Академический Документы
Профессиональный Документы
Культура Документы
The Initial Distribution Volume of Glucose and Cardiac Output in The Critically Ill
Загружено:
Cristina LopezИсходное описание:
Оригинальное название
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
The Initial Distribution Volume of Glucose and Cardiac Output in The Critically Ill
Загружено:
Cristina LopezАвторское право:
Доступные форматы
28
The initial distribution
volume of glucose and
cardiac output in the
critically ill
Blood or plasma glucose concentration can be measured
accurately and rapidly. However, after a glucose challenge
metabolism may modify glucose kinetics, so that glucose has
not been used as an indicator for dilution volumetry. To test
the hypothesis that the initial distribution volume of glucose
(IDVG) reflects cardiac output rather than glucose metabolism
in the critically ill, the relationship between IDVG and thermodilution cardiac output was evaluated at 27 points in 13
non-surgical, critically ill patients without congestive heart failure. The IDVG was calculated from incremental plasma glucose
concentrations using a one compartment model. Correlations
were obtained between the IDVG and cardiac output (r = 0.89,
n = 27, P < 0.001), and between the incrementalplasma glucose concentrations three minutes after the injection and the
IDVG (r = 0.94, n = 27, P < 0.001). No difference was found
between the IDVG with or without continuous insulin infusions. The results indicate that the IDVG reflects cardiac output
rather than glucose metabolism in patients without congestive
heart failure.
ll est possible de mesurer la concentration plasmatique du glucose avec prdcision et rapiditd. Cependent, apr~s un test dTzyperglycdmie provoqude, le mdtabolisme peut modifier le cyndtique du glucose. Pour cette raison le glucose n'est pas employd
comme indicateur pour l'analyse volumdtrique par la mdthode
de dilution. Pour vdrifier 17~ypoth~se selon laquelle le volume
de distribution initial du glucose (VDIG) reflkte le debit cardiaque plutrt que le mdtabolisme glucidique chez le grand real-
Key words
INTENSIVECARE"
MEASUREMENTTECHNIQUES:cardiac output;
METABOLISM"glucose;
PHARMACOK1NET1CS:distribution
From: the Department of Anesthesiology,Universityof
Hirosaki, School of Medicine, Hirosaki-Shi, Aomori-Ken,036
Japan
Address correspondence to: Dr. Ishihara, Current address:
Department of Anesthesiology,Southwestern Medical Center,
5323 Harry Hines Blvd., Dallas, Tx 75235. Fax 214/590-6945.
Acceptedfor publication 4th September, 1992.
CAN J ANAESTH 1993 / 40:1 / pp 28-31
I-lironori Ishihara MD, Yuki Shimodate MD,
Himaki Koh MD, Ken-ichi Isozaki MD,
Toshihito Tsubo MD, Akitomo Matsuki MD
ade, la relation entre VDIG et debit cardiaque est compar~e
27 moments chez 13 grands malades non chirurgicaux sans insuffisance cardiaque. Le VDIG est calcul~ ~ partir de concentrations plasmatiques croissantes dans un modble ~ compartiment unique. On d~termine la correlation entre VDIG et d~bit
cardiaque (r = 0,89, n = 27, P <0,001), et entre les concentrations croissantes de glucose plasmatique trois minutes aprbs
l~njection et le VDIG (r = 0,94, n = 27, P < 0,001). II n'y
a pas de diffdrence entre le VDIG mesur~ avec ou sans perfusions d'insuline. Les rdsultats d~montrent que le VDIG reflkte
plus le d~bit cardiaque que le m&abolisme glucidique chez le
malade qui ne pr~sente pas d'insuffisance cardiaque.
The initial volume of distribution, or the central compartment of the kinetic description of drug disposition,
is that volume in which a drug appears to mix instantaneously before being distributed throughout the remainder of its distribution volume by mixing, flow, and diffusion. 1 One may speculate that the initial volume of
distribution for several drugs is composed mainly of the
blood volume and the vessel rich group of tissues, and
is determined by cardiac output, regional blood flow and
the characteristics of a particular drug. 2 After an intravenous bolus injection, drug concentrations in blood may
be higher in individuals with poor perfusion (e.g., shock)
than individuals with better perfusion. 3 Presumably, cardiac output plays an important role in determining the
initial distribution volume of the administered drugs.
