feelings even
when I dont
like them
low
high
ACCEPTANCE
SCALE
I spend
most of my time on
attentional autopilot
high
low
low
I constantly
struggle with
my thoughts
and feelings
DEFUSION
SCALE
I see each of
my thoughts
as just one of
many ways to
think about
things what
I do next is up
to me
high
low
I am clear
about what I
choose to
value in life
I dont
know what
I want
from life
My thoughts tell me
how things really
are and what I need
to do
The person I call
me is my
thoughts and
feelings about
myself
VALUES
CLARITY SCALE
I dont manage
to act on the
things I care
about
low
SELF AS
CONTEXT
SCALE
low
COMMITMENT &
TAKING ACTION
SCALE
high
I identify the
actions I need
to take to put
my values into
practice, and I
see them
through
high
The person I call me
knows what I am
thinking and feeling
but is distinct from
that process
Figure 1. Clinical descriptions of low and high presence of the six ACT processes of change. Note. Based on the ACT ADVISOR by David
Chantry and used with permission.
processes of change: acceptance, defusion, being present,
self as context, values, and behavioral commitments, all
of which have considerable support outside of larger
treatment packages (Hayes et al., 2006; Ruiz, 2010). As
can be seen in Figure 1, each of these processes of change
is at one end of a continuum and its opposite process
of change is at the other. Consistent with the functional
philosophy that ACT is based on, the more functional
end of this spectrum is context dependent. For example,
being defused from anxious thoughts can be useful
when giving an important lecture, but some fusion with
thoughts might be useful when one is about to engage in
a dangerous activity. Part of what is taught in ACT is
developing the discrimination between these ends of each
process of change and knowing how to effectively engage
each behavior.
Acceptance. Acceptance involves actively embracing
inner experiences, while they are presently occurring, as
ongoing inner experiences. This is an action; it is not an
attitude or an opinion. We can choose to behave acceptingly
or we can work to regulate our inner experiences.
Acceptance is different than tolerance because acceptance
is viewed as a choice and involves a more welcoming stance
towards the inner experience. Acceptance targets the
context that an inner experience occurs in and decreases
the effort that one exerts to control or regulate certain inner
experiences. Acceptance is applied to inner experiences
that foster experiential avoidance, which is attempting to
reduce or avoid unwanted inner experiences when doing so
results in negative effects on one's functioning (Hayes,
Wilson, Gifford, Follette, & Strosahl, 1996). An example of
experiential avoidance could be where an individual with an
Please cite this article as: Twohig, Acceptance and Commitment Therapy, Cognitive and Behavioral Practice (2012), doi:10.1016/
j.cbpra.2012.04.003
Introduction: Basics of ACT
anxiety disorder either avoids or escapes situations that
bring on anxiety, or while in an anxiety-producing situation
engages in inner dialogue aimed at lessening that anxiety.
Conversely, acceptance not only involves actively being in
situations that bring on anxiety, but treating one's anxiety
in a welcoming way while it is there. Thus, while doing
exposure exercises, the therapist might ask, How open are
you to your anxiety? rather than How much anxiety are
you feeling?
Cognitive defusion. Cognitive defusion involves altering the context in which inner experiences occur in an
attempt to decrease their automatic impact and importance, allowing them to be seen as an ongoing process.
Written another way, cognitive defusion can be thought of
as reducing the literal meaning of inner experiences so
that thoughts are experienced as just thoughts, feelings
are just feelings, and bodily sensations are just bodily
sensations. Cognitive defusion is the opposite of cognitive
fusion, which is where the inner experiences are taken
literally and have a large amount of power over one's
actions. Cognitive defusion and cognitive fusion are both
useful; it is just that they need to be flexibly applied to
different situations. For example, when one is doing taxes
or grocery shopping, being fused might be useful as the
work is completed with greater speed and accuracy.
Whereas, if one is having the thought, I am worthless, it
might be more useful for the person to experience that
thought as just words and sounds and choose to not let it
influence one's actions.
Being present. Being present is when we experience
our inner experiences and events in our environments as
occurring now as opposed to focusing on events in the
past or in the future. Being present is generally defined as
flexible, fluid, and voluntary attention to internal and
external events as they are occurring, without attachment
to evaluation or judgment. Being present with one's
internal and external environment helps in experiencing
the world as it really is occurring and decreases the impact
of the cognitively constructed world. Being present entails
at least three skills: the ability to regulate attention to the
now; openly and fully experiencing what is occurring; and
labeling and describing these events in a nonjudgmental
manner. The flip side of being present is being attached
to a cognitive representation of the past or the future.
Common examples of not being present occur while
ruminating or worrying. In both these situations, the
individual is not in contact with the events that are
occurring currently, but engaged with events that have
already occurred or might occur. A client with rumination
or worry might be taught to recognize when they are not
aware of the present moment, notice its occurrence, and
refocus their attention to their current inner experiences
and events in their current environment. In ACT, it is less
about being present, but being able to notice when one is
not, and flexibly shifting attention to the present if it is in
the person's best interest.
Self as context. The conceptualized self is the you that
is constructed that is based upon self-evaluations and
categorizations. It is what we believe ourselves to be. The
clinical issue is that people will attempt to protect, retain,
or shield that conceptualization of the self even when
it leads to ineffective action. For example, if a person has
labeled himself as depressed, he may very well engage in
behaviors that continue to maintain that self-description
of depressed, out of a basic belief that a self must be
protected. In ACT, we work to develop a sense of self as
context, where the self is the place of awareness or perspective taking that allows internal and external events
to be experienced from I/here/now without being
defined by those events. From this sense of self as the
context where inner experiences occur, but is not defined
by them, we can choose to follow and adhere to our senses
of who we are in some situations and not in others. Similar
to other ACT processes, flexibility in this area is desired.
Self as context is thought to be facilitated by cognitive
defusion applied to the conceptualization of self, and by
mindfulness or other awareness exercises, showing the
interplay among the six ACT processes.
Values. In ACT, values are elements of life that we
care about that motivate us to engage in certain activities.
