Академический Документы
Профессиональный Документы
Культура Документы
Trends in Obstetric Anaesthesia in A Tertiary Hospital in Nigeria: A Four-Year Review
Оригинальное название
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Trends in Obstetric Anaesthesia in A Tertiary Hospital in Nigeria: A Four-Year Review
Авторское право:
Доступные форматы
IOSR Journal of Dental and Medical Sciences (IOSR-JDMS)
e-ISSN: 2279-0853, p-ISSN: 2279-0861.Volume 14, Issue 1 Ver. III (Jan. 2015), PP 72-76
www.iosrjournals.org
Trends in Obstetric Anaesthesia in a Tertiary Hospital in Nigeria:
A Four-Year Review
Bassey E. Edem1, StephenD Ngwan2, Donald U. Oshio1, Stephen A. Anzaku3
1
Department of Anaesthesia, Federal Medical Centre, Makurdi, Nigeria
Department of Obstetrics and Gynaecology, Federal Medical Centre, Makurdi, Nigeria
3
Department of Obstetrics and Gynaecology, College of Health Sciences, Bingham
University, Karu, Jos Campus, Jos, Nigeria
Abstract:
Background: Obstetric anaesthesia has a vital role in the outcome of obstetric surgeries and in the past three
decades, the pattern has changed from predominantly general anaesthesia to regional, mostly spinal,
anaesthesia. The objective of this study was to investigate the trends in obstetric anaesthesia practice in a
Federal Medical Centre and offer explanation for any change observed.
Materials And Methods: This was a retrospective study of the obstetric anaesthesia unit of the department of
anaesthesia and the labour ward of the hospital from 1stJanuary 2010 to 31st December,2013. Data extracted
from the records included the age of the parturients, indications for surgery, types of Caesarean section, types
of anaesthesia, the grade of anaesthetists, total deliveries and Caesarean section rates.
Results: The totaldelivery for the period was 11,003 and the Caesarean section rate was 15.5%.In 2010 and
2011, general anaesthesia was the main type of anaesthesia accounting for 76.2% and 76.7% respectively.
However, in 2012 there was a drastic reduction in the use of general anaesthesia to 33.5% while spinal rose
from 23.3% in 2011 to 66.5% in 2012. By 2013, 70.9% of the cases were done under spinal while 29.1% were
done under general anaesthesia.There was no mortality in 2010 and 2012. In 2011, there was 1 (0.2%)
mortality and 3 (0.6%) in 2013.
Conclusion: The first two years of the study revealed that most of the obstetric procedureswere done under
general anaesthesia and was predominantly practiced by Nurse Anaesthetists. The last two years showed
predominant use of spinal anaesthesia. This was as a result of the arrival of a Consultant Anaesthetist. Training
and retention of qualified physician practitioners is recommended.
Keywords: Trends, obstetric anaesthesia, spinal anaesthesia, Caesarean section
I.
Introduction
Over the last triennium, the pattern of obstetric anaesthesia has been moving from general anaesthesia
towards regional anaesthesia1. Regional obstetric anaesthesia can be done under spinal or epidural2. Spinal
anaesthesia has become predominant method of inducing anaesthesia for obstetric procedures 3.Spinal
anaesthesia has lots of advantages over general anaesthesia. A meta-analysis of studies in the literature has
shown that spinal anaesthesia is 16 times safer than general anaesthesia for obstetric procedures4. In a review of
ASA closed claims report over a ten year period, Hawkins found that spinal anaesthesia was associated with
decrease in high-severity injury claims than general anaesthesia1,4.Compared to general anaesthesia, regional
anaesthesia is associated with less maternal mortality4,5. The fewer drugs used in regional anaesthesia results in
fewer drug reactions. It allows for a more direct experience of childbirth by the parturients and faster neonatalmaternal bonding. It causes decreased blood loss thus reducing the need for blood transfusions5. The addition of
neuraxial opioids provides for excellent postoperative pain control6. Despite the numerous advantages of
regional anaesthesia, some resource-poor settings still show preponderance toward the use of general
anaesthesia7.
The objective of the study was to investigate the trend of anaesthesia administered for obstetric
procedures in the hospital under review and proffer explanation for any change in trend observed.
II.
