Академический Документы
Профессиональный Документы
Культура Документы
Metabolism: Obesity and Asthma: Beyond T 2 Inflammation
Загружено:
Irina Luciana DumitriuОригинальное название
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Metabolism: Obesity and Asthma: Beyond T 2 Inflammation
Загружено:
Irina Luciana DumitriuАвторское право:
Доступные форматы
M ET ABO LI S M CL IN I CA L A N D E XP E RI ME N TAL XX ( 2 01 4 ) X XX X XX
Available online at www.sciencedirect.com
Metabolism
www.metabolismjournal.com
Obesity and asthma: beyond TH2 inflammation
Luiz O.S. Leiria a , Milton A. Martins b , Mrio J.A. Saad a,
a
b
Department of Internal Medicine, Faculty of Medical Sciences, State University of Campinas, Campinas, SP, Brazil
Department of Medicine, School of Medicine, University de So Paulo, So Paulo, SP, Brazil
A R T I C LE I N FO
AB S T R A C T
Article history:
Obesity is a major risk factor for asthma. Likewise, obesity is known to increase disease
Received 19 March 2014
severity in asthmatic subjects and also to impair the efficacy of first-line treatment
Accepted 3 October 2014
medications for asthma, worsening asthma control in obese patients. This concept is in
agreement with the current understanding that some asthma phenotypes are not
Keywords:
accompanied by detectable inflammation, and may not be ameliorated by classical anti-
Insulin
inflammatory therapy. There are growing evidences suggesting that the obesity-related
Adiponectin
asthma phenotype does not necessarily involve the classical TH2-dependent inflammatory
Leptin
process. Hormones involved in glucose homeostasis and in the pathogeneses of obesity
Airway hyperreactivity
likely directly or indirectly link obesity and asthma through inflammatory and noninflammatory pathways. Furthermore, the endocrine regulation of the airway-related preganglionic nerves likely contributes to airway hyperreactivity (AHR) in obese states. In this
review, we focused our efforts on understanding the mechanism underlying obesity-related
asthma by exploring the TH2-independent mechanisms leading to this disease.
2014 Elsevier Inc. All rights reserved.
1.
Introduction
Obesity has emerged as an important risk factor for asthma
[1,2]. There has been a remarkable increase in the prevalence
of obesity worldwide as a consequence of the modern eating
habits associated with a sedentary lifestyle [3]. Along with the
growing prevalence of obesity and metabolic syndrome, a
concomitant rise in the incidence of asthma has been
observed in the last few years [1]. Nevertheless, obesity is
known to increase disease severity in asthmatic subjects [4]
and also to impair the efficacy of first-line medications to
treat asthma, worsening disease control in obese and
overweight patients [58].
Asthma is characterized by chronic inflammation in lung
tissue, mucus production and abnormal bronchoconstriction.
Inflammation includes the presence of CD4 T helper 2 (TH2) cells
and their associated cytokines, as well as eosinophilic infiltration. Effector TH2 cells enhance the eosinophilic survival through
the secretion of IL-5 and, in addition, facilitate mast cell survival
by releasing IL-9. Likewise, eosinophils contribute to antigen
specific production of IL-4 and IL-13, which in turn are required
for increased muscle reactivity [9].
Abbreviations: AHR, airway hyperreactivity; AKT, RAC-alpha serine/threonine-protein kinase; AMPK, adenosine monophosphateactivated kinase; ARPF, airway-related pre-ganglionic fibers; ASM, airway smooth muscle; BAL, bronchoalveolar lavage; BMI, body mass
index; BTSM, bovine tracheal smooth muscle; cGMP, cyclic guanosine monophosphate; CNS, central nervous system; eNOS, endothelial
nitric oxide synthase; HMW, high molecular weight; IL, interleukin; ILC-3, innate lymphoid cells type 3; iNOS, inducible nitric oxide
synthase; IR, insulin receptor; IRS-1, insulin receptor substrate; LMW, low molecular weight; NFB, nuclear factor kappa B; NLRP3, pyrin
domain-containing protein 3; TH2, T helper 2; PI3K, phosphoinositide-3 kinase; PPAR, peroxisome-proliferator activated receptor alpha;
sGC, soluble guanylyl cyclase; TNF-, tumor necrosis factor alpha.
Corresponding author at: Department of Internal Medicine, Faculty of Medical SciencesFCM, State University of CampinasUNICAMP,
Rua Tesslia Vieira de Camargo, 126 Cidade Universitria Zeferino Vaz, 13083-887 Campinas, SP, Brazil.
E-mail address: msaad@fcm.unicamp.br (M.J.A. Saad).
http://dx.doi.org/10.1016/j.metabol.2014.10.002
0026-0495/ 2014 Elsevier Inc. All rights reserved.
Please cite this article as: Leiria LOS, et al, Obesity and asthma: beyond TH2 inflammation, Metabolism (2014), http://dx.doi.org/
10.1016/j.metabol.2014.10.002
M ET ABOL I S M CL IN I CA L A N D E XP E RI ME N TAL XX ( 2 01 4 ) X XX XX X
Despite the established concept of asthma being the presence
of local inflammation as basic criterion for the onset of disease,
some asthma phenotypes are not accompanied by detectable
inflammation [10]. There is an emerging theory supporting the
idea that asthma phenotype incident in obese patients does not
necessarily involve inflammatory lung injury [1113]. Several
researchers have found no relationship between obesity-associated asthma and eosinophilic inflammation, after measuring
sputum eosinophils [1416] or exhaled nitric oxide [16], while
others have attributed airway hyperreactivity (AHR) in obese
patients to obesity-related changes in lung mechanics as a
consequence of the decreased pulmonary functional volume
[11]. Individuals who are obese breathe with low lung volumes.
This can lead to reduced airway caliber and increased airway
resistance during tidal breathing. In addition, independently of
lung volume, individuals who are obese also present increased
elastic load [11,13].
Compared with subjects in the normal weight range, lung
volume and airway caliber were reduced in subjects with
increased body mass index (BMI), in a linear fashion [11].
Furthermore, studies support the idea that adipose tissue
location is a determinant factor linking obesity and asthma, as
abdominal fat mass was found to influence airway distribution
more than for other fat locations [17,18], suggesting that
adipokines released from these white fat deposits are likely to
contribute to disease. Taken together, these studies have led to
the general consensus that airway inflammation is not the
unique and essential mechanism driving the association between obesity and asthma that it was first thought to be; the
reason that corticosteroid anti-inflammatory drugs are less
effective in the treatment of asthma in overweight and obese
patients [58,19]. In accordance with those findings, a recent
experimental study detected AHR in high-fat fed obese mice in
an inflammation-independent manner [20], highlighting the
possibility that metabolic changes induced by obesity/diabetes
would mediate inflammatory-independent AHR phenotype in
obese patients.
On the other hand, a number of clinical studies have
suggested that obesity enhances inflammatory injury in the
lungs of asthmatic patients [2123] and, accordingly, experimental studies have also reported an increase in local inflammation
in the lung from high-fat fed obese mice challenged with
ovalbumin, compared to those from non-obese mice [2426].
Another study with obese asthmatic patients revealed an
increase in the eosinophil number located at the airway wall,
but not at the lumen, suggesting that location of eosinophils in
the lungs is crucial to the pathogeneses of disease [22].
Paradoxically, eosinophilic infiltration has a beneficial role in
the adipose tissue, where it sustains alternatively activated
macrophages, which importantly contribute to metabolic homeostasis. This way, it seems that at least in TH2-dependent
asthma in obese patients, redistribution of eosinophils from the
adipose tissue to the lungs appears to be a plausible mechanism
underlying this pathophysiology [27]. Nonetheless, it seems that
either inflammation-dependent or -independent phenotypes
could be detected in obese subjects and, for different reasons
both of them lead to an impairment of asthma control in these
patients. Although it is well-established that hormones that
control metabolism such as insulin, leptin and adiponectin,
modulate airway responsiveness, their functional role in asthma
and their underlying molecular mechanisms remain unclear.
Moreover, conflicting studies in the literature associate the
hormone levels in obesity state that both TH2-dependent or
-independent asthma phenotypes exist [10,24,25]. In the next
sections, we have focused our efforts on understanding the
influence and contribution of the non-TH2 components such as
leptin, insulin, adiponectin and low-grade inflammation, to the
pathophysiology of obesity-related asthma.
2.
Early-onset vs. late-onset obese-asthma
phenotypes
Asthma may develop in obese children or in obese adults for
different reasons and it may involve different pathophysiological mechanisms. The most frequent asthma phenotype,
early-onset asthma, occurs in a TH2-dependent fashion, with
children and adolescents often presenting with higher eosinophilic infiltration levels and/or activity in the lungs. Prospective studies with school-aged populations showed that
asthma prevalence and incidence increase with the presence
of obesity [28]. A recent study demonstrated that atopic
asthmatic in obese children and adolescents presented an
increased eosinophilic activity in comparison asthma in nonobese patients [23], which indicates that along with the
increased incidence of asthma in obese children, disease
severity is even higher in these subjects.
On the other hand, in some circumstances, such as for
obesity, asthma may develop in the absence of T-helper 2
(TH2)-inflammation in the lungs [10]. This peculiar asthma
phenotype is known to have a later onset (~ 40 years) and to
be minimally allergic and, as a consequence, has a worse
response to glucocorticoid treatment. Several studies have
recently explored the non-TH2 components of obesity-related
asthma and novel mechanisms (see next sections) have been
recently described in order to explain the causative relationship between these two diseases. Therefore, taking into
account the current state of knowledge, one could infer that
while the TH2-dependent early-onset asthma phenotype can
be potentiated by obesity, the later-onset asthma phenotype
is likely to be a consequence of obesity-induced metabolic
changes and the condition appears to be driven by distinct
mechanisms. Nevertheless, the mechanisms involved in both
types of asthma need to be better comprehended in order to
help drive new approaches to diagnosis and therapeutics.