Glucose itself appears in the blood physiologically and
can be given repeatedly and safely in small amounts even
in critically ill patients. Accurate and rapid blood glucose
determinations have also become available in the ICU.
However, complicating factors involving glucose ufiliTation and/or endogenous glucose production in the body
may modify plasma glucose concentrations shortly after
a glucose challenge in critically ill patients, and thus the
initial distribution volume of glucose (IDVG) may fail
to reflect cardiac output.
The purpose of the present study was to test the hypothesis that the IDVG reflects cardiac output in critically
ill patients.
Ishihara et al.: THE
I N I T I A L D I S T R I B U T I O N VOLUME OF GLUCOSE AND C A R D I A C OUTPUT IN TH E C R I T I C A L L Y ILL
Methods
Patients
The protocol was approved by the ethical committee of
the University of Hirosaki School of Medicine and each
patient gave informed consent. Patients eligible for inclusion in this study had a thermodilution pulmonary
artery catheter inserted for clinical indications unrelated
to this study. Thirteen non-surgical patients admitted to
the general ICU were enrolled. Post-surgical patients, patients with hyperglycaemia (plasma glucose concentration
>25 mmol. L-I), or patients with congestive heart failure
judged from high pulmonary artery wedge pressure (>20
mmHg), echocardiogram or chest x-ray examination were
excluded from the study. Ten patients were on vasoactive
drugs and two patients required continuous insulin infusions (Table 1). A total of 27 comparisons between the
IDVG and the thermodilution cardiac output were performed.
Methods
A bolus of 25 ml glucose, 20% (5g), was given over 30
sec through the proximal injectate port of a balloon-tip,
flow-directed pulmonary artery catheter (Baxter Model
93A0-741 H-7.5F) which was placed in the right internal
jugular vein. A glucose solution (5-22%) for routine nutritional support was also infused through another central
venous line using an electric pump at a constant rate,
ranging from 0.1 g. kg -1- hr -1 to 0.4 g. kg -I 9hr -l at least
one hour before the 5g glucose challenge and throughout
the procedure. The cardiovascular state remained unchanged throughout the procedures, judged from the
ECG monitor and direct arterial pressure recordings. Serial blood samples were obtained, through an indwelling
radial artery catheter, immediately before and three, five
and seven minutes after the glucose injection. Isotonic
saline with small amounts of heparin was used to flush
the arterial line. Each 2 ml blood sample was collected
in a heparinized syringe and plasma was separated immediately by centrifuge. Plasma glucose concentrations
were determined using a glucose oxidase method (Fuji
Co. Ltd. Glu 20 glucose analyzer). All measurements
in the sample were performed in duplicate and averaged.
The coefficient of variation was less than 1% for repeated
glucose measurements (range: 4-17 retool. L-I).
Calculation of the IDVG
The IDVG was calculated using a one compartment
model from the excess or incremental plasma glucose
decay curve after glucose administration. In the one compartment model, the volume of distribution (Vd) is calculated as follows:
Vd = Dose/C0
29
where Dose = amount of drug administered. Co = initial
plasma concentration at time zero after instantaneously
distribution, but before the start of elimination 2. The
IDVG was determined using a "least squares" regression
technique to find the line of best fit. Residuals were
weighted by the inverse-square of the plasma levels. Residual sums of squares (SS) for each curve were examined
to evaluate the exponential term of the pharmacokinetic
model, 4 and convergence was assumed when the relative
change in the weighted sum of squares was less than
1 X 10-2.
Calculation of cardiac output
Thermodilution cardiac output was measured using a
balloon-tip flow-directed pulmonary artery catheter (Baxter Model 93A-741 H-7.5F). The correct position of each
catheter was confirmed by pressure tracings and chest
x-ray examination. Cardiac output was determined by
triplicate measurements with 10 ml isotonic saline solution
at < 12~ C injected in less than four seconds immediately
after the completion of taking blood samples for glucose
determinations. The thermal signals were analyzed using
a cardiac output computer (Baxter SAT2). The correlation of variation for repeated measurements was less
than 6%.
All equipment including the glucose analyzer were calibrated according to manufacturer's recommendations
before and after the study. Numerical data were analyzed
for Mean 5: SD and linear regression. A P value of
< 0.05 identified statistically significant differences.
