Академический Документы
Профессиональный Документы
Культура Документы
ENC Part I
Загружено:
JohnVincentPagadduАвторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
ENC Part I
Загружено:
JohnVincentPagadduАвторское право:
Доступные форматы
Pediatrics II
ESSENTIAL NEWBORN CARE
In December 2000, 189 Heads of States or
Governments
jointly
endorsed
the
Millennium Declaration which committed
signatories to achieving 8 millennium
development goals by the year 2015. Of
the 8 goals, Goals 4 and 5 relate to
reduction of child mortality by two-thirds
and improvement of maternal health.
Dr. Wangdali
From 1988-1998, there was a steep decline
in the <5 year old mortality rate due to the
various
programs
geared
towards
improving child health.
From 1998-2008, there was a smaller
decrease despite the maintenance of these
programs.
Neonatal mortality rate has remained
unchanged despite the advances in
technology (ventilators), drug therapy
(surfactant, broad-spectrum antibiotics),
and increase in the number of specialists
caring for the newborn (neonatologists and
pediatricians).
If we are to decrease the child mortality
rate, we need to address the causes of
neonatal mortality.
MAJOR CAUSES OF UNDER FIVE
DEATHS
Kat and JV
Doctor of Medicine - II
Page 1 of 6
Is the risk of dying less in the higher
economic brackets in the country?
The average neonatal mortality in the
country is 15/1000 live births.
In the lowest socio-economic quintile,
it is 20/1000 live births, while in the
least poor it is 10/1000 live births.
This shows that being in the highest
wealth quintile does not give one a
significant advantage because the
neonatal mortality rate is not far from
the national average.
the neonatal mortality rate in a first
world country like Japan is only
2.4/1000 live births.
3 out of 4 newborns die in the first
week of life, specifically the first 2
days of life.
Existing
perinatal
conditions
predispose the newborn to an
increased risk of dying immediately
after delivery.
Globally, approximately 10 million
children die each year.
This is the Lancet Child Survival Series
which
looked
at
preventive
interventions to save childrens lives.
Kat and JV
Doctor of Medicine - II
Page 2 of 6
With 23 interventions we can prevent
6 million of the 10 million global under
five deaths.
Notice that the only 2-digit figure in
the table is breastfeeding at 13%, yet
not enough emphasis is placed on
breastfeeding
as
a
life-saving
intervention.
Compare this with the giving of
antibiotics for PROM as interns, we
were assigned journal reports or given
demerits for failing to order this in
the mothers chart, yet it contributes
to only an estimated 1% reduction in
childhood mortality.
Good nutrition through breastfeeding,
appropriate complementary feeding,
supplementation OR fortification can
already prevent 2.5 million deaths.
being treated as an infection control
problem. The first thing the team
leader asked was: How much
colostrum did the cases receive?
Answer: Not a drop.
In Baguio General Hospital, babies
were routinely removed from their
mothers at birth, placed in a
nursery, and given infant formula.
The graph at the bottom shows the
high incidence of sepsis among
these babies.
A few years ago, a sepsis outbreak in
an NCR hospital became front-page
news despite the fact that all large
hospitals
nationwide
have
experienced being in the same
situation. At the end of the outbreak,
a total of 32 term babies who were
born healthy succumbed to sepsis.
The father of one of these babies
wrote to the WHO in Geneva saying
that he saved money so that his wife
could deliver in a hospital, only to
have the baby die from infection.
WHO referred the case to the Office of
the WHO Representative to the
country and an investigating team
was formed. When the team arrived
at the hospital, the outbreak was
Kat and JV
Dra. Clavano instituted a new
regimen that allowed mothers and
babies to room together, and
encouraged women to breastfeed
on demand. The results were
dramatic: the incidence of oral
thrush, diarrhea, clinical sepsis,
and death were drastically reduced
Doctor of Medicine - II
Page 3 of 6
during the intensification of the
breastfeeding program.
This contributed to the formation
of the Baby Friendly Hospital
Initiative.
In the Philippines, Dra. Clavano
continued to advocate against the
use of infant formulas, work that
contributed to the 1986 Philippine
National Milk Code, and the 1992
Rooming-In and Breastfeeding Act.