Materials And Methods
Setting
The study was conducted at the department of anaesthesia of the Federal Medical Centre, Makurdi,
Benue State,Northcentral of Nigeria. With a bed space of 500, the hospital offers specialist medical and surgical
care to a population of5million people8. This is a tertiary hospital involved in the Residency Training
programme with accreditations in obstetrics and gynaecology, surgery, family medicine amongst others. It also
receives referrals from the neighbouring states of Taraba, Kogi, Nasarawa and Cross River.
DOI: 10.9790/0853-14137276
www.iosrjournals.org
72 | Page
Trends in obstetric anaesthesia in a tertiary hospital in Nigeria: a four-year review
Study design
This was a retrospective descriptive study of all the parturients who had Caesarean section in the
Federal Medical Centre, Makurdi,from January 2010 to December 2013. The anaesthetic and maternity records
of the hospital were reviewed. All those who had Caesarean sections in the hospital were included in the study.
Those who had spontaneous vaginal or assisted delivery in the operating room were excluded from the study.
Data Analysis
Data extracted from therecords included the Caesarean section rate andtotal deliveries.Information
extracted from those who had Caesarean section were the age of the parturients, the indication for surgery, type
of Caesarean section based on timing, type of anaesthesia and the grade of anaesthetists, and total yearly
deliveries.The data was analysed using descriptive statistics.
III.
Results
The total delivery was 2338 in 2010, 3144 in 2011, 2577 in 2012 and 2944 in 2013. The Caesarean rate
was 14.2% in 2010, 14.6% in 2011, 16.8% in 2012 and 16.2% in 2013. The mean Caesarean rate was 15.5%.
A total of 1701 anaesthetics were administered for the four-year period under review. Of these, 332 were done
in 2010, 459 in 2011, 433 in 2012 and 477 in 2013.
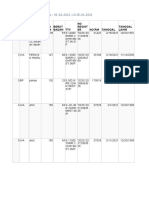
Fifty four per cent of the cases were done on parturients within the age range of 20-29 years whereas 2.2% of
the procedure was done on those forty years or older. (Table 1).
Table 1: Shows the age distribution of the parturients
Age of parturients
10-19
20-29
30-39
40
Not indicated
Total
frequency
64
919
574
37
107
1701
Percentage (%)
3.8
54.0
33.7
2.2
6.3
100
The commonest indication for Caesarean section was one or more previous sections as shown in table 2.
Table 2: showing the indications for Caesarean section
Indication for Operation
Cephalopelvic disproportion
Fetal distress
One or more previous C/S
Hypertensive disorders of pregnancy
Antepartum haemorrhage
Obstructed labour
Cord prolapse
Abnormal presentations/lie
Others
Total
Frequency
132
140
236
160
142
116
27
167
581
1701
Percentage (%)
7.8
8.2
13.9
9.4
8.3
6.8
1.6
9.8
34.2
100
Majority of the Caesarean sections were done as emergency as shown in table 3
Table 3 showing the type of Caesarean section based on timing
Type
Elective
Emergency
Total
Frequency
266
1435
1701
Percentage (%)
15.6
84.4
100
In 2010 and 2011, general anaesthesia was the main type of anaesthesia given for Caesarean section
accounting for 76.2 and 76.7% respectively. However, in 2012 there was a drastic reduction in the use of
general anaesthesia to 33.5% while spinal rose from 23.3% in 2011 to 66.5% in 2012. By 2013, 70.9% of the
cases were done under spinal while 29.1% were done under general anaesthesia. See figure 1.In 2010 and 2011,
most of the cases were done by nurse anaesthetists. In 2012, most of the cases were done by the Consultant
anaesthetist and Resident doctors. In 2013, the nurse anaesthetists did more of the cases. See table 5.
Table 5: Depicts the grade of Anaesthetists
Year
2010
2011
DOI: 10.9790/0853-14137276
Grade of anaesthetist
Nurse Anaesthetist
Resident
Consultant
Nurse Anaesthetist
Resident
Number of cases done
317
15
0
435
22
www.iosrjournals.org
73 | Page
Trends in obstetric anaesthesia in a tertiary hospital in Nigeria: a four-year review
2012
2013
Consultant
Nurse Anaesthetist
Resident
Consultant
Nurse Anaesthetist
Resident
Consultant
2
191
159
83
269
143
65
In 2010, intra-operative maternal mortality was zero while in 2011, there was one mortality (0.2%). In
2012, mortality was zero and in 2013 there were three mortalities (0.6%).