3.
Asthma control in obesity
Asthma is usually controlled with low doses of inhaled
corticosteroids; this is regarded as first-line treatment for
the disease. Approximately 10% of asthmatic patients need
the maximum inhaled dose, and around 1% of the cases
require chronic oral treatment with glucocorticoids (so-called
glucocorticoid-dependent asthma). However, in some special
cases the patients are glucocorticoid resistant. Glucocorticoid
resistance is defined as asthma symptoms showing no
clinical improvement after treatment with high-dose oral
glucocorticoids. Notwithstanding, glucocorticoid resistance
was reported to be prevalent in obese asthma patients [29].
Please cite this article as: Leiria LOS, et al, Obesity and asthma: beyond TH2 inflammation, Metabolism (2014), http://dx.doi.org/
10.1016/j.metabol.2014.10.002
M ET ABO LI S M CL IN I CA L A N D E XP E RI ME N TAL XX ( 2 01 4 ) X XX X XX
Another clinical study, which aimed to assess the relationship between BMI and the response to combined therapy
with the inhaled GC fluticasone and the long-acting 2agonist salmeterol, reported that although the combination of
both drugs was more effective in controlling asthma than
fluticasone alone, the odds of achieving well-controlled
asthma were significantly lower in obese subjects [30].
Peters-Golden et al. [5] reported that a population of obese
asthmatic patients presented with an impaired response to the
inhaled corticosteroid, whereas the response to the leukotriene
receptor antagonist montelukast remained stable. Conversely, a
combination of fluticasone/salmeterol yielded greater improvements in asthma outcomes in comparison with montelukast
over a range of BMIs [7]. Recently published experimental studies
have suggested that metabolic changes induced by high-fat fed
obese mice result in increased parasympathetic activity, which
results in an increase of acetylcholine levels in the lungs, thus
producing AHR [19,31]. These findings highlight the possible use
of the antimuscarinics as adjuvant drugs in the treatment of
asthma in obese subjects.
In fact, the resistance of obese mice to glucocorticoids
highlights the fact that the contributions of metabolic and
hormonal components resultant from obesity are likely to be
determinant in the obesity-related asthma phenotype. Corroborating this theory, studies have reported that weight loss
improves asthma control [32,33]. After bariatric surgery,
asthmatic patients experienced significant improvement in
their responsiveness to glucocorticoids and in their quality of
life [33]. In this subpopulation of asthmatic patients, only the
pharmacological control of disease does not achieve a good
response. Metabolic and weight control is likely to be
essential for asthma management in obese subjects.
4.
Adiponectin and its protective role in asthma
Adiponectin is a polypeptide hormone that is exclusively secreted
by adipocytes and regulates several metabolic processes such as
fatty acid oxidation and glucose homeostasis [34]. Adiponectin
exists in at least three different higher-order complexes [35,36].
These complexes have been identified as the high molecular weight
(HMW) form, low molecular weight (LMW) form, and trimeric form,
which could play different roles in metabolic homeostasis [36].
Adiponectin directly regulates some metabolic processes involved
in glucose homeostasis such as insulin sensitivity [37], and obesityinduced changes in adiponectin levels influence glucose uptake [38].
In this context, the HMW form is the main one involved in
mediating the insulin-sensitizing effects of adiponectin [3942].
Enhancement in the ratio of blood HMW form relative to total
adiponectin levels positively correlates with improvements in
insulin sensitivity during treatment with an insulin-sensitizing
drug [43]. There is a general consensus that changes in plasma
HMW form levels may be more relevant to the prediction of insulin
resistance than are total plasma adiponectin levels.
Adiponectin plays a physiological role through the activation of AdipoR1 and AdipoR2 receptors, which in turn mediate
the regulation of normal glucose metabolism and insulin
sensitivity. Despite being largely homologous (approximately
67% amino acid identity) the signal transduction differs
between both receptor types. AdipoR1 and AdipoR2 mediate
their insulin sensitizing effects by activating AMP activating
kinase (AMPK) and PPAR-, respectively [44]. Several research
investigations in murine experimental models of obesity pointed
out a protective role of adiponectin against pulmonary disease,
as its obesity-related deficiency is associated with AHR [45]. Highfat fed obese mice showed reduced adiponectin levels, increased
eosinophilic infiltration in the peribronchovascular space and
increased eosinophil levels in the bronchoalveolar lavage (BAL),
suggesting an inverse correlation between adiponectin levels
and the lung inflammation-associated asthma phenotype [24].
Moreover, Medoff et al. [46] showed that adiponectin-deficient
mice (APN/) exhibit higher eosinophilic and monocyte infiltration in the airways and pulmonary vascular remodeling as a
consequence of the elevated lung chemokine levels. Accordingly,
it was recently demonstrated that adiponectin has a protective
role in the murine inflammatory response to subacute ozone
exposure, leading to decreased neutrophil recruitment and
decreased expression of cytokines and chemokines, especially
IL-17 [47]. An increase in ozone-induced neutrophilic infiltration
was found in adiponectin-deficient mice (Adipo/), which is
likely to be due to increased IL-17 originating from interstitial
macrophages and T cells in those animals [47]. These findings
highlighted the possible involvement of a neutrophilic inflammatory process in obesity-associated asthma. Although the more
common TH2 activation-dependent asthma phenotype leads to
airway eosinophilia, asthma can also involve airway neutrophilic
inflammation, which in turn is clinically important, as most
severe forms of asthma involve elevated neutrophil levels and
sputum neutrophils negatively correlate with lung function
[48,49,21]. Furthermore, adiponectin may also work as a protective anti-apoptotic agent against bronchial epithelium injury
caused by ozone exposure [50].
Despite
the
well-documented
correlation
between
adiponectin levels and asthma induced in murine models of
obesity, the translation to humans does not always produce the
same findings, as the published clinical studies present conflicting results. Recent studies showed no correlation between
adiponectin levels and obesity-linked asthma in adult populations of lean and obese asthmatics [51,52]. On the other hand,
another study showed that postmenopausal patients without
metabolic syndrome showed increased levels of leptin and
decreased levels of adiponectin, which were positively correlated
with asthma incidence in those women [53]. Furthermore, low
serum adiponectin was more important than body mass index
(BMI) in predicting the risk for asthma incidence among women
[54]. It is likely that the single measurement of BAL and blood
levels was not efficient to determine whether adiponectin really
participates in the pathophysiology of obesity-related asthma
and, in addition, this relationship may be more complex and
could vary substantially depending on the degree of airway
inflammation and asthma control.
5.
Role for leptin in obesity-induced asthma
The adipocyte-derived hormone leptin is a key regulator in
long-term body weight and energy homeostasis and works
by regulating satiety and energy expenditure [55,56].
Humans or mice with a lack of leptin or its central nervous
system (CNS)-expressed leptin receptors (LRb) display
Please cite this article as: Leiria LOS, et al, Obesity and asthma: beyond TH2 inflammation, Metabolism (2014), http://dx.doi.org/
10.1016/j.metabol.2014.10.002
M ET ABOL I S M CL IN I CA L A N D E XP E RI ME N TAL XX ( 2 01 4 ) X XX XX X
severe obesity and diabetes along with a variety of autonomic complications [5760].
Stimulation of leptin receptor (LRb) activates the Jak2
tyrosine kinase to promote the phosphorylation of intracellular tyrosine residues on LRb. One of these residues recruits
the suppressor of cytokine signaling 3 (SOCS3) and the
protein-tyrosine phosphatase SHP-2. SHP-2 recruits GRB2 to
trigger ERK signaling. Two additional phosphorylated LRb
residues recruit signal transducers and activators of transcription (STAT3 and STAT5), which then translocate to the
nucleus to modulate gene transcription [61].
Pro-inflammatory adipokines such as leptin are increased
in the visceral adipose tissue of obese people, and increases in
leptin levels are associated with AHR [18]. Obese patients with
a history of adult-onset asthma presented increased macrophage infiltration in the visceral adipose tissues concomitant
with enhanced serum levels of leptin in the absence of airway
inflammation. All of these parameters were restored after
bariatric surgery. Moreover, airway epithelial cells were found
to express receptors for the different adipokines [18]. As a
whole, the above-mentioned findings suggest that at least in
this population, physiopathology of the late-onset asthma
associated with obesity primarily involves an adipose tissue
inflammatory process rather than airway inflammation.
Although LRbs are expressed in several tissues [62,63],
gene-targeting studies have indicated that the brain has a
predominant role in leptins physiology [64,65]. Although the
most recognized actions of leptin take place at the hypothalamus level, extra-hypothalamic actions have been described
[66]. Leptin increases airway diameter in mice through the
inhibition of central cholinergic tone [19]. Moreover, replacement of leptin in ob/ob mice was sufficient to normalize lung
mechanics [19]. As the disruption of leptin signaling is often
found in obese subjects, leading to a state of leptin resistance,
it is likely that leptin-defective action at the level of
parasympathetic outflow is also involved in the pathophysiology of obesity-induced airway hyperresponsiveness.
Taking into account the current knowledge, the proinflammatory and central regulatory roles of leptin in the
airways appear to coexist with obesity-associated asthma, at
least in animal models. It is likely that increased levels of
leptin in conjunction with its defective metabolic action result
in an augment of parasympathetic outflow into the lungs and
an increase in inflammatory processes, leading to worsening
of asthma symptoms in obese patients. As most of the studies
in humans only correlate blood leptin levels with respiratory
parameters, further investigations are required to elucidate
how leptin works at the molecular level in obese asthmatics.
6.