While there are some common values that most people
share, values are individually chosen. Values are often
contrasted with goals. Goals are obtainable, such as a
marriage. Values can only be instantiated as an aspect of
ongoing action, such as being a loving and kind husband,
and thus are more like adverbs than nouns. They can
be pursued across one's life, but they cannot be possessed
like objects. They can provide guidance, meaning, and
purpose for our actions. Functionally, clarifying values
affects the reinforcing and punishing functions of events
involved in pursuing those values. Thus, helping clarify
a client's values should help make it more likely that he
will approach stimuli that originally fostered avoidance;
in addition, reinforcers that were having little effect
may become more powerful. For example, telling a client
diagnosed with an anxiety disorder that approaching an
anxiety-provoking stimuli (and allowing the anxiety to be
there without defense) brings him a step closer to being
able to attend an event at his child's school (if parenting is a
value) would increase the reinforcing value of experiencing
anxiety.
Behavioral commitments. This is the area of ACT
where traditional behavior change procedures are
Please cite this article as: Twohig, Acceptance and Commitment Therapy, Cognitive and Behavioral Practice (2012), doi:10.1016/
j.cbpra.2012.04.003
Twohig
incorporated into therapy. All other processes in ACT
serve to either alter the context in which inner
experiences occur, or alter the reinforcing or punishing
effects of stimuli. Committed action is more skill based
and generally involves enacting one's values while
practicing acceptance, defusion, being present, and
treating oneself as the context where inner experiences
occur. Committed action is the continuous redirection of
behavior so as to construct larger and larger patterns of
flexible and effective behavior linked to a value. It involves
defining personal goals along a path and acting on those
goals, while practicing the other ACT strategies, thus
building larger patterns of values-oriented action. Any
behavioral intervention method can be incorporated as
part of ACT as long as it is consistent with the other ACT
processes. This can include exposure exercises, fading
procedures, or skills training activities.
Basic Therapeutic Stance
Probably one of the most notable aspects of ACT is that
it is experientially oriented. At times this means it is difficult
to move from its written description to its implementation.
In describing ACT we are using language and cognition to
teach skills that are designed in part to undermine typical
language and cognitive processes. In a sense we are fighting
fire with fire. For example, we are trying to help clients take
language less literally through conversation; we are trying to
loosen the grip of rules but in the process teaching the rule
that rules cannot be trusted; and, finally, to clarify one's
values but also hold those values lightly as they are likely to
shift over time. Thus, often the least direct or rule-forming
ways of teaching ACT processes are utilized. ACT relies
heavily on metaphors or stories, exercises and role-plays
are common in session, and examples from the client's
or the therapist's lives are also used to help develop psychological flexibility. ACT is usually not implemented
didactically; rather, a therapeutic context where these processes can be taught and practiced is common. The therapist might attempt to bring up target inner experiences
during therapy and help the client to practice using the six
processes while that inner experience is present.
One final part of ACT that may be different from some
other therapies is that in ACT, the therapist deliberately
tries to model these six ACT processes within the session.
This occurs moment to moment in session in the way
that the therapist responds to his or her inner experiences
during therapy, but also the manner in which the therapist responds to the client's inner experiences. For
example, when a client shows emotion, the therapist
would not attempt to save the client from that emotion,
but rather, show acceptance of that emotion by openly
talking about it and showing openness to its emotional
impact on the therapist. By showing acceptance of the
client's emotions and modeling the six ACT processes with
regard to the emotions that the therapist is feeling, ACT
processes are being facilitated without formal exercises.
One useful way to think about ACT is that it seeks to
establish a new context in which inner experiences are not
causal and one's behavior is guided by what he or she
chooses to hold as important in life. For example, the
feeling of depression, when viewed from an accepting and
defused standpoint, may have little influence on one's
actions; instead, client actions can be influenced by
personal values. As this context becomes powerful enough
that it is carried outside of session, it is hoped that the client
then contacts actual contingencies in the world and learns
how to function better within them.
Empirical Support for ACT
There is growing support for ACT across a broad group
of social concerns, but before these outcomes are reviewed,
the manner in which this approach and model are evaluated should be addressed. Based on the functional model
from which ACT was developed, there are no inherently
problematic behaviors. Some types of behaviors are very
likely to be problematic, but a functional assessment should
occur before that is determined. Thus, there is no
particular thought or style of thinking that is problematic
from this model; the issue is really what response the
thought leads to. Again, using OCD as an example,
obsessive thoughts are only problematic when they are
taken literally and lead to behaviors that get in the way
of the person's functioning. If someone can learn to
just notice the obsession and continue in a meaningful
direction in life, the form or frequency of that thought
would have a small impact on behavior and not need to
be addressed clinically. This highlights ACT's greater focus
on functioning rather than symptom reduction per se. This
can be contrary to how change is defined for some disorders. This issue was highlighted in a recent metaanalysis
of ACT conducted by Powers, Zum Vrde Sive Vrding,
and Emmelkamp (2009) that showed that ACT for chronic
pain had near zero effect sizes for pain intensity, but those
same effect sizes were large if using behavioral functioning
as the dependent variable (Levin & Hayes, 2009).
ACT has been tested for a surprisingly large set of
social issues, many of which are not diagnosable, although
many are (Hayes et al., 2006; Ruiz, 2010). Specifically,
ACT has been shown to be effective for a variety of anxiety
disorders (e.g., Codd, Twohig, Crosby & Enno, 2011),
mood disorders (e.g., Zettle & Rains, 1989), substance
use disorders (e.g., Hayes et al., 2004), psychotic disorders
(e.g., Gaudiano & Herbert, 2006), eating disorders and
weight issues (e.g., Juarascio, Forman, & Herbert, 2010),
impulse control disorders (e.g., Woods, Wetterneck, &
Flessner, 2006), personality disorders (Gratz & Gunderson,
Please cite this article as: Twohig, Acceptance and Commitment Therapy, Cognitive and Behavioral Practice (2012), doi:10.1016/
j.cbpra.2012.04.003
Introduction: Basics of ACT
2006), as well as issues confronted in behavioral medicine
(Gundy, Woidneck, Pratt, Christian, & Twohig, 2011).
ACT has also been successfully used with children (Coyne,
McHugh & Martinez, 2012) and is being applied to
individuals with developmental disabilities or brain injury
(e.g., Soo, Tate, & Lane-Brown, 2011), although in the
latter case data are not out yet. In addition, ACT has been
shown to be useful with a variety of issues that are not
diagnosable, such as parental distress associated with
raising children with developmental disorders (Blackledge
& Hayes, 2006), stigma issues (Masuda et al., 2007), helping
professionals adopt empirically supported interventions
(Varra, Hayes, Roget, & Fisher, 2008), infertility stress
(Peterson & Eifert, 2011), and marital distress (Peterson
et al., 2009), to name a few. Recent reviews and metaanalyses have suggested that ACT is more effective than
control conditions but has not been shown to be more
effective than other empirically established psychosocial
treatments such as more traditional CBT packages (st,
2008; Powers et al., 2009), although the empirical arguments are complex and in flux (e.g., Gaudiano, 2009; Levin
& Hayes, 2009; Powers & Emmelkamp, 2009).