IV.
Limitations
The data were manually extracted as there is no computerised record keeping at the centre. In the first
two years of the study, the entire operations in the theatre were lumped into one record thus making the retrieval
of obstetric cases cumbersome. The record for 2010 and major part of 2011 did not differentiate the type of
general anaesthesia given. So both total intravenous anaesthesia and general anaesthesia with endotracheal
intubation were counted as general anaesthesia for the purpose of the review.
V.
Discussion
The commonest indication for elective Caesarean section in this study was one or more previous
sections which agree with most studies done in Nigeria9. Most of the Caesarean sections in the study were
emergencies. By 2010 and 2011, there was a predominance of general anaesthesia use for Caesarean sectionat
the centre under review with 76.2% and 76.6% of the cases being done under general anaesthesia respectively.
Spinal anaesthesia accounted for 23.8% and 23.4% of the cases respectively. Thisis in contrast with findings
from the surveys conducted in 1981 and 1992 by Hawkins et al that revealed that in the United States,
asignificant proportion of Caesarean sections were performed under regionalanaesthesia and there was a
corresponding decrease in those performed under general anaesthesia3. In a tertiary hospital in Boston, United
States, Palanisamy reported that only 0.5-1% of Caesarean section were done under general anaesthesia
indicating that almost all were done under regional anaesthesia10. That study further revealed that in half of the
very few who received general anaesthesia, a perceived lack of time to institute neuraxial block was the reason
for the institution of general anaesthesia.In a Singaporean maternity hospital in 2004, Kan reported a general
anaesthesia use of 20.4% for Caesarean delivery with close to 80% done under regional anaesthesia 11.
Studies coming out of the developing world tend to show a trend that was more of general anaesthesia.
In Malawi, Fenton reported that the trend of obstetric anaesthesia that was towards general anaesthesia was
associated with increased maternal and perinatal mortality7. In the University of Nigeria Teaching Hospital in
Eastern Nigeria, Okafor reported that by 2004, only 18% of the Caesarean deliveries were done under spinal
anaesthesia12. We found that the finding of a predominantly general anaesthesia-based obstetric delivery system
seemed to be common in most resource-poor settings. This is in spite of the fact that spinal anaesthesia has
become the gold standard for obstetric anaesthesia worldwide13. The finding of a mostly general as against
regional technique was due to a lack of skilled manpower to teach and sustain the practice of regional
anaesthesia technique at the centre. A related regional technique, the epidural, was found to have been used in
0.7% of cases in a district hospital in Nigeria out of a total of 2878 anaesthetics delivered over a two-year
period2.
In the hospital under review, there was no Consultant Anaesthetist on the employment of the hospital
as at 2010 and 2011. This accounted for the low percentage of cases done under spinal. The one or two nurse
anaesthetists who attempted to do the few spinals were discouraged by the complication of severe hypotension
that often followed the procedure.
During the years 2010 and 2011, the anaesthesia workforce was few and mostly Nurse Anaesthetists in
the centre under review. This accounted for the predominantly general anaesthesia that was entirely total
intravenous anaesthesia without any form of airway protection for the parturients. This again brings to the fore
the intractable problem of manpower development in anaesthesia. Okafor 14 observed that the ratio of
anaesthetists to the population in parts of the developing world is 1:300000 as compared to 1:10000 in the
Western world. As at the time of the study, there was only one Consultant Anaesthetist practicing in the entire
state with a population of about 5miliion 8.The problem of the dearth of manpower in anaesthesia is at the root of
poor development in anaesthesia and obstetric anaesthesia practice in particular in sub Saharan Africa14. In a
related study about the dearth of epidural anaesthesia skill in a district hospital in Abuja, Nigeria, Edem et al
observed that it was directly a result of the unavailability of physician anaesthetists to practice and teach the
skill to the few nurse anaesthetists who formed the bedrock of anaesthesia service delivery there2.
DOI: 10.9790/0853-14137276
www.iosrjournals.org
74 | Page
Trends in obstetric anaesthesia in a tertiary hospital in Nigeria: a four-year review
That over 70% of obstetric procedures were still done under general anaesthesia ten years into the third
millennium is a cause for concern. To bring the standard of care at the Centre to a global minimum, there was an
urgent need to appoint and retain a Consultant Anaesthetist for the Centre.