Results
The mean plasma glucose concentration immediately before the glucose injection was 10.9 + 3.6 mmol. L -1. The
concentration reached 14.1 + 3.9 mmol. L -l three minutes after the injection, 13.6 -I- 3.8 mmol. L -1 at five
minutes, and 13.3 + 3.8 mmol- L -1 at seven minutes.
The residual sums of squares (SS) for each IDVG
curve were less than 7 10 -3, which was small enough
to allow a one compartment model fit. The IDVG and
thermodilution cardiac output varied markedly among
the patients, ranging from 3.4 L to 11.6 L for the IDVG,
and ranging from 1.3 L . min -I to 14.0 L . rain -l for the
cardiac output, respectively.
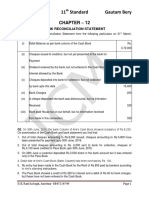
Correlations were obtained between the IDVG and
cardiac output (r = 0.89, P < 0.001) (Figure 1), and
between the incremental glucose concentrations at three
minutes postinjection and the IDVG (r = 0.94, P <
0.001) (Figure 2). No correlation was found between the
IDVG and the preinjection plasma glucose concentration
(r = 0.007). No difference was found between the IDVG
with or without continuous infusions of insulin or vasoactive drugs.
CANADIAN JOURNAL OF ANAESTHESIA
30
TABLE Patientcharacteristics
No
Age
M/ F
Diagnosis
45
21
26
73
47
39
23
79
62
73
75
30
75
F
M
M
F
M
M
M
M
M
M
M
M
M
Post CPR
Post CPR
Burn
Burn
Burn
Adrenal crisis
Chest injury
ARDS
Bronchialasthma
Aspiration pneumonitis
AMI
Sepsis
Hypovolaemia
2
3
4
5
6
7
8
9
10
I1
12
13
Vasoactive drugs
(#g " kg-1" rain-t)
Comparisons
1
3
1
2
5
3
3
2
2
1
1
2
1
Insulin
(U" hr-I)
NE2, DOAI0
NE0.4-2.0
DOA3-10
3-4
2-5
DOAI0
DOB3
E0.1,TheoS.5
E0.5
DOA3
DOA4
DOAI0
CPR: Cardio-Pulmonary Resuscitation,ARDS: Adult Respiratory Distress Syndrome, AMI: Actute MyocardialInfarction, NE: Norepinephrine,
E: Epinephrine, DOA: Dopamine, DOB: Dohutamine, Theo: Theophylline
IDVG(I)
CO (I.min "1)
15
Y = 1.27X - 2.87
r = 0,89
1]
n=27
10
9
Y=- 1.98X+ 14.60
"\
%\
r=-0.94
n=27
7
2
;o
il
IDVG (I)
FIGURE 1 Relationshipbetween the initial distribution volume of
glucose (IDVG) and cardiac output (CO)
OD
Discussion
The present study demonstrated that (1) the residual sums
(SS) of each I D V G curve were small enough to allow
a one compartment model to be fit, that (2) the I D V G
and cardiac output varied markedly among patients, and
(3) that a close relationship was observed between the
I D V G and thermodilution cardiac output. A one compartment model, however, is a gross over-simplification
for most drugs. Models for glucose distribution and utilization in m a n contain at least two glucose pools, one
of which turns over slowly, and is insulin dependent. The
other, fast pool, may be divided into blood and an r
travascular spaoes, and is insulin independent, s'6 In the
present study all data were collected after the three min-
2
1
Incremental Plasma Glucose Concentration
at three minutes Postinjection
FIGURE 2 Relationshipbetween the incrementalplasma glucose
concentration at three minutes postinjcctionand the initial distribution
volume of glucose(IDVG)
Ishihara et aL: .THE I N I T I A L DISTRIBUTION VOLUME OF GLUCOSE AND CARDIAC OUTPUT IN THE CRITICALLY ILL 31
utes postinjeetion in order to ensure that the assumption
of complete mixing within the initial distribution volume
is satisfied, 5,7 and postequilibration data within the seven
minutes postinjection were fitted to a one compartment
model because a fast pool is thought to be uniformly
mixed within 10 to 15 min. 5
The initial distribution volume for several drugs is determined by cardiac output, regional blood flow and the
characteristics of a particular drug.2 The present results
also suggested that cardiac output plays an important
role in determining the IDVG. Using a four compartment
model proposed by Cunningham and Heath 5 the fast pool
might be 174-188 ml. kg -I of blood when cardiac output
was assigned 100 ml. kg q.