Insulin and airway smooth muscle (ASM)
hyperresponsiveness
Obese individuals have an increased risk for the development
of insulin resistance and diabetes [67,68]. Insulin resistance is
defined as the inability of insulin to promote glucose uptake
through the tissue, especially adipose tissue, skeletal muscle
and liver [68]. Moreover, insulin resistance has a central role
in the onset of type 2 diabetes and is an early indication of this
disease. Over the past few years, several researches have shown
that subclinical inflammatory processes in either hypothalamus
or peripheral tissues drive the different molecular mechanisms
underlying insulin resistance in obesity and type 2 diabetes
[69,70]. An increasing body of literature has suggested a positive
correlation between insulin resistance/hyperinsulinemia and
asthma [71]. A cross-sectional study in an adult population
showed that insulin resistant and obese patients have increased
odds of having aeroallergen sensitization and asthma. The
authors raised the hypothesis that common pathways underlie
the physiopathology of obesity-induced asthma and obesityinduced insulin resistance. Insulin resistance was found to be
positively correlated with asthma in children [72]. A correlation
between insulin resistance and IL-6, leptin and TNF- was also
found in this population, and was independent of the BMI scores,
suggesting that insulin resistance could play a role in asthma
physiopathology independently of obesity.
Along with the increase in blood glucose levels, obese and
insulin-resistant
subjects
present
a
compensatory
hyperinsulinemia, which in turn produces various secondary
complications such as benign prostatic hyperplasia [73] and
polycystic ovary syndrome [74]. Nevertheless, such obesityrelated secondary comorbidities are indeed the result of the
direct action of insulin through the activation of mitogenactivated protein kinase (MAPK) pathways [73], leading in general
to a tissue remodeling process. Along with its well-recognized
metabolic and proliferative effects, insulin also promotes several
direct motor effects [7577]. Insulin is an important mediator of
vasorelaxation through a mechanism that involves endothelium-dependent nitric oxide (NO) production [78].
Insulin-mediated NO generation by endothelial cells results from upstream activation of the RAC-alpha serine/
threonine-protein kinase (AKT) pathway [79], which in turn
activates endothelial NO synthase (eNOS) through serine 1177
phosphorylation [80]. NO-mediated vasodilation takes place
as a consequence of the diffusion to vascular smooth muscle
cells, where it activates soluble guanylyl cyclase (sGC), leading
to the formation of cyclic guanosine monophosphate (cGMP).
A similar relaxant effect of insulin was also recently demonstrated in the urinary bladder, where it promotes NO release
from mucosal cells to smooth muscle [77]. To date, insulin has
been shown to produce the opposite effect in the airways.
Previous studies reported that insulin could facilitate [81] or
induce ASM contraction through an epithelium-independent
manner [82]. Schaafsma et al. [82] reported that high doses of
insulin produced sustained ASM contractions which were
dependent on p42/p44 MAP kinase and Rho-kinase, and were
mediated by the production of contractile prostaglandins.
Insulin was also reported to induce contractile protein
accumulation in addition to producing the formation of
large, elongate and contractile ASM cells in a time-dependent
fashion [82]. Long-term exposure of bovine tracheal smooth
muscle (BTSM) to insulin (1 M) resulted in increases in
smooth muscle myosin and calponin protein expression,
which were dependent on the Rho kinase- and PI3-kinase
activation. However, a pro-inflammatory role for insulin has
also been reported in rodent models of type 1 diabetes
mellitus (T1DM). A reduced ASM contraction accompanied
by a marked reduction in the number of degranulated mast
cells and in histamine levels was observed in diabetic rats
upon exposure to the antigen [83]. A complete recovery of the
Please cite this article as: Leiria LOS, et al, Obesity and asthma: beyond TH2 inflammation, Metabolism (2014), http://dx.doi.org/
10.1016/j.metabol.2014.10.002
M ET ABO LI S M CL IN I CA L A N D E XP E RI ME N TAL XX ( 2 01 4 ) X XX X XX
asthmatic phenotype was detected with the replacement of
insulin in T1DM rats, strongly suggesting that insulinmodulated mast cell degranulation and ASM reactivity was
occurring [83].
Another interesting study [84] showed that an antigen
challenge induces pre-synaptic neuronal M2 muscarinic receptor dysfunction, leading to increased acetylcholine release from
airway-located cholinergic nerves. However, antigen-sensitized
T1DM rats were protected against M2 receptor dysfunction and
eosinophilic infiltration into the lungs and related cholinergic
nerves. Furthermore, insulin replacement restored airway
eosinophilia and removed the protection that diabetes provided
to the neuronal M2 muscarinic receptors, restoring ASM
hyperresponsiveness induced by the antigen challenge [84].
The above-mentioned findings are consistent with a previous
epidemiological study that reported an inverse relationship
between atopy and T1DM [85].
Although there is consistent evidence that high doses of
insulin and a lack of insulin cause opposite effects in ASM
responsiveness, the effects of hyperinsulinemia as a consequence of obesity-related insulin resistance have not been
investigated yet and additional studies in insulin resistant
murine models would be useful to better elucidate the
pathophysiology of obesity-associated asthma and the role
of insulin in this dysfunction. Nevertheless, insulin regulates
hepatic glucose production by activating parasympathetic
pre-ganglionic fibers from dorsal vagal complex (DVC) at the
brainstem [86], located at the vicinity of the nucleus ambiguus
(NA), which in turn innervate the airways. Vagal preganglionic neurons that innervate the airways arise primarily from
the rostral NA (rNA) and to a lesser degree from the rostral
portion of the dorsal motor nucleus of the vagus [87]. It is
plausible that insulin may also regulate bronchial contractile
responses by modulating the vagal tonus that originates from
these nucleuses (Fig. 1). In addition, insulin receptors were
detected at the NA; however, functional evidence of insulin
action at this specific nucleus has not yet been reported and
further studies are required in order to shed light on this issue.
7.
Sub-clinical non-TH2 inflammation in obesity-related asthma
Macrophages may exist in two different states: the proinflammatory state, also known as M1, which secretes proinflammatory cytokines, and the M2 state, which is antiinflammatory and expresses mainly IL-10, IL-1RA, and arginase-1 that are, in general, involved in dampening inflammation and also in the tissue repair process [88] (Fig. 2).
Obesity-induced adipose tissue inflammation is a physiopathological process characterized by an inflammatory response, which is mainly driven by infiltrated M1-type
macrophages [88]. M1 macrophages are highly inflammatory
mononuclear cells that are able to release pro-inflammatory
adipokines/chemokines (e.g. tumor necrosis factor (TNF)-,
interleukin (IL)-1, IL-6, and monocyte chemotacticpeptide
(MCP)-1) into the circulation [89] (Fig. 2). This pro-inflammatory environment is not characteristic of acute inflammation
and thus this state is named "low-grade inflammation" or
"subclinical inflammation". Subclinical inflammation in the
key peripheral tissues, such as adipose tissue, liver and
skeletal muscle, underlies the physiopathology of insulin
LEAN
Insulin
OBESE
Insulin
Leptin
Brainstem
Brainstem
Ach
Ach
Parasympathetic
nerves
Ach
Adiponectin
Anti-inflammatory
action
Leptin
Parasympathetic
nerves
Ach
Adiponectin
Leptin
Anti-inflammatory
action
Pro-inflammatory
action
Insulin
Contractility
Mastocyte
degranulation
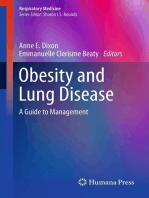
Fig. 1 View of the hormonal regulation of airway responsiveness under physiological and obesity conditions. (a) In a normal
state, adiponectin plays an anti-inflammatory role, while leptin negatively modulates airway-related pre-ganglionic neurons.
(b) In obesity/insulin resistant condition, there is a reduction in adiponectin levels in contrast to enhanced leptin and insulin
levels, which in turn plays a pro-inflammatory role in the lungs along with increased parasympathetic outflow into the
airways. Ach: acetylcholine; LR: leptin resistance.
Please cite this article as: Leiria LOS, et al, Obesity and asthma: beyond TH2 inflammation, Metabolism (2014), http://dx.doi.org/
10.1016/j.metabol.2014.10.002
M ET ABOL I S M CL IN I CA L A N D E XP E RI ME N TAL XX ( 2 01 4 ) X XX XX X
LEAN
OBESE
TNF-
IL-6
IL1-
IL-10
Arginase-1
Anti-inflammatory
pathway
IL-17A
Subclinical
Non-TH2 inflammation
AHR
= M1 macrophage
= ILC3 cells
= M2 macrophage
=Adipocite
Fig. 2 Scheme of the sub-clinical inflammation in lungs from obese and lean mice. In a lean state, M2 macrophage-released
anti-inflammatory cytokines maintain normal lung functions, while in an obese state polarized M1 macrophages release proinflammatory cytokines, inducing low-grade non-TH2 inflammation and airway hyper-reactivity (AHR). IL-1- induces IL-17
release from innate lymphoid cells (ILCs) 3 (ILC-3), facilitating airway reactivity in obesity.
resistance in obesity and type 2 diabetes, as well as its resultant
complications. Macrophage-released chemokines, such as TNF-
and IL-1, trigger a pro-inflammatory signaling cascade through
the activation of TNF and IL receptors (TNFR and ILR), respectively. Activation of both TNFRs and ILRs leads to activation of cJun N-terminal kinase (JNK) that triggers insulin receptor
substrate (IRS-1) inhibition. JNK signaling (TNF-/JNK signaling)
is a key mechanism leading to peripheral insulin resistance
[90,91] and the resultant diabetic complications. Notwithstanding, pro-inflammatory chemokines/adipokines released into the
blood by adipose tissue may drive the physiopathology of various
secondary complications to obesity in peripheral tissues.