The trend in 2012 started to show a reversal of the general anaesthesia based obstetrics procedures
towards a more spinal based delivery system.See figure 1. Spinal anaesthesia use rose from 23.3% in 2011 to
66.5% of all anaesthetics given for Caesarean sections in 2012 in the Centre. This meant that general
anaesthesia decreased to 33.5% in that year down from 76.7% in 2011. This was a 286% increase. This finding
is in agreement with that of Okafor 12 in a teaching hospital in Eastern Nigeria where the rate of spinal use for
caesarean section rose from 18% in 2003 to 48% in 2004. However, while Okafor found 267% increase in the
rate of utilisation of spinal as against general anaesthesia, our study revealed 286% increase in use. The reversal
in the trend of obstetric anaesthesia was as a result of the arrival of a Consultant Anaesthetist by December 2011
at the Centre. A massive training programme for the Nurse Anaesthetists by the Consultant and posting of
Resident doctors to the department led to a change in the type of anaesthesia given to the parturients. The last
decade has witnessed the trend turning towards the use of spinal anaesthesia in many places in the Sub-region.
However, the rate of the use of general anaesthesia for Caesarean section, though greatly reduced at the Centre,
is still high compared to the United States and European rates. However, the rate seems to agree with the
findings in the study from Kan in Singapore11 and Chan in Malaysia15. In view of the international goal that 8090% of all Caesarean deliveries be done under spinal anaesthesia for the protection of future mothers 5, there is
need to sustain the practice of spinal anaesthesia at the Centre.
In 2013, the trend towards spinal anaesthesia continued to increase with a total of 70.9% of the cases
done under spinal anaesthesia in the centre under review. This figure tallies with the finding of Okafor who
reported a 71% use of spinal on the fourth year of their review in 2006.
The number of obstetric procedures handled by the nurses in 2010 was 317 out of the total 332 cases
handled in that year. A Resident doctor handled 15 of the cases. Since most of the nurses did not have the skill
at performing spinal anaesthesia, most of the cases were carried out under general anaesthesia. This accounted
for the low rate of spinal anaesthesia found in the study. There was no qualified Physician Anaesthetist to train
and supervise the Nurses. The same finding continued in 2011 with the Nurses handling most of the cases and
the spinal rate still low. However, by 2012, the number of cases handled by the nurses dropped. This was a
direct result of the arrival of a Consultant Anaesthetist who embarked on training of the Nurses in regional
anaesthetic techniques. Residents were also posted to the department who joined in receiving the training. The
result was the rapid increase in the use of spinal anaesthesia for obstetric procedures from 23% in 2010 to 66.5%
in 2012. As the nurses learned and perfected the skill in regional technique, the number of cases handled by
them again rose in 2012 as well as the rate of use of spinal anaesthesia.
The findings in this study show that the trend of obstetric anaesthesia in the Centre under review is
rapidly moving towards the global standards of a regional - driven obstetric anaesthesia service. This has been
as a result of the sourcing of appropriately trained physician anaesthesia manpower who worked hard to train the
others to conform to the global standards. There is therefore the need to train enough physicians to continue to
insist on standards of care to improve safety to both the parturients and the new-borns.
Acknowledgement
The authors wish to acknowledge the assistance of AdaOpita, a Registered Nurse Anaesthetist who
helped in the preparation of the script.
References
[1].
[2].
[3].
[4].
[5].
[6].
[7].
[8].
[9].
[10].
Davies JM. Obstetric Anesthesia Closed Claims Trends Over Last Three Decades. ASA Newsletter 2004; 68: 12-14.
Edem BE,Anzaku SA,Agan TU, Oku OO. Audit of epidural anaesthesia service at a district hospital in Nigeria. Highland Med Res J
2014; 14: 35-38.
Hawkins JL, Gibbs CP, Orleans M, et al. Obstetric anesthesia workforcesurvey, 1981 versus 1992. Anesthesiology1997; 87:135143.
Hawkins JL, Koonin LM, et al. Anesthesia related deaths during obstetric delivery in the United States, 1979-1990.
Anesthesiology1997; 86: 277-284.
Fyneface-Ogan S. Anesthesia for Cesarean Section. In: Salim R (ed) Cesarean Delivery. InTech, Available from
http://www.intechopen.com/books/cesareandelivery. Accessed on 23/10/14.