Although 14C labeled glucose has been reported as an
indicator to measure the extracellular water content, Sglucose has not been used as an indicator in dilution volumetry because the plasma glucose concentration after
glucose injection may be influenced by glucose utilization,
endogenous glucose production and the continuous infusion of glucose throughout the procedure. However,
these modifying factors might be negligible judged from
the observations that (1) no consistent relationship was
obtained between the IDVG and the plasma glucose concent.ration immediately before the glucose bolus was
given, and (2) no differences in the IDVG values were
observed with or without insulin infusions in the present
study. In our previous study9 no consistent relationship
was observed between the IDVG and plasma insulin concentrations during and after abdominal surgery. However,
tracer techniques are required to determine the role of
these modifications accurately.
Although all data in the present study were derived
from uncontrolled critically ill patients, cardiac output
can be grossly predicted by the IDVG (r = 0.89) without
a thermodilution pulmonary catheter, and the IDVG can
be predicted by only two plasma glucose determinations
(r = --0.94): immediately before glucose is given and three
minutes after the injection.
We l~ reported that a relationship between the IDVG
and cardiac output (r = 0.65, P < 0.05) was observed
in a patient with phaeochromocytoma who showed
marked haemodynamic instability during the peroperaive
period with an excessive accumulation of fluids. In addition, during the period of the present study are patient
who had obvious congestive heart failure showed decreases in cardiac output (2-3 L- min -t) despite increases
in the IDVG (6-7 L), and the patient was not included
in the present study. Thus, we excluded post surgical patients as well as patients with apparent congestive heart
failure from the present study. However, we could not
convincingly demonstrate that patients in the present
study did not have some fluid accumulation. Further
study is required to examine the effect of fluid accumulation on the IDVG and cardiac output.
In conclusion, the present results indicate that the
IDVG and thermodilution cardiac output in the critically
ill vary markedly among patients, and support the hypothesis that the IDVG in patients, without obvious congestive heart failure, reflects cardiac output rather than
glucose metabolism.
Acknowledgements
The authors wish to thank Professor Y. Tanaka (Kyoto,
Japan), and Emeritus Professor J. McIntyre (Edmonton,
Canada), Professor D. Grimaud (Nice, France) and Dr.
E. Major (Swansea, UK) for their valuable comments,
Y. Satoh for his technical assistance, and Miss M. Kudoh
for her secretarial help.
References
1 Riggs DS. The mathematical approach to physiological
8
9
problems: a critical primer. Cambridge, MA: MIT press,
1963.
Ghoneim M, Pearson K. Pharmacokinetics of drugs administered intravenously.In: Scurf C, Feldman S, Soni N
(Eds). ScientificFoundations of Anaesthesia, 4th ed.,
Chicago: Year Book Medical Publishers, 1990: 559-71.
Bermet LZ, Sheiner LB. Pharmacokinetics:The dynamics
of drug absorption, distribution, and elimination.In:
Goodman Gilman A, Goodman LS, Rail TW, Murad F
(Eds). The Pharmacological Basis of Therapeutics., New
York: Macmillian Publishing Co., 1985: 3-34.
Yamaoka K, Tanigawara Y, Nakagawa T. Uno T. A pharmacokinetic analysis program (MULTI) for microcomputer. J Pharm Dyn 1981; 4: 879-85.
Cunningham VZ Heath DE An interpretation of the
intravenous glucose tolerance test in the light of recent findings on the kinetics of glucose and insulin in man. Clin Sci
Mol Med 1978; 54: 161-73.
Cobelli C, Bier DM, Ferrannini E. Modeling glucose metabolism in man: Theory and Practice. Horm Metab Res
(Sup#) 1990; 24: 1-10.
Avram M J, Krejcie TC, Henthorn TK. The relationship of
age to the pharmacokineticsof early drug distribution: The
concurrent disposition of thiopental and indocyaninegreen.
Anesthesiology 1990; 72: 403-11.
Wick AN,, Drury DR, Mackay EM. Glucose space of the
body. Am J Physiol 1950; 163: 224-8.
Ishihara H, Tanioka E Katagai H, et al. Effectsof and surgery on glucose space in man. Jap J Anesth 1986;35: 1057--60.