Obesity-related asthma is associated with the presence of
increased amounts of TNF- and interleukins such as IL-6 and
IL-1 in the lung, even in the absence of an antigenic
challenge. Williams et al. [92] evaluated the impact of
TNFR2-receptor deficiency on the low-grade systemic inflammation associated with obesity and reported that obese mice
with deletion of TNFR2 were protected against innate airway
hyperactivity and presented with reduced levels of IL-17A in
comparison with controls. These findings are in accordance
with recent research in humans that showed there was a
population of alveolar macrophages with pro-inflammatory
responses to leptin stimulation in overweight asthmatics,
who also presented with increased levels of TNF- in these
alveolar macrophages [93].
Indeed, non-TH2 signaling pathways are likely to regulate
asthma. Recent studies suggest that innate lymphoid cells
(ILCs) contribute to AHR in mice. ILC-3 s produce IL-22 and IL17 and are required for important processes such as lymphoid
organogenesis, host defense in the skin, lungs, and gut and
they are also active in the lungs in some models of asthma
and in the gut in patients with colitis [94]. A previous study
reported that IL-17 can directly cause AHR [95] and might be
pathogenic in airway diseases [46]. A role for ILC-3 s producing IL-17A, thus causing the AHR associated with obesity has
recently been proposed [96]. In a recent paper, Kim et al. [96],
showed that obesity induced by a high-fat diet in mice
triggered the activation of an NLRP3 inflammasome in
macrophages resident on adipose tissue and in the lungs,
resulting in an amplification in IL-1 production, which in
turn facilitates AHR through interleukin-17 (IL-17)-producing
ILC-3 cells; this is a novel mechanism that has not been
previously linked with airway disease (Fig. 2). Moreover, both
IL-6 and IL-17A have been shown to play a pivotal role in the
pathogeneses of asthma in obese mice following a challenge
with subacute ozone exposition [45,97]; however, the mechanism by which these interleukins directly trigger
bronchoconstriction remains unknown. Both papers used
genetic adiponectin-deficient mice, showing a possible correlation between adiponectin deficiency and low-grade inflammation in the lungs. Notwithstanding, a possible potentiating
effect of M1-released chemokines towards TH2 inflammation
in the lungs from obese mice must be considered. It was
reported in a recent paper that long-term treatment with
metformin in high-fat fed ovalbumin-challenged mice was
Please cite this article as: Leiria LOS, et al, Obesity and asthma: beyond TH2 inflammation, Metabolism (2014), http://dx.doi.org/
10.1016/j.metabol.2014.10.002
M ET ABO LI S M CL IN I CA L A N D E XP E RI ME N TAL XX ( 2 01 4 ) X XX X XX
able to reduce pulmonary eosinophilia by decreasing nitric
oxide metabolite (NOx) production as a consequence of
inhibition of lung NFkB p65-binding to the iNOS promoter
region, which fails to be activated by TNF- [98]. These data
shed light on the possibility of a cross-talk between M1
macrophage-released TNF- and TH2-dependent inflammation, which may take place in obesity conditions.
Current knowledge does not enable us to obtain definitive
conclusions about how the cross-talk between adipokines
and pro-inflammatory cytokines takes place in the lungs.
Nevertheless, further investigations to study the mechanisms
by which adipokines and insulin regulate low-grade inflammation in the lungs are required to improve our understanding of the physiopathology of obesity-associated AHR.
8.
Conclusions
Mechanisms underlying obesity-related asthma are not well
comprehended yet and they are likely to involve at least two
phenotypes, which could be linked or not with TH2-dependent inflammation. Distribution and location of adipose
tissue and its adipokine release are determinant factors
influencing this correlation. Furthermore, hormones involved
in glucose homeostasis and in the pathogeneses of obesity are
likely to directly or indirectly link obesity and asthma;
however, further studies are required in order to elucidate
how changes in blood levels of these substances interact with
lung components and subsequently modify the lungs functionality, thus affecting airway responsiveness. Clinical and
basic studies highlighted the association between adipokines
or insulin with pro-inflammatory mediators and showed that
in accordance with other obesity-associated diseases, lowgrade inflammation may be determinant for the pathogeneses of asthma in obese patients. One key factor in clarifying
the association between asthma and obesity is to understand
the intercommunication between the innate immune system
signals in the lung and the adipose tissue, and to know how
insulin and adipokines mediate this conversation. Furthermore, central pathways regulating airway contractility are
likely to modulate bronchial contractility in an obese state, as
insulin and leptin signaling pathways are impaired in
hypothalamic and extra-hypothalamic nuclei in this condition, influencing other peripheral functions, such as respiratory functions.
The clinical and experimental studies presented here
lead us to infer that it is not obesity per se, but metabolic
changes (insulin resistance, leptin resistance and reduced
circulating levels of adiponectin) that accompany obesity,
which potentiate AHR directly or through cross-talk with
inflammatory pathways.
Further studies are necessary to identify the differential
mechanisms underlying the distinct asthma phenotypes that
are prevalent in obese populations. By establishing wellcharacterized markers for each phenotype, the correct diagnoses and treatment of obese-related asthma would be
facilitated. According to the results to date it is clear that the
glucocorticoid treatment does not suffice for achieving good
asthma management in obese patients. Weight loss, metabolic control and/or adjuvant pharmacological treatment with
antimuscarinics might be a useful strategy to improve disease
control in these patients.
Author Contributions
LOSL and MJAS designed the manuscript, performed the research,
discussed the articles and wrote the paper. MAM also researched
the papers included in the review and wrote the paper. All
authors read and approved the final version of the manuscript.
Funding
This study was supported by grants from INCT-Obesidade e
Diabetes and Research, Innovation and Dissemination Centers (CEPID) that are supported by Conselho Nacional de
Pesquisa (CNPq) and Fundao de Amparo Pesquisa do
Estado de So Paulo (FAPESP).
Acknowledgments
We would like to thank CNPQ and FAPESP for providing
funding for this study.
Conflict of interest
The authors declare that they have no competing interests.
REFERENCES
[1] Ford ES. The epidemiology of obesity and asthma. J Allergy
Clin Immunol 2005;115:897909.
[2] Taylor B, Mannino D, Brown C, Crocker D, Twum-Baah N,
Holguin F. Body mass index and asthma severity in the
National Asthma Survey. Thorax 2008;63:1420.
[3] Popkin BM. Global nutrition dynamics: the world is shifting
rapidly toward a diet linked with noncommunicable diseases.
Am J Clin Nutr 2006;84:28998.
[4] Akerman MJ, Calacanis CM, Madsen MK. Relationship between
asthma severity and obesity. J Asthma 2004;41:5216.
[5] Peters-Golden M, Swern A, Bird SS, Hustad CM, Grant E,
Edelman JM. Influence of body mass index on the response to
asthma controller agents. Eur Respir J 2006;27:495503.
[6] Sutherland ER, Lehman EB, Teodorescu M, Wechsler ME.
National Heart, Lung, and Blood Institute's Asthma Clinical
Research Network. Body mass index and phenotype in
subjects with mild-to-moderate persistent asthma. J Allergy
Clin Immunol 2009;123:132834.
[7] Camargo Jr CA, Boulet LP, Sutherland ER, Busse WW, Yancey SW,
Emmett AH, et al. Body mass index and response to asthma
therapy: fluticasone propionate/salmeterol versus montelukast.
J Asthma 2010;47:7682.
[8] Telenga ED, Tideman SW, Kerstjens HA, Hacken NH, Timens W,
Postma DS, et al. Obesity in asthma: more neutrophilic
inflammation as a possible explanation for a reduced treatment
response. Allergy 2012;67:10608.
[9] Locksley RM. Asthma and allergic inflammation. Cell 2010;
140:77783.
Please cite this article as: Leiria LOS, et al, Obesity and asthma: beyond TH2 inflammation, Metabolism (2014), http://dx.doi.org/
10.1016/j.metabol.2014.10.002
M ET ABOL I S M CL IN I CA L A N D E XP E RI ME N TAL XX ( 2 01 4 ) X XX XX X
[10] Wenzel SE. Asthma phenotypes: the evolution from clinical
to molecular approaches. Nat Med 2012;18:71625.
[11] King GG, Brown NJ, Diba C, Thorpe CW, Muoz P, Marks GB,
et al. The effects of body weight on airway calibre. Eur Respir J
2005;25:896901.
[12] Chapman DG, Berend N, King GG, Salome CM. Increased
airway closure is a determinant of airway
hyperresponsiveness. Eur Respir J 2008;32:15639.
[13] Farah CS, Kermode JA, Downie SR, Brown NJ, Hardaker KM,
Berend N, et al. Obesity is a determinant of asthma control
independent of inflammation and lung mechanics. Chest
2011;140:65966.
[14] Lessard A, Turcotte H, Cormier Y, Boulet LP. Obesity and
asthma: a specific phenotype? Chest 2008;134:31723.
[15] Todd DC, Armstrong S, DSilva L, Allen CJ, Hargreave FE,
Parameswaran K. Effect of obesity on airway inflammation: a
cross-sectional analysis of body mass index and sputum cell
counts. Clin Exp Allergy 2007;37:104954.
[16] Sutherland TJ, Cowan JO, Young S, Goulding A, Grant AM,
Williamson A, et al. The association between obesity and
asthma: interactions between systemic and airway inflammation. Am J Respir Crit Care Med 2008;178:46975.
[17] Shore SA. Obesity and asthma: location, location, location.
Eur Respir J 2013;41:2534.
[18] Sideleva O, Suratt BT, Black KE, Tharp WG, Pratley RE,
Forgione P, et al. Obesity and asthma: an inflammatory
disease of adipose tissue not the airway. Am J Respir Crit Care
Med 2012;186:598605.
[19] Camargo Jr CA, Sutherland ER, Bailey W, Castro M, Yancey SW,
Emmett AH, et al. Effect of increased body mass index on asthma
risk, impairment and response to asthma controller therapy in
African Americans. Curr Med Res Opin 2010;26:162935.