A similar study done in Ghana with
half the number of babies also
shows the same dose-response
relationship between initiation of
breastfeeding and risk of infectionrelated death. This dose response
curve is very strong evidence for
the
protective
property
of
breastfeeding.
This study was done in Nepal
involving 23,000 breastfed babies.
It looked at the risk of infectionrelated death correlated with the
time of initiation of breastfeeding
(in hours).
If breastfeeding is started within
an hour after birth, the risk of
infection-related death is 1.
If
breastfeeding is started after 1
hour but within the 1st 24 hours,
the risk doubles to 2.
If
breastfeeding is started after 3
days, there is a four-fold increase
in the risk of infection-related
death.
Kat and JV
This is a randomized controlled
trial that studied the type of
feeding received by low birth
weight babies against the risk of
serious illness.
The result of the study was
significant in that it showed that
the less breastmilk the baby
receives, the higher the risk of
serious illness.
Doctor of Medicine - II
Page 4 of 6
In a baseline study of consecutive
deliveries in 51 of the largest
hospitals in 9 regions in the
Philippines, the incidences of
neonatal sepsis, neonatal and
maternal
mortalities
were
obtained. In that hospital study,
the neonatal sepsis rate was 6%.
There is no available data for
sepsis rates in babies delivered at
home.
Newborn mortality was 16.8/1000
live births in home deliveries vs
16/1000 live births in hospitals.
Does this mean that hospital
deliveries
do
not
have
an
advantage over home deliveries?
Even
more
glaring
are
the
statistics for maternal mortality:
162/100,000 deliveries if homebased vs. 234/100,000 hospital
deliveries.
These figures only goes to show
that we need to institute measures
that will allow mothers and
newborns to benefit from safe and
quality care.
Giving
antenatal
steroids
to
mothers who are in preterm labor
has several beneficial outcomes in
the neonate.
Foremost among these is the
overall reduction in neonatal death
with an RR of 0.69.
There is also a reduction in the
incidences of respiratory distress
syndrome and cerebroventricular
hemorrhage.
Contrary to the notion that steroids
will suppress the immune system,
there is also a reduction in sepsis
in the first 48 hours of the
newborns life.
It likewise does not increase the
risk of death, chorioamnionitis or
peurperal sepsis in the mother.
What Immediate Newborn Care
Practices Save Lives?
Implementation of the ENC protocol has
the potential to avert approximately 70
percent of newborn deaths that are due
to preventable causes.
Kat and JV
Betametasone is the preferred
steroid because it is associated with
less periventricular leukomalacia, a
disorder of the white matter of the
brain. However it is much more
expensive and is not always readily
available.
Doctor of Medicine - II
Page 5 of 6
Dexamethasone is more available and
is easily obtained; it should always be
in the E-cart of your facility for
immediate access when a mother
comes in preterm labor.
If a quick delivery is expected and
dexa can be given only once, can we
double the dose and give 12 mg q12
hours? Studies have shown that there
Kat and JV
is no additional benefit to using higher
or more frequent doses.
If a mother with asthma has been
taking oral steroids for 1 week, can
we defer the dexa? We should still
give it because the absorption of
other forms of steroids is unreliable.