10 lshihara H, Tanioka F, Isozaki K, Matsuki A, Oyama T.
Postoperative management of diabetic patients in 1CU. In:
Matsuki A, Ishihara H, Oyama T (Eds). Endocrine
Response to Anesthesia and Intensive Care. Amsterdam:
Elsevier Science Publishers, 1990: 221--6.
Вам также может понравиться
- Hyperglycemia and Neurological Outcome in Patients With Head InjuryДокумент7 страницHyperglycemia and Neurological Outcome in Patients With Head InjuryOsQ_drОценок пока нет
- Efficacy of Hyperventilation, Blood Pressure Elevation, and Metabolic Suppression Therapy in Controlling Intracranial Pressure After Head InjuryДокумент9 страницEfficacy of Hyperventilation, Blood Pressure Elevation, and Metabolic Suppression Therapy in Controlling Intracranial Pressure After Head InjuryAik NoeraОценок пока нет
- Poststroke Hyperglycemia: Natural History and Immediate ManagementДокумент5 страницPoststroke Hyperglycemia: Natural History and Immediate ManagementEsteban Martin Chiotti KaneshimaОценок пока нет
- 2008 IVD GlucoseДокумент6 страниц2008 IVD GlucoseJeltsin Chávarry AratíaОценок пока нет
- How Does Empagliflozin Improve Arterial Stiffness in Patients With Type 2 Diabetes Mellitus - Sub Analysis of A Clinical TrialДокумент12 страницHow Does Empagliflozin Improve Arterial Stiffness in Patients With Type 2 Diabetes Mellitus - Sub Analysis of A Clinical TrialMarshall ThompsonОценок пока нет
- Assessment and Treatment of Hyperglycemia in Critically IllДокумент6 страницAssessment and Treatment of Hyperglycemia in Critically IllYousif ElmasryОценок пока нет
- Stroke and LipidДокумент4 страницыStroke and LipidvenniariskiaОценок пока нет
- J Clin Med ResДокумент9 страницJ Clin Med ResPutrimarlien20Оценок пока нет
- Hyperglycemia Has A Stronger Relation With Outcome in Trauma Patients Than in Other Critically Ill PatientsДокумент12 страницHyperglycemia Has A Stronger Relation With Outcome in Trauma Patients Than in Other Critically Ill PatientsAfkar30Оценок пока нет
- Desantis 2006Документ15 страницDesantis 2006Hoàng ThôngОценок пока нет
- 10 Glycemic Control in Perioperative PeriodДокумент5 страниц10 Glycemic Control in Perioperative PeriodAna-Maria CroitoruОценок пока нет
- 1678 4227 Anp 77 12 0848Документ7 страниц1678 4227 Anp 77 12 0848Sango AyraОценок пока нет
- Age +estimated+glomerular+filtration+rate+and+ejection+fraction+score+predicts+contrast-Induced+acute+kidney+injury+in+patients+with+diabetes+and+chronic+kidney+disease +insight+from+the+TRACK-D+studyДокумент5 страницAge +estimated+glomerular+filtration+rate+and+ejection+fraction+score+predicts+contrast-Induced+acute+kidney+injury+in+patients+with+diabetes+and+chronic+kidney+disease +insight+from+the+TRACK-D+studyangga_darmawan26Оценок пока нет
- Bern Jak 2021Документ6 страницBern Jak 2021Meirina KhairatОценок пока нет
- Research ArticleДокумент11 страницResearch ArticleLilis FazriahОценок пока нет
- Keywords:-Acute Coronary Syndrome, Triglycerides, HighДокумент6 страницKeywords:-Acute Coronary Syndrome, Triglycerides, HighInternational Journal of Innovative Science and Research TechnologyОценок пока нет
- Cam Kai GermanyДокумент16 страницCam Kai GermanyPatricia WulandariОценок пока нет
- The Effect of Aerobic Exercise On Blood and Plasma Viscosity On Cardiac Health Club ParticipantsДокумент4 страницыThe Effect of Aerobic Exercise On Blood and Plasma Viscosity On Cardiac Health Club ParticipantsDedy SavradinataОценок пока нет
- Full Text 01Документ8 страницFull Text 01febyОценок пока нет