Eldridge J. Obstetric anaesthesia and analgesia. In: Allman KG, Wilson IH (eds). Oxford Handbook of Anaesthesia, 2 ed. Oxford,
Oxford University Press, 2007, 695-756.
Fenton PM, Whitty CJM, Reynolds F. Caesarean section in Malawi: Prospective study of early maternal and perinatal mortality. Br
Med J 2003; 327-337.
Population of Benue State of Nigeria 2006, National Population Commission, http://www.citypopulation.de/php/nigeriaadmin.php?adm1id=NGA007. Accessed 23/10/14, 19:07hours.
Chama CM, El-Nafaty AU, Idrisa A. Caesarean morbidity and mortality of Maiduguri, Nigeria. J ObstetGynaecol2000; 20: 45-48.
Palanisamy A, Mitani AA, Tsen LC. General anesthesia for cesarean delivery at a tertiary care hospital from 2000 to 2005: a
retrospective analysis and 10-year update. Int J ObstetAnesth 2011; 20: 10-16.
DOI: 10.9790/0853-14137276
www.iosrjournals.org
75 | Page
Trends in obstetric anaesthesia in a tertiary hospital in Nigeria: a four-year review
[11].
[12].
[13].
[14].
[15].
Kan RK, Lew E, Yeo SW, Thomas E. General anesthesiafor cesarean section in a Singapore maternity hospital: a retrospective
survey. Int J ObstetAnesth2004; 13: 221-226.
Okafor UV, Ezegwui HU, Ekwazi K. Trends of different forms of anaesthesia for caesarean section in South-eastern Nigeria. J
ObstetGynaecol 2009; 29: 392-395.
Dyer RA, Reed AR, James MF. Obstetric anaesthesia in low-resource setting. Best Practice & Research Clinical Obstetrics and
Gynaecology 2010; 24: 401-412.
OkaforUV. Evolution of obstetric anaesthesia in West Africa: current trends.Int J ObstetAnesth2006; 15: 175.
Chan YK, Ng KP, Chiu CL. Trends in obstetric anaesthesia and analgesia over a ten year period in the University Malaya Medical
Centre, Kuala Lumpur. Int J ObstetAnesth 2002; 11: 176-179.
Figure 1: Bar Chart Showing Trend Of Obstetric Anaesthesia 2010-2013
DOI: 10.9790/0853-14137276
www.iosrjournals.org
76 | Page
Вам также может понравиться
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryОт EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryРейтинг: 3.5 из 5 звезд3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)От EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Рейтинг: 4.5 из 5 звезд4.5/5 (119)
- Never Split the Difference: Negotiating As If Your Life Depended On ItОт EverandNever Split the Difference: Negotiating As If Your Life Depended On ItРейтинг: 4.5 из 5 звезд4.5/5 (838)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaОт EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaРейтинг: 4.5 из 5 звезд4.5/5 (265)
- The Little Book of Hygge: Danish Secrets to Happy LivingОт EverandThe Little Book of Hygge: Danish Secrets to Happy LivingРейтинг: 3.5 из 5 звезд3.5/5 (399)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyОт EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyРейтинг: 3.5 из 5 звезд3.5/5 (2219)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeОт EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeРейтинг: 4 из 5 звезд4/5 (5794)
- Team of Rivals: The Political Genius of Abraham LincolnОт EverandTeam of Rivals: The Political Genius of Abraham LincolnРейтинг: 4.5 из 5 звезд4.5/5 (234)
- The Emperor of All Maladies: A Biography of CancerОт EverandThe Emperor of All Maladies: A Biography of CancerРейтинг: 4.5 из 5 звезд4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreОт EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreРейтинг: 4 из 5 звезд4/5 (1090)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersОт EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersРейтинг: 4.5 из 5 звезд4.5/5 (344)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceОт EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceРейтинг: 4 из 5 звезд4/5 (890)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureОт EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureРейтинг: 4.5 из 5 звезд4.5/5 (474)
- The Unwinding: An Inner History of the New AmericaОт EverandThe Unwinding: An Inner History of the New AmericaРейтинг: 4 из 5 звезд4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)От EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Рейтинг: 4 из 5 звезд4/5 (98)