Support for the Model
As hopefully is evident from the overarching strategy
presented here, outcomes and comparisons between
treatments is only a part of this research agenda (Hayes,
Villatte, Levin, & Hildebrandt, 2011). The issue is really in
the effectiveness of this larger line of research. If this
agenda helps to move the field forward in a meaningful
way, then it succeeded; if it does not help science progress
and help more people who are suffering, then it failed.
There appears to be evidence that this is a successful line
of research and the original goals of prediction and influence
with precision, scope, and depth seem to be supported. Prediction exists in that those with greater levels of psychological inflexibility in general suffer more and have
greater pathology (Hayes et al., 2006). Influence appears
to be supported based on the evidence that this work
is helpful clinically (Powers et al., 2009). The precision
of the model is supported in that the applied model is
supported by the basic research on language and cognition. Additionally, precision exists in that, thus far, the
evidence has generally supported psychological flexibility
as the process of change in ACT versus alternative models
such as how often or what types of thoughts occur (e.g.,
Bach & Hayes, 2002; see review by Hayes et al., 2006).
Finally, scope exists in that research within ACT seems
consistent with other lines of research both within RFT
(e.g., McHugh & Stewart, 2012) and within lines of
research that are not part of this general research program. For example, the work on thought suppression is
consistent with an ACT model of dealing with problematic
cognitions (Wenzlaff & Wegner, 2000). The way inner
experiences are addressed in ACT is also consistent with
modern accounts of behavioral processes like extinction,
which no longer suggest that behaviors are unlearned but
rather become contextually controlled (Bouton, 2000).
Contents of Special Series on ACT and Summary
of Introduction
This special series contains eight empirical papers
that are consistent with the ACT model. There are three
randomized controlled trials of ACT versus treatment as
usual: psychosocial coping with late-stage ovarian cancer
(Rost, Wilson, Buchanan, Hildebrandt, & Mutch, this
issue), borderline personality disorder (Morton, Snowdon,
Gopold, & Guymer, this issue), and depression (Folke,
Parling, & Melin, this issue). Clarke and colleagues (Clarke,
Kingston, Wilson, Bolderston, & Remington, this issue) also
provide data on ACT for treatment-resistant clients but
do so within an open trial. The multiple baseline across
participants design was used to test the effects of ACT for
self-stigma around sexual orientation (Yadavaia & Hayes,
this issue) or ACT plus behavior therapy for trichotillomania (Crosby, Dehlin, Mitchell, & Twohig, this issue).
Psychometric data on a new assessment device for values
that has both research and clinical utility is presented
(Lundgren, Luoma, Dahl, Strosahl, & Melin, this issue). In
a more basic experiment, Hussey and Barnes-Holmes (this
issue) use RFT to guide an experiment on implicit attitudes
and levels of depression and psychological flexibility.
Clearly there is a lot more work to do, but based on the
new data that are presented in this special series and the
evidence reviewed herein, this appears to be a line of work
that is worth continuing. Hopefully, it is clear that this
line of research is much more than just does ACT work for
this or that, but that the work includes theoretical and
philosophical writings; laboratory work on language and
cognition and other behavioral principles that are applied
to humans; development and refinement of the psychological constructs addressed in ACT; measure development; clinical technique development; intervention testing;
and the testing of the purported processes of change in the
treatment once it is delivered. Some of this work occurs in
basic laboratories and other work occurs in more applied
contexts; regardless, a focus on linking and translating this
work across levels of analysis is needed. Basic and applied
researchers need to continue to communicate and ask for
answers from each other. This approach appears to be an
endeavor that many of us who fall under the CBT label are
interested in and goes well beyond the brand ACT, and is
really about helping those who need it.
References
Bach, P., & Hayes, S. C. (2002). The use of acceptance and commitment
therapy to prevent the rehospitalization of psychotic patients: A
randomized controlled trial. Journal of Consulting and Clinical Psychology,
70, 11291139. http://dx.doi.org/10.1037/0022-006X.70.5.1129
Please cite this article as: Twohig, Acceptance and Commitment Therapy, Cognitive and Behavioral Practice (2012), doi:10.1016/
j.cbpra.2012.04.003
Twohig
Blackledge, J. T., & Hayes, S. C. (2006). Using acceptance and
commitment training in the support of parents of children
diagnosed with autism. Child & Family Behavior Therapy, 28, 118.
http://dx.doi.org/10.1300/J019v28n01_01.
Bouton, M. E. (2000). A learning theory perspective on lapse, relapse,
and the maintenance of behavior change. Health Psychology, 19,
5763. http://dx.doi.org/10.1037/0278-6133.19.Supp l1.57.
Clarke, S., Kingston, J., Wilson, K. G., Bolderston, H., & Remington, B.
(this issue). Acceptance and commitment therapy for a heterogeneous group of treatment resistant clients: A treatment
development study. Cognitive and Behavioral Practice.
Codd, R. T., III, Twohig, M. P., Crosby, J. M., & Enno, A. (2011). Treatment
of three anxiety disorder cases with acceptance and commitment
therapy in a private practice. Journal of Cognitive Psychotherapy, 25,
203217. http://dx.doi.org/10.1891/0889-8391.25.3.203.
Coyne, L. W., McHugh, L., & Martinez, E. R. (2012). Acceptance and
commitment therapy (ACT): Advances and applications with
children, adolescents, and families. Child and Adolescent Psychiatric
Clinics of North America, 20, 379399. http://dx.doi.org/10.1016/
j.chc.2011.01.010.
Crosby, J. M., Dehlin, J. P., Mitchell, P. R., & Twohig, M. P. (this issue).
Acceptance and commitment therapy and habit reversal training for
the treatment of trichotillomania. Cognitive and Behavioral Practice.
Dougher, M. J., & Hayes, S. C. (2000). Clinical behavior analysis. In M. J.