- Mayo Clinic Proceedings: Critical Glucose Control: The Devil Is in The DetailsДокумент4 страницыMayo Clinic Proceedings: Critical Glucose Control: The Devil Is in The DetailstfurrahmanОценок пока нет
- The Efficacy and Safety of Triple Vs Dual Combination of ARB, CCB, and DiureticsДокумент9 страницThe Efficacy and Safety of Triple Vs Dual Combination of ARB, CCB, and DiureticsLucky PratamaОценок пока нет
- Validation of A Glucose Meter at An Intensive Care UnitДокумент7 страницValidation of A Glucose Meter at An Intensive Care UnitRodas GetachewОценок пока нет
- 1 s2.0 0049384887903586 MainДокумент8 страниц1 s2.0 0049384887903586 Mainong251183Оценок пока нет
- Ijccm 20 653Документ5 страницIjccm 20 653Saifuddin HaswareОценок пока нет
- Continuous Hemodynamic MonitoringДокумент54 страницыContinuous Hemodynamic MonitoringOrion JohnОценок пока нет
- FluidДокумент190 страницFluidAndrias OzОценок пока нет
- 21Документ5 страниц21Guhan KAОценок пока нет
- Results With Respect To Intraprocedural Myocardial Contrast EchocardiographyДокумент16 страницResults With Respect To Intraprocedural Myocardial Contrast EchocardiographySavira Tapi-TapiОценок пока нет
- Review Article: Elevated Blood Pressure in The Acute Phase of Stroke and The Role of Angiotensin Receptor BlockersДокумент8 страницReview Article: Elevated Blood Pressure in The Acute Phase of Stroke and The Role of Angiotensin Receptor BlockersPatrick RamosОценок пока нет
- Jurnal Internasional Korea DMДокумент9 страницJurnal Internasional Korea DMzahradeswitamuftiОценок пока нет
- Changes in Plasma Fibrinogen, Homocysteine and Lipid Profile in Coronary Artery Disease Patients of North Indian (Punjab) Popu-LationДокумент4 страницыChanges in Plasma Fibrinogen, Homocysteine and Lipid Profile in Coronary Artery Disease Patients of North Indian (Punjab) Popu-LationMaya RustamОценок пока нет
- Weber 2016Документ10 страницWeber 2016Rafaela Queiroz MascarenhasОценок пока нет
- Relatia Dintre Arteroscleroza Si Colesterol SericДокумент7 страницRelatia Dintre Arteroscleroza Si Colesterol SericBeniamin BorotaОценок пока нет
- Glucose Variability - FullДокумент12 страницGlucose Variability - FullAlina PopaОценок пока нет
- Indications and Hemoglobin Thresholds For Red Blood Cell Transfusion in The Adult - UpToDateДокумент39 страницIndications and Hemoglobin Thresholds For Red Blood Cell Transfusion in The Adult - UpToDateAhmed MostafaОценок пока нет
- Diab 7Документ9 страницDiab 7marsim92Оценок пока нет
- Research Journal of Pharmaceutical, Biological and Chemical SciencesДокумент9 страницResearch Journal of Pharmaceutical, Biological and Chemical SciencesMuhammad ZubaidiОценок пока нет
- Correlation Between Pediatric Open Heart Surgery Outcomes and Arterial-Mixed Venous Oxygen Saturation DifferencesДокумент4 страницыCorrelation Between Pediatric Open Heart Surgery Outcomes and Arterial-Mixed Venous Oxygen Saturation DifferencesJust MahasiswaОценок пока нет
- 302 Cardiovascular Risk: AssessmentДокумент1 страница302 Cardiovascular Risk: AssessmentLêHữuHoàiОценок пока нет
- Correlates of Acute Insulin Resistance in The Early Phase of Non-Diabetic ST-elevation Myocardial InfarctionДокумент9 страницCorrelates of Acute Insulin Resistance in The Early Phase of Non-Diabetic ST-elevation Myocardial InfarctionmeliabudiОценок пока нет
- Recombinant Activated Factor VII For Hemorrhage After Pediatric Cardiac SurgeryДокумент7 страницRecombinant Activated Factor VII For Hemorrhage After Pediatric Cardiac SurgeryYulii Di Bulan JulyОценок пока нет