[20] Arteaga-Solis E, Zee T, Emala CW, Vinson C, Wess J, Karsenty G.
Inhibition of leptin regulation of parasympathetic signaling as
a cause of extreme body weight-associated asthma. Cell Metab
2013;17:3548.
[21] Scott HA, Gibson PG, Garg ML, Wood LG. Airway inflammation is augmented by obesity and fatty acids in asthma. Eur
Respir J 2011;38:594602.
[22] Desai D, Newby C, Symon FA, Haldar P, Shah S, Gupta S.
Elevated sputum interleukin-5 and submucosal eosinophilia
in obese individuals with severe asthma. Am J Respir Crit
Care Med 2013;188:65763.
[23] Grotta MB, Squebola-Cola DM, Toro AA, Ribeiro MA, Mazon SB,
Ribeiro JD, et al. Obesity increases eosinophil activity in
asthmatic children and adolescents. BMC Pulm Med 2013;13:39.
[24] Calixto MC, Lintomen L, Schenka A, Saad MJ, Zanesco A,
Antunes E. Obesity enhances eosinophilic inflammation in a
murine model of allergic asthma. Br J Pharmacol 2010;159:
61725.
[25] Mito N, Kitada C, Hosoda T, Sato K. Effect of diet-induced
obesity on ovalbumin-specific immune response in a murine
asthma model. Metabolism 2002;51:12416.
[26] Lintomen L, Calixto MC, Schenka A, Antunes E. Allergeninduced bone marrow eosinophilopoiesis and airways eosinophilic inflammation in leptin-deficient ob/ob mice. Obesity
(Silver Spring) 2012;20:195965.
[27] Lloyd CM, Saglani S. Eosinophils in the Spotlight: Finding the
link between obesity and asthma. Nat Med 2013;19:9767.
[28] Boulet LP. Asthma and obesity. Clin Exp Allergy 2013;43:821.
[29] Barnes PJ, Adcock IM. Glucocorticoid resistance in inflammatory diseases. Lancet 2009;373:190517.
[30] Boulet LP, Franssen E. Influence of obesity on response to
fluticasone with or without salmeterol in moderate asthma.
Respir Med 2007;101:22407.
[31] Nie Z, Jacoby DB, Fryer AD. Hyperinsulinemia potentiates
airway responsiveness to parasympathetic nerve stimulation
in obese rats. Am J Respir Cell Mol Biol 2014. http://dx.doi.org/
10.1165/rcmb.2013-0452OC.
[32] Al-Alwan A, Bates JH, Chapman DG, Kaminsky DA, DeSarno MJ,
Irvin CG, et al. The nonallergic asthma of obesity. A matter of
distal lung compliance. Am J Respir Crit Care Med 2014;189:
1494502.
[33] Dixon AE, Pratley RE, Forgione PM, Kaminsky DA, WhittakerLeclair LA, Griffes LA, et al. Effects of obesity and bariatric
surgery on airway hyperresponsiveness, asthma control, and
inflammation. J Allergy Clin Immunol 2011;128:50815.
[34] Scherer PE, Williams S, Fogliano M, Baldini G, Lodish HF. A
novel serum protein similar to C1q, produced exclusively in
adipocytes. J Biol Chem 1995;270:267469.
[35] Schraw T, Wang ZV, Halberg N, Hawkins M, Scherer PE.
Plasma adiponectin complexes have distinct biochemical
characteristics. Endocrinology 2008;149(5):227082.
[36] Tsao TS, Murrey HE, Hug C, Lee DH, Lodish HF. Oligomerization state-dependent activation of NF-kappa B signaling
pathway by adipocyte complement-related protein of 30 kDa
(Acrp30). J Biol Chem 2002;277:2935962.
[37] Yamauchi T, Kamon J, Ito Y, Tsuchida A, Yokomizo T, Kita S,
et al. Cloning of adiponectin receptors that mediate antidiabetic metabolic effects. Nature 2003;423:7629.
[38] Berg AH, Combs TP, Du X, Brownlee M, Scherer PE. The
adipocyte-secreted protein Acrp30 enhances hepatic insulin
action. Nat Med 2001;7:94753.
[39] Pajvani UB, Du X, Combs TP, Berg AH, Rajala MW, Schulthess T,
et al. Structure-function studies of the adipocyte-secreted
hormone Acrp30/adiponectin. Implications for metabolic regulation and bioactivity. J Biol Chem 2003;278:907385.
[40] Waki H, Yamauchi T, Kamon J, Ito Y, Uchida S, Kita S, et al.
Impaired multimerization of human adiponectin mutants
associated with diabetes. Molecular structure and multimer
formation of adiponectin. J Biol Chem 2003;278:4035263.
[41] Kadowaki T, Yamauchi T, Kubota N, Hara K, Ueki K, Tobe K.
Adiponectin and adiponectin receptors in insulin resistance,
diabetes, and the metabolic syndrome. J Clin Invest 2006;116:
178492.
[42] Li S, Shin HJ, Ding EL, van Dam RM. Adiponectin levels and
risk of type 2 diabetes: a systematic review and metaanalysis. JAMA 2009;302:17988.
[43] Pajvani UB, Hawkins M, Combs TP, Rajala MW, Doebber T,
Berger JP, et al. Complex distribution, not absolute amount of
adiponectin, correlates with thiazolidinedione-mediated improvement in insulin sensitivity. J Biol Chem 2004;279:
1215262.
[44] Yamauchi T, Nio Y, Maki T, Kobayashi M, Takazawa T, Iwabu M,
et al. Targeted disruption of AdipoR1 and AdipoR2 causes
abrogation of adiponectin binding and metabolic actions. Nat
Med 2007;13:3329.
[45] Williams AS, Kasahara DI, Verbout NG, Fedulov AV, Zhu M,
Si H, et al. Role of the adiponectin binding protein, Tcadherin(Cdh13), in allergic airways responses in mice. PLoS
One 2012;7:e41088.
[46] Medoff BD, Okamoto Y, Leyton P, Weng M, Sandall BP, Raher MJ,
et al. Adiponectin deficiency increases allergic airway inflammation and pulmonary vascular remodeling. Am J Respir Cell
Mol Biol 2009;41:397406.
[47] Kasahara DI, Kim HY, Williams AS, Verbout NG, Tran J, Si H,
et al. Pulmonary inflammation induced by subacute ozone is
augmented in adiponectin-deficient mice: role of IL-17A. J
Immunol 2012;188:455867.
[48] Fahy JV, Kim KW, Liu J, Boushey HA. Prominent neutrophilic
inflammation in sputum from subjects with asthma exacerbation. J Allergy Clin Immunol 1995;95:84352.
[49] Ordonez CL, Shaughnessy TE, Matthay MA, Fahy JV. Increased
neutrophil numbers and il-8 levels in airway secretions in
acute severe asthma: clinical and biologic significance. Am J
Respir Crit Care Med 2000;161:118590.
[50] Zhu XL, Qin XQ, Xiang Y, Tan YR, Qu XP, Liu HJ. Adipokine
adiponectin is a potential protector to human bronchial
Please cite this article as: Leiria LOS, et al, Obesity and asthma: beyond TH2 inflammation, Metabolism (2014), http://dx.doi.org/
10.1016/j.metabol.2014.10.002
M ET ABO LI S M CL IN I CA L A N D E XP E RI ME N TAL XX ( 2 01 4 ) X XX X XX
[51]
[52]
[53]
[54]
[55]
[56]
[57]
[58]
[59]
[60]
[61]
[62]
[63]
[64]
[65]
[66]
[67]
[68]
[69]
[70]
epithelial cell for regulating proliferation, wound repair and
apoptosis: comparison with leptin and resistin. Peptides
2013;40:3441.
Jartti T, Saarikoski L, Jartti L, Lisinen I, Jula A, Huupponen R,
et al. Obesity, adipokines and asthma. Allergy 2009;64:7707.
Holguin F, Rojas M, Brown LA, Fitzpatrick AM. Airway and
plasma leptin and adiponectin in lean and obese asthmatics
and controls. J Asthma 2011;48:21723.
Aydin M, Koca C, Ozol D, Uysal S, Yildirim Z, Kavakli HS, et al.
Interaction of metabolic syndrome with asthma in postmenopausal women: role of adipokines. Inflammation 2013;
36:12328.
Sood A, Qualls C, Schuyler M, Thyagarajan B, Steffes MW,
Smith LJ, et al. Low serum adiponectin predicts future risk for
asthma in women. Am J Respir Crit Care Med 2012;186:417.
Schwartz MW, Porte Jr D. Diabetes, obesity, and the brain.
Science 2005;307:3759.
Elmquist JK, Coppari R, Balthasar N, Ichinose M, Lowell BB.
Identifying hypothalamic pathways controlling food intake,
body weight, and glucose homeostasis. J Comp Neurol 2005;
493:6371.
Campfield LA, Smith FJ, Guisez Y, Devos R, Burn P. Recombinant mouse OB protein: evidence for a peripheral signal
linking adiposity and central neural networks. Science 1995;
269:5469.
Tartaglia LA, Dembski M, Weng X, Deng N, Culpepper J, Devos R,
et al. Identification and expression cloning of a leptin receptor,
OB-R. Cell 1995;83:126371.
Montague CT, Farooqi IS, Whitehead JP, Soos MA, Rau H,
Wareham NJ, et al. Congenital leptin deficiency is associated
with severe early-onset obesity in humans. Nature 1997;387:
9038.
Clment K, Vaisse C, Lahlou N, Cabrol S, Pelloux V, Cassuto D,
et al. A mutation in the humanleptin receptor gene causes
obesity and pituitary dysfunction. Nature 1998;392:398401.