- PHYSIOLOGY OF PREGNANCYДокумент50 страницPHYSIOLOGY OF PREGNANCYEvy Wulandari100% (3)
- Episiotomy and Perineal TearsДокумент21 страницаEpisiotomy and Perineal TearsJeevan VelanОценок пока нет
- Youth Entrepreneurship: Opportunities and Challenges in IndiaДокумент5 страницYouth Entrepreneurship: Opportunities and Challenges in IndiaInternational Organization of Scientific Research (IOSR)100% (1)
- Maternity Workbook Summer NUR 2021Документ26 страницMaternity Workbook Summer NUR 2021ghaidaaОценок пока нет
- Effects of Formative Assessment On Mathematics Test Anxiety and Performance of Senior Secondary School Students in Jos, NigeriaДокумент10 страницEffects of Formative Assessment On Mathematics Test Anxiety and Performance of Senior Secondary School Students in Jos, NigeriaInternational Organization of Scientific Research (IOSR)100% (1)
- Test Bank For Maternal Child Nursing Care 6th Edition by PerryДокумент36 страницTest Bank For Maternal Child Nursing Care 6th Edition by Perrygoodgeonneogaeanjlf6y100% (38)
- Factors Affecting Success of Construction ProjectДокумент10 страницFactors Affecting Success of Construction ProjectInternational Organization of Scientific Research (IOSR)Оценок пока нет
- Nursing Care of A Postpartal Woman and FamilyДокумент44 страницыNursing Care of A Postpartal Woman and FamilyEvelyn Medina100% (1)
- Q1MCN - NurseslabsДокумент4 страницыQ1MCN - NurseslabsdhodejunlОценок пока нет
- The Effect of Instructional Methods and Locus of Control On Students' Speaking Ability (An Experimental Study in State Senior High School 01, Cibinong Bogor, West Java)Документ11 страницThe Effect of Instructional Methods and Locus of Control On Students' Speaking Ability (An Experimental Study in State Senior High School 01, Cibinong Bogor, West Java)International Organization of Scientific Research (IOSR)Оценок пока нет
- Study The Changes in Al-Ahwaz Marshal Using Principal Component Analysis and Classification TechniqueДокумент9 страницStudy The Changes in Al-Ahwaz Marshal Using Principal Component Analysis and Classification TechniqueInternational Organization of Scientific Research (IOSR)Оценок пока нет
- Philosophical Analysis of The Theories of Punishment in The Context of Nigerian Educational SystemДокумент6 страницPhilosophical Analysis of The Theories of Punishment in The Context of Nigerian Educational SystemInternational Organization of Scientific Research (IOSR)Оценок пока нет
- Project Based Learning Tools Development On Salt Hydrolysis Materials Through Scientific ApproachДокумент5 страницProject Based Learning Tools Development On Salt Hydrolysis Materials Through Scientific ApproachInternational Organization of Scientific Research (IOSR)Оценок пока нет
- Development of Dacum As Identification Technique On Job Competence Based-Curriculum in High Vocational EducationДокумент5 страницDevelopment of Dacum As Identification Technique On Job Competence Based-Curriculum in High Vocational EducationInternational Organization of Scientific Research (IOSR)Оценок пока нет
- Enhancing Pupils' Knowledge of Mathematical Concepts Through Game and PoemДокумент7 страницEnhancing Pupils' Knowledge of Mathematical Concepts Through Game and PoemInternational Organization of Scientific Research (IOSR)Оценок пока нет
- Students' Perceptions of Grammar Teaching and Learning in English Language Classrooms in LibyaДокумент6 страницStudents' Perceptions of Grammar Teaching and Learning in English Language Classrooms in LibyaInternational Organization of Scientific Research (IOSR)Оценок пока нет
- Need of Non - Technical Content in Engineering EducationДокумент3 страницыNeed of Non - Technical Content in Engineering EducationInternational Organization of Scientific Research (IOSR)Оценок пока нет
- Necessary Evils of Private Tuition: A Case StudyДокумент6 страницNecessary Evils of Private Tuition: A Case StudyInternational Organization of Scientific Research (IOSR)Оценок пока нет