Dougher (Ed.), Clinical behavior analysis (pp. 1125). Reno, NV:
Context Press.
Folke, F., Parling, T., & Melin, L. (this issue). Acceptance and commitment
therapy for depression: A preliminary randomized clinical trial for
unemployed on long-term sick leave. Cognitive and Behavioral Practice.
Gaudiano, B. A. (2009). st's (2008) methodological comparison of
clinical trials of acceptance and commitment therapy versus
cognitive behavior therapy: Matching apples with oranges? Behaviour
Research and Therapy, 47, 10661070. http://dx.doi.org/10.1016/
j.brat. 2009.07.020.
Gaudiano, B. A., & Herbert, J. D. (2006). Acute treatment of inpatients
with psychotic symptoms using Acceptance and Commitment
Therapy: Pilot results. Behaviour Research and Therapy, 44, 415437.
http://dx.doi.org/10.1016/j.brat.2005.02.007.
Gratz, K. L., & Gunderson, J. G. (2006). Preliminary data on acceptancebased emotion regulation group intervention for deliberate selfharm among women with borderline personality disorder. Behavior
Therapy, 37, 2535. http://dx.doi.org/10.1016/j.beth.2005.03.002.
Gundy, J. M., Woidneck, M. R., Pratt, K. M., Christian, A. W., & Twohig,
M. P. (2011). Acceptance and commitment therapy: The state of
the evidence in the field of health psychology. Scientific Review of
Mental Health Practice, 8, 2335.
Hayes, S. C. (1989). Rule-governed behavior: Cognition, contingencies, and
instructional control. New York, NY: Plenum Press.
Hayes, S. C. (2004). Acceptance and commitment therapy, relational
frame theory, and the third wave of behavioral and cognitive
therapies. Behavior Therapy, 35, 639665. http://dx.doi.org/10.1016/
S0005-7894(04)80013-3.
Hayes, S. C., Barnes-Holmes, D., & Roche, B. (2001). Relational frame
theory: A post-Skinnerian account of human language and cognition.
New York, NY: Kluwer Academic/Plenum.
Hayes, S. C., Hayes, L. J., & Reese, H. W. (1988). Finding the
philosophical core: A review of Stephen C. Popper's World
Hypotheses. Journal of Experimental Analysis of Behavior, 50, 97111.
http://dx.doi.org/10.1901/jeab.1988.50-97.
Hayes, S. C., Hayes, L. J., Reese, H. W., & Sarbin, T. R. (1993). Analytic
goals and the varieties of scientific contextualism. In S. C. Hayes,
L. J. Reese, & T. R. Sarbin (Eds.), Varieties of scientific contextualism
(pp. 1127). Reno, NV: Context Press.
Hayes, S. C., Luoma, J. B., Bond, F. W., Masuda, A., & Lillis, J. (2006).
Acceptance and commitment therapy: Model, processes and outcomes. Behaviour Research and Therapy, 44, 125. http://dx.doi.org/
10.1016/j.brat.2005.06.006.
Hayes, S. C., Wilson, K. G., Gifford, E. V., Bissett, R., Piasecki, M., Batten, S.
V., . . . Gregg, J. (2004). A preliminary trial of twelve-step facilitation
and acceptance and commitment therapy with polysubstance-abusing
methadone-maintained opiate addicts. Behavior Therapy, 35, 667688.
http://dx.doi.org/10.1016/S0005-7894(04)80014-5.
Hayes, S. C., Villatte, M., Levin, M., & Hildebrandt, M. (2011). Open,
aware, and active: Contextual approaches as an emerging trend in
the behavioral and cognitive therapies. Annual Review of Clinical
Psychology, 7, 141168. http://dx.doi.org/10.1146/annurevclinpsy-032210-104449.
Hayes, S. C., Wilson, K. G., Gifford, E. V., Follette, V. M., &
Strosahl, K. (1996). Experiential avoidance and behavioral
disorders: A functional dimensional approach to diagnosis and
treatment. Journal of Consulting and Clinical Psychology, 64, 11521168.
http://dx.doi.org/10.1037/0022-006X.64.6.1152.
Hofmann, S. G., & Asmundson, G. J. G. (2008). Acceptance and
mindfulness-based therapy: New wave or old hat? Clinical Psychology
Review, 28, 116. http://dx.doi.org/10.1016/j.cpr. 2007.09.003.
Hooper, N., Saunders, J., & McHugh, L. (2010). The derived
generalization of thought suppression. Learning & Behavior, 38,
160168. http://dx.doi.org/10.3758/LB.38.2.160.
Hussey I., & Barnes-Holmes, D. (this issue). The Implicit Relational
Assesssment Procedure as a measure of implicit depression and
the role of psychological inflexibility. Cognitive and Behavioral
Practice.
Juarascio, A. S., Forman, E. M., & Herbert, J. D. (2010). Acceptance
and commitment therapy versus cognitive therapy for the treatment
of comorbid eating pathology. Behavior Modification, 34, 175190.
http://dx.doi.org/10.1177/0145445510363472.
Levin, M., & Hayes, S. C. (2009). Is Acceptance and Commitment Therapy
superior to established treatment comparisons? Psychotherapy and
Psychosomatics, 78. http://dx.doi.org/10.1159/000235979.
Lundgren, T., Luoma, J. B., Dahl, J., Strosahl, K., & Melin, L. (this
issue). The Bull's-Eye Values Survey: A psychometric evaluation.
Cognitive and Behavioral Practice.
Masuda, A., Hayes, S. C., Fletcher, L. B., Seignourel, P. J., Bunting, K.,
Herbst, S. A., . . . Lillis, J. (2007). Impact of acceptance and
commitment therapy versus education on stigma toward people
with psychological disorders. Behaviour Research and Therapy, 45,
27642772. http://dx.doi.org/10.1016/j.brat.2007.05.008.
McHugh, L., & Stewart, I. (2012). The self and perspective taking: Contributions
and applications from modern behavioral science. Reno, NV: Context Press.
Morton, J., Snowdon, S., Gopold, M., & Guymer, E. (this issue).
Acceptance and commitment therapy group treatment for
symptoms of borderline personality disorder: A public sector
pilot study. Cognitive and Behavioral Practice.
st, L. G. (2008). Efficacy of the third wave of behavioral therapies: A
systematic review and meta-analysis. Behaviour Research and Therapy,
46, 296321. http://dx.doi.org/10.1016/j.brat.2007.12.005.