Myers Jr MG, Olson DP. Central nervous system control of
metabolism. Nature 2012;491:35763.
Zamorano PL, Mahesh VB, De Sevilla LM, Chorich LP, Bhat GK,
Brann DW. Expression and localization of the leptin receptor
in endocrine and neuroendocrine tissues of the rat. Neuroendocrinology 1997;65:2238.
Fei H, Okano HJ, Li C, Lee GH, Zhao C, Darnell R, et al.
Anatomic localization of alternatively spliced leptin receptors (Ob-R) in mouse brain and other tissues. Proc Natl Acad
Sci U S A 1997;94:70015.
Cohen P, Zhao C, Cai X, Montez JM, Rohani SC, Feinstein P,
et al. Selective deletion of leptin receptor in neurons leads to
obesity. J Clin Invest 2001;108:111321.
de Luca C, Kowalski TJ, Zhang Y, Elmquist JK, Lee C, Kilimann
MW, et al. Complete rescue of obesity, diabetes, and
infertility in db/db mice by neuron-specific LEPR-B
transgenes. J Clin Invest 2005;115:348493.
Li B, Shi Z, Cassaglia PA, Brooks VL. Leptin acts in the
forebrain to differentially influence baroreflex control of
lumbar, renal, and splanchnic sympathetic nerve activity
and heart rate. Hypertension 2013;61:8129.
Desprs JP, Lemieux I. Abdominal obesity and metabolic
syndrome. Nature 2006;444:8817.
Saad MJ, Carvalheira JB, Velloso LA. Birth weight and type 2
diabetes in adults. JAMA 2009;301:1539.
Tsukumo DM, Carvalho-Filho MA, Carvalheira JB, Prada PO,
Hirabara SM, Schenka AA, et al. Loss-of-function mutation in
Toll-like receptor 4 prevents diet-induced obesity and insulin
resistance. Diabetes 2007;56:198698.
Milanski M, Degasperi G, Coope A, Morari J, Denis R, Cintra DE,
et al. Saturated fatty acids produce an inflammatory response
predominantly through the activation of TLR4 signaling in
hypothalamus: implications for the pathogenesis of obesity. J
Neurosci 2009;29:35970.
[71] Thuesen BH, Husemoen LL, Hersoug LG, Pisinger C, Linneberg A.
Insulin resistance as a predictor of incident asthma-like
symptoms in adults. Clin Exp Allergy 2009;39:7007.
[72] Arshi M, Cardinal J, Hill RJ, Davies PS, Wainwright C. Asthma
and insulin resistance in children. Respirology 2010;15:
77984.
[73] Vikram A, Jena GB, Ramarao P. Increased cell proliferation
and contractility of prostate in insulin resistant rats: linking
hyperinsulinemia with benign prostate hyperplasia. Prostate
2010;70:7989.
[74] Carvalho CR, Carvalheira JB, Lima MH, Zimmerman SF,
Caperuto LC, Amanso A, et al. Novel signal transduction
pathway for luteinizing hormone and its interaction with
insulin: activation of Janus kinase/signal transducer and
activator of transcription and phosphoinositol 3-kinase/Akt
pathways. Endocrinology 2003;144:63847.
[75] Zecchin HG, Priviero FB, Souza CT, Zecchin KG, Prada PO,
Carvalheira JB, et al. Defective insulin and acetylcholine
induction of endothelial cell-nitric oxide synthase through
insulin receptor substrate/Akt signaling pathway in aorta of
obese rats. Diabetes 2007;56:101424.
[76] Contreras C, Snchez A, Martnez P, Raposo R, Climent B,
Garca-Sacristn A, et al. Insulin resistance in penile arteries
from a rat model of metabolic syndrome. Br J Pharmacol 2010;
161:35064.
[77] Leiria LO, Sollon C, Bu FR, Mnica FZ, D'Ancona CL, De Nucci G,
et al. Insulin relaxes bladder via PI3K/AKT/eNOS pathway
activation in mucosa: unfolded protein response-dependent
insulin resistance as a cause of obesity-associated overactive
bladder. J Physiol 2013;591:225973.
[78] Scherrer U, Randin D, Vollenweider P, Vollenweider L, Nicod P.
Nitric oxide release accounts for insulins vascular effects in
humans. J Clin Invest 1994;94:25115.
[79] Lee JH, Ragolia L. AKT phosphorylation is essential for
insulin-induced relaxation of rat vascular smooth muscle
cells. Am J Physiol Cell Physiol 2006;291:C135565.
[80] Dimmeler S, Fleming I, Fisslthaler B, Hermann C, Busse R,
Zeiher AM. Activation of nitric oxide synthase in endothelial
cells by Akt-dependent phosphorylation. Nature 1999;399:
6015.
[81] Belmonte KE, Jacoby DB, Fryer AD. Increased function of
inhibitory neuronal M2 muscarinic receptors in diabetic rat
lungs. Br J Pharmacol 1997;121:128794.
[82] Schaafsma D, Gosens R, Ris JM, Zaagsma J, Meurs H,
Nelemans SA. Insulin induces airway smooth muscle contraction. Br J Pharmacol 2007;150:13642.
[83] Cavalher-Machado SC, de Lima WT, Damazo AS, de Frias
Carvalho V, Martins MA, e Silva PM, et al. Down-regulation of
mast cell activation and airway reactivity in diabetic rats: role
of insulin. Eur Respir J 2004;24:5528.
[84] Belmonte KE, Fryer AD, Costello RW. Role of insulin in
antigen-induced airway eosinophilia and neuronal M2 muscarinic receptor dysfunction. J Appl Physiol 1998;85:170818.
[85] Douek IF, Leech NJ, Gillmor HA, Bingley PJ, Gale EA. Children
with type-1 diabetes and their unaffected siblings have fewer
symptoms of asthma. Lancet 1999;353:1850.
[86] Filippi BM, Yang CS, Tang C, Lam TK. Insulin activates Erk1/2
signaling in the dorsal vagal complex to inhibit glucose
production. Cell Metab 2012;16:50010.
[87] Kc P, Martin RJ. Role of central neurotransmission and
chemoreception on airway control. Respir Physiol Neurobiol
2010;173:21322.
[88] Oliveira AG, Araujo TG, Carvalho BM, Guadagnini D, Rocha GZ,
Bagarolli RA, et al. Acute exercise induces a phenotypic switch
in adipose tissue macrophage polarization in diet-induced
obese rats. Obesity (Silver Spring) 2013;21:254556.
[89] Clria J, Gonzlez-Priz A, Lpez-Vicario C, Rius B, Titos E.
New insights into the role of macrophages in adipose tissue
inflammation and fatty liver disease: modulation by
Please cite this article as: Leiria LOS, et al, Obesity and asthma: beyond TH2 inflammation, Metabolism (2014), http://dx.doi.org/
10.1016/j.metabol.2014.10.002
10
[90]
[91]
[92]
[93]
[94]
M ET ABOL I S M CL IN I CA L A N D E XP E RI ME N TAL XX ( 2 01 4 ) X XX XX X
endogenous omega-3 Fatty Acid-derived lipid mediators.
Front Immunol 2011;2:49.
Hotamisligil GS, Peraldi P, Budavari A, Ellis R, White MF,
Spiegelman BM. IRS- 1-mediated inhibition of insulin receptor
tyrosine kinase activity in TNF-alpha-and obesity-induced
insulin resistance. Science 2006;271:6658.
Hotamisligil GS. Inflammation and metabolic disorders.
Nature 2006;444:8607.
Williams AS, Chen L, Kasahara DI, Si H, Wurmbrand AP,
Shore SA. Obesity and airway responsiveness: role of TNFR2.
Pulm Pharmacol Ther 2013;26:44454.
Lugogo NL, Hollingsworth JW, Howell DL, Que LG, Francisco D,
Church TD, et al. Alveolar macrophages from overweight/
obese subjects with asthma demonstrate a proinflammatory
phenotype. Am J Respir Crit Care Med 2012;186:40411.
Coccia M, Harrison OJ, Schiering C, Asquith MJ, Becher B,
Powrie F, et al. IL-1beta mediates chronic intestinal inflammation by promoting the accumulation of IL-17A secreting
[95]
[96]
[97]
[98]
innate lymphoid cells and CD4(1) Th17 cells. J Exp Med 2012;
209:1595609.
Kudo M, Melton AC, Chen C, Engler MB, Huang KE, Ren X, et al.
IL-17A produced by alphabeta T cells drives airway hyperresponsiveness in mice and enhances mouse and human
airway smooth muscle contraction. Nat Med 2012;18:54754.
Kim HY, Lee HJ, Chang YJ, Pichavant M, Shore SA, Fitzgerald KA,
et al. Interleukin-17-producing innate lymphoid cells and the
NLRP3 inflammasome facilitate obesity-associated airway
hyperreactivity. Nat Med 2014;20:5461.
Kasahara DI, Kim HY, Mathews JA, Verbout NG, Williams AS,
Wurmbrand AP, et al. Pivotal role of IL-6 in the
hyperinflammatory responses to subacute ozone in
adiponectin deficient mice. Am J Physiol Lung Cell Mol
Physiol 2014;306:L50820.
Calixto MC, Lintomen L, Andr DM, et al. Metformin attenuates
the exacerbation of the allergic eosinophilic inflammation in
high fat-diet-induced obesity in mice. PLoS One 2013;8:e76786.