- Child Mortality Among Teenage Mothers in OJU MetropolisДокумент6 страницChild Mortality Among Teenage Mothers in OJU MetropolisInternational Organization of Scientific Research (IOSR)Оценок пока нет
- Geohydrological Study of Weathered Basement Aquifers in Oban Massif and Environs Southeastern Nigeria: Using Remote Sensing and Geographic Information System TechniquesДокумент14 страницGeohydrological Study of Weathered Basement Aquifers in Oban Massif and Environs Southeastern Nigeria: Using Remote Sensing and Geographic Information System TechniquesInternational Organization of Scientific Research (IOSR)Оценок пока нет
- Microencapsulation For Textile FinishingДокумент4 страницыMicroencapsulation For Textile FinishingInternational Organization of Scientific Research (IOSR)Оценок пока нет
- Comparison of Psychological Variables Within Different Positions of Players of The State Junior Boys Ball Badminton Players of ManipurДокумент4 страницыComparison of Psychological Variables Within Different Positions of Players of The State Junior Boys Ball Badminton Players of ManipurInternational Organization of Scientific Research (IOSR)Оценок пока нет
- Comparison of Explosive Strength Between Football and Volley Ball Players of Jamboni BlockДокумент2 страницыComparison of Explosive Strength Between Football and Volley Ball Players of Jamboni BlockInternational Organization of Scientific Research (IOSR)Оценок пока нет
- Investigation of Wear Loss in Aluminium Silicon Carbide Mica Hybrid Metal Matrix CompositeДокумент5 страницInvestigation of Wear Loss in Aluminium Silicon Carbide Mica Hybrid Metal Matrix CompositeInternational Organization of Scientific Research (IOSR)Оценок пока нет
- Comparison of Selected Anthropometric and Physical Fitness Variables Between Offencive and Defencive Players of Kho-KhoДокумент2 страницыComparison of Selected Anthropometric and Physical Fitness Variables Between Offencive and Defencive Players of Kho-KhoInternational Organization of Scientific Research (IOSR)Оценок пока нет
- Lipoproteins and Lipid Peroxidation in Thyroid DisordersДокумент6 страницLipoproteins and Lipid Peroxidation in Thyroid DisordersInternational Organization of Scientific Research (IOSR)Оценок пока нет
- Advancing Statistical Education Using Technology and Mobile DevicesДокумент9 страницAdvancing Statistical Education Using Technology and Mobile DevicesInternational Organization of Scientific Research (IOSR)Оценок пока нет
- Study of Effect of Rotor Speed, Combing-Roll Speed and Type of Recycled Waste On Rotor Yarn Quality Using Response Surface MethodologyДокумент9 страницStudy of Effect of Rotor Speed, Combing-Roll Speed and Type of Recycled Waste On Rotor Yarn Quality Using Response Surface MethodologyInternational Organization of Scientific Research (IOSR)Оценок пока нет
- A Review On Refrigerants, and Effects On Global Warming For Making Green EnvironmentДокумент4 страницыA Review On Refrigerants, and Effects On Global Warming For Making Green EnvironmentInternational Organization of Scientific Research (IOSR)Оценок пока нет
- Application of Xylanase Produced by Bacillus Megaterium in Saccharification, Juice Clarification and Oil Extraction From Jatropha Seed KernelДокумент8 страницApplication of Xylanase Produced by Bacillus Megaterium in Saccharification, Juice Clarification and Oil Extraction From Jatropha Seed KernelInternational Organization of Scientific Research (IOSR)Оценок пока нет
- Comparative Effect of Daily Administration of Allium Sativum and Allium Cepa Extracts On Alloxan Induced Diabetic RatsДокумент6 страницComparative Effect of Daily Administration of Allium Sativum and Allium Cepa Extracts On Alloxan Induced Diabetic RatsInternational Organization of Scientific Research (IOSR)Оценок пока нет
- Core Components of The Metabolic Syndrome in Nonalcohlic Fatty Liver DiseaseДокумент5 страницCore Components of The Metabolic Syndrome in Nonalcohlic Fatty Liver DiseaseInternational Organization of Scientific Research (IOSR)Оценок пока нет