Peterson, B. D., & Eifert, G. H. (2011). Using Acceptance and Commitment
Therapy to treat infertility stress. Cognitive and Behavioral Practice, 18,
577587. http://dx.doi.org/10.1016/j.cbpra.2010.03.004.
Peterson, B. D., Eifert, G. H., Feingold, T., & Davidson, S. (2009). Using
acceptance and commitment therapy to treat distressed couples:
A case study with two couples. Cognitive and Behavioral Practice, 16,
430442. http://dx.doi.org/10.1016/j.cbpra.2008.12.009.
Powers, M. B., & Emmelkamp, P. M. G. (2009). Response to Is
Acceptance and Commitment Therapy superior to established
treatment comparisons? Psychotherapy and Psychosomatics, 78,
380381. http://dx.doi.org/10.1159/000235979.
Powers, M. B., Zum Vrde Sive Vrding, M. B., & Emmelkamp, P. M. G.
(2009). Acceptance and commitment therapy: A meta-analytic review.
Psychotherapy and Psychosomatics, 78, 7380. http://dx.doi.org/
10.1159/000190790.
Rost, A. D., Wilson, K. G., Buchanan, E., Hildebrandt, M. J., & Mutch D.
(this issue). Improving psychological adjustment among late-stage
ovarian cancer patients: Examining the role of avoidance in
treatment. Cognitive and Behavioral Practice.
Ruiz, F. J. (2010). A review of Acceptance and Commitment Therapy
(ACT) empirical evidence: Correlational, experimental psychopathology, component and outcome studies. International Journal of
Psychology & Psychological Therapy, 10, 125162. http://dx.doi.org/
10.1080/028457199439937.
Soo, C., Tate, R. L., & Lane-Brown, A. (2011). A systematic review of
Acceptance and Commitment Therapy (ACT) for managing
anxiety: Applicability for people with acquired brain injury? Brain
Impairment, 12, 5470.
Please cite this article as: Twohig, Acceptance and Commitment Therapy, Cognitive and Behavioral Practice (2012), doi:10.1016/
j.cbpra.2012.04.003
Introduction: Basics of ACT
Varra, A. A., Hayes, S. C., Roget, N., & Fisher, G. (2008). A randomized
control trial examining the effect of acceptance and commitment
training on clinician willingness to use evidence-based pharmacotherapy. Journal of Consulting and Clinical Psychology, 76, 449458.
http://dx.doi.org/10.1037/0022-006X.76.3.449.
Wenzlaff, R. M., & Wegner, D. M. (2000). Thought suppression. Annual
Review of Psychology, 51, 5991. http://dx.doi.org/10.1146/
annurev.psych.51.1.59.
Wilson, K. G., & Hayes, S. C. (1996). Resurgence of derived stimulus
relations. Journal of the Experimental Analysis of Behavior, 66,
267281. http://dx.doi.org/10.1901/jeab.1996.66-267.
Woods, D. W., Wetterneck, C. T., & Flessner, C. A. (2006). A controlled
evaluation of acceptance and commitment therapy plus habit
reversal for trichotillomania. Behaviour Research and Therapy, 44,
639656. http://dx.doi.org/10.1016/j.brat.2005.05.006.
Yadavaia, J. E., & Hayes, S. C. (this issue). Acceptance and
Commitment Therapy for self-stigma around sexual orientation:
A multiple baseline evaluation. Cognitive and Behavioral Practice.
Zettle, R. D., & Rains, J. C. (1989). Group cognitive and contextual
therapies in treatment of depression. Journal of Clinical Psychology,
45(3), 436445. http://dx.doi.org/10.1002/1097-4679(198905)
45:3b436::AID-JCLP2270450314N3.0.CO;2-L.
I would like to thank Dr. Maureen Whittal for the opportunity to edit
this special series and her guidance through the process. I would also
like to thank Dr. Steven Hayes for his comments and edits to an earlier
version of this paper.
Address correspondence to Michael P. Twohig, Ph.D., Utah
State University, 2810 Old Main HI, Logan, UT 84322; e-mail:
michael.twohig@usu.edu.
Received: February 24 2012
Accepted: April 13 2012
Available online xxxx
Please cite this article as: Twohig, Acceptance and Commitment Therapy, Cognitive and Behavioral Practice (2012), doi:10.1016/
j.cbpra.2012.04.003
Вам также может понравиться
- Cognitive DefusionДокумент15 страницCognitive DefusionMR2692Оценок пока нет
- Luoma Cognitive DefusionДокумент17 страницLuoma Cognitive Defusionnelu onoОценок пока нет
- Cognitive Behavioral Group Therapy: Challenges and OpportunitiesОт EverandCognitive Behavioral Group Therapy: Challenges and OpportunitiesОценок пока нет
- Acceptance and Commitment Therapy - An OverviewДокумент28 страницAcceptance and Commitment Therapy - An OverviewDidina_Ina100% (3)
- Dialectical Behavior Therapy: A Contemporary Guide for PractitionersОт EverandDialectical Behavior Therapy: A Contemporary Guide for PractitionersОценок пока нет
- Relational Frame Theory, Acceptance and Commitment Therapy, and A Functional Analytic Definition of MindfulnessДокумент22 страницыRelational Frame Theory, Acceptance and Commitment Therapy, and A Functional Analytic Definition of Mindfulnessdor8661Оценок пока нет
- The Application of Acceptance and Commitment Therapy To Obsessive Compulsive DisorderДокумент11 страницThe Application of Acceptance and Commitment Therapy To Obsessive Compulsive DisorderAnonymous Ax12P2srОценок пока нет
- Psychological Flexibility As A Mechanism PDFДокумент28 страницPsychological Flexibility As A Mechanism PDFPedro GuimarãesОценок пока нет
- The Role of Self in Acceptance and Commitment TherapyДокумент25 страницThe Role of Self in Acceptance and Commitment TherapyMark KovalОценок пока нет
- Acceptance and Commitment Therapy (ACT) Contacts, Resources, and ReadingsДокумент30 страницAcceptance and Commitment Therapy (ACT) Contacts, Resources, and ReadingsAnonymous Ax12P2srОценок пока нет
- Emotion Regulation in ACT - Steven C. HayesДокумент13 страницEmotion Regulation in ACT - Steven C. HayesVartax100% (2)
- Dymond, S., Roche, B. (2013) - Advances in Relational Frame Theory PDFДокумент298 страницDymond, S., Roche, B. (2013) - Advances in Relational Frame Theory PDFVartax100% (2)