Please cite this article as: Leiria LOS, et al, Obesity and asthma: beyond TH2 inflammation, Metabolism (2014), http://dx.doi.org/
10.1016/j.metabol.2014.10.002
Вам также может понравиться
- Impact of Obesity On Respiratory Disorder SeverityДокумент94 страницыImpact of Obesity On Respiratory Disorder SeverityThaman ThimmaiahОценок пока нет
- Adiponect Dça Pulm 2014Документ16 страницAdiponect Dça Pulm 2014Cristie AraujoОценок пока нет
- 1 s2.0 S0929664615003460 MainДокумент7 страниц1 s2.0 S0929664615003460 MainEva GarciaОценок пока нет
- Pathophysiology of Asthma - StatPearls - NCBI BookshelfДокумент7 страницPathophysiology of Asthma - StatPearls - NCBI BookshelfJEAN CERNA SOLISОценок пока нет
- EU Baffi2016 - MetabДокумент33 страницыEU Baffi2016 - MetabDumitru BiniucОценок пока нет
- PCRM Chronic Obstructive Pulmonary Disease - Nutrition Guide For CliniciansДокумент5 страницPCRM Chronic Obstructive Pulmonary Disease - Nutrition Guide For CliniciansRJAY VINCENT BUENAFEОценок пока нет
- Respiratory Research: Diet and Asthma: Looking Back, Moving ForwardДокумент7 страницRespiratory Research: Diet and Asthma: Looking Back, Moving ForwardRiski DohartuaОценок пока нет
- Asthma: Signs and SymptomsДокумент57 страницAsthma: Signs and SymptomsAjp Ryuzaki CaesarОценок пока нет
- Ojo Asmra Ilnk Treat y OutДокумент6 страницOjo Asmra Ilnk Treat y OutJulio Juarez MolinaОценок пока нет
- CopdДокумент14 страницCopdMohd Farid Bin RosliОценок пока нет
- ASTHMAДокумент17 страницASTHMAvinda astri permatasariОценок пока нет
- CHEST Nov 2005Документ183 страницыCHEST Nov 2005rizjkuramaОценок пока нет
- Fast Facts: Asthma: Improve patient self-management and drug use, achieve asthma controlОт EverandFast Facts: Asthma: Improve patient self-management and drug use, achieve asthma controlОценок пока нет
- Asthma: A. Practice EssentialsДокумент8 страницAsthma: A. Practice EssentialsCandha NurcahyaОценок пока нет
- Acute Severe AsthmaДокумент5 страницAcute Severe AsthmaRizsa Aulia DanestyОценок пока нет
- Obesity and AsthmaДокумент26 страницObesity and AsthmaDumitru BiniucОценок пока нет
- Content ServerДокумент11 страницContent ServerVerónica Duménez JofréОценок пока нет
- Asthma MedscapeДокумент21 страницаAsthma MedscapeDnyanesh LimayeОценок пока нет
- BackgroundДокумент18 страницBackgroundsanasharОценок пока нет
- Asthma: Practice EssentialsДокумент12 страницAsthma: Practice EssentialsIda WilonaОценок пока нет
- Emphysema BrochureДокумент2 страницыEmphysema Brochureapi-242394302Оценок пока нет
- Ashtma Timeline T2Документ21 страницаAshtma Timeline T2ISABEL SOFIA CABARCAS COGOLLOОценок пока нет
- Manejo de Status AsmaticoДокумент17 страницManejo de Status Asmaticobuqmir6977Оценок пока нет
- CAM Therapies For Symptoms Management of Asthma and COPDДокумент14 страницCAM Therapies For Symptoms Management of Asthma and COPDCharlyn MoellersОценок пока нет
- Asthma Case PresentationДокумент3 страницыAsthma Case Presentationfernandezrachelle44Оценок пока нет
- Acute Exacerbation of COPD Nursing Application of Evidence-Based GuidelinesДокумент17 страницAcute Exacerbation of COPD Nursing Application of Evidence-Based GuidelinesCandice ChengОценок пока нет
- Fisiopatologia de Asma en Obseidad No AlergicoДокумент9 страницFisiopatologia de Asma en Obseidad No AlergicoJimmyОценок пока нет
- Acute Lung InjuryДокумент5 страницAcute Lung InjuryKinanti Devia LarasatiОценок пока нет
- 2° Artículo de EpocДокумент10 страниц2° Artículo de EpocveroarujogonzalesОценок пока нет
- An Official American Thoracic Workshop Report Obesity and AsthmaДокумент11 страницAn Official American Thoracic Workshop Report Obesity and Asthmaडा. सत्यदेव त्यागी आर्यОценок пока нет
- Status AsthmaticusДокумент22 страницыStatus AsthmaticusGali Kesuma100% (1)
- Update On Severe Asthma: What We Know and What We NeedДокумент8 страницUpdate On Severe Asthma: What We Know and What We Needtaksim2011Оценок пока нет
- Asthma Thesis TopicsДокумент5 страницAsthma Thesis Topicsgjfcp5jb100% (1)
- Asthma Dissertation IdeasДокумент6 страницAsthma Dissertation IdeasPaperWriterServiceSingapore100% (1)
- Spirometry and DiabetesДокумент2 страницыSpirometry and DiabetesEliana MuisОценок пока нет
- Diagnosis and Treatment of Chronic CoughОт EverandDiagnosis and Treatment of Chronic CoughSang Heon ChoОценок пока нет
- Thorax00329 0017Документ2 страницыThorax00329 0017Dário Talita SantanaОценок пока нет
- Gastro Oesophageal RefluxДокумент7 страницGastro Oesophageal Refluxjustifieda13Оценок пока нет
- Clinical Updates in the Management of Severe Asthma: New Strategies for Individualizing Long-term CareОт EverandClinical Updates in the Management of Severe Asthma: New Strategies for Individualizing Long-term CareОценок пока нет
- DNB - Vol31 - Nosuppl 5 - 786Документ6 страницDNB - Vol31 - Nosuppl 5 - 786Nagib MuhammadОценок пока нет
- Obesity and Lung Disease: A Guide to ManagementОт EverandObesity and Lung Disease: A Guide to ManagementAnne E. DixonОценок пока нет
- Batuk EfektifДокумент11 страницBatuk EfektifDadi ArdiansyahОценок пока нет
- Mechanical Ventilation - Lessons From The ARDSNet TrialДокумент5 страницMechanical Ventilation - Lessons From The ARDSNet TrialRDG20202Оценок пока нет
- Ers 2012.fullДокумент15 страницErs 2012.fullLinto JohnОценок пока нет
- Asthma, Obesity, and Microbiota - A Complex Immunological InteractionДокумент33 страницыAsthma, Obesity, and Microbiota - A Complex Immunological InteractionMarcelo CosendeyОценок пока нет
- Copd Nihilismo BuenisimoДокумент8 страницCopd Nihilismo BuenisimoJose Lopez FuentesОценок пока нет
- The Systemic Face of Airway Diseases: The Role of C-Reactive ProteinДокумент3 страницыThe Systemic Face of Airway Diseases: The Role of C-Reactive ProteinHarli FeryadiОценок пока нет
- Allergy-Asthma ConnectionДокумент11 страницAllergy-Asthma ConnectionLaras Bani WasesoОценок пока нет
- Management of Cough An Empiric Integrative Approach To TheДокумент12 страницManagement of Cough An Empiric Integrative Approach To TheDavid PazОценок пока нет
- Asthma in Pregnancy 2020Документ10 страницAsthma in Pregnancy 2020Rosintchi MirsalОценок пока нет
- Airway Inflammation and Remodelling in Asthma - Cause and Effect?Документ13 страницAirway Inflammation and Remodelling in Asthma - Cause and Effect?Pauroosh KaushalОценок пока нет
- Immunology of Asthma and Chronic Obstructive Pulmonary DiseaseДокумент10 страницImmunology of Asthma and Chronic Obstructive Pulmonary DiseaseClaudio Luis VenturiniОценок пока нет
- Impact of Immunoglobulin E and Airway Obstruction On BronchiectasisДокумент7 страницImpact of Immunoglobulin E and Airway Obstruction On BronchiectasisRichie Irvanto CiandraОценок пока нет
- Liu (Obesity-Associated Metabolic Signatures in Asthma) 2018Документ20 страницLiu (Obesity-Associated Metabolic Signatures in Asthma) 2018Luis Taborda BarataОценок пока нет
- Status AsmatikusДокумент8 страницStatus AsmatikusFebrianaОценок пока нет
- HSNS264 Assessment 1Документ6 страницHSNS264 Assessment 1Sophie AndersonОценок пока нет
- Relacion Entre Disfagia y EPOCДокумент6 страницRelacion Entre Disfagia y EPOCtatiana gonzalezОценок пока нет
- COPD Una Enfermedad Multicomponente 2005Документ13 страницCOPD Una Enfermedad Multicomponente 2005rafodoc221968Оценок пока нет
- Eosinophil Biology in COPD: EditorialДокумент2 страницыEosinophil Biology in COPD: EditorialAbby OliivasОценок пока нет
- Jurnal DR ATSДокумент8 страницJurnal DR ATSQonita Aizati QomaruddinОценок пока нет
- Osha 3162Документ40 страницOsha 3162Irina Luciana Dumitriu100% (1)
- AT R-At R Cross Talk: Cross Regulation of Angiotensin Ii Type 1 Receptor and The Angiotensin Ii Type 2 ReceptorДокумент5 страницAT R-At R Cross Talk: Cross Regulation of Angiotensin Ii Type 1 Receptor and The Angiotensin Ii Type 2 ReceptorIrina Luciana DumitriuОценок пока нет
- 3 s2.0 B9780128013649000195 MainДокумент5 страниц3 s2.0 B9780128013649000195 MainIrina Luciana DumitriuОценок пока нет
- Preclinical and Clinical Development of Angiotensin Peptides (Mas/Ang (1-7) / ACE-2) : Future Clinical ApplicationДокумент6 страницPreclinical and Clinical Development of Angiotensin Peptides (Mas/Ang (1-7) / ACE-2) : Future Clinical ApplicationIrina Luciana DumitriuОценок пока нет