- A Randomised Study of The Impact of The SGLT2 Inhibitor Dapagliflozin On Microvascular and Macrovascular CirculationДокумент9 страницA Randomised Study of The Impact of The SGLT2 Inhibitor Dapagliflozin On Microvascular and Macrovascular CirculationPujiyantoОценок пока нет
- PHD Thomas Larsen Effect of CholecalciferolДокумент8 страницPHD Thomas Larsen Effect of CholecalciferolbabakirisssОценок пока нет
- Evaluation Study of Congestive Heart Failure and Pulmonary Artery Catheterization EffectivenessДокумент9 страницEvaluation Study of Congestive Heart Failure and Pulmonary Artery Catheterization EffectivenessMelisa AnaОценок пока нет
- 01.cir.90.1.35 6Документ8 страниц01.cir.90.1.35 6NYONGKERОценок пока нет
- 2023, Kawai - Serum Angiotensin Converting Enzyme Levels Indicating Early Sarcoidosis Diagnosis andДокумент8 страниц2023, Kawai - Serum Angiotensin Converting Enzyme Levels Indicating Early Sarcoidosis Diagnosis andAlexandra TofanОценок пока нет
- The Usefulness of A Laser Doppler in The Measurement of Toe Blood PressuresДокумент8 страницThe Usefulness of A Laser Doppler in The Measurement of Toe Blood PressuressalemОценок пока нет
- Higado Graso No Alcoholico y Niveles de PCRДокумент6 страницHigado Graso No Alcoholico y Niveles de PCRperuliz19Оценок пока нет
- Anti-Inflammatory and Metabolic Effects of Candesartan in Hypertensive PatientsДокумент5 страницAnti-Inflammatory and Metabolic Effects of Candesartan in Hypertensive PatientsBarbara Sakura RiawanОценок пока нет
- ILN Biomarker 2016Документ6 страницILN Biomarker 2016AlienОценок пока нет
- Background Safety Outcomes: Group Baseline 3 Months P 6 Months P 12 Months P NYH AДокумент1 страницаBackground Safety Outcomes: Group Baseline 3 Months P 6 Months P 12 Months P NYH APaolaОценок пока нет
- Objective: Methods: Results: Conclusions:: What's Known On This SubjectДокумент12 страницObjective: Methods: Results: Conclusions:: What's Known On This SubjectAnonymous AzkHFgubueОценок пока нет
- EMPA REG OUTCOME The Cardiologist S Point 2017 The American Journal of MedДокумент6 страницEMPA REG OUTCOME The Cardiologist S Point 2017 The American Journal of MedAlina PopaОценок пока нет
- Vasopressin and Methylprednisolone and HemodynamicДокумент8 страницVasopressin and Methylprednisolone and Hemodynamicaida154Оценок пока нет
- Research Article Baseline Serum Uric Acid Levels Are Associated With All-Cause Mortality in Acute Coronary Syndrome Patients After Percutaneous Coronary InterventionДокумент9 страницResearch Article Baseline Serum Uric Acid Levels Are Associated With All-Cause Mortality in Acute Coronary Syndrome Patients After Percutaneous Coronary InterventionmikeОценок пока нет
- 1595 FullДокумент7 страниц1595 FullHerly Maulida SurdhawatiОценок пока нет
- Risk of Systolic HT in Elderly metaanalysis-EHJ 2000Документ8 страницRisk of Systolic HT in Elderly metaanalysis-EHJ 2000UwOОценок пока нет
- Stratton2006 Article AdditiveEffectsOfGlycaemiaAndBДокумент9 страницStratton2006 Article AdditiveEffectsOfGlycaemiaAndBmohamed alshoshanОценок пока нет
- 116 229 1 SMДокумент6 страниц116 229 1 SMsinlookerОценок пока нет
- Installation Manual: 1.2 External Dimensions and Part NamesДокумент2 страницыInstallation Manual: 1.2 External Dimensions and Part NamesSameh MohamedОценок пока нет
- Jurnal Gerd PDFДокумент6 страницJurnal Gerd PDFdilaОценок пока нет
- Proposal Semister ProjectДокумент7 страницProposal Semister ProjectMuket AgmasОценок пока нет
- Epoxy Data - AF35LVE TDS - ED4 - 11.17Документ8 страницEpoxy Data - AF35LVE TDS - ED4 - 11.17HARESH REDDYОценок пока нет