- Niklas Törneke-Learning RFT - An Introduction To Relational Frame Theory and Its Clinical Application-Context Press (2010)Документ290 страницNiklas Törneke-Learning RFT - An Introduction To Relational Frame Theory and Its Clinical Application-Context Press (2010)Anahi Pegoraro100% (11)
- Acceptance and Commitment Therapy (ACT) Contacts, Resources, and ReadingsДокумент30 страницAcceptance and Commitment Therapy (ACT) Contacts, Resources, and Readingsfriedl377203100% (1)
- Practical Guide To Acceptance and Commit Men TherapyДокумент399 страницPractical Guide To Acceptance and Commit Men TherapyAlejandro García100% (6)
- ACT Guide FinalДокумент25 страницACT Guide Finalrama krishna100% (3)
- ACCEPTANCE AND Commitment TherapyДокумент71 страницаACCEPTANCE AND Commitment TherapyPedro Guimarães100% (1)
- State of The Research & Literature Address: ACT With Children, Adolescents and ParentsДокумент13 страницState of The Research & Literature Address: ACT With Children, Adolescents and Parentslibreria14Оценок пока нет
- Acceptance & Commitment Therapy - IntroductionДокумент12 страницAcceptance & Commitment Therapy - IntroductionKaryl Christine AbogОценок пока нет
- Innovations in Acceptance and Commitment Therapy Clinical Advancements and Applications in ACTДокумент368 страницInnovations in Acceptance and Commitment Therapy Clinical Advancements and Applications in ACTFábio Vacaro Culau100% (3)
- FACT Kirk Strosahl Presentation PDFДокумент11 страницFACT Kirk Strosahl Presentation PDFAlexander ZelenukhinОценок пока нет
- Acceptance and Commitment Therapy For Leadership and Change ManagersДокумент10 страницAcceptance and Commitment Therapy For Leadership and Change ManagersmysticblissОценок пока нет
- ACT D Therapist Manual PDFДокумент132 страницыACT D Therapist Manual PDFedw68100% (2)
- The Essential Guide To The ACT Matrix A StepbyStep Approach To Using The ACT Matrix Model in Clinical Practice NodrmДокумент365 страницThe Essential Guide To The ACT Matrix A StepbyStep Approach To Using The ACT Matrix Model in Clinical Practice NodrmRan Almog100% (21)
- Learning ACT - An Acceptance and Commitment Therapy Skills-Training Manual For Therapists (PDFDrive)Документ379 страницLearning ACT - An Acceptance and Commitment Therapy Skills-Training Manual For Therapists (PDFDrive)Wesley Ramalho100% (2)
- ACT Guide FinalДокумент24 страницыACT Guide FinalJohnОценок пока нет
- The ACT Matrix K. Polk B.Schoendorff PDFДокумент281 страницаThe ACT Matrix K. Polk B.Schoendorff PDFÁngela María Páez Buitrago100% (17)
- Strosahl ACBS ACT Brief Intervention WorkshopДокумент17 страницStrosahl ACBS ACT Brief Intervention WorkshopJay MikeОценок пока нет
- ACT & Mindfulness at Work - Steven C. Hayes, Frank W. Bond, Dermot Barnes-HolДокумент186 страницACT & Mindfulness at Work - Steven C. Hayes, Frank W. Bond, Dermot Barnes-HolDavid Espinola100% (4)
- Ellis, 2005Документ16 страницEllis, 2005Jonathon BenderОценок пока нет
- Functional Analityc PsychotherapyДокумент290 страницFunctional Analityc PsychotherapyViviana92% (13)
- Kevin L. Polk PDFДокумент281 страницаKevin L. Polk PDFLeilanneArjonesОценок пока нет
- 1 RFT LearningДокумент68 страниц1 RFT LearningJéssica Lays RibeiroОценок пока нет
- ++++polk, Shoendorff, Webster y Olaz (2016) The Essential Guide For ACT MatrixДокумент287 страниц++++polk, Shoendorff, Webster y Olaz (2016) The Essential Guide For ACT MatrixVictor Canales100% (2)
- Acceptance and Commitment Training (ACT) in The WorkplaceДокумент37 страницAcceptance and Commitment Training (ACT) in The Workplacem2r71964Оценок пока нет
- Perspective TakingДокумент274 страницыPerspective TakingCarolina Silveira100% (2)
- Actand 1 PDFДокумент298 страницActand 1 PDFRoger100% (2)
- 2014 - The Big Book of ACT Metaphors - Jill A. StoddardДокумент191 страница2014 - The Big Book of ACT Metaphors - Jill A. StoddardCAMILA MEJIA LOZANOОценок пока нет
- ACT Made Simple - The Extra Bits - by Russ Harris - Textbook Support Materials - November 2021 UpdateДокумент7 страницACT Made Simple - The Extra Bits - by Russ Harris - Textbook Support Materials - November 2021 UpdateH A100% (1)
- Howard Kirschenbaum Values Clarification in Counseling and Psychotherapy Practical Strategies For Individual and Group Settings Oxford University Press 2013Документ225 страницHoward Kirschenbaum Values Clarification in Counseling and Psychotherapy Practical Strategies For Individual and Group Settings Oxford University Press 2013Andjelija Simic100% (2)
- Acceptance and Commitment Therapy For TH - Walser, Robyn (Author) PDFДокумент270 страницAcceptance and Commitment Therapy For TH - Walser, Robyn (Author) PDFMoniica Macias100% (11)
- Big Book of ACT Metaphors, The - Hayes, Steven C., Stoddard, Jill A., Afari, Niloofar PDFДокумент250 страницBig Book of ACT Metaphors, The - Hayes, Steven C., Stoddard, Jill A., Afari, Niloofar PDFÁngela María Páez Buitrago96% (47)
- ACT Training Manual For Substance Abuse CounselorsДокумент9 страницACT Training Manual For Substance Abuse CounselorsSiro Vaquero CabezaОценок пока нет
- STRESS - Craig Huffman - ACT Ultim Guide To Using ACT To Treat Stress, Includ Mindfulness ExercДокумент80 страницSTRESS - Craig Huffman - ACT Ultim Guide To Using ACT To Treat Stress, Includ Mindfulness ExercCarlos Silva100% (1)
- A Contextual Behavioral Guide To The Self (2019)Документ252 страницыA Contextual Behavioral Guide To The Self (2019)Fábio Vacaro CulauОценок пока нет
- ACT Forms Handout Andrews 2011Документ32 страницыACT Forms Handout Andrews 2011Anonymous Ax12P2sr100% (8)
- Mitment Therapy Skillstraining Manual For TherapistsДокумент322 страницыMitment Therapy Skillstraining Manual For TherapistsAlejandro Picco100% (8)