- The Angiotensin AT Receptor in Myocardial Infarction: Elena KaschinaДокумент7 страницThe Angiotensin AT Receptor in Myocardial Infarction: Elena KaschinaIrina Luciana DumitriuОценок пока нет
- AT R-At R Cross Talk: Cross Regulation of Angiotensin Ii Type 1 Receptor and The Angiotensin Ii Type 2 ReceptorДокумент5 страницAT R-At R Cross Talk: Cross Regulation of Angiotensin Ii Type 1 Receptor and The Angiotensin Ii Type 2 ReceptorIrina Luciana DumitriuОценок пока нет
- 3 s2.0 B9780128013649000195 MainДокумент5 страниц3 s2.0 B9780128013649000195 MainIrina Luciana DumitriuОценок пока нет
- The Angiotensin AT Receptor in Myocardial Infarction: Elena KaschinaДокумент7 страницThe Angiotensin AT Receptor in Myocardial Infarction: Elena KaschinaIrina Luciana DumitriuОценок пока нет
- DalyKavanagh2001 PDFДокумент9 страницDalyKavanagh2001 PDFIrina Luciana DumitriuОценок пока нет
- Extras de Cont / Account: 2. Valuta / Currency 3. Data Extras / Statement DateДокумент1 страницаExtras de Cont / Account: 2. Valuta / Currency 3. Data Extras / Statement DateIrina Luciana DumitriuОценок пока нет
- Lead in Blood Many ContriesДокумент1 страницаLead in Blood Many ContriesIrina Luciana DumitriuОценок пока нет
- Animal Models With A Genetic Alteration of AT Expression: AbbreviationsДокумент6 страницAnimal Models With A Genetic Alteration of AT Expression: AbbreviationsIrina Luciana DumitriuОценок пока нет
- JTP 1004Документ3 страницыJTP 1004Irina Luciana DumitriuОценок пока нет
- Esti2015 P-0093Документ36 страницEsti2015 P-0093Irina Luciana DumitriuОценок пока нет
- Respiratory DiseaseДокумент3 страницыRespiratory DiseaseIrina Luciana DumitriuОценок пока нет
- Occupational and Recreational Musculoskeletal Disorders 2017Документ30 страницOccupational and Recreational Musculoskeletal Disorders 2017Irina Luciana DumitriuОценок пока нет
- Pulmonary Aspergillosis 2011 - Tabel BoliДокумент19 страницPulmonary Aspergillosis 2011 - Tabel BoliIrina Luciana DumitriuОценок пока нет
- Daly Kavanagh 2001Документ9 страницDaly Kavanagh 2001Irina Luciana DumitriuОценок пока нет
- Chronic Pulmonary Aspergillosis An Updated On Diagnosis and TreatmentДокумент13 страницChronic Pulmonary Aspergillosis An Updated On Diagnosis and TreatmentCahrun CarterОценок пока нет
- Clinical Manifestations and Treatment Outcomes ofДокумент5 страницClinical Manifestations and Treatment Outcomes ofIrina Luciana DumitriuОценок пока нет
- Work-Related Voice DisorderДокумент18 страницWork-Related Voice DisorderIrina Luciana DumitriuОценок пока нет
- Lead Toxicity As An Etiology For Abdominal Pain in The Emergency Department 2014Документ6 страницLead Toxicity As An Etiology For Abdominal Pain in The Emergency Department 2014Irina Luciana DumitriuОценок пока нет
- Occupational and Environmental Medicine: Chapter ContentsДокумент3 страницыOccupational and Environmental Medicine: Chapter ContentsIrina Luciana DumitriuОценок пока нет
- Acquired Peripheral Neuropathies 2017Документ44 страницыAcquired Peripheral Neuropathies 2017Irina Luciana DumitriuОценок пока нет
- ASPERGILOZA INVAZIVA 2015 - Prezentare de Caz - AspergilozaДокумент5 страницASPERGILOZA INVAZIVA 2015 - Prezentare de Caz - AspergilozaIrina Luciana Dumitriu100% (1)
- Principles of Occupational and Environmental DiseaseДокумент15 страницPrinciples of Occupational and Environmental DiseaseIrina Luciana DumitriuОценок пока нет
- Alvarez 2014 Guidelines For The Diagnosis and Monitoring of SilicosisДокумент8 страницAlvarez 2014 Guidelines For The Diagnosis and Monitoring of SilicosisIrina Luciana DumitriuОценок пока нет
- Asthma in The Workplace 2016Документ35 страницAsthma in The Workplace 2016Irina Luciana DumitriuОценок пока нет
- 2010+cavitated ConglomerateMass in Silicosis Indicating TBCДокумент4 страницы2010+cavitated ConglomerateMass in Silicosis Indicating TBCIrina Luciana DumitriuОценок пока нет
- 2013 - Aspergilloma Mimicking A Lung CancerДокумент3 страницы2013 - Aspergilloma Mimicking A Lung CancerIrina Luciana DumitriuОценок пока нет
- Chapter 2 Inflamation (B)Документ86 страницChapter 2 Inflamation (B)مختبرات ابوسارةОценок пока нет
- (Nestor L. Muller) Imaging of Pulmonary InfectionsДокумент232 страницы(Nestor L. Muller) Imaging of Pulmonary InfectionsNouga Sarraj100% (1)
- 143 SG 9Документ43 страницы143 SG 9cake girlsОценок пока нет
- Tropical Infectious Diseases PDFДокумент1 788 страницTropical Infectious Diseases PDFMax Izarra Almonacid0% (1)
- Immunology-Notes, Sam Roman PDFДокумент57 страницImmunology-Notes, Sam Roman PDFTejus PradeepОценок пока нет
- Acute Inflammation Robbins Basic Pathology Inflammation Repair PDFДокумент24 страницыAcute Inflammation Robbins Basic Pathology Inflammation Repair PDFJessica Bittar Camargo100% (1)
- Textbook of Surgery For Dental Students-smile4DrДокумент400 страницTextbook of Surgery For Dental Students-smile4DrRotariu Ana Maria100% (8)
- Tuberculosis - StatPearls - NCBI BookshelfДокумент10 страницTuberculosis - StatPearls - NCBI BookshelfDhany karubuyОценок пока нет
- General Principles of Microbial Pathogenesis: MicrobiologyДокумент5 страницGeneral Principles of Microbial Pathogenesis: MicrobiologyAbi SulitОценок пока нет
- Periradicular Lesions (Chapter 5)Документ28 страницPeriradicular Lesions (Chapter 5)revlieeОценок пока нет
- Journal of Clinical InvestigationДокумент20 страницJournal of Clinical InvestigationSaul MachicadoОценок пока нет
- Pathology Assignment 2Документ5 страницPathology Assignment 2MahaaaОценок пока нет
- Oxidative Stress and Inflammation in The Liver: John J. Lemasters and Hartmut JaeschkeДокумент14 страницOxidative Stress and Inflammation in The Liver: John J. Lemasters and Hartmut JaeschkeLeonard LeonardОценок пока нет
- Dendritic Cell Therapy PDFДокумент12 страницDendritic Cell Therapy PDFგიორგი ანთაძეОценок пока нет
- Acute Pneumonia: Richard T. Ellison III and Gerald R. DonowitzДокумент30 страницAcute Pneumonia: Richard T. Ellison III and Gerald R. DonowitzNilay ChatterjeeОценок пока нет
- Cells at Work Analysis FormatДокумент3 страницыCells at Work Analysis FormatHomer LaguadorОценок пока нет
- 6 Helpful Ways To Boost Immune HealthДокумент6 страниц6 Helpful Ways To Boost Immune HealthDennis Noel BejerОценок пока нет
- Crohn 1 EspДокумент8 страницCrohn 1 EspRomina GonzálezОценок пока нет
- VETM 3004-LECTURE#2 Cells of The Immune System: Lecturer: Shirene M. Singh Date: Friday 6 September, 2019 Time: 8-9 AmДокумент30 страницVETM 3004-LECTURE#2 Cells of The Immune System: Lecturer: Shirene M. Singh Date: Friday 6 September, 2019 Time: 8-9 Ampainx7Оценок пока нет
- Laboratory - Week 4 (Cytokines, in Vitro Phagocytosis)Документ8 страницLaboratory - Week 4 (Cytokines, in Vitro Phagocytosis)rennel ybarolaОценок пока нет
- Alteration of Host Cell Behavior by PathogensДокумент7 страницAlteration of Host Cell Behavior by PathogensAbhijit SatpatiОценок пока нет
- UntitledДокумент334 страницыUntitledLocalVet TunariОценок пока нет
- 4life Transfer Factor: Which Product Is Right For Me?Документ1 страница4life Transfer Factor: Which Product Is Right For Me?jhimsyОценок пока нет
- Nutrition: Basic Nutritional InvestigationДокумент7 страницNutrition: Basic Nutritional InvestigationAndriana VilijencovaОценок пока нет
- Macrophage and Osteoblast Response To Micro and Nano Hydroxyapatite - A ReviewДокумент13 страницMacrophage and Osteoblast Response To Micro and Nano Hydroxyapatite - A Reviewnano_journalОценок пока нет
- Patogenesis TBДокумент46 страницPatogenesis TBJaya Semara PutraОценок пока нет
- 1 &2. Acute Inflammation..Документ140 страниц1 &2. Acute Inflammation..Asmara SyedОценок пока нет
- Inflammation: Cardinal Signs of InflammationДокумент9 страницInflammation: Cardinal Signs of InflammationGeoffreyОценок пока нет
- Pathophysiology of Typhoid FeverДокумент3 страницыPathophysiology of Typhoid FeverinadweguiaОценок пока нет
- Stevens Immuno Sero Answer Key 1Документ19 страницStevens Immuno Sero Answer Key 1Henry ChenОценок пока нет