- Auxin Induced Germination and Plantlet Regeneration Via Rhizome Section Culture in Spiranthes Sinensis (Pers.) Ames: A Vulnerable Medicinal Orchid of Kashmir HimalayaДокумент4 страницыAuxin Induced Germination and Plantlet Regeneration Via Rhizome Section Culture in Spiranthes Sinensis (Pers.) Ames: A Vulnerable Medicinal Orchid of Kashmir HimalayaInternational Organization of Scientific Research (IOSR)Оценок пока нет
- Research Analysis On Sustainability Opportunities and Challenges of Bio-Fuels Industry in IndiaДокумент7 страницResearch Analysis On Sustainability Opportunities and Challenges of Bio-Fuels Industry in IndiaInternational Organization of Scientific Research (IOSR)Оценок пока нет
- Parametric Optimization of Single Cylinder Diesel Engine For Specific Fuel Consumption Using Palm Seed Oil As A BlendДокумент6 страницParametric Optimization of Single Cylinder Diesel Engine For Specific Fuel Consumption Using Palm Seed Oil As A BlendInternational Organization of Scientific Research (IOSR)Оценок пока нет
- Ethiopia MDSR Revised GuidelinesДокумент83 страницыEthiopia MDSR Revised GuidelinesAnonymous zDhsgt100% (1)
- Resume CompleteДокумент4 страницыResume Completeapi-382457984Оценок пока нет
- Nursing Practice II - Community Health Nursing and Care of The Mother and Child - RNpediaДокумент13 страницNursing Practice II - Community Health Nursing and Care of The Mother and Child - RNpediaBrianMarBeltranОценок пока нет
- FMGE DEC - 2019 (WWW - Medmutant.xyz)Документ46 страницFMGE DEC - 2019 (WWW - Medmutant.xyz)aditya jyothisОценок пока нет
- IUGR New Concepts - AJOG Review PDFДокумент13 страницIUGR New Concepts - AJOG Review PDFivanОценок пока нет
- Midwife Essay TopicsДокумент1 страницаMidwife Essay Topicsmal6640Оценок пока нет
- Benefits of Women in Zambian EmployementДокумент10 страницBenefits of Women in Zambian EmployementFrancis MbeweОценок пока нет
- Procedure For Vaginal Examination 2.1 PDFДокумент8 страницProcedure For Vaginal Examination 2.1 PDFAlfonso AnggriawanОценок пока нет
- Annotated Bib-BirthingДокумент3 страницыAnnotated Bib-Birthingapi-312719022Оценок пока нет
- Fetal DistressДокумент48 страницFetal DistressLenny SucalditoОценок пока нет
- Third Trimester Workup and Dr. Pratima Mittal's AlgorithmsДокумент37 страницThird Trimester Workup and Dr. Pratima Mittal's AlgorithmsAparna MohanОценок пока нет
- Stages of LaborДокумент12 страницStages of LabortejaОценок пока нет
- Model Answer Final Exame 2013 Reproductive Health NursingДокумент18 страницModel Answer Final Exame 2013 Reproductive Health NursingadamОценок пока нет
- Endalews CV CredentialsДокумент18 страницEndalews CV CredentialsAmoure TubeeОценок пока нет
- REPUBLIC ACT No 11148Документ15 страницREPUBLIC ACT No 11148Ann Manalocon100% (1)
- CHAPTER 3 WH QuestionДокумент4 страницыCHAPTER 3 WH Questiondarajati septia wОценок пока нет
- Hepatitis B Immunization Coverage Evaluation Amongst 12 23 Months Slum Children of Delhi, IndiaДокумент284 страницыHepatitis B Immunization Coverage Evaluation Amongst 12 23 Months Slum Children of Delhi, IndiaAnonymous x8fY69Crn100% (2)
- Laporan Kunjungan Pustu KlampokДокумент61 страницаLaporan Kunjungan Pustu Klampokranggie nindya slamanthaОценок пока нет
- Pregnant Over 40Документ31 страницаPregnant Over 40Daniel Andre S. SomorayОценок пока нет
- AnnualSummaryofVS20001307 Full PDFДокумент14 страницAnnualSummaryofVS20001307 Full PDFchupitoОценок пока нет
- Severe Tear Patient HandoutДокумент12 страницSevere Tear Patient HandoutIzz ShuhaimiОценок пока нет
- Dolichocephaly - Understanding Breech Head' Molding - The Midwife, The Mother and The BreechДокумент3 страницыDolichocephaly - Understanding Breech Head' Molding - The Midwife, The Mother and The BreechBianca LauraОценок пока нет
- Gupta, Charu - Women in Nazi GermanyДокумент10 страницGupta, Charu - Women in Nazi GermanyClara LimaОценок пока нет
- 9 - Clinical Management (STRATOG 2015 SBAs)Документ12 страниц9 - Clinical Management (STRATOG 2015 SBAs)w yОценок пока нет