- J., Stewart, I., Martell, C., & Kaplan, J.S. (2014) - ACT and RFT in Relationships PDFДокумент298 страницJ., Stewart, I., Martell, C., & Kaplan, J.S. (2014) - ACT and RFT in Relationships PDFVartax100% (6)
- Learning Process-Based Therapy - NodrmДокумент169 страницLearning Process-Based Therapy - NodrmBrintrok100% (12)
- Mitch Fryling & Linda Hayes - Motivation in Behavior Analysis: A CritiqueДокумент9 страницMitch Fryling & Linda Hayes - Motivation in Behavior Analysis: A CritiqueIrving Pérez Méndez0% (1)
- Process Based CBT Digital ExamДокумент464 страницыProcess Based CBT Digital ExamPsico Orientador100% (6)
- Kirk D. Strosahl, Patricia J. Robinson, Thomas Gustavsson Brief Interventions For Radical Change Principles and Practice of Focused Acceptance and Commitment Therapy PDFДокумент297 страницKirk D. Strosahl, Patricia J. Robinson, Thomas Gustavsson Brief Interventions For Radical Change Principles and Practice of Focused Acceptance and Commitment Therapy PDFebiznes100% (18)
- The Big Book of ACT Metaphors-2014-1Документ250 страницThe Big Book of ACT Metaphors-2014-1cristian vargas100% (3)
- Problem Solving TherapyДокумент43 страницыProblem Solving Therapyjoseph_r9512Оценок пока нет
- Hayes. Learning ACT An Acceptance and Commitment Therapy Skills Training Manual For TherapistsДокумент466 страницHayes. Learning ACT An Acceptance and Commitment Therapy Skills Training Manual For TherapistsNuni95% (21)
- Wilson, D.S., Hayes, S.C. & Biglan, A. (2018). Evolution and contextual behavioral science an integrated framework for understanding, predicting and influencing human behavior. Oakland Context Press..pdfДокумент390 страницWilson, D.S., Hayes, S.C. & Biglan, A. (2018). Evolution and contextual behavioral science an integrated framework for understanding, predicting and influencing human behavior. Oakland Context Press..pdfjesus100% (3)
- Jason B. Luoma, Steven C. Hayes, Robyn D. Walser - Learning ACT - An Acceptance and Commitment Therapy Skills Training Manual For Therapists (2017, Context Press) PDFДокумент466 страницJason B. Luoma, Steven C. Hayes, Robyn D. Walser - Learning ACT - An Acceptance and Commitment Therapy Skills Training Manual For Therapists (2017, Context Press) PDFMurilo MartinsОценок пока нет
- Acceptance and Commitment Therapy For Individuals With DisabilitiesДокумент11 страницAcceptance and Commitment Therapy For Individuals With Disabilitiesjoao1504Оценок пока нет
- Nightmare Rehearsal and Sleep Hygiene - Russ Harris - WWW - imlearningACTДокумент7 страницNightmare Rehearsal and Sleep Hygiene - Russ Harris - WWW - imlearningACTRan AlmogОценок пока нет
- The Essential Guide To The ACT Matrix A StepbyStep Approach To Using The ACT Matrix Model in Clinical Practice NodrmДокумент365 страницThe Essential Guide To The ACT Matrix A StepbyStep Approach To Using The ACT Matrix Model in Clinical Practice NodrmRan Almog100% (21)
- How Is RO-DBT Different From DBT - NewHarbingerДокумент9 страницHow Is RO-DBT Different From DBT - NewHarbingerRan Almog50% (2)
- Chronic Pain ACTДокумент8 страницChronic Pain ACTRan AlmogОценок пока нет
- Hexaflex and TriflexДокумент3 страницыHexaflex and TriflexRan AlmogОценок пока нет
- ACT With DepressionДокумент9 страницACT With DepressionRan Almog100% (1)
- Baumeister - How The Self Became A ProblemДокумент14 страницBaumeister - How The Self Became A ProblemRan AlmogОценок пока нет
- Client Centered Assessment CaseДокумент5 страницClient Centered Assessment CaseHon “Issac” KinHoОценок пока нет
- Oswald in Youth HouseДокумент3 страницыOswald in Youth HouseGreg ParkerОценок пока нет
- Blackness and Disability Edited by Christopher BellДокумент171 страницаBlackness and Disability Edited by Christopher BellXian XianОценок пока нет
- Ham D PDFДокумент2 страницыHam D PDFNeach GaoilОценок пока нет
- Therapeutic ProcessДокумент24 страницыTherapeutic ProcessJavier Tracy Anne0% (1)
- Malignant Self LoveДокумент116 страницMalignant Self LoveIon Prinos100% (4)
- Letters CompДокумент5 страницLetters CompAnscarОценок пока нет
- Paul S. Appelbaum M.DДокумент54 страницыPaul S. Appelbaum M.DMarkingsonCaseОценок пока нет
- Behaviour Research and Therapy: Alan E. KazdinДокумент12 страницBehaviour Research and Therapy: Alan E. KazdinDroguОценок пока нет
- VoyeurismДокумент10 страницVoyeurismMilton ThiraviyamОценок пока нет
- Syllabus of Nursing Officer 2023Документ5 страницSyllabus of Nursing Officer 2023raviОценок пока нет
- Dissertation Proposal TextДокумент2 страницыDissertation Proposal TextJithin ThomasОценок пока нет
- Reflection Paper On Zion CentreДокумент2 страницыReflection Paper On Zion CentreDanielle Andrea CalderonОценок пока нет
- A Brief Overview of Four Principles of Neuropsychological Rehabilitation. George P. PrigatanoДокумент2 страницыA Brief Overview of Four Principles of Neuropsychological Rehabilitation. George P. PrigatanoGuillermo AlcaláОценок пока нет
- Gender Dysphoria and Social AnxietyДокумент9 страницGender Dysphoria and Social AnxietyJellybabyОценок пока нет
- A Mental Health Chatbot For Regulating Emotions (SERMO) - Concept and Usability TestДокумент12 страницA Mental Health Chatbot For Regulating Emotions (SERMO) - Concept and Usability TestMadhanDhonianОценок пока нет
- 7 Types of ADHD PDFДокумент3 страницы7 Types of ADHD PDFAamir Malik67% (3)
- (PPT) PSYCH - M - Theories of PersonalityДокумент93 страницы(PPT) PSYCH - M - Theories of PersonalitynikkiОценок пока нет
- Abnormal PsychologyДокумент8 страницAbnormal PsychologyLouise Agravio100% (1)
- Sensory BagДокумент3 страницыSensory Bagapi-541744798Оценок пока нет
- Sakhi Concept Note - WebsiteДокумент3 страницыSakhi Concept Note - WebsiteSuryamaniОценок пока нет