Doctor of Medicine - II
Page 6 of 6
Вам также может понравиться
- Fever Headache Dizziness Seizure Nausea Vomiting: - X Cough DOB Constipation Diarrhea - X Abd. Pain: Location: QualityДокумент2 страницыFever Headache Dizziness Seizure Nausea Vomiting: - X Cough DOB Constipation Diarrhea - X Abd. Pain: Location: QualityJohnVincentPagadduОценок пока нет
- Systemic Response To InjuryДокумент15 страницSystemic Response To InjuryJohnVincentPagaddu100% (1)
- Critical Appraisal by John Vincent Pagaddu, M.D.Документ91 страницаCritical Appraisal by John Vincent Pagaddu, M.D.JohnVincentPagadduОценок пока нет
- Local Mechanisms Affect MAPДокумент1 страницаLocal Mechanisms Affect MAPJohnVincentPagadduОценок пока нет
- The BronchiДокумент64 страницыThe BronchiJohnVincentPagadduОценок пока нет
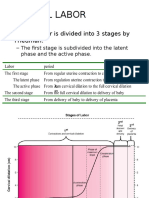
- Normal Labor: - Normal Labor Is Divided Into 3 Stages by FriedmanДокумент13 страницNormal Labor: - Normal Labor Is Divided Into 3 Stages by FriedmanJohnVincentPagadduОценок пока нет
- Self-Reliance and ProcurementДокумент16 страницSelf-Reliance and ProcurementJohnVincentPagadduОценок пока нет
- Etiology: Pneumoniae. Nontypeable Haemophilus Influenzae and Moraxella Catarrhalis May Be Significant Pathogens inДокумент4 страницыEtiology: Pneumoniae. Nontypeable Haemophilus Influenzae and Moraxella Catarrhalis May Be Significant Pathogens inJohnVincentPagadduОценок пока нет
- Bio StatisticsДокумент16 страницBio StatisticsJohnVincentPagadduОценок пока нет
- Mollusc I Pox VirusДокумент2 страницыMollusc I Pox VirusJohnVincentPagadduОценок пока нет
- Sanctity and ScarcityДокумент33 страницыSanctity and ScarcityJohnVincentPagaddu100% (1)
- HealthДокумент5 страницHealthJohnVincentPagadduОценок пока нет
- Derma Sample Exam For Practicals (Skin and Lesions)Документ42 страницыDerma Sample Exam For Practicals (Skin and Lesions)JohnVincentPagaddu100% (1)
- Surgery Ortho TraumaДокумент8 страницSurgery Ortho TraumaJohnVincentPagadduОценок пока нет
- Types of Mixtures LabДокумент2 страницыTypes of Mixtures LabJohnVincentPagadduОценок пока нет
- Population Mortality: Reported By: Group Four TFEG1 Biology 160 Lab AY 2010-2011 2 SemesterДокумент57 страницPopulation Mortality: Reported By: Group Four TFEG1 Biology 160 Lab AY 2010-2011 2 SemesterJohnVincentPagadduОценок пока нет
- Pediaortho Hand OutДокумент119 страницPediaortho Hand OutJohnVincentPagadduОценок пока нет
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeОт EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeРейтинг: 4 из 5 звезд4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingОт EverandThe Little Book of Hygge: Danish Secrets to Happy LivingРейтинг: 3.5 из 5 звезд3.5/5 (400)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceОт EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceРейтинг: 4 из 5 звезд4/5 (895)
- The Yellow House: A Memoir (2019 National Book Award Winner)От EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Рейтинг: 4 из 5 звезд4/5 (98)
- The Emperor of All Maladies: A Biography of CancerОт EverandThe Emperor of All Maladies: A Biography of CancerРейтинг: 4.5 из 5 звезд4.5/5 (271)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryОт EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryРейтинг: 3.5 из 5 звезд3.5/5 (231)
- Never Split the Difference: Negotiating As If Your Life Depended On ItОт EverandNever Split the Difference: Negotiating As If Your Life Depended On ItРейтинг: 4.5 из 5 звезд4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureОт EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureРейтинг: 4.5 из 5 звезд4.5/5 (474)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaОт EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaРейтинг: 4.5 из 5 звезд4.5/5 (266)
- The Unwinding: An Inner History of the New AmericaОт EverandThe Unwinding: An Inner History of the New AmericaРейтинг: 4 из 5 звезд4/5 (45)