- Work of Asha Bhavan Centre - A Nonprofit Indian Organisation For Persons With DisabilityДокумент10 страницWork of Asha Bhavan Centre - A Nonprofit Indian Organisation For Persons With DisabilityAsha Bhavan CentreОценок пока нет
- LYON Conditions of Secondment 3500EUR enДокумент4 страницыLYON Conditions of Secondment 3500EUR enabdu1lahОценок пока нет
- Pre-Operative Check Up of Farm Tools, ImplementsДокумент19 страницPre-Operative Check Up of Farm Tools, ImplementsLaurence Fabiala50% (2)
- BRS PDFДокумент14 страницBRS PDFGautam KhanwaniОценок пока нет
- 15 UrinalysisДокумент9 страниц15 UrinalysisJaney Ceniza تОценок пока нет
- Governance StructureДокумент1 страницаGovernance StructureJoydip MukhopadhyayОценок пока нет
- BDC 6566Документ6 страницBDC 6566jack.simpson.changОценок пока нет
- Musa Paradisiaca L. and Musa Sapientum L.: A Phytochemical and Pharmacological ReviewДокумент8 страницMusa Paradisiaca L. and Musa Sapientum L.: A Phytochemical and Pharmacological ReviewDeviОценок пока нет
- Shoulder Joint Position Sense Improves With ElevationДокумент10 страницShoulder Joint Position Sense Improves With ElevationpredragbozicОценок пока нет
- Material Rate PWD 2014...........Документ70 страницMaterial Rate PWD 2014...........Shamsul IslamОценок пока нет
- Periodontology Question BankДокумент44 страницыPeriodontology Question BankVanshika Jain100% (6)
- Science 7 - Q2 - M7Документ16 страницScience 7 - Q2 - M7RAMOS ERLYN P.Оценок пока нет
- 2nd Term Study Guide 4th Grade Feb 2024 Cambridge ObjectivesДокумент8 страниц2nd Term Study Guide 4th Grade Feb 2024 Cambridge Objectivessofi.cardenas1968Оценок пока нет
- Nature and Nurture - How They Play A Role in Serial Killers and THДокумент40 страницNature and Nurture - How They Play A Role in Serial Killers and THJ.A.B.AОценок пока нет
- Soft Tissue SarcomaДокумент19 страницSoft Tissue SarcomaEkvanDanangОценок пока нет
- W4. Grade 10 Health - Q1 - M4 - v2Документ22 страницыW4. Grade 10 Health - Q1 - M4 - v2Jesmael PantalunanОценок пока нет
- Pescatarian Mediterranean Diet Cookbook 2 - Adele TylerДокумент98 страницPescatarian Mediterranean Diet Cookbook 2 - Adele Tylerrabino_rojoОценок пока нет
- IS 4049-Part-IДокумент5 страницIS 4049-Part-ISrinivas KadivetiОценок пока нет
- Case Exercise On Layer Unit (2000 Birds)Документ2 страницыCase Exercise On Layer Unit (2000 Birds)Priya KalraОценок пока нет
- Topic 7: Respiration, Muscles and The Internal Environment Chapter 7B: Muscles, Movement and The HeartДокумент4 страницыTopic 7: Respiration, Muscles and The Internal Environment Chapter 7B: Muscles, Movement and The HeartsalmaОценок пока нет
- HDFC Life Insurance (HDFCLIFE) : 2. P/E 58 3. Book Value (RS) 23.57Документ5 страницHDFC Life Insurance (HDFCLIFE) : 2. P/E 58 3. Book Value (RS) 23.57Srini VasanОценок пока нет
- Poverty and Children's Personal RelationshipsДокумент87 страницPoverty and Children's Personal RelationshipsJoe OgleОценок пока нет
- Evidence Based DesignДокумент4 страницыEvidence Based Designmartinadam82Оценок пока нет
- Estrogen Dominance-The Silent Epidemic by DR Michael LamДокумент39 страницEstrogen Dominance-The Silent Epidemic by DR Michael Lamsmtdrkd75% (4)
- Teleperformance Global Services Private Limited: Full and Final Settlement - December 2023Документ3 страницыTeleperformance Global Services Private Limited: Full and Final Settlement - December 2023vishal.upadhyay9279Оценок пока нет
- Pamet and PasmethДокумент4 страницыPamet and PasmethBash De Guzman50% (2)