- Why Am I Always Angry?: Anger and The BrainДокумент4 страницыWhy Am I Always Angry?: Anger and The BrainSasidharan Rajendran100% (1)
- Borderline Personality Disorder Diagnosis and 2017 The Journal For Nurse PRДокумент2 страницыBorderline Personality Disorder Diagnosis and 2017 The Journal For Nurse PRracm89Оценок пока нет
- A Companion To Fish's Clinical PsychopathologyДокумент77 страницA Companion To Fish's Clinical PsychopathologyRobbydjan Christopher80% (5)
- Reactive Attachment Disorder PDFДокумент28 страницReactive Attachment Disorder PDFSerdar Serdaroglu100% (1)
- Dizzines - PregledniДокумент9 страницDizzines - PregledniInes StrenjaОценок пока нет
- Summary Report On Gestalt TherapyДокумент27 страницSummary Report On Gestalt Therapyconsult monz100% (2)
- DID Screening SheetДокумент5 страницDID Screening SheetIsaac CruzОценок пока нет
- Child Impact of Traumatic Event Scale EnglishДокумент3 страницыChild Impact of Traumatic Event Scale EnglishFloОценок пока нет
- 3 5326 Characteristics Matrix - InputДокумент6 страниц3 5326 Characteristics Matrix - Inputapi-313154885Оценок пока нет
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedОт EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedРейтинг: 5 из 5 звезд5/5 (81)
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionОт EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionРейтинг: 4 из 5 звезд4/5 (404)
- The Age of Magical Overthinking: Notes on Modern IrrationalityОт EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityРейтинг: 4 из 5 звезд4/5 (29)
- ADHD is Awesome: A Guide to (Mostly) Thriving with ADHDОт EverandADHD is Awesome: A Guide to (Mostly) Thriving with ADHDРейтинг: 5 из 5 звезд5/5 (2)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeОт EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeРейтинг: 2 из 5 звезд2/5 (1)
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsОт EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsОценок пока нет
- Love Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)От EverandLove Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)Рейтинг: 3 из 5 звезд3/5 (1)
- Why We Die: The New Science of Aging and the Quest for ImmortalityОт EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityРейтинг: 4 из 5 звезд4/5 (5)
- Manipulation: The Ultimate Guide To Influence People with Persuasion, Mind Control and NLP With Highly Effective Manipulation TechniquesОт EverandManipulation: The Ultimate Guide To Influence People with Persuasion, Mind Control and NLP With Highly Effective Manipulation TechniquesРейтинг: 4.5 из 5 звезд4.5/5 (1412)
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.От EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Рейтинг: 4.5 из 5 звезд4.5/5 (110)
- Mindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessОт EverandMindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessРейтинг: 4.5 из 5 звезд4.5/5 (328)
- Raising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsОт EverandRaising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsРейтинг: 4.5 из 5 звезд4.5/5 (170)
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsОт EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsРейтинг: 4 из 5 звезд4/5 (4)
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsОт EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsРейтинг: 5 из 5 звезд5/5 (1)
- The Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeОт EverandThe Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeРейтинг: 4.5 из 5 звезд4.5/5 (253)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaОт EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaРейтинг: 4.5 из 5 звезд4.5/5 (266)
- When the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisОт EverandWhen the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisРейтинг: 3.5 из 5 звезд3.5/5 (2)
- The Marshmallow Test: Mastering Self-ControlОт EverandThe Marshmallow Test: Mastering Self-ControlРейтинг: 4.5 из 5 звезд4.5/5 (59)
- Cult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryОт EverandCult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryРейтинг: 4 из 5 звезд4/5 (45)
- Outlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisОт EverandOutlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisРейтинг: 4 из 5 звезд4/5 (1)
- Empath: The Survival Guide For Highly Sensitive People: Protect Yourself From Narcissists & Toxic Relationships. Discover How to Stop Absorbing Other People's PainОт EverandEmpath: The Survival Guide For Highly Sensitive People: Protect Yourself From Narcissists & Toxic Relationships. Discover How to Stop Absorbing Other People's PainРейтинг: 4 из 5 звезд4/5 (95)
- Summary: Limitless: Upgrade Your Brain, Learn Anything Faster, and Unlock Your Exceptional Life By Jim Kwik: Key Takeaways, Summary and AnalysisОт EverandSummary: Limitless: Upgrade Your Brain, Learn Anything Faster, and Unlock Your Exceptional Life By Jim Kwik: Key Takeaways, Summary and AnalysisРейтинг: 5 из 5 звезд5/5 (8)
- Troubled: A Memoir of Foster Care, Family, and Social ClassОт EverandTroubled: A Memoir of Foster Care, Family, and Social ClassРейтинг: 4.5 из 5 звезд4.5/5 (27)
- Mind in the Making: The Seven Essential Life Skills Every Child NeedsОт EverandMind in the Making: The Seven Essential Life Skills Every Child NeedsРейтинг: 4 из 5 звезд4/5 (35)
- Sleep Stories for Adults: Overcome Insomnia and Find a Peaceful AwakeningОт EverandSleep Stories for Adults: Overcome Insomnia and Find a Peaceful AwakeningРейтинг: 4 из 5 звезд4/5 (3)
- The Secret of the Golden Flower: A Chinese Book Of LifeОт EverandThe Secret of the Golden Flower: A Chinese Book Of LifeРейтинг: 5 из 5 звезд5/5 (4)