- Team of Rivals: The Political Genius of Abraham LincolnОт EverandTeam of Rivals: The Political Genius of Abraham LincolnРейтинг: 4.5 из 5 звезд4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyОт EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyРейтинг: 3.5 из 5 звезд3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreОт EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreРейтинг: 4 из 5 звезд4/5 (1090)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersОт EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersРейтинг: 4.5 из 5 звезд4.5/5 (344)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)От EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Рейтинг: 4.5 из 5 звезд4.5/5 (121)
- Atisara Krimi - 2018 BAMS DetailДокумент12 страницAtisara Krimi - 2018 BAMS DetailmasdfgОценок пока нет
- 2) Incaaam PP ThreadliftДокумент47 страниц2) Incaaam PP ThreadliftFitri Fratiwi100% (4)
- Orofacial CleftsДокумент19 страницOrofacial CleftsTj AngelaОценок пока нет
- An Overview of Methods Used For Estimation of Time Since Death PDFДокумент12 страницAn Overview of Methods Used For Estimation of Time Since Death PDFFajar SodiqiОценок пока нет
- Antibiotics, Misuse and ConsequencesДокумент67 страницAntibiotics, Misuse and Consequencestummalapalli venkateswara raoОценок пока нет
- GERD (Gastroesophageal Reflux Disease)Документ112 страницGERD (Gastroesophageal Reflux Disease)Mharj Alfelor Cecilio100% (7)
- ElectrocardiogramДокумент17 страницElectrocardiogramvinnu kalyanОценок пока нет
- Verbalizing Importance of Adequate Nutrition Feeds Self UnassistedДокумент2 страницыVerbalizing Importance of Adequate Nutrition Feeds Self UnassistedMasruri EfendyОценок пока нет
- SECOND Semester, AY 2022-2023: Mission VisionДокумент34 страницыSECOND Semester, AY 2022-2023: Mission Visionjeyyy BonesssОценок пока нет
- 302 PpJ. Grayson, Freedom From Obsessive Compulsive Disorder A Personalized Recovery Program For LivingДокумент2 страницы302 PpJ. Grayson, Freedom From Obsessive Compulsive Disorder A Personalized Recovery Program For LivingMohammad Shoyyad L IkhsanОценок пока нет
- Neurodegenerative DiseasesДокумент2 страницыNeurodegenerative DiseasesBerniceTanОценок пока нет
- MSDS Jun-Air SJ-27FДокумент8 страницMSDS Jun-Air SJ-27FJuan Eduardo LoayzaОценок пока нет
- Natal PlanetsДокумент290 страницNatal PlanetsAnonymous PErKNy9100% (1)
- Basic First Aid TrainingДокумент32 страницыBasic First Aid Trainingtukaram patilОценок пока нет
- Occupational Health in Indonesia: Astrid Sulistomo Dep. of Community Medicine FmuiДокумент99 страницOccupational Health in Indonesia: Astrid Sulistomo Dep. of Community Medicine FmuiDea MaharaniОценок пока нет
- Papadopoulos15 5Документ28 страницPapadopoulos15 5Ellizabeth LilantiОценок пока нет
- Vijayalakshmi MenopauseДокумент7 страницVijayalakshmi MenopauseakankshaОценок пока нет
- Spiritual Wrestling PDFДокумент542 страницыSpiritual Wrestling PDFJames CuasmayanОценок пока нет
- Suppositories Phardose LectureДокумент41 страницаSuppositories Phardose LecturePeter Paul RecaboОценок пока нет
- MenopauseДокумент21 страницаMenopauseDr K AmbareeshaОценок пока нет
- ACLS Full Lesson Plans PDFДокумент60 страницACLS Full Lesson Plans PDFVictoriano Mendez100% (1)
- Immediate Dental Implant 1Документ13 страницImmediate Dental Implant 1alkhalijia dentalОценок пока нет
- Complete DentureДокумент57 страницComplete Denturedr_ahmad_zuhdi100% (3)
- Gwich'in EthnobotanyДокумент72 страницыGwich'in EthnobotanyNatalia Alexandra Bernal QuinteroОценок пока нет
- Clinical Findings and Management of PertussisДокумент10 страницClinical Findings and Management of PertussisAGUS DE COLSAОценок пока нет
- Grand Case Pres FDARДокумент11 страницGrand Case Pres FDARMika SaldañaОценок пока нет
- Patient'S Case Performa FileДокумент13 страницPatient'S Case Performa Filevipul tandonОценок пока нет
- Esmee Sabina 19-5372 PDFДокумент3 страницыEsmee Sabina 19-5372 PDFEsme SabinaОценок пока нет
- Essene FastingДокумент48 страницEssene FastingEnoch Gandhislilbrother Abraham90% (10)
- Glove Utilization in The Prevention of Cross Transmission - A Systematic Review 2015Документ12 страницGlove Utilization in The Prevention of Cross Transmission - A Systematic Review 2015CTОценок